Simple Summary
The role of microRNAs (miRNAs) as oncological biomarkers has been studied over the past ten years, with largely inconsistent results. In order to help researchers discuss the complexity of the subject and create standardized protocols for future study to combine findings from around the world, this systematic review attempts to collect data regarding the diagnostic power of urinary miRNAs in Renal Cell Carcinoma (RCC).
Abstract
Background and Objective. The significance of microRNAs (miRNAs) in relation to neoplastic diseases; such as renal carcinoma carcinoma (RCC); has been brought to light by recent studies. Analyzing the main urinary miRNAs implicated in RCC and their potential diagnostic use was the goal of this systematic review of the literature. Methods. This systematic review was performed following the PROSPERO protocol CRD42024550716. Our literature search strategies were deciding which database to include (Pubmed; EMBASE and Clinicaltrial.gov) and composing strings with words related to urinary miRNA in patients with RCC. Key findings and limitations. After screening; 10 papers were included from the 593 records that the systematic review found. No miRNA was investigated in more than one paper by different authors. The miR-210 and let-7 family were the most investigated and resulted upregulated in RCC cases compared to controls. Five papers reported different expression of miRNAs in urine samples before and after surgery: miR-15a; miR-34a-5p; miR-200a-3p; miR-205-5p; miR-210; miR-210-3p; miR-365a-3p and let-7d-5p levels decreased after nephrectomy. Meta-analysis was not performed since the included studies were heterogeneous; in terms of studied miRNA; of the normalizer used during stabilization phase; and histologic type of RCC (clear cell RCC; papillary RCC; unspecified RCC). Conclusions. Considering the variability and heterogeneity of the obtained results; as well as the vastness of the topic; expanding research in this field appears highly promising. To support further advancements; it would be useful to establish a database that consolidates international findings.
1. Introduction
Renal cell carcinoma (RCC) is the sixth most common tumor diagnosed in men and the tenth in women. It accounts for 3% of all cancers, with higher incidence in Western countries. In 2022, kidney cancer had an incidence rate of 4.4 new cases per 100,000 individuals worldwide, resulting in a total of 434,000 new diagnoses [1].
RCC ranks thirteenth as a cause of cancer-related mortality worldwide. In all types of RCC, prognosis worsens with stage and histopathological grade. One of the challenges in kidney cancer diagnosis is its silent behavior until advanced stages. Due to the asymptomatic course, especially in the early stages, about 60% of RCC are identified incidentally by abdominal US or CT [2].
Approximately 30% of patients are diagnosed with metastatic disease, underscoring the importance of early detection. Currently, the diagnosis of kidney cancer is predominantly based on radiological imaging such as ultrasound scan, computed tomography (CT) scans and magnetic resonance imaging (MRI). Also, renal mass biopsy can provide information, to characterize the mass and distinguish between benign and malignant lesions, thus guiding appropriate treatment decisions. In recent years, however, a new diagnostic modality has gained attention for its potential in kidney cancer: liquid biopsy. A minimally invasive test, liquid biopsy offers the ability to analyze biomarkers found in peripheral blood and urine, providing valuable insights into tumor characteristics without the need for tissue samples. This approach is particularly promising for diagnosing kidney tumors, determining their histological type, and assessing potential resistance to pharmacological treatments. Liquid biopsy encompasses several key biomarkers, including circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), exosomes, and microRNAs (miRNAs) [3].
The latter are small, non-coding RNAs, typically 21–23 nucleotides long, which regulate gene expression by binding to the 3' untranslated region (3'UTR) of target messenger RNAs (mRNAs). This binding prevents the translation of the mRNA into protein, effectively inhibiting the expression of the gene. MiRNAs play a critical role in regulating key processes such as tumor initiation, invasion, metastasis, and resistance to therapy. Altered miRNA expression profiles have been observed in various cancers, including kidney cancer, making them potential biomarkers for early detection and prognosis. Importantly, circulating miRNAs have been shown to be remarkably stable in bodily fluids, such as blood and urine, making them ideal candidates for non-invasive diagnostic testing. Liquid biopsy, through the analysis of miRNAs and other biomarkers, holds great promise for improving the diagnosis and management of kidney cancer [4].
Liquid biopsy may become a cornerstone of kidney cancer diagnostics, offering significant advantages over traditional methods by enabling earlier, less invasive, and more personalized patient care. The aim of this systematic review was to investigate the most promising urinary miRNAs associated with RCC.
