Influence of CAD/CAM Milling and 3D-Printing Fabrication Methods on the Mechanical Properties of 3-Unit Interim Fixed Dental Prosthesis after Thermo-Mechanical Aging Process
Abstract
:1. Introduction
2. Materials and Methods
2.1. Master Model Preparation
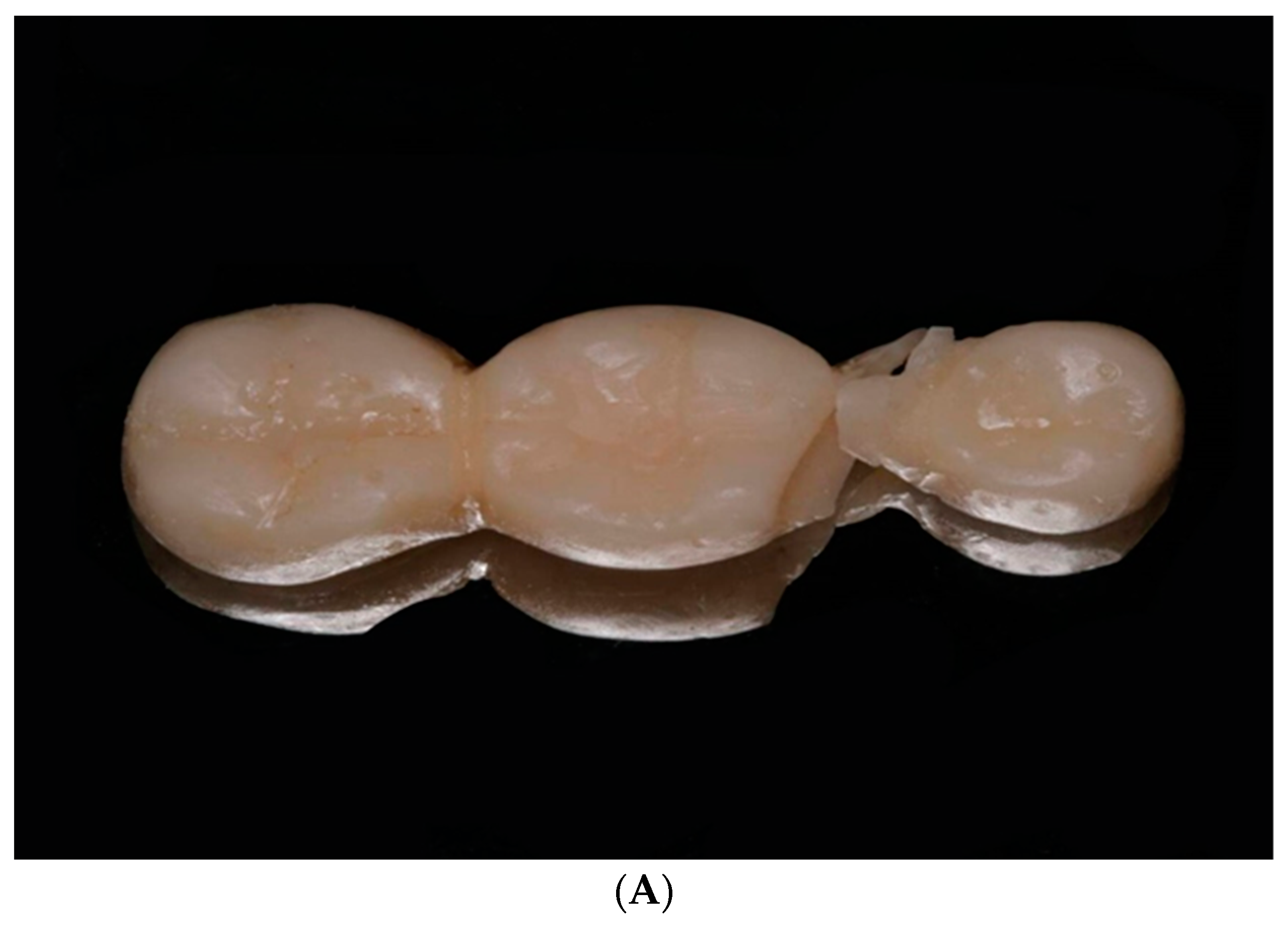
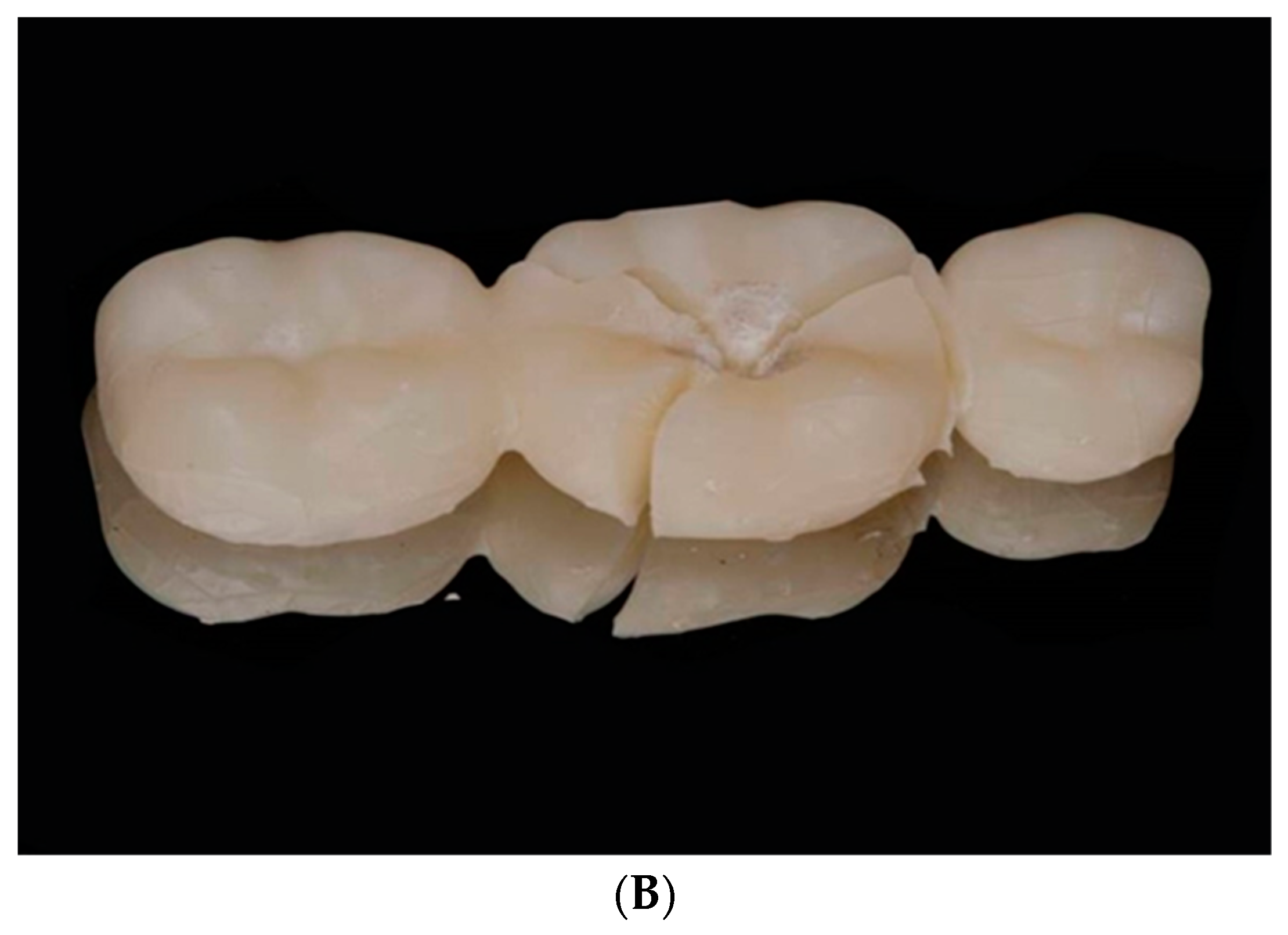
2.2. Fabrication of the Conventional 3-Unit IFDPs
2.3. Fabrication of Milled 3-Unit IFDP
2.4. Fabrication of 3-Printed 3-Unit IFDP by 2 Printing Technologies
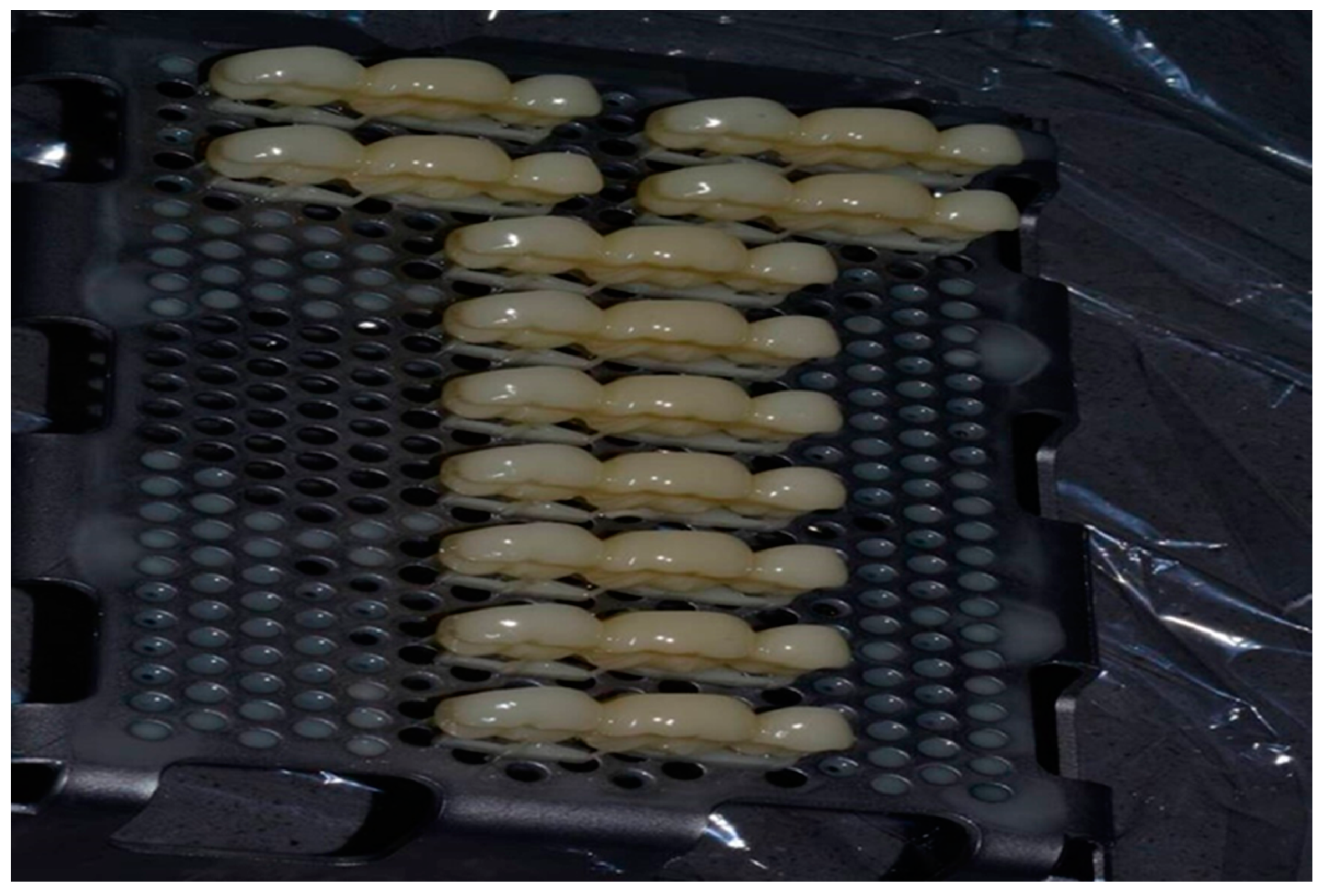
2.5. Thermomechanical Aging of All Study Materials of 3-Unit IFDP
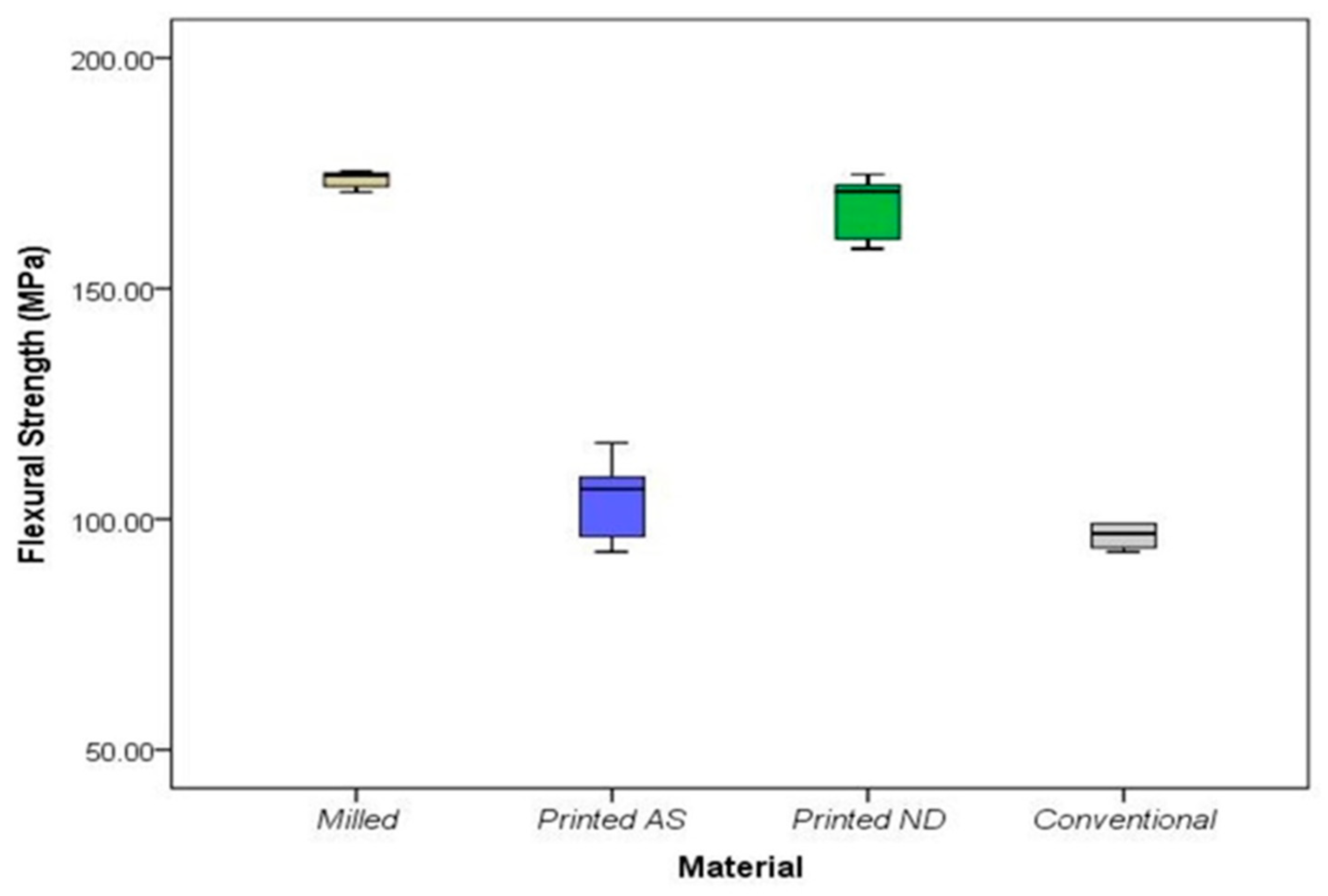
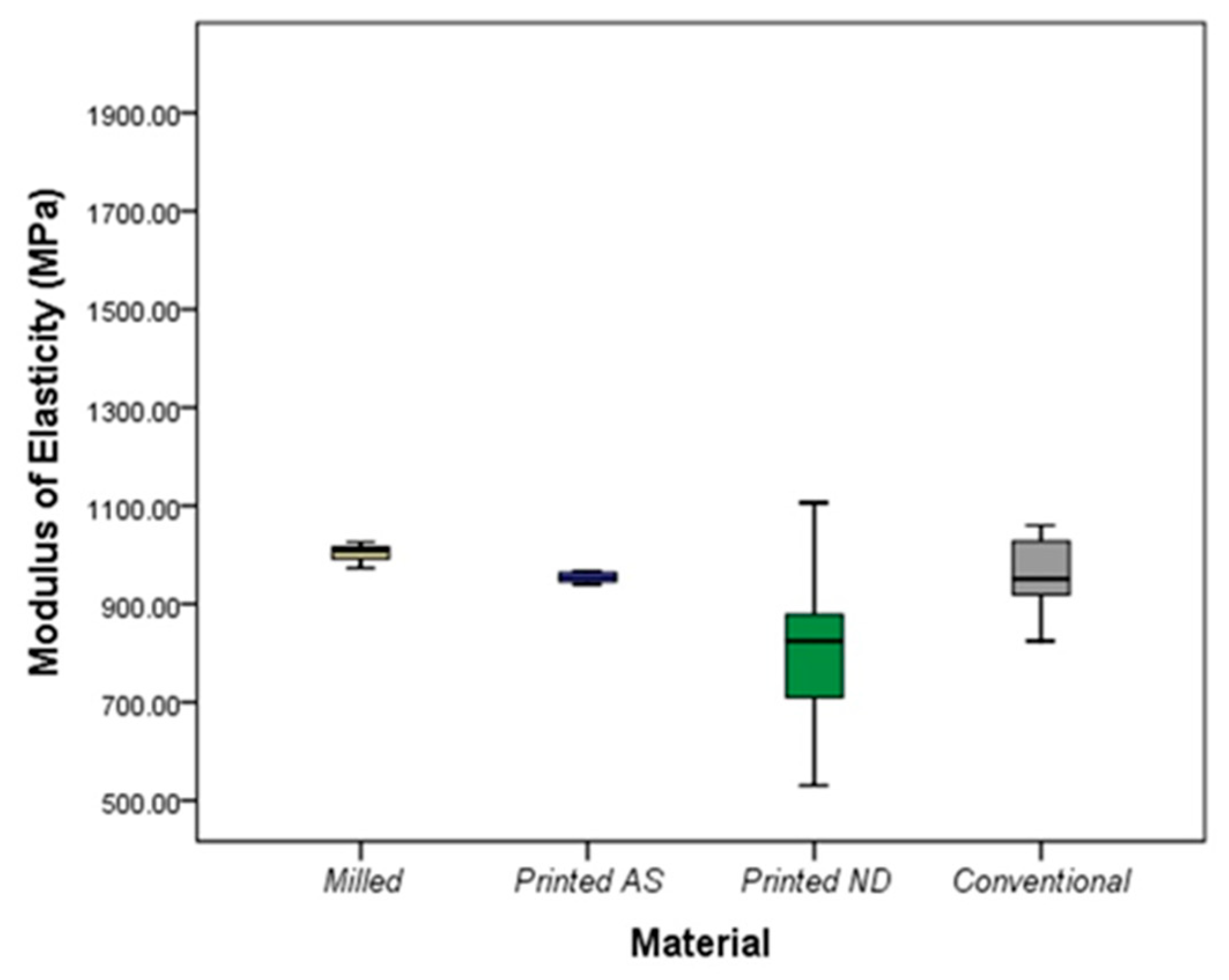
2.6. Flexural Strength and Elastic Modulus of 3-Unit IFDP
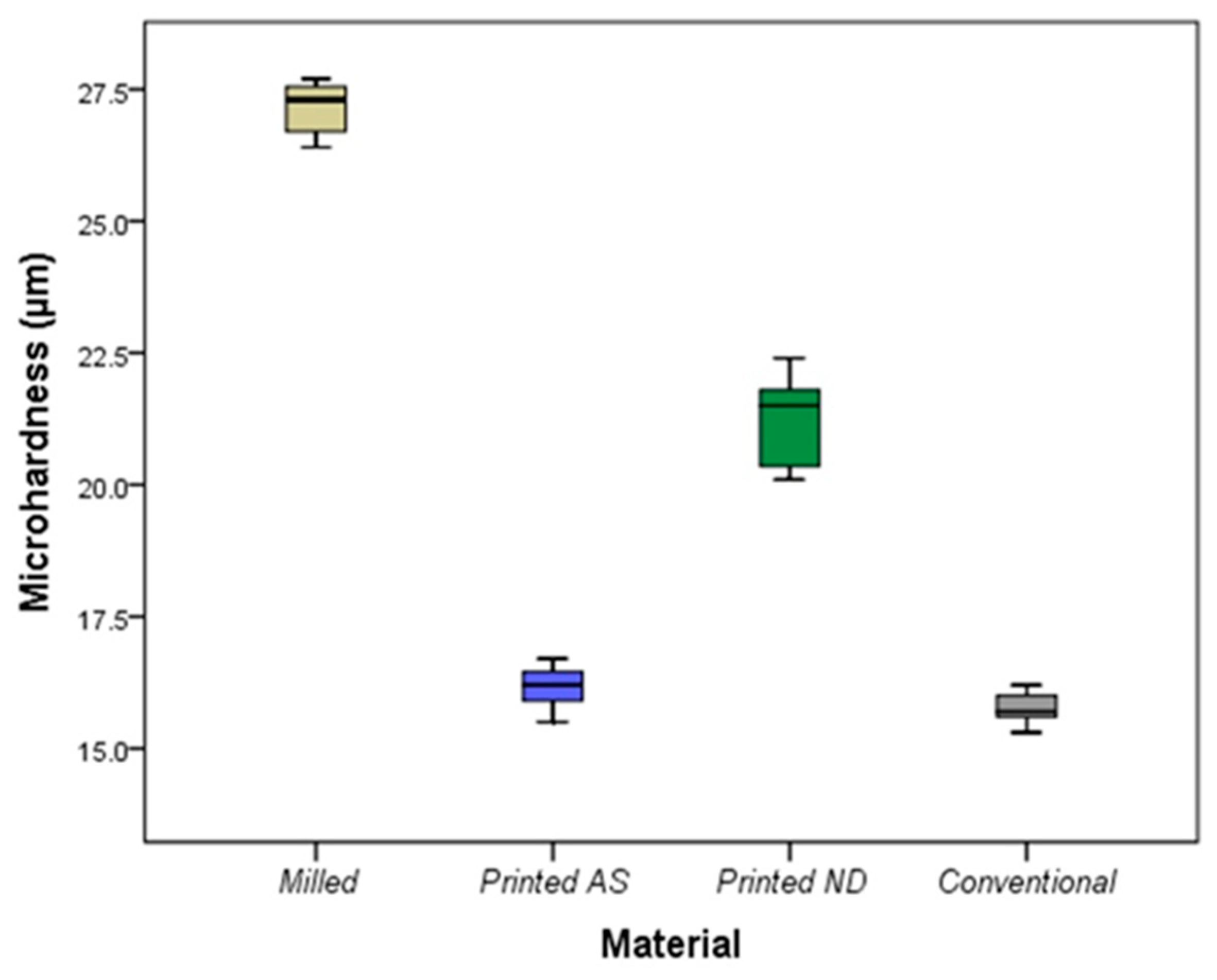
2.7. Surface Microhardness Test
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Akiba, S.; Takamizawa, T.; Tsujimoto, A.; Moritake, N.; Ishyii, R.; Barkmeier, W.; Latta, M.A.; Miyazaki, M. Influence of different curing modes on flexural properties, fracture toughness, and wear behavior of dual-cure provisional resin-based composites. Dent. Mater. J. 2019, 38, 728–737. [Google Scholar] [CrossRef] [PubMed]
- Pascutti, F.; Kreve, S.; Carvalho, G.; Grecco, P.; Franco, A.; Dias, S. Evaluation in vitro of Flexural Strength of Three Resins for Provisional Crowns in CAD/CAM System. J. Dent. Sci. 2017, 5, 75–81. [Google Scholar]
- Al-Qahtani, A.S.; Tulbah, H.I.; Binhasan, M.; Abbasi, M.S.; Ahmed, N.; Shabib, S.; Farooq, I.; Aldahian, N.; Nisar, S.S.; Tanveer, S.A.; et al. Surface Properties of Polymer Resins Fabricated with Subtractive and Additive Manufacturing Techniques. Polymers 2021, 13, 4077. [Google Scholar] [CrossRef] [PubMed]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L. Characterization of the mechanical properties of CAD/CAM polymers for interim fixed restorations. Dent. Mater. J. 2020, 39, 319–325. [Google Scholar] [CrossRef]
