Fracture Resistance of Class II MOD Cavities Restored by Direct and Indirect Techniques and Different Materials Combination
Abstract
:1. Introduction
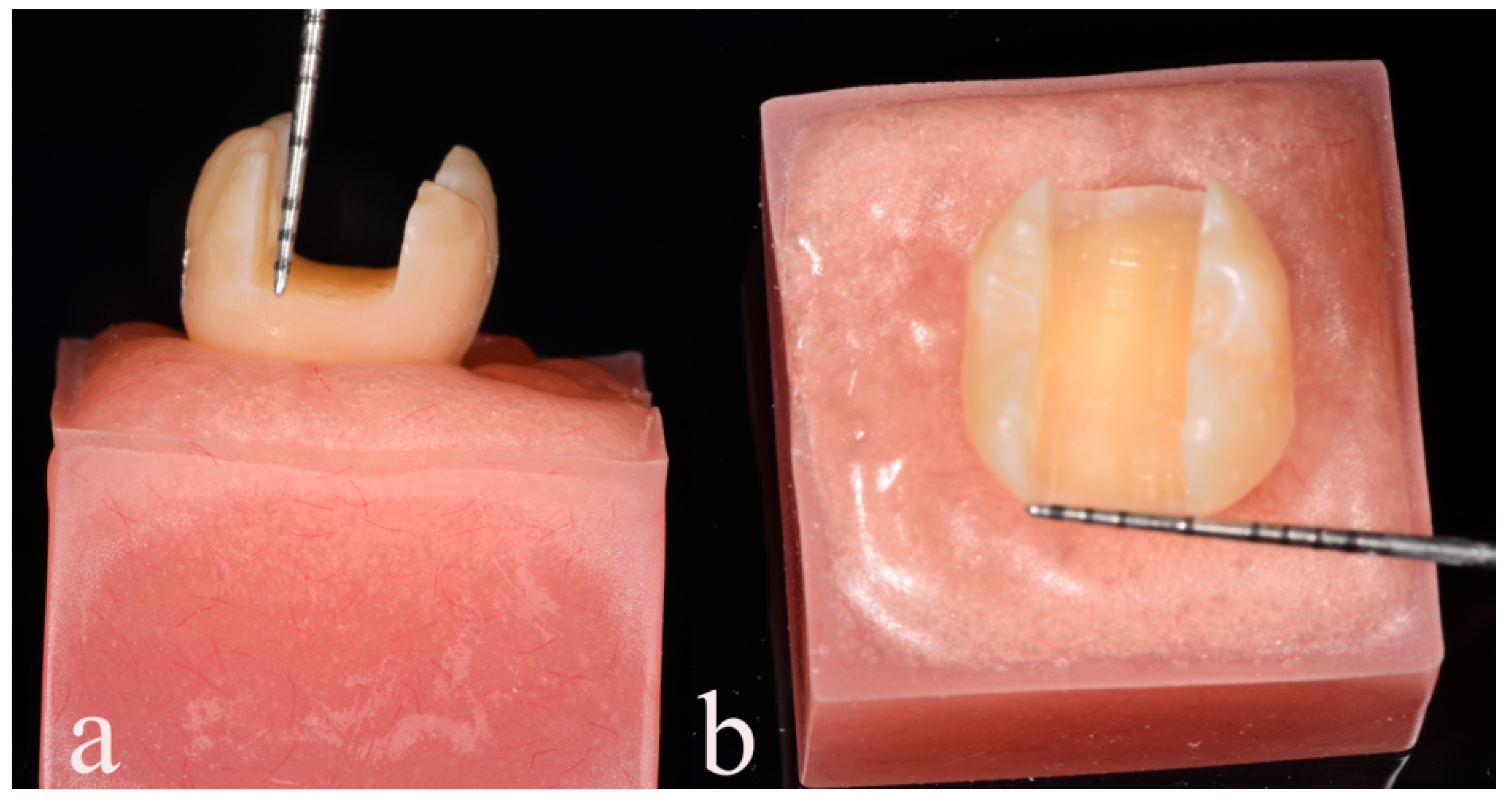
2. Materials and Methods
- Type I—Minimal fracture or minor crack within the crown;
- Type II—Loss of less than half of the crown structure;
- Type III—Crown fracture extending through the midline, with displacement or loss of half of the crown;
- Type IV—Loss of more than half of the crown structure;
- Type V—Severe fracture involving both tooth and crown components.