Our primary research question (RQ) is: What urinary miRNA are differentially expressed in adult patients with RCC compared to healthy individuals?
Our secondary RC is: What urinary miRNA expresses different behavior before and after surgery in RCC patients?
2. Material and Methods
The review was performed following the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) 2020 guidelines [5,6] integrated with the Synthesis Without Meta-analysis (SWiM) checklist [7] (Supplementary Tables S1 and S2). The protocol of this systematic review was registered in PROSPERO (CRD42024550716) [8].
We established the following inclusion criteria adhering to the PICO framework (Population, Intervention, Comparator, Outcome).
- -
- Population: Adult (≥18 years old) patients with RCC;
- -
- Intervention: Measurement of circulating or cell-free miRNA in urine samples of patients with RCC;
- -
- Comparator/Control: Healthy subjects or patients with RCC after surgery;
- -
- Outcome (main): Different expression of miRNA in urine samples between patients with RCC and healthy subjects through diagnostic accuracy measurements. Outcome (additional): Different expression of miRNA in urine samples of patients with RCC before and after surgery through diagnostic accuracy measurements.
The types of studies included were prospective cohort studies, randomized controlled trials, cross-sectional studies and case–control studies and case series.
The exclusion criteria were:
- -
- pediatric patients and adult patients with benign renal tumors;
- -
- measurement of RNA other than circulating or cell-free miRNA in blood samples of patients with RCC (snRNA, ccRNA, exosomal RNA, lncRNA…);
- -
- reviews and metanalysis, abstracts, letters and meeting report.
Our literature search strategies were deciding which database to include (Pubmed, EMBASE and Clinicaltrial.gov) and composing strings with words related to urinary miRNA in patients with RCC.
The software Mendeley Desktop [9] was used to import bibliographic citations. Then, the results were exported in a Microsoft Excel spreadsheet used for title/abstract and full text selection [10].
The study selection process was performed by three independent review authors (LG, FP, PM). Initially the reviewers selected the records through the titles and abstracts according to the inclusion criteria. When disagreement incurred, it was solved through discussion and, when necessary, a supervisor (GC, AP) was involved. After that, four other review authors screened the full texts of the potential eligible studies.
Eleven independent reviewers (LG, FP, MR, ES, AV, RLM, FR, PM, MG, LDA, RE) performed data extraction using a table including a list of extracted data. All the reviewers were thoroughly instructed on how to fill the table to secure consistency. Disagreements on data extracted were solved involving a supervisor (GC, AP).
We extracted from each study:
- -
- bibliographic data: first author, publication year and citation;
- -
- study characteristics: study design, country, number of centers, sample size;
- -
- participant characteristics: disease, gender, age;
- -
- intervention characteristics: type of miRNA, dosage method and phase;
- -
- control characteristics: healthy subjects or patients with RCC in other phases;
- -
- study outcomes.
We decided not to perform metanalysis because we expected excessive heterogeneity between studies in matter of type of miRNA, extraction method and normalizers used.
Whereas dichotomous data were aggregated as pooled risk ratio (RR), continuous data were aggregated as mean difference (MD). The inverse variance approach and the random effect model were adopted. We reported 95% confidence intervals.
The risk of bias assessment was performed by two independent reviewers (LG, MR) that received clear instructions for the use of critical appraisal tools, Cochrane Risk of Bias Tool (RoB 2) for RCT and ROBINS-E (Risk Of Bias In Non-Randomized Studies–of Exposure) for non-randomized studies [11]. After conducting a pilot phase to ensure homogeneous evaluation, the records were classified low risk, some concerns, high risk or very high risk.
Certainty assessment was performed by a reviewer (LG) using GRADE (Grading of Recommendations Assessment, Development and Evaluation) method [12]. Since the papers were not comparable because they studied different miRNAs extracted and treated with different methods, we did not evaluate the overall inconsistency but discussed them singularly. We categorized the records in high, moderate, low or very low quality.