- Liebermann, A.; Wimmer, T.; Schmidlin, P.R.; Scherer, H.; Löffler, P.; Roos, M.; Stawarczyk, B. Physicomechanical characterization of polyetheretherketone and current esthetic dental CAD/CAM polymers after aging in different storage media. J. Prosthet. Dent. 2016, 115, 321–328.e2. [Google Scholar] [CrossRef]
- Rayyan, M.M.; Aboushelib, M.; Sayed, N.M.; Ibrahim, A.; Jimbo, R. Comparison of interim restorations fabricated by CAD/CAM with those fabricated manually. J Prosthet. Dent. 2015, 114, 414–419. [Google Scholar] [CrossRef]
- Shim, J.; Kim, H.; Park, S.; Yun, H.; Ryu, J. Comparison of Various Implant Provisional Resin Materials for Cytotoxicity and Attachment to Human Gingival Fibroblasts. Int. J. Oral. Maxillofac. Implants 2019, 34, 390–396. [Google Scholar] [CrossRef]
- Digholkar, S.; Madhav, V.N.V.; Palaskar, J. Evaluation of the flexural strength and microhardness of provisional crown and bridge materials fabricated by different methods. J. Indian. Prosthodont. Soc. 2016, 16, 328–334. [Google Scholar]
- Reeponmaha, T.; Angwaravong, O.; Angwarawong, T. Comparison of fracture strength after thermo-mechanical aging between provisional crowns made with CAD/CAM and conventional method. J. Adv. Prosthodont. 2020, 12, 218–224. [Google Scholar] [CrossRef]
- Schwantz, J.K.; Oliveira-Ogliari, A.; Meereis, C.T.; Leal, F.B.; Ogliari, F.A.; Moraes, R.R. Characterization of Bis-Acryl Composite Resins for Provisional Restorations. Braz. Dent. J. 2017, 28, 354–361. [Google Scholar] [CrossRef]
