Dermoscopy of Scalp Melanoma: Report of Three Cases
Abstract
:1. Introduction
2. Observations
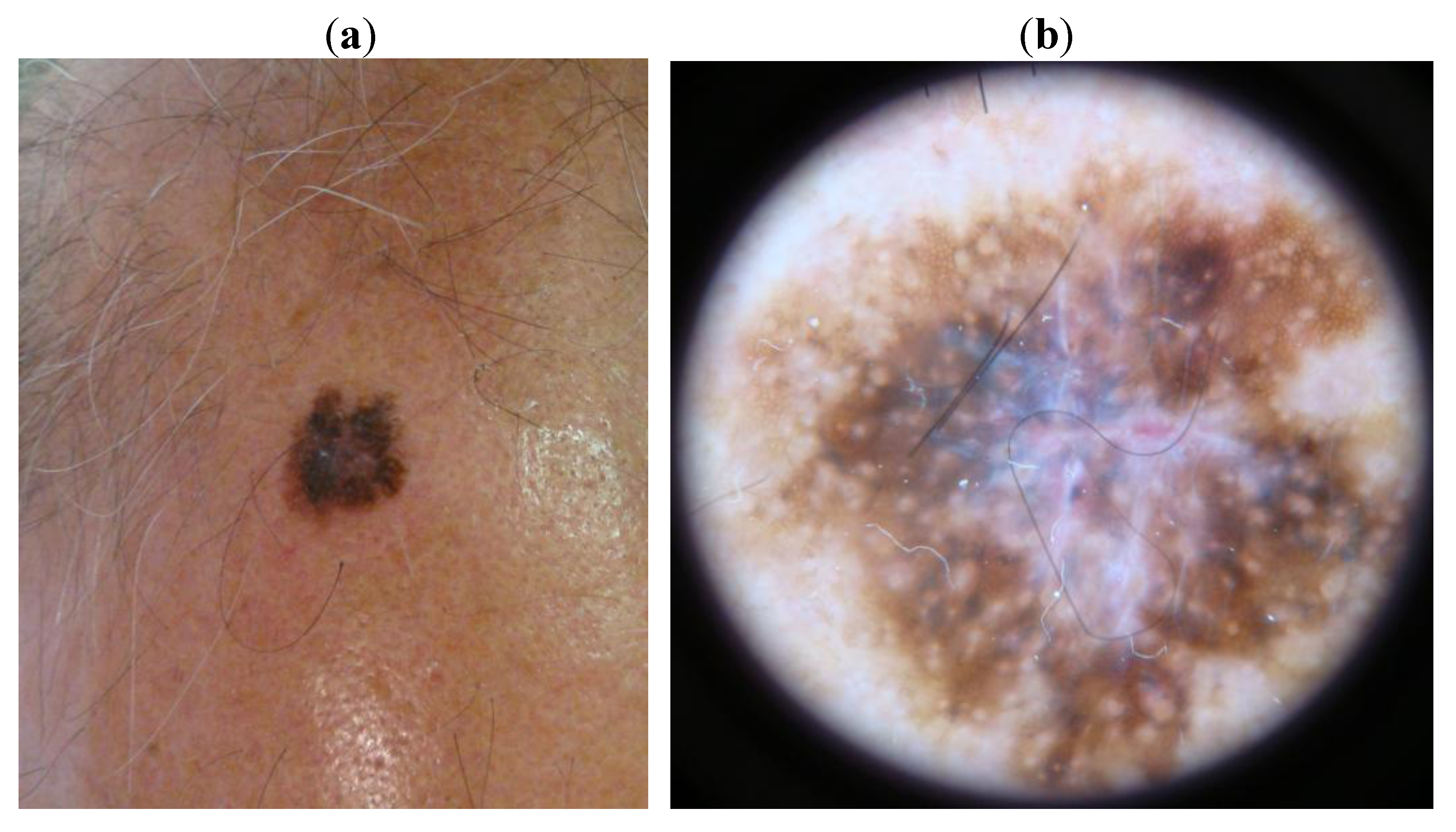
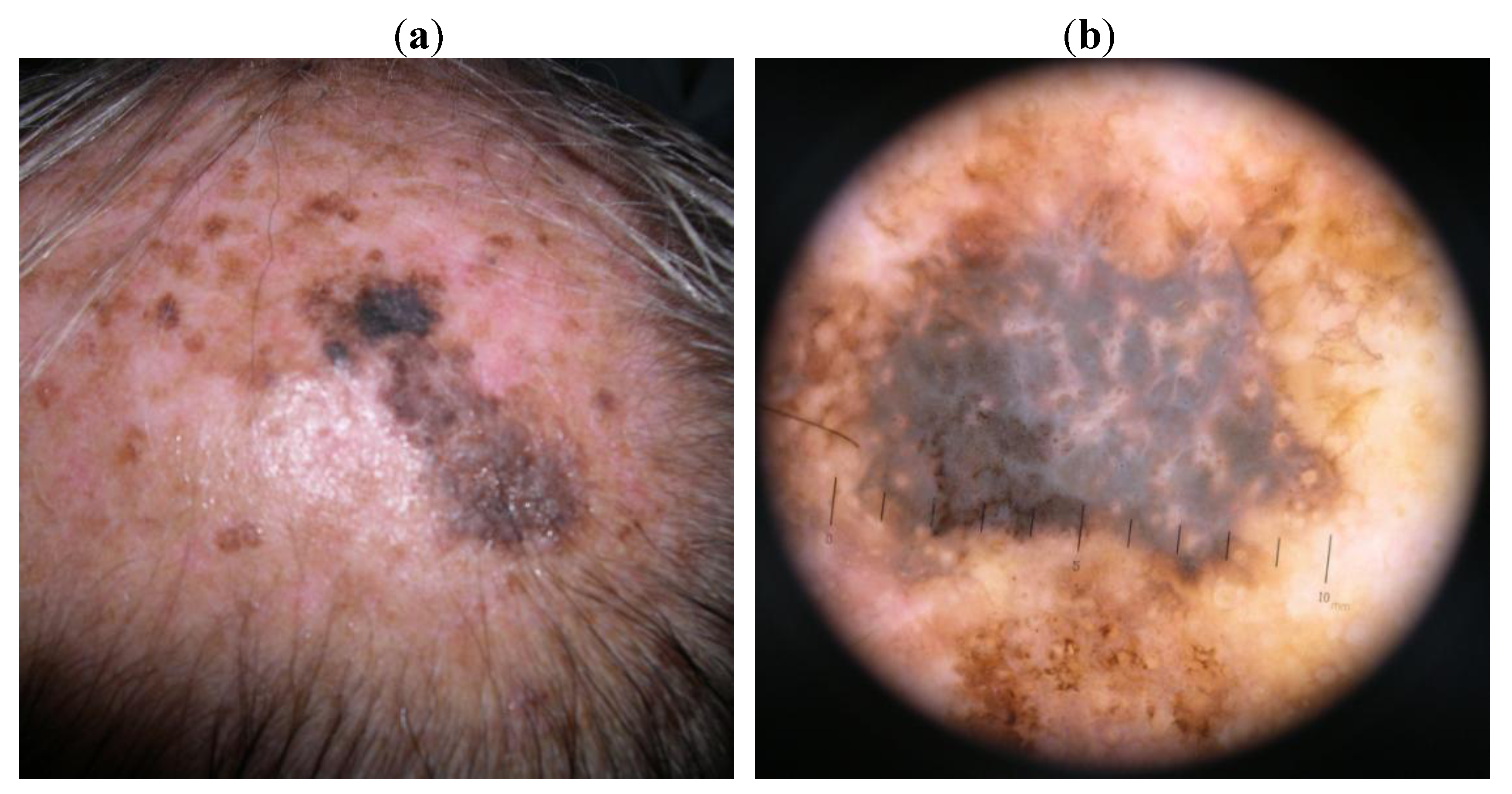

3. Discussion
4. Conclusions
References
- Armstrong, B.K.; Kicker, A. Cutaneous melanoma. Cancer Surv. 1994, 19–20, 219–240. [Google Scholar]
- Greenlee, R.T.; Murray, T.; Bolden, S.; Wingo, P.A. Cancer statistics, 2000. CA Cancer J. Clin. 2000, 50, 7–33. [Google Scholar] [CrossRef]
- Armstrong, B.K.; Kricker, A. The epidemiology of UV induced skin cancer. J. Photochem. Photobio. B, Biol. 2001, 63, 8–18. [Google Scholar]
- Jemal, A.; Siegel, R.; Ward, E.; Hao, Y.; Xu, J.; Thun, M.J. Cancer statistics, 2009. CA Cancer J. Clin. 2009, 59, 225–249. [Google Scholar] [CrossRef]
- Lachiewicz, A.M.; Berwick, M.; Wiggins, C.L.; Thomas, N.E. Survival differences between patients with scalp or neck melanoma and those with melanoma of other sites in the surveillance, epidemiology, and end results (seer) program. Arch. Dermatol. 2008, 144, 515–521. [Google Scholar] [CrossRef]
- Benmeir, P.; Baruchin, A.; Lusthaus, S.; Weinberg, A.; Ad-El, D.; Nahlieli, O.; Neuman, A.; Wexler, M.R. Melanoma of the Scalp: The Invisible Killer. Plast. Reconst. Surg. 1995, 95, 496–500. [Google Scholar] [CrossRef]
