Simple Summary
The role of p53 immunohistochemistry (IHC) in predicting disease progression in prostate cancer (PCa) was investigated, revealing an unmet need to better understand the interpretation of p53 nuclear expression. This study was conducted at the DC VA Medical Center and involved 84 patients (majority self-identified as African American) with PCa diagnosed between 1996 and 2021. Nuclear expression of p53 was scored in various specimens according to the intensity (0, 1+, 2+, 3+) and percentage (0%, <1%, 1–5%, >5%) of p53-positive tumor cells. In total, 40% of patients were found to have p53 expression, with 21% showing maximum intensity (3+). Maximum intensity was significantly associated with a higher Grade Group (p < 0.001), elevated PSA levels at the time of biopsy (p < 0.001), biochemical recurrence (p < 0.001), and metastasis (p < 0.001). Notably, only patients who developed metastatic disease were found to have maximum p53 intensity. This study underscores the importance of evaluating p53 nuclear intensity, in addition to percentage p53 positivity, to predict disease progression in PCa.
Abstract
Background: Next-generation sequencing has revealed TP53 alterations in localized prostate cancer (PCa), suggesting growing clinical potential for p53 immunohistochemistry (IHC). Prior research supports the use of IHC for the detection of p53 overexpression to predict the presence of TP53 alterations known to be associated with adverse outcomes. However, to reach a consensus definition of p53 overexpression in PCa, further insights are needed. This study aimed to compare two fundamental approaches of evaluating p53 expression across a variety of specimens regarding PCa progression. Methods: This study included 84 patients (75% self-identified as African American) diagnosed with PCa between 1996 and 2021 at the DC VA Medical Center. Representative sections of core biopsies, radical prostatectomies, transurethral prostate resections, and metastatic deposits were examined. p53 nuclear expression was scored according to the highest intensity observed (0, 1+, 2+, 3+) and the percentage (0%, <1%, 1–5%, >5%) of tumor cells expressing any level of intensity in the aggregate tumor area. All slides were reviewed by two independent pathologists. Pertinent clinical data were collected. Results: A total of 34 patients (40%) exhibited p53 nuclear expression, of which 18 (21%) showed the maximum (3+) intensity. The presence of maximum intensity, regardless of percentage, was found to be associated with Grade Group (p < 0.001), higher PSA at biopsy (p < 0.001), BCR (p < 0.001) and metastasis (p < 0.001). Importantly, maximum p53 intensity was identified only in patients who developed metastatic disease. Conclusions: Maximum (3+) p53 nuclear intensity of any percentage is highly associated with disease progression in PCa, suggesting that optimal determination of p53 overexpression should incorporate intensity.
Keywords:
prostate cancer; p53; TP53; biomarker; immunohistochemistry; African American; progression 1. Introduction
Prostate cancer (PCa) remains the most commonly diagnosed non-cutaneous cancer among men in the United States and the second leading cause of cancer-related death [1]. However, the clinical outcome is variable, from indolent to aggressive disease that is metastatic at time of presentation [2,3]. Although many patients experience a relatively protracted clinical course, a distinct subset of patients, even when diagnosed early, succumb to their disease prematurely. Historically, the challenge for clinicians has been to better risk-stratify patients in hopes of avoiding either under- or overtreatment both at the time of diagnosis and/or after follow-up interventions [4]. Despite extensive research to identify biomarkers in PCa, few studies have garnered significant clinical traction to address this unmet, yet critical, need [5,6].
The p53 protein mediates tumor suppression functions by regulating DNA repair, cell cycle arrest, apoptosis, autophagy, homeostasis, and cell senescence [7]. Accumulating nuclear p53 as a result of DNA damage activates genes that initiate cell cycle arrest and p53-mediated apoptosis. As such, functioning p53 is crucial for maintaining genomic integrity and preventing malignant transformation. TP53 is found to be altered in over 50% of human cancers, which has been causatively linked to both cancer initiation and progression, including the promotion of metastatic disease [8]. Increased utilization of next-generation sequencing (NGS) has revealed the presence of recurrent alterations in TP53 in approximately 6–7% of patients with localized PCa and up to 50% of patients with advanced disease [9,10,11]. However, observed rates of TP53 alterations in PCa vary, as indicated by a report of racial differences in TP53, where mutations occurred less frequently in African American males versus those of European descent [12]. Although the exact impact of specific TP53 alterations in PCa remains to be determined, loss of tumor-suppressive functions of wild-type p53 and mutant p53 gain of function have been described, including direct cross-talk between p53 and androgen receptor signaling pathways [13,14]. Prior studies have shown an association between TP53 alterations in primary prostate tumors and disease recurrence and progression [15,16,17,18,19,20]. Moreover, the presence of mutations in TP53 in PCa is associated with shorter overall survival [21].
Therefore, determining a patient’s TP53 mutational status is prognostically relevant in PCa. However, sequencing every tissue specimen is neither desirable nor an optimal use of resources. p53 immunohistochemistry (IHC) has been shown to be a good surrogate marker for underlying mutations in TP53 [22,23,24,25]. We have shown before that in radical prostatectomy (RP) specimens from patients with PCa, high levels of p53 nuclear expression was suggestive of the presence of pathogenic TP53 alterations, and, together with lymphovascular invasion (LVI) status, enhances the early prognostication of PCa progression and development of metastatic disease [26]. Thus, p53 IHC staining is a conceivable, cost-effective screening tool for molecular testing, as in other malignancies [27]. While guidelines for interpreting aberrant p53 expression exist in other tumors, a broad consensus is currently lacking in PCa, necessitating further investigation [28,29]. Although some studies have used the percentage of p53 nuclear expression as a threshold for overexpression, others have prioritized nuclear intensity or a combination of both [16,22,26,30,31,32]. Hence, before such a biomarker can be routinely implemented in PCa, a tumor-specific standard for p53 overexpression is necessary. Therefore, this study aims to compare two fundamental approaches for assessing p53 nuclear expression across a range of specimen sources with regard to PCa progression, in an effort to achieve a more optimal interpretation of p53 IHC findings.