3. Results
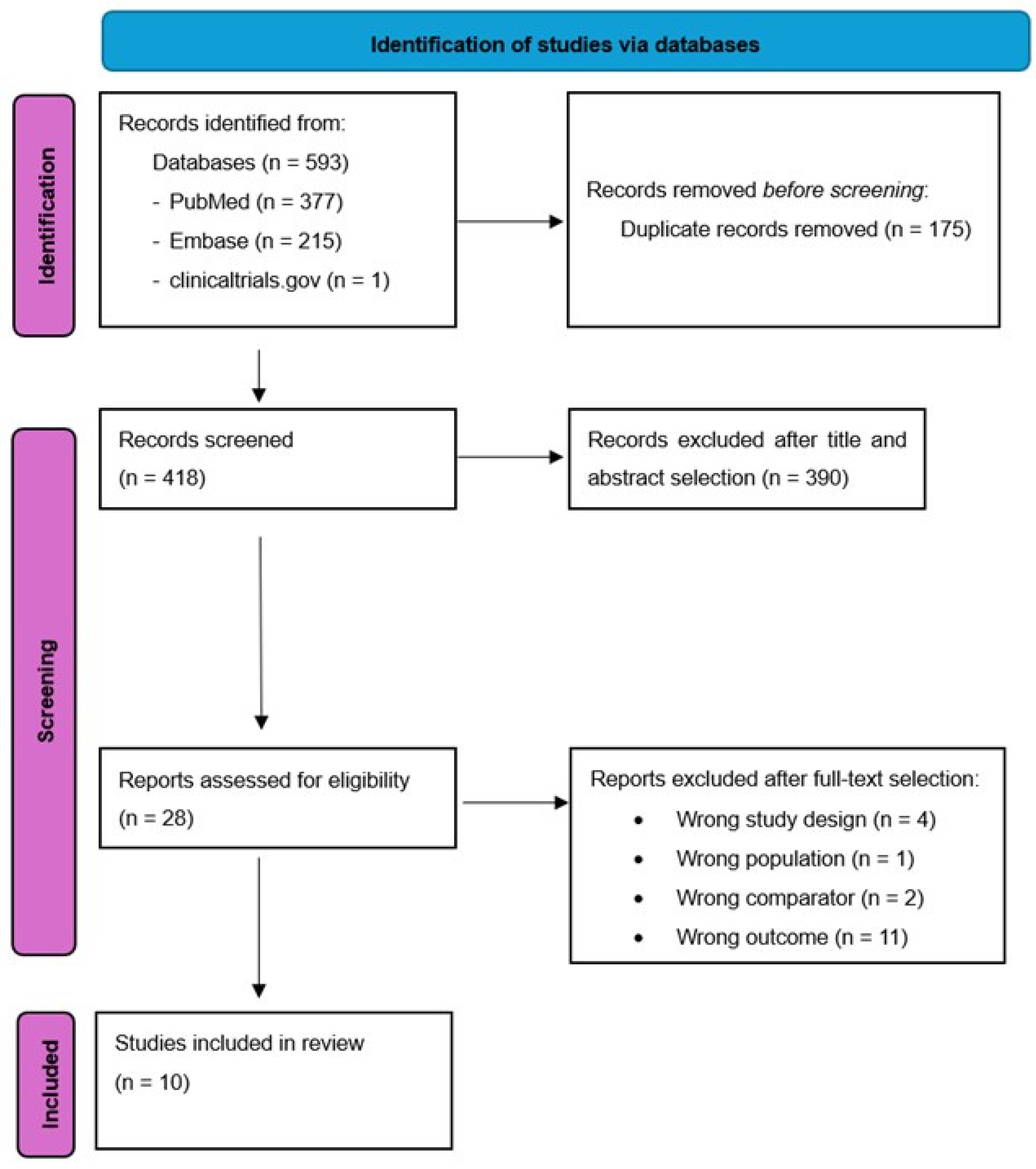
The initial research strategy identified 593 studies (377 from Pubmed, 215 from EMBASE and 1 from Clinicaltrials.gov), 175 of them were duplicates and were excluded. Of the remaining 418 studies, 28 remained after title and abstract selection. On the basis on full text selection, 18 articles were excluded. The remaining 10 were included [13,14,15,16,17,18,19,20,21,22] in the final selection (Figure 1, PRISMA 2020 flow diagram). Supplementary Table S3 lists the excluded studies and the reasons for their exclusion. The primary cause of exclusion was wrong outcome (11 records). Other reasons for exclusion were wrong study design, wrong population and wrong comparator.
Figure 1.
PRISMA 2020 flow diagram.
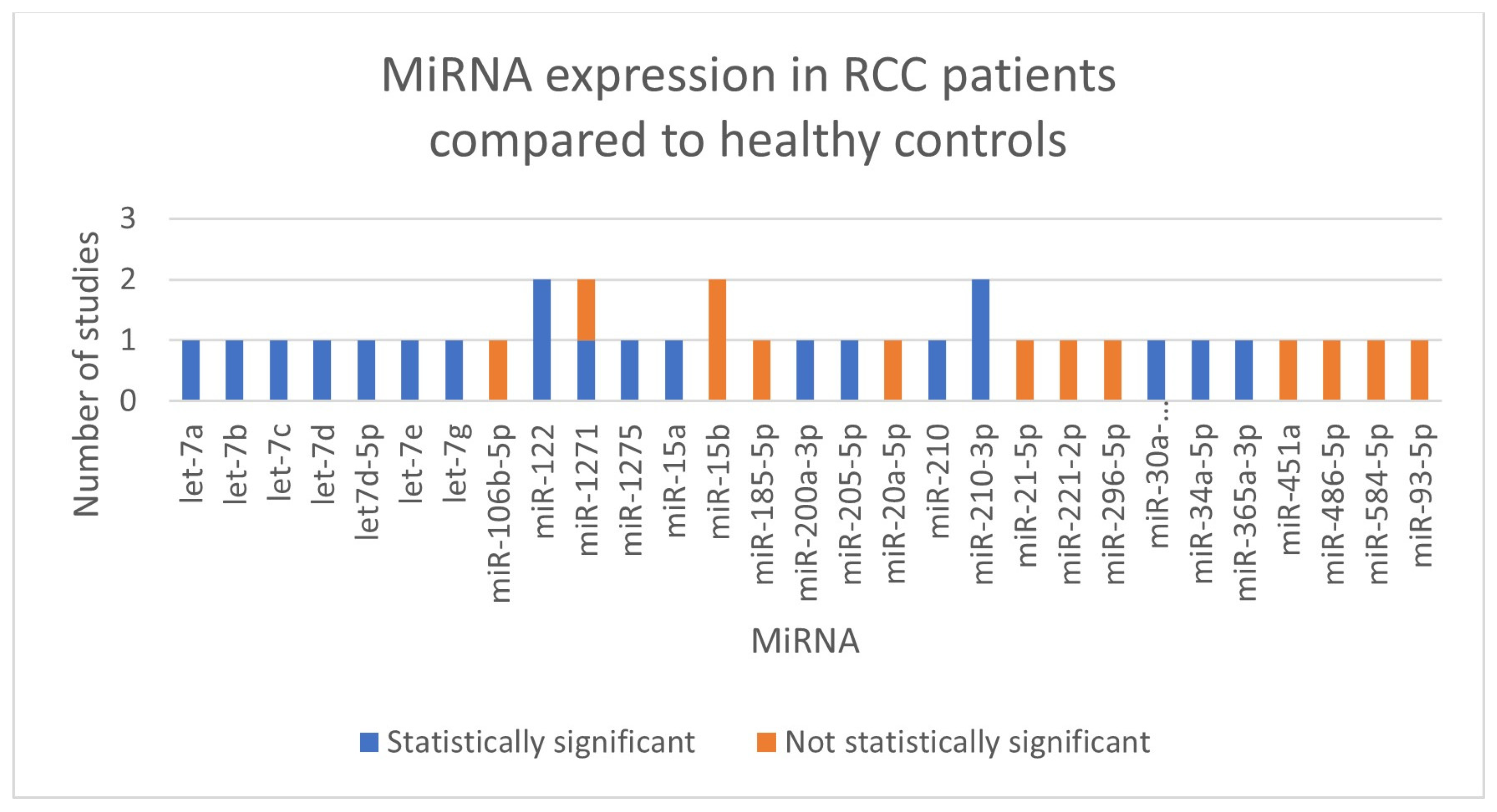
We did not perform meta-analyses because the included studies were not uniform in terms of the kind of RCC (clear cell RCC, papillary RCC, not defined RCC), the normalizer used during the stabilization phase, and the miRNA that was investigated (showed in Figure 2). In Table 1, we outlined the main characteristics and findings of the included studies. Every record that was included was a diagnostic accuracy study.
Figure 2.
Summary of miRNAs expressed in our selection of studies.

Table 1.
Included studies, main characteristics and summarized results. RCC (Renal cell carcinoma); ccRCC (clear cell RCC); pRCC (papillary RCC); chRCC (chromophobe RCC); ↑ (overexpressed); ↓ (underexpressed).