- Lee, J.; Clark, S.R.; Tantbirojn, D.; Korioth, T.V.P.; Hill, A.E.; Versluis, A. Strength and stiffness of interim materials and interim fixed dental prostheses when tested at different loading rates. J. Prosthet. Dent. 2022, 127, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Coelho, C.; Calamote, C.; Pinto, A.C.; Esteves, J.L.; Ramos, A.; Escuin, T.; Souza, J.C.M. Comparison of CAD-CAM and traditional chairside processing of 4-unit interim prostheses with and without cantilevers: Mechanics, fracture behavior, and finite element analysis. J. Prosthet. Dent. 2021, 125, 543.e1–543.e10. [Google Scholar] [CrossRef] [PubMed]
- Taşın, S.; Ismatullaev, A. Comparative evaluation of the effect of thermocycling on the mechanical properties of conventionally polymerized, CAD-CAM milled, and 3D-printed interim materials. J. Prosthet. Dent. 2022, 127, 173.e1–173.e8. [Google Scholar] [CrossRef] [PubMed]
- Astudillo-Rubio, D.; Delgado-Gaete, A.; Bellot-Arcís, C.; Montiel-Company, J.M.; Pascual-Moscardó, A.; Almerich-Silla, J.M. Mechanical properties of provisional dental materials: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0193162. [Google Scholar]
- Singh, A.; Garg, S. Comparative Evaluation of Flexural Strength of Provisional Crown and Bridge Materials-An Invitro Study. J. Clin. Diagn. Res. 2016, 10, ZC72–ZC77. [Google Scholar] [CrossRef] [PubMed]
- Huettig, F.; Prutscher, A.; Goldammer, C.; Kreutzer, C.A.; Weber, H. First clinical experiences with CAD/CAM-fabricated PMMA-based fixed dental prostheses as long-term temporaries. Clin. Oral. Investig. 2016, 20, 161–168. [Google Scholar] [CrossRef]