2. Methods and Materials
2.1. Patient Selection
We randomly selected 84 patients diagnosed with PCa between 1996 and 2021 at the Washington DC Veterans Affairs Medical Center (DC VAMC). The resulting cohort reflects a representative cross-section of patients receiving care at this single VA facility. Patients were included if adequate formalin-fixed paraffin-embedded (FFPE) tumor tissue was available. Clinical information, including age, race/ethnicity, Gleason score, Grade Group, PSA at time of biopsy, development of biochemical recurrence (BCR), disease stage at diagnosis, and development of metastatic disease, was retrieved. Localized low risk was defined as AJCC stage I, locally advanced disease as AJCC stage II and III, and metastatic disease as AJCC stage IV. This study was approved by the DC VAMC Institutional Review Board IRBNet#1651999 on 28 October 2021.
2.2. Tumor Tissue Selection
Representative sections of random (non-targeted) prostate core biopsies, RPs, transurethral resections of prostate (TURPs), and distant metastatic deposits were included. A representative formalin fixed paraffin-embedded (FFPE) block from each patient was selected. Index (dominant) tumors from aforementioned specimens were selected upon histological examination of hematoxylin and eosin (H&E) slides.
2.3. Immunohistochemistry
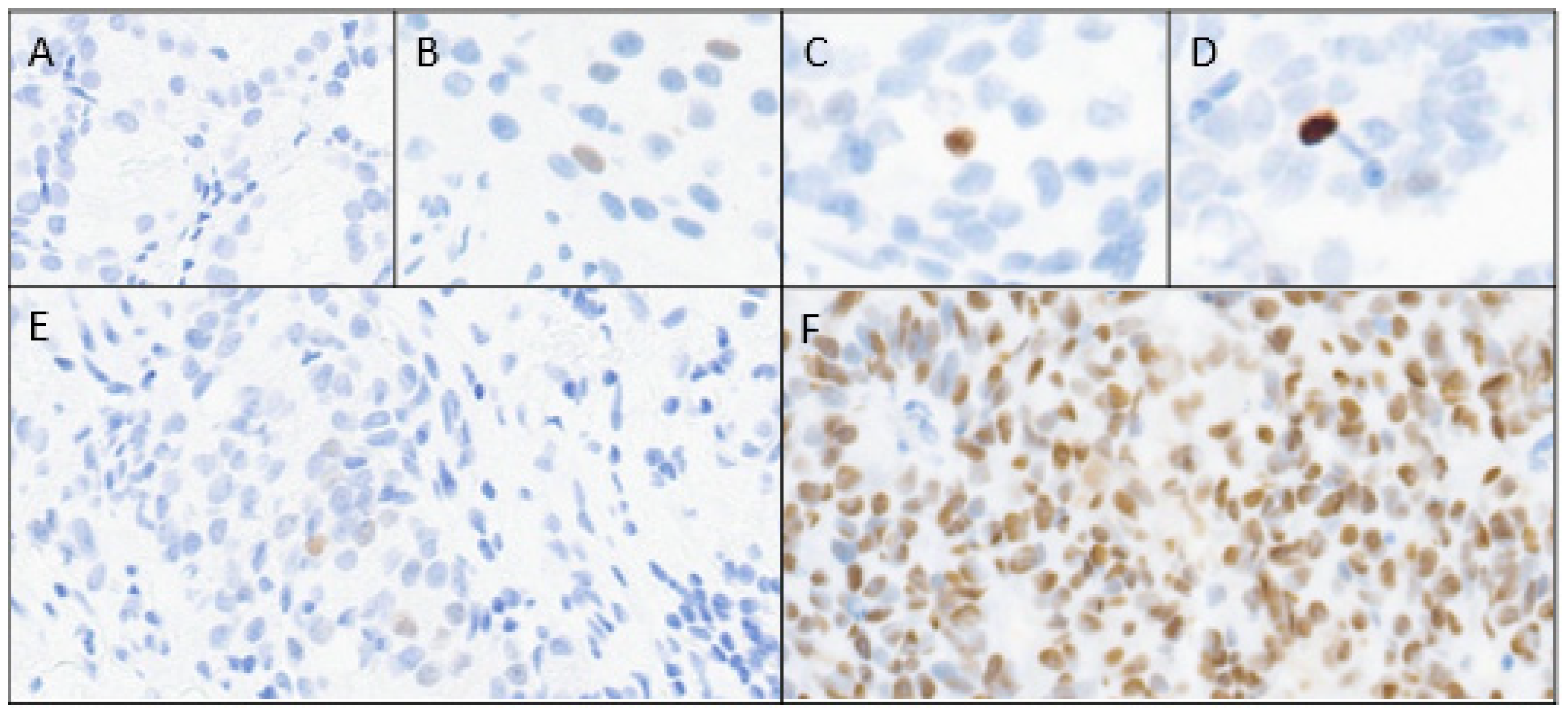
Consecutive four-micron-thick unstained tumor sections were prepared for immunostaining with p53 (anti-p53 mouse monoclonal antibody DO-7, Biocare Medical, Pacheco, CA, USA), and anti-podoplanin antibody (D2-40, Biocare Medical) was used to identify LVI. Selected slides were also stained with CD34 (QBEND 10, Agilent DAKO, Santa Clara, CA, USA) and CD31 (JC70A, Agilent DAKO, Santa Clara, CA, USA) to determine LVI. p53 nuclear expression was manually scored according to the highest intensity observed (0 absent, 1+ light, 2+ medium, or 3+ maximum) and the percentage of tumor cells expressing any level of intensity of the aggregate index tumor area (0%, <1%, 1–5%, and >5%) at 200× magnification (Figure 1).
Figure 1.
p53 nuclear expression scoring; intensity (A–D) and percentage (E,F) of tumor. (A) 0 (absent); (B) 1+ (light); (C) 2+ (medium); (D) 3+ (maximum); (E) ≤5%; (F) >5%.
