In Vitro Comparison of Surface Roughness, Flexural, and Microtensile Strength of Various Glass-Ionomer-Based Materials and a New Alkasite Restorative Material
Abstract
1. Introduction
2. Materials and Methods
2.1. Surface Roughness Tests
2.2. Flexural Strength
2.3. Microtensile Bond Strength (μTBS)
2.4. Statistical Analysis
3. Results
4. Discussion
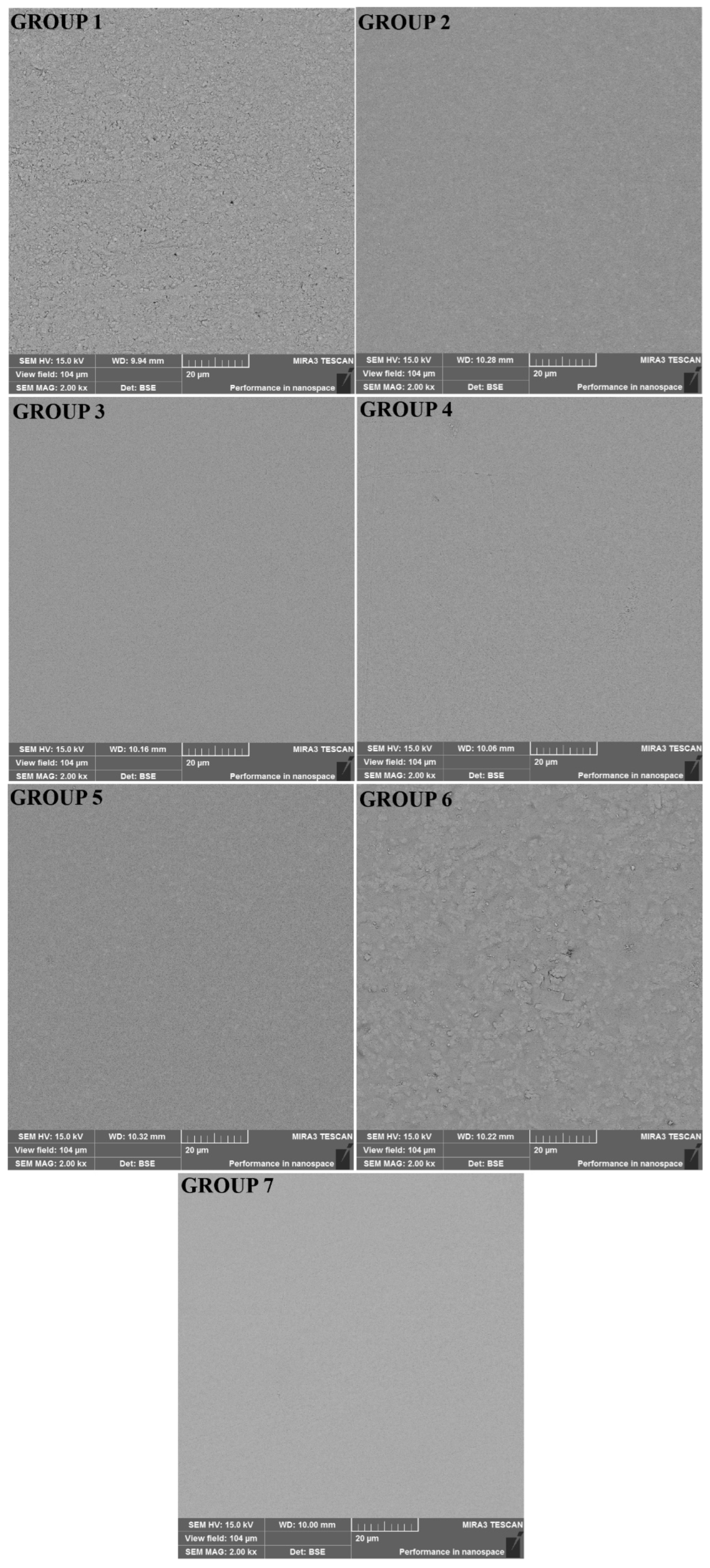
4.1. Surface Roughness
4.2. Flexural Strength
4.3. Microtensile Bond Strength
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kumar, S.A.; Ajitha, P. Evaluation of compressive strength between Cention N and high copper amalgam-An in vitro study. Drug Invent. Today 2019, 12, 255–257. [Google Scholar]
- Bezerra, I.M.; Brito, A.C.M.; de Sousa, S.A.; Santiago, B.M.; Cavalcanti, Y.W.; de Almeida, L.F.D. Glass ionomer cements compared with composite resin in restoration of noncarious cervical lesions: A systematic review and meta-analysis. Heliyon 2020, 6, e03969. [Google Scholar] [CrossRef] [PubMed]
- Zimmerli, B.; Strub, M.; Jeger, F.; Stadler, O.; Lussi, A. Composite materials: Composition, properties and clinical applications. A literature review. Schweiz. Mon. Zahnmed. Rev. Mens. Suisse D’odonto-Stomatol. Riv. Mens. Svizz. Odontol. Stomatol. 2010, 120, 972–986. [Google Scholar]
- Hiremath, G.; Horati, P.; Naik, B. Evaluation and comparison of flexural strength of Cention N with resin-modified glass-ionomer cement and composite-An in vitro study. J. Conserv. Dent. 2022, 25, 288–291. [Google Scholar] [CrossRef] [PubMed]
- Mishra, A.; Singh, G.; Singh, S.; Agarwal, M.; Qureshi, R.; Khurana, N. Comparative Evaluation of Mechanical Properties of Cention N with Conventionally used Restorative Materials—An In Vitro Study. Int. J. Prosthodont. Restor. Dent. 2018, 8, 120–124. [Google Scholar] [CrossRef]
- Panpisut, P.; Toneluck, A. Monomer conversion, dimensional stability, biaxial flexural strength, and fluoride release of resin-based restorative material containing alkaline fillers. Dent. Mater. J. 2020, 39, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Sadananda, V.; Shetty, C.; Hegde, M.; Bhat, G. Alkasite restorative material: Flexural and compressive strength evaluation. Res. J. Pharm. Biol. Chem. Sci. 2018, 9, 2179. [Google Scholar]
- Scientific Documentation of Cention N, Ivoclar Vivadent AG. Available online: https://downloadcenter.ivoclar.com/#search-text=cention&details=23015 (accessed on 26 January 2023).
- Iftikhar, N.; Devashish, B.S.; Gupta, N.; Natasha Ghambir, R.-S. A Comparative Evaluation of Mechanical Properties of Four Different Restorative Materials: An In Vitro Study. Int. J. Clin. Pediatr. Dent. 2019, 12, 47. [Google Scholar] [CrossRef]
- Chole, D.; Shah, H.; Kundoor, S.; Bakle, S.; Gandhi, N.; Hatte, N. In Vitro Comparision of Flexural Strength of Cention-N, BulkFill Composites, Light-Cure Nanocomposites And Resin-Modified Glass Ionomer Cement. IOSR J. Dent. Med. Sci. (IOSR-JDMS) 2018, 17, 79–82. [Google Scholar]
- Loomans, B.A.; Cardoso, M.V.; Opdam, N.J.; Roeters, F.J.; De Munck, J.; Huysmans, M.C.; Van Meerbeek, B. Surface roughness of etched composite resin in light of composite repair. J. Dent. 2011, 39, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Scholz, K.J.; Bittner, A.; Cieplik, F.; Hiller, K.A.; Schmalz, G.; Buchalla, W.; Federlin, M. Micromorphology of the Adhesive Interface of Self-Adhesive Resin Cements to Enamel and Dentin. Materials 2021, 14, 492. [Google Scholar] [CrossRef] [PubMed]
- Cazzaniga, G.; Ottobelli, M.; Ionescu, A.; Garcia-Godoy, F.; Brambilla, E. Surface properties of resin-based composite materials and biofilm formation: A review of the current literature. Am. J. Dent. 2015, 28, 311–320. [Google Scholar] [PubMed]
- Candan, M.; Ünal, M. The effect of various asthma medications on surface roughness of pediatric dental restorative materials: An atomic force microscopy and scanning electron microscopy study. Microsc. Res. Tech. 2021, 84, 271–283. [Google Scholar] [CrossRef] [PubMed]
- Gladys, S.; Van Meerbeek, B.; Braem, M.; Lambrechts, P.; Vanherle, G. Comparative physico-mechanical characterization of new hybrid restorative materials with conventional glass-ionomer and resin composite restorative materials. J. Dent. Res. 1997, 76, 883–894. [Google Scholar] [CrossRef] [PubMed]
- Ünal, M.; Candan, M.; İpek, İ.; Küçükoflaz, M.; Özer, A. Evaluation of the microhardness of different resin-based dental restorative materials treated with gastric acid: Scanning electron microscopy-energy dispersive X-ray spectroscopy analysis. Microsc. Res. Tech. 2021, 84, 2140–2148. [Google Scholar] [CrossRef] [PubMed]
- Marghalani, H.Y. Effect of filler particles on surface roughness of experimental composite series. J. Appl. Oral Sci. Rev. FOB 2010, 18, 59–67. [Google Scholar] [CrossRef]
- de Sousa-Lima, R.X.; de Lima, J.F.M.; Silva de Azevedo, L.J.; de Freitas Chaves, L.V.; Alonso, R.C.B.; Borges, B.C.D. Surface morphological and physical characterizations of glass ionomer cements after sterilization processes. Microsc. Res. Tech. 2018, 81, 1208–1213. [Google Scholar] [CrossRef]
- Maktabi, H.; Ibrahim, M.; Alkhubaizi, Q.; Weir, M.; Xu, H.; Strassler, H.; Fugolin, A.P.P.; Pfeifer, C.S.; Melo, M.A.S. Underperforming light curing procedures trigger detrimental irradiance-dependent biofilm response on incrementally placed dental composites. J. Dent. 2019, 88, 103110. [Google Scholar] [CrossRef]
- Alfawaz, Y. Impact of Polishing Systems on the Surface Roughness and Microhardness of Nanocomposites. J. Contemp. Dent. Pract. 2017, 18, 647–651. [Google Scholar] [CrossRef]
- Kaminedi, R.; Penumatsa, N.; Priya, T.; Baroudi, K. The influence of finishing/polishing time and cooling system on surface roughness and microhardness of two different types of composite resin restorations. J. Int. Soc. Prev. Community Dent. 2014, 4, S99–S104. [Google Scholar] [CrossRef]
- Gumustas, B.; Sismanoglu, S. Effectiveness of different resin composite materials for repairing noncarious amalgam margin defects. J. Conserv. Dent. JCD 2018, 21, 627–631. [Google Scholar] [CrossRef] [PubMed]
- Setty, A.; Nagesh, J.; Marigowda, J.; Shivanna, A.; Paluvary, S.; Ashwathappa, G. Comparative evaluation of surface roughness of novel resin composite Cention N with Filtek Z350 XT: In vitro study. Int. J. Oral Care Res. 2019, 7, 15. [Google Scholar] [CrossRef]
- Bollen, C.M.; Lambrechts, P.; Quirynen, M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: A review of the literature. Dent. Mater. Off. Publ. Acad. Dent. Mater. 1997, 13, 258–269. [Google Scholar] [CrossRef]
- Kiran, N.K.; Chowdhary, N.; John, D.; Reddy, R.; Shidhara, A.; Pavana, M.P. Comparative Evaluation of Mechanical Properties of Cention-N And Type IX GIC-An In Vitro Study. Int. J. Curr. Adv. Res. 2019, 8, 20498–20501. [Google Scholar] [CrossRef]
- Yao, C.; Ahmed, M.H.; Zhang, F.; Mercelis, B.; Van Landuyt, K.L.; Huang, C.; Van Meerbeek, B. Structural/Chemical Characterization and Bond Strength of a New Self-Adhesive Bulk-fill Restorative. J. Adhes. Dent. 2020, 22, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Naz, F.; Khan, A.; Kader, M.; Gelban, L.; Mousa, N.; Hakeem, A. Comparative evaluation of mechanical and physical properties of a new bulk-fill alkasite with conventional restorative materials. Saudi Dent. J. 2020, 33, 666–673. [Google Scholar] [CrossRef] [PubMed]
- Eligetti, T.; Dola, B.; Kamishetty, S.; Gaddala, N.; Swetha, A.; Bandari, J. Comparative Evaluation of Shear Bond Strength of Cention N with Other Aesthetic Restorative Materials to Dentin: An in Vitro Study. Ann. Rom. Soc. Cell Biol. 2021, 25, 12707–12714. [Google Scholar]
- Oznurhan, F.; Olmez, A. Morphological analysis of the resin-dentin interface in cavities prepared with Er,Cr:YSGG laser or bur in primary teeth. Photomed. Laser Surg. 2013, 31, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Valencia, J.; Felix, V. Alkasites, a New Alternative to Amalgam. Report of a Clinical Case. Acta Sci. Dent. Sci. 2019, 3, 11–19. [Google Scholar] [CrossRef]
- Butera, A.; Pascadopoli, M.; Gallo, S.; Lelli, M.; Tarterini, F.; Giglia, F.; Scribante, A. SEM/EDS Evaluation of the Mineral Deposition on a Polymeric Composite Resin of a Toothpaste Containing Biomimetic Zn-Carbonate Hydroxyapatite (microRepair(®)) in Oral Environment: A Randomized Clinical Trial. Polymers 2021, 13, 2740. [Google Scholar] [CrossRef]
| Materials | Code | Composition | Manufacturer | LOT Number |
|---|---|---|---|---|
| Universal Restorative 200 | COMP | Bis-GMA, Bis-EMA, UDMA, silica/zirconia, Filler 60% (volume) | 3M ESPE, St Paul, MN 55144, USA | NA06972 |
| Dyract XP | DYRA | UDMA, TCB resin, TEGDMA, trimethacrylate resin. 73 wt% Strontiumalumino-sodium-fluoro-phosphor-silicate | Dentsply, Konstanz, Germany | 2003000720 |
| Nova Glass LC | NOVA | Powder: Floro Alumino Silicate Glass, Pigments Liquid: Composite m resins 25–27% (Hema, dimethacrylates), Catalists, Stabilisators | Imicryl, Konya, Türkiye | 20031 |
| Fuji II LC Capsule | FUJI | 2-hydroxyethyl methacrylate, Polyacrylic acid, and water. 58 wt% Fluoro-aluminumsilicate | GC, Tokyo, Japan | 1908281 |
| Glass Liner | LINER | Glasionomerpulver, 1,6-Hexandioldimethacrylate, Bisphenol-A-bis (hydroxypropylmethacrylat), Isomere, 4-tert.-Butyl-N,N-dimethylaniline, Campherchinon | Willmann & Pein GmbH, Barmstedt, Germany | 187576 |
| Cention N | CENT | Powder: Barium aluminum silicate glass, ytterbium trifluoride, isofiller, calcium barium aluminum fluorosