Polymer-Based Hydrogel Loaded with Honey in Drug Delivery System for Wound Healing Applications
Abstract
:1. Introduction
2. The Phase of Wound Healing

3. Classification of Wound Dressings
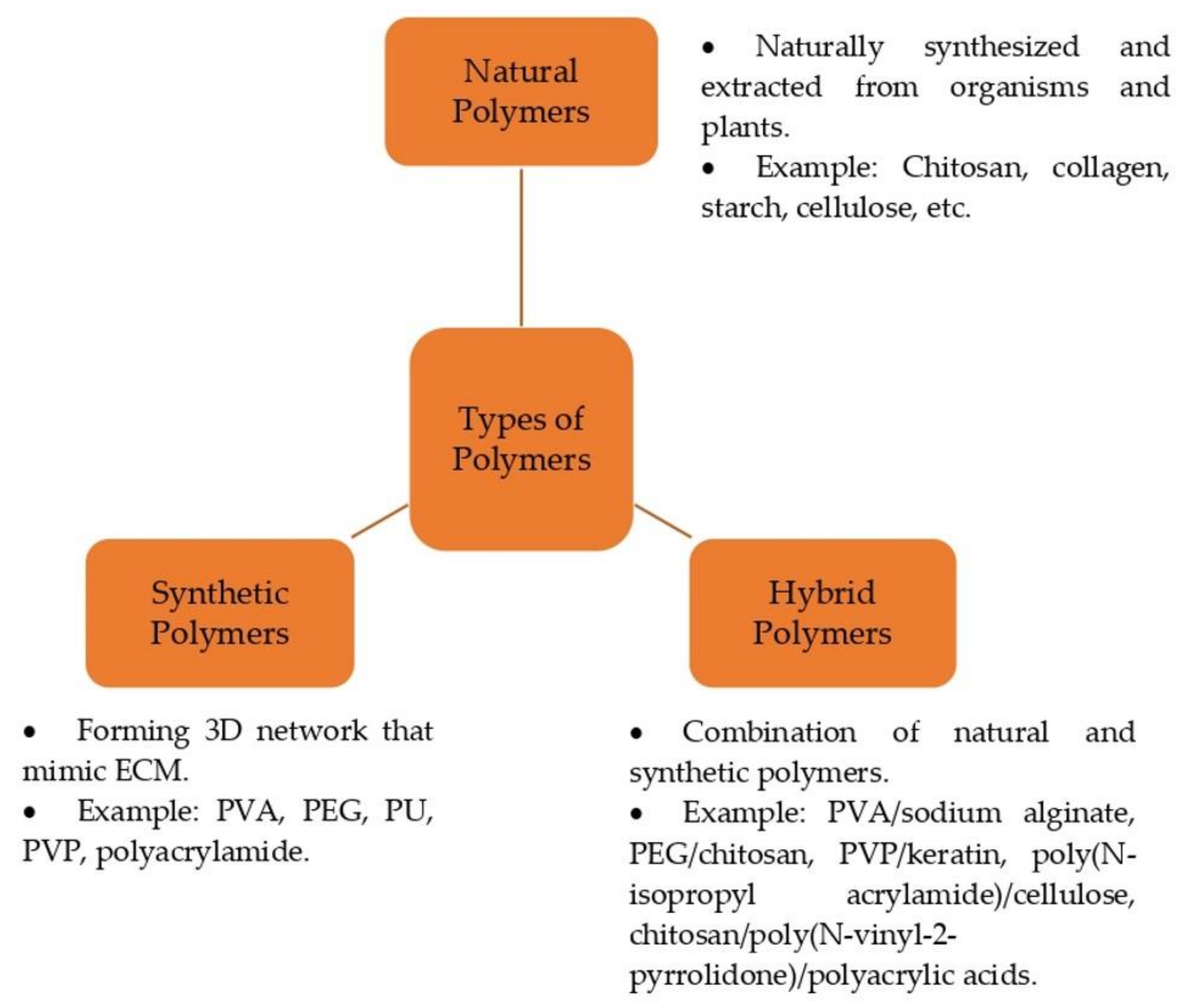
4. Polymer-Based Hydrogels for Wound Healing
4.1. Natural Polymer
4.2. Synthetic Polymer
4.3. Hybrid-Based Polymers
5. Physicochemical Properties and Composition of Honey
6. Biological Activity of Honey in Wound Healing
7. Application of Honey-Based Hydrogel for Wound Healing
8. Cell Migration and Proliferation on Honey-Based Wound Dressings
9. Toxicological Information of Honey-Based Wound Dressings
10. Regulatory Information of Honey-Based Wound Dressing
11. Patent Information on Honey-Based Wound Dressings
12. Commercialized Product of Honey-Based Wound Dressings
13. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shi, C.; Wang, C.; Liu, H.; Li, Q.; Li, R.; Zhang, Y.; Liu, Y.; Shao, Y.; Wang, J. Selection of Appropriate Wound Dressing for Various Wounds. Front. Bioeng. Biotechnol. 2020, 8, 182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilkinson, H.N.; Hardman, M.J. Wound healing: Cellular mechanisms and pathological outcomes. Open Biol. 2020, 10, 200223. [Google Scholar] [CrossRef] [PubMed]
- Dhivya, S.; Padma, V.V.; Santhini, E. Wound dressings—A review. Biomedicine 2015, 5, 22. [Google Scholar] [CrossRef] [PubMed]
- Ghomi, E.R.; Khalili, S.; Khorasani, S.N.; Neisiany, R.E.; Ramakrishna, S. Wound dressings: Current advances and future directions. J. Appl. Polym. Sci. 2019, 136, 47738. [Google Scholar] [CrossRef] [Green Version]
- Su, J.; Li, J.; Liang, J.; Zhang, K.; Li, J. Hydrogel Preparation Methods and Biomaterials for Wound Dressing. Life 2021, 11, 1016. [Google Scholar] [CrossRef]
- Bosworth, L.A.; Downes, S. Electrospinning for Tissue Regeneration; Woodhead Publishing Limited EBooks: Amsterdam, The Netherlands, 2011. [Google Scholar] [CrossRef]
- Kalaycıoğlu, Z.; Kahya, N.; Adımcılar, V.; Kaygusuz, H.; Torlak, E.; Akın-Evingür, G.; Erim, F.B. Antibacterial nano cerium oxide/chitosan/cellulose acetate composite films as potential wound dressing. Eur. Polym. J. 2020, 133, 109777. [Google Scholar] [CrossRef]
- Chin, C.-Y.; Jalil, J.; Ng, P.Y.; Ng, S.-F. Development and formulation of Moringa oleifera standardised leaf extract film dressing for wound healing application. J. Ethnopharmacol. 2018, 212, 188–199. [Google Scholar] [CrossRef]
- Bustamante-Torres, M.; Romero-Fierro, D.; Arcentales-Vera, B.; Palomino, K.; Magaña, H.; Bucio, E. Hydrogels Classification According to the Physical or Chemical Interactions and as Stimuli-Sensitive Materials. Gels 2021, 7, 182. [Google Scholar] [CrossRef]
- Brumberg, V.; Astrelina, T.; Malivanova, T.; Samoilov, A. Modern Wound Dressings: Hydrogel Dressings. Biomedicines 2021, 9, 1235. [Google Scholar] [CrossRef]
- Gavan, A.; Colobatiu, L.; Hanganu, D.; Bogdan, C.; Olah, N.K.; Achim, M.; Mirel, S. Development and Evaluation of Hydrogel Wound Dressings Loaded with Herbal Extracts. Processes 2022, 10, 242. [Google Scholar] [CrossRef]
- Chai, Q.; Jiao, Y.; Yu, X. Hydrogels for Biomedical Applications: Their Characteristics and the Mechanisms behind Them. Gels 2017, 3, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aderibigbe, B.A. Hybrid-Based Wound Dressings: Combination of Synthetic and Biopolymers. Polymers 2022, 14, 3806. [Google Scholar] [CrossRef] [PubMed]
- Hamedi, H.; Moradi, S.; Hudson, S.M.; Tonelli, A.E. Chitosan based hydrogels and their applications for drug delivery in wound dressings: A review. Carbohydr. Polym. 2018, 199, 445–460. [Google Scholar] [CrossRef] [PubMed]
- Khorasani, M.T.; Joorabloo, A.; Adeli, H.; Mansoori-Moghadam, Z.; Moghaddam, A. Design and optimization of process parameters of polyvinyl (alcohol)/chitosan/nano zinc oxide hydrogels as wound healing materials. Carbohydr. Polym. 2018, 207, 542–554. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Niazi, M.B.K.; Jahan, Z.; Ahmad, T.; Hussain, A.; Pervaiz, E.; Janjua, H.A.; Hussain, Z. In-vitro and in-vivo study of superabsorbent PVA/Starch/g-C3N4/Ag@TiO2 NPs hydrogel membranes for wound dressing. Eur. Polym. J. 2020, 130, 109650. [Google Scholar] [CrossRef]
- Xue, H.; Hu, L.; Xiong, Y.; Zhu, X.; Wei, C.; Cao, F.; Zhou, W.; Sun, Y.; Endo, Y.; Liu, M.; et al. Quaternized chitosan-Matrigel-polyacrylamide hydrogels as wound dressing for wound repair and regeneration. Carbohydr. Polym. 2019, 226, 115302. [Google Scholar] [CrossRef]
- Koehler, J.; Brandl, F.; Goepferich, A. Hydrogel wound dressings for bioactive treatment of acute and chronic wounds. Eur. Polym. J. 2018, 100, 1–11. [Google Scholar] [CrossRef]
- Alven, S.; Nqoro, X.; Aderibigbe, B.A. Polymer-Based Materials Loaded with Curcumin for Wound Healing Applications. Polymers 2020, 12, 2286. [Google Scholar] [CrossRef]
- Yaghoobi, R.; Kazerouni, A.; Kazerouni, O. Evidence for Clinical Use of Honey in Wound Healing as an Anti-bacterial, Anti-inflammatory Anti-oxidant and Anti-viral Agent: A Review. Jundishapur J. Nat. Pharm. Prod. 2013, 8, 100–104. [Google Scholar] [CrossRef] [Green Version]
- Mandal, M.D.; Mandal, S. Honey: Its medicinal property and antibacterial activity. Asian Pac. J. Trop. Biomed. 2011, 1, 154–160. [Google Scholar] [CrossRef] [Green Version]
- Minden-Birkenmaier, B.A.; Bowlin, G.L. Honey-Based Templates in Wound Healing and Tissue Engineering. Bioengineering 2018, 5, 46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gopal, R.; Lo, A.Z.K.; Masrol, M.; Lai, C.-H.; Zain, N.M.; Saidin, S. Susceptibility of Stingless Bee, Giant Bee and Asian Bee Honeys Incorporated Cellulose Hydrogels in Treating Wound Infection. Malays. J. Fundam. Appl. Sci. 2021, 17, 242–252. [Google Scholar] [CrossRef]
- Noori, S.; Kokabi, M.; Hassan, Z.M. Poly(vinyl alcohol)/chitosan/honey/clay responsive nanocomposite hydrogel wound dressing. J. Appl. Polym. Sci. 2018, 135, 46311. [Google Scholar] [CrossRef]
- Tavakoli, J.; Tang, Y. Honey/PVA hybrid wound dressings with controlled release of antibiotics: Structural, physico-mechanical and in-vitro biomedical studies. Mater. Sci. Eng. C 2017, 77, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, N.; Ima-Nirwana, S.; Mohamed, I.N.; Mohamed, N.; Chin, K.; Shuid, A.N. Wound Healing Properties of Selected Natural Products. Int. J. Environ. Res. Public Health 2018, 15, 2360. [Google Scholar] [CrossRef] [Green Version]
- Benito-Martínez, S.; Pérez-Köhler, B.; Rodríguez, M.; Izco, J.M.; Recalde, J.I.; Pascual, G. Wound Healing Modulation through the Local Application of Powder Collagen-Derived Treatments in an Excisional Cutaneous Murine Model. Biomedicines 2022, 10, 960. [Google Scholar] [CrossRef]
- Zuliani-Alvarez, L.; Midwood, K.S. Fibrinogen-Related Proteins in Tissue Repair: How a Unique Domain with a Common Structure Controls Diverse Aspects of Wound Healing. Adv. Wound Care 2014, 4, 273–285. [Google Scholar] [CrossRef] [Green Version]
- Fredric, S.; Gowda, D.V.; Yashashwini, M. Wafers for Wound Healing. J. Chem. Pharm. Res. 2015, 7, 450–468. Available online: https://www.jocpr.com/articles/wafers-for-wound-healing.pdf (accessed on 14 May 2023).
- Frykberg, R.G.; Banks, J. Challenges in the Treatment of Chronic Wounds. Adv. Wound Care 2015, 4, 560–582. [Google Scholar] [CrossRef] [Green Version]
- Gainza, G.; Villullas, S.; Pedraz, J.L.; Hernandez, R.M.; Igartua, M. Advances in drug delivery systems (DDSs) to release growth factors for wound healing and skin regeneration. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 1551–1573. [Google Scholar] [CrossRef]
- Gonzalez, A.C.D.O.; Costa, T.F.; de Araújo Andrade, Z.; Medrado, A.R.A.P. Wound healing—A literature review. An. Bras. Dermatol. 2016, 91, 614–620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alven, S.; Peter, S.; Mbese, Z.; Aderibigbe, B.A. Polymer-Based Wound Dressing Materials Loaded with Bioactive Agents: Potential Materials for the Treatment of Diabetic Wounds. Polymers 2022, 14, 724. [Google Scholar] [CrossRef] [PubMed]
- Stoica, A.E.; Chircov, C.; Grumezescu, A.M. Nanomaterials for Wound Dressings: An Up-to-Date Overview. Molecules 2020, 25, 2699. [Google Scholar] [CrossRef] [PubMed]
- Ndlovu, S.P.; Ngece, K.; Alven, S.; Aderibigbe, B.A. Gelatin-Based Hybrid Scaffolds: Promising Wound Dressings. Polymers 2021, 13, 2959. [Google Scholar] [CrossRef]
- Vivcharenko, V.; Przekora, A. Modifications of Wound Dressings with Bioactive Agents to Achieve Improved Pro-Healing Properties. Appl. Sci. 2021, 11, 4114. [Google Scholar] [CrossRef]
- Mandla, S.; Huyer, L.D.; Radisic, M. Review: Multimodal bioactive material approaches for wound healing. APL Bioeng. 2018, 2, 021503. [Google Scholar] [CrossRef] [Green Version]
- Weller, C.D.; Team, V.; Sussman, G. First-Line Interactive Wound Dressing Update: A Comprehensive Review of the Evidence. Front. Pharmacol. 2020, 11, 155. [Google Scholar] [CrossRef] [Green Version]
- Schoukens, G. 5—Bioactive dressings to promote wound healing. In Advanced Textiles for Wound Care; Elsevier: Amsterdam, The Netherlands, 2019; pp. 135–167. [Google Scholar] [CrossRef]
- Savoji, H.; Godau, B.; Hassani, M.S.; Akbari, M. Skin Tissue Substitutes and Biomaterial Risk Assessment and Testing. Front. Bioeng. Biotechnol. 2018, 6, 86. [Google Scholar] [CrossRef]
- Ho, T.-C.; Chang, C.-C.; Chan, H.-P.; Chung, T.-W.; Shu, C.-W.; Chuang, K.-P.; Duh, T.-H.; Yang, M.-H.; Tyan, Y.-C. Hydrogels: Properties and applications in Biomedicine. Molecules 2022, 27, 2902. [Google Scholar] [CrossRef]
- Pourshahrestani, S.; Zeimaran, E.; Kadri, N.A.; Mutlu, N.; Boccaccini, A.R. Polymeric Hydrogel Systems as Emerging Biomaterial Platforms to Enable Hemostasis and Wound Healing. Adv. Health Mater. 2020, 9, 2000905. [Google Scholar] [CrossRef]
- Chen, T.; Chen, Y.; Rehman, H.U.; Chen, Z.; Yang, Z.; Wang, M.; Li, H.; Liu, H. Ultratough, Self-Healing, and Tissue-Adhesive Hydrogel for Wound Dressing. ACS Appl. Mater. Interfaces 2018, 10, 33523–33531. [Google Scholar] [CrossRef]
- Wang, H.; Xu, Z.; Zhao, M.; Liu, G.; Wu, J. Advances of hydrogel dressings in diabetic wounds. Biomater. Sci. 2020, 9, 1530–1546. [Google Scholar] [CrossRef] [PubMed]
- Reddy, M.S.B.; Ponnamma, D.; Choudhary, R.; Sadasivuni, K.K. A Comparative Review of Natural and Synthetic Biopolymer Composite Scaffolds. Polymers 2021, 13, 1105. [Google Scholar] [CrossRef] [PubMed]
- Ramineni, S.K. Mucoadhesive Films for Treatment of Local Oral Disorders: Development, Characterization and In Vivo Testing. Ph.D. Thesis, University of Kentucky, Lexington, KY, USA, 2013. Available online: https://uknowledge.uky.edu/cbme_etds/19 (accessed on 14 May 2023).
- Suamte, L.; Tirkey, A.; Babu, P.J. Design of 3D smart scaffolds using natural, synthetic and hybrid derived polymers for skin regenerative applications. Smart Mater. Med. 2023, 4, 243–256. [Google Scholar] [CrossRef]
- Negut, I.; Dorcioman, G.; Grumezescu, V. Scaffolds for Wound Healing Applications. Polymers 2020, 12, 2010. [Google Scholar] [CrossRef] [PubMed]
- Donnaloja, F.; Jacchetti, E.; Soncini, M.; Raimondi, M.T. Natural and Synthetic Polymers for Bone Scaffolds Optimization. Polymers 2020, 12, 905. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nune, S.K.; Rama, K.S.; Dirisala, V.R.; Chavali, M. Electrospinning of Collagen Nanofiber Scaffolds for Tissue Repair and Regeneration; Elsevier EBooks: Amsterdam, The Netherlands, 2017; pp. 281–311. [Google Scholar] [CrossRef]
- Kamoun, E.A.; Kenawy, E.-R.S.; Chen, X. A review on polymeric hydrogel membranes for wound dressing applications: PVA-based hydrogel dressings. J. Adv. Res. 2017, 8, 217–233. [Google Scholar] [CrossRef]
- Jayakumar, A.; Radoor, S.; Radhakrishnan, E.K.; Nair, I.; Siengchin, S.; Siengchin, S. Soy Protein-Based Polymer Blends and Composites; Elsevier EBooks: Amsterdam, The Netherlands, 2022; pp. 39–57. [Google Scholar] [CrossRef]
- Aswathy, S.; Narendrakumar, U.; Manjubala, I. Commercial hydrogels for biomedical applications. Heliyon 2020, 6, e03719. [Google Scholar] [CrossRef]
- Follmann, H.D.; Messias, I.; Queiroz, M.V.O.; Araujo, R.A.; Rubira, A.F.; Muniz, E.C. Designing hybrid materials with multifunctional interfaces for wound dressing, electrocatalysis, and chemical separation. J. Colloid Interface Sci. 2019, 533, 106–125. [Google Scholar] [CrossRef]
- Kong, F.; Fan, C.; Yang, Y.; Lee, B.H.; Wei, K. 5-hydroxymethylfurfural-embedded poly (vinyl alcohol)/sodium alginate hybrid hydrogels accelerate wound healing. Int. J. Biol. Macromol. 2019, 138, 933–949. [Google Scholar] [CrossRef] [PubMed]
- Masood, N.; Ahmed, R.; Tariq, M.; Ahmed, Z.; Masoud, M.S.; Ali, I.; Asghar, R.; Andleeb, A.; Hasan, A. Silver nanoparticle impregnated chitosan-PEG hydrogel enhances wound healing in diabetes induced rabbits. Int. J. Pharm. 2019, 559, 23–36. [Google Scholar] [CrossRef] [PubMed]
- Tajik, F.; Eslahi, N.; Rashidi, A.; Rad, M.M. Hybrid antibacterial hydrogels based on PVP and keratin incorporated with lavender extract. J. Polym. Res. 2021, 28, 1–10. [Google Scholar] [CrossRef]
- Zubik, K.; Singhsa, P.; Wang, Y.; Manuspiya, H.; Narain, R. Thermo-Responsive Poly(N-Isopropylacrylamide)-Cellulose Nanocrystals Hybrid Hydrogels for Wound Dressing. Polymers 2017, 9, 119. [Google Scholar] [CrossRef] [Green Version]
- Rasool, A.; Ata, S.; Islam, A. Stimuli responsive biopolymer (chitosan) based blend hydrogels for wound healing application. Carbohydr. Polym. 2019, 203, 423–429. [Google Scholar] [CrossRef]
- Eteraf-Oskouei, T.; Najafi, M. Traditional and Modern Uses of Natural Honey in Human Diseases: A Review. Iran. J. Basic Med. Sci. 2013, 16, 731–742. [Google Scholar]
- Al-Kafaween, M.A.; Alwahsh, M.; Hilmi, A.B.M.; Abulebdah, D.H. Physicochemical Characteristics and Bioactive Compounds of Different Types of Honey and Their Biological and Therapeutic Properties: A Comprehensive Review. Antibiotics 2023, 12, 337. [Google Scholar] [CrossRef]
- Lim, D.C.C.; Abu Bakar, M.F.; Majid, M. Nutritional composition of stingless bee honey from different botanical origins. IOP Conf. Ser. Earth Environ. Sci. 2019, 269, 012025. [Google Scholar] [CrossRef] [Green Version]
- Alvarez-Suarez, J.M.; Gasparrini, M.; Simal-Gandara, J.; Mazzoni, L.; Giampieri, F. The Composition and Biological Activity of Honey: A Focus on Manuka Honey. Foods 2014, 3, 420–432. [Google Scholar] [CrossRef] [Green Version]
- Samarghandian, S.; Farkhondeh, T.; Samini, F. Honey and health: A review of recent clinical research. Pharmacogn. Res. 2017, 9, 121–127. [Google Scholar]
- Mieles, J.Y.; Vyas, C.; Aslan, E.; Humphreys, G.; Diver, C.; Bartolo, P. Honey: An Advanced Antimicrobial and Wound Healing Biomaterial for Tissue Engineering Applications. Pharmaceutics 2022, 14, 1663. [Google Scholar] [CrossRef]
- Bahari, N.; Hashim, N.; Akim, A.M.; Maringgal, B. Recent Advances in Honey-Based Nanoparticles for Wound Dressing: A Review. Nanomaterials 2022, 12, 2560. [Google Scholar] [CrossRef] [PubMed]
- Anis, A.; Sharshar, A.; El Hanbally, S.; Sadek, Y. A Novel Organic Composite Accelerates Wound Healing: Experimental and Clinical Study in Equine. J. Equine Vet.-Sci. 2021, 99, 103406. [Google Scholar] [CrossRef]
- Yilmaz, A.C.; Aygin, D. Honey Dressing In Wound Treatment: A Systematic Review. Complement. Ther. Med. 2020, 51, 102388. [Google Scholar] [CrossRef] [PubMed]
- Tashkandi, H. Honey in wound healing: An updated review. Open Life Sci. 2021, 16, 1091–1100. [Google Scholar] [CrossRef]
- Al-Jadi, A.-M.; Enchang, F.K.; Yusoff, K.M. The effect of Malaysian honey and its major components on the proliferation of cultured fibroblasts. Turk. J. Med. Sci. 2014, 44, 733–740. [Google Scholar] [CrossRef]
- Thirupathi, K.; Raorane, C.J.; Ramkumar, V.; Ulagesan, S.; Santhamoorthy, M.; Raj, V.; Krishnakumar, G.S.; Phan, T.T.V.; Kim, S.-C. Update on Chitosan-Based Hydrogels: Preparation, Characterization, and Its Antimicrobial and Antibiofilm Applications. Gels 2022, 9, 35. [Google Scholar] [CrossRef]
- Oryan, A.; Alemzadeh, E.; Moshiri, A. Biological properties and therapeutic activities of honey in wound healing: A narrative review and meta-analysis. J. Tissue Viability 2016, 25, 98–118. [Google Scholar] [CrossRef]
- Vaou, N.; Stavropoulou, E.; Voidarou, C.; Tsigalou, C.; Bezirtzoglou, E. Towards Advances in Medicinal Plant Antimicrobial Activity: A Review Study on Challenges and Future Perspectives. Microorganisms 2021, 9, 2041. [Google Scholar] [CrossRef]
- Liu, E.; Gao, H.; Zhao, Y.; Pang, Y.; Yao, Y.; Yang, Z.; Zhang, X.; Wang, Y.; Yang, S.; Ma, X.; et al. The potential application of natural products in cutaneous wound healing: A review of preclinical evidence. Front. Pharmacol. 2022, 13, 900439. [Google Scholar] [CrossRef]
- Bodnar, R.J. Epidermal Growth Factor and Epidermal Growth Factor Receptor: The Yin and Yang in the Treatment of Cutaneous Wounds and Cancer. Adv. Wound Care 2013, 2, 24–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.; Kyriakides, T.R. The role of extracellular matrix in the pathophysiology of diabetic wounds. Matrix Biol. Plus 2020, 6–7, 100037. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.S.; Singh, O.; Bhagel, P.S.; Moses, S.; Shukla, S.; Mathur, R.K. Honey dressing versus silver sulfadiazene dressing for wound healing in burn patients: A retrospective study. J. Cutan. Aesthetic Surg. 2011, 4, 183. [Google Scholar] [CrossRef] [PubMed]
- Pasupuleti, V.R.; Sammugam, L.; Ramesh, N.; Gan, S.H. Honey, Propolis, and Royal Jelly: A comprehensive review of their biological actions and health benefits. Oxidative Med. Cell. Longev. 2017, 2017, 1–21. [Google Scholar] [CrossRef] [Green Version]
- Molan, P.C. Re-introducing honey in the management of wounds and ulcers—Theory and practice. J. Wound Ostomy Cont. Nurs. 2002, 48, 28–40. [Google Scholar]
- Ousey, K.; Cutting, K.; Rogers, A.; Rippon, M. The importance of hydration in wound healing: Reinvigorating the clinical perspective. J. Wound Care 2016, 25, 122–130. [Google Scholar] [CrossRef]
- Sood, A.; Granick, M.S.; Tomaselli, N.L. Wound Dressings and Comparative Effectiveness Data. Adv. Wound Care 2014, 3, 511–529. [Google Scholar] [CrossRef] [Green Version]
- Esa, N.E.F.; Ansari, M.N.M.; Razak, S.I.A.; Ismail, N.I.; Jusoh, N.; Zawawi, N.A.; Jamaludin, M.I.; Sagadevan, S.; Nayan, N.H.M. A Review on Recent Progress of Stingless Bee Honey and Its Hydrogel-Based Compound for Wound Care Management. Molecules 2022, 27, 3080. [Google Scholar] [CrossRef]
- Chopra, H.; Bibi, S.; Kumar, S.; Khan, M.S.; Kumar, P.; Singh, I. Preparation and Evaluation of Chitosan/PVA Based Hydrogel Films Loaded with Honey for Wound Healing Application. Gels 2022, 8, 111. [Google Scholar] [CrossRef]
- Lo, A.Z.K.; Lukman, S.K.; Lai, C.-H.; Zain, N.M.; Saidin, S. Stingless Bee Honey Incorporated Cellulose Hydrogel/Poly(Lactic-Co-Glycolic Acid) Patch as an Alternative Treatment for Aphthous Stomatitis. Cell. Chem. Technol. 2021, 55, 539–603. [Google Scholar] [CrossRef]
- Zekry, S.S.A.; Abdellatif, A.; Azzazy, H.M. Fabrication of pomegranate/honey nanofibers for use as antibacterial wound dressings. Wound Med. 2020, 28, 100181. [Google Scholar] [CrossRef]
- Samraj.S, M.D.; Kirupha, S.D.; Elango, S.; Vadodaria, K. Fabrication of nanofibrous membrane using stingless bee honey and curcumin for wound healing applications. J. Drug Deliv. Sci. Technol. 2021, 63, 102271. [Google Scholar] [CrossRef]
- El-Kased, R.F.; Amer, R.I.; Attia, D.; Elmazar, M.M. Honey-based hydrogel: In vitro and comparative In vivo evaluation for burn wound healing. Sci. Rep. 2017, 7, 9692. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, X.; Fan, L.; Ma, L.; Wang, Y.; Lin, S.; Yu, F.; Pan, X.; Luo, G.; Zhang, D.; Wang, H. Green electrospun Manuka honey/silk fibroin fibrous matrices as potential wound dressing. Mater. Des. 2017, 119, 76–84. [Google Scholar] [CrossRef]
- Durai, B.; Sizing, S. Development and Evaluation of Chitosan Honey Hydrogel Sheets as Wound Dressing. Int. J. Pharm. Bio. Sci. 2015, 6, 26–37. Available online: http://www.ijpbs.net/cms/php/upload/3829_pdf.pdf (accessed on 14 May 2023).
- Zohdi, R.M.; Zakaria, Z.A.B.; Yusof, N.; Mustapha, N.M.; Abdullah, M.N.H. Gelam (Melaleuca spp.) Honey-Based Hydrogel as Burn Wound Dressing. Evid.-Based Complement. Altern. Med. 2011, 2012, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Khoo, Y.-T.; Halim, A.S.; Singh, K.-K.B.; Mohamad, N.-A. Wound contraction effects and antibacterial properties of Tualang honey on full-thickness burn wounds in rats in comparison to hydrofibre. BMC Complement. Altern. Med. 2010, 10, 48. [Google Scholar] [CrossRef] [Green Version]
- Liang, C.-C.; Park, A.Y.; Guan, J.-L. In vitro scratch assay: A convenient and inexpensive method for analysis of cell migration in vitro. Nat. Protoc. 2007, 2, 329–333. [Google Scholar] [CrossRef] [Green Version]
- Jonkman, J.E.N.; Cathcart, J.A.; Xu, F.; Bartolini, M.E.; Amon, J.E.; Stevens, K.M.; Colarusso, P. An introduction to the wound healing assay using live-cell microscopy. Cell Adhes. Migr. 2014, 8, 440–451. [Google Scholar] [CrossRef] [Green Version]
- Grada, A.; Otero-Viñas, M.; Prieto-Castrillo, F.P.; Obagi, Z.; Falanga, V. Research Techniques Made Simple: Analysis of Collective Cell Migration Using the Wound Healing Assay. J. Investig. Dermatol. 2017, 137, e11–e16. [Google Scholar] [CrossRef] [Green Version]
- Chaudhary, A.; Bag, S.; Banerjee, P.; Chatterjee, J. Wound healing efficacy of Jamun honey in diabetic mice model through reepithelialization, collagen deposition and angiogenesis. J. Tradit. Complement. Med. 2019, 10, 529–543. [Google Scholar] [CrossRef] [PubMed]
- Ranzato, E.; Martinotti, S.; Burlando, B. Honey exposure stimulates wound repair of human dermal fibroblasts. Burn. Trauma 2013, 1, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ebadi, P.; Fazeli, M. Evaluation of the potential in vitro effects of propolis and honey on wound healing in human dermal fibroblast cells. S. Afr. J. Bot. 2020, 137, 414–422. [Google Scholar] [CrossRef]
- Lau, X.Y.; Taib, H.; Berahim, Z.; Ahmad, A.; Zainuddin, S.L.A. The Effect of Tualang Honey on Human Periodontal Ligament Fibroblast Proliferation and Alkaline Phosphatase Level. Sains Malays. 2015, 44, 1021–1025. [Google Scholar] [CrossRef]
- Shamloo, A.; Aghababaie, Z.; Afjoul, H.; Jami, M.; Bidgoli, M.R.; Vossoughi, M.; Ramazani, A.; Kamyabhesari, K. Fabrication and evaluation of chitosan/gelatin/PVA hydrogel incorporating honey for wound healing applications: An in vitro, in vivo study. Int. J. Pharm. 2020, 592, 120068. [Google Scholar] [CrossRef] [PubMed]
- Sarhan, W.A.; Azzazy, H.M.E.; El-Sherbiny, I.M. Honey/Chitosan Nanofiber Wound Dressing Enriched with Allium sativum and Cleome droserifolia: Enhanced Antimicrobial and Wound Healing Activity. ACS Appl. Mater. Interfaces 2016, 8, 6379–6390. [Google Scholar] [CrossRef] [PubMed]
- Scepankova, H.; Combarros-Fuertes, P.; Fresno, J.M.; Tornadijo, M.E.; Dias, M.S.; Pinto, C.A.; Saraiva, J.A.; Estevinho, L.M. Role of Honey in Advanced Wound Care. Molecules 2021, 26, 4784. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Zhou, J.; Xu, Y. Study of the in vitro cytotoxicity testing of medical devices. Biomed. Rep. 2015, 3, 617–620. [Google Scholar] [CrossRef] [Green Version]
- Tang, Y.; Lan, X.; Liang, C.; Zhong, Z.; Xie, R.; Zhou, Y.; Miao, X.; Wang, H.; Wang, W. Honey loaded alginate/PVA nanofibrous membrane as potential bioactive wound dressing. Carbohydr. Polym. 2019, 219, 113–120. [Google Scholar] [CrossRef]
- A Minden-Birkenmaier, B.; Neuhalfen, R.M.; Janowiak, B.E.; Sell, S.A. Preliminary Investigation and Characterization of Electrospun Polycaprolactone and Manuka Honey Scaffolds for Dermal Repair. J. Eng. Fibers Fabr. 2015, 10, 155892501501000. [Google Scholar] [CrossRef]
- Center for Devices and Radiological Health—U.S. Food and Drug Administration. Medical Devices. Available online: https://www.fda.gov/medical-devices (accessed on 14 May 2023).
- EMA. Scientific Guidelines. European Medicines Agency. Available online: https://www.ema.europa.eu/en/human-regulatory/research-development/scientific-guidelines (accessed on 14 May 2023).
- China’s National Medical Products Administration (NMPA). Global Regulatory Partners, Inc. Available online: https://globalregulatorypartners.com/countries/china-national-national-medical-products-administration-nmpa/ (accessed on 14 May 2023).
- TGA. Therapeutic Goods Administration (TGA). Available online: https://www.tga.gov.au/ (accessed on 14 May 2023).
- HSA. Guidance Documents for Medical Devices. HSA. Available online: https://www.hsa.gov.sg/medical-devices/guidance-documents (accessed on 14 May 2023).
- Guideline—Medical Device Authority (MDA). Portal.mda.gov.my. Available online: https://portal.mda.gov.my/doc-list/guideline.html (accessed on 14 May 2023).
- Assakina, L. FAQ: Product Registration. National Pharmaceutical Regulatory Agency (NPRA). Available online: https://www.npra.gov.my/index.php/en/component/content/article/37-english/faq/623-product-registration.html?Itemid=1391 (accessed on 14 May 2023).
- Ministry of Health. Drug Registration Guidance Document (DRGD). Available online: https://www.npra.gov.my/easyarticles/images/users/1153/DRGD%20January%202023/Complete-Drug-Registration-Guidance-Document-DRGD-3rd-Edition-3rd-Revision-July-2022.pdf (accessed on 14 May 2023).
- Young, M.; Smith, M.A. Standard and Evaluation of Healthcare Quality, Safety, and Person Centered Care; PubMed; StatPearls Publishing: Philadelphia, PA, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK576432/ (accessed on 14 May 2023).
- Heerschap, C.; Nicholas, A.; Whitehead, M. Wound management: Investigating the interprofessional decision-making process. Int. Wound J. 2018, 16, 233–242. [Google Scholar] [CrossRef] [Green Version]
- Mayfield, D.L. Medical Patents and How New Instruments or Medications Might Be Patented. Mo. Med. 2016, 113, 456–462. [Google Scholar] [PubMed]
- Bhattacharya, S.; Saha, C. Intellectual property rights: An overview and implications in pharmaceutical industry. J. Adv. Pharm. Technol. Res. 2011, 2, 88–93. [Google Scholar] [CrossRef]
- Gwak, J.H.; Sohn, S.Y. Identifying the trends in wound-healing patents for successful investment strategies. PLoS ONE 2017, 12, e0174203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laurano, R.; Boffito, M.; Ciardelli, G.; Chiono, V. Wound dressing products: A translational investigation from the bench to the market. Eng. Regen. 2022, 3, 182–200. [Google Scholar] [CrossRef]
- Sen, C.K.; Gordillo, G.M.; Roy, S.; Kirsner, R.; Lambert, L.; Hunt, T.K.; Gottrup, F.; Gurtner, G.C.; Longaker, M.T. Human skin wounds: A major and snowballing threat to public health and the economy. Wound Repair Regen. 2009, 17, 763–771. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caskey, P.R. Use of Honey in Dressings. U.S. Patent US7714183B2, 11 May 2010. Available online: https://patents.google.com/patent/US7714183B2/en (accessed on 14 May 2023).
- Edmonds, J.W. Wound Dressings Comprising a Carboxymethyl Cellulose Fabric Impregnated with Honey. WIPO (PCT) WO2002087644A1, 7 November 2002. Available online: https://patents.google.com/patent/WO2002087644A1/en (accessed on 14 May 2023).
- Mousa, M.A. Honey Preparations. U.S. Patent US5980875A, 11 November 1999. Available online: https://patents.google.com/patent/US5980875A/en?oq=US5980875A+ (accessed on 14 May 2023).
- Payne, H.K.; Devenish, G.F. Honey Impregnated Composite Dressing Having Super Absorbency and Intelligent Management of Wound Exudate and Method of Making Same. U.S. Patent US9107974B2, 18 August 2015. Available online: https://patents.google.com/patent/US9107974B2/en (accessed on 14 May 2023).
- Peter, T. Therapeutic Honey and Method of Producing Same. AU Patent AU2006272366B2, 22 September 2011. Available online: https://patents.google.com/patent/AU2006272366B2/en (accessed on 14 May 2023).
- Wardell, M.R. Wound Healing Compositions Comprising Buckwheat Honey and Methylglyoxal and Methods of Use. U.S. Patent 10500235, 10 December 2019. Available online: https://patents.google.com/patent/US10500235B2/en (accessed on 14 May 2023).
- Cotton, S. Compositions and Dressings for the Treatment of Wounds. WIPO (PCT) WO2007045931A2, 26 April 2007. Available online: https://patents.google.com/patent/WO2007045931A2/en (accessed on 14 May 2023).
- Molan, P. Honey Based Wound Dressing. U.S. Patent US6956144B2, 18 October 2005. Available online: https://patents.google.com/patent/US6956144B2/en (accessed on 14 May 2023).
- Roy, P.; Lewis, M. Improvements in and Relating to the Use of Honey in Dressing. AU Patent AU2007100007A4, 1 February 2007. Available online: https://patents.google.com/patent/AU2007100007A4/en (accessed on 14 May 2023).
- Pieper, B. Honey-Based Dressings and Wound Care. J. Wound Ostomy Cont. Nurs. 2009, 36, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Clark, M.; Adcock, L. Honey for Wound Management: A Review of Clinical Effectiveness and Guidelines. Canadian Agency for Drugs and Technologies in Health. Ottawa, Canada. 2018. Available online: https://www.ncbi.nlm.nih.gov/books/NBK538361/#_ncbi_dlg_cpyrght_NBK538361 (accessed on 14 May 2023).
- Nguyen, H.M.; Le, T.T.N.; Nguyen, A.T.; Le, H.N.T.; Pham, T.T. Biomedical materials for wound dressing: Recent advances and applications. RSC Adv. 2023, 13, 5509–5528. [Google Scholar] [CrossRef]
- U.S. Food & Drug Administration. 510(k) Summary for Derma Sciences Medihoney Gel Dressings with Active Manuka Honey. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf8/K080315.pdf (accessed on 14 May 2023).
- Medline. TheraHoney: Honey Wound Dressings. Available online: https://www.medline.com/media/catalog/Docs/MKT/LIT241_BRO_TheraHoney_1673178.pdf (accessed on 14 May 2023).
- Actilite Manuka Honey Impregnated Tulle Dressing. Available online: https://medicaldressings.co.uk/actilite-manuka-honey-impregnated-tulle-dressing/ (accessed on 14 May 2023).
- Algivon—100% Manuka Honey. Advancis Medical. Available online: https://uk.advancismedical.com/products/algivon (accessed on 14 May 2023).
- Medline. 100% Medical Grade Manuka Honey. Available online: https://www.medline.com/media/catalog/Docs/MKT/manuka%20honey%20v4.pdf (accessed on 14 May 2023).




| Bioactive Substances | Advantages | Disadvantages | References |
|---|---|---|---|
| Honey |
|
| [20] |
| Epidermal Growth Factor |
|
| [75] |
| ECM Protein |
|
| [76] |
| Silver sulfadiazine |
|
| [77] |
| Type of Formulation | Formulation Matrices | Percentage of Honey in the Formulation | Site of Application | Findings | References |
|---|---|---|---|---|---|
| Cellulose hydrogel | Sodium carbomethyl cellulose (SCMC)/hydroxypropyl methyl cellulose (HPMC)/polyethylene glycol (PEG)/honey | Kelulut honey (22%) Tualang honey (22%) Asian honey (33%) | Human skin fibroblast cells | All samples showed higher cell viability (<90–100%) compared to control group. Kelulut honey > Asian honey > Tualang honey. | [23] |
| Hybrid hydrogel film | 6% w/w PVA/3, 6, 10% w/w borax/honey | 5 g honey | Human fibroblast cells | All samples with different borax concentrations showed <90% cell viability compared to control group. | [25] |
| Hybrid hydrogel | Cellulose/poly(lactic-co-glycolic acid)(PLGA)/Kelulut honey | Not stated | Human skin fibroblast cell | Honey hydrogel showed maximum cell viability with 218.35 ± 7.80% compared to control. | [84] |
| Nanofibrous hydrogel | Pomegranate/PVA/honey | Manuka honey: 25% Bee venom honey: 0.01% Lyophilized multiflora honey: 25% | L929 mouse fibroblast cells | All hydrogel scaffolds with different concentrations (and different types of honey) showed <100% cell viability compared to control group, which indicates that all hydrogels have no cytotoxicity against skin cells. Promotes cell migration and proliferation. | [85] |
| Hybrid hydrogel | 3% v/v chitosan/5% w/v gelatin/10% w/v PVA/Iran honey | 0, 5, 10, and 20% v/v honey | Human fibroblast cells | Chitosan-based hydrogel showed non-toxicity impacts on the cells, and showed highest biocompatibility. It demonstrated that the addition of honey-based hydrogel could offer the cells with nutrients and increase cell proliferation. | [99] |
| Electrospun nanofibrous hydrogel |
| 30% w/v(25, 50, 75, 100% extraction) | HFD4 human fibroblast cells |
| [100] |
| Electrospun nanofibrous hydrogel |
| 0, 5, 10, 15, and 20% v/v honey | NIH3T3 fibroblast cells |
| [103] |
| Electrospun nanofibrous hydrogel sheet | Poly(ε-caprolactone)(PCL)/Manuka honey | 1%, 5%, 10%, and 20% v/v | Fibroblast cells | Sample with 20% honey showed the highest cell viability compared to other group and control group. | [104] |
| Country Name | Regulatory Body | Regulatory Guidelines | Classification of Wound Dressings | Regulatory Requirements | References |
|---|---|---|---|---|---|
| United States | USFDA | 21 CFR Part 820 | Class I: low to moderate risk Class II: moderate to high risk Class III: high risk | Premarket approval or 510(k) application is required. | [105] |
| Europe | EMA | Council Directive 93/42/EEC | Class I: low risk Class IIa & IIb: medium risk Class III: high risk | Quality Management Systems (QMS) approval is required. | [106] |
| China | NMPA | Medical Devices Act | Class I: low to moderate risk Class II: moderate to high risk Class III: high risk | Application form is required, and need an approval before marketing. | [107] |
| Australia | TGA | Australian Therapeutic Goods Regulations | Class I: low risk Class II: medium risk | EU approval and CE markage is required. | [108] |
| Singapore | HSA | Health Product Act | Class A: Low-risk Class B: Moderate-risk Class C: High-risk Class D: In vitro diagnostic (IVD) medical devices | Approval is required. | [109] |
| Malaysia | MDA | Medical Devices Act 2012 (Act 737) | Class A: Low-risk Class B: Low to moderate-risk Class C: Moderate to high-risk Class D: High-risk | Conformity Assessment Body (CAB) approval is required. | [110] |
| Type of Patents | Inventor(s) | Issued | Assignee | Descriptions | References |
|---|---|---|---|---|---|
| US7714183B2 Use of honey in dressings | Phillip Roy Caskey | 11 May 2010 | Derma Science Inc |
| [120] |
| WO2002087644A1 Wound dressings comprising a carboxymethyl cellulose fabric impregnated with honey | James William Edmonds | 7 November 2002 | Not listed | The patent describes the wound dressings comprising honey as also containing carboxymethyl cellulose filaments in amounts up to 50% of the weight of the honey, preferably in the form of a fabric. | [121] |
| US5980875A Honey preparations | Mahmoud A. Mousa | 11 November 1999 | Not listed |
| [122] |
| US9107974B2 Honey impregnated composite dressing having super-absorbency and an intelligent management of wound exudate, and methods of making the same | Howard Kenneth Payne, Gregory Frank Devenish | 18 August 2015 | Links Medical Products Inc |
| [123] |
| AU2006272366B2 Therapeutic honey and method of producing same | Peter Taylor | 22 September 2011 | Honey Research & Development Pty Ltd. |
| [124] |
| US10500235B2 Wound healing compositions comprising buckwheat honey and methylglyoxal and methods of use | Mark R. Wardell | 10 December 2019 | San Melix Laboratories Inc, Sanmelix Laboratories Inc |
| [125] |
| WO2007045931A2 Compositions and dressings for the treatment of wounds | Stephen Cotton | 26 April 2007 | Not listed |
| [126] |
| US6956144B2 Honey-based wound dressing | Peter Molan | 18 October 2005 | ApiMed Medical Honey Ltd. |
| [127] |
| AU2007100007A4 Improvements in and Relating to the use of Honey in Dressings | Phillip Roy, Caskey, Mardi Lewis | 1 February 2007 | ApiMed Medical Honey Ltd. |
| [128] |
| Type of Dressing | Examples/Products | Intended Usage | References |
|---|---|---|---|
| Hydrocolloid Dressing | MediHoney® |
| [132] |
| Film Dressing | TheraHoney® |
| [133] |
| Foam Dressing | Actilite® |
| [134] |
| Alginate Dressing | Algivon® |
| [135] |
| Mesh Dressing | Activon® |
| [136] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yasin, S.N.N.; Said, Z.; Halib, N.; Rahman, Z.A.; Mokhzani, N.I. Polymer-Based Hydrogel Loaded with Honey in Drug Delivery System for Wound Healing Applications. Polymers 2023, 15, 3085. https://doi.org/10.3390/polym15143085
Yasin SNN, Said Z, Halib N, Rahman ZA, Mokhzani NI. Polymer-Based Hydrogel Loaded with Honey in Drug Delivery System for Wound Healing Applications. Polymers. 2023; 15(14):3085. https://doi.org/10.3390/polym15143085
Chicago/Turabian StyleYasin, Siti Nor Najihah, Zulfahmi Said, Nadia Halib, Zulaiha A Rahman, and Noor Izzati Mokhzani. 2023. "Polymer-Based Hydrogel Loaded with Honey in Drug Delivery System for Wound Healing Applications" Polymers 15, no. 14: 3085. https://doi.org/10.3390/polym15143085
APA StyleYasin, S. N. N., Said, Z., Halib, N., Rahman, Z. A., & Mokhzani, N. I. (2023). Polymer-Based Hydrogel Loaded with Honey in Drug Delivery System for Wound Healing Applications. Polymers, 15(14), 3085. https://doi.org/10.3390/polym15143085