A p53 range of >5% or less was applied based on results from a prior study [26]. Rare cases with exclusive cytoplasmic staining were considered negative, equivalent to “absent” or “0%” p53 expression. LVI was considered positive when tumor cells were identified within spaces lined by the endothelium, delineated by anti-podoplanin (D2-40), CD31 or CD34 immunoreactivity. All slides were reviewed independently by two pathologists (W.R.G, V.E.N) who were blinded to the clinical data. Discrepancies between the two pathologists were resolved by consensus.
2.4. Mutational Analysis
DNA NGS was performed on FFPE tissue at Foundation Medicine or at our institution to identify TP53 alterations in a subset of patients with metastatic disease. Results were available for a select number of patients (n = 29).
2.5. Statistical Analysis
Descriptive statistics are reported for demographics and clinical characteristics. For continuous variables, mean and standard deviation (SD) are reported if they are normally distributed. Otherwise, mean, and interquartile range (IQR) are reported. For categorical variables, frequency and percentage are reported. Chi-square tests or Fisher’s exact tests (when the expected count was <5) were used to evaluate the association between p53 intensity and categorical variables, including race/ethnicity, D2-40 LVI positivity, Gleason score, Total Gleason Score, Grade Group, BCR, development of metastatic disease, and presence of TP53 mutations. Two-sample t-tests were used to evaluate the association between p53 intensity and variables including age and PSA at diagnosis. The statistically significant level of all the tests was set to 0.05. All statistical analyses were performed using R Statistical Software (version 4.2.2).
3. Results
Relevant clinical data, such as the following, were available for analysis from a total of 84 patients, including index tumors: 50 core biopsies, 14 RPs, 7 TURPs, and 13 metastatic deposits. Demographic information and clinical characteristics are shown in Table 1.

Table 1.
Patients’ demographic and clinical characteristics, stratified by p53 staining intensity.
The mean age at diagnosis for the complete cohort was 64.1 years (SD 7.48 years), and 63 out of the 84 patients (75%) self-identified as African American. In total, 16 patients (19.1%) were found to have Grade Group 1 disease, 19 patients (22.6%) Grade Group 2, 4 patients (4.8%) Grade Group 3, 20 patients (23.8%) Grade Group 4, and 12 patients (14.3%) Grade Group 5. For 13 patients (15.5%), the Grade Group was not applicable due to the convention of not grading metastatic foci. The median PSA at the time of biopsy was 11.6 ng/mL (IQR 6.35–73.60). The median time of follow-up was 6.2 years for all patients.
The dynamic range of p53 immunohistochemical signals observed in tumor nuclei at various percentages of expression is shown in Table 2.

Table 2.
p53 nuclear IHC expression profile in metastatic and non-metastatic disease categories.
In general, the intensity of the signal was associated with the percentage of expression and with the Grade Group of the tumor. All patients with >5% p53 expression of the tumor showed at least one malignant nucleus with maximum (3+) intensity. Overall, 34 tumors (40% of all tumors) exhibited p53 nuclear expression, of which 18 (21.4% of all tumors) showed maximum (3+) intensity regardless of the percentage of positive nuclei. Of these 18 tumors, 4 were obtained from patients with locally advanced (AJCC stage II or III) PCa at the time of diagnosis, and 13 were obtained from those with de novo metastatic disease after further work-up (Table 1). When the percentage of positive nuclei was considered as well, 7 out of the 18 tumors (39%) with maximum (3+) intensity were found to have expression detected in at least 5% of tumor cells. Notably, 11 of 18 (61%) patients with maximum (3+) intensity displayed immunoreactivity in less than 5% of tumor cells. The presence of maximum (3+) intensity p53 expression was not associated with the type of specimen (core biopsy, RP, TURP, or distant metastatic deposit) (Table 1; p = 0.468).
No statistical differences were observed between the presence or absence of maximum (3+) p53 staining and age at diagnosis or ethnicity (Table 1). Importantly, a significant difference was observed between Grade Group and p53 intensity (p < 0.001). Maximum (3+) expression for p53 was associated with a higher Grade Group, and all cases with maximum (3+) intensity were Grade Group 3 or higher. In contrast, patients with low expression of p53 (1+ or 2+ intensity) were more frequently in a lower Grade Group (1 or 2). In addition, maximum (3+) intensity for p53 was associated with a higher PSA level at the time of biopsy (p < 0.001). While patients with a maximum (3+) p53 intensity showed a median PSA level of 172 ng/mL (IQR 26.19–700), the value was 8.30 ng/mL (IQR 6.10–20.20) for patients with less-than-maximum p53 intensity. In line with these results, the occurrence of BCR in patients without metastatic disease at diagnosis was more frequent with a maximum (3+) intensity of p53 (27.8% vs. 22.7%, p < 0.001). When using maximum (3+) intensity as the sole criterion for p53 overexpression, a significant difference was observed between metastatic and non-metastatic patients. Specifically, 18 out of 46 (39%) tumors from patients with metastasis on biopsy, or those who developed metastatic disease, were positive for maximum (3+) p53 staining, compared to 0 out of 38 (0%) tumors from patients without metastatic disease (p < 0.001) (Table 2). Interestingly, when maximum (3+) p53 intensity was combined with expression in greater than 5% of tumor cells to determine overexpression, the difference between the two groups remained significant (p = 0.015). However, the percentage of p53 overexpressed metastatic tumors was reduced to 15% (7 out of 46 tumors). Importantly, maximum (3+) p53 staining was identified only in patients who were diagnosed with, or eventually developed, metastatic disease.
TP53 sequencing data were available for 29 patients, 27 with metastatic disease and 2 without. A total of 12 mutations in TP53 were identified in 10 patients. Corresponding TP53 sequencing data with IHC results are shown in Table 3.

Table 3.
TP53 mutation and p53 IHC pattern in patients with prostate cancer.
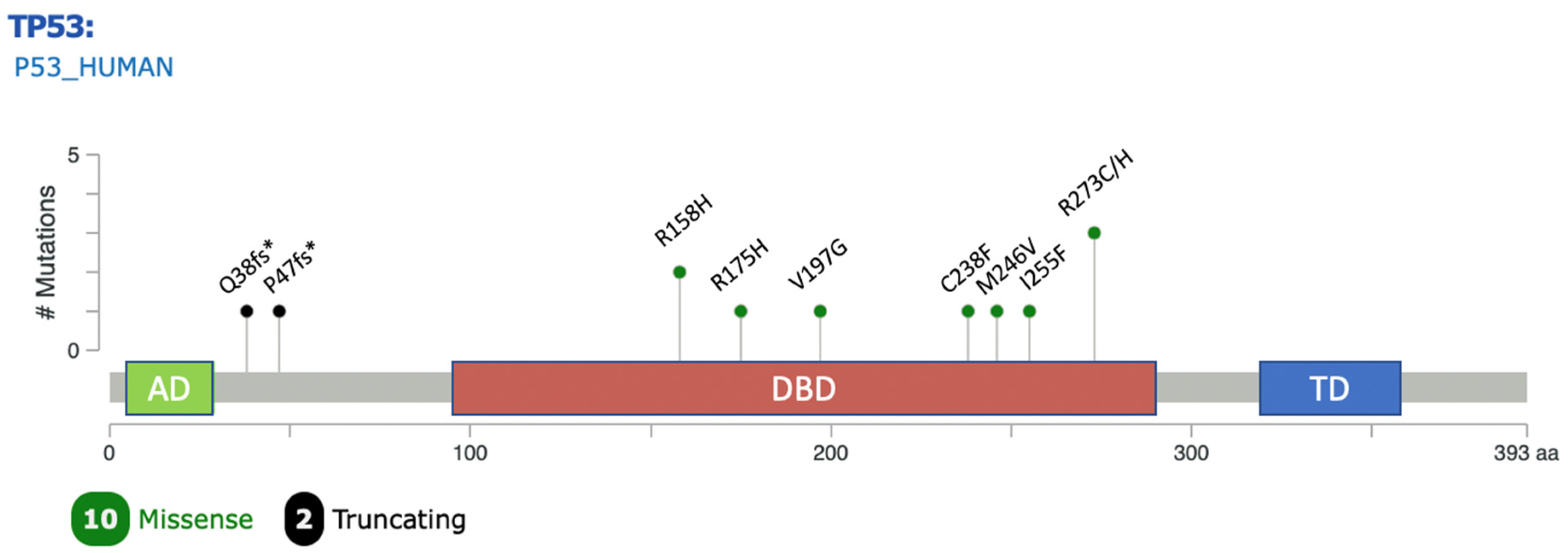
All alterations were observed in tumor specimens from patients who were diagnosed with, or eventually developed, metastatic disease. The majority of mutations (10/12) were missense variants located in the DNA-binding domain of TP53 (Figure 2).
Figure 2.
Lollipop plot showing position and frequency of mutations in TP53 observed in the study across protein domains. Plot generated using the Mutation Mapper tool in cBioportal [33]. AD: transactivation domain; DBD: DNA binding domain; TD: tetramerization domain.
The other two mutations observed in two patients were frameshift deletions in the N-terminal domain resulting in truncated p53 (null mutations) that failed to be recognized by the antibody we used. Interestingly, almost all patients with an in-frame missense TP53 variant showed maximum (3+) intensity by IHC, and the majority expressed p53 in over 5% of tumor cells. Indeed, only one patient with the missense R273H showed an absence of p53 expression (score 0), which could be explained by the extremely low variant allelic frequency (0.13%) observed. Statistical analysis revealed a significant association between the presence of a missense TP53 variant and maximum (3+) IHC intensity (p < 0.01) in the mutated subset (Table 4). This significant association persisted when the level of p53 expression was present in greater than 5% of tumor cells (p < 0.01). Due to the limited number of sequenced tumors, we cannot definitively conclude whether maximum (3+) IHC intensity can be a surrogate for the presence of TP53 mutations. However, our data demonstrate that the presence of missense mutations is significantly associated with maximum (3+) p53 expression on IHC.

Table 4.
Association between TP53 mutational status and p53 nuclear IHC expression profile. For the analysis, the two patients with a frameshift deletion were excluded as this resulted in a null mutation.
In summary, the presence of maximum (3+) p53 nuclear expression, regardless of percentage, was found to be significantly associated with a higher Grade Group (p < 0.001), higher PSA at the time of biopsy (p < 0.001), the development of BCR (p < 0.001) and metastatic disease (p < 0.001). Moreover, the presence of missense mutations in TP53 was found to be significantly associated with the presence of maximum (3+) p53 intensity, even when the percentage of tumor cells was less than 5%.
4. Discussion
The tumor suppressor TP53 is one of the most frequently mutated genes in malignant tumors and has been found to be crucial for tumor initiation, progression and metastasis [34]. Although alterations in TP53 were initially thought to be late events in PCa oncogenesis and associated with androgen resistance, deep molecular profiling of metastatic castration-sensitive PCa and even localized PCa highlighted the existence of recurrent genomic alterations in TP53 as well [31,35,36]. Conveniently, IHC can be used as an acceptable surrogate to identify TP53 alterations. However, a lack of standardization along with variability in prior study designs has hampered the implementation of p53 IHC as a prognostic marker and screening tool in PCa.
In the present study, two fundamentally different, and commonly applied, approaches to assess p53 nuclear expression were evaluated as predictors of PCa progression, namely intensity (0, 1+, 2+, 3+) observed and percentage (0%, <1%, 1–5%, and >5%) of tumor cells expressing any level of intensity. We observed that the presence of maximum (3+) p53 nuclear intensity by IHC was significantly correlated with predictors of worse outcomes (Grade Group, Gleason score, higher PSA level at diagnosis, and development of BCR and metastasis) regardless of the percentage of p53 nuclear expression. While prior studies did not always share the same methodology for evaluating p53 expression in PCa, many, if not most, consistently showed that “positive”, “overexpressed”, “altered”, or “aberrant” p53 expression is associated with more aggressive disease, which is consistent with our findings [16,26,37,38]. Studies that lack this association tend to use overly restrictive criteria for labeling p53 expression as being overexpressed [39,40]. Due to the prostate being a less cellularly active organ compared to ovaries, for example, it is prudent to conclude that the percentage threshold for p53 immunoreactivity is inherently lower as well, as p53 activity tends to be directly correlated with proliferation rate [41,42].
The intensity of p53 on IHC proved to be strongly associated with disease progression, more so than percent tumor expression. This result can at least be partially explained by sampling, as the majority of our specimens represented random core biopsies, which may underestimate overall p53 expression. RP specimens are likely superior for estimating the true percentage of aberrant p53 expression, as they are more representative of the lesion and minimize sampling bias [43]. However, core biopsies usually provide the primary diagnosis, and using p53 intensity may be useful to predict worse outcome independently of percent tumoral expression, as suggested previously [32]. Our observation that maximum nuclear intensity was detected only in patients with metastatic disease at diagnosis, or patients who would develop metastatic disease during follow-up, highlights the potential of this marker to inform us about the severity and likelihood of the progression of disease independently of other pathology-related factors. Although the number of patients in this study is too small to arrive at a definitive conclusion, these findings suggest that detecting maximum (3+) p53 nuclear intensity should raise concerns that the patient has, or will develop, advanced disease during follow-up.
Furthermore, recognition of maximum (3+) p53 nuclear intensity by IHC, regardless of percent tumoral positivity, appears to be a practical approach that may benefit the routine practice of surgical pathology. In our study, concordant p53 expression levels for maximum nuclear intensity reached 94% of cases between our two pathologists, who have varying degrees of experience (>25 years and <5 years). Discrepancies were resolved with follow-up consensus in 100% of cases. In contrast, exact determination of percent expression over a range of intensities would likely place unacceptable demands on routine clinical practice unless automated imaging analysis is introduced. However, when a single numerical percentage cut-off of >5% was applied, concordance for this criterion increased to greater than 90%. In the future, automated computer analysis of digitalized pathology images may circumvent the current limitations of inter-observer variability and labor-intensive estimation of tumor expression to better evaluate tumoral p53 expression in PCa, which is known to be focal and variable.
We showed that conducting a manual estimation of p53 nuclear expression using the primary criterion of maximum (3+) p53 nuclear intensity is a feasible and practical approach. Owing to the focal nature of p53 expression, we conclude that in day-to-day practice, optimal screening of PCa with p53 IHC should not be limited to the index tumor alone, and should ideally include examination of additional higher grade tumor foci. Of note is that the absence of p53 nuclear expression in tissue specimens other than RP should not by itself automatically raise concerns of a possible TP53 deletion (null mutation) owing to the aforementioned focal expression of p53. However, a complete absence of p53 expression in RP specimens, after careful review in cases with higher grade (GG4, GG5) lesions, may raise the possibility of a null TP53 mutation (frameshift, truncating mutations). Moreover, prior research has shown that prostate tumors can be completely negative for p53 IHC staining, yet still harbor underlying TP53 mutations [37]. Although the incidence of these “silent” mutations is small and their impact is unclear, they do highlight the limitations of p53 IHC. A proposed interpretation of p53 nuclear expression in PCa, shown in Table 5, considers the aforementioned observations from this study.

Table 5.
Proposed interpretation of p53 IHC expression in prostate cancer. Null p53 expression not accounted for in either RP (A) or non-RP (B) specimens. (A) Interpretation of IHC p53 expression profile in radical prostatectomy specimens. (B) Interpretation of IHC p53 expression profile in non-radical prostatectomy specimens.
As alluded to earlier, our study is limited by its skewed representation of tissue sources examined (i.e., majority core biopsies) and its moderate sample size, which possibly also explains the lack of statistical significance of LVI in our cohort. The fact that p53 IHC nuclear expression, even with a moderate sample size, was highly associated with disease progression speaks to its overall weight and importance. Other limitations include the retrospective nature of this study and pathology review performed by two pathologists with a close working history. Another important weakness worth discussing is the integrity of RP specimens. As is common practice, RP specimens are quartered to fit an entire cross-section on standardized glass slides. This practical consideration complicates the evaluation of the overall percentage of p53 expression when a tumor spans multiple glass slides, resulting in possible over- or underestimation. Careful and precise percentage estimation is more accurate when performed on whole-mount slides. However, the use of whole-mount processed RP specimens, in general, is limited. In this sense, our review of quartered RP specimens can be viewed as a strength as it more accurately reflects the reality most pathologists face in everyday practice. In terms of sequencing data, molecular testing is heavily skewed towards patients who have developed metastatic disease and lacks the ability for comprehensive testing of negative or low-expressing p53 tumors. A final weakness of our study involves its lumping of cytoplasmic p53 expression together with the negative category. While extremely rare in PCa, the biologic implications of cytoplasmic expression is not well understood [44,45]. Topics not specifically addressed are the issues of null p53 expression and how to select cases deserving of p53 IHC staining. With regard to the latter, further studies are needed to identify patients who may benefit the most from incorporating this biomarker. Hypothetically, patients classified as having Grade Group 3 disease and/or belonging to the intermediate risk category could qualify for p53 IHC to improve the stratification of these historically challenging groups of patients.
The fact that our cohort is predominantly composed of patients who identified as African American could be seen as both a strength and a limitation. Most prior studies reviewing p53 IHC in PCa have had inversed proportions of African American and Caucasian patients, raising questions about the prevalence of p53 IHC expression in this minority population [12,46,47]. One study did observe that TP53 is less frequently altered in African American patients when compared to patients of European ancestry [33,48]. Interestingly, we found no difference in p53 expression (intensity or percentage) between African American patients and other ethnicities included in our cohort, suggesting that p53 may be a valid biomarker for this minority population.