- Alt, V.; Hannig, M.; Wöstmann, B.; Balkenhol, M. Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent. Mater. 2011, 27, 339–347. [Google Scholar] [CrossRef]
- Ellakany, P.; Aly, N.M.; Al-Harbi, F. Accuracy of 3D Printed and Digital Casts Produced from Intraoral and Extraoral Scanners with Different Scanning Technologies: In Vitro Study. J. Prosthodont. 2022, 31, 521–528. [Google Scholar] [CrossRef]
- Abad-Coronel, C.; Carrera, E.; Córdova, N.M.; Fajardo, J.I.; Aliaga, P. Comparative Analysis of Fracture Resistance between CAD/CAM Materials for Interim Fixed Prosthesis. Materials 2021, 14, 7791. [Google Scholar] [CrossRef]
- Alp, G.; Murat, S.; Yilmaz, B. Comparison of Flexural Strength of Different CAD/CAM PMMA-Based Polymers. J. Prosthodont. 2019, 28, e491–e495. [Google Scholar] [CrossRef]
- Yao, J.; Li, J.; Wang, Y.; Huang, H. Comparison of the flexural strength and marginal accuracy of traditional and CAD/CAM interim materials before and after thermal cycling. J. Prosthet. Dent. 2014, 112, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Dureja, I.; Yadav, B.; Malhotra, P.; Dabas, N.; Bhargava, A.; Pahwa, R. A comparative evaluation of vertical marginal fit of provisional crowns fabricated by computer-aided design/computer-aided manufacturing technique and direct (intraoral technique) and flexural strength of the materials: An in vitro study. J. Indian. Prosthodont. Soc. 2018, 18, 314–320. [Google Scholar] [PubMed]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Simoneti, D.M.; Pereira-Cenci, T.; dos Santos, M.B.F. Comparison of material properties and biofilm formation in interim single crowns obtained by 3D printing and conventional methods. J. Prosthet. Dent. 2022, 127, 168–172. [Google Scholar] [CrossRef]