- Rigual, N.R.; Cheney, R.T.; Iwenofu, O.H.; Li, Q.; Loree, T.R.; Popat, S.R.; Merzianu, M. Idiosyncrasies of scalp melanoma. Laryngoscope 2007, 117, 1354–1358. [Google Scholar] [CrossRef]
- Phieffer, L.S.; Jones, E.C.; Tonneson, M.G.; Kriegel, D.A. Melanoma of the scalp: an underdiagnosed malignancy? Cutis 2002, 69, 362–364. [Google Scholar]
- Shumate, C.R.; Carlson, G.W.; Giacco, G.G.; Guinee, V.F.; Byers, R.M. The prognostic implications of location for scalp melanoma. Am. J. Surg. 1991, 162, 315–319. [Google Scholar] [CrossRef]
- Friedmann, R.J.; Rigel, D.S.; Silverman, M.; Kopf, AW. The continued importance of the early detection of malignant melanoma. CA Cancer J. Clin. 1991, 41, 201–226. [Google Scholar] [CrossRef]
- Zalaudek, I.; Leinweber, B.; Soyer, H.P.; Petrillo, G.; Brongo, S.; Argenziano, G. Dermoscopic features of melanoma on the scalp. J. Am. Acad. Dermatol. 2004, 51, 88–90. [Google Scholar] [CrossRef]
- Sahin, M.T.; Demir, M.A.; Yoleri, L.; Can, M.; Ozturkcan, S. Blue naevus with satellitosis mimicking malignant melanoma. J. Eur. Acad. Dermatol. Venerol. 2001, 15, 570–573. [Google Scholar]
- Zalaudek, I.; Giacomel, J.S.; Leinweber, B. Scalp Melanoma. In Color Atlas of Melanocytic Lesions of the Skin; Springer-Verlag: Berlin-Heidelberg, Germany, 2007; pp. 265–269. [Google Scholar]