5. Conclusions
Maximum (3+) p53 nuclear intensity is a valuable prognostic marker of PCa progression, regardless of percentage positivity and independent of specimen source. Therefore, p53 overexpression, as characterized in this study, may serve as a useful screening tool for improved risk stratification and optimized patient care in a subset of patients.
Author Contributions
Conceptualization, W.R.G. and V.E.N.; methodology, C.J.L., R.R., M.J. and V.E.N.; formal analysis, S.L. and G.D.; investigation, W.R.G., C.J.L., M.J. and V.E.N.; data curation, C.J.L.; writing—original draft preparation, W.R.G.; writing—review and editing, W.R.G., M.M.D., C.J.L., R.R., M.J. and V.E.N.; visualization, C.J.L.; supervision, M.J. and V.E.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially supported by Prostate Cancer Foundation (PCF) grant 19VALO01.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Washington DC VA Medical Center (IRBNet#1651999, 28 October 2021).
Informed Consent Statement
Patient consent was waived due to de-identification of published materials.
Data Availability Statement
Data are contained within the article.
Acknowledgments
We thank Lyvouch Filkoski for the excellent technical assistance.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Siegel, R.L.; Miller, K.D.; Wagle, N.S.; Jemal, A. Cancer statistics, 2023. CA Cancer J. Clin. 2023, 73, 17–48. [Google Scholar] [CrossRef] [PubMed]
- Hamdy, F.C.; Donovan, J.L.; Lane, J.A.; Metcalfe, C.; Davis, M.; Turner, E.L.; Martin, R.M.; Young, G.J.; Walsh, E.I.; Bryant, R.J.; et al. Fifteen-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer. N. Engl. J. Med. 2023, 388, 1547–1558. [Google Scholar] [CrossRef] [PubMed]
- Litwin, M.S.; Tan, H.-J. The Diagnosis and Treatment of Prostate Cancer: A Review. JAMA 2017, 317, 2532–2542. [Google Scholar] [CrossRef]
- Nagata, M.; Tanimoto, T.; Kami, M. Quality-of-life effects of prostate-specific antigen screening. N. Engl. J. Med. 2012, 367, 1861–1862. [Google Scholar] [CrossRef]
- Farha, M.W.; Salami, S.S. Biomarkers for prostate cancer detection and risk stratification. Ther. Adv. Urol. 2022, 14, 17562872221103988. [Google Scholar] [CrossRef]
- Chen, J.-Y.; Wang, P.-Y.; Liu, M.-Z.; Lyu, F.; Ma, M.-W.; Ren, X.-Y.; Gao, X.-S. Biomarkers for Prostate Cancer: From Diagnosis to Treatment. Diagnostics 2023, 13, 3350. [Google Scholar] [CrossRef]
- Ozaki, T.; Nakagawara, A. Role of p53 in Cell Death and Human Cancers. Cancers 2011, 3, 994–1013. [Google Scholar] [CrossRef]
- Olivier, M.; Hollstein, M.; Hainaut, P. TP53 mutations in human cancers: Origins, consequences, and clinical use. Cold Spring Harb. Perspect. Biol. 2010, 2, a001008. [Google Scholar] [CrossRef]
- Quigley, D.A.; Dang, H.X.; Zhao, S.G.; Lloyd, P.; Aggarwal, R.; Alumkal, J.J.; Foye, A.; Kothari, V.; Perry, M.D.; Bailey, A.M.; et al. Genomic Hallmarks and Structural Variation in Metastatic Prostate Cancer. Cell 2018, 174, 758–769. [Google Scholar] [CrossRef]
- Robinson, D.; Van Allen, E.M.; Wu, Y.-M.; Schultz, N.; Lonigro, R.J.; Mosquera, J.-M.; Montgomery, B.; Taplin, M.-E.; Pritchard, C.C.; Attard, G.; et al. Integrative clinical genomics of advanced prostate cancer. Cell 2015, 161, 1215–1228. [Google Scholar] [CrossRef]
- Cancer Genome Atlas Research Network. The Molecular Taxonomy of Primary Prostate Cancer. Cell 2015, 163, 1011–1025. [Google Scholar] [CrossRef] [PubMed]
- Mahal, B.A.; Alshalalfa, M.; Kensler, K.H.; Chowdhury-Paulino, I.; Kantoff, P.; Mucci, L.A.; Schaeffer, E.M.; Spratt, D.; Yamoah, K.; Nguyen, P.L.; et al. Racial Differences in Genomic Profiling of Prostate Cancer. N. Engl. J. Med. 2020, 383, 1083–1085. [Google Scholar] [CrossRef] [PubMed]
- Navone, N.M.; Troncoso, P.; Pisters, L.L.; Goodrow, T.L.; Palmer, J.L.; Nichols, W.W.; Eschenbach, A.C.V.; Conti, C.J. p53 Protein Accumulation and Gene Mutation in the Progression of Human Prostate Carcinoma. JNCI 1993, 85, 1657–1669. [Google Scholar] [CrossRef]
- Alimirah, F.; Panchanathan, R.; Chen, J.; Zhang, X.; Ho, S.-M.; Choubey, D. Expression of Androgen Receptor Is Negatively Regulated By p53. Neoplasia 2007, 9, 1152–1159. [Google Scholar] [CrossRef]
- Heidenberg, H.B.; Sesterhenn, I.A.; Gaddipati, J.P.; Weghorst, C.M.; Buzard, G.S.; Moul, J.W.; Srivastava, S. Alteration of the tumor suppressor gene p53 in a high fraction of hormone refractory prostate cancer. J. Urol. 1995, 154, 414–421. [Google Scholar] [CrossRef]
