Amorphous Solid Dispersion as Drug Delivery Vehicles in Cancer
Abstract
1. Introduction
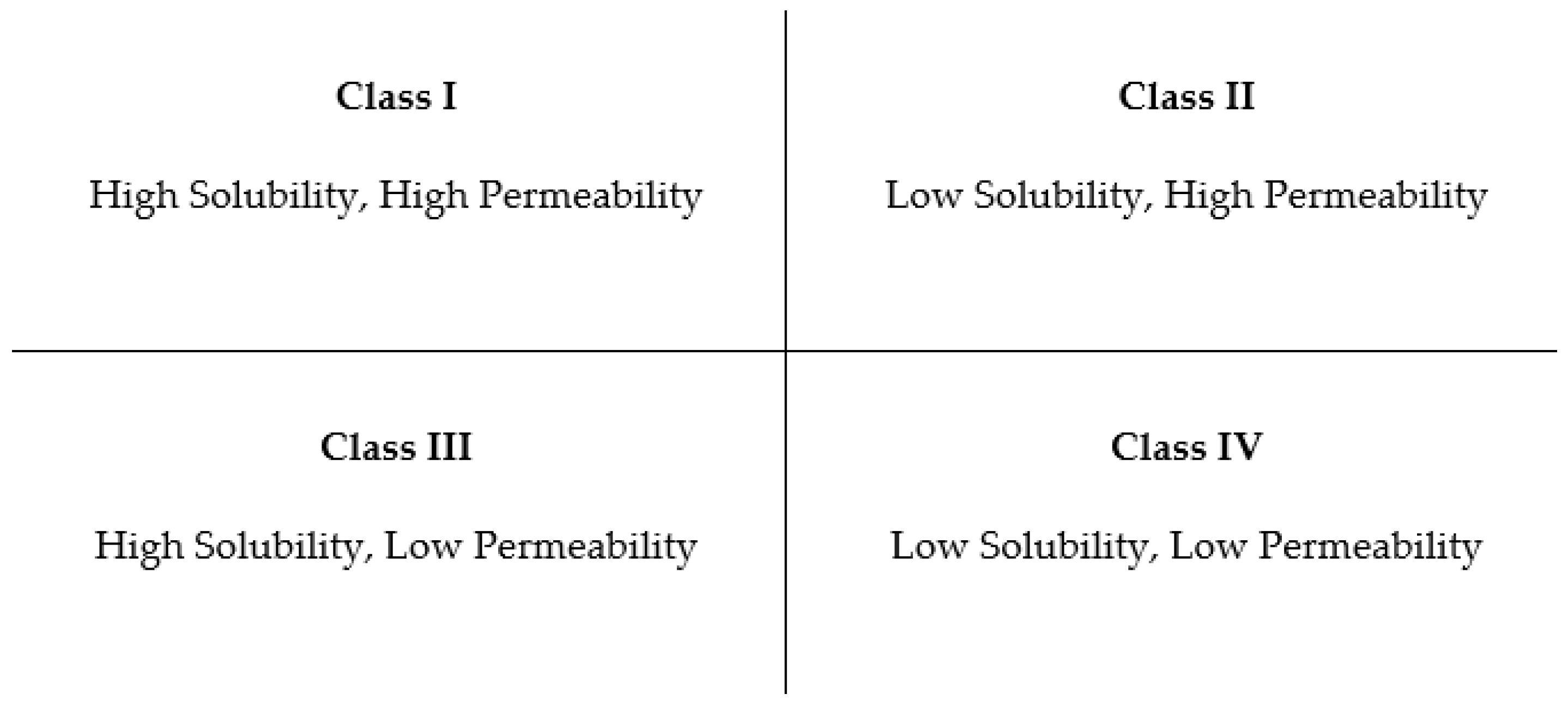
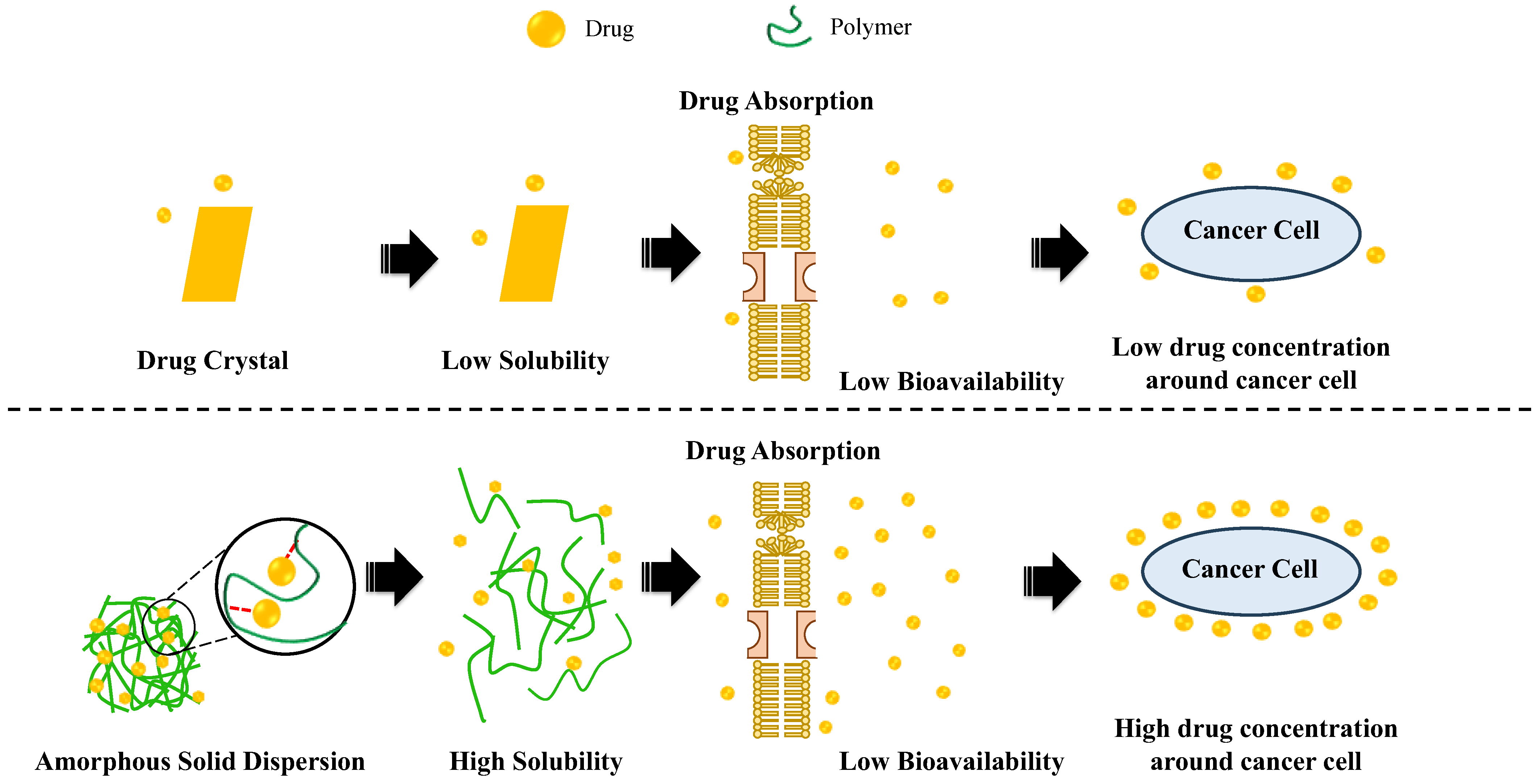
2. Anticancer Drugs
3. Amorphous Solid Dispersion
3.1. Polymers as Carrier Matrix
3.1.1. Inhibition of Drug Crystallization
3.1.2. Antiplasticization
3.1.3. Intermolecular Interaction of Drug–Polymer
3.1.4. Molecular Mobility Suppression of Amorphous Drugs in Amorphous Solid Dispersion
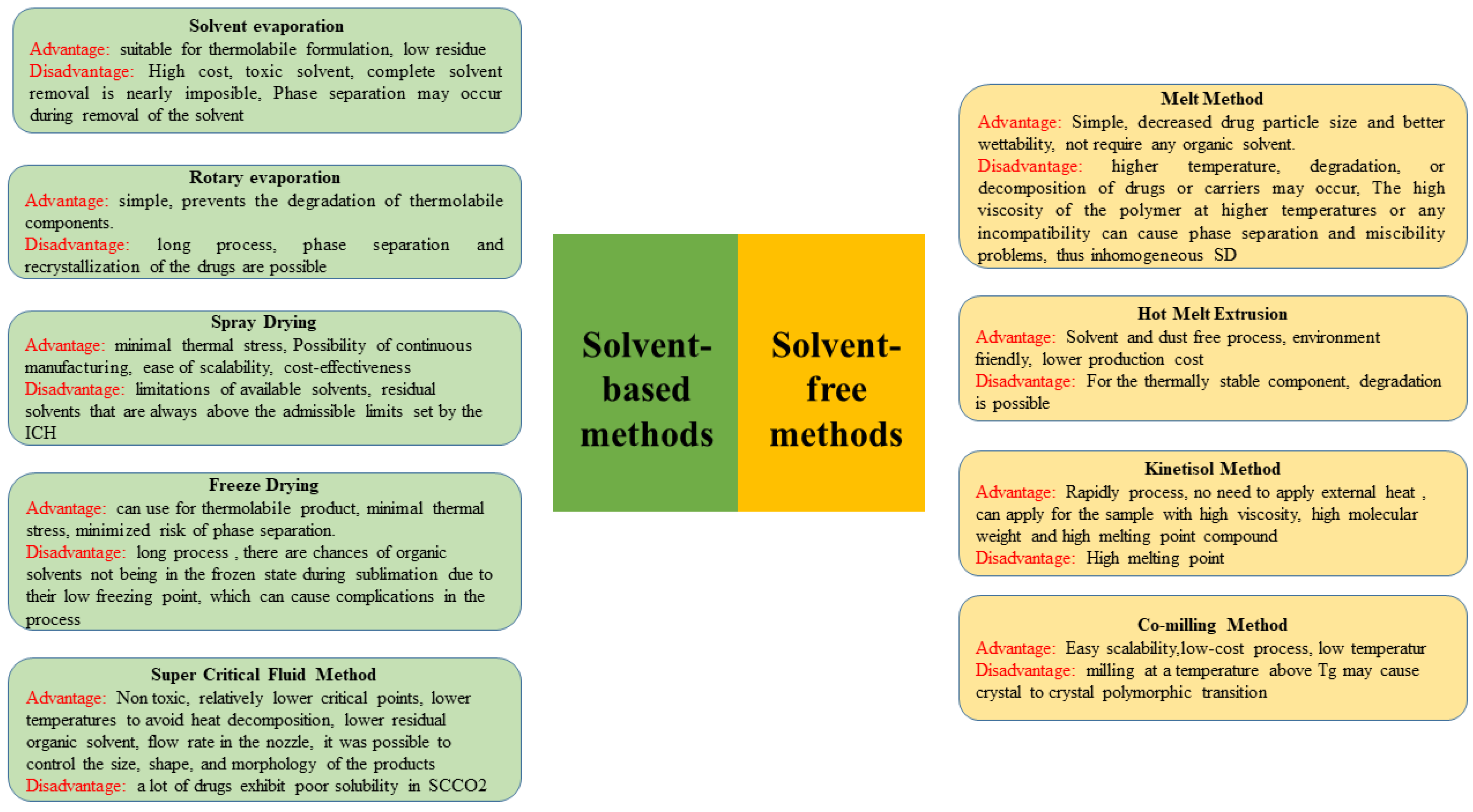
4. Preparation of ASD
4.1. Solvent-Based Methods
4.1.1. Solvent Method
4.1.2. Rotary Evaporation
4.1.3. Spray Drying
4.1.4. Freeze Drying
4.1.5. Supercritical Fluid Method
4.2. Solvent-Free Methods
4.2.1. Melting Method
4.2.2. Hot Melt Extrusion (HME)
4.2.3. Kinetisol Method
4.2.4. Co-Milling Method
5. Characterization of ASD
5.1. X-ray Powder Diffraction (XRPD)
5.2. Thermal Analysis
5.3. Spectroscopy
5.4. Water Vapor Sorption
5.5. Solid-State Nuclear Magnetic Resonance
5.6. Inverse Gas Chromatography
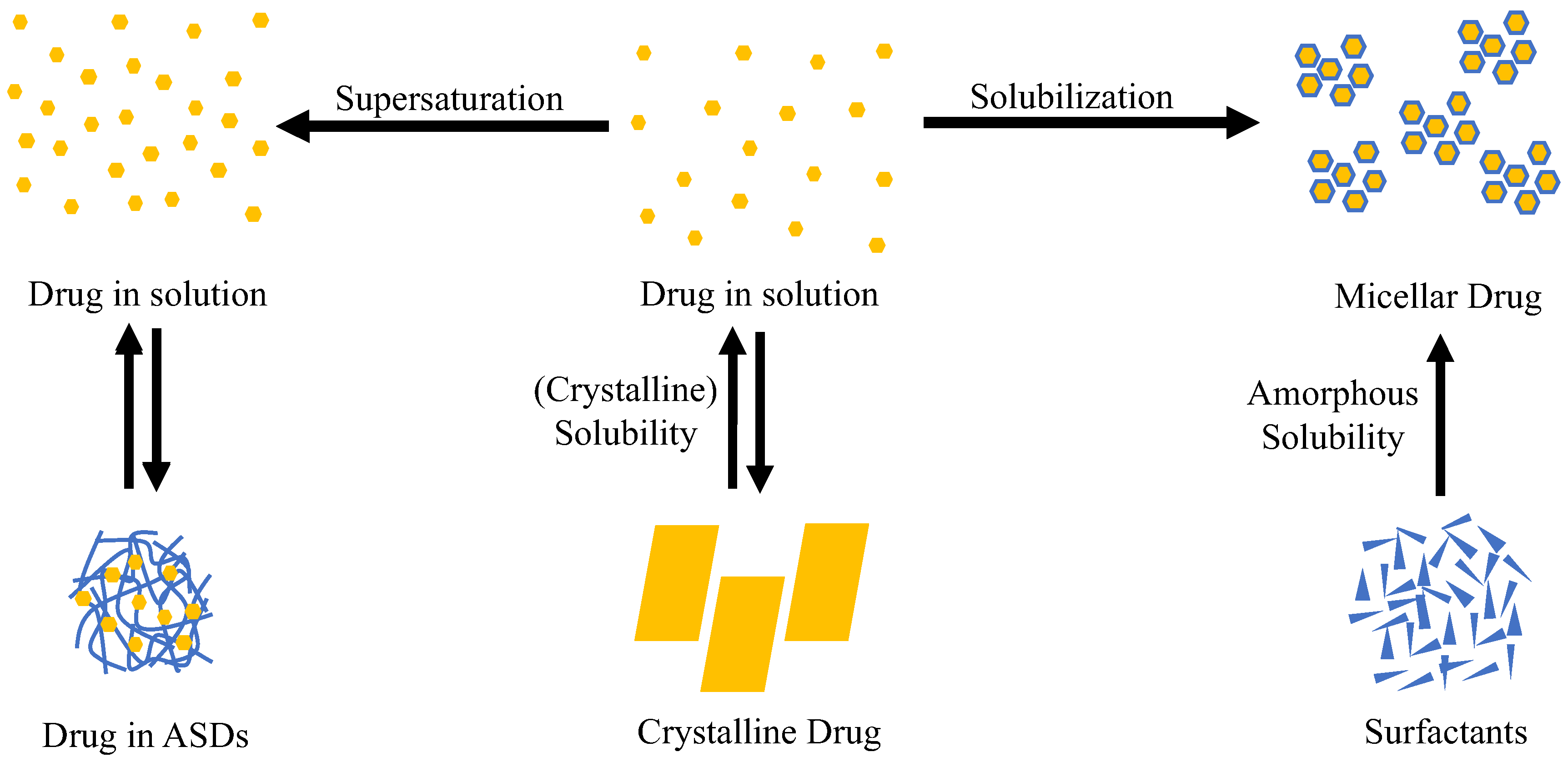
6. Dissolution of ASDs
Dissolution Mechanism
- (a)
- Carrier-controlled release. Water penetrates the polymer, causing the creation of an extremely viscous gel layer through which the drug molecules should diffuse. The concentration in the dissolving medium was controlled by that of the drug in the ASD and the volume of the release medium, resulting in a delayed release. Furthermore, drug-rich particles were formed when the amorphous solubility limit was exceeded.