- Florell, S.R.; Boucher, K.M.; Leachman, S.A.; Azmi, F.; Harris, R.M.; Malone, J.C.; Martignoni, G.; Bowen, G.M.; Gerwels, J.W.; Hood, A.F. Histopathologic recognition of involved margins of lentigo maligna excised by staged excision. Arch. Dermatol. 2003, 139, 595–604. [Google Scholar] [CrossRef]
© 2010 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Torres, F.; Fabbrocini, G.; Hirata, S.H.; Yamada, S.; De Vita, V.; Annunziata, M.C.; Tosti, A. Dermoscopy of Scalp Melanoma: Report of Three Cases. Cancers 2010, 2, 1597-1601. https://doi.org/10.3390/cancers2031597
Torres F, Fabbrocini G, Hirata SH, Yamada S, De Vita V, Annunziata MC, Tosti A. Dermoscopy of Scalp Melanoma: Report of Three Cases. Cancers. 2010; 2(3):1597-1601. https://doi.org/10.3390/cancers2031597
Chicago/Turabian StyleTorres, Fernanda, Gabriella Fabbrocini, Sergio Henrique Hirata, Sergio Yamada, Valerio De Vita, Maria Carmela Annunziata, and Antonella Tosti. 2010. "Dermoscopy of Scalp Melanoma: Report of Three Cases" Cancers 2, no. 3: 1597-1601. https://doi.org/10.3390/cancers2031597
APA StyleTorres, F., Fabbrocini, G., Hirata, S. H., Yamada, S., De Vita, V., Annunziata, M. C., & Tosti, A. (2010). Dermoscopy of Scalp Melanoma: Report of Three Cases. Cancers, 2(3), 1597-1601. https://doi.org/10.3390/cancers2031597