- Bauer, J.J.; Sesterhenn, I.A.; Mostofi, K.F.; McLeod, D.G.; Srivastava, S.; Moul, J.W. p53 nuclear protein expression is an independent prognostic marker in clinically localized prostate cancer patients undergoing radical prostatectomy. Clin. Cancer Res. 1995, 1, 1295–1300. [Google Scholar]
- Moul, J.W.; Bettencourt, M.C.; Sesterhenn, I.A.; Mostofi, F.K.; McLeod, D.G.; Srivastava, S.; Bauer, J.J. Protein expression of p53, bcl-2, and KI-67 (MIB-1) as prognostic biomarkers in patients with surgically treated, clinically localized prostate cancer. Surgery 1996, 120, 159–166. [Google Scholar] [CrossRef]
- Bauer, J.J.; Sesterhenn, I.A.; Mostofi, F.K.; McLeod, D.G.; Srivastava, S.; Moul, J.W. Elevated levels of apoptosis regulator proteins p53 and bcl-2 are independent prognostic biomarkers in surgically treated clinically localized prostate cancer. J. Urol. 1996, 156, 1511–1516. [Google Scholar] [CrossRef]
- Nyquist, M.D.; Corella, A.; Coleman, I.; De Sarkar, N.; Kaipainen, A.; Ha, G.; Gulati, R.; Ang, L.; Chatterjee, P.; Lucas, J.; et al. Combined TP53 and RB1 Loss Promotes Prostate Cancer Resistance to a Spectrum of Therapeutics and Confers Vulnerability to Replication Stress. Cell Rep. 2020, 31, 107669. [Google Scholar] [CrossRef]
- Hamid, A.A.; Gray, K.P.; Shaw, G.; MacConaill, L.E.; Evan, C.; Bernard, B.; Loda, M.; Corcoran, N.M.; Van Allen, E.M.; Choudhury, A.D.; et al. Compound Genomic Alterations of TP53, PTEN, and RB1 Tumor Suppressors in Localized and Metastatic Prostate Cancer. Eur. Urol. 2019, 76, 89–97. [Google Scholar] [CrossRef]
- Maddah, M.M.; Hedayatizadeh-Omran, A.; Moosazadeh, M.; Alizadeh-Navaei, R. Evaluation of the Prognostic Role of TP53 Gene Mutations in Prostate Cancer Outcome: A Systematic Review and Meta-Analysis. Clin. Genitourin Cancer 2024, 22, 102226. [Google Scholar] [CrossRef] [PubMed]
- Guedes, L.B.; Almutairi, F.; Haffner, M.C.; Rajoria, G.; Liu, Z.; Klimek, S.; Zoino, R.; Yousefi, K.; Sharma, R.; De Marzo, A.M.; et al. Analytic, Preanalytic, and Clinical Validation of p53 IHC for Detection of TP53 Missense Mutation in Prostate Cancer. Clin. Cancer Res. 2017, 23, 4693–4703. [Google Scholar] [CrossRef] [PubMed]
- Kluth, M.; Harasimowicz, S.; Burkhardt, L.; Grupp, K.; Krohn, A.; Prien, K.; Gjoni, J.; Haß, T.; Galal, R.; Graefen, M.; et al. Clinical significance of different types of p53 gene alteration in surgically treated prostate cancer. Int. J. Cancer 2014, 135, 1369–1380. [Google Scholar] [CrossRef] [PubMed]
- Stopsack, K.H.; Salles, D.C.; Vaselkiv, J.B.; Grob, S.T.; Mucci, L.A.; Lotan, T.L. p53 Immunohistochemistry to Identify Very High-risk Primary Prostate Cancer: A Prospective Cohort Study with Three Decades of Follow-up. Eur. Urol. Oncol. 2023, 6, 110–112. [Google Scholar] [CrossRef]
- Hall, M.C.; Navone, N.M.; Troncoso, P.; Pollack, A.; Zagars, G.K.; von Eschenbach, A.C.; Conti, C.J.; Chung, L.W. Frequency and characterization of p53 mutations in clinically localized prostate cancer. Urology 1995, 45, 470–475. [Google Scholar] [CrossRef]
- Gesztes, W.; Schafer, C.; Young, D.; Fox, J.; Jiang, J.; Chen, Y.; Kuo, H.-C.; Mwamukonda, K.B.; Dobi, A.; Burke, A.P.; et al. Focal p53 protein expression and lymphovascular invasion in primary prostate tumors predict metastatic progression. Sci. Rep. 2022, 12, 5404. [Google Scholar] [CrossRef]
- Orellana, T.J.; Kim, H.; Beriwal, S.; Bhargava, R.; Berger, J.; Buckanovich, R.J.; Coffman, L.G.; Courtney-Brooks, M.; Mahdi, H.; Olawaiye, A.B.; et al. Cost-effectiveness analysis of tumor molecular classification in high-risk early-stage endometrial cancer. Gynecol Oncol. 2022, 164, 129–135. [Google Scholar] [CrossRef]
- Höhn, A.K.; Brambs, C.E.; Hiller, G.G.R.; May, D.; Schmoeckel, E.; Horn, L.-C. 2020 WHO Classification of Female Genital Tumors. Geburtshilfe Frauenheilkd. 2021, 81, 1145–1153. [Google Scholar] [CrossRef]
- Vermij, L.; Léon-Castillo, A.; Singh, N.; Powell, M.E.; Edmondson, R.J.; Genestie, C.; Khaw, P.; Pyman, J.; McLachlin, C.M.; Ghatage, P.; et al. p53 immunohistochemistry in endometrial cancer: Clinical and molecular correlates in the PORTEC-3 trial. Mod. Pathol. 2022, 35, 1475–1483. [Google Scholar] [CrossRef]
- Quinn, D.I.; Stricker, P.D.; Kench, J.G.; Grogan, J.; Haynes, A.-M.; Henshall, S.M.; Grygiel, J.J.; Delprado, W.; Turner, J.J.; Horvath, L.G.; et al. p53 nuclear accumulation as an early indicator of lethal prostate cancer. Br. J. Cancer 2019, 121, 578–583. [Google Scholar] [CrossRef]
- Schlomm, T.; Iwers, L.; Kirstein, P.; Jessen, B.; Köllermann, J.; Minner, S.; Passow-Drolet, A.; Mirlacher, M.; Milde-Langosch, K.; Graefen, M.; et al. Clinical significance of p53 alterations in surgically treated prostate cancers. Mod. Pathol. 2008, 21, 1371–1378. [Google Scholar] [CrossRef] [PubMed]