Statistical Analysis
3. Results
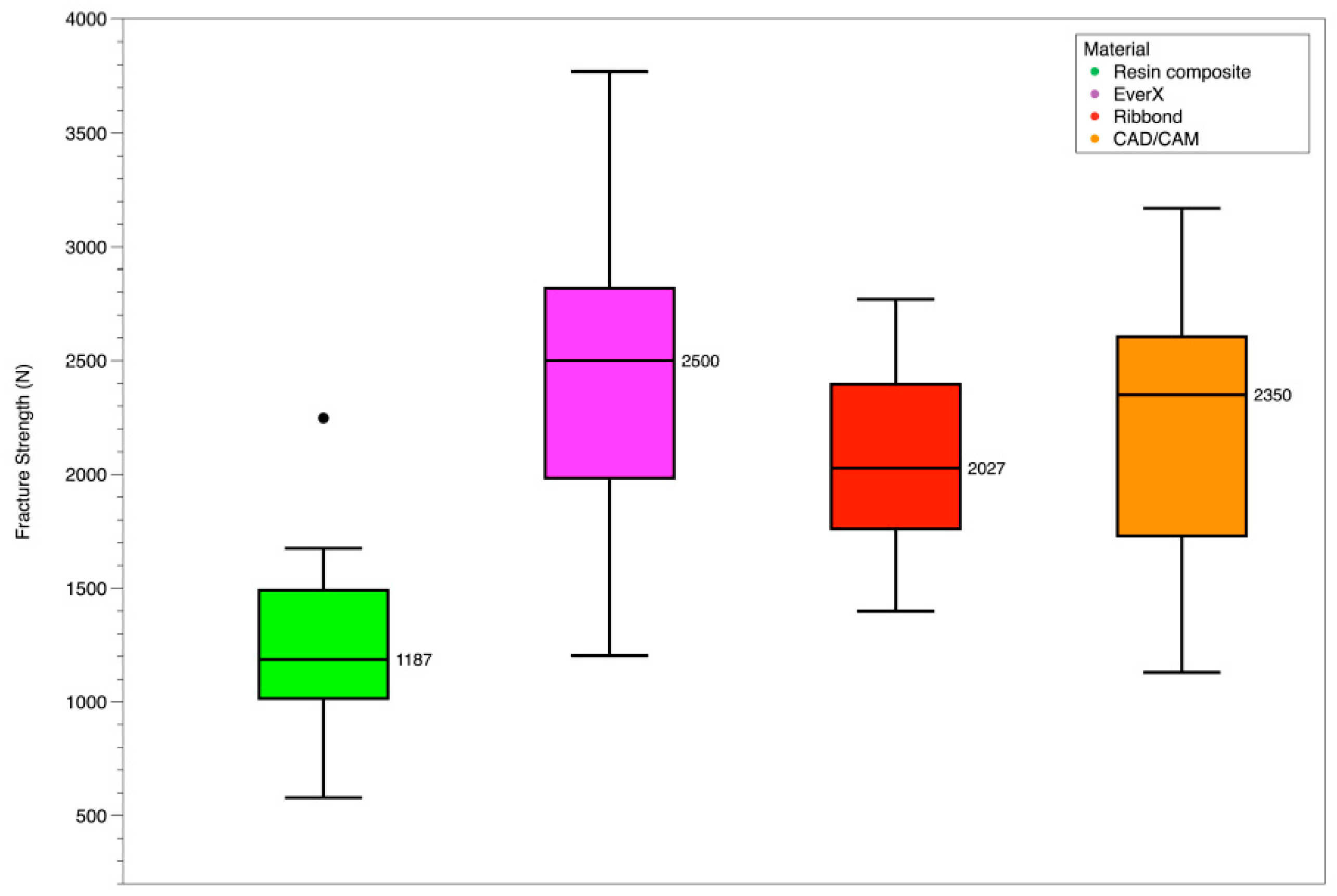
Peak Fracture Toughness
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferracane, J.L. Resin-based composite performance: Are there some things we can’t predict? Dent. Mater. 2013, 29, 51–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schlichting, L.H.; Magne, P. Double-milled CAD-CAM composite resin restorations: A proof-of-concept approach to producing histoanatomic bilaminar restorations. J. Prosthet. Dent. 2020, 124, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Beyer, C.; Schwahn, C.; Meyer, G.; Söhnel, A. What German dentists choose for their teeth: A Web-based survey of molar restorations and their longevity. J. Prosthet. Dent. 2021, 125, 805–814. [Google Scholar] [CrossRef]
- Bayne, S.C.; Ferracane, J.L.; Marshall, G.W.; Marshall, S.J.; van Noort, R. The Evolution of Dental Materials over the Past Century: Silver and Gold to Tooth Color and Beyond. J. Dent. Res. 2019, 98, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Soares, L.M.; Razaghy, M.; Magne, P. Optimization of large MOD restorations: Composite resin inlays vs. short fiber-reinforced direct restorations. Dent. Mater. 2018, 34, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Sarrett, D. Clinical challenges and the relevance of materials testing for posterior composite restorations. Dent. Mater. 2005, 21, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Yadav, R.; Kumar, M. Dental restorative composite materials: A review. J. Oral Biosci. 2019, 61, 78–83. [Google Scholar] [CrossRef]
- Fugolin, A.P.P.; Pfeifer, C.S. New Resins for Dental Composites. J. Dent. Res. 2017, 96, 1085–1091. [Google Scholar] [CrossRef]
- Roussou, K.; Nikolaidis, A.K.; Ziouti, F.; Arhakis, A.; Arapostathis, K.; Koulaouzidou, E.A. Cytotoxic Evaluation and Determination of Organic and Inorganic Eluates from Restorative Materials. Molecules 2021, 26, 4912. [Google Scholar] [CrossRef]
- Wiltshire, W.A.; Ferreira, M.R.; Ligthelm, A.J. Allergies to dental materials. Quintessence Int. 1996, 27, 513–520. [Google Scholar]
- Unemori, M.; Matsuya, Y.; Akashi, A.; Goto, Y.; Akamine, A. Composite resin restoration and postoperative sensitivity: Clinical follow-up in an undergraduate program. J. Dent. 2001, 29, 7–13. [Google Scholar] [CrossRef] [Green Version]
- Jafarpour, S.; El-Badrawy, W.; Jazi, H.; McComb, D. Effect of Composite Insertion Technique on Cuspal Deflection Using an In Vitro Simulation Model. Oper. Dent. 2012, 37, 299–305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nedeljkovic, I.; De Munck, J.; VanLoy, A.; Declerck, D.; Lambrechts, P.; Peumans, M.; Teughels, W.; Van Meerbeek, B.; Van Landuyt, K.L. Secondary caries: Prevalence, characteristics, and approach. Clin. Oral Investig. 2020, 24, 683–691. [Google Scholar] [CrossRef]