- Henderson, J.Y.; Korioth, T.V.P.; Tantbirojn, D.; Versluis, A. Failure load of milled, 3D-printed, and conventional chairside-dispensed interim 3-unit fixed dental prostheses. J. Prosthet. Dent. 2022, 127, 275.e1–275.e7. [Google Scholar] [CrossRef]
- Ellakany, P.; Aly, N.M.; Al-Harbi, F. A comparative study assessing the precision and trueness of digital and printed casts produced from several intraoral and extraoral scanners in full arch and short span (3-unit FPD) scanning: An in vitro study. J. Prosthodont. 2022. [Google Scholar] [CrossRef]
- Lee, W.S.; Lee, D.H.; Lee, K.B. Evaluation of internal fit of interim crown fabricated with CAD/CAM milling and 3D printing system. J. Adv. Prosthodont. 2017, 9, 265–270. [Google Scholar] [CrossRef]
- Abduo, J.; Lyons, K.; Bennamoun, M. Trends in computer-aided manufacturing in prosthodontics: A review of the available streams. Int. J. Dent. 2014, 2014, 783948. [Google Scholar] [CrossRef]
- Darwish, L.R.; Al-Qady, A.; El-Wakad, M.T.; Farag, M.M.; Darwish, R.R. Trends in 3D Printing Implants for Medical and Dental Applications. Ref. Modul. Mater. Sci. Mater. Eng. 2022, 4, 871–901. [Google Scholar] [CrossRef]
- Aati, S.; Akram, Z.; Ngo, H.; Fawzy, A.S. Development of 3D printed resin reinforced with modified ZrO2 nanoparticles for long-term provisional dental restorations. Dent. Mater. 2021, 37, e360–e374. [Google Scholar] [CrossRef]
- Ellakany, P.; Al-Harbi, F.; El Tantawi, M.; Mohsen, C. Evaluation of the accuracy of digital and 3D-printed casts compared with conventional stone casts. J. Prosthet. Dent. 2022, 127, 438–444. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef] [PubMed]
- Alshamrani, A.A.; Raju, R.; Ellakwa, A. Effect of Printing Layer Thickness and Postprinting Conditions on the Flexural Strength and Hardness of a 3D-Printed Resin. Biomed. Res. Int. 2022, 2022, 8353137. [Google Scholar] [CrossRef] [PubMed]
- Nakonieczny, D.S.; Kern, F.; Dufner, L.; Antonowicz, M.; Matus, K. Alumina and Zirconia-Reinforced Polyamide PA-12 Composites for Biomedical Additive Manufacturing. Materials 2021, 14, 6201. [Google Scholar] [CrossRef] [PubMed]
- Nakonieczny, D.S.; Kern, F.; Dufner, L.; Dubiel, A.; Antonowicz, M.; Matus, K. Effect of calcination temperatures on the phase composition, morphology and thermal properties of ZrO2 and Al2O3 for biomedical applications modified with APTES (3-aminopropyltriethoxysilane). Materials 2021, 14, 6651. [Google Scholar] [CrossRef]
- Kolb, C.; Gumpert, K.; Wolter, H.; Sextl, G. Highly translucent dental resin composites through refractive index adaption using zirconium dioxide nanoparticles and organic functionalization. Dent. Mater. 2020, 36, 1332–1342. [Google Scholar] [CrossRef] [PubMed]
- Aati, S.; Shrestha, B.; Fawzy, A. Cytotoxicity and antimicrobial efficiency of ZrO2 nanoparticles reinforced 3D printed resins. Dent. Mater. 2022, 38, 1432–1442. [Google Scholar] [CrossRef] [PubMed]
- Niem, T.; Youssef, N.; Wöstmann, B. Influence of accelerated ageing on the physical properties of CAD/CAM restorative materials. Clin. Oral. Investig. 2020, 24, 2415–2425. [Google Scholar] [CrossRef]
- Suralik, K.M.; Sun, J.; Chen, C.-Y.; Lee, S.J. Effect of Fabrication Method on Fracture Strength of Provisional Implant-Supported Fixed Dental Prostheses. Prosthesis 2020, 2, 325–332. [Google Scholar] [CrossRef]
- Scotti, C.K.; Velo, M.M.d.A.C.; Rizzante, F.A.P.; Nascimento, T.R.d.L.; Mondelli, R.F.L.; Bombonatti, J.F.S. Physical and surface properties of a 3D-printed composite resin for a digital workflow. J. Prosthet. Dent. 2020, 124, 614.e1–614.e5. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods. 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Kadam, P.; Bhalerao, S. Sample size calculation. Int. J. Ayurveda Res. 2010, 1, 55–57. [Google Scholar] [PubMed]
- Zimmermann, M.; Ender, A.; Attin, T.; Mehl, A. Fracture load of three-unit full-contour fixed dental prostheses fabricated with subtractive and additive CAD/CAM technology. Clin. Oral Investig. 2020, 24, 1035–1042. [Google Scholar] [CrossRef] [PubMed]
- Peñate, L.; Basilio, J.; Roig, M.; Mercadé, M. Comparative study of interim materials for direct fixed dental prostheses and their fabrication with CAD/CAM technique. J. Prosthet. Dent. 2015, 114, 248–253. [Google Scholar] [CrossRef]
- Wimmer, T.; Ender, A.; Roos, M.; Stawarczyk, B. Fracture load of milled polymeric fixed dental prostheses as a function of connector cross-sectional areas. J. Prosthet. Dent. 2013, 110, 288–295. [Google Scholar] [CrossRef]
- Karaokutan, I.; Sayin, G.; Kara, O. In vitro study of fracture strength of provisional crown materials. J. Adv. Prosthodont. 2015, 7, 27–31. [Google Scholar] [CrossRef]
- Park, S.M.; Park, J.M.; Kim, S.K.; Heo, S.J.; Koak, J.Y. Flexural Strength of 3D-Printing Resin Materials for Provisional Fixed Dental Prostheses. Materials 2020, 13, 3970. [Google Scholar] [CrossRef]
- ISO 10477:2018; Dentistry-Polymer-Based Crown and Veneering Materials. International Organization for Standardization: Geneva, Switzerland. Available online: https://www.iso.org/standard/68235.html (accessed on 13 September 2022).
- Pieniak, D.; Walczak, A.; Walczak, M.; Przystupa, K.; Niewczas, A.M. Hardness and Wear Resistance of Dental Biomedical Nanomaterials in a Humid Environment with Non-Stationary Temperatures. Materials 2020, 13, 1255. [Google Scholar] [CrossRef]
- Heintze, S.D.; Monreal, D.; Reinhardt, M.; Eser, A.; Peschke, A.; Reinshagen, J.; Rousson, V. Fatigue resistance of all-ceramic fixed partial dentures—Fatigue tests and finite element analysis. Dent. Mater. 2020, 34, 494–507. [Google Scholar] [CrossRef]


| Interim Materials Used | Composition | Abbreviation | Trade Name and Manufacturer | Type of Machine Used | Manufacturing Technique | Laser Beam Intensity | Post Curing Phase |
|---|---|---|---|---|---|---|---|
| Auto-polymerized polymethyl methacrylate resin (auto-polymerized PMMA) | Methyl methacrylates N, N-diméthyl-p-toluidine Methyl methacrylate and ethyl methacrylate copolymer | Conventional resin | Unifast Trad, GC chemicals, Tokyo, Japan | - | Manual | - | - |
| CAD/CAM PMMA blocks | Cross-linked Polymethyl methacrylate-based polymer | Milled resin | Telio CAD; Ivoclar Vivadent | CAM milling machine (PM 7, Ivoclar, Vivade) | Milling | - | - |
| 3D-printed composite resins | Microfilled Methacrylic oligomers & phosphine oxides | SLA ND resin | NextDent C&B MFH, Soesterburg, The Netherlands | 405 nm UV LED NextDent 5100 3D | 3D printing SLA | 405 nm UV LED | LC-D Print Box, 3D systems, Vertex Dental B.V., Soesterberg, Netherland |
| 3D-printed composite resin | Photopolymerized Methacrylate resin | DLP AS resin | ASIGA DentaTooth, ASIGA, Erfurt, Germany | Asiga MAX UV | 3D printing DLP | UV LED (385–405 nm) | Asiga Flash UV Curing Chamber, Erfurt, Germany |
| Milled | DLP AS | SLA ND | Conventional | KWT p Value | |
|---|---|---|---|---|---|
| Mean ± SD | |||||
| Microhardness (µm) | 27.13 ± 0.52 | 16.16 ± 0.43 | 21.19 ± 0.91 | 15.77 ± 0.32 | <0.001 * |
| Force at break (N) | 1794.06 ± 34.83 | 1067.57 ± 91.85 | 1720.26 ± 71.18 | 1008.23 ± 62.87 | <0.001 * |
| Flexural strength (MPa) | 174.42 ± 3.39 | 103.79 ± 8.93 | 167.25 ± 6.92 | 98.02 ± 6.11 | <0.001 * |
| Elastic modulus (MPa) | 1003.71 ± 18.57 | 951.13 ± 68.61 | 805.47 ± 190.37 | 961.48 ± 84.76 | 0.04 * |
| Group | Compared to | p Value | |
|---|---|---|---|
| Microhardness | Milled | DLP AS | 0.002 * |
| SLA ND | 0.67 | ||
| Conventional | <0.001 * | ||
| DLP AS | SLA ND | 0.30 | |
| Conventional | 1.00 | ||
| SLA ND | Conventional | 0.03 * | |
| Force at break | Milled | DLP AS | 0.005 * |
| SLA ND | 1.00 | ||
| Conventional | 0.001 * | ||
| DLP AS | SLA ND | 0.08 | |
| Conventional | 1.00 | ||
| SLA ND | Conventional | 0.02 * | |
| Flexural strength | Milled | DLP AS | 0.005 * |
| SLA ND | 1.00 | ||
| Conventional | 0.001 * | ||
| DLP AS | SLA ND | 0.08 | |
| Conventional | 1.00 | ||
| SLA ND | Conventional | 0.02 * | |
| Elastic modulus | Milled | DLP AS | 0.86 |
| SLA ND | 0.02 * | ||
| Conventional | 1.00 | ||
| DLP AS | SLA ND | 0.92 | |
| Conventional | 1.00 | ||
| SLA ND | Conventional | 0.51 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ellakany, P.; Fouda, S.M.; Mahrous, A.A.; AlGhamdi, M.A.; Aly, N.M. Influence of CAD/CAM Milling and 3D-Printing Fabrication Methods on the Mechanical Properties of 3-Unit Interim Fixed Dental Prosthesis after Thermo-Mechanical Aging Process. Polymers 2022, 14, 4103. https://doi.org/10.3390/polym14194103
Ellakany P, Fouda SM, Mahrous AA, AlGhamdi MA, Aly NM. Influence of CAD/CAM Milling and 3D-Printing Fabrication Methods on the Mechanical Properties of 3-Unit Interim Fixed Dental Prosthesis after Thermo-Mechanical Aging Process. Polymers. 2022; 14(19):4103. https://doi.org/10.3390/polym14194103
Chicago/Turabian StyleEllakany, Passent, Shaimaa M. Fouda, Amr A. Mahrous, Maram A. AlGhamdi, and Nourhan M. Aly. 2022. "Influence of CAD/CAM Milling and 3D-Printing Fabrication Methods on the Mechanical Properties of 3-Unit Interim Fixed Dental Prosthesis after Thermo-Mechanical Aging Process" Polymers 14, no. 19: 4103. https://doi.org/10.3390/polym14194103
APA StyleEllakany, P., Fouda, S. M., Mahrous, A. A., AlGhamdi, M. A., & Aly, N. M. (2022). Influence of CAD/CAM Milling and 3D-Printing Fabrication Methods on the Mechanical Properties of 3-Unit Interim Fixed Dental Prosthesis after Thermo-Mechanical Aging Process. Polymers, 14(19), 4103. https://doi.org/10.3390/polym14194103