- Harmon, S.A.; Gesztes, W.; Young, D.; Mehralivand, S.; McKinney, Y.; Sanford, T.; Sackett, J.; Cullen, J.; Rosner, I.L.; Srivastava, S.; et al. Prognostic Features of Biochemical Recurrence of Prostate Cancer Following Radical Prostatectomy Based on Multiparametric MRI and Immunohistochemistry Analysis of MRI-guided Biopsy Specimens. Radiology 2021, 299, 613–623. [Google Scholar] [CrossRef] [PubMed]
- Cerami, E.; Gao, J.; Dogrusoz, U.; Gross, B.E.; Sumer, S.O.; Aksoy, B.A.; Jacobsen, A.; Byrne, C.J.; Heuer, M.L.; Larsson, E.; et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012, 2, 401–404. [Google Scholar] [CrossRef] [PubMed]
- Kastenhuber, E.R.; Lowe, S.W. Putting p53 in Context. Cell 2017, 170, 1062–1078. [Google Scholar] [CrossRef]
- De Laere, B.; Oeyen, S.; Mayrhofer, M.; Whitington, T.; van Dam, P.-J.; Van Oyen, P.; Ghysel, C.; Ampe, J.; Ost, P.; Demey, W.; et al. TP53 Outperforms Other Androgen Receptor Biomarkers to Predict Abiraterone or Enzalutamide Outcome in Metastatic Castration-Resistant Prostate Cancer. Clin. Cancer Res. 2019, 25, 1766–1773. [Google Scholar] [CrossRef]
- Eastham, J.A.; Stapleton, A.M.; Gousse, A.E.; Timme, T.L.; Yang, G.; Slawin, K.M.; Wheeler, T.M.; Scardino, P.T.; Thompson, T.C. Association of p53 mutations with metastatic prostate cancer. Clin. Cancer Res. 1995, 1, 1111–1118. [Google Scholar]
- Griewe, G.L.; Dean, R.C.; Zhang, W.; Young, D.; Sesterhenn, I.A.; Shanmugam, N.; McLeod, D.G.; Moul, J.W.; Srivastava, S. p53 Immunostaining guided laser capture microdissection (p53-LCM) defines the presence of p53 gene mutations in focal regions of primary prostate cancer positive for p53 protein. Prostate Cancer Prostatic Dis. 2003, 6, 281–285. [Google Scholar] [CrossRef]
- Petrescu, A.; Mârzan, L.; Codreanu, O.; Niculescu, L. Immunohistochemical detection of p53 protein as a prognostic indicator in prostate carcinoma. Rom. J. Morphol. Embryol. 2006, 47, 143–146. [Google Scholar]
- Che, M.; DeSilvio, M.; Pollack, A.; Grignon, D.J.; Venkatesan, V.M.; Hanks, G.E.; Sandler, H.M. RTOG Prognostic value of abnormal p53 expression in locally advanced prostate cancer treated with androgen deprivation and radiotherapy: A study based on RTOG 9202. Int. J. Radiat. Oncol. Biol. Phys. 2007, 69, 1117–1123. [Google Scholar] [CrossRef]
- Stattin, P.; Damber, J.E.; Modig, H.; Bergh, A. Pretreatment p53 immunoreactivity does not infer radioresistance in prostate cancer patients. Int. J. Radiat. Oncol. Biol. Phys. 1996, 35, 885–889. [Google Scholar] [CrossRef]
- Verma, R.; Gupta, V.; Singh, J.; Verma, M.; Gupta, G.; Gupta, S.; Sen, R.; Ralli, M. Significance of p53 and ki-67 expression in prostate cancer. Urol. Ann. 2015, 7, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Sasor, A.; Wagrowska-Danilewicz, M.; Danilewicz, M. Ki-67 antigen and P53 protein expression in benign and malignant prostatic lesions. Immunohistochemical quantitative study. Pol. J. Pathol. 2000, 51, 31–36. [Google Scholar] [PubMed]
- Stackhouse, G.B.; Sesterhenn, I.A.; Bauer, J.J.; Mostofi, F.K.; Connelly, R.R.; Srivastava, S.K.; Moul, J.W. p53 and bcl-2 immunohistochemistry in pretreatment prostate needle biopsies to predict recurrence of prostate cancer after radical prostatectomy. J. Urol. 1999, 162, 2040–2045. [Google Scholar] [CrossRef] [PubMed]
- Baptiste, N.; Prives, C. p53 in the cytoplasm: A question of overkill? Cell 2004, 116, 487–489. [Google Scholar] [CrossRef]
- Green, D.R.; Kroemer, G. Cytoplasmic functions of the tumour suppressor p53. Nature 2009, 458, 1127–1130. [Google Scholar] [CrossRef]
- Liu, W.; Zhang, Y.; Wei, S.; Bae, S.; Yang, W.-H.; Smith, G.J.; Mohler, J.L.; Fontham, E.T.H.; Bensen, J.T.; Sonpavde, G.P.; et al. A CD24-p53 axis contributes to African American prostate cancer disparities. Prostate 2020, 80, 609–618. [Google Scholar] [CrossRef]
- Powell, I.J.; Dyson, G.; Land, S.; Ruterbusch, J.; Bock, C.H.; Lenk, S.; Herawi, M.; Everson, R.; Giroux, C.N.; Schwartz, A.G.; et al. Genes associated with prostate cancer are differentially expressed in African American and European American men. Cancer Epidemiol Biomark. Prev. 2013, 22, 891–897. [Google Scholar] [CrossRef]
- Lindquist, K.J.; Paris, P.L.; Hoffmann, T.J.; Cardin, N.J.; Kazma, R.; Mefford, J.A.; Simko, J.P.; Ngo, V.; Chen, Y.; Levin, A.M.; et al. Mutational Landscape of Aggressive Prostate Tumors in African American Men. Cancer Res. 2016, 76, 1860–1868. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).