A total of 10 studies, involving 611 patients, investigated expression levels of miRNAs and their diagnostic role in RCC. Following serum extraction, all studies normalized the miRNAs using either endogenous or synthetic controls. Cel-miR-39 was the most often used normalizer.
No miRNA was investigated in more than one paper by different authors, although miR-122, miR-1271-5p, miR-15b-5p and miR-210-3p were studied twice by the same authors [14,15,21,22].
One of the most consistently investigated miRNAs across the records was the miR-210 family, which showed significant upregulation in urine samples from RCC patients, particularly those with clear cell RCC (ccRCC) [17,21,22].
The let-7 family miRNAs (let-7a, let-7b, let-7c, let-7d, let-7d-5p, let-7e, and let-7g), were also frequently investigated [16,19]. The authors found that all let-7 miRNAs levels were significantly elevated in the urine of RCC patients compared to healthy controls.
Another prominent miRNA was miR-122, which was found to be overexpressed in urine samples from ccRCC patients by Cochetti et al. [14,15]. Moreover, the authors developed the diagnostic algorithm 7p-urinary score that analyzed miR-122-5p, miR-1271-5p, and miR-15b-5p and three internal controls to better distinguish between miRNAs expression levels in cases and controls.
Other upregulated miRNAs were miR-15a, miR-30a-5pme, miR-34a-5p, miR-200a-3p, miR-205-5p, miR-365a-3p and miR-1275 [13,18,19,20].
Five papers reported different expression of miRNAs in urine samples before and after surgery: miR-15a, miR-34a-5p, miR-200a-3p, miR-205-5p, miR-210, miR-210-3p, miR-365a-3p and let-7d-5p levels decreased after nephrectomy, highlighting their possible utility in monitoring disease progression or response to treatment [17,18,19,21,22].
Risk of Bias and Certainty Assessment for Included Studies
Since all of the included studies were non-randomized diagnostic accuracy studies, the ROBINS-E tool (Table 2) was used to evaluate the methodological quality [11].

Table 2.
Risk of bias and certainty assessment of included studies. 1—no confounding factors mentioned; 2—small cohort (<200 participants between patients and controls considering all phases of the study).
Five low-risk studies and five records with some concerns of risk were included in the overall risk of bias during the critical appraisal phase. Most studies presented some concerns because no confounding factors were mentioned.
The GRADE tool was used to complete the certainty assessment phase [12]. Non-randomized case–control studies were deemed good quality since all of the research used highly sophisticated laboratory equipment to detect miRNA urine levels objectively.
Studies that included at least 200 patients and controls in each phase were considered sufficient for numerosity because the variable considered were genetic materials. Only one study fulfilled this requirement, and, because of that, it was considered high quality [20]. Out of the remaining articles, five studies were deemed low quality, and four papers were categorized as moderate quality.
4. Discussion
This systematic review, encompassing 10 studies, provides a detailed examination of urinary miRNAs as potential diagnostic biomarkers for RCC, identifying the limitations of studies conducted to date and future prospects for improving the selection of these miRNAs to increase their diagnostic power.
The miR-210 family was the most investigated as urinary biomarker. Both miR-210 and miR-210-3p were upregulated before surgery and down-regulated after surgery. This pattern of expression was noted in both tissue and urine samples, reinforcing the validity of the miR-210 family as a key player in RCC biology and its potential as a biomarker for early detection and follow-up. The miR-210 family is also the most investigated as serum biomarker in the literature [23].
The review revealed a heterogeneous set of miRNAs investigated, indicating that research focuses on a wide range of miRNAs, with the same marker rarely being reported across multiple studies.
Several studies have identified promising urinary miRNAs for noninvasive diagnosis of RCC. Despite variability in results and differences in study designs, populations and methodologies, some key patterns have emerged in terms of the most frequently studied miRNAs and general trends in their expression.
Whereas the miRNAs were not relevantly expressed in RCC patients could be due to fluctuations of urinary levels or laboratory equipment not sensitive enough to lower concentrations. The lack of internationally validated tests for laboratory investigations constituted an obstacle to this research field.
The role of urinary miRNAs as potential biomarker for follow-up in patients after adjuvant therapy has not been addressed in the literature yet, but once reliable miRNAs will be assessed, it could lead to interesting discoveries regarding potential response index to chemotherapy for RCC patients.
