An Overview of Scaffolds and Biomaterials for Skin Expansion and Soft Tissue Regeneration: Insights on Zinc and Magnesium as New Potential Key Elements
Abstract
1. Introduction
2. Mechanotransduction in Skin

3. The Influence of Mechanical Forces on the Structure and Function of the Skin
4. Skin Expansion in Reconstructive Surgery
5. Scaffold Fabrication Methods Used for Tissue Engineering
6. Materials Used for Skin Tissue Engineering
6.1. Natural Materials
6.1.1. Silk
6.1.2. Chitosan
6.1.3. Collagen Type I
6.1.4. Elastin
6.1.5. Silicon
6.2. Synthetic Bioresorbable Polymers
6.2.1. Polycaprolactone (PCL)
6.2.2. Poly(d,l-lactic-co-glycolic acid) (PLGA)
6.3. Absorbable Metallic Materials
6.3.1. Magnesium (Mg)
Magnesium and Its Alloys for Medical Applications
6.3.2. Zinc (Zn)
Zinc and Its Alloys for Medical Applications
6.3.3. Zn–Mg Alloys
7. Experimental Studies of Magnesium and Zinc in Soft Tissue Engineering
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Ingber, D. Integrins as mechanochemical transducers. Curr. Opin. Cell Biol. 1991, 3, 841–848. [Google Scholar] [CrossRef]
- Davidson, J.M.; Aquino, A.M.; Woodward, S.C.; Wilfinger, W.W. Sustained microgravity reduces intrinsic wound healing and growth factor responses in the rat. FASEB J. 1999, 13, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Jhala, D.V.; Kale, R.K.; Singh, R.P. Microgravity Alters Cancer Growth and Progression. Curr. Cancer Drug Targets 2014, 14, 394–406. [Google Scholar] [CrossRef] [PubMed]
- Farahani, R.M.; A DiPietro, L. Microgravity and the implications for wound healing. Int. Wound J. 2008, 5, 552–561. [Google Scholar] [CrossRef]
- Evans, N.D.; Oreffo, R.; Healy, E.; Thurner, P.; Man, Y. Epithelial mechanobiology, skin wound healing, and the stem cell niche. J. Mech. Behav. Biomed. 2013, 28, 397–409. [Google Scholar] [CrossRef]
- Silver, F.H.; Siperko, L.M.; Seehra, G.P. Mechanobiology of force transduction in dermal tissue. Ski. Res. Technol. 2003, 9, 3–23. [Google Scholar] [CrossRef] [PubMed]
- Tranquillo, R.T.; Durrani, M.A.; Moon, A.G. Tissue engineering science: Consequences of cell traction force. Cytotechnology 1992, 10, 225–250. [Google Scholar] [CrossRef]
- Takei, T.; Mills, I.; Arai, K.; Sumpio, B.E. Molecular Basis for Tissue Expansion: Clinical Implications for the Surgeon. Plast. Reconstr. Surg. 1998, 102, 247–258. [Google Scholar] [CrossRef]
- Huang, S.; Ingber, D.E. The structural and mechanical complexity of cell-growth control. Nature 1999, 1, E131–E138. [Google Scholar] [CrossRef]
- Wang, J.H.-C.; Thampatty, B.P. An Introductory Review of Cell Mechanobiology. Biomech. Model. Mechanobiol. 2006, 5, 1–16. [Google Scholar] [CrossRef]
- Huang, S.; Ingber, D.E. Shape-Dependent Control of Cell Growth, Differentiation, and Apoptosis: Switching between Attractors in Cell Regulatory Networks. Exp. Cell Res. 2000, 261, 91–103. [Google Scholar] [CrossRef] [PubMed]
- Herndon, D.N.; Barrow, R.E.; Rutan, R.L.; Rutan, T.C.; Desai, M.H.; Abston, S. A Comparison of Conservative Versus Early Excision. Therapies in severely burned patients. Ann. Surg. 1989, 209, 547–553; discussion 552–553. [Google Scholar] [CrossRef] [PubMed]
- Langer, R.; Vacanti, J. Tissue engineering. Science 1993, 260, 920–926. [Google Scholar] [CrossRef] [PubMed]
- Karp, J.M.; Langer, R. Development and therapeutic applications of advanced biomaterials. Curr. Opin. Biotechnol. 2007, 18, 454–459. [Google Scholar] [CrossRef]
- Ikada, Y. Challenges in tissue engineering. J. R. Soc. Interface 2006, 3, 589–601. [Google Scholar] [CrossRef]
- Tepole, A.B.; Ploch, C.J.; Wong, J.; Gosain, A.K.; Kuhl, E. Growing skin: A computational model for skin expansion in reconstructive surgery. J. Mech. Phys. Solids 2011, 59, 2177–2190. [Google Scholar] [CrossRef]
- Neumann, C.G. The expansion of an area of skin by progressive distention of a subcutaneous balloon; use of the method for securing skin for subtotal reconstruction of the ear. Plast. Reconstr. Surg. 1957, 19, 124–130. [Google Scholar] [CrossRef]
- Wagh, M.; Dixit, V. Tissue expansion: Concepts, techniques and unfavourable results. Indian J. Plast. Surg. 2013, 46, 333–348. [Google Scholar] [CrossRef]
- Langer, R.; Tirrell, D.A. Designing materials for biology and medicine. Nature 2004, 428, 487–492. [Google Scholar] [CrossRef]
- Wong, V.W.; Longaker, M.T.; Gurtner, G.C. Soft tissue mechanotransduction in wound healing and fibrosis. Semin. Cell Dev. Biol. 2012, 23, 981–986. [Google Scholar] [CrossRef]
- Zöllner, A.M.; Tepole, A.B.; Kuhl, E. On the biomechanics and mechanobiology of growing skin. J. Theor. Biol. 2012, 297, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.H.-C.; Thampatty, B.P.; Lin, J.-S.; Im, H.-J. Mechanoregulation of gene expression in fibroblasts. Gene 2007, 391, 1–15. [Google Scholar] [CrossRef]
- Derderian, C.A.; Bastidas, N.; Lerman, O.Z.; Bhatt, K.A.; Lin, S.-E.; Voss, J.; Holmes, J.W.; Levine, J.P.; Gurtner, G.C. Mechanical Strain Alters Gene Expression in an in Vitro Model of Hypertrophic Scarring. Ann. Plast. Surg. 2005, 55, 69–75; discussion 75. [Google Scholar] [CrossRef] [PubMed]
- Silver, F.H.; Siperko, L.M. Mechanosensing and Mechanochemical Transduction: How Is Mechanical Energy Sensed and Converted Into Chemical Energy in an Extracellular Matrix? Crit. Rev. Biomed. Eng. 2003, 31, 78. [Google Scholar] [CrossRef]
- Wong, V.; Levi, K.; Akaishi, S.; Schultz, G.; Dauskardt, R. Scar zones: Region-specific differences in skin tension may determine incisional scar formation. Plast. Reconstr. Surg. 2012, 129, 1272–1276. [Google Scholar] [CrossRef]
- Montesano, R.; Orci, L. Transforming growth factor beta stimulates collagen-matrix contraction by fibroblasts: Implications for wound healing. Proc. Natl. Acad. Sci. USA 1988, 85, 4894–4897. [Google Scholar] [CrossRef] [PubMed]
- Halfter, W.; Liverani, D.; Vigny, M.; Monard, D. Deposition of extracellular matrix along the pathways of migrating fibroblasts. Cell Tissue Res. 1990, 262, 467–481. [Google Scholar] [CrossRef] [PubMed]
- Sander, E.A.; Barocas, V.H.; Tranquillo, R.T. Initial Fiber Alignment Pattern Alters Extracellular Matrix Synthesis in Fibroblast-Populated Fibrin Gel Cruciforms and Correlates with Predicted Tension. Ann. Biomed. Eng. 2010, 39, 714–729. [Google Scholar] [CrossRef]
- Wong, V.W.; Akaishi, S.; Longaker, M.T.; Gurtner, G.C. Pushing Back: Wound Mechanotransduction in Repair and Regeneration. J. Investig. Dermatol. 2011, 131, 2186–2196. [Google Scholar] [CrossRef]
- Ko, K.S.; McCulloch, C.A. Intercellular Mechanotransduction: Cellular Circuits That Coordinate Tissue Responses to Mechanical Loading. Biochem. Biophys. Res. Commun. 2001, 285, 1077–1083. [Google Scholar] [CrossRef]
- Geffeney, S.L.; Goodman, M.B. How We Feel: Ion Channel Partnerships that Detect Mechanical Inputs and Give Rise to Touch and Pain Perception. Neuron 2012, 74, 609–619. [Google Scholar] [CrossRef] [PubMed]
- Powell, H.M.; McFarland, K.L.; Butler, D.L.; Supp, D.M.; Boyce, S.T. Uniaxial Strain Regulates Morphogenesis, Gene Expression, and Tissue Strength in Engineered Skin. Tissue Eng. Part A 2010, 16, 1083–1092. [Google Scholar] [CrossRef] [PubMed]
- De Filippo, R.E.; Atala, A. Stretch and Growth: The Molecular and Physiologic Influences of Tissue Expansion. Plast. Reconstr. Surg. 2002, 109, 2450–2462. [Google Scholar] [CrossRef] [PubMed]
- Tepole, A.B.; Gart, M.; Gosain, A.K.; Kuhl, E. Characterization of living skin using multi-view stereo and isogeometric analysis. Acta Biomater. 2014, 10, 4822–4831. [Google Scholar] [CrossRef] [PubMed]
- Wilhelmi, B.J.; Blackwell, S.J.; Mancoll, J.S.; Phillips, L.G. Creep vs. Stretch: A Review of the Viscoelastic Properties of Skin. Ann. Plast. Surg. 1998, 41, 215–219. [Google Scholar] [CrossRef]
- LoGiudice, J.; Gosain, A.K. Pediatric Tissue Expansion: Indications and Complications. J. Craniofacial Surg. 2003, 14, 866–872. [Google Scholar] [CrossRef] [PubMed]
- Filho, P.T.B.; Neves, R.I.; Gemperli, R.; Kaweski, S.; Kahler, S.H.; Banducci, D.R.; Manders, E.K. Soft-Tissue Expansion in Lower Extremity Reconstruction. Clin. Plast. Surg. 1991, 18, 593–599. [Google Scholar] [CrossRef]
- Beauchene, J.; Chambers, M.; Peterson, A.; Scott, P. Biochemical, biomechanical, and physical changes in the skin in an experimental animal model of therapeutic tissue expansion. J. Surg. Res. 1989, 47, 507–514. [Google Scholar] [CrossRef]
- Pietramaggiori, G.; Liu, P.; Scherer, S.S.; Kaipainen, A.; Prsa, M.J.; Mayer, H.; Newalder, J.; Alperovich, M.; Mentzer, S.J.; Konerding, M.A.; et al. Tensile Forces Stimulate Vascular Remodeling and Epidermal Cell Proliferation in Living Skin. Ann. Surg. 2007, 246, 896–902. [Google Scholar] [CrossRef]
- Purnell, C.A.; Gart, M.S.; Buganza-Tepole, A.; Tomaszewski, J.P.; Topczewska, J.M.; Kuhl, E.; Gosain, A.K. Determining the Differential Effects of Stretch and Growth in Tissue-Expanded Skin: Combining Isogeometric Analysis and Continuum Mechanics in a Porcine Model. Dermatol. Surg. 2018, 44, 48–52. [Google Scholar] [CrossRef]
- Huang, C.; Akaishi, S.; Ogawa, R. Mechanosignaling pathways in cutaneous scarring. Arch. Dermatol. Res. 2012, 304, 589–597. [Google Scholar] [CrossRef] [PubMed]
- Hinz, B.; Gabbiani, G. Mechanisms of force generation and transmission by myofibroblasts. Curr. Opin. Biotechnol. 2003, 14, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Aarabi, S.; Bhatt, K.A.; Shi, Y.; Paterno, J.; Chang, E.I.; Loh, S.A.; Holmes, J.W.; Longaker, M.T.; Yee, H.; Gurtner, G.C. Mechanical load initiates hypertrophic scar formation through decreased cellular apoptosis. FASEB J. 2007, 21, 3250–3261. [Google Scholar] [CrossRef] [PubMed]
- Ismavel, R.; Samuel, S.; Boopalan, P.R.J.V.C.; Chittaranjan, S.B. A Simple Solution for Wound Coverage by Skin Stretching. J. Orthop. Trauma 2011, 25, 127–132. [Google Scholar] [CrossRef]
- Lancerotto, L.; Chin, M.S.; Freniere, B.; Lujan-Hernandez, J.R.; Li, Q.; Vasquez, A.V.; Bassetto, F.; Del Vecchio, D.A.; Lalikos, J.F.; Orgill, D.P. Mechanisms of Action of External Volume Expansion Devices. Plast. Reconstr. Surg. 2013, 132, 569–578. [Google Scholar] [CrossRef]
- Ingber, D.E. Tensegrity: The architectural basis of cellular mechanotransduction. Annu. Rev. Physiol. 1997, 59, 575–599. [Google Scholar] [CrossRef]
- Orgill, D.P.; Bayer, L. Negative pressure wound therapy: Past, present and future. Int. Wound J. 2013, 10 (Suppl. S1), 15–19. [Google Scholar] [CrossRef]
- Lancerotto, L.; Bayer, L.R.; Orgill, D.P. Mechanisms of action of microdeformational wound therapy. Semin. Cell Dev. Biol. 2012, 23, 987–992. [Google Scholar] [CrossRef]
- Omar, M.T.; Alghadir, A.; Al-Wahhabi, K.K.; Al-Askar, A.B. Efficacy of shock wave therapy on chronic diabetic foot ulcer: A single-blinded randomized controlled clinical trial. Diabetes Res. Clin. Pract. 2014, 106, 548–554. [Google Scholar] [CrossRef]
- Ottomann, C.; Stojadinovic, A.; Lavin, P.T.; Gannon, F.H.; Heggeness, M.H.; Thiele, R.; Schaden, W.; Hartmann, B. Prospective Randomized Phase II Trial of Accelerated Reepithelialization of Superficial Second-Degree Burn Wounds Using Extracorporeal Shock Wave Therapy. Ann. Surg. 2012, 255, 23–29. [Google Scholar] [CrossRef]
- Ennis, W.J.; Foremann, P.; Mozen, N.; Massey, J.; Conner-Kerr, T.; Meneses, P. Ultrasound therapy for recalcitrant diabetic foot ulcers: Results of a randomized, double-blind, controlled, multicenter study. Ostomy Wound Manag. 2005, 51, 24–39. [Google Scholar]
- Kloth, L.C. Electrical Stimulation for Wound Healing: A Review of Evidence from In Vitro Studies, Animal Experiments, and Clinical Trials. Int. J. Low. Extrem. Wounds 2005, 4, 23–44. [Google Scholar] [CrossRef] [PubMed]
- El-Sabbagh, A.H. Negative pressure wound therapy: An update. Chin. J. Traumatol. 2017, 20, 103–107. [Google Scholar] [CrossRef]
- Wiegand, C.; White, R. Microdeformation in wound healing. Wound Repair Regen. 2013, 21, 793–799. [Google Scholar] [CrossRef]
- Nuutila, K.; Siltanen, A.; Peura, M.; Harjula, A.; Nieminen, T.; Vuola, J.; Kankuri, E.; Aarnio, P. Gene expression profiling of negative-pressure-treated skin graft donor site wounds. Burns 2013, 39, 687–693. [Google Scholar] [CrossRef] [PubMed]
- McNulty, A.K.; Schmidt, M.; Feeley, T.; Kieswetter, K. Effects of negative pressure wound therapy on fibroblast viability, chemotactic signaling, and proliferation in a provisional wound (fibrin) matrix. Wound Repair Regen. 2007, 15, 838–846. [Google Scholar] [CrossRef] [PubMed]
- Greene, A.K.; Puder, M.; Roy, R.; Arsenault, D.; Kwei, S.; Moses, M.; Orgill, D. Microdeformational wound therapy: Effects on angiogenesis and matrix metalloproteinases in chronic wounds of 3 debilitated patients. Ann. Plast. Surg. 2006, 56, 418–422. [Google Scholar] [CrossRef]
- Lu, F.; Ogawa, R.; Nguyen, D.T.; Chen, B.; Guo, D.; Helm, D.L.; Zhan, Q.; Murphy, G.F.; Orgill, D.P. Microdeformation of Three-Dimensional Cultured Fibroblasts Induces Gene Expression and Morphological Changes. Ann. Plast. Surg. 2011, 66, 296–300. [Google Scholar] [CrossRef]
- Junker, J.P.; Kamel, R.A.; Caterson, E.; Eriksson, E.; Nuutila, K.; Patil, P.S.; Fathollahipour, S.; Inmann, A.; Pant, A.; Amini, R.; et al. Clinical Impact Upon Wound Healing and Inflammation in Moist, Wet, and Dry Environments. Adv. Wound Care 2013, 2, 348–356. [Google Scholar] [CrossRef]
- Walmsley, G.G.; Maan, Z.N.; Wong, V.W.; Duscher, D.; Hu, M.S.; Zielins, E.R.; Wearda, T.; Muhonen, E.; McArdle, A.; Tevlin, R.; et al. Scarless wound healing: Chasing the holy grail. Plast. Reconstr. Surg. 2015, 135, 907–917. [Google Scholar] [CrossRef]
- Ud-Din, S.; Volk, S.W.; Bayat, A. Regenerative healing, scar-free healing and scar formation across the species: Current concepts and future perspectives. Exp. Dermatol. 2014, 23, 615–619. [Google Scholar] [CrossRef] [PubMed]
- Nauta, A.; Gurtner, G.; Longaker, M. Wound healing and regenerative strategies. Oral Dis. 2011, 17, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Reinke, J.M.; Sorg, H. Wound repair and regeneration. Eur. Surg. Res. 2012, 49, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Holfeld, J.; Schaden, W.; Orgill, D.; Ogawa, R. Mechanotherapy: Revisiting physical therapy and recruiting mechanobiology for a new era in medicine. Trends Mol. Med. 2013, 19, 555–564. [Google Scholar] [CrossRef] [PubMed]
- Akaishi, S.; Akimoto, M.; Hyakusoku, H.; Ogawa, R. 142B: The relationship between keloid growth pattern and stretching tension-visual analysis using the finite element method. Ann Plast. Surg. 2008, 60, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Akaishi, S.; Ogawa, R.; Hyakusoku, H. Keloid and hypertrophic scar: Neurogenic inflammation hypotheses. Med. Hypotheses 2008, 71, 32–38. [Google Scholar] [CrossRef]
- Ogawa, R.; Okai, K.; Tokumura, F.; Mori, K.; Ohmori, Y.; Huang, C.; Hyakusoku, H.; Akaishi, S. The relationship between skin stretching/contraction and pathologic scarring: The important role of mechanical forces in keloid generation. Wound Repair Regen. 2012, 20, 149–157. [Google Scholar] [CrossRef]
- Ogawa, R. Mechanobiology of scarring. Wound Repair Regen. 2011, 19 (Suppl. S1), s2–s9. [Google Scholar] [CrossRef]
- Ogawa, R.; Akaishi, S.; Kuribayashi, S.; Miyashita, T. Keloids and Hypertrophic Scars Can Now Be Cured Completely: Recent Progress in Our Understanding of the Pathogenesis of Keloids and Hypertrophic Scars and the Most Promising Current Therapeutic Strategy. J. Nippon. Med. Sch. 2016, 83, 46–53. [Google Scholar] [CrossRef]
- Metcalfe, A.D.; Ferguson, M.W. Tissue engineering of replacement skin: The crossroads of biomaterials, wound healing, embryonic development, stem cells and regeneration. J. R. Soc. Interface 2006, 4, 413–437. [Google Scholar] [CrossRef]
- Rajendran, A.K.; Sankar, D.; Amirthalingam, S.; Kim, H.D.; Rangasamy, J.; Hwang, N.S. Trends in mechanobiology guided tissue engineering and tools to study cell-substrate interactions: A brief review. Biomater. Res. 2023, 27, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Butler, D.L.; Goldstein, S.A.; Guldberg, R.E.; Guo, X.E.; Kamm, R.; Laurencin, C.T.; McIntire, L.V.; Mow, V.C.; Nerem, R.M.; Sah, R.L.; et al. The Impact of Biomechanics in Tissue Engineering and Regenerative Medicine. Tissue Eng. Part B Rev. 2009, 15, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.-Y.; Mow, V.C.; Ateshian, G.A. The Role of Flow-Independent Viscoelasticity in the Biphasic Tensile and Compressive Responses of Articular Cartilage. J. Biomech. Eng. 2001, 123, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Walker, M.; Godin, M.; Harden, J.L.; Pelling, A.E. Time dependent stress relaxation and recovery in mechanically strained 3D microtissues. APL Bioeng. 2020, 4, 036107. [Google Scholar] [CrossRef] [PubMed]
- Onal, S.; Alkaisi, M.M.; Nock, V. Microdevice-based mechanical compression on living cells. iScience 2022, 25, 105518. [Google Scholar] [CrossRef]
- Ning, L.; Gil, C.J.; Hwang, B.; Theus, A.S.; Perez, L.; Tomov, M.L.; Bauser-Heaton, H.; Serpooshan, V. Biomechanical factors in three-dimensional tissue bioprinting. Appl. Phys. Rev. 2020, 7, 041319. [Google Scholar] [CrossRef]
- Kaner, D.; Friedmann, A. Soft tissue expansion with self-filling osmotic tissue expanders before vertical ridge augmentation: A proof of principle study. J. Clin. Periodontol. 2010, 38, 95–101. [Google Scholar] [CrossRef]
- Mertens, C.; Thiele, O.; Engel, M.; Seeberger, R.; Hoffmann, J.; Freier, K. The Use of Self-Inflating Soft Tissue Expanders Prior to Bone Augmentation of Atrophied Alveolar Ridges. Clin. Implant. Dent. Relat. Res. 2013, 17, 44–51. [Google Scholar] [CrossRef]
- Johnson, T.M.; Lowe, L.; Brown, M.D.; Sullivan, M.J.; Nelson, B.R. Histology and Physiology of Tissue Expansion. J. Dermatol. Surg. Oncol. 1993, 19, 1074–1078. [Google Scholar] [CrossRef]
- Rivera, R.; LoGiudice, J.; Gosain, A.K. Tissue expansion in pediatric patients. Clin. Plast. Surg. 2005, 32, 35–44. [Google Scholar] [CrossRef]
- Uijlenbroek, H.J.J.; Liu, Y.; He, J.F.; Visscher, C.; van Waas, M.A.J.; Wismeyer, D. Expanding soft tissue with Osmed® tissue expanders in the goat maxilla. Clin. Oral Implant. Res. 2010, 22, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Berge, S.J.; Wiese, K.G.; von Lindern, J.J.; Niederhagen, B.; Appel, T.; Reich, R.H. Tissue expansion using osmotically active hydrogel systems for direct closure of the donor defect of the radial forearm flap. Plast. Reconstr. Surg. 2001, 108, 1–5, discussion 6–7. [Google Scholar] [CrossRef] [PubMed]
- Ronert, M.A.M.; Hofheinz, H.M.; Manassa, E.M.; Asgarouladi, H.; Olbrisch, R.R.M. The Beginning of a New Era in Tissue Expansion: Self-Filling Osmotic Tissue Expander—Four-Year Clinical Experience. Plast. Reconstr. Surg. 2004, 114, 1025–1031. [Google Scholar] [CrossRef] [PubMed]
- Obdeijn, M.C.; Nicolai, J.-P.A.; Werker, P.M. The osmotic tissue expander: A three-year clinical experience. J. Plast. Reconstr. Aesthetic Surg. 2009, 62, 1219–1222. [Google Scholar] [CrossRef] [PubMed]
- Chummun, S.; Addison, P.; Stewart, K.J. The osmotic tissue expander: A 5-year experience. J. Plast. Reconstr. Aesthet. Surg. 2010, 63, 2128–2132. [Google Scholar] [CrossRef]
- Arneja, J.S.; Gosain, A.K. Giant congenital melanocytic nevi. Plast. Reconstr. Surg. 2009, 124 (Suppl. S1), 1e–13e. [Google Scholar] [CrossRef]
- Moustafa, D.; Blundell, A.R.; Hawryluk, E.B. Congenital melanocytic nevi. Curr. Opin. Pediatr. 2020, 32, 491–497. [Google Scholar] [CrossRef]
- Formby, P.; Flint, J.; Gordon, W.T.; Fleming, M.; Andersen, R.C. Use of a Continuous External Tissue Expander in the Conversion of a Type IIIB Fracture to a Type IIIA Fracture. Orthopedics 2013, 36, e249–e251. [Google Scholar] [CrossRef]
- Radovan, C. Breast Reconstruction after Mastectomy Using the Temporary Expander. Plast. Reconstr. Surg. 1982, 69, 207–208. [Google Scholar] [CrossRef]
- Argenta, L.C.M.; Marks, M.W.M.; Grabb, W.C.M. Selective Use of Serial Expansion in Breast Reconstruction. Ann. Plast. Surg. 1983, 11, 188–195. [Google Scholar] [CrossRef]
- Brobmann, G.F.; Huber, J. Effects of Different-Shaped Tissue Expanders on Transluminal Pressure, Oxygen Tension, Histopathologic Changes, and Skin Expansion in Pigs. Plast. Reconstr. Surg. 1985, 76, 731–745. [Google Scholar] [CrossRef] [PubMed]
- Van Rappard, J.H.; Molenaar, J.; Van Doorn, K.; Sonneveld, G.J.; Borghouts, J.M. Surface-area increase in tissue expansion. Plast. Reconstr. Surg. 1988, 82, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Pietila, J.P. Tissue expansion and skin circulation. Simultaneous monitoring by laser Doppler flowmetry and transcutaneous oximetry. Scand. J. Plast. Reconstr. Surg. Hand Surg. 1990, 24, 135–140. [Google Scholar]
- Van Damme, P.A.; Heidbüchel, K.L.; Kuijpers-Jagtman, A.-M.; Maltha, J.C.; Freihofer, H.P.M. Cranio-maxillo-facial tissue expansion, experimentally based or clinically empiric? A review of the literature. J. Cranio Maxillofac. Surg. 1992, 20, 61–69. [Google Scholar] [CrossRef]
- Austad, E.D.; Rose, G.L. A self-inflating tissue expander. Plast. Reconstr. Surg. 1982, 70, 588–594. [Google Scholar] [CrossRef] [PubMed]
- Wiese, K. Osmotically induced tissue expansion with hydrogels: A new dimension in tissue expansion? A preliminary report. J. Cranio-Maxillofac. Surg. 1993, 21, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Wiese, K.G.; Vogel, M.; Guthoff, R.; Gundlach, K.K. Treatment of congenital anophthalmos with self-inflating polymer expanders: A new method. J. Cranio-Maxillofac. Surg. 1999, 27, 72–76. [Google Scholar] [CrossRef]
- Wiese, K.G.; Heinemann, D.E.H.; Ostermeier, D.; Peters, J.H. Biomaterial properties and biocompatibility in cell culture of a novel self-inflating hydrogel tissue expander. J. Biomed. Mater. Res. 2000, 54, 179–188. [Google Scholar] [CrossRef]
- Hoffmann, J.F. Tissue expansion in the head and neck. Facial Plast. Surg. Clin. N. Am. 2005, 13, 315–324, vii. [Google Scholar] [CrossRef]
- Downes, R.; Lavin, M.; Collin, R. Hydrophilic expanders for the congenital anophthalmic socket. Adv. Ophthalmic Plast. Reconstr. Surg. 1992, 9, 57–61. [Google Scholar]
- Bell, C.L.; Peppas, N.A. Water, solute and protein diffusion in physiologically responsive hydrogels of poly(methacrylic acid-g-ethylene glycol). Biomaterials 1996, 17, 1203–1218. [Google Scholar] [CrossRef] [PubMed]
- Varga, J.; Janovak, L.; Varga, E.; Eros, G.; Dekany, I.; Kemeny, L. Acrylamide, Acrylic Acid and N-Isopropylacrylamide Hydrogels as Osmotic Tissue Expanders. Ski. Pharmacol. Physiol. 2009, 22, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Freeman, F.; Browe, D.; Nulty, J.; Von Euw, S.; Grayson, W.; Kelly, D. Biofabrication of multiscale bone extracellular matrix scaffolds for bone tissue engineering. Eur. Cells Mater. 2019, 38, 168–187. [Google Scholar] [CrossRef] [PubMed]
- Mikos, A.G.; Thorsen, A.J.; Czerwonka, L.A.; Bao, Y.; Langer, R.; Winslow, D.N.; Vacanti, J.P. Preparation and characterization of poly(l-lactic acid) foams. Polymers 1994, 35, 1068–1077. [Google Scholar] [CrossRef]
- Haugen, H.; Ried, V.; Brunner, M.; Will, J.; Wintermantel, E. Water as foaming agent for open cell polyurethane structures. J. Mater. Sci. Mater. Med. 2004, 15, 343–346. [Google Scholar] [CrossRef]
- Parks, K.L.; Beckman, E.J. Generation of microcellular polyurethane foams via polymerization in carbon dioxide. II: Foam formation and characterization. Polym. Eng. Sci. 1996, 36, 2417–2431. [Google Scholar] [CrossRef]
- Lee, K.-W.D.; Chan, P.K.; Feng, X. Morphology development and characterization of the phase-separated structure resulting from the thermal-induced phase separation phenomenon in polymer solutions under a temperature gradient. Chem. Eng. Sci. 2004, 59, 1491–1504. [Google Scholar] [CrossRef]
- Thomson, R.C.; Wake, M.C.; Yaszemski, M.J.; Mikos, A.G. Biodegradable polymer scaffolds to regenerate organs. Adv. Polym. Sci. 1995, 122, 245–274. [Google Scholar] [CrossRef]
- Liapis, A.; Bruttini, R. A theory for the primary and secondary drying stages of the freeze-drying of pharmaceutical crystalline and amorphous solutes: Comparison between experimental data and theory. Sep. Technol. 1994, 4, 144–155. [Google Scholar] [CrossRef]
- Pikal, M.; Shah, S.; Roy, M.; Putman, R. The secondary drying stage of freeze drying: Drying kinetics as a function of temperature and chamber pressure. Int. J. Pharm. 1990, 60, 203–207. [Google Scholar] [CrossRef]
- Vergnol, G.; Ginsac, N.; Rivory, P.; Meille, S.; Chenal, J.M.; Balvay, S.; Chevalier, J.; Hartmann, D.J. In vitro and in vivo evaluation of a polylactic acid-bioactive glass composite for bone fixation devices. J. Biomed. Mater. Res. B 2016, 104, 180–191. [Google Scholar] [CrossRef] [PubMed]
- Del Bakhshayesh, A.R.; Annabi, N.; Khalilov, R.; Akbarzadeh, A.; Samiei, M.; Alizadeh, E.; Alizadeh-Ghodsi, M.; Davaran, S.; Montaseri, A. Recent advances on biomedical applications of scaffolds in wound healing and dermal tissue engineering. Artif. Cells Nanomed. Biotechnol. 2018, 46, 691–705. [Google Scholar] [CrossRef] [PubMed]
- Bracaglia, L.G.; Smith, B.T.; Watson, E.; Arumugasaamy, N.; Mikos, A.G.; Fisher, J.P. 3D printing for the design and fabrication of polymer-based gradient scaffolds. Acta Biomater. 2017, 56, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Nyberg, E.L.; Farris, A.L.; Hung, B.P.; Dias, M.; Garcia, J.R.; Dorafshar, A.H.; Grayson, W.L. 3D-Printing Technologies for Craniofacial Rehabilitation, Reconstruction, and Regeneration. Ann. Biomed. Eng. 2016, 45, 45–57. [Google Scholar] [CrossRef]
- Lee, M.J.; Kim, S.E.; Park, J.; Ahn, G.Y.; Yun, T.H.; Choi, I.; Kim, H.; Choi, S. Curcumin-loaded biodegradable polyurethane scaffolds modified with gelatin using 3D printing technology for cartilage tissue engineering. Polym. Adv. Technol. 2019, 30, 3083–3090. [Google Scholar] [CrossRef]
- Wang, Y.; Kim, H.-J.; Vunjak-Novakovic, G.; Kaplan, D.L. Stem cell-based tissue engineering with silk biomaterials. Biomaterials 2006, 27, 6064–6082. [Google Scholar] [CrossRef]
- Rising, A.; Nimmervoll, H.; Grip, S.; Fernandez-Arias, A.; Storckenfeldt, E.; Knight, D.P.; Vollrath, F.; Engström, W. Spider Silk Proteins—Mechanical Property and Gene Sequence. Zool. Sci. 2005, 22, 273–281. [Google Scholar] [CrossRef]
- Foo, C.W.P.; Kaplan, D.L. Genetic engineering of fibrous proteins: Spider dragline silk and collagen. Adv. Drug Deliv. Rev. 2002, 54, 1131–1143. [Google Scholar] [CrossRef]
- Vollrath, F.; Knight, D.P. Liquid crystalline spinning of spider silk. Nature 2001, 410, 541–548. [Google Scholar] [CrossRef]
- Gosline, J.M.; Guerette, P.A.; Ortlepp, C.S.; Savage, K.N. The mechanical design of spider silks: From fibroin sequence to mechanical function. J. Exp. Biol. 1999, 202 Pt 23, 3295–3303. [Google Scholar] [CrossRef]
- Jin, H.-J.; Kaplan, D.L. Mechanism of silk processing in insects and spiders. Nature 2003, 424, 1057–1061. [Google Scholar] [CrossRef] [PubMed]
- Lazaris, A.; Arcidiacono, S.; Huang, Y.; Zhou, J.F.; Duguay, F.; Chretien, N.; Welhs, E.A.; Soares, J.W.; Karatzas, C.N. High-toughness Spider Silk Fibers Spun from Soluble Recombinant Silk Produced in Mammalian Cells. Science 2002, 295, 472–476. [Google Scholar] [CrossRef] [PubMed]
- Winkler, S.; Kaplan, D.L. Molecular biology of spider silk. Rev. Mol. Biotechnol. 2000, 74, 85–93. [Google Scholar] [CrossRef]
- Bini, E.; Knight, D.P.; Kaplan, D.L. Mapping Domain Structures in Silks from Insects and Spiders Related to Protein Assembly. J. Mol. Biol. 2003, 335, 27–40. [Google Scholar] [CrossRef]
- Simmons, A.H.; Michal, C.A.; Jelinski, L.W. Molecular Orientation and Two-Component Nature of the Crystalline Fraction of Spider Dragline Silk. Science 1996, 271, 84–87. [Google Scholar] [CrossRef] [PubMed]
- Prince, J.T.; McGrath, K.P.; DiGirolamo, C.M.; Kaplan, D.L. Construction, Cloning, and Expression of Synthetic Genes Encoding Spider Dragline Silk. Biochemistry 1995, 34, 10879–10885. [Google Scholar] [CrossRef] [PubMed]
- Gotoh, Y.; Tsukada, M.; Minoura, N. Effect of the chemical modification of the arginyl residue in Bombyx mori silk fibroin on the attachment and growth of fibroblast cells. J. Biomed. Mater. Res. 1998, 39, 351–357. [Google Scholar] [CrossRef]
- Inouye, K.; Kurokawa, M.; Nishikawa, S.; Tsukada, M. Use of Bombyx mori silk fibroin as a substratum for cultivation of animal cells. J. Biochem. Biophys. Methods 1998, 37, 159–164. [Google Scholar] [CrossRef]
- Sofia, S.; McCarthy, M.B.; Gronowicz, G.; Kaplan, D.L. Functionalized silk-based biomaterials for bone formation. J. Biomed. Mater. Res. 2000, 54, 139–148. [Google Scholar] [CrossRef]
- Chen, J.; Altman, G.H.; Karageorgiou, V.; Horan, R.; Collette, A.; Volloch, V.; Colabro, T.; Kaplan, D.L. Human bone marrow stromal cell and ligament fibroblast responses on RGD-modified silk fibers. J. Biomed. Mater. Res. A 2003, 67, 559–570. [Google Scholar] [CrossRef]
- Yang, M. Silk-based biomaterials. Microsc. Res. Tech. 2017, 80, 321–330. [Google Scholar] [CrossRef]
- Santin, M.; Motta, A.; Freddi, G.; Cannas, M. In vitro evaluation of the inflammatory potential of the silk fibroin. J. Biomed. Mater. Res. 1999, 46, 382–389. [Google Scholar] [CrossRef]
- Sugihara, A.; Sugiura, K.; Morita, H.; Ninagawa, T.; Tubouchi, K.; Tobe, R.; Izumiya, M.; Horio, T.; Abraham, N.G.; Ikehara, S. Promotive effects of a silk film on epidermal recovery from full-thickness skin wounds. Proc. Soc. Exp. Biol. Med. 2000, 225, 58–64. [Google Scholar] [CrossRef]
- Meinel, L.; Hofmann, S.; Karageorgiou, V.; Kirker-Head, C.; McCool, J.; Gronowicz, G.; Zichner, L.; Langer, R.; Vunjak-Novakovic, G.; Kaplan, D.L. The inflammatory responses to silk films in vitro and in vivo. Biomaterials 2005, 26, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Minoura, N.; Tsukada, M.; Nagura, M. Physico-chemical properties of silk fibroin membrane as a biomaterial. Biomaterials 1990, 11, 430–434. [Google Scholar] [CrossRef] [PubMed]
- Chiarini, A.; Petrini, P.; Bozzini, S.; Dal Pra, I.; Armato, U. Silk fibroin/poly(carbonate)-urethane as a substrate for cell growth: In vitro interactions with human cells. Biomaterials 2003, 24, 789–799. [Google Scholar] [CrossRef] [PubMed]
- Yeo, J.H.; Lee, K.G.; Kim, H.C.; Oh, Y.L.; Kim, A.-J.; Kim, S.Y. The Effects of PVA/Chitosan/Fibroin (PCF)-Blended Spongy Sheets on Wound Healing in Rats. Biol. Pharm. Bull. 2000, 23, 1220–1223. [Google Scholar] [CrossRef] [PubMed]
- Katti, D.S.; Robinson, K.W.; Ko, F.K.; Laurencin, C.T. Bioresorbable nanofiber-based systems for wound healing and drug delivery: Optimization of fabrication parameters. J. Biomed. Mater. Res. B Appl. Biomater. 2004, 70, 286–296. [Google Scholar] [CrossRef]
- Chen, J.-P.; Chen, S.-H.; Lai, G.-J. Preparation and characterization of biomimetic silk fibroin/chitosan composite nanofibers by electrospinning for osteoblasts culture. Nanoscale Res. Lett. 2012, 7, 170. [Google Scholar] [CrossRef]
- Li, W.J.; Danielson, K.G.; Alexander, P.G.; Tuan, R.S. Biological response of chondrocytes cultured in three-dimensional nanofibrous poly(epsilon-caprolactone) scaffolds. J. Biomed. Mater. Res. A 2003, 67, 1105–1114. [Google Scholar] [CrossRef]
- Yoshimoto, H.; Shin, Y.; Terai, H.; Vacanti, J. A biodegradable nanofiber scaffold by electrospinning and its potential for bone tissue engineering. Biomaterials 2003, 24, 2077–2082. [Google Scholar] [CrossRef] [PubMed]
- Dornish, M.; Kaplan, D.; Skaugrud, O. Standards and guidelines for biopolymers in tissue-engineered medical products: ASTM alginate and chitosan standard guides. American Society for Testing and Materials. Ann. N. Y. Acad. Sci. 2001, 944, 388–397. [Google Scholar] [CrossRef] [PubMed]
- VandeVord, P.J.; Matthew, H.W.; DeSilva, S.P.; Mayton, L.; Wu, B.; Wooley, P.H. Evaluation of the biocompatibility of a chitosan scaffold in mice. J. Biomed. Mater. Res. 2002, 59, 585–590. [Google Scholar] [CrossRef]
- Madihally, S.V.; Flake, A.W.; Matthew, H.W.T. Maintenance of CD34 Expression During Proliferation of CD34+ Cord Blood Cells on Glycosaminoglycan Surfaces. Stem Cells 1999, 17, 295–305. [Google Scholar] [CrossRef]
- Mo, X.; Xu, C.; Kotaki, M.; Ramakrishna, S. Electrospun P(LLA-CL) nanofiber: A biomimetic extracellular matrix for smooth muscle cell and endothelial cell proliferation. Biomaterials 2004, 25, 1883–1890. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Inai, R.; Kotaki, M.; Ramakrishna, S. Aligned biodegradable nanofibrous structure: A potential scaffold for blood vessel engineering. Biomaterials 2003, 25, 877–886. [Google Scholar] [CrossRef]
- Khil, M.-S.; Cha, D.-I.; Kim, H.-Y.; Kim, I.-S.; Bhattarai, N. Electrospun nanofibrous polyurethane membrane as wound dressing. J. Biomed. Mater. Res. B Appl. Biomater. 2003, 67, 675–679. [Google Scholar] [CrossRef]
- Şenel, S.; McClure, S.J. Potential applications of chitosan in veterinary medicine. Adv. Drug Deliv. Rev. 2004, 56, 1467–1480. [Google Scholar] [CrossRef]
- Chow, K.S.; Khor, E. Novel Fabrication of Open-Pore Chitin Matrixes. Biomacromolecules 2000, 1, 61–67. [Google Scholar] [CrossRef]
- Shin, M.; Yoshimoto, H.; Vacanti, J.P. In Vivo Bone Tissue Engineering Using Mesenchymal Stem Cells on a Novel Electrospun Nanofibrous Scaffold. Tissue Eng. 2004, 10, 33–41. [Google Scholar] [CrossRef]
- Shin, M.; Ishii, O.; Sueda, T.; Vacanti, J. Contractile cardiac grafts using a novel nanofibrous mesh. Biomaterials 2004, 25, 3717–3723. [Google Scholar] [CrossRef] [PubMed]
- Taravel, M.; Domard, A. Collagen and its interaction with chitosan: II. Influence of the physicochemical characteristics of collagen. Biomaterials 1995, 16, 865–871. [Google Scholar] [CrossRef] [PubMed]
- Taravel, M.N.; Domard, A. Collagen and its interactions with chitosan, III some biological and mechanical properties. Biomaterials 1996, 17, 451–455. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.-N.; Chung, S.-H.; Yoo, G.; Ko, S.-W. Water-soluble chitin as a wound healing accelerator. Biomaterials 1999, 20, 2139–2145. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Wang, H.; He, B.; Chen, J. A preliminary in vitro study on the fabrication and tissue engineering applications of a novel chitosan bilayer material as a scaffold of human neofetal dermal fibroblasts. Biomaterials 2000, 22, 331–336. [Google Scholar] [CrossRef]
- Wang, L.; Khor, E.; Wee, A.; Lim, L.Y. Chitosan-alginate PEC membrane as a wound dressing: Assessment of incisional wound healing. J. Biomed. Mater. Res. 2002, 63, 610–618. [Google Scholar] [CrossRef]
- Fratzl, P.; Misof, K.; Zizak, I.; Rapp, G.; Amenitsch, H.; Bernstorff, S. Fibrillar structure and mechanical properties of collagen. J. Struct. Biol. 1998, 122, 119–122. [Google Scholar] [CrossRef]
- Franchi, M.; Trirè, A.; Quaranta, M.; Orsini, E.; Ottani, V. Collagen Structure of Tendon Relates to Function. Sci. World J. 2007, 7, 404–420. [Google Scholar] [CrossRef]
- Hofmann, H.; Fietzek, P.; Kühn, K. The role of polar and hydrophobic interactions for the molecular packing of type I collagen: A three-dimensional evaluation of the amino acid sequence. J. Mol. Biol. 1978, 125, 137–165. [Google Scholar] [CrossRef]
- Matthews, J.A.; Wnek, G.E.; Simpson, D.G.; Bowlin, G.L. Electrospinning of Collagen Nanofibers. Biomacromolecules 2002, 3, 232–238. [Google Scholar] [CrossRef]
- Gelse, K.; Poschl, E.; Aigner, T. Collagens—Structure, function, and biosynthesis. Adv. Drug Deliv. Rev. 2003, 55, 1531–1546. [Google Scholar] [CrossRef] [PubMed]
- Abdollahiyan, P.; Oroojalian, F.; Hejazi, M.; de la Guardia, M.; Mokhtarzadeh, A. Nanotechnology, and scaffold implantation for the effective repair of injured organs: An overview on hard tissue engineering. J. Control. Release 2021, 333, 391–417. [Google Scholar] [CrossRef] [PubMed]
- Hulmes, D.J.S.; Miller, A. Molecular packing in collagen. Nature 1981, 293, 239–240. [Google Scholar] [CrossRef] [PubMed]
- Mithieux, S.M.; Weiss, A.S. Elastin. Adv. Protein Chem. 2005, 70, 437–461. [Google Scholar]
- Fazio, M.J.; Mattei, M.G.; Passage, E.; Chu, M.L.; Black, D.; Solomon, E.; Davidson, J.M.; Uitto, J. Human elastin gene: New evidence for localization to the long arm of chromosome 7. Am. J. Hum. Genet. 1991, 48, 696–703. [Google Scholar]
- Rosenbloom, J.; Abrams, W.R.; Mecham, R. Extracellular matrix 4: The elastic fiber. FASEB J. 1993, 7, 1208–1218. [Google Scholar] [CrossRef]
- Muiznieks, L.D.; Jensen, S.A.; Weiss, A.S. Structural changes and facilitated association of tropoelastin. Arch. Biochem. Biophys. 2003, 410, 317–323. [Google Scholar] [CrossRef]
- Sandberg, L.B.; Soskel, N.T.; Leslie, J.G. Elastin structure, biosynthesis, and relation to disease states. N. Engl. J. Med. 1981, 304, 566–579. [Google Scholar] [CrossRef]
- Uitto, V.-J.; Larjava, H. Extracellular Matrix Molecules and their Receptors: An Overview with Special Emphasis on Periodontal Tissues. Crit. Rev. Oral Biol. Med. 1991, 2, 323–354. [Google Scholar] [CrossRef]
- Rnjak, J.; Wise, S.G.; Mithieux, S.M.; Weiss, A.S. Severe Burn Injuries and the Role of Elastin in the Design of Dermal Substitutes. Tissue Eng. Part B Rev. 2011, 17, 81–91. [Google Scholar] [CrossRef]
- Ramirez, F. Pathophysiology of the microfibril/elastic fiber system: Introduction. Matrix Biol. 2000, 19, 455–456. [Google Scholar] [CrossRef] [PubMed]
- Nouri, K.; Jimenez, G.P.; Harrison-Balestra, C.; Elgart, G.W. 585-nm pulsed dye laser in the treatment of surgical scars starting on the suture removal day. Dermatol. Surg. 2003, 29, 65–73; discussion 73. [Google Scholar] [PubMed]
- Powell, J.T.; Vine, N.; Crossman, M. On the accumulation of d-aspartate in elastin and other proteins of the ageing aorta. Atherosclerosis 1992, 97, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Hinek, A.; Wang, Y.; Liu, K.; Mitts, T.F.; Jimenez, F. Proteolytic digest derived from bovine Ligamentum Nuchae stimulates deposition of new elastin-enriched matrix in cultures and transplants of human dermal fibroblasts. J. Dermatol. Sci. 2005, 39, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Carlisle, E.M. Silicon as a trace nutrient. Sci. Total Environ. 1988, 73, 95–106. [Google Scholar] [CrossRef]
- Wei, S.; Ma, J.-X.; Xu, L.; Gu, X.-S.; Ma, X.-L. Biodegradable materials for bone defect repair. Mil. Med. Res. 2020, 7, 1–25. [Google Scholar] [CrossRef]
- Sarker, B.; Lyer, S.; Arkudas, A.; Boccaccini, A.R. Collagen/silica nanocomposites and hybrids for bone tissue engineering. Nanotechnol. Rev. 2013, 2, 427–447. [Google Scholar] [CrossRef]
- Dong, C.; Lv, Y. Application of Collagen Scaffold in Tissue Engineering: Recent Advances and New Perspectives. Polymers 2016, 8, 42. [Google Scholar] [CrossRef]
- Khanna, A.; Zamani, M.; Huang, N.F. Extracellular Matrix-Based Biomaterials for Cardiovascular Tissue Engineering. J. Cardiovasc. Dev. Dis. 2021, 8, 137. [Google Scholar] [CrossRef]
- Szurkowska, K.; Kolmas, J. Hydroxyapatites enriched in silicon—Bioceramic materials for biomedical and pharmaceutical applications. Prog. Nat. Sci. Mater. 2017, 27, 401–409. [Google Scholar] [CrossRef]
- Al-Harbi, N.; Mohammed, H.; Al-Hadeethi, Y.; Bakry, A.S.; Umar, A.; Hussein, M.A.; Abbassy, M.A.; Vaidya, K.G.; Al Berakdar, G.; Mkawi, E.M.; et al. Silica-Based Bioactive Glasses and Their Applications in Hard Tissue Regeneration: A Review. Pharmaceuticals 2021, 14, 75. [Google Scholar] [CrossRef] [PubMed]
- Hao, S.; Wang, M.; Yin, Z.; Jing, Y.; Bai, L.; Su, J. Microenvironment-targeted strategy steers advanced bone regeneration. Mater. Today Bio 2023, 22, 100741. [Google Scholar] [CrossRef]
- Gao, C.; Peng, S.; Feng, P.; Shuai, C. Bone biomaterials and interactions with stem cells. Bone Res. 2017, 5, 17059. [Google Scholar] [CrossRef] [PubMed]
- Tian, B.; Liu, Y. Antibacterial applications and safety issues of silica-based materials: A review. Int. J. Appl. Ceram. Technol. 2020, 18, 289–301. [Google Scholar] [CrossRef]
- Song, R.; Murphy, M.; Li, C.; Ting, K.; Soo, C.; Zheng, Z. Current development of biodegradable polymeric materials for biomedical applications. Drug Des. Dev. Ther. 2018, 12, 3117–3145. [Google Scholar] [CrossRef]
- Labet, M.; Thielemans, W. Synthesis of polycaprolactone: A review. Chem. Soc. Rev. 2009, 38, 3484–3504. [Google Scholar] [CrossRef]
- Kweon, H.; Yoo, M.K.; Park, I.K.; Kim, T.H.; Lee, H.C.; Lee, H.S.; Oh, J.S.; Akaike, T.; Cho, C.S. A novel degradable polycaprolactone networks for tissue engineering. Biomaterials 2003, 24, 801–808. [Google Scholar] [CrossRef]
- Woodward, S.C.; Brewer, P.S.; Moatamed, F.; Schindler, A.; Pitt, C.G. The intracellular degradation of poly(epsilon-caprolactone). J. Biomed. Mater. Res. 1985, 19, 437–444. [Google Scholar] [CrossRef]
- Pitt, G.G.; Gratzl, M.M.; Kimmel, G.L.; Surles, J.; Sohindler, A. Aliphatic polyesters II. The degradation of poly (DL-lactide), poly (ε-caprolactone), and their copolymers in vivo. Biomaterials 1981, 2, 215–220. [Google Scholar] [CrossRef]
- Sinha, V.R.; Bansal, K.; Kaushik, R.; Kumria, R.; Trehan, A. Poly-epsilon-caprolactone microspheres and nanospheres: An overview. Int. J. Pharm. 2004, 278, 1–23. [Google Scholar] [CrossRef]
- Coombes, A.; Rizzi, S.; Williamson, M.; Barralet, J.; Downes, S.; Wallace, W. Precipitation casting of polycaprolactone for applications in tissue engineering and drug delivery. Biomaterials 2003, 25, 315–325. [Google Scholar] [CrossRef] [PubMed]
- Uhrich, K.E.; Cannizzaro, S.M.; Langer, R.S.; Shakesheff, K.M. Polymeric Systems for Controlled Drug Release. Chem. Rev. 1999, 99, 3181–3198. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.S. Synthesis, Characterization, Biodegradation, and Drug Delivery Application of Biodegradable Lactic/Glycolic Acid Polymers: Part III. Drug Delivery Application. Artif. Cells Blood Substit. Biotechnol. 2004, 32, 575–591. [Google Scholar] [CrossRef] [PubMed]
- Makadia, H.K.; Siegel, S.J. Poly lactic-co-glycolic acid (PLGA) As biodegradable controlled drug delivery carrier. Polymers 2011, 3, 1377–1397. [Google Scholar] [CrossRef]
- Shirazi, R.N.; Aldabbagh, F.; Erxleben, A.; Rochev, Y.; McHugh, P. Nanomechanical properties of poly(lactic-co-glycolic) acid film during degradation. Acta Biomater. 2014, 10, 4695–4703. [Google Scholar] [CrossRef]
- Dzobo, K.; Thomford, N.E.; Senthebane, D.A.; Shipanga, H.; Rowe, A.; Dandara, C.; Pillay, M.; Motaung, K.S.C.M. Advances in regenerative medicine and tissue engineering: Innovation and transformation of medicine. Stem Cells Int. 2018, 2018, 2495848. [Google Scholar] [CrossRef]
- Han, F.; Wang, J.; Ding, L.; Hu, Y.; Li, W.; Yuan, Z.; Guo, Q.; Zhu, C.; Yu, L.; Wang, H.; et al. Tissue Engineering and Regenerative Medicine: Achievements, Future, and Sustainability in Asia. Front. Bioeng. Biotechnol. 2020, 8, 83. [Google Scholar] [CrossRef]
- Witkowska, D.; Rowińska-Żyrek, M. Biophysical approaches for the study of metal-protein interactions. J. Inorg. Biochem. 2019, 199, 110783. [Google Scholar] [CrossRef]
- Churchfield, L.A.; Tezcan, F.A. Design and Construction of Functional Supramolecular Metalloprotein Assemblies. Acc. Chem. Res. 2019, 52, 345–355. [Google Scholar] [CrossRef]
- Nastri, F.; D’alonzo, D.; Leone, L.; Zambrano, G.; Pavone, V.; Lombardi, A. Engineering Metalloprotein Functions in Designed and Native Scaffolds. Trends Biochem. Sci. 2019, 44, 1022–1040. [Google Scholar] [CrossRef]
- Lin, P.-H.; Sermersheim, M.; Li, H.; Lee, P.H.U.; Steinberg, S.M.; Ma, J. Zinc in Wound Healing Modulation. Nutrients 2017, 10, 16. [Google Scholar] [CrossRef] [PubMed]
- Tenaud, I.; Sainte-Marie, I.; Jumbou, O.; Litoux, P.; Dreno, B. In vitro modulation of keratinocyte wound healing integrins by zinc, copper and manganese. Brit. J. Dermatol. 1999, 140, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Chen, L.; Yuan, Q.; Gu, Z.; Wu, J. Tofu-Based Hybrid Hydrogels with Antioxidant and Low Immunogenicity Activity for Enhanced Wound Healing. J. Biomed. Nanotechnol. 2019, 15, 1371–1383. [Google Scholar] [CrossRef] [PubMed]
- Coelho, T.S.; Halicki, P.C.B.; Silva, L.; Vicenti, J.R.d.M.; Gonçalves, B.L.; da Silva, P.E.A.; Ramos, D.F. Metal-based antimicrobial strategies against intramacrophage Mycobacterium tuberculosis. Lett. Appl. Microbiol. 2020, 71, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Zhang, E.; Zhao, X.; Hu, J.; Wang, R.; Fu, S.; Qin, G. Antibacterial metals and alloys for potential biomedical implants. Bioact. Mater. 2021, 6, 2569–2612. [Google Scholar] [CrossRef]
- Eming, S.A.; Martin, P.; Tomic-Canic, M. Wound repair and regeneration: Mechanisms, signaling, and translation. Sci. Transl. Med. 2014, 6, 265sr6. [Google Scholar] [CrossRef]
- Ashtiani, R.E.; Alam, M.; Tavakolizadeh, S.; Abbasi, K. The Role of Biomaterials and Biocompatible Materials in Implant-Supported Dental Prosthesis. Evid. Based Complement. Altern. Med. 2021, 2021, 3349433. [Google Scholar] [CrossRef]
- Long, M.; Rack, H.J. Titanium alloys in total joint replacement—A materials science perspective. Biomaterials 1998, 19, 1621–1639. [Google Scholar] [CrossRef]
- Li, Y.; Jahr, H.; Lietaert, K.; Pavanram, P.; Yilmaz, A.; Fockaert, L.I.; Leeflang, M.A.; Pouran, B.; Gonzalez-Garcia, Y.; Weinans, H.; et al. Additively manufactured biodegradable porous iron. Acta Biomater. 2018, 77, 380–393. [Google Scholar] [CrossRef]
- Wang, X.; Xu, S.; Zhou, S.; Xu, W.; Leary, M.; Choong, P.; Qian, M.; Brandt, M.; Xie, Y.M. Topological design and additive manufacturing of porous metals for bone scaffolds and orthopaedic implants: A review. Biomaterials 2016, 83, 127–141. [Google Scholar] [CrossRef]
- You, J.; Zhang, Y.; Zhou, Y. Strontium Functionalized in Biomaterials for Bone Tissue Engineering: A Prominent Role in Osteoimmunomodulation. Front. Bioeng. Biotechnol. 2022, 10, 928799. [Google Scholar] [CrossRef]
- Bulina, N.V.; Vinokurova, O.B.; Prosanov, I.Y.; Vorobyev, A.M.; Gerasimov, K.B.; Borodulina, I.A.; Pryadko, A.; Botvin, V.V.; Surmeneva, M.A.; Surmenev, R.A. Mechanochemical synthesis of strontium- and magnesium-substituted and cosubstituted hydroxyapatite powders for a variety of biomedical applications. Ceram. Int. 2022, 48, 35217–35226. [Google Scholar] [CrossRef]
- Iseri, L.T.; French, J.H. Magnesium: Nature’s physiologic calcium blocker. Am. Heart J. 1984, 108, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Arora, K.; Beard, W.A.; Wilson, S.H.; Schlick, T. Critical role of magnesium ions in DNA polymerase beta’s closing and active site assembly. J. Am. Chem. Soc. 2004, 126, 8441–8453. [Google Scholar] [CrossRef] [PubMed]
- Panaghie, C.; Zegan, G.; Sodor, A.; Cimpoeșu, N.; Lohan, N.-M.; Istrate, B.; Roman, A.-M.; Ioanid, N. Analysis of Degradation Products of Biodegradable ZnMgY Alloy. Materials 2023, 16, 3092. [Google Scholar] [CrossRef] [PubMed]
- Wallach, S. Effects of magnesium on skeletal metabolism. Magnes. Trace Elem. 1989, 9, 1–14. [Google Scholar]
- Cowan, J. Structural and catalytic chemistry of magnesium-dependent enzymes. BioMetals 2002, 15, 225–235. [Google Scholar] [CrossRef]
- Sissi, C.; Palumbo, M. Effects of magnesium and related divalent metal ions in topoisomerase structure and function. Nucleic Acids Res. 2009, 37, 702–711. [Google Scholar] [CrossRef]
- Haftek, M.; Abdayem, R.; Guyonnet-Debersac, P. Skin Minerals: Key Roles of Inorganic Elements in Skin Physiological Functions. Int. J. Mol. Sci. 2022, 23, 6267. [Google Scholar] [CrossRef]
- Chandrasekaran, N.C.; Weir, C.; Alfraji, S.; Grice, J.; Roberts, M.S.; Barnard, R.T. Effects of magnesium deficiency—More than skin deep. Exp. Biol. Med. 2014, 239, 1280–1291. [Google Scholar] [CrossRef]
- Del Rosso, J.; Zeichner, J.; Alexis, A.; Cohen, D.; Berson, D. Understanding the Epidermal Barrier in Healthy and Compromised Skin: Clinically Relevant Information for the Dermatology Practitioner: Proceedings of an Expert Panel Roundtable Meeting. J. Clin. Aesthetic Dermatol. 2016, 9 (Suppl. S1), S2–S8. [Google Scholar]
- Denda, M.; Katagiri, C.; Hirao, T.; Maruyama, N.; Takahashi, M. Some magnesium salts and a mixture of magnesium and calcium salts accelerate skin barrier recovery. Arch. Dermatol. Res. 1999, 291, 560–563. [Google Scholar] [CrossRef] [PubMed]
- Denda, M. New strategies to improve skin barrier homeostasis. Adv. Drug Deliv. Rev. 2002, 54 (Suppl. S1), S123–S130. [Google Scholar] [CrossRef]
- Denda, M. Methodology to improve epidermal barrier homeostasis: How to accelerate the barrier recovery? Int. J. Cosmet. Sci. 2009, 31, 79–86. [Google Scholar] [CrossRef]
- Jahnen-Dechent, W.; Ketteler, M. Magnesium basics. Clin. Kidney J. 2012, 5 (Suppl. S1), i3–i14. [Google Scholar] [CrossRef]
- Njau, S.; Epivatianos, P.; Tsoukali-Papadopoulou, H.; Psaroulis, D.; Stratis, J. Magnesium, calcium and zinc fluctuations on skin induced injuries in correlation with time of induction. Forensic Sci. Int. 1991, 50, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Proksch, E.; Nissen, H.-P.; Bremgartner, M.; Urquhart, C. Bathing in a magnesium-rich Dead Sea salt solution improves skin barrier function, enhances skin hydration, and reduces inflammation in atopic dry skin. Int. J. Dermatol. 2005, 44, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Rude, R.K.; Adams, J.S.; Ryzen, E.; Endres, D.B.; Niimi, H.; Horst, R.L.; Haddad, J.G.; Singer, F.R. Low Serum Concentrations of 1,25-Dihydroxyvitamin D in Human Magnesium Deficiency. J. Clin. Endocrinol. Metab. 1985, 61, 933–940. [Google Scholar] [CrossRef] [PubMed]
- Sahota, O.; Mundey, M.K.; San, P.; Godber, I.M.; Hosking, D.J. Vitamin D insufficiency and the blunted PTH response in established osteoporosis: The role of magnesium deficiency. Osteoporos. Int. 2006, 17, 1013–1021. [Google Scholar] [CrossRef]
- Nie, X.; Sun, X.; Wang, C.; Yang, J. Effect of magnesium ions/Type I collagen promote the biological behavior of osteoblasts and its mechanism. Regen. Biomater. 2019, 7, 53–61. [Google Scholar] [CrossRef]
- Shigematsu, T.; Tajima, S.; Nishikawa, T.; Murad, S.; Pinnell, S.R.; Nishioka, I. Inhibition of collagen hydroxylation by lithospermic acid magnesium salt, a novel compound isolated from Salviae miltiorrhizae Radix. Biochim. Biophys. Acta (BBA) Gen. Subj. 1994, 1200, 79–83. [Google Scholar] [CrossRef]
- Müller, W.; Iffland, R.; Firsching, R. Relationship between magnesium and elastic fibres. Magnes. Res. 1993, 6, 215–222. [Google Scholar] [PubMed]
- Muller, W.; Firsching, R. Differentiation of Oxytalan Fibers from Elastic Fibers with Reagents for Detection of Magnesium. Ann. Anat. 1992, 174, 357–359. [Google Scholar] [CrossRef] [PubMed]
- Heinz, A. Elastases and elastokines: Elastin degradation and its significance in health and disease. Crit. Rev. Biochem. Mol. Biol. 2020, 55, 252–273. [Google Scholar] [CrossRef] [PubMed]
- Senni, K.; Foucault-Bertaud, A.; Godeau, G. Magnesium and connective tissue. Magnes. Res. 2003, 16, 70–74. [Google Scholar]
- Heinegård, D.; Wieslander, J.; Sheehan, J.; Paulsson, M.; Sommarin, Y. Separation and characterization of two populations of aggregating proteoglycans from cartilage. Biochem. J. 1985, 225, 95–106. [Google Scholar] [CrossRef]
- Yamaguchi, Y.; Mann, D.M.; Ruoslahti, E. Negative regulation of transforming growth factor-beta by the proteoglycan decorin. Nature 1990, 346, 281–284. [Google Scholar] [CrossRef]
- Nunes, A.M.; Minetti, C.A.; Remeta, D.P.; Baum, J. Magnesium Activates Microsecond Dynamics to Regulate Integrin-Collagen Recognition. Structure 2018, 26, 1080–1090.e5. [Google Scholar] [CrossRef]
- Harjunpää, H.; Asens, M.L.; Guenther, C.; Fagerholm, S.C. Cell Adhesion Molecules and Their Roles and Regulation in the Immune and Tumor Microenvironment. Front. Immunol. 2019, 10, 1078. [Google Scholar] [CrossRef]
- Danen, E.H.; Sonnenberg, A. Integrins in regulation of tissue development and function. J. Pathol. 2003, 200, 471–480. [Google Scholar] [CrossRef]
- Lange, T.S.; Bielinsky, A.K.; Kirchberg, K.; Bank, I.; Herrmann, K.; Krieg, T.; Scharffetter-Kochanek, K. Mg2+ and Ca2+ differentially regulate beta 1 integrin-mediated adhesion of dermal fibroblasts and keratinocytes to various extracellular matrix proteins. Exp. Cell Res. 1994, 214, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Lange, T.S.; Kirchberg, K.; Bielinsky, A.K.; Leuker, A.; Bank, I.; Ruzicka, T.; Scharffetter-Kochanek, K. Divalent cations (Mg2+, Ca2+) differentially influence the beta1 integrin-mediated migration of human fibroblasts and keratinocytes to different extracellular matrix proteins. Exp. Dermatol. 1995, 4, 130–137. [Google Scholar] [CrossRef]
- Stelling, M.P.; Motta, J.M.; Mashid, M.; Johnson, W.E.; Pavão, M.S.; Farrell, N.P. Metal ions and the extracellular matrix in tumor migration. FEBS J. 2019, 286, 2950–2964. [Google Scholar] [CrossRef]
- Antoniac, I.; Miculescu, M.; Păltânea, V.M.; Stere, A.; Quan, P.H.; Păltânea, G.; Robu, A.; Earar, K. Magnesium-Based Alloys Used in Orthopedic Surgery. Materials 2022, 15, 1148. [Google Scholar] [CrossRef]
- Brandt-Wunderlich, C.; Ruppelt, P.; Zumstein, P.; Schmidt, W.; Arbeiter, D.; Schmitz, K.-P.; Grabow, N. Mechanical behavior of in vivo degraded second generation resorbable magnesium scaffolds (RMS). J. Mech. Behav. Biomed. Mater. 2018, 91, 174–181. [Google Scholar] [CrossRef]
- Qin, Y.; Wen, P.; Guo, H.; Xia, D.; Zheng, Y.; Jauer, L.; Poprawe, R.; Voshage, M.; Schleifenbaum, J.H. Additive manufacturing of biodegradable metals: Current research status and future perspectives. Acta Biomater. 2019, 98, 3–22. [Google Scholar] [CrossRef] [PubMed]
- Amukarimi, S.; Mozafari, M. Biodegradable magnesium-based biomaterials: An overview of challenges and opportunities. Medcomm 2021, 2, 123–144. [Google Scholar] [CrossRef] [PubMed]
- Seetharaman, S.; Sankaranarayanan, D.; Gupta, M. Magnesium-Based Temporary Implants: Potential, Current Status, Applications, and Challenges. J. Funct. Biomater. 2023, 14, 324. [Google Scholar] [CrossRef]
- Kim, Y.-K.; Lee, K.-B.; Kim, S.-Y.; Bode, K.; Jang, Y.-S.; Kwon, T.-Y.; Jeon, M.H.; Lee, M.-H. Gas formation and biological effects of biodegradable magnesium in a preclinical and clinical observation. Sci. Technol. Adv. Mater. 2018, 19, 324–335. [Google Scholar] [CrossRef]
- Fiorentini, D.; Cappadone, C.; Farruggia, G.; Prata, C. Magnesium: Biochemistry, Nutrition, Detection, and Social Impact of Diseases Linked to Its Deficiency. Nutrients 2021, 13, 1136. [Google Scholar] [CrossRef]
- Swaminathan, R. Magnesium metabolism and its disorders. Clin. Biochem. Rev. 2003, 24, 47–66. [Google Scholar] [PubMed]
- Gonzalez, J.; Hou, R.Q.; Nidadavolu, E.P.; Willumeit-Römer, R.; Feyerabend, F. Magnesium degradation under physiological conditions—Best practice. Bioact. Mater. 2018, 3, 174–185. [Google Scholar] [CrossRef] [PubMed]
- Xin, Y.; Huo, K.; Tao, H.; Tang, G.; Chu, P.K. Influence of aggressive ions on the degradation behavior of biomedical magnesium alloy in physiological environment. Acta Biomater. 2008, 4, 2008–2015. [Google Scholar] [CrossRef] [PubMed]
- Törne, K.; Örnberg, A.; Weissenrieder, J. The influence of buffer system and biological fluids on the degradation of magnesium. J. Biomed. Mater. Res. Part B Appl. Biomater. 2016, 105, 1490–1502. [Google Scholar] [CrossRef]
- Kokubo, T.; Takadama, H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials 2006, 27, 2907–2915. [Google Scholar] [CrossRef]
- Oyane, A.; Kim, H.-M.; Furuya, T.; Kokubo, T.; Miyazaki, T.; Nakamura, T. Preparation and assessment of revised simulated body fluids. J. Biomed. Mater. Res. A 2003, 65, 188–195. [Google Scholar] [CrossRef]
- Gu, X.N.; Zheng, Y.F.; Chen, L.J. Influence of artificial biological fluid composition on the biocorrosion of potential orthopedic Mg-Ca, AZ31, AZ91 alloys. Biomed. Mater. 2009, 4, 065011. [Google Scholar] [CrossRef]
- Zhang, J.; Kong, N.; Shi, Y.; Niu, J.; Mao, L.; Li, H.; Xiong, M.; Yuan, G. Influence of proteins and cells on in vitro corrosion of Mg-Nd-Zn-Zr alloy. Corros. Sci. 2014, 85, 477–481. [Google Scholar] [CrossRef]
- Johnson, I.; Jiang, W.; Liu, H. The Effects of Serum Proteins on Magnesium Alloy Degradation in Vitro. Sci. Rep. 2017, 7, 14335. [Google Scholar] [CrossRef]
- Gao, Y.; Wang, L.; Li, L.; Gu, X.; Zhang, K.; Xia, J.; Fan, Y. Effect of stress on corrosion of high-purity magnesium in vitro and in vivo. Acta Biomater. 2018, 83, 477–486. [Google Scholar] [CrossRef]
- Liu, M.; Wang, J.; Zhu, S.; Zhang, Y.; Sun, Y.; Wang, L.; Guan, S. Corrosion fatigue of the extruded Mg-Zn-Y-Nd alloy in simulated body fluid. J. Magnes. Alloy 2020, 8, 231–240. [Google Scholar] [CrossRef]
- Bian, D.; Zhou, W.; Liu, Y.; Li, N.; Zheng, Y.; Sun, Z. Fatigue behaviors of HP-Mg, Mg-Ca and Mg-Zn-Ca biodegradable metals in air and simulated body fluid. Acta Biomater. 2016, 41, 351–360. [Google Scholar] [CrossRef]
- Zhen, Z.; Xi, T.-F.; Zheng, Y.-F. A review on in vitro corrosion performance test of biodegradable metallic materials. Trans. Nonferrous Met. Soc. China 2013, 23, 2283–2293. [Google Scholar] [CrossRef]
- Mei, D.; Lamaka, S.V.; Lu, X.; Zheludkevich, M.L. Selecting medium for corrosion testing of bioabsorbable magnesium and other metals—A critical review. Corros. Sci. 2020, 171, 108722. [Google Scholar] [CrossRef]
- Claes, L. Mechanical characterization of biodegradable implants. Clin. Mater. 1992, 10, 41–46. [Google Scholar] [CrossRef]
- Fard, M.G.; Sharifianjazi, F.; Kazemi, S.S.; Rostamani, H.; Bathaei, M.S. Laser-Based Additive Manufacturing of Magnesium Alloys for Bone Tissue Engineering Applications: From Chemistry to Clinic. J. Manuf. Mater. Process. 2022, 6, 158. [Google Scholar] [CrossRef]
- Sotomi, Y.; Onuma, Y.; Collet, C.; Tenekecioglu, E.; Virmani, R.; Kleiman, N.S.; Serruys, P.W. Bioresorbable Scaffold the Emerging Reality and Future Directions. Circ. Res. 2017, 120, 1341–1352. [Google Scholar] [CrossRef]
- Wang, J.L.; Xu, J.K.; Hopkins, C.; Chow, D.H.K.; Qin, L. Biodegradable Magnesium-Based Implants in Orthopedics—A General Review and Perspectives. Adv. Sci. 2020, 7, 1902443. [Google Scholar] [CrossRef]
- Witte, F. The history of biodegradable magnesium implants: A review. Acta Biomater. 2010, 6, 1680–1692. [Google Scholar] [CrossRef]
- Willumeit, R.; Fischer, J.; Feyerabend, F.; Hort, N.; Bismayer, U.; Heidrich, S.; Mihailova, B. Chemical surface alteration of biodegradable magnesium exposed to corrosion media. Acta Biomater. 2011, 7, 2704–2715. [Google Scholar] [CrossRef]
- Banerjee, P.C.; Al-Saadi, S.; Choudhary, L.; Harandi, S.E.; Singh, R. Magnesium Implants: Prospects and Challenges. Materials 2019, 12, 136. [Google Scholar] [CrossRef]
- Yin, M.; Xu, F.; Ding, H.; Tan, F.; Song, F.; Wang, J. Incorporation of magnesium ions into photo-crosslinked alginate hydrogel enhanced cell adhesion ability. J. Tissue Eng. Regen. Med. 2015, 9, 1088–1092. [Google Scholar] [CrossRef]
- Roh, H.-S.; Lee, C.-M.; Hwang, Y.-H.; Kook, M.-S.; Yang, S.-W.; Lee, D.; Kim, B.-H. Addition of MgO nanoparticles and plasma surface treatment of three-dimensional printed polycaprolactone/hydroxyapatite scaffolds for improving bone regeneration. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 74, 525–535. [Google Scholar] [CrossRef]
- Yuan, Z.; Wei, P.; Huang, Y.; Zhang, W.; Chen, F.; Zhang, X.; Mao, J.; Chen, D.; Cai, Q.; Yang, X. Injectable PLGA microspheres with tunable magnesium ion release for promoting bone regeneration. Acta Biomater. 2018, 85, 294–309. [Google Scholar] [CrossRef]
- Witte, F.; Kaese, V.; Haferkamp, H.; Switzer, E.; Meyer-Lindenberg, A.; Wirth, C.J.; Windhagen, H. In vivo corrosion of four magnesium alloys and the associated bone response. Biomaterials 2005, 26, 3557–3563. [Google Scholar] [CrossRef] [PubMed]
- Feyerabend, F.; Fischer, J.; Holtz, J.; Witte, F.; Willumeit, R.; Drücker, H.; Vogt, C.; Hort, N. Evaluation of short-term effects of rare earth and other elements used in magnesium alloys on primary cells and cell lines. Acta Biomater. 2010, 6, 1834–1842. [Google Scholar] [CrossRef] [PubMed]
- Antoniac, I.; Paltanea, V.M.; Paltanea, G.; Antoniac, A.; Nemoianu, I.V.; Petrescu, M.I.; Dura, H.; Bodog, A.D. Additive Manufactured Magnesium-Based Scaffolds for Tissue Engineering. Materials 2022, 15, 8693. [Google Scholar] [CrossRef] [PubMed]
- Zhang, E.; Yang, L.; Xu, J.; Chen, H. Microstructure, mechanical properties and bio-corrosion properties of Mg-Si(-Ca, Zn) alloy for biomedical application. Acta Biomater. 2010, 6, 1756–1762. [Google Scholar] [CrossRef]
- Istrate, B.; Munteanu, C.; Antoniac, I.V.; Lupescu, S.C. Current Research Studies of Mg-Ca-Zn Biodegradable Alloys Used as Orthopedic Implants-Review. Crystals 2022, 12, 1468. [Google Scholar] [CrossRef]
- Ben-Hamu, G.; Eliezer, D.; Shin, K.S. The role of Si and Ca on new wrought Mg-Zn-Mn based alloy. Mat. Sci. Eng. A 2007, 447, 35–43. [Google Scholar] [CrossRef]
- Turan, B. A Brief Overview from the Physiological and Detrimental Roles of Zinc Homeostasis via Zinc Transporters in the Heart. Biol. Trace Elem. Res. 2018, 188, 160–176. [Google Scholar] [CrossRef] [PubMed]
- Jackson, M.J.; Lowe, N.M. Physiological-Role of Zinc. Food Chem. 1992, 43, 233–238. [Google Scholar] [CrossRef]
- Maret, W. Zinc in Cellular Regulation: The Nature and Significance of “Zinc Signals”. Int. J. Mol. Sci. 2017, 18, 2285. [Google Scholar] [CrossRef]
- Vallee, B.L.; Falchuk, K.H.; Hashimoto, A.; Nakagawa, M.; Tsujimura, N.; Miyazaki, S.; Kizu, K.; Goto, T.; Komatsu, Y.; Matsunaga, A.; et al. The biochemical basis of zinc physiology. Physiol. Rev. 1993, 73, 79–118. [Google Scholar] [CrossRef] [PubMed]
- Beyersmann, D.; Haase, H. Functions of zinc in signaling, proliferation and differentiation of mammalian cells. BioMetals 2001, 14, 331–341. [Google Scholar] [CrossRef]
- Haase, H.; Maret, W. Intracellular zinc fluctuations modulate protein tyrosine phosphatase activity in insulin/insulin-like growth factor-1 signaling. Exp. Cell Res. 2003, 291, 289–298. [Google Scholar] [CrossRef]
- Andreini, C.; Bertini, I.; Rosato, A. Metalloproteomes: A Bioinformatic Approach. Acc. Chem. Res. 2009, 42, 1471–1479. [Google Scholar] [CrossRef]
- Brylinski, M.; Skolnick, J. FINDSITE-metal: Integrating evolutionary information and machine learning for structure-based metal-binding site prediction at the proteome level. Proteins: Struct. Funct. Bioinform. 2010, 79, 735–751. [Google Scholar] [CrossRef]
- Maret, W. Zinc Coordination Environments in Proteins as Redox Sensors and Signal Transducers. Antioxid. Redox Signal. 2006, 8, 1419–1441. [Google Scholar] [CrossRef]
- Cousins, R.J.; Liuzzi, J.P.; Lichten, L.A. Mammalian zinc transport, trafficking, and signals. J. Biol. Chem. 2006, 281, 24085–24089. [Google Scholar] [CrossRef]
- Eide, D.J. Zinc transporters and the cellular trafficking of zinc. Biochim. Biophys. Acta (BBA) Mol. Cell Res. 2006, 1763, 711–722. [Google Scholar] [CrossRef]
- Bentley, P.J. Influx of Zinc by Channel Catfish (Ictalurus-Punctatus)—Uptake from External Environmental Solutions. Comp. Biochem. Physiol. C-Pharmacol. Toxicol. Endocrinol. 1992, 101, 215–217. [Google Scholar] [CrossRef]
- Hogstrand, C.; Verbost, P.M.; Bonga, S.E.; Wood, C.M. Mechanisms of zinc uptake in gills of freshwater rainbow trout: Interplay with calcium transport. Am. J. Physiol. Integr. Comp. Physiol. 1996, 270, R1141–R1147. [Google Scholar] [CrossRef]
- Haase, H.; Ober-Blöbaum, J.L.; Engelhardt, G.; Hebel, S.; Heit, A.; Heine, H.; Rink, L. Zinc Signals Are Essential for Lipopolysaccharide-Induced Signal Transduction in Monocytes. Perspect. Surg. 2008, 181, 6491–6502. [Google Scholar] [CrossRef]
- Haase, H.; Rink, L. Functional Significance of Zinc-Related Signaling Pathways in Immune Cells. Annu. Rev. Nutr. 2009, 29, 133–152. [Google Scholar] [CrossRef]
- Haase, H.; Hebel, S.; Engelhardt, G.; Rink, L. Flow cytometric measurement of labile zinc in peripheral blood mononuclear cells. Anal. Biochem. 2006, 352, 222–230. [Google Scholar] [CrossRef]
- Frassinetti, S.; Bronzetti, G.; Caltavuturo, L.; Cini, M.; Della Croce, C. The role of zinc in life: A review. J. Environ. Pathol. Tox. 2006, 25, 597–610. [Google Scholar] [CrossRef] [PubMed]
- Lansdown, A.B.G.; Mirastschijski, U.; Stubbs, N.; Scanlon, E.; Agren, M.S. Zinc in wound healing: Theoretical, experimental, and clinical aspects. Wound Repair Regener. 2007, 15, 2–16. [Google Scholar] [CrossRef] [PubMed]
- Ågren, M.S. Percutaneous Absorption of Zinc from Zinc Oxide Applied Topically to Intact Skin in Man. Dermatology 1990, 180, 36–39. [Google Scholar] [CrossRef]
- Henzel, J.H.; DeWeese, M.S.; Lichti, E.L. Zinc concentrations within healing wounds. Significance of postoperative zincuria on availability and requirements during tissue repair. Arch. Surg. 1970, 100, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Michaelsson, G.; Ljunghall, K.; Danielson, B.G. Zinc in epidermis and dermis in healthy subjects. Acta Derm. Venereol. 1980, 60, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Portnoy, B.; Dyer, A.; Molokhia, A. Neutron activation analysis of trace elements in skin. IX. Rubidium in normal skin. Br. J. Dermatol. 1981, 105, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Hanada, K.; Sawamura, D.; Hashimoto, I.; Kida, K.; Naganuma, A. Epidermal Proliferation of the Skin in Metallothionein-Null Mice. J. Investig. Dermatol. 1998, 110, 259–262. [Google Scholar] [CrossRef] [PubMed]
- Iwata, M.; Takebayashi, T.; Ohta, H.; Alcalde, R.E.; Itano, Y.; Matsumura, T. Zinc accumulation and metallothionein gene expression in the proliferating epidermis during wound healing in mouse skin. Histochem. Cell Biol. 1999, 112, 283–290. [Google Scholar] [CrossRef]
- Lansdown, A.B.G. Metallothioneins: Potential therapeutic aids for wound healing in the skin. Wound Repair Regen. 2002, 10, 130–132. [Google Scholar] [CrossRef]
- Lansdown, A.B.G. Calcium: A potential central regulator in wound healing in the skin. Wound Repair Regen. 2002, 10, 271–285. [Google Scholar] [CrossRef]
- Sakamoto, M.; Tzeng, S.; Fukuyama, K.; Epstein, W.L. Light-scattering studies of cation-stimulated filament assembly of newborn rat epidermal keratin. Biochim. Et Biophys. Acta (BBA) Protein Struct. 1980, 624, 205–210. [Google Scholar] [CrossRef]
- Lansdown, A. Morphological variations in keratinising epithelia in the beagle. Veter. Rec. 1985, 116, 127–130. [Google Scholar] [CrossRef]
- Henkin, R.I.; Schecter, P.J.; Friedewald, W.T.; Demets, D.L.; Raff, M. A double blind study of the effects of zinc sulfate on taste and smell dysfunction. Am. J. Med. Sci. 1976, 272, 285–299. [Google Scholar] [CrossRef]
- Ravanti, L.; Kähäri, V.M. Matrix metalloproteinases in wound repair (review). Int. J. Mol. Med. 2000, 6, 391–798. [Google Scholar] [CrossRef]
- Plum, L.M.; Rink, L.; Haase, H. The Essential Toxin: Impact of Zinc on Human Health. Int. J. Environ. Res. Public Health 2010, 7, 1342–1365. [Google Scholar] [CrossRef] [PubMed]
- Wessels, I.; Maywald, M.; Rink, L. Zinc as a Gatekeeper of Immune Function. Nutrients 2017, 9, 1286. [Google Scholar] [CrossRef]
- Ranasinghe, P.; Wathurapatha, W.; Ishara, M.; Jayawardana, R.; Galappatthy, P.; Katulanda, P.; Constantine, G. Effects of Zinc supplementation on serum lipids: A systematic review and meta-analysis. Nutr. Metab. 2015, 12, 1–16. [Google Scholar] [CrossRef]
- Sum, E.Y.; O’Reilly, L.A.; Jonas, N.; Lindeman, G.J.; Visvader, J.E. The LIM Domain Protein Lmo4 Is Highly Expressed in Proliferating Mouse Epithelial Tissues. J. Histochem. Cytochem. 2005, 53, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.-H.; Ying, D.-J.; Mi, J.-H.; Zhang, W.; Dong, S.-W.; Sun, J.-S.; Zhang, J.-P. The zinc finger protein A20 protects endothelial cells from burns serum injury. Burns 2004, 30, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Cousins, R.J.; Leinart, A.S. Tissue-specific regulation of zinc metabolism and metallothionein genes by interleukin 1. FASEB J. 1988, 2, 2884–2890. [Google Scholar] [CrossRef]
- Lansdown, A.B.G.; Sampson, B.; Rowe, A. Sequential changes in trace metal, metallothionein and calmodulin concentrations in healing skin wounds. J. Anat. 1999, 195 Pt 3, 375–386. [Google Scholar] [CrossRef]
- Savlov, E.D.; Strain, W.H.; Huegin, F. Radiozinc studies in experimental wound healing. J. Surg. Res. 1962, 2, 209–212. [Google Scholar] [CrossRef]
- Bernstein, I.; Chakrabarti, S.; Kumaroo, K.; Sibrack, L. Synthesis of protein in the mammalian epidermis. J. Investig. Dermatol. 1970, 55, 291–302. [Google Scholar] [CrossRef][Green Version]
- Tenaud, I.; Leroy, S.; Chebassier, N.; Dreno, B. Zinc, copper and manganese enhanced keratinocyte migration through a functional modulation of keratinocyte integrins. Exp. Dermatol. 2000, 9, 407–416. [Google Scholar] [CrossRef]
- Zhu, D.; Cockerill, I.; Su, Y.; Zhang, Z.; Fu, J.; Lee, K.-W.; Ma, J.; Okpokwasili, C.; Tang, L.; Zheng, Y.; et al. Mechanical Strength, Biodegradation, and in Vitro and in Vivo Biocompatibility of Zn Biomaterials. ACS Appl. Mater. Interfaces 2019, 11, 6809–6819. [Google Scholar] [CrossRef] [PubMed]
- Mostaed, E.; Sikora-Jasinska, M.; Drelich, J.W.; Vedani, M. Zinc-based alloys for degradable vascular stent applications. Acta Biomater. 2018, 71, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Vojtěch, D.; Kubásek, J.; Šerák, J.; Novák, P. Mechanical and corrosion properties of newly developed biodegradable Zn-based alloys for bone fixation. Acta Biomater. 2011, 7, 3515–3522. [Google Scholar] [CrossRef]
- Venezuela, J.J.D.; Johnston, S.; Dargusch, M.S. The Prospects for Biodegradable Zinc in Wound Closure Applications. Adv. Healthc. Mater. 2019, 8, e1900408. [Google Scholar] [CrossRef] [PubMed]
- Bowen, P.K.; Drelich, J.; Goldman, J. Zinc Exhibits Ideal Physiological Corrosion Behavior for Bioabsorbable Stents. Adv. Mater. 2013, 25, 2577–2582. [Google Scholar] [CrossRef]
- Wu, J.; Wang, L.; He, J.; Zhu, C. In vitro cytotoxicity of Cu(2)(+), Zn(2)(+), Ag(+) and their mixtures on primary human endometrial epithelial cells. Contraception 2012, 85, 509–518. [Google Scholar] [CrossRef]
- Yoo, M.H.; Lee, J.Y.; Lee, S.E.; Koh, J.Y.; Yoon, Y.H. Protection by pyruvate of rat retinal cells against zinc toxicity in vitro, and pressure-induced ischemia in vivo. Investig. Ophthalmol. Vis. Sci. 2004, 45, 1523–1530. [Google Scholar] [CrossRef]
- Rodilla, V.; Miles, A.T.; Jenner, W.; Hawksworth, G.M. Exposure of cultured human proximal tubular cells to cadmium, mercury, zinc and bismuth: Toxicity and metallothionein induction. Chem. Interact. 1998, 115, 71–83. [Google Scholar] [CrossRef]
- Cheng, J.; Liu, B.; Wu, Y.; Zheng, Y. Comparative in vitro Study on Pure Metals (Fe, Mn, Mg, Zn and W) as Biodegradable Metals. J. Mater. Sci. Technol. 2013, 29, 619–627. [Google Scholar] [CrossRef]
- Bordbar-Khiabani, A.; Ebrahimi, S.; Yarmand, B. In-vitro corrosion and bioactivity behavior of tailored calcium phosphate-containing zinc oxide coating prepared by plasma electrolytic oxidation. Corros. Sci. 2020, 173, 108781. [Google Scholar] [CrossRef]
- Yang, H.; Wang, C.; Liu, C.; Chen, H.; Wu, Y.; Han, J.; Jia, Z.; Lin, W.; Zhang, D.; Li, W.; et al. Evolution of the degradation mechanism of pure zinc stent in the one-year study of rabbit abdominal aorta model. Biomaterials 2017, 145, 92–105. [Google Scholar] [CrossRef] [PubMed]
- Li, H.F.; Xie, X.H.; Zheng, Y.F.; Cong, Y.; Zhou, F.Y.; Qiu, K.J.; Wang, X.; Chen, S.H.; Huang, L.; Tian, L.; et al. Development of biodegradable Zn-1X binary alloys with nutrient alloying elements Mg, Ca and Sr. Sci. Rep. 2015, 5, 10719. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Cockerill, I.; Wang, Y.; Qin, Y.-X.; Chang, L.; Zheng, Y.; Zhu, D. Zinc-Based Biomaterials for Regeneration and Therapy. Trends Biotechnol. 2019, 37, 428–441. [Google Scholar] [CrossRef] [PubMed]
- Xia, P.; Lian, S.; Wu, Y.; Yan, L.; Quan, G.; Zhu, G. Zinc is an important inter-kingdom signal between the host and microbe. Veter. Res. 2021, 52, 1–14. [Google Scholar] [CrossRef]
- Wei, Y.; Wang, J.; Wu, S.; Zhou, R.; Zhang, K.; Zhang, Z.; Liu, J.; Qin, S.; Shi, J. Nanomaterial-Based Zinc Ion Interference Therapy to Combat Bacterial Infections. Front. Immunol. 2022, 13, 899992. [Google Scholar] [CrossRef]
- Rutherford, D.; Jíra, J.; Kolářová, K.; Matolínová, I.; Mičová, J.; Remeš, Z.; Rezek, B. Growth Inhibition of Gram-Positive and Gram-Negative Bacteria by Zinc Oxide Hedgehog Particles. Int. J. Nanomed. 2021, 16, 3541–3554. [Google Scholar] [CrossRef]
- Su, Y.; Wang, K.; Gao, J.; Yang, Y.; Qin, Y.-X.; Zheng, Y.; Zhu, D. Enhanced cytocompatibility and antibacterial property of zinc phosphate coating on biodegradable zinc materials. Acta Biomater. 2019, 98, 174–185. [Google Scholar] [CrossRef]
- Li, G.; Yang, H.; Zheng, Y.; Chen, X.-H.; Yang, J.-A.; Zhu, D.; Ruan, L.; Takashima, K. Challenges in the use of zinc and its alloys as biodegradable metals: Perspective from biomechanical compatibility. Acta Biomater. 2019, 97, 23–45. [Google Scholar] [CrossRef]
- Zheng, Y.F.; Gu, X.N.; Witte, F. Biodegradable metals. Mat. Sci. Eng. R 2014, 77, 1–34. [Google Scholar] [CrossRef]
- Venezuela, J.; Dargusch, M. The influence of alloying and fabrication techniques on the mechanical properties, biodegradability and biocompatibility of zinc: A comprehensive review. Acta Biomater. 2019, 87, 1–40. [Google Scholar] [CrossRef]
- Chen, K.; Lu, Y.; Tang, H.; Gao, Y.; Zhao, F.; Gu, X.; Fan, Y. Effect of strain on degradation behaviors of WE43, Fe and Zn wires. Acta Biomater. 2020, 113, 627–645. [Google Scholar] [CrossRef] [PubMed]
- Bowen, P.K.; Seitz, J.M.; Guillory, R.J., 2nd; Braykovich, J.P.; Zhao, S.; Goldman, J.; Drelich, J.W. Evaluation of wrought Zn-Al alloys (1, 3, and 5 wt % Al) through mechanical and in vivo testing for stent applications. J. Biomed. Mater. Res. B Appl. Biomater. 2018, 106, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Mostaed, E.; Sikora-Jasinska, M.; Mostaed, A.; Loffredo, S.; Demir, A.; Previtali, B.; Mantovani, D.; Beanland, R.; Vedani, M. Novel Zn-based alloys for biodegradable stent applications: Design, development and in vitro degradation. J. Mech. Behav. Biomed. Mater. 2016, 60, 581–602. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Li, P.; Shen, G.; Mo, X.; Zhou, C.; Alexander, D.; Rupp, F.; Geis-Gerstorfer, J.; Zhang, H.; Wan, G. Appropriately adapted properties of hot-extruded Zn-0.5Cu-xFe alloys aimed for biodegradable guided bone regeneration membrane application. Bioact. Mater. 2021, 6, 975–989. [Google Scholar] [CrossRef]
- García-Mintegui, C.; Córdoba, L.C.; Buxadera-Palomero, J.; Marquina, A.; Jiménez-Piqué, E.; Ginebra, M.-P.; Cortina, J.L.; Pegueroles, M. Zn-Mg and Zn-Cu alloys for stenting applications: From nanoscale mechanical characterization to in vitro degradation and biocompatibility. Bioact. Mater. 2021, 6, 4430–4446. [Google Scholar] [CrossRef]
- Hu, Y.; Guo, X.; Qiao, Y.; Wang, X.; Lin, Q. Preparation of medical Mg–Zn alloys and the effect of different zinc contents on the alloy. J. Mater. Sci. Mater. Med. 2022, 33, 1–13. [Google Scholar] [CrossRef]
- Kubasek, J.; Dvorsky, D.; Sedy, J.; Msallamova, S.; Levorova, J.; Foltan, R.; Vojtech, D. The Fundamental Comparison of Zn-2Mg and Mg-4Y-3RE Alloys as a Perspective Biodegradable Materials. Materials 2019, 12, 3745. [Google Scholar] [CrossRef]
- Yang, H.; Jia, B.; Zhang, Z.; Qu, X.; Li, G.; Lin, W.; Zhu, D.; Dai, K.; Zheng, Y. Alloying design of biodegradable zinc as promising bone implants for load-bearing applications. Nat. Commun. 2020, 11, 1–16. [Google Scholar] [CrossRef]
- Sezer, N.; Evis, Z.; Kayhan, S.M.; Tahmasebifar, A.; Koç, M. Review of magnesium-based biomaterials and their applications. J. Magnes. Alloy 2018, 6, 23–43. [Google Scholar] [CrossRef]
- Liu, J.; Sonshine, D.A.; Shervani, S.; Hurt, R.H. Controlled Release of Biologically Active Silver from Nanosilver Surfaces. ACS Nano 2010, 4, 6903–6913. [Google Scholar] [CrossRef]
- Jiang, J.; Pi, J.; Cai, J. The Advancing of Zinc Oxide Nanoparticles for Biomedical Applications. Bioinorg. Chem. Appl. 2018, 2018, 1062562. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Chen, L.; Yin, M.; Xu, S.; Liang, Z. Review on magnesium and magnesium-based alloys as biomaterials for bone immobilization. J. Mater. Res. Technol. 2023, 23, 4396–4419. [Google Scholar] [CrossRef]
- Mutlu, N.; Liverani, L.; Kurtuldu, F.; Galusek, D.; Boccaccini, A.R. Zinc improves antibacterial, anti-inflammatory and cell motility activity of chitosan for wound healing applications. Int. J. Biol. Macromol. 2022, 213, 845–857. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Zheng, Y.; Cheng, Y.; Zhong, S.; Xi, T. In vitro corrosion and biocompatibility of binary magnesium alloys. Biomaterials 2009, 30, 484–498. [Google Scholar] [CrossRef] [PubMed]
- Levy, G.K.; Goldman, J.; Aghion, E. The Prospects of Zinc as a Structural Material for Biodegradable Implants—A Review Paper. Metals 2017, 7, 402. [Google Scholar] [CrossRef]
- Gong, H.; Wang, K.; Strich, R.; Zhou, J.G. In vitro biodegradation behavior, mechanical properties, and cytotoxicity of biodegradable Zn-Mg alloy. J. Biomed. Mater. Res. B Appl. Biomater. 2015, 103, 1632–1640. [Google Scholar] [CrossRef]
- Chen, Y.; Xu, Z.; Smith, C.; Sankar, J. Recent advances on the development of magnesium alloys for biodegradable implants. Acta Biomater. 2014, 10, 4561–4573. [Google Scholar] [CrossRef]
- Agarwal, S.; Curtin, J.; Duffy, B.; Jaiswal, S. Biodegradable magnesium alloys for orthopaedic applications: A review on corrosion, biocompatibility and surface modifications. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 68, 948–963. [Google Scholar] [CrossRef]
- Kubasek, J.; Vojtech, D.; Jablonska, E.; Pospisilova, I.; Lipov, J.; Ruml, T. Structure, mechanical characteristics and in vitro degradation, cytotoxicity, genotoxicity and mutagenicity of novel biodegradable Zn-Mg alloys. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 58, 24–35. [Google Scholar] [CrossRef]
- Kubasek, J.; Pospisilova, I.; Vojtech, D.; Jablonska, E.; Ruml, T. Structural, Mechanical and Cytotoxicity Characterization of As-Cast Biodegradable Zn-xMg (x = 0.8–8.3%) alloys. Mater. Tehnol. 2014, 48, 623–629. [Google Scholar]
- Murni, N.; Dambatta, M.; Yeap, S.; Froemming, G.; Hermawan, H. Cytotoxicity evaluation of biodegradable Zn–3Mg alloy toward normal human osteoblast cells. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 49, 560–566. [Google Scholar] [CrossRef] [PubMed]
- Sheu, T.-J.; Schwarz, E.M.; Martinez, D.A.; O’Keefe, R.J.; Rosier, R.N.; Zuscik, M.J.; Puzas, J.E. A Phage Display Technique Identifies a Novel Regulator of Cell Differentiation. J. Biol. Chem. 2003, 278, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Luo, Q.; Zhang, X.; Qiu, J.; Qian, S.; Liu, X. Co-implantation of magnesium and zinc ions into titanium regulates the behaviors of human gingival fibroblasts. Bioact. Mater. 2020, 6, 64–74. [Google Scholar] [CrossRef] [PubMed]
- Sazegar, G.; Reza, A.H.S.; Behravan, E. The effects of supplemental zinc and honey on wound healing in rats. Iran. J. Basic Med. Sci 2011, 14, 391–398. [Google Scholar]
- Lansdown, A. Influence of zinc oxide in the closure of open skin wounds. Int. J. Cosmet. Sci. 1993, 15, 83–85. [Google Scholar] [CrossRef]
- Apelqvist, J.; Larsson, J.; Lstenstrom, A. Topical treatment of necrotic foot ulcers in diabetic patients: A comparative trial of DuoDerm and MeZinc. Br. J. Dermatol. 1990, 123, 787–792. [Google Scholar] [CrossRef]
- Agren, M. Zinc oxide increases degradation of collagen in necrotic wound tissue. Br. J. Dermatol. 1993, 129, 221–222. [Google Scholar] [CrossRef]
- Nagase, H.; Visse, R.; Murphy, G. Structure and function of matrix metalloproteinases and TIMPs. Cardiovasc. Res. 2006, 69, 562–573. [Google Scholar] [CrossRef]
- Moreno-Eutimio, M.A.; Espinosa-Monroy, L.; Orozco-Amaro, T.; Torres-Ramos, Y.; Montoya-Estrada, A.; Hicks, J.J.; Rodríguez-Ayala, E.; Del Moral, P.; Moreno, J.; Cueto-García, J. Enhanced healing and anti-inflammatory effects of a carbohydrate polymer with zinc oxide in patients with chronic venous leg ulcers: Preliminary results. Arch. Med. Sci. 2016, 14, 336–344. [Google Scholar] [CrossRef]
- Mirastschijski, U.; Haaksma, C.J.; Tomasek, J.J.; Ågren, M.S. Matrix metalloproteinase inhibitor GM 6001 attenuates keratinocyte migration, contraction and myofibroblast formation in skin wounds. Exp. Cell Res. 2004, 299, 465–475. [Google Scholar] [CrossRef]
- A Cabral-Pacheco, G.; Garza-Veloz, I.; La Rosa, C.C.-D.; Ramirez-Acuña, J.M.; A Perez-Romero, B.; Guerrero-Rodriguez, J.F.; Martinez-Avila, N.; Martinez-Fierro, M.L. The Roles of Matrix Metalloproteinases and Their Inhibitors in Human Diseases. Int. J. Mol. Sci. 2020, 21, 9739. [Google Scholar] [CrossRef] [PubMed]
- Ågren, M.S.; Andersen, L.; Heegaard, A.M.; Jorgensen, L.N. Effect of parenteral zinc sulfate on colon anastomosis repair in the rat. Int. J. Color. Dis. 2008, 23, 857–861. [Google Scholar] [CrossRef] [PubMed]
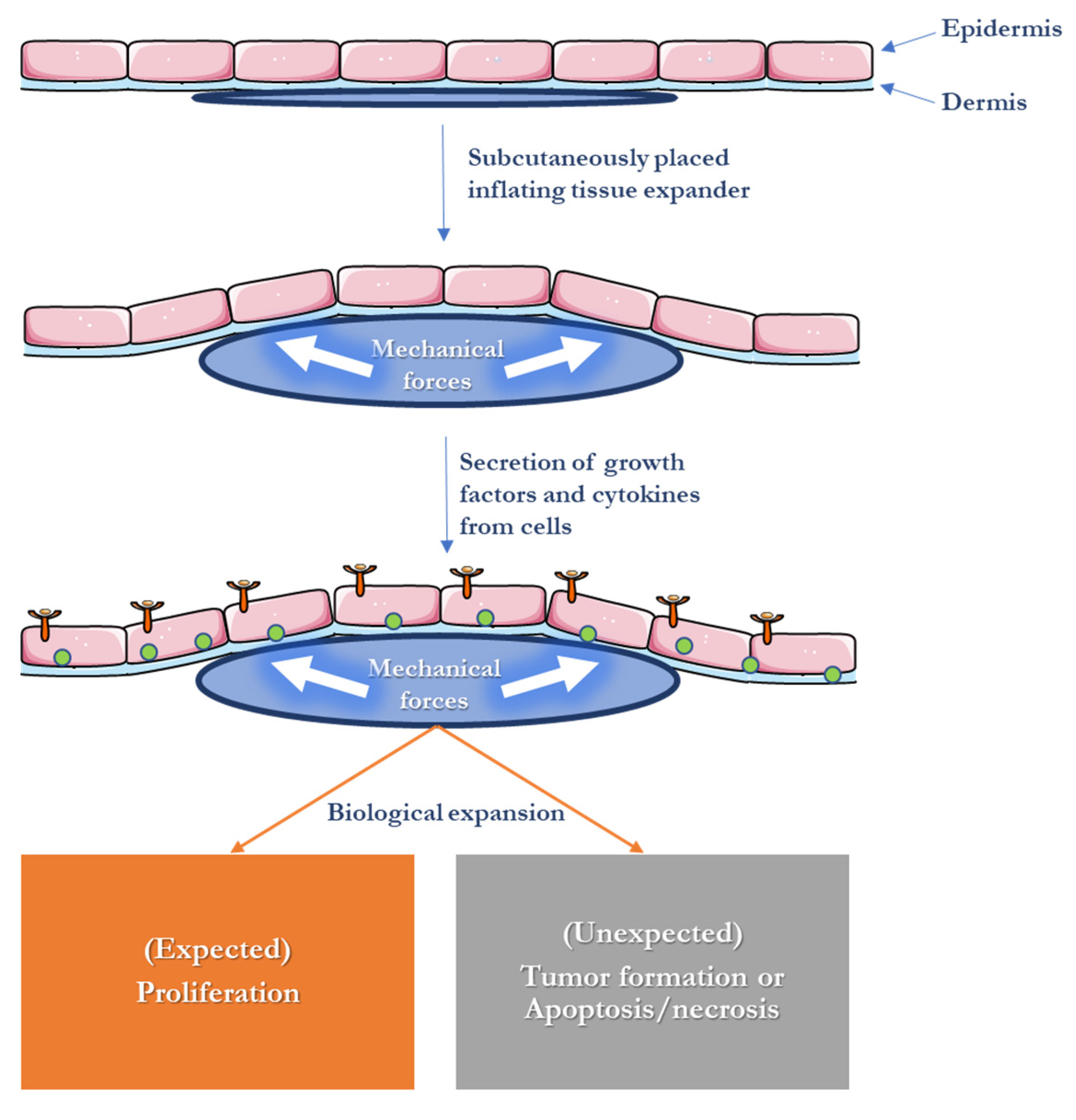

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hassan, N.; Krieg, T.; Zinser, M.; Schröder, K.; Kröger, N. An Overview of Scaffolds and Biomaterials for Skin Expansion and Soft Tissue Regeneration: Insights on Zinc and Magnesium as New Potential Key Elements. Polymers 2023, 15, 3854. https://doi.org/10.3390/polym15193854
Hassan N, Krieg T, Zinser M, Schröder K, Kröger N. An Overview of Scaffolds and Biomaterials for Skin Expansion and Soft Tissue Regeneration: Insights on Zinc and Magnesium as New Potential Key Elements. Polymers. 2023; 15(19):3854. https://doi.org/10.3390/polym15193854
Chicago/Turabian StyleHassan, Nourhan, Thomas Krieg, Max Zinser, Kai Schröder, and Nadja Kröger. 2023. "An Overview of Scaffolds and Biomaterials for Skin Expansion and Soft Tissue Regeneration: Insights on Zinc and Magnesium as New Potential Key Elements" Polymers 15, no. 19: 3854. https://doi.org/10.3390/polym15193854
APA StyleHassan, N., Krieg, T., Zinser, M., Schröder, K., & Kröger, N. (2023). An Overview of Scaffolds and Biomaterials for Skin Expansion and Soft Tissue Regeneration: Insights on Zinc and Magnesium as New Potential Key Elements. Polymers, 15(19), 3854. https://doi.org/10.3390/polym15193854