- (b)
- Congruent release (dissolution-controlled release). Drug and polymer were released quickly and simultaneously into the dissolving solvent, creating a noticeable supersaturation effect. In this case, the polymer played a crucial role in stabilizing the supersaturated condition in solution. The overall medication dose and the volume of the release medium regulate the supersaturation concentration.
- (c)
- Controlled drug release. The polymer dissolved in the medium, leaving the amorphous drug to dissolve at a drug-controlled rate. There is a possibility of the crystallization of the drug when employing this technique. Furthermore, the formation of drug-rich particles was theoretically possible when the amorphous state of the medications was stable enough. However, no experimental data pertaining to this review were identified.
7. Stability of Amorphous Solid Dispersion
7.1. Factor Affecting Stability
7.1.1. Thermodynamic Aspect
7.1.2. Molecular Mobility
7.1.3. Temperature
7.1.4. Moisture
8. ASD for Cancer Therapy
9. Discussion
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Torre, L.A.; Bray, F.; Siegel, R.L.; Ferlay, J.; Lortet-Tieulent, J.; Jemal, A. Global Cancer Statistics, 2012. CA Cancer J. Clin. 2015, 65, 87–108. [Google Scholar] [CrossRef] [PubMed]
- Haberman, A. MIT Study Finds That the Probability of Clinical Trial Success Is Nearly 40% Higher than Previously Thought. Available online: https://biopharmconsortium.com/2018/03/14/mit-study-finds-that-the-probability-of-clinical-trial-success-is-nearly-40-higher-than-previously-thought/ (accessed on 24 June 2023).
- Adams, D.J. The Valley of Death in Anticancer Drug Development: A Reassessment. Trends Pharmacol. Sci. 2012, 33, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Di, L.; Fish, P.V.; Mano, T. Bridging Solubility between Drug Discovery and Development. Drug Discov. Today 2012, 17, 486–495. [Google Scholar] [CrossRef] [PubMed]
- Hoelder, S.; Clarke, P.A.; Workman, P. Discovery of Small Molecule Cancer Drugs: Successes, Challenges and Opportunities. Mol. Oncol. 2012, 6, 155–176. [Google Scholar] [CrossRef] [PubMed]
- Tran, P.; Pyo, Y.-C.; Kim, D.-H.; Lee, S.-E.; Kim, J.-K.; Park, J.-S. Overview of the Manufacturing Methods of Solid Dispersion Technology for Improving the Solubility of Poorly Water-Soluble Drugs and Application to Anticancer Drugs. Pharmaceutics 2019, 11, 132. [Google Scholar] [CrossRef] [PubMed]
- Sawicki, E.; Schellens, J.H.M.; Beijnen, J.H.; Nuijen, B. Inventory of Oral Anticancer Agents: Pharmaceutical Formulation Aspects with Focus on the Solid Dispersion Technique. Cancer Treat. Rev. 2016, 50, 247–263. [Google Scholar] [CrossRef] [PubMed]
- Truong, D.H.; Tran, T.H.; Ramasamy, T.; Choi, J.Y.; Choi, H.-G.; Yong, C.S.; Kim, J.O. Preparation and Characterization of Solid Dispersion Using a Novel Amphiphilic Copolymer to Enhance Dissolution and Oral Bioavailability of Sorafenib. Powder Technol. 2015, 283, 260–265. [Google Scholar] [CrossRef]
- Boudou-Rouquette, P.; Narjoz, C.; Golmard, J.L.; Thomas-Schoemann, A.; Mir, O.; Taieb, F.; Durand, J.-P.; Coriat, R.; Dauphin, A.; Vidal, M.; et al. Early Sorafenib-Induced Toxicity Is Associated with Drug Exposure and UGTIA9 Genetic Polymorphism in Patients with Solid Tumors: A Preliminary Study. PLoS ONE 2012, 7, e42875. [Google Scholar] [CrossRef]
- Boudou-Rouquette, P.; Ropert, S.; Mir, O.; Coriat, R.; Billemont, B.; Tod, M.; Cabanes, L.; Franck, N.; Blanchet, B.; Goldwasser, F. Variability of Sorafenib Toxicity and Exposure over Time: A Pharmacokinetic/Pharmacodynamic Analysis. Oncologist 2012, 17, 1204–1212. [Google Scholar] [CrossRef]
- Straubinger, R.M. Biopharmaceutics of Paclitaxel (Taxol): Formulation, Activity, and Pharmacokinetics, 1st ed.; Suffness, M., Ed.; CRC Press: Boca Raton, FL, USA, 1995. [Google Scholar]
- Weiss, R.B.; Donehower, R.C.; Wiernik, P.H.; Ohnuma, T.; Gralla, R.J.; Trump, D.L.; Baker, J.R.; Van Echo, D.A.; Von Hoff, D.D.; Leyland-Jones, B. Hypersensitivity Reactions from Taxol. J. Clin. Oncol. 1990, 8, 1263–1268. [Google Scholar] [CrossRef]
- Rowinsky, E.K.; Eisenhauer, E.A.; Chaudhry, V.; Arbuck, S.G.; Donehower, R.C. Clinical Toxicities Encountered with Paclitaxel (Taxol). Semin. Oncol. 1993, 20, 1–15. [Google Scholar] [PubMed]
- Holm, T.P.; Kokott, M.; Knopp, M.M.; Boyd, B.J.; Berthelsen, R.; Quodbach, J.; Löbmann, K. Development of a Multiparticulate Drug Delivery System for In Situ Amorphisation. Eur. J. Pharm. Biopharm. 2022, 180, 170–180. [Google Scholar] [CrossRef] [PubMed]
- Bi, Y.; Xiao, D.; Ren, S.; Bi, S.; Wang, J.; Li, F. The Binary System of Ibuprofen-Nicotinamide Under Nanoscale Confinement: From Cocrystal to Coamorphous State. J. Pharm. Sci. 2017, 106, 3150–3155. [Google Scholar] [CrossRef] [PubMed]
- Azad, M.; Moreno, J.; Davé, R. Stable and Fast-Dissolving Amorphous Drug Composites Preparation via Impregnation of Neusilin® UFL2. J. Pharm. Sci. 2018, 107, 170–182. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, K.; Kojima, T.; Karashima, M.; Ikeda, Y. Physicochemical Evaluation and Developability Assessment of Co-Amorphouses of Low Soluble Drugs and Comparison to the Co-Crystals. Chem. Pharm. Bull. 2016, 64, 1739–1746. [Google Scholar] [CrossRef] [PubMed]
- Van den Mooter, G. The Use of Amorphous Solid Dispersions: A Formulation Strategy to Overcome Poor Solubility and Dissolution Rate. Drug Discov. Today Technol. 2012, 9, e79–e85. [Google Scholar] [CrossRef] [PubMed]
- Pandi, P.; Bulusu, R.; Kommineni, N.; Khan, W.; Singh, M. Amorphous Solid Dispersions: An Update for Preparation, Characterization, Mechanism on Bioavailability, Stability, Regulatory Considerations and Marketed Products. Int. J. Pharm. 2020, 586, 119560. [Google Scholar] [CrossRef]
- Jermain, S.V.; Brough, C.; Williams, R.O. Amorphous Solid Dispersions and Nanocrystal Technologies for Poorly Water-Soluble Drug Delivery—An Update. Int. J. Pharm. 2018, 535, 379–392. [Google Scholar] [CrossRef]
- Shah, N.; Iyer, R.M.; Mair, H.-J.; Choi, D.; Tian, H.; Diodone, R.; Fahnrich, K.; Pabst-Ravot, A.; Tang, K.; Scheubel, E.; et al. Improved Human Bioavailability of Vemurafenib, a Practically Insoluble Drug, Using an Amorphous Polymer-Stabilized Solid Dispersion Prepared by a Solvent-Controlled Coprecipitation Process. J. Pharm. Sci. 2013, 102, 967–981. [Google Scholar] [CrossRef]
- Barros, A.A.A.; Alves, A.; Nunes, C.; Coimbra, M.A.; Pires, R.A.; Reis, R.L. Carboxymethylation of Ulvan and Chitosan and Their Use as Polymeric Components of Bone Cements. Acta Biomater. 2013, 9, 9086–9097. [Google Scholar] [CrossRef]
- Blagden, N.; de Matas, M.; Gavan, P.T.; York, P. Crystal Engineering of Active Pharmaceutical Ingredients to Improve Solubility and Dissolution Rates. Adv. Drug Deliv. Rev. 2007, 59, 617–630. [Google Scholar] [CrossRef]
- Veber, D.F.; Johnson, S.R.; Cheng, H.-Y.; Smith, B.R.; Ward, K.W.; Kopple, K.D. Molecular Properties That Influence the Oral Bioavailability of Drug Candidates. J. Med. Chem. 2002, 45, 2615–2623. [Google Scholar] [CrossRef] [PubMed]
- Baghel, S.; Cathcart, H.; O’Reilly, N.J. Polymeric Amorphous Solid Dispersions: A Review of Amorphization, Crystallization, Stabilization, Solid-State Characterization, and Aqueous Solubilization of Biopharmaceutical Classification System Class II Drugs. J. Pharm. Sci. 2016, 105, 2527–2544. [Google Scholar] [CrossRef] [PubMed]
- Fizazi, K.; Tran, N.; Fein, L.; Matsubara, N.; Rodriguez-Antolin, A.; Alekseev, B.Y.; Özgüroğlu, M.; Ye, D.; Feyerabend, S.; Protheroe, A.; et al. Abiraterone plus Prednisone in Metastatic, Castration-Sensitive Prostate Cancer. N. Engl. J. Med. 2017, 377, 352–360. [Google Scholar] [CrossRef] [PubMed]
- National Center for Biotechnology Information PubChem Compound Summary for CID 9821849, Abiraterone Acetate. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Abiraterone-acetate (accessed on 5 July 2023).
- Rini, B.I.; Escudier, B.; Tomczak, P.; Kaprin, A.; Szczylik, C.; Hutson, T.E.; Michaelson, M.D.; Gorbunova, V.A.; Gore, M.E.; Rusakov, I.G.; et al. Comparative Effectiveness of Axitinib versus Sorafenib in Advanced Renal Cell Carcinoma (AXIS): A Randomised Phase 3 Trial. Lancet 2011, 378, 1931–1939. [Google Scholar] [CrossRef] [PubMed]
- National Center for Biotechnology Information PubChem Compound Summary for CID 6450551, Axitinib. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Axitinib (accessed on 5 July 2023).
- Cortes, J.E.; Gambarcorti-Passerini, C. Final Analysis of the Efficacy and Safety of Bosutinib in the Treatment of Chronic Phase Chronic Myeloid Leukemia Patients with Resistance or Intolerance to Imatinib. Blood Cancer Journal. Blood Cancer J. 2018, 8, 69. [Google Scholar]
- National Center for Biotechnology Information PubChem Compound Summary for CID 11990828, Bosutinib Monohydrate. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Bosutinib-monohydrate (accessed on 5 July 2023).
- Schlumberger, M.; Jarzab, B.; Cabanillas, M.E.; Robinson, B.; Pacini, F.; Ball, D.W.; McCaffrey, J.; Newbold, K.; Allison, R.; Martins, R.G.; et al. A Phase II Trial of the Multitargeted Tyrosine Kinase Inhibitor Lenvatinib (E7080) in Advanced Medullary Thyroid Cancer. Clin. Cancer Res. 2016, 22, 44–53. [Google Scholar] [CrossRef]
- National Center for Biotechnology Information PubChem Compound Summary for CID 25102847, Cabozantinib. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Cabozantinib (accessed on 5 July 2023).
- Shaw, A.T.; Solomon, B.J.; Besse, B.; Bauer, T.M.; Lin, C.-C.; Soo, R.A.; Riely, G.J.; Ou, S.-H.I.; Clancy, J.S.; Li, S.; et al. ALK Resistance Mutations and Efficacy of Lorlatinib in Advanced Anaplastic Lymphoma Kinase-Positive Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2019, 37, 1370–1379. [Google Scholar] [CrossRef]
- Soria, J.-C.; Tan, D.S.W.; Chiari, R.; Wu, Y.-L.; Paz-Ares, L.; Wolf, J.; Geater, S.L.; Orlov, S.; Cortinovis, D.; Yu, C.-J.; et al. First-Line Ceritinib versus Platinum-Based Chemotherapy in Advanced ALK -Rearranged Non-Small-Cell Lung Cancer (ASCEND-4): A Randomised, Open-Label, Phase 3 Study. Lancet 2017, 389, 917–929. [Google Scholar] [CrossRef]
- National Center for Biotechnology Information PubChem Compound Summary for CID 57379345, Ceritinib. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Ceritinib (accessed on 5 July 2023).
- Long, G.V.; Stroyakovskiy, D.; Gogas, H.; Levchenko, E.; de Braud, F.; Larkin, J.; Garbe, C.; Jouary, T.; Hauschild, A.; Grob, J.-J.; et al. Dabrafenib and Trametinib versus Dabrafenib and Placebo for Val600 BRAF-Mutant Melanoma: A Multicentre, Double-Blind, Phase 3 Randomised Controlled Trial. Lancet 2015, 386, 444–451. [Google Scholar] [CrossRef]
- Pubchem Dabrafenib. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Dabrafenib (accessed on 6 June 2023).
- Zhang, L.; Ma, S. Effect of Erlotinib in Combination with Chemotherapy on EGFR-Mutated Non-Small Cell Lung Cancer: A Meta-Analysis. Int. J. Clin. Exp. Pathol. 2020, 13, 2590–2600. [Google Scholar]
- Pubchem Erlotinib. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Erlotinib (accessed on 6 June 2023).
- Xu, Z.; Zhang, Y.; Li, N.; Liu, P.; Gao, L.; Gao, X.; Tie, X. Efficacy and Safety of Lapatinib and Trastuzumab for HER2-Positive Breast Cancer: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. BMJ Open 2017, 7, e013053. [Google Scholar] [CrossRef] [PubMed]
- Pubchem Lapatinib. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Lapatinib (accessed on 6 June 2023).
- Stone, R.M.; Mandrekar, S.J.; Sanford, B.L.; Laumann, K.; Geyer, S.; Bloomfield, C.D.; Thiede, C.; Prior, T.W.; Döhner, K.; Marcucci, G.; et al. Midostaurin plus Chemotherapy for Acute Myeloid Leukemia with a FLT3 Mutation. N. Engl. J. Med. 2017, 377, 454–464. [Google Scholar] [CrossRef] [PubMed]
- Pubchem Midostaurin. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Midostaurin (accessed on 6 June 2023).
- Chan, A.; Delaloge, S.; Holmes, F.A.; Moy, B.; Iwata, H.; Harvey, V.J.; Robert, N.J.; Silovski, T.; Gokmen, E.; von Minckwitz, G.; et al. Neratinib after Trastuzumab-Based Adjuvant Therapy in Patients with HER2-Positive Breast Cancer (ExteNET): A Multicentre, Randomised, Double-Blind, Placebo-Controlled, Phase 3 Trial. Lancet Oncol. 2016, 17, 367–377. [Google Scholar] [CrossRef] [PubMed]
- FDA NERLYNX (Neratinib) Tablets. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/208051s000lbl.pdf (accessed on 24 June 2023).
- Kantarjian, H.M.; Giles, F.J.; Bhalla, K.N.; Pinilla-Ibarz, J.; Larson, R.A.; Gattermann, N.; Ottmann, O.G.; Hochhaus, A.; Radich, J.P.; Saglio, G.; et al. Nilotinib Is Effective in Patients with Chronic Myeloid Leukemia in Chronic Phase after Imatinib Resistance or Intolerance: 24-Month Follow-up Results. Blood 2011, 117, 1141–1145. [Google Scholar] [CrossRef] [PubMed]
- Pubchem Nilotinib. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Nilotinib (accessed on 6 June 2023).
- Liu, X.; Wang, Q.; Yang, G. Nintedanib Promotes Antitumor Immunity and Inhibits Hepatocellular Carcinoma Growth: A Potential Combination Therapy with Sorafenib. Gut 2019, 68, 672–685. [Google Scholar]
- Pubchem Nintedanib. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Nintedanib#section=Solubility (accessed on 6 June 2023).
- Sternberg, C.N.; Davis, I.D.; Mardiak, J.; Szczylik, C.; Lee, E.; Wagstaff, J.; Barrios, C.H.; Salman, P.; Gladkov, O.A.; Kavina, A.; et al. Pazopanib in Locally Advanced or Metastatic Renal Cell Carcinoma: Results of a Randomized Phase III Trial. J. Clin. Oncol. 2010, 28, 1061–1068. [Google Scholar] [CrossRef]
- Pubchem Pazopanib. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Pazopanib (accessed on 6 June 2023).
- Dlugosz, A.A.; Talpaz, M.; Neubauer, M. Phase I Trial of the Hedgehog Pathway Inhibitor Sonidegib (LDE225) in Advanced Solid Tumors. Clin. Cancer Res. 2015, 21, 1302–1309. [Google Scholar]
- European Medicines Agency Odomzo International Non-Proprietary Name: Sonidegib. Available online: https://www.ema.europa.eu/en/documents/assessment-report/odomzo-epar-public-assessment-report_en.pdf (accessed on 24 June 2023).
- Robert, C.; Karaszewska, B.; Schachter, J.; Rutkowski, P.; Mackiewicz, A.; Stroiakovski, D.; Lichinitser, M.; Dummer, R.; Grange, F.; Mortier, L.; et al. Improved Overall Survival in Melanoma with Combined Dabrafenib and Trametinib. N. Engl. J. Med. 2015, 372, 30–39. [Google Scholar] [CrossRef]
- FDA Center for Drug Evaluation and Research, Application Number: 204114Orig1s000 Clinical Pharmacology and Biopharmaceutics Review(s). Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2013/204114orig1s000clinpharmr.pdf (accessed on 24 June 2023).
- Flaherty, K.T.; Infante, J.R.; Daud, A.; Gonzalez, R.; Kefford, R.F.; Sosman, J.; Hamid, O.; Schuchter, L.; Cebon, J.; Ibrahim, N.; et al. Combined BRAF and MEK Inhibition in Melanoma with BRAF V600 Mutations. N. Engl. J. Med. 2012, 367, 1694–1703. [Google Scholar] [CrossRef]
- Pubchem Vemurafenib. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Vemurafenib (accessed on 6 June 2023).
- Grothey, A.; Van Cutsem, E.; Sobrero, A.; Siena, S.; Falcone, A.; Ychou, M.; Humblet, Y.; Bouché, O.; Mineur, L.; Barone, C.; et al. Regorafenib Monotherapy for Previously Treated Metastatic Colorectal Cancer (CORRECT): An International, Multicentre, Randomised, Placebo-Controlled, Phase 3 Trial. Lancet 2013, 381, 303–312. [Google Scholar] [CrossRef] [PubMed]
- FDA Center for Drug Evaluation and Research, Application Number: 204369Orig1s000 Clinical Pharmacology and Biopharmaceutics Review(s). Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2013/204369orig1s000clinpharmr.pdf (accessed on 24 June 2023).
- Singh, S.S.; Saluja, S.S. Everolimus in Advanced Hormone Receptor-Positive, HER2-Negative Breast Cancer: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Breast Cancer Res. Treat. 2021, 185, 147–160. [Google Scholar]
- FDA Center for Drug Evaluation and Research, Application Number: 203985Orig1s000 Clinical Pharmacology and Biopharmaceutics Review(s). Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/203985Orig1s000ClinPharmR.pdf (accessed on 24 June 2023).
- Wei, A.H.; Montesinos, P.; Ivanov, V.; DiNardo, C.D.; Novak, J.; Laribi, K.; Kim, I.; Stevens, D.A.; Fiedler, W.; Pagoni, M.; et al. Venetoclax plus LDAC for Newly Diagnosed AML Ineligible for Intensive Chemotherapy: A Phase 3 Randomized Placebo-Controlled Trial. Blood 2020, 135, 2137–2145. [Google Scholar] [CrossRef] [PubMed]
- National Center for Biotechnology Information PubChem Compound Summary for CID 49846579, Venetoclax. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Venetoclax (accessed on 5 July 2023).
- Mateo, J.; Lord, C.J.; Serra, V.; Tutt, A.; Balmaña, J.; Castroviejo-Bermejo, M.; Cruz, C.; Oaknin, A.; Kaye, S.B.; de Bono, J.S. A Decade of Clinical Development of PARP Inhibitors in Perspective. Ann. Oncol. 2019, 30, 1437–1447. [Google Scholar] [CrossRef] [PubMed]
- National Center for Biotechnology Information PubChem Compound Summary for CID 23725625, Olaparib. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Olaparib (accessed on 5 July 2023).
- Shekunov, B. Kinetics of Crystallization and Glass Transition in Amorphous Materials. Cryst. Growth Des. 2020, 20, 95–106. [Google Scholar] [CrossRef]
- Vo, C.L.-N.; Park, C.; Lee, B.-J. Current Trends and Future Perspectives of Solid Dispersions Containing Poorly Water-Soluble Drugs. Eur. J. Pharm. Biopharm. 2013, 85, 799–813. [Google Scholar] [CrossRef] [PubMed]
- Gibaldi, M.; Feldman, S. Establishment of Sink Conditions in Dissolution Rate Determinations. Theoretical Considerations and Application to Nondisintegrating Dosage Forms. J. Pharm. Sci. 1967, 56, 1238–1242. [Google Scholar] [CrossRef]
- Al-Obaidi, H.; Brocchini, S.; Buckton, G. Anomalous Properties of Spray Dried Solid Dispersions. J. Pharm. Sci. 2009, 98, 4724–4737. [Google Scholar] [CrossRef]
- Baldrick, P. Pharmaceutical Excipient Testing—A Regulatory and Preclinical Perspective, 4th ed.; Swarbick, J., Ed.; CRC Press: Boca Raton, FL, USA, 2013. [Google Scholar]
- Zhang, S.; Lee, T.W.Y.; Chow, A.H.L. Thermodynamic and Kinetic Evaluation of the Impact of Polymer Excipients on Storage Stability of Amorphous Itraconazole. Int. J. Pharm. 2019, 555, 394–403. [Google Scholar] [CrossRef]
- Ueda, K.; Higashi, K.; Moribe, K. Mechanistic Elucidation of Formation of Drug-Rich Amorphous Nanodroplets by Dissolution of the Solid Dispersion Formulation. Int. J. Pharm. 2019, 561, 82–92. [Google Scholar] [CrossRef]
- Shaker, M.A.; Elbadawy, H.M.; Shaker, M.A. Improved Solubility, Dissolution, and Oral Bioavailability for Atorvastatin-Pluronic® Solid Dispersions. Int. J. Pharm. 2020, 574, 118891. [Google Scholar] [CrossRef] [PubMed]
- Smeets, A.; Koekoekx, R.; Ruelens, W.; Smet, M.; Clasen, C.; Van den Mooter, G. Gastro-Resistant Encapsulation of Amorphous Solid Dispersions Containing Darunavir by Coaxial Electrospraying. Int. J. Pharm. 2020, 574, 118885. [Google Scholar] [CrossRef] [PubMed]
- Iwashita, M.; Hashizume, K.; Umehara, M.; Ishigami, T.; Onishi, S.; Yamamoto, M.; Higashi, K.; Moribe, K. Development of Nobiletin–Methyl Hesperidin Amorphous Solid Dispersion: Novel Application of Methyl Hesperidin as an Excipient for Hot-Melt Extrusion. Int. J. Pharm. 2019, 558, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Yuvaraja, K.; Khanam, J. Enhancement of Carvedilol Solubility by Solid Dispersion Technique Using Cyclodextrins, Water Soluble Polymers and Hydroxyl Acid. J. Pharm. Biomed. Anal. 2014, 96, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, C.N.; Pham, C.V.; Le Thien, G.; Ngoc, B.T.; Le Thi, H.; Huyen, C.P.T.; Thi, T.N. Immediate-Released Pelletized Solid Dispersion Containing Fenofibrate: Formulation, In Vitro Characterization, and Bioequivalence Studies in Experimental Beagle Dogs. Int. J. Pharm. 2019, 570, 118661. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, K.; Suzuki, K.; Fukiage, M.; Matsuda, M.; Nishida, Y.; Oikawa, M.; Fujita, T. Impact of Degree of Supersaturation on the Dissolution and Oral Absorption Behaviors of Griseofulvin Amorphous Solid Dispersions. J. Drug Deliv. Sci. Technol. 2020, 56, 101172. [Google Scholar] [CrossRef]
- McFall, H.; Sarabu, S.; Shankar, V.; Bandari, S.; Murthy, S.N.; Kolter, K.; Langley, N.; Kim, D.W.; Repka, M.A. Formulation of Aripiprazole-Loaded PH-Modulated Solid Dispersions via Hot-Melt Extrusion Technology: In Vitro and In Vivo Studies. Int. J. Pharm. 2019, 554, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Monschke, M.; Wagner, K.G. Amorphous Solid Dispersions of Weak Bases with PH-Dependent Soluble Polymers to Overcome Limited Bioavailability Due to Gastric PH Variability—An In-Vitro Approach. Int. J. Pharm. 2019, 564, 162–170. [Google Scholar] [CrossRef]
- Knopp, M.M.; Olesen, N.E.; Holm, P.; Langguth, P.; Holm, R.; Rades, T. Influence of Polymer Molecular Weight on Drug–Polymer Solubility: A Comparison between Experimentally Determined Solubility in PVP and Prediction Derived from Solubility in Monomer. J. Pharm. Sci. 2015, 104, 2905–2912. [Google Scholar] [CrossRef]
- Jahangiri, A.; Barzegar-Jalali, M.; Garjani, A.; Javadzadeh, Y.; Hamishehkar, H.; Rameshrad, M.; Adibkia, K. Physicochemical Characterization and Pharmacological Evaluation of Ezetimibe-PVP K30 Solid Dispersions in Hyperlipidemic Rats. Colloids Surf. B Biointerfaces 2015, 134, 423–430. [Google Scholar] [CrossRef]
- Liu, X.; Lu, M.; Guo, Z.; Huang, L.; Feng, X.; Wu, C. Improving the Chemical Stability of Amorphous Solid Dispersion with Cocrystal Technique by Hot Melt Extrusion. Pharm. Res. 2012, 29, 806–817. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Liu, Y.; Liu, T.; Zhao, L.; Zhao, J.; Feng, N. Development and In-Vivo Assessment of the Bioavailability of Oridonin Solid Dispersions by the Gas Anti-Solvent Technique. Int. J. Pharm. 2011, 411, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Marasini, N.; Tran, T.H.; Poudel, B.K.; Cho, H.J.; Choi, Y.K.; Chi, S.-C.; Choi, H.-G.; Yong, C.S.; Kim, J.O. Fabrication and Evaluation of PH-Modulated Solid Dispersion for Telmisartan by Spray-Drying Technique. Int. J. Pharm. 2013, 441, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Nagy, Z.K.; Balogh, A.; Démuth, B.; Pataki, H.; Vigh, T.; Szabó, B.; Molnár, K.; Schmidt, B.T.; Horák, P.; Marosi, G.; et al. High Speed Electrospinning for Scaled-up Production of Amorphous Solid Dispersion of Itraconazole. Int. J. Pharm. 2015, 480, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.-D.; Sung, J.H.; Kim, K.K.; Kim, D.W.; Kim, J.O.; Lee, B.-J.; Yong, C.S.; Choi, H.-G. Novel Valsartan-Loaded Solid Dispersion with Enhanced Bioavailability and No Crystalline Changes. Int. J. Pharm. 2012, 422, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Sawicki, E.; Beijnen, J.H.; Schellens, J.H.M.; Nuijen, B. Pharmaceutical Development of an Oral Tablet Formulation Containing a Spray Dried Amorphous Solid Dispersion of Docetaxel or Paclitaxel. Int. J. Pharm. 2016, 511, 765–773. [Google Scholar] [CrossRef] [PubMed]
- Wilson, V.; Lou, X.; Osterling, D.J.; Stolarik, D.F.; Jenkins, G.; Gao, W.; Zhang, G.G.Z.; Taylor, L.S. Relationship between Amorphous Solid Dispersion In Vivo Absorption and In Vitro Dissolution: Phase Behavior during Dissolution, Speciation, and Membrane Mass Transport. J. Control. Release 2018, 292, 172–182. [Google Scholar] [CrossRef]
- Herbrink, M.; Schellens, J.H.M.; Beijnen, J.H.; Nuijen, B. Improving the Solubility of Nilotinib through Novel Spray-Dried Solid Dispersions. Int. J. Pharm. 2017, 529, 294–302. [Google Scholar] [CrossRef]
- Kadajji, V.G.; Betageri, G.V. Water Soluble Polymers for Pharmaceutical Applications. Polymers 2011, 3, 1972–2009. [Google Scholar] [CrossRef]
- Cui, Y. A Material Science Perspective of Pharmaceutical Solids. Int. J. Pharm. 2007, 339, 3–18. [Google Scholar] [CrossRef]
- Donnelly, C.; Tian, Y.; Potter, C.; Jones, D.S.; Andrews, G.P. Probing the Effects of Experimental Conditions on the Character of Drug-Polymer Phase Diagrams Constructed Using Flory-Huggins Theory. Pharm. Res. 2015, 32, 167–179. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, K. Theory and Practice of Supersaturatable Formulations for Poorly Soluble Drugs. Ther. Deliv. 2015, 6, 339–352. [Google Scholar] [CrossRef] [PubMed]
- Dengale, S.J.; Hussen, S.S.; Krishna, B.S.M.; Musmade, P.B.; Gautham Shenoy, G.; Bhat, K. Fabrication, Solid State Characterization and Bioavailability Assessment of Stable Binary Amorphous Phases of Ritonavir with Quercetin. Eur. J. Pharm. Biopharm. 2015, 89, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Shen, T.D.; Sun, B.R.; Xin, S.W. Effects of Metalloids on the Thermal Stability and Glass Forming Ability of Bulk Ferromagnetic Metallic Glasses. J. Alloys Compd. 2015, 631, 60–66. [Google Scholar] [CrossRef]
- Kozmidis-Petrović, A.F. Dynamic Fragility and Reduced Glass Transition Temperature as a Pair of Parameters for Estimating Glass Forming Ability. J. Non Cryst. Solids 2015, 417–418, 1–9. [Google Scholar] [CrossRef]
- Kawakami, K.; Harada, T.; Yoshihashi, Y.; Yonemochi, E.; Terada, K.; Moriyama, H. Correlation between Glass-Forming Ability and Fragility of Pharmaceutical Compounds. J. Phys. Chem. B 2015, 119, 4873–4880. [Google Scholar] [CrossRef] [PubMed]
- Milne, M.; Liebenberg, W.; Aucamp, M. The Stabilization of Amorphous Zopiclone in an Amorphous Solid Dispersion. AAPS PharmSciTech 2015, 16, 1190–1202. [Google Scholar] [CrossRef]
- Pina, M.F.; Pinto, J.F.; Sousa, J.J.; Craig, D.Q.M.; Zhao, M. Generation of Hydrate Forms of Paroxetine HCl from the Amorphous State: An Evaluation of Thermodynamic and Experimental Predictive Approaches. Int. J. Pharm. 2015, 481, 114–124. [Google Scholar] [CrossRef]
- Janssens, S.; Van den Mooter, G. Review: Physical Chemistry of Solid Dispersions. J. Pharm. Pharmacol. 2009, 61, 1571–1586. [Google Scholar] [CrossRef]
- Surwase, S.A.; Itkonen, L.; Aaltonen, J.; Saville, D.; Rades, T.; Peltonen, L.; Strachan, C.J. Polymer Incorporation Method Affects the Physical Stability of Amorphous Indomethacin in Aqueous Suspension. Eur. J. Pharm. Biopharm. 2015, 96, 32–43. [Google Scholar] [CrossRef]
- Tian, Y.; Jones, D.S.; Andrews, G.P. An Investigation into the Role of Polymeric Carriers on Crystal Growth within Amorphous Solid Dispersion Systems. Mol. Pharm. 2015, 12, 1180–1192. [Google Scholar] [CrossRef] [PubMed]
- Laitinen, R.; Löbmann, K.; Strachan, C.J.; Grohganz, H.; Rades, T. Emerging Trends in the Stabilization of Amorphous Drugs. Int. J. Pharm. 2013, 453, 65–79. [Google Scholar] [CrossRef] [PubMed]
- Luk, E.; Sandoval, A.J.; Cova, A.; Müller, A.J. Anti-Plasticization of Cassava Starch by Complexing Fatty Acids. Carbohydr. Polym. 2013, 98, 659–664. [Google Scholar] [CrossRef] [PubMed]
- Penzel, E.; Reigert, J.; Schneider, H.A. The Glass Transition Temperature of Random Copolymers: 1. Experimental Data and the Gordon-Taylor Equation. Polymers 1997, 38, 325–337. [Google Scholar] [CrossRef]
- Wlodarski, K.; Sawicki, W.; Kozyra, A.; Tajber, L. Physical Stability of Solid Dispersions with Respect to Thermodynamic Solubility of Tadalafil in PVP-VA. Eur. J. Pharm. Biopharm. 2015, 96, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Sathigari, S.K.; Radhakrishnan, V.K.; Davis, V.A.; Parsons, D.L.; Babu, R.J. Amorphous-State Characterization of Efavirenz—Polymer Hot-Melt Extrusion Systems for Dissolution Enhancement. J. Pharm. Sci. 2012, 101, 3456–3464. [Google Scholar] [CrossRef] [PubMed]
- Couchman, P.R.; Karasz, F.E. A Classical Thermodynamic Discussion of the Effect of Composition on Glass-Transition Temperatures. Macromolecules 1978, 11, 117–119. [Google Scholar] [CrossRef]
- Paudel, A.; Worku, Z.A.; Meeus, J.; Guns, S.; Van den Mooter, G. Manufacturing of Solid Dispersions of Poorly Water Soluble Drugs by Spray Drying: Formulation and Process Considerations. Int. J. Pharm. 2013, 453, 253–284. [Google Scholar] [CrossRef]
- Meng, F.; Trivino, A.; Prasad, D.; Chauhan, H. Investigation and Correlation of Drug Polymer Miscibility and Molecular Interactions by Various Approaches for the Preparation of Amorphous Solid Dispersions. Eur. J. Pharm. Sci. 2015, 71, 12–24. [Google Scholar] [CrossRef]
- Mistry, P.; Mohapatra, S.; Gopinath, T.; Vogt, F.G.; Suryanarayanan, R. Role of the Strength of Drug–Polymer Interactions on the Molecular Mobility and Crystallization Inhibition in Ketoconazole Solid Dispersions. Mol. Pharm. 2015, 12, 3339–3350. [Google Scholar] [CrossRef]
- Kothari, K.; Ragoonanan, V.; Suryanarayanan, R. The Role of Polymer Concentration on the Molecular Mobility and Physical Stability of Nifedipine Solid Dispersions. Mol. Pharm. 2015, 12, 1477–1484. [Google Scholar] [CrossRef] [PubMed]
- Ayenew, Z.; Paudel, A.; Van den Mooter, G. Can Compression Induce Demixing in Amorphous Solid Dispersions? A Case Study of Naproxen–PVP K25. Eur. J. Pharm. Biopharm. 2012, 81, 207–213. [Google Scholar] [CrossRef] [PubMed]
- LaFountaine, J.S.; McGinity, J.W.; Williams, R.O. Challenges and Strategies in Thermal Processing of Amorphous Solid Dispersions: A Review. AAPS PharmSciTech 2016, 17, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Lehmkemper, K.; Kyeremateng, S.O.; Heinzerling, O.; Degenhardt, M.; Sadowski, G. Impact of Polymer Type and Relative Humidity on the Long-Term Physical Stability of Amorphous Solid Dispersions. Mol. Pharm. 2017, 14, 4374–4386. [Google Scholar] [CrossRef] [PubMed]
- Tantishaiyakul, V.; Kaewnopparat, N.; Ingkatawornwong, S. Properties of Solid Dispersions of Piroxicam in Polyvinylpyrrolidone. Int. J. Pharm. 1999, 181, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Balani, P.N.; Wong, S.Y.; Ng, W.K.; Widjaja, E.; Tan, R.B.H.; Chan, S.Y. Influence of Polymer Content on Stabilizing Milled Amorphous Salbutamol Sulphate. Int. J. Pharm. 2010, 391, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Muela, S.; Escalera, B.; Peña, M.Á.; Bustamante, P. Influence of Temperature on the Solubilization of Thiabendazole by Combined Action of Solid Dispersions and Co-Solvents. Int. J. Pharm. 2010, 384, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Knopp, M.M.; Nguyen, J.H.; Becker, C.; Francke, N.M.; Jørgensen, E.B.; Holm, P.; Holm, R.; Mu, H.; Rades, T.; Langguth, P. Influence of Polymer Molecular Weight on In Vitro Dissolution Behavior and In Vivo Performance of Celecoxib:PVP Amorphous Solid Dispersions. Eur. J. Pharm. Biopharm. 2016, 101, 145–151. [Google Scholar] [CrossRef]
- Jachowicz, R.; Czech, A. Preparation and Evaluation of Piroxicam–HPMCAS Solid Dispersions for Ocular Use. Pharm. Dev. Technol. 2008, 13, 495–504. [Google Scholar] [CrossRef]
- Kojima, T.; Higashi, K.; Suzuki, T.; Tomono, K.; Moribe, K.; Yamamoto, K. Stabilization of a Supersaturated Solution of Mefenamic Acid from a Solid Dispersion with EUDRAGIT® EPO. Pharm. Res. 2012, 29, 2777–2791. [Google Scholar] [CrossRef]
- Xie, T.; Gao, W.; Taylor, L.S. Impact of Eudragit EPO and Hydroxypropyl Methylcellulose on Drug Release Rate, Supersaturation, Precipitation Outcome and Redissolution Rate of Indomethacin Amorphous Solid Dispersions. Int. J. Pharm. 2017, 531, 313–323. [Google Scholar] [CrossRef] [PubMed]
- Patra, C.N.; Priya, R.; Swain, S.; Kumar Jena, G.; Panigrahi, K.C.; Ghose, D. Pharmaceutical Significance of Eudragit: A Review. Futur. J. Pharm. Sci. 2017, 3, 33–45. [Google Scholar] [CrossRef]
- Li, J.; Li, C.; Zhang, H.; Gao, X.; Wang, T.; Wang, Z.; Zheng, A. Preparation of Azithromycin Amorphous Solid Dispersion by Hot-Melt Extrusion: An Advantageous Technology with Taste Masking and Solubilization Effects. Polymers 2022, 14, 495. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, T.; Aso, Y.; Yoshioka, S.; Kawanishi, T. Differences in Crystallization Rate of Nitrendipine Enantiomers in Amorphous Solid Dispersions with HPMC and HPMCP. Int. J. Pharm. 2011, 407, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Chen, H.; Wang, Y.; Wang, R.; Xu, J.; Zhang, C. Amorphous Solid Dispersions: Role of the Polymer and Its Importance in Physical Stability and In Vitro Performance. Pharmaceutics 2022, 14, 1747. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, M.; Hu, J.; Gao, P.; Li, L.; Ali-Reynolds, A.; Chal, B.; Gupta, V.; Ma, C.; Mahajan, N.; Akrami, A.; et al. Enhanced Bioavailability of a Poorly Soluble VR1 Antagonist Using an Amorphous Solid Dispersion Approach: A Case Study. Mol. Pharm. 2008, 5, 981–993. [Google Scholar] [CrossRef] [PubMed]
- Monschke, M.; Wagner, K.G. Impact of HPMCAS on the Dissolution Performance of Polyvinyl Alcohol Celecoxib Amorphous Solid Dispersions. Pharmaceutics 2020, 12, 541. [Google Scholar] [CrossRef] [PubMed]
- Onoue, S.; Sato, H.; Kawabata, Y.; Mizumoto, T.; Hashimoto, N.; Yamada, S. In Vitro and In Vivo Characterization on Amorphous Solid Dispersion of Cyclosporine A for Inhalation Therapy. J. Control. Release 2009, 138, 16–23. [Google Scholar] [CrossRef]
- Liu, P.; Zhou, J.; Chang, J.; Liu, X.; Xue, H.; Wang, R.; Li, Z.; Li, C.; Wang, J.; Liu, C. Soluplus-Mediated Diosgenin Amorphous Solid Dispersion with High Solubility and High Stability: Development, Characterization and Oral Bioavailability. Drug Des. Devel. Ther. 2020, 14, 2959–2975. [Google Scholar] [CrossRef]
- Janssens, S.; Denivelle, S.; Rombaut, P.; Van den Mooter, G. Influence of Polyethylene Glycol Chain Length on Compatibility and Release Characteristics of Ternary Solid Dispersions of Itraconazole in Polyethylene Glycol/Hydroxypropylmethylcellulose 2910 E5 Blends. Eur. J. Pharm. Sci. 2008, 35, 203–210. [Google Scholar] [CrossRef]
- Shirke, S.H.; Shete, A.S.; Doijad, R.C. Enhancement of Dissolution Rate of Indomethacin by Kollicoat IR Based Solid Dispersions. Pharm. Lett. 2015, 7, 64–73. [Google Scholar]
- Portero, A.; Remuñán-López, C.; Vila-Jato, J.L. Effect of Chitosan and Chitosan Glutamate Enhancing the Dissolution Properties of the Poorly Water Soluble Drug Nifedipine. Int. J. Pharm. 1998, 175, 75–84. [Google Scholar] [CrossRef]
- Zhong, L.; Zhu, X.; Luo, X.; Su, W. Dissolution Properties and Physical Characterization of Telmisartan–Chitosan Solid Dispersions Prepared by Mechanochemical Activation. AAPS PharmSciTech 2013, 14, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Le, T.-T.; Elyafi, A.K.E.; Mohammed, A.R.; Al-Khattawi, A. Delivery of Poorly Soluble Drugs via Mesoporous Silica: Impact of Drug Overloading on Release and Thermal Profiles. Pharmaceutics 2019, 11, 269. [Google Scholar] [CrossRef] [PubMed]
- Seljak, K.B.; Kocbek, P.; Gasperlin, M. Mesoporous Silica Nanoparticles as Delivery Carriers: An Overview of Drug Loading Techniques. J. Drug Deliv. Sci. Technol. 2020, 59, 101906. [Google Scholar] [CrossRef]
- ICH Q3C (R8) Residual Solvents—Scientific Guideline. Available online: https://www.ema.europa.eu/en/ich-q3c-r8-residual-solvents-scientific-guideline (accessed on 31 July 2023).
- Leuner, C.; Dressman, J. Improving Drug Solubility for Oral Delivery Using Solid Dispersions. Eur. J. Pharm. Biopharm. 2000, 50, 47–60. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, N.G.; Kakran, M.; Li, L.; Judeh, Z.M.A.; Muller, R.H. Dissolution Enhancement of a Poorly Water-Soluble Antimalarial Drug by Means of a Modified Multi-Fluid Nozzle Pilot Spray Drier. Mater. Sci. Eng. 2011, 31, 391–399. [Google Scholar] [CrossRef]
- Dohrn, S.; Luebbert, C.; Lehmkemper, K.; Kyeremateng, S.O.; Degenhardt, M.; Sadowski, G. Solvent influence on the phase behavior and glass transition of Amorphous Solid Dispersions. Eur. J. Pharm. Biopharm. 2021, 158, 132–142. [Google Scholar] [CrossRef]
- Serajuddin, A.T. Solid Dispersion of Poorly Water-Soluble Drugs: Early Promises, Subsequent Problems, and Recent Breakthroughs. J. Pharm. Sci. 1999, 88, 1058–1066. [Google Scholar] [CrossRef]
- Eren, Z.S.; Tunçer, S.; Gezer, G.; Yildirim, L.T.; Banerjee, S.; Yilmaz, A. Improved Solubility of Celecoxib by Inclusion in SBA-15 Mesoporous Silica: Drug Loading in Different Solvents and Release. Microporous Mesoporous Mater. 2016, 235, 211–223. [Google Scholar] [CrossRef]
- Hillerström, A.; Van Stam, J.; Andersson, M. Ibuprofen Loading into Mesostructured Silica Using Liquid Carbon Dioxide as a Solvent. Green. Chem. 2009, 11, 662. [Google Scholar] [CrossRef]
- Belhadj-Ahmed, F.; Badens, E.; Llewellyn, P.; Denoyel, R.; Charbit, G. Impregnation of Vitamin E Acetate on Silica Mesoporous Phases Using Supercritical Carbon Dioxide. J. Supercrit. Fluids 2009, 51, 278–286. [Google Scholar] [CrossRef]
- Vasconcelos, T.; Marques, S.; Das Neves, J.; Sarmento, B. Amorphous Solid Dispersions: Rational Selection of a Manufacturing Process. Adv. Drug Deliv. Rev. 2016, 100, 85–101. [Google Scholar] [CrossRef] [PubMed]
- Borde, S.; Paul, S.K.; Chauhan, H. Ternary Solid Dispersions: Classification and Formulation Considerations. Drug Dev. Ind. Pharm. 2021, 47, 1011–1028. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Singh, A.; Salwan, R.; Bhanot, R.; Rahar, S.; Dhawan, R.K. An Informative Review on Solid Dispersion. GSC Biol. Pharm. Sci. 2023, 23, 114–121. [Google Scholar] [CrossRef]
- Bajracharya, R.; Lee, S.H.; Song, J.G.; Kim, M.; Lee, K.; Han, H.-K. Development of a Ternary Solid Dispersion Formulation of LW6 to Improve the In Vivo Activity as a BCRP Inhibitor: Preparation and In Vitro/In Vivo Characterization. Pharmaceutics 2019, 11, 206. [Google Scholar] [CrossRef] [PubMed]
- Bennett, R.C.; Brough, C.; Miller, D.A.; O’Donnell, K.P.; Keen, J.M.; Hughey, J.R.; Williams, R.O.; McGinity, J.W. Preparation of Amorphous Solid Dispersions by Rotary Evaporation and KinetiSol Dispersing: Approaches to Enhance Solubility of a Poorly Water-Soluble Gum Extract. Drug Dev. Ind. Pharm. 2015, 41, 382–397. [Google Scholar] [CrossRef]
- Santos, L.F.S.; de Jesus, R.A.; Costa, J.A.S.; Gouveia, L.G.T.; de Mesquita, M.E.; Navickiene, S. Evaluation of MCM-41 and MCM-48 Mesoporous Materials as Sorbents in Matrix Solid Phase Dispersion Method for the Determination of Pesticides in Soursop Fruit (Annona Muricata). Inorg. Chem. Commun. 2019, 101, 45–51. [Google Scholar] [CrossRef]
- Bhardwaj, V.; Trasi, N.S.; Zemlyanov, D.Y.; Taylor, L.S. Surface Area Normalized Dissolution to Study Differences in Itraconazole-Copovidone Solid Dispersions Prepared by Spray-Drying and Hot Melt Extrusion. Int. J. Pharm. 2018, 540, 106–119. [Google Scholar] [CrossRef]
- Li, N.; Taylor, L.S. Tailoring Supersaturation from Amorphous Solid Dispersions. J. Control. Release 2018, 279, 114–125. [Google Scholar] [CrossRef]
- Bhujbal, S.V.; Mitra, B.; Jain, U.; Gong, Y.; Agrawal, A.; Karki, S.; Taylor, L.S.; Kumar, S.; Zhou, Q. Pharmaceutical Amorphous Solid Dispersion: A Review of Manufacturing Strategies. Acta Pharm. Sin. B 2021, 11, 2505–2536. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.T.; Potter, C.B.; Mohammadpour, M.; Albadarin, A.B.; Walker, G.M. Design of Spray Dried Ternary Solid Dispersions Comprising Itraconazole, Soluplus and HPMCP: Effect of Constituent Compositions. Int. J. Pharm. 2017, 519, 356–372. [Google Scholar] [CrossRef]
- Wostry, M.; Plappert, H.; Grohganz, H. Preparation of Co-Amorphous Systems by Freeze-Drying. Pharmaceutics 2020, 12, 941. [Google Scholar] [CrossRef] [PubMed]
- Kunz, C.; Schuldt-Lieb, S.; Gieseler, H. Freeze-Drying From Organic Cosolvent Systems, Part 1: Thermal Analysis of Cosolvent-Based Placebo Formulations in the Frozen State. J. Pharm. Sci. 2018, 107, 887–896. [Google Scholar] [CrossRef] [PubMed]
- Tran, P.H.-L.; Tran, T.T.-D.; Park, J.B.; Lee, B.-J. Controlled Release Systems Containing Solid Dispersions: Strategies and Mechanisms. Pharm. Res. 2011, 28, 2353–2378. [Google Scholar] [CrossRef] [PubMed]
- Sridhar, I.; Doshi, A.; Joshi, B.; Wankhede, V.; Doshi, J. Solid Dispersions: An Approach to Enhance Solubility of Poorly Water Soluble Drug. J. Sci. Innov. Res. 2013, 2, 685–694. [Google Scholar]
- Fitriani, L.; Haqi, A.; Zaini, E. Preparation and Characterization of Solid Dispersion Freeze-Dried Efavirenz—Polyvinylpyrrolidone K-30. J. Adv. Pharm. Technol. Res. 2016, 7, 105. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.R.; Lee, P.I. Effect of Extent of Supersaturation on the Evolution of Kinetic Solubility Profiles. Mol. Pharm. 2017, 14, 206–220. [Google Scholar] [CrossRef]
- Ha, E.-S.; Kim, J.-S.; Baek, I.-H.; Yoo, J.-W.; Jung, Y.; Moon, H.R.; Kim, M.-S. Development of Megestrol Acetate Solid Dispersion Nanoparticles for Enhanced Oral Delivery by Using a Supercritical Antisolvent Process. Drug Des. Devel. Ther. 2015, 9, 4269–4277. [Google Scholar] [CrossRef]
- Mishima, K.; Honjo, M.; Sharmin, T.; Ito, S.; Kawakami, R.; Kato, T.; Misumi, M.; Suetsugu, T.; Orii, H.; Kawano, H.; et al. Gas-Saturated Solution Process to Obtain Microcomposite Particles of Alpha Lipoic Acid/Hydrogenated Colza Oil in Supercritical Carbon Dioxide. Pharm. Dev. Technol. 2015, 21, 1049707. [Google Scholar] [CrossRef]
- Krupa, A.; Descamps, M.; Willart, J.-F.; Jachowicz, R.; Danède, F. High Energy Ball Milling and Supercritical Carbon Dioxide Impregnation as Co-Processing Methods to Improve Dissolution of Tadalafil. Eur. J. Pharm. Sci. 2016, 95, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Yin, X.; Daintree, L.S.; Ding, S.; Ledger, D.M.; Wang, B.; Zhao, W.; Qi, J.; Wu, W.; Han, J. Itraconazole Solid Dispersion Prepared by a Supercritical Fluid Technique: Preparation, In Vitro Characterization, and Bioavailability in Beagle Dogs. Drug Des. Devel. Ther. 2015, 9, 2801–2810. [Google Scholar] [PubMed]
- Mendonsa, N.; Almutairy, B.; Kallakunta, V.R.; Sarabu, S.; Thipsay, P.; Bandari, S.; Repka, M.A. Manufacturing Strategies to Develop Amorphous Solid Dispersions: An Overview. J. Drug Deliv. Sci. Technol. 2020, 55, 101459. [Google Scholar] [CrossRef] [PubMed]
- Sarode, A.L.; Sandhu, H.; Shah, N.; Malick, W.; Zia, H. Hot Melt Extrusion for Amorphous Solid Dispersions: Temperature and Moisture Activated Drug–Polymer Interactions for Enhanced Stability. Mol. Pharm. 2013, 10, 3665–3675. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.; Gala, U.; Chauhan, H. Classification of Solid Dispersions: Correlation to (i) Stability and Solubility (Ii) Preparation and Characterization Techniques. Drug Dev. Ind. Pharm. 2015, 41, 1401–1415. [Google Scholar] [CrossRef] [PubMed]
- Patil, H.; Tiwari, R.V.; Repka, M.A. Hot-Melt Extrusion: From Theory to Application in Pharmaceutical Formulation. AAPS PharmSciTech 2016, 17, 20–42. [Google Scholar] [CrossRef] [PubMed]
- Censi, R.; Gigliobianco, M.; Casadidio, C.; Di Martino, P. Hot Melt Extrusion: Highlighting Physicochemical Factors to Be Investigated While Designing and Optimizing a Hot Melt Extrusion Process. Pharmaceutics 2018, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Gao, N.; Guo, M.; Fu, Q.; He, Z. Application of Hot Melt Extrusion to Enhance the Dissolution and Oral Bioavailability of Oleanolic Acid. Asian J. Pharm. Sci. 2017, 12, 66–72. [Google Scholar] [CrossRef]
- Sharma, A.D.; Jain, C.P. Solid Dispersion: A Promising Technique to Enhance Solubility of Poorly Water Soluble Drug. Int. J. Drug Deliv. 2011, 3, 149–170. [Google Scholar]
- Ellenberger, D.J.; Miller, D.A.; Williams, R.O. Expanding the Application and Formulation Space of Amorphous Solid Dispersions with KinetiSol®: A Review. AAPS PharmSciTech 2018, 19, 1933–1956. [Google Scholar] [CrossRef]
- DiNunzio, J.C.; Brough, C.; Hughey, J.R.; Miller, D.A.; Williams, R.O., III; McGinity, J.W. Fusion Production of Solid Dispersions Containing a Heat-Sensitive Active Ingredient by Hot Melt Extrusion and Kinetisol® Dispersing. Eur. J. Pharm. Biopharm. 2010, 74, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Hughey, J.R.; Keen, J.M.; Miller, D.A.; Brough, C.; McGinity, J.W. Preparation and Characterization of Fusion Processed Solid Dispersions Containing a Viscous Thermally Labile Polymeric Carrier. Int. J. Pharm. 2012, 438, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Gu, B.; Linehan, B.; Tseng, Y.-C. Optimization of the Büchi B-90 Spray Drying Process Using Central Composite Design for Preparation of Solid Dispersions. Int. J. Pharm. 2015, 491, 208–217. [Google Scholar] [CrossRef]
- Miller, D.A.; Keen, J.M. KinetiSol®-Based Amorphous Solid Dispersions. In Amorphous Solid. Dispersions; Springer: New York, NY, USA, 2014; pp. 567–577. [Google Scholar]
- LaFountaine, J.S.; Prasad, L.K.; Brough, C.; Miller, D.A.; McGinity, J.W.; Williams, R.O. Thermal Processing of PVP- and HPMC-Based Amorphous Solid Dispersions. AAPS PharmSciTech 2016, 17, 120–132. [Google Scholar] [CrossRef] [PubMed]
- Caron, V.; Hu, Y.; Tajber, L.; Erxleben, A.; Corrigan, O.I.; McArdle, P.; Healy, A.M. Amorphous Solid Dispersions of Sulfonamide/Soluplus® and Sulfonamide/PVP Prepared by Ball Milling. AAPS PharmSciTech 2013, 14, 464–474. [Google Scholar] [CrossRef] [PubMed]
- Slámová, M.; Prausová, K.; Epikaridisová, J.; Brokešová, J.; Kuentz, M.; Patera, J.; Zámostný, P. Effect of Co-Milling on Dissolution Rate of Poorly Soluble Drugs. Int. J. Pharm. 2021, 597, 120312. [Google Scholar] [CrossRef]
- Szafraniec, J.; Antosik, A.; Knapik-Kowalczuk, J.; Kurek, M.; Syrek, K.; Chmiel, K.; Paluch, M.; Jachowicz, R. Planetary Ball Milling and Supercritical Fluid Technology as a Way to Enhance Dissolution of Bicalutamide. Int. J. Pharm. 2017, 533, 470–479. [Google Scholar] [CrossRef] [PubMed]
- Dedroog, S.; Huygens, C.; Van den Mooter, G. Chemically Identical but Physically Different: A Comparison of Spray Drying, Hot Melt Extrusion and Cryo-Milling for the Formulation of High Drug Loaded Amorphous Solid Dispersions of Naproxen. Eur. J. Pharm. Biopharm. 2019, 135, 1–12. [Google Scholar] [CrossRef]
- Descamps, M.; Willart, J.F. Perspectives on the Amorphisation/Milling Relationship in Pharmaceutical Materials. Adv. Drug Deliv. Rev. 2016, 100, 51–66. [Google Scholar] [CrossRef]
- Engers, D.; Teng, J.; Jimenez-Novoa, J.; Gent, P.; Hossack, S.; Campbell, C.; Thomson, J.; Ivanisevic, I.; Templeton, A.; Byrn, S.; et al. A Solid-State Approach to Enable Early Development Compounds: Selection and Animsal Bioavailability Studies of an Itraconazole Amorphous Solid Dispersion. J. Pharm. Sci. 2010, 99, 3901–3922. [Google Scholar] [CrossRef]
- Al-Obaidi, H.; Lawrence, M.J.; Al-Saden, N.; Ke, P. Investigation of Griseofulvin and Hydroxypropylmethyl Cellulose Acetate Succinate Miscibility in Ball Milled Solid Dispersions. Int. J. Pharm. 2013, 443, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Moes, J.; Koolen, S.; Huitema, A.; Schellens, J.; Beijnen, J.; Nuijen, B. Development of an Oral Solid Dispersion Formulation for Use in Low-Dose Metronomic Chemotherapy of Paclitaxel. Eur. J. Pharm. Biopharm. 2013, 83, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Xin, T.; Ye, T.; Yang, X.; Pan, W. Solid Dispersion in the Development of a Nimodipine Delayed-Release Tablet Formulation. Asian J. Pharm. Sci. 2014, 9, 35–41. [Google Scholar] [CrossRef]
- Chauhan, A. Powder XRD Technique and Its Applications in Science and Technology. J. Anal. Bioanal. Tech. 2014, 5, 212. [Google Scholar] [CrossRef]
- Zhu, Q.; Toth, S.J.; Simpson, G.J.; Hsu, H.-Y.; Taylor, L.S.; Harris, M.T. Crystallization and Dissolution Behavior of Naproxen/Polyethylene Glycol Solid Dispersions. J. Phys. Chem. B 2013, 117, 1494–1500. [Google Scholar] [CrossRef] [PubMed]
- Bøtker, J.P.; Karmwar, P.; Strachan, C.J.; Cornett, C.; Tian, F.; Zujovic, Z.; Rantanen, J.; Rades, T. Assessment of Crystalline Disorder in Cryo-Milled Samples of Indomethacin Using Atomic Pair-Wise Distribution Functions. Int. J. Pharm. 2011, 417, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Nollenberger, K.; Gryczke, A.; Meier, C.; Dressman, J.; Schmidt, M.U.; Brühne, S. Pair Distribution Function X-ray Analysis Explains Dissolution Characteristics of Felodipine Melt Extrusion Products. J. Pharm. Sci. 2009, 98, 1476–1486. [Google Scholar] [CrossRef]
- Baird, J.A.; Taylor, L.S. Evaluation of Amorphous Solid Dispersion Properties Using Thermal Analysis Techniques. Adv. Drug Deliv. Rev. 2012, 64, 396–421. [Google Scholar] [CrossRef]
- Raut, D.M.; Sakharkar, D.M.; Bodke, P.S.; Mahajan, D.T. Determination of Traces of Amorphous Carvidilol Content in Carvedilol Drug Substance and Drug Product Using Modulated Differential Scanning Colorimetry. Pharm. Lett. 2011, 3, 1–12. [Google Scholar]
- Ford, J.L.; Mann, T.E. Fast-Scan DSC and Its Role in Pharmaceutical Physical Form Characterisation and Selection. Adv. Drug Deliv. Rev. 2012, 64, 422–430. [Google Scholar] [CrossRef]
- Jones, D.S.; Tian, Y.; Abu-Diak, O.; Andrews, G.P. Pharmaceutical Applications of Dynamic Mechanical Thermal Analysis. Adv. Drug Deliv. Rev. 2012, 64, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Bunker, M.; Chen, X.; Parker, A.P.; Patel, N.; Roberts, C.J. Nanoscale Thermal Analysis of Pharmaceutical Solid Dispersions. Int. J. Pharm. 2009, 380, 170–173. [Google Scholar] [CrossRef] [PubMed]
- Ewing, A.V.; Clarke, G.S.; Kazarian, S.G. Stability of Indomethacin with Relevance to the Release from Amorphous Solid Dispersions Studied with ATR-FTIR Spectroscopic Imaging. Eur. J. Pharm. Sci. 2014, 60, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Forster, A.; Hempenstall, J.; Rades, T. Characterization of Glass Solutions of Poorly Water-Soluble Drugs Produced by Melt Extrusion with Hydrophilic Amorphous Polymers. J. Pharm. Pharmacol. 2010, 53, 303–315. [Google Scholar] [CrossRef] [PubMed]
- Loh, G.O.K.; Tan, Y.T.F.; Peh, K.K. Hydrophilic Polymer Solubilization on Norfloxacin Solubility in Preparation of Solid Dispersion. Powder Technol. 2014, 256, 462–469. [Google Scholar] [CrossRef]
- Bugay, D.E. Characterization of the Solid-State: Spectroscopic Techniques. Adv. Drug Deliv. Rev. 2001, 48, 43–65. [Google Scholar] [CrossRef] [PubMed]
- Furuyama, N.; Hasegawa, S.; Hamaura, T.; Yada, S.; Nakagami, H.; Yonemochi, E.; Terada, K. Evaluation of Solid Dispersions on a Molecular Level by the Raman Mapping Technique. Int. J. Pharm. 2008, 361, 12–18. [Google Scholar] [CrossRef]
- Sinclair, W.; Leane, M.; Clarke, G.; Dennis, A.; Tobyn, M.; Timmins, P. Physical Stability and Recrystallization Kinetics of Amorphous Ibipinabant Drug Product by Fourier Transform Raman Spectroscopy. J. Pharm. Sci. 2011, 100, 4687–4699. [Google Scholar] [CrossRef]
- Kanaujia, P.; Lau, G.; Ng, W.K.; Widjaja, E.; Schreyer, M.; Hanefeld, A.; Fischbach, M.; Saal, C.; Maio, M.; Tan, R.B.H. Investigating the Effect of Moisture Protection on Solid-State Stability and Dissolution of Fenofibrate and Ketoconazole Solid Dispersions Using PXRD, HSDSC and Raman Microscopy. Drug Dev. Ind. Pharm. 2011, 37, 1026–1035. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, C.; Chen, Z.; Su, C.; Hageman, M.; Hussain, M.; Haskell, R.; Stefanski, K.; Qian, F. Drug–Polymer–Water Interaction and Its Implication for the Dissolution Performance of Amorphous Solid Dispersions. Mol. Pharm. 2015, 12, 576–589. [Google Scholar] [CrossRef]
- Ticehurst, M.D.; Basford, P.A.; Dallman, C.I.; Lukas, T.M.; Marshall, P.V.; Nichols, G.; Smith, D. Characterisation of the Influence of Micronisation on the Crystallinity and Physical Stability of Revatropate Hydrobromide. Int. J. Pharm. 2000, 193, 247–259. [Google Scholar] [CrossRef] [PubMed]
- Enose, A.A.; Dasan, P.K.; Sivaramakrishnan, H.; Shah, S.M. Formulation and Characterization of Solid Dispersion Prepared by Hot Melt Mixing: A Fast Screening Approach for Polymer Selection. J. Pharm. 2014, 2014, 105382. [Google Scholar] [CrossRef] [PubMed]
- Punčochová, K.; Heng, J.Y.Y.; Beránek, J.; Štěpánek, F. Investigation of Drug–Polymer Interaction in Solid Dispersions by Vapour Sorption Methods. Int. J. Pharm. 2014, 469, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Lane, R.A.; Buckton, G. The Novel Combination of Dynamic Vapour Sorption Gravimetric Analysis and near Infra-Red Spectroscopy as a Hyphenated Technique. Int. J. Pharm. 2000, 207, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Paudel, A.; Geppi, M.; Mooter, G. Van den Structural and Dynamic Properties of Amorphous Solid Dispersions: The Role of Solid-State Nuclear Magnetic Resonance Spectroscopy and Relaxometry. J. Pharm. Sci. 2014, 103, 2635–2662. [Google Scholar] [CrossRef] [PubMed]
- Yuan, X.; Sperger, D.; Munson, E.J. Investigating Miscibility and Molecular Mobility of Nifedipine-PVP Amorphous Solid Dispersions Using Solid-State NMR Spectroscopy. Mol. Pharm. 2014, 11, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Litvinov, V.M.; Guns, S.; Adriaensens, P.; Scholtens, B.J.R.; Quaedflieg, M.P.; Carleer, R.; Van den Mooter, G. Solid State Solubility of Miconazole in Poly[(Ethylene Glycol)-g-Vinyl Alcohol] Using Hot-Melt Extrusion. Mol. Pharm. 2012, 9, 2924–2932. [Google Scholar] [CrossRef]
- Ito, A.; Watanabe, T.; Yada, S.; Hamaura, T.; Nakagami, H.; Higashi, K.; Moribe, K.; Yamamoto, K. Prediction of Recrystallization Behavior of Troglitazone/Polyvinylpyrrolidone Solid Dispersion by Solid-State NMR. Int. J. Pharm. 2010, 383, 18–23. [Google Scholar] [CrossRef]
- Dahlberg, C.; Millqvist-Fureby, A.; Schuleit, M.; Furó, I. Relationships between Solid Dispersion Preparation Process, Particle Size and Drug Release—An NMR and NMR Microimaging Study. Eur. J. Pharm. Biopharm. 2010, 76, 311–319. [Google Scholar] [CrossRef]
- Ho, R.; Heng, J.Y.Y. A Review of Inverse Gas Chromatography and Its Development as a Tool to Characterize Anisotropic Surface Properties of Pharmaceutical Solids. KONA Powder Part. J. 2013, 30, 164–180. [Google Scholar] [CrossRef]
- Buckton, G.; Gill, H. The Importance of Surface Energetics of Powders for Drug Delivery and the Establishment of Inverse Gas Chromatography. Adv. Drug Deliv. Rev. 2007, 59, 1474–1479. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Zhu, L.; Wu, T.; Cai, T.; Gunn, E.M.; Yu, L. Stability of Amorphous Pharmaceutical Solids: Crystal Growth Mechanisms and Effect of Polymer Additives. AAPS J. 2012, 14, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, S.; Ke, P.; Buckton, G. Determination of the Structural Relaxation at the Surface of Amorphous Solid Dispersion Using Inverse Gas Chromatography. J. Pharm. Sci. 2009, 98, 2133–2139. [Google Scholar] [CrossRef] [PubMed]
- Miyanishi, H.; Nemoto, T.; Mizuno, M.; Mimura, H.; Kitamura, S.; Iwao, Y.; Noguchi, S.; Itai, S. Evaluation of Crystallization Behavior on the Surface of Nifedipine Solid Dispersion Powder Using Inverse Gas Chromatography. Pharm. Res. 2013, 30, 502–511. [Google Scholar] [CrossRef] [PubMed]
- Schittny, A.; Huwyler, J.; Puchkov, M. Mechanisms of Increased Bioavailability through Amorphous Solid Dispersions: A Review. Drug Deliv. 2020, 27, 110–127. [Google Scholar] [CrossRef] [PubMed]
- Dalsin, M.C.; Tale, S.; Reineke, T.M. Solution-State Polymer Assemblies Influence BCS Class II Drug Dissolution and Supersaturation Maintenance. Biomacromolecules 2014, 15, 500–511. [Google Scholar] [CrossRef] [PubMed]
- Aleandri, S.; Jankovic, S.; Kuentz, M. Towards a Better Understanding of Solid Dispersions in Aqueous Environment by a Fluorescence Quenching Approach. Int. J. Pharm. 2018, 550, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Simonelli, A.P.; Mehta, S.C.; Higuchi, W.I. Dissolution Rates of High Energy Polyvinylpyrrolidone (PVP)-Sulfathiazole Coprecipitates. J. Pharm. Sci. 1969, 58, 538–549. [Google Scholar] [CrossRef]
- Craig, D.Q.M. The mechanisms of drug release from solid dispersions in water-soluble polymers. Int. J. Pharm. 2001, 231, 131–144. [Google Scholar] [CrossRef]
- Puncochova, K.; Ewing, A.V.; Gajdosova, M.; Sarvasova, N.; Kazarian, S.G.; Beranek, J.; Stapanek, F. Identifying the Mechanisms of Drug Release from Amorphous Solid Dispersions Using MRI and ATR-FTIR Spectroscopic Imaging. Int. J. Pharm. 2015, 483, 256–267. [Google Scholar] [CrossRef]
- Szafrniec, J.; Antosik, A.; Kowalczuk, J.K.; Chmiel, K.; Kurek, M.; Gawlak, K.; Paluch, M.; Jachowicz, R. Enhanced Dissolution of Solid Dispersions Containing Bicalutamide Subjected to Mechanical Stress. Int. J. Pharm. 2018, 542, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.D.; Lee, P.I. Probing the Mechanisms of Drug Release from Amorphous Solid Dispersions in Medium-Soluble and Medium-Insoluble Carriers. J. Control. Release 2015, 211, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.D.; Lee, P.I. Evolution of Supersaturation of Amorphous Pharmaceuticals: The Effect of Rate of Supersaturation Generation. Mol. Pharm. 2013, 10, 4330–4346. [Google Scholar] [CrossRef] [PubMed]
- Saboo, S.; Mugheirbi, N.A.; Zemlyanov, D.Y.; Kestur, U.S.; Taylor, L.S. Congruent Release of Drug and Polymer: A “Sweet Spot” in the Dissolution of Amorphous Solid Dispersions. J. Control. Release 2019, 298, 68–82. [Google Scholar] [CrossRef]
- Indulkar, A.S.; Waters, J.E.; Mo, H.; Gao, Y.; Raina, S.A.; Zhang, G.G.Z.; Taylor, L.S. Origin of Nanodroplet Formation Upon Dissolution of an Amorphous Solid Dispersion: A Mechanistic Isotope Scrambling Study. J. Pharm. Sci. 2017, 106, 1998–2008. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.M.; Beig, A.; Carr, R.A.; Webster, G.K.; Dahan, A. The Solubility-Permeability Interplay When Using Cosolvents for Solubilization: Revising the Way We Use Solubility-Enabling Formulations. Mol. Pharm. 2012, 9, 581–591. [Google Scholar] [CrossRef] [PubMed]
- Six, K.; Verreck, G.; Peeters, J.; Brewster, M.; Mooter, G. Van Den Increased Physical Stability and Improved Dissolution Properties of Itraconazole, a Class II Drug, by Solid Dispersions That Combine Fast- and Slow-Dissolving Polymers. J. Pharm. Sci. 2004, 93, 124–131. [Google Scholar] [CrossRef] [PubMed]
- International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use Ich Harmonised Tripartite Guideline Stability Testing of New Drug Substances and Products Q1A(R2); The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH): Geneva, Switzerland, 2003.
- Nagapudi, K.; Jona, J. Amorphous Active Pharmaceutical Ingredients in Preclinical Studies: Preparation, Characterization, and Formulation. Curr. Bioact. Compd. 2008, 400, 213–224. [Google Scholar] [CrossRef]
- Newman, A.; Ngapudi, K.; Wenslow, R. Amorphous Solid Dispersions: A Robust Platform to Address Bioavailability Challenges. Ther. Deliv. 2015, 6, 247–261. [Google Scholar] [CrossRef]
- Korhonen, O.; Bhugra, C.; Pikal, M.J. Correlation between Molecular Mobility and Crystal Growth of Amorphous Phenobarbital and Phenobarbital with Polyvinylpyrrolidone and L-Proline. J. Pharm. Sci. 2008, 97, 3830–3841. [Google Scholar] [CrossRef]
- Wegiel, L.; Mauer, L.J.; Edgar, K.J.; Taylor, L.S. Crystallization of Amorphous Solid Dispersions of Resveratrol during Preparation and Storage—Impact of Different Polymers. J. Pharm. Sci. 2013, 102, 171–184. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Li, M.; Jia, L.; Chen, M.; Du, S.; Gong, J. Investigation of Drug–Polymer Miscibility, Molecular Interaction, and Their Effects on the Physical Stabilities and Dissolution Behaviors of Norfloxacin Amorphous Solid Dispersions. Cryst. Growth Des. 2020, 20, 2952–2964. [Google Scholar] [CrossRef]
- Moseson, D.E.; Parker, A.S.; Beaudoin, S.P.; Taylor, L.S. Amorphous Solid Dispersions Containing Residual Crystallinity: Influence of Seed Properties and Polymer Adsorption on Dissolution Performance. Eur. J. Pharm. Sci. 2020, 146, 105276. [Google Scholar] [CrossRef] [PubMed]
- Kapourani, A.; Vardaka, E.; Katopodis, K.; Kachrimanis, K.; Barmpalexis, P. Crystallization Tendency of APIs Possessing Different Thermal and Glass Related Properties in Amorphous Solid Dispersions. Int. J. Pharm. 2020, 579, 119–149. [Google Scholar] [CrossRef] [PubMed]
- Monschke, M.; Kayser, K.; Wagner, K.G. Processing of Polyvinyl Acetate Phthalate in Hot-Melt Extrusion-Preparation of Amorphous Solid Dispersions. Pharmaceutics 2020, 12, 337. [Google Scholar] [CrossRef] [PubMed]
- Lapuk, S.E.; Zubaidullina, L.S.; Ziganshin, M.A.; Mukhametzyanov, T.A.; Schick, C.; Gerasimov, A. V Kinetic Stability of Amorphous Solid Dispersions with High Content of the Drug: A Fast Scanning Calorimetry Investigation. Int. J. Pharm. 2019, 562, 113–123. [Google Scholar] [CrossRef]
- Blaabjerg, L.I.; Bulduk, B.; Lindenberg, E.; Lobmann, K.; Rades, T.; Grohganz, H. Influence of Glass Forming Ability on the Physical Stability of Supersaturated Amorphous Solid Dispersions. J. Pharm. Sci. 2019, 108, 2561–2569. [Google Scholar] [CrossRef] [PubMed]
- Garcia, J.C.M.; Rzoska, S.J.; Rzoska, A.D.; Garcia, J.M.; Mauro, J.C. Divergent Dynamics and the Kauzmann Temperature in Glass Forming Systems. Nat. Portf. 2014, 4, 5160. [Google Scholar]
- Rumondor, A.C.F.; Wikstrom, H.; Van Eerdenbrugh, B.; Taylor, L.S. Understanding the Tendency of Amorphous Solid Dispersions to Undergo Amorphous-Amorphous Phase Separation in the Presence of Absorbed Moisture. AAPS PharmSciTech 2011, 12, 1209–1219. [Google Scholar] [CrossRef]
- Li, J.; Hubert, M.; Pinnamaneni, S.; Tao, L.; Zhao, J.; Sharif, S.; Ramakrishnan, R.K.; Nazarenko, S. Effect of Moisture Sorption on Free Volume and Relaxation of Spray Dried Dispersions: Relation to Drug Recrystallization. J. Pharm. Sci. 2020, 109, 1050–1058. [Google Scholar] [CrossRef]
- Chavan, R.B.; Bhargavi, N.; Lodagekar, A.; Shastri, N.R. Near Infra Red Spectroscopy: A Tool for Solid State Characterization. Drug Discov. Today 2017, 22, 1835–1843. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Wang, X.; Zhang, Y.; Huang, K.; Liu, H.; Xu, D.; Li, S.; Liu, Q.; Huang, J.; Yao, H.; et al. Improved Solubility, Dissolution Rate, and Oral Bioavailability of Main Biflavonoids from Selaginella Doederleinii Extract by Amorphous Solid Dispersion. Drug Deliv. 2020, 27, 309–322. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.S.; Cho, N.H.; Kim, D.-H.; Park, J.-S. Comparison of Paclitaxel Solid Dispersion and Polymeric Micelles for Improved Oral Bioavailability and In Vitro Anti-Cancer Effects. Mater. Sci. Eng. 2019, 100, 247–259. [Google Scholar] [CrossRef]
- Liu, M.; Lai, Z.; Zhu, L.; Ding, X.; Tong, X.; Wang, Z.; Bi, Q.; Tan, N. Novel Amorphous Solid Dispersion Based on Natural Deep Eutectic Solvent for Enhancing Delivery of Anti-Tumor RA-XII by Oral Administration in Rats. Eur. J. Pharm. Sci. 2021, 166, 105931. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Mintoo, M.J.; Mondhe, D.M.; Bharate, S.B.; Vishwakarma, R.A.; Bharate, S.S. Binary and Ternary Solid Dispersions of an Anticancer Preclinical Lead, IIIM-290: In Vitro and In Vivo Studies. Int. J. Pharm. 2019, 570, 118683. [Google Scholar] [CrossRef]
- Buckley, S.T.; Frank, K.J.; Fricker, G.; Brandl, M. Biopharmaceutical Classification of Poorly Soluble Drugs with Respect to “Enabling Formulations”. Eur. J. Pharm. Sci. 2013, 50, 8–16. [Google Scholar] [CrossRef]
- Ma, Y.; He, H.; Fan, W.; Li, Y.; Zhang, W.; Zhao, W.; Qi, J.; Lu, Y.; Dong, X.; Wu, W. In Vivo Fate of Biomimetic Mixed Micelles as Nanocarriers for Bioavailability Enhancement of Lipid-Drug Conjugates. ACS Biomater. Sci. Eng. 2017, 3, 2399–2409. [Google Scholar] [CrossRef] [PubMed]
- Alagga, A.A.; Gupta, V. Drug Absorption. Available online: https://www.ncbi.nlm.nih.gov/books/NBK557405/ (accessed on 1 August 2023).
- Deng, L.; Wang, Y.; Gong, T.; Sun, X.; Zhang, Z.-R. Dissolution and Bioavailability Enhancement of Alpha-Asarone by Solid Dispersions via Oral Administration. Drug Deliv. Ind. Pharm. 2017, 43, 1817–1826. [Google Scholar] [CrossRef]
- Shi, C.; Tong, Q.; Fang, J.; Wang, C.; Wu, J.; Wang, W. Preparation, Characterization and In Vivo Studies of Amorphous Solid Dispersion of Berberine with Hydrogenated Phosphatidylcholine. Eur. J. Pharm. Sci. 2015, 74, 11. [Google Scholar] [CrossRef]
- Fong, S.Y.K.; Martins, S.M.; Brandl, M.; Brandl, A.B. Solid Phospholipid Dispersions for Oral Delivery of Poorly Soluble Drugs: Investigation Into Celecoxib Incorporation and Solubility-In Vitro Permeability Enhancement. J. Pharm. Sci. 2016, 105, 1113–1123. [Google Scholar] [CrossRef]
- Jacobsen, A.-C.; Elvang, P.A.; Brandl, A.B.; Brandl, M. A Dynamic In Vitro Permeation Study on Solid Mono- and Diacyl-Phospholipid Dispersions of Celecoxib. Eur. J. Pharm. Sci. 2019, 127, 199–207. [Google Scholar] [CrossRef]
- Ueda, K.; Higashi, K.; Kataoka, M.; Yamashita, S.; Yamamoto, K.; Moribe, K. Inhibition Mechanism of Hydroxypropyl Methylcellulose Acetate Succinate on Drug Crystallization in Gastrointestinal Fluid and Drug Permeability from a Supersaturated Solution. Eur. J. Pharm. Sci. 2014, 62, 293–300. [Google Scholar] [CrossRef]

| No. | Anticancer Drug | Structure | Anticancer Activity | Water Solubility | References |
|---|---|---|---|---|---|
| 1. | Abiraterone acetate | 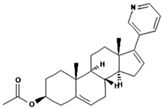 | Inhibition of the CYP17A1 enzyme involved in androgen production in the body. | 0.00305 mg/mL. | [26,27] |
| 2. | Axitinib | 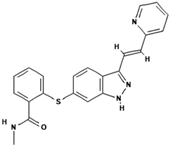 | Inhibits vascular endothelial growth factor receptor (VEGFR), tyrosine kinase receptor. | Over 0.0002 mg/mL in aqueous media with pH ranging from 1.1 to 7.8. Solubility increases with decreasing pH. | [28,29] |
| 3. | Bosutinib monohydrate |  | Inhibition of the protein kinase enzyme BCR-ABL, which plays an important role in cell development and proliferation. | Highly soluble at pH ≤ 5 (2 mg/mL) and the solubility reduces when pH increase (>5). | [30,31] |
| 4. | Cabozantinib | 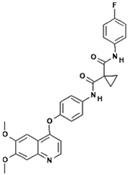 | Inhibition of MET, RET, and angiogenesis pathways. | Practically insoluble in pH > 4. | [32,33] |
| 5. | Ceritinib | 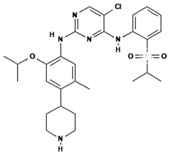 | Binds to the ALK kinase tyrosine domain and prevents phosphorylation of downstream substrates, inhibiting signaling pathways that promote cancer cell growth. | Practically insoluble in water (0.02 mg/mL). pH-dependent solubility and pH increases become sparingly soluble with a solubility of 11 mg/mL at pH = 1 and 0.0002 mg/mL at pH = 6.8. | [34,35,36] |
| 6. | Dabrafenib |  | Inhibits abnormally activated BRAF proteins, which are responsible for cancer cell growth and proliferation. | Very slightly soluble at pH 1 and practically insoluble above pH 4. | [37,38] |
| 7. | Erlotinib | 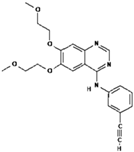 | Inhibits epidermal growth factor receptor (EGFR) activity on cancer cells. | 0.01402 mg/mL at 25 °C. | [39,40] |
| 8. | Lapatinib | 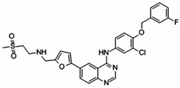 | Inhibits HER2 and EGFR activity. | 0.007 mg/mL at 25 °C. | [41,42] |
| 9. | Midostaurin | 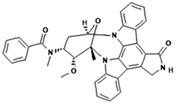 | Inhibits overactivity of FLT3 protein involved in cancer cell growth and proliferation. | <1 mg/mL (very slightly soluble). | [43,44] |
| 10. | Neratinib | 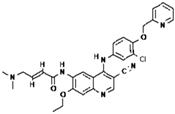 | Inhibits HER2 overactivity involved in cancer cell growth and proliferation. | Sparingly soluble at pH 1.2 (32.90 mg/mL) and insoluble at pH ≥ 5.0 (0.08 mg/mL or less). | [45,46] |
| 11. | Nilotinib | 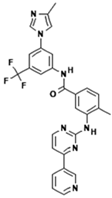 | Inhibits the overactivity of BCR-ABL proteins involved in cancer cell growth and proliferation. | 2.4 × 10−5 mg/mL at 25 °C. | [47,48] |
| 12. | Nintedanib | 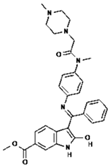 | Inhibition of three receptor tyrosine kinases involved in angiogenesis, namely, platelet-derived growth factor (PDGF)-type receptor, vascular endothelial growth factor (VEGF)-type receptor, and fibroblast growth factor (FGF)-type receptor. | 0.00966 mg/mL at 25 °C. | [49,50] |
| 13. | Pazopanib | 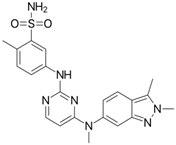 | Inhibits several receptor tyrosine kinases, including VEGFR, PDGFR, FGFR, KIT, and RET. One of the main targets of pazopanib is VEGFR. | 0.0033 mg/mL at 25 °C. | [51,52] |
| 14. | Sonidegib | 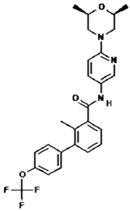 | Inhibits the Hedgehog pathway, which is a signaling pathway involved in cell growth and differentiation. | Practically insoluble. | [53,54] |
| 15. | Trametinib | 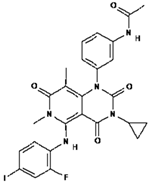 | Inhibiting the MEK enzyme, trametinib interferes with the RAS/RAF/MEK/ERK pathway and stops cancer cell proliferation. | Practically insoluble. | [55,56] |
| 16. | Vemurafenib | 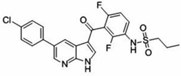 | Inhibition of pathologically activated BRAF enzyme activity in melanoma with BRAF V600E mutation. | Practically insoluble (<0.0001 mg/mL). | [57,58] |
| 17. | Regorafenib | 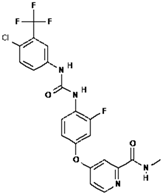 | Inhibits specific enzymes involved in cell growth pathways and angiogenesis (formation of new blood vessels). Protein kinases involved in cancer cell growth pathways such as VEGFR, PDGFR, FGFR, KIT, and RET. | Practically insoluble. | [59,60] |
| 18. | Everolimus | 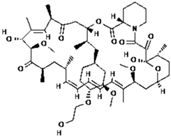 | Inhibition of target of rapamycin (mTOR) in cancer cells. | Practically insoluble (<0.1 mg/mL). | [61,62] |
| 19. | Venetoclax |  | Inhibition of B-cell lymphoma anti-apoptotic protein 2 (BCL-2). | Practically insoluble. | [63,64] |
| 20. | Olaparib | 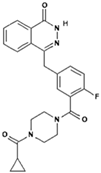 | Inhibition of the PARP enzyme, which plays a role in repairing DNA damage. | Practically insoluble 0.1 mg/mL. | [65,66] |
| Active Compound | Polymer | Method | Results | References |
|---|---|---|---|---|
| Itraconazole | Polyvinylpyrrolidone vinyl acetate copolymer 88 and Hydroxy propyl methylcellulose acetate succinate | Solvent evaporation | HPMCAS showed good storage stability at an extended RH of more than 60% compared with PVPVA | [72] |
| Glibenclamide | Hypromellose acetate succinate | Anti-solvent addition method | Improved dissolution leads to the formation of glibenclamide-rich amorphous droplets | [73] |
| Atorvastatin | Pluronic F127 and Pluronic F68 | Fusion method | Improved solubility and bioavailability compared to plain atorvastatin | [74] |
| Darunavir | HPMC/PVP | Coaxial electrospraying | Increase in drug-loading capacity and effect of gastro resistance on the molecule | [75] |
| Nobiletin | Methyl hesperidin mixture | Hot melt extrusion | Increased dissolution rate up to 7.5 times, permeability increases, and stable for up to 6 months under accelerated stability test conditions | [76] |
| Carvedilol | Β-cyclodextrin and hydroxypropyl-β-cyclodextrin | Complexation and kneading technique | A stable complex is formed and the dissolution rate increases in the range of pH 6.8 and 7.4 | [77] |
| Fenofibrate | PVP K30, HPMC E6, HPMC E15 | Hot melt extrusion | Significantly higher dissolution than the pure drug | [78] |
| Griseofulvin | Polyvinylpyrrolidone vinyl acetate polymer | Freeze drying | Significantly increased dissolution rate and oral absorption | [79] |
| Aripiprazole | Kollidon 12 PF | Hot melt extrusion | Increased dissolution compared to ordinary active substances and the use of acidifier increases bioavailability compared to not using it | [80] |
| Nevirapine | HPMCAS, hydroxypropyl methylcellulose phthalate, and Eudragit L100-55 | Hot melt extrusion | Shows good dissolution because it is made with enteric polymers that are not affected by gastric pH | [81] |
| Indomethacin | PVP K25 | Spray drying | Increased solubility, and improve physical stability | [82] |
| Ezetimibe | PVP K30 | Solvent Method | Improved oral bioavailability | [83] |
| Carbamazepine | Methylcellulose | Hot melt extrusion | Increased dissolution compared to crystalline forms | [84] |
| Oridonin | PVP K17 | Gas anti-solvent technique | Increased oral bioavailability | [85] |
| Telmisartan | PVP K30 | Spray drying | Increased dissolution rate (around 3-fold) due to the optimum pH-modulated formulation | [86] |
| Itraconazole | PVP Vinyl Acetate | Electrospinning method | Improved dissolution rate and dissolution properties | [87] |
| Valsartan | HPMC | Spray drying | Increased solubility, dissolution, and bioavailability | [88] |
| Docetaxel and Paclitaxel | PVP K30 | Spray drying | Increased solubility | [89] |
| Enzalutamide | HPMC and PVP-VA | Solvent evaporation | Increased dissolution, slower precipitation into aggregates of amorphous, increased bioavailability (in rats) | [90] |
| Nilotinib | Soluplus® | Spray drying | Increased solubility, increased bioavailability | [91] |
| Polymers | Polymer Types | Molecular Weight (Da) | Transition Glass Temperature (°C) | Study | Reference |
|---|---|---|---|---|---|
| Povidone K25 | Vinyl and its derivatives | 30 | 153 | PVP K25 can improve the stability of amorphous drugs | [115,116,117] |
| Povidone K17 | 10 | 140 | PVP K17 showed better results than PVP K90 in terms of solubility | [85,116,118] | |
| Povidone K30 | 50 | 160 | PVP K30 has the most optimal crystallization inhibition activity than other PVPs that have lower or higher molecular weights | [116,119,120,121] | |
| Carbomer | Polyacrylates and methacrylates | 7 × 105–4 × 109 | 100–105 | The addition of carbomer leads to prolonged dissolution | [122] |
| Eudragit® EPO | 135 | 52 | At low pH, EPO improved the solubility of crystalline and amorphous forms of the drug but did not inhibit crystallization | [116,123,124] | |
| Eudragit® RL PO | 32 | 63 | Eudragit® RL PO combined with hot melt extrusion method can solve the problems of bitter taste and poor solubility | [116,125,126] | |
| Hydroxypropylmethylcellulose (HPMC) | Cellulose and its derivatives | 10,000–1,500,000 | 170–180 | The presence of HPMC acts as crystallization inhibitor by increasing supersaturation degree of drug | [127,128] |
| Hypromellose acetate succinate (HPMCAS) | 55,000–90,000 | 113 ± 2 | HPMCAS stabilized supersaturated drug solution, increases dissolution, and also acts as a precipitation inhibitor. | [129,130] | |
| Methyl cellulose | 10,000–220,000 | 175 | [116,131] | ||
| Soluplus® | Other miscellaneous | 90,000–140,000 | ~70 | Soluplus® enhances bioavailability by increase solubility based on the results of in vitro dissolution test | [84,132] |
| Kollicoat® IR | ~45,000 | 45 | Kollicoat® IR improves water penetration and wettability of drugs and leads to improved dissolution rate | [116,133,134] | |
| Chitosan | 10,000–1,000,000 | 203 | Chitosan can increase the rate of dissolution, accompanied by a decrease in crystallinity and size of the drug which can increase dissolution | [135,136] |
| Drug | Polymer | Interaction | Results | Reference |
|---|---|---|---|---|
| Total biflavonoid extract from Selaginella deoderleinii (TBESD) | PVP K30 | FTIR: There was a shift in the C=O peak of PVP K-30 in TBESD-ASD from 1662.37 cm−1 to 1657.56 cm−1, indicating a hydrogen bond interaction between PVP K-30 and biflavonoids in TBESD, which indicates the hydrogen bonding interaction between PVP K-30 and biflavonoids in TBESD. | The results of the in vivo assay were that oral administration of TBESD-ASD to xenograft tumor-bearing mice resulted in a significant reduction in microvascular density and tumor size. | [248] |
| Low-dose paclitaxel | PVP K30 + sodium lauryl sulfate (SLS) | FTIR: There is a peak in the spectrum of the C=O group at 1700 cm−1 where the sharp double peak of paclitaxel di-hydrate turns into a single blunt peak, indicating the interaction of hydrogen groups. | Paclitaxel solid dispersion formulation (ModraPac100 capsules) has (almost) the same pharmacokinetic profile as the low-dose paclitaxel premix solution. | [187] |
| Paclitaxel (PTX) | PVP/VA S-630 TPGS | FTIR: Changes The peak spectra of amide I (-CO-NH-) in the SD4 and SD9 formulations significantly changed from 1645.2 cm−1 in paclitaxel to 1677.8 cm−1 (SD4) and 1660.8 cm−1 (SD9), indicating hydrogen bond interactions. | SD4 and SD9 formulations have significantly increased anticancer effects on breast cancer cells compared to PTX alone. | [249] |
| RA-XII isolated from R. yunnanensis | PVP K17 PVP K90 PVP K30 | FTIR: There is a shift in the spectrum of O-H and C=O groups, which indicates the hydrogen interaction between RA-XII and PVP. | The ASD formulation of RA-XII inhibited the proliferation of RKO cells better than free RA-XII. ASD formulation of RA- XII has a stronger therapeutic effect on colon cancer cells. | [250] |
| IIIM-290 | PEG-PPG-PEG PVP K-30 Gom Xanthan | FTIR: The presence of peak broadening in the hydroxyl group (O-H) region indicates the hydrogen bonding interaction of drug–polymer. | Solid dispersion injection in mice with Ehrlich ascites carcinoma resulted in a 1.9-fold increase in plasma exposure, resulting in 31–43% tumor inhibition. | [251] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Budiman, A.; Handini, A.L.; Muslimah, M.N.; Nurani, N.V.; Laelasari, E.; Kurniawansyah, I.S.; Aulifa, D.L. Amorphous Solid Dispersion as Drug Delivery Vehicles in Cancer. Polymers 2023, 15, 3380. https://doi.org/10.3390/polym15163380
Budiman A, Handini AL, Muslimah MN, Nurani NV, Laelasari E, Kurniawansyah IS, Aulifa DL. Amorphous Solid Dispersion as Drug Delivery Vehicles in Cancer. Polymers. 2023; 15(16):3380. https://doi.org/10.3390/polym15163380
Chicago/Turabian StyleBudiman, Arif, Annisa Luthfiyah Handini, Mutia Nur Muslimah, Neng Vera Nurani, Eli Laelasari, Insan Sunan Kurniawansyah, and Diah Lia Aulifa. 2023. "Amorphous Solid Dispersion as Drug Delivery Vehicles in Cancer" Polymers 15, no. 16: 3380. https://doi.org/10.3390/polym15163380
APA StyleBudiman, A., Handini, A. L., Muslimah, M. N., Nurani, N. V., Laelasari, E., Kurniawansyah, I. S., & Aulifa, D. L. (2023). Amorphous Solid Dispersion as Drug Delivery Vehicles in Cancer. Polymers, 15(16), 3380. https://doi.org/10.3390/polym15163380