Another potential role for urinary miRNAs as predictors of metastases in higher stages of RCC is under investigation: in 2023, one study found that miR-191-5p, miR-324-3p, and miR-186-5p exhibited a strong association with metastasis development in patients with pathological T3 (pT3) tumors [24]. In our selection, only one study evaluated the correlation of urinary level of miRNAs in metastatic patients: urinary miR-30a-5pme levels had an 80% sensitivity, 71% specificity, and 73% accuracy in differentiating patients with metastases (both synchronous and metachronous) from those without metastatic disease [20].
The main strength of our review is that, to our knowledge, it represents the first analysis specifically focused on urinary markers and the diagnosis of ccRCC. Another key strength of our review is the inclusion of rigorous methodological tools, including risk of bias assessment and certainty of evidence evaluation, approaches absent in prior reviews [23,24].
Compared to the review conducted by Aveta et al. [23], that analyzed the urinary miRNAs involved in all urological cancers, we adopted stricter selection criteria concerning circulating or cell-free miRNAs, focusing exclusively on RCC.
When compared to the previous review, our findings align in identifying significant miRNAs in patients with ccRCC, such as miRNA-15a 25, as well as the family of let-7 miRNAs.
Tito et al. also confirmed the role of miRNAs miR-122, miR-1271, miR-15b, and miR-210-3p, presenting results that align with the findings of our review [24].
In light of the latest advancements in RCC diagnosis, our review provides an updated overview of additional miRNAs, including miRNA-210, miR-30a-5p, miRNA-1275, let-7d-5p, miR-205-5p, miR-34a-5p, and miR-365a-3p.
Despite progress, the studies conducted so far have several limitations that restrict their clinical application. First, variability in miRNA extraction and quantification methodologies may affect the reproducibility of results. Second, the small clinical sample sizes used and the lack of large-scale multicenter studies limit the validity of the results obtained. In addition, the biological heterogeneity of RCC and the presence of subtypes with different molecular characteristics further complicate data interpretation.
One of the critical issues that has emerged from the previous systematic reviews published to date on urinary miRNAs is the lack of a specific selection of studies based on the histotype of RCC. This limitation has several important implications.
Indeed, one of the selection criteria of our review was to specifically investigate the diagnostic role of miRNAs in ccRCC. Although this is a methodological limitation in that it narrows the focus of the review, the absence of a specific selection of urinary miRNAs by histotype in previous reviews has led to heterogeneous results that do not accurately reflect biological differences between subtypes [25]. On the other hand, our approach is a strength because it allows for more accurate and targeted results and lays the foundation for validating more specific and reliable biomarkers for diagnosis and follow-up of patients with ccRCC, thus improving the clinical accuracy of these biomarkers.
The main limitations of this review included the limited number of databases considered for study selection and to evaluate only the miRNAs involved in RCC studies, excluding the potential association with other histological types.
Therefore, going forward, further large-scale clinical trials are needed to establish the role of urinary miRNAs as valid and reliable biomarkers. In order to improve future studies on the diagnostic role of miRNAs, the following suggestions could be helpful:
- Collaboration between research centers and clinical institutions is considered essential to validate these biomarkers in different populations and clinical settings.
- Studies evaluating urinary miRNAs multiple times in homogeneous populations could resolve the issue of intraindividual and interindividual fluctuation of miRNA in urine.
- Standardized procedures for data reporting and sample collecting must be created to enhance study comparability, increase the reliability of the results and avoid future inconsistencies among studies.
- Technological advances in miRNAs detection, such as next-generation sequencing and machine learning-based analysis, may increase sensitivity and specificity, improving the viability of miRNA-based diagnostics in standard clinical settings.
- The accuracy of diagnosis may be increased by combining miRNAs with additional biomarkers, such as protein or genetic biomarkers.
- Further studies with longer follow-up of pT3 and pT4 RCC patients would enrich our current knowledge about urinary miRNAs as potential predictors of metastases and response index to adjuvant therapy.
- To reduce risk of bias and increase the quality of future studies, it is crucial to identify and account for relevant confounding factors and apply the analysis to larger, independent cohorts to ensure their generalizability and clinical applicability.
5. Conclusions
Considering the variability and heterogeneity of the obtained results, as well as the vastness of the topic, expanding research in this field appears highly promising. To support further advancements, it would be useful to establish a database that consolidates international findings.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers17081336/s1, Supplementary Table S1: PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist 2020. Supplementary Table S2: SWiM (Synthesis without metanalysis) checklist. Supplementary Table S3: List of full text excluded.