- McHugh, L.E.J.; Politi, I.; Al-Fodeh, R.S.; Fleming, G.J.P. Implications of resin-based composite (RBC) restoration on cuspal deflection and microleakage score in molar teeth: Placement protocol and restorative material. Dent. Mater. 2017, 33, e329–e335. [Google Scholar] [CrossRef]
- Ausiello, P.; Ciaramella, S.; De Benedictis, A.; Lanzotti, A.; Tribst, J.P.M.; Watts, D.C. The use of different adhesive filling material and mass combinations to restore class II cavities under loading and shrinkage effects: A 3D-FEA. Comput. Methods Biomech. Biomed. Eng. 2021, 24, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Kim, R.; Ferracane, J.L.; Lee, I.B. Influence of the Compliance and Layering Method on the Wall Deflection of Simulated Cavities in Bulk-fill Composite Restoration. Oper. Dent. 2016, 41, e183–e194. [Google Scholar] [CrossRef]
- Ausiello, P.; Ciaramella, S.; Di Rienzo, A.; Lanzotti, A.; Ventre, M.; Watts, D.C. Adhesive class I restorations in sound molar teeth incorporating combined resin-composite and glass ionomer materials: CAD-FE modeling and analysis. Dent. Mater. 2019, 35, 1514–1522. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Milani, T. Short-fiber Reinforced MOD Restorations of Molars with Severely Undermined Cusps. J. Adhes. Dent. 2023, 25, 99–106. [Google Scholar] [CrossRef]
- Spitznagel, F.A.; Scholz, K.J.; Strub, J.R.; Vach, K.; Gierthmuehlen, P.C. Polymer-infiltrated ceramic CAD/CAM inlays and partial coverage restorations: 3-year results of a prospective clinical study over 5 years. Clin. Oral Investig. 2018, 22, 1973–1983. [Google Scholar] [CrossRef]
- Aziz, A.M.; El-Mowafy, O.; Tenenbaum, H.C.; Lawrence, H.P. Clinical performance of CAD-CAM crowns provided by predoctoral students at the University of Toronto. J. Prosthet. Dent. 2022, 127, 729–736. [Google Scholar] [CrossRef]
- Magne, P. Efficient 3D finite element analysis of dental restorative procedures using micro-CT data. Dent. Mater. 2007, 23, 539–548. [Google Scholar] [CrossRef]
- Ordinola-Zapata, R.; Lin, F.; Nagarkar, S.; Perdigão, J. A critical analysis of research methods and experimental models to study the load capacity and clinical behaviour of the root filled teeth. Int. Endod. J. 2022, 55, 471–494. [Google Scholar] [CrossRef]
- Choi, A.H.; Conway, R.C.; Ben-Nissan, B. Finite-element modeling and analysis in nanomedicine and dentistry. Nanomedicine 2014, 9, 1681–1695. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, S. Finite element analysis: A boon to dentistry. J. Oral Biol. Craniofacial Res. 2014, 4, 200–203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hofsteenge, J.W.; Hogeveen, F.; Cune, M.S.; Gresnigt, M.M. Effect of immediate dentine sealing on the aging and fracture strength of lithium disilicate inlays and overlays. J. Mech. Behav. Biomed. Mater. 2020, 110, 103906. [Google Scholar] [CrossRef] [PubMed]