Author Contributions
G.C., A.P. and E.M. conceptualized the review. G.C. and L.G. chose all methodology details. L.G. was in charge of the strings’ computation for literature research and wrote and submitted the PROSPERO protocol. The study selection process was performed by three independent review authors (L.G., F.P. and P.M.). Data extraction was performed by eleven independent reviewers (L.G., F.P., M.R., E.S., A.V., R.L.M., F.R., P.M., M.G., L.D.A., R.E., M.M. and G.V.), while G.C. and A.P. supervised the process. L.G. and M.R. conducted the risk of bias assessment. L.G. performed the certainty assessment. P.M., M.R., E.S. and L.G. wrote the manuscript, while G.C. administered the supervision of the review. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Delahunt, B.; Eble, J.N.; Samaratunga, H.; Thunders, M.; Yaxley, J.W.; Egevad, L. Staging of renal cell carcinoma: Current progress and potential advances. Pathology 2021, 53, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Steliarova-Foucher, E.; Lortet-Tieulent, J.; Rosso, S.; Coebergh, J.W.W.; Comber, H.; Forman, D.; Bray, F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries in 2012. Eur. J. Cancer 2013, 49, 1374–1403. [Google Scholar] [CrossRef] [PubMed]
- Di Meo, A.; Bartlett, J.; Cheng, Y.; Pasic, M.D.; Yousef, G.M. Liquid biopsy: A step forward towards precision medicine in urologic malignancies. Mol. Cancer 2017, 16, 80. [Google Scholar] [CrossRef] [PubMed]
- Figueredo, D.d.S.; Gitaí, D.L.G.; de Andrade, T.G. Daily variations in the expression of miR-16 and miR-181a in human leukocytes. Blood Cells Mol. Dis. 2015, 54, 364–368. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. Supplementary Material to: PRISMA 2020 Explanation and Elaboration: Updated Guidance and Exemplars for Reporting Systematic Reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 2020, 368, l6890. [Google Scholar] [CrossRef]
- Guadagni, L.; Cochetti, G.; Paladini, A.; Russo, M.; Pastore, F.; Saqer, E.; La Mura, R.; Vitale, A.; Ricci, F.; Mangione, P.; et al. Available online: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024550716 (accessed on 8 December 2024).
- Mendeley Ltd. Mendeley Desktop; Mendeley Ltd.: London, UK, 2021; Available online: https://www.mendeley.com/ (accessed on 16 February 2025).
- Microsoft Corporation. Microsoft Excel; Microsoft Corporation: 2018. Available online: https://office.microsoft.com/excel (accessed on 16 February 2025).
- Higgins, J.P.; Morgan, R.L.; Rooney, A.A.; Taylor, K.W.; Thayer, K.A.; Silva, R.A.; Lemeris, C.; Akl, E.A.; Bateson, T.F.; Berkman, N.D.; et al. A tool to assess risk of bias in non-randomized follow-up studies of exposure effects (ROBINS-E). Environ. Int. 2024, 186, 108602. [Google Scholar] [CrossRef]
- Schünemann, H.; Brożek, J.; Guyatt, G.; Oxman, A. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations; The GRADE Working Group: 2013. Available online: https://gdt.gradepro.org/app/handbook/handbook.html (accessed on 1 October 2013).
- Bustos, M.A.; Gottlieb, J.; Choe, J.; Suyeon, R.; Lin, S.Y.; Allen, W.M.; Krasne, D.L.; Wilson, T.G.; Hoon, D.S.; Linehan, J.A. Diagnostic miRNA Signatures in Paired Tumor, Plasma, and Urine Specimens From Renal Cell Carcinoma Patients. Clin. Chem. 2023, 70, 261–272. [Google Scholar] [CrossRef]
- Cochetti, G.; Cari, L.; Nocentini, G.; Maulà, V.; Suvieri, C.; Cagnani, R.; De Vermandois, J.A.R.; Mearini, E. Detection of urinary miRNAs for diagnosis of clear cell renal cell carcinoma. Sci. Rep. 2020, 10, 21290. [Google Scholar] [CrossRef]
- Cochetti, G.; Cari, L.; Maulà, V.; Cagnani, R.; Paladini, A.; Del Zingaro, M.; Nocentini, G.; Mearini, E. Validation in an Independent Cohort of MiR-122, MiR-1271, and MiR-15b as Urinary Biomarkers for the Potential Early Diagnosis of Clear Cell Renal Cell Carcinoma. Cancers 2022, 14, 1112. [Google Scholar] [CrossRef] [PubMed]
- Fedorko, M.; Juracek, J.; Stanik, M.; Svoboda, M.; Poprach, A.; Buchler, T.; Pacik, D.; Dolezel, J.; Slaby, O. Detection of let-7 miRNAs in urine supernatant as potential diagnostic approach in non-metastatic clear-cell renal cell carcinoma. Biochem. Medica 2017, 27, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Zhao, A.; Péoch, M.; Cottier, M.; Mottet, N. Detection of urinary cell-free miR-210 as a potential tool of liquid biopsy for clear cell renal cell carcinoma. Urol. Oncol. Semin. Orig. Investig. 2017, 35, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Mytsyk, Y.; Dosenko, V.; Borys, Y.; Kucher, A.; Gazdikova, K.; Busselberg, D.; Caprnda, M.; Kruzliak, P.; Farooqi, A.A.; Lubov, M. MicroRNA-15a expression measured in urine samples as a potential biomarker of renal cell carcinoma. Int. Urol. Nephrol. 2018, 50, 851–859. [Google Scholar] [CrossRef]
- Oto, J.; Herranz, R.; Plana, E.; Sánchez-González, J.V.; Pérez-Ardavín, J.; Hervás, D.; Fernández-Pardo, Á.; Cana, F.; Vera-Donoso, C.D.; Martínez-Sarmiento, M.; et al. Identification of miR-20a-5p as Robust Normalizer for Urine microRNA Studies in Renal Cell Carcinoma and a Profile of Dysregulated microRNAs. Int. J. Mol. Sci. 2021, 22, 7913. [Google Scholar] [CrossRef]
- Outeiro-Pinho, G.; Barros-Silva, D.; Aznar, E.; Sousa, A.-I.; Vieira-Coimbra, M.; Oliveira, J.; Gonçalves, C.S.; Costa, B.M.; Junker, K.; Henrique, R.; et al. MicroRNA-30a-5pme: A novel diagnostic and prognostic biomarker for clear cell renal cell carcinoma in tissue and urine samples. J. Exp. Clin. Cancer Res. 2020, 39, 98. [Google Scholar] [CrossRef]
- Petrozza, V.; Pastore, A.L.; Palleschi, G.; Tito, C.; Porta, N.; Ricci, S.; Marigliano, C.; Costantini, M.; Simone, G.; Di Carlo, A.; et al. Secreted MiR-210-3p as Non-Invasive Biomarker in Clear Cell Renal Cell Carcinoma. Oncotarget 2017, 8, 69551–69558. [Google Scholar] [CrossRef]
- Petrozza, V.; Costantini, M.; Tito, C.; Giammusso, L.M.; Sorrentino, V.; Cacciotti, J.; Porta, N.; Iaiza, A.; Pastore, A.L.; Di Carlo, A.; et al. Emerging role of secreted miR-210-3p as potential biomarker for clear cell Renal Cell Carcinoma metastasis. Cancer Biomark. 2020, 27, 181–188. [Google Scholar] [CrossRef]
- Aveta, A.; Cilio, S.; Contieri, R.; Spena, G.; Napolitano, L.; Manfredi, C.; Franco, A.; Crocerossa, F.; Cerrato, C.; Ferro, M.; et al. Urinary MicroRNAs as Biomarkers of Urological Cancers: A Systematic Review. Int. J. Mol. Sci. 2023, 24, 10846. [Google Scholar] [CrossRef]
- Tito, C.; De Falco, E.; Rosa, P.; Iaiza, A.; Fazi, F.; Petrozza, V.; Calogero, A. Circulating microRNAs from the Molecular Mechanisms to Clinical Biomarkers: A Focus on the Clear Cell Renal Cell Carcinoma. Genes 2021, 12, 1154. [Google Scholar] [CrossRef]
- von Brandenstein, M.; Schlosser, M.; Herden, J.; Heidenreich, A.; Störkel, S.; Fries, J.W.U. MicroRNAs as Urinary Biomarker for Oncocytoma. Dis. Markers 2018, 2018, 6979073. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).