- Batalha-Silva, S.; de Andrada, M.A.; Maia, H.P.; Magne, P. Fatigue resistance and crack propensity of large MOD composite resin restorations: Direct versus CAD/CAM inlays. Dent. Mater. 2013, 29, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Murakami, N.; Wakabayashi, N. Finite element contact analysis as a critical technique in dental biomechanics: A review. J. Prosthodont. Res. 2014, 58, 92–101. [Google Scholar] [CrossRef]
- Kwon, Y.; Ferracane, J.; Lee, I.-B. Effect of layering methods, composite type, and flowable liner on the polymerization shrinkage stress of light cured composites. Dent. Mater. 2012, 28, 801–809. [Google Scholar] [CrossRef]
- Park, J.; Chang, J.; Ferracane, J.; Lee, I.B. How should composite be layered to reduce shrinkage stress: Incremental or bulk filling? Dent. Mater. 2008, 24, 1501–1505. [Google Scholar] [CrossRef]
- Kaisarly, D.; El Gezawi, M.; Keßler, A.; Rösch, P.; Kunzelmann, K.-H. Shrinkage vectors in flowable bulk-fill and conventional composites: Bulk versus incremental application. Clin. Oral Investig. 2021, 25, 1127–1139. [Google Scholar] [CrossRef]
- Garoushi, S.; Gargoum, A.; Vallittu, P.K.; Lassila, L. Short fiber-reinforced composite restorations: A review of the current literature. J. Investig. Clin. Dent. 2018, 9, 12330. [Google Scholar] [CrossRef] [PubMed]
- Besegato, J.F.; Jussiani, E.I.; Andrello, A.C.; Fernandes, R.V.; Salomão, F.M.; Vicentin, B.L.S.; Dezan-Garbelini, C.C.; Hoeppner, M.G. Effect of light-curing protocols on the mechanical behavior of bulk-fill resin composites. J. Mech. Behav. Biomed. Mater. 2019, 90, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Algamaiah, H.; Silikas, N.; Watts, D.C. Polymerization shrinkage and shrinkage stress development in ultra-rapid photo-polymerized bulk fill resin composites. Dent. Mater. 2021, 37, 559–567. [Google Scholar] [CrossRef]
- Dejak, B.; Młotkowski, A. A comparison of stresses in molar teeth restored with inlays and direct restorations, including polymerization shrinkage of composite resin and tooth loading during mastication. Dent. Mater. 2015, 31, e77–e87. [Google Scholar] [CrossRef]
- Molnár, J.; Fráter, M.; Sáry, T.; Braunitzer, G.; Vallittu, P.K.; Lassila, L.; Garoushi, S. Fatigue performance of endodontically treated molars restored with different dentin replacement materials. Dent. Mater. 2022, 38, e83–e93. [Google Scholar] [CrossRef] [PubMed]
- Fráter, M.; Sáry, T.; Vincze-Bandi, E.; Volom, A.; Braunitzer, G.; Szabó, P.B.S.; Garoushi, S.; Forster, A. Fracture Behavior of Short Fiber-Reinforced Direct Restorations in Large MOD Cavities. Polymers 2021, 13, 2040. [Google Scholar] [CrossRef]
- Fráter, M.; Sáry, T.; Braunitzer, G.; Balázs Szabó, P.; Lassila, L.; Vallittu, P.K.; Garoushi, S. Fatigue failure of anterior teeth without ferrule restored with individualized fiber-reinforced post-core foundations. J. Mech. Behav. Biomed. Mater. 2021, 118, 104440. [Google Scholar] [CrossRef]
- Fráter, M.; Forster, A.; Keresztúri, M.; Braunitzer, G.; Nagy, K. In vitro fracture resistance of molar teeth restored with a short fibre-reinforced composite material. J. Dent. 2014, 42, 1143–1150. [Google Scholar] [CrossRef]
- Battancs, E.; Sáry, T.; Molnár, J.; Braunitzer, G.; Skolnikovics, M.; Schindler, Á.; Szabó, P.B.; Garoushi, S.; Fráter, M. Fracture Resistance and Microleakage around Direct Restorations in High C-Factor Cavities. Polymers 2022, 14, 3463. [Google Scholar] [CrossRef]
- Rudo, D.N.; Karbhari, V.M. Physical behaviors of fiber reinforcement as applied to tooth stabilization. Dent. Clin. N. Am. 1999, 43, 7–35. [Google Scholar] [CrossRef]
- Belli, S.; Erdemir, A.; Ozcopur, M.; Eskitascioglu, G. The effect of fibre insertion on fracture resistance of root filled molar teeth with MOD preparations restored with composite. Int. Endod. J. 2005, 38, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Başaran, E.G.; Ayna, E.; Vallittu, P.K.; Lassila, L.V. Load bearing capacity of fiber-reinforced and unreinforced composite resin CAD/CAM-fabricated fixed dental prostheses. J. Prosthet. Dent. 2013, 109, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Dyer, S.R.; Lassila, L.V.; Jokinen, M.; Vallittu, P.K. Effect of fiber position and orientation on fracture load of fiber-reinforced composite. Dent. Mater. 2004, 20, 947–955. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K. Use of woven glass fibres to reinforce a composite veneer. A fracture resistance and acoustic emission study. J. Oral Rehabil. 2002, 29, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Rocca, G.T.; Saratti, C.M.; Poncet, A.; Feilzer, A.J.; Krejci, I. The influence of FRCs reinforcement on marginal adaptation of CAD/CAM composite resin endocrowns after simulated fatigue loading. Odontology 2016, 104, 220–232. [Google Scholar] [CrossRef] [PubMed]
- Garoushi, S.; Tanner, J.; Keulemans, F.; Le Bell-Rönnlöf, A.M.; Lassila, L.; Vallittu, P.K. Fiber Reinforcement of Endodontically Treated Teeth: What Options Do We Have? Literature Review. Eur. J. Prosthodont. Restor. Dent. 2020, 28, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Mangoush, E.; Garoushi, S.; Lassila, L.; Vallittu, P.K.; Säilynoja, E. Effect of Fiber Reinforcement Type on the Performance of Large Posterior Restorations: A Review of In Vitro Studies. Polymers 2021, 13, 3682. [Google Scholar] [CrossRef]
- Gale, M.; Darvell, B. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Burke, F.J. Fracture resistance of teeth restored with dentin-bonded crowns constructed in a leucite-reinforced ceramic. Dent. Mater. 1999, 15, 359–362. [Google Scholar] [CrossRef]
- Hellmann, D.; Giannakopoulos, N.N.; Schmitter, M.; Lenz, J.; Schindler, H.J. Anterior and posterior neck muscle activation during a variety of biting tasks. Eur. J. Oral Sci. 2012, 120, 326–334. [Google Scholar] [CrossRef]
- Bakke, M. Bite Force and Occlusion. Semin. Orthod. 2006, 12, 120–126. [Google Scholar] [CrossRef]
- Nishigawa, K.; Bando, E.; Nakano, M. Quantitative study of bite force during sleep associated bruxism. J. Oral Rehabil. 2001, 28, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, C.; Dionysopoulos, D.; Tolidis, K.; Kouros, P.; Koliniotou-Koumpia, E.A.; Tsitrou, E. Structural Integrity Evaluation of Large MOD Restorations Fabricated with a Bulk-Fill and a CAD/CAM Resin Composite Material. Oper. Dent. 2019, 44, 312–321. [Google Scholar] [CrossRef] [PubMed]
- Davidson, C.L.; De Gee, A.J. Relaxation of Polymerization Contraction Stresses by Flow in Dental Composites. J. Dent. Res. 1984, 63, 146–148. [Google Scholar] [CrossRef]
- Chai, H.; Lawn, B.R. Fracture resistance of molar teeth with mesial-occlusal-distal (MOD) restorations. Dent. Mater. 2017, 33, e283–e289. [Google Scholar] [CrossRef]
- Soares, C.J.; Faria-E-Silva, A.L.; Rodrigues, M.P.; Vilela, A.B.F.; Pfeifer, C.S.; Tantbirojn, D.; Versluis, A. Polymerization shrinkage stress of composite resins and resin cements—What do we need to know? Braz. Oral Res. 2017, 31, e62. [Google Scholar] [CrossRef] [Green Version]
- Butterworth, C.; Ellakwa, A.E.; Shortall, A. Fibre-Reinforced Composites in Restorative Dentistry. Dent. Updat. 2003, 30, 300–306. [Google Scholar] [CrossRef]
- Goldberg, A.J.; Burstone, C.J. The use of continuous fiber reinforcement in dentistry. Dent. Mater. 1992, 8, 197–202. [Google Scholar] [CrossRef]
- Jakab, A.; Volom, A.; Sáry, T.; Vincze-Bandi, E.; Braunitzer, G.; Alleman, D.; Garoushi, S.; Fráter, M. Mechanical Performance of Direct Restorative Techniques Utilizing Long Fibers for “Horizontal Splinting” to Reinforce Deep MOD Cavities—An Updated Literature Review. Polymers 2022, 14, 1438. [Google Scholar] [CrossRef]
- Garoushi, S.; Vallittu, P.K.; Lassila, L.V. Short glass fiber reinforced restorative composite resin with semi-inter penetrating polymer network matrix. Dent. Mater. 2007, 23, 1356–1362. [Google Scholar] [CrossRef]
- Ayad, M.F.; Maghrabi, A.A.; García-Godoy, F. Resin composite polyethylene fiber reinforcement: Effect on fracture resistance of weakened marginal ridges. Am. J. Dent. 2010, 23, 133. [Google Scholar] [PubMed]
- Sadr, A.; Bakhtiari, B.; Hayashi, J.; Luong, M.N.; Chen, Y.W.; Chyz, G.; Chan, D.; Tagami, J. Effects of fiber reinforcement on adaptation and bond strength of a bulk-fill composite in deep preparations. Dent. Mater. 2020, 36, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Garoushi, S.; Kaleem, M.; Shinya, A.; Vallittu, P.K.; Satterthwaite, J.D.; Watts, D.C.; Lassila, L.V. Creep of experimental short fiber-reinforced composite resin. Dent. Mater. J. 2012, 31, 737–741. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Material | Type | Composition | Manufacture | |
|---|---|---|---|---|
| Ribbond | Polyethylene fibers | Preimpregnated, silanized, plasma-treated, leno-woven, ultra-high modulus polyethylene fibers. | Ribbond | |
| Matrix | Fillers | |||
| EverX posterior | Millimeter-scale short-fiber-reinforced composite | Bis-GMA, TEGDMA, PMMA. | Silicon dioxide (max. 5 wt%), Barium glass (max. 70 wt%) E-glass fiber (max. 15 wt%). | GC |
| Brilliant Crios | nano-hybrid CAD/CAM composite block | (28.4 wt%) cross-linked Bis-GMA, bis-EMA, UDMA | Amorphous SiO2 (<20 nm), barium glass (<1 nm), bis-EMA, UDMA, inorganic pigments: ferrous oxide or titanium dioxide | Coltene Whaledent AG |
| Tetric | Nano-hybrid composite | (18.8 wt%) BisGMA, TEGDMA, UDMA | Barium glass filler, Ytterbium trifluoride, mixed oxide (63.5 wt%), polymer (17 wt%), additive, catalysts, pigments, stabilizers (0.7 wt%) Particle size: 0.04–3 μm | Ivoclar Vivadent Schaan, Liechtenstein. |
| Material | Peak Fracture (N) |
|---|---|
| Resin composite | 1242 ± 436 |
| EverX | 2471 ± 761 |
| CAD/CAM | 2166 ± 615 |
| Ribbond | 1923 ± 492 |
| Mode of Fracture | Group 1 Resin Composite | Group 2 E verx | Group 3 Ribbond | Group 4 CAD/CAM |
|---|---|---|---|---|
| TYPE I (Minimal fracture or crack in the crown) | 0 | 2 | 4 | 0 |
| TYPE II (Less than half of the crown lost) | 0 | 9 | 4 | 3 |
| TYPE III (Half of the crown displaced or lost) | 5 | 4 | 5 | 7 |
| TYPE IV (More than half of the crown lost) | 6 | 0 | 2 | 5 |
| TYPE V (Severe fracture of the tooth and/or crown) | 7 | 0 | 0 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsertsidou, V.; Mourouzis, P.; Dionysopoulos, D.; Pandoleon, P.; Tolidis, K. Fracture Resistance of Class II MOD Cavities Restored by Direct and Indirect Techniques and Different Materials Combination. Polymers 2023, 15, 3413. https://doi.org/10.3390/polym15163413
Tsertsidou V, Mourouzis P, Dionysopoulos D, Pandoleon P, Tolidis K. Fracture Resistance of Class II MOD Cavities Restored by Direct and Indirect Techniques and Different Materials Combination. Polymers. 2023; 15(16):3413. https://doi.org/10.3390/polym15163413
Chicago/Turabian StyleTsertsidou, Vasiliki, Petros Mourouzis, Dimitrios Dionysopoulos, Panagiotis Pandoleon, and Kosmas Tolidis. 2023. "Fracture Resistance of Class II MOD Cavities Restored by Direct and Indirect Techniques and Different Materials Combination" Polymers 15, no. 16: 3413. https://doi.org/10.3390/polym15163413
APA StyleTsertsidou, V., Mourouzis, P., Dionysopoulos, D., Pandoleon, P., & Tolidis, K. (2023). Fracture Resistance of Class II MOD Cavities Restored by Direct and Indirect Techniques and Different Materials Combination. Polymers, 15(16), 3413. https://doi.org/10.3390/polym15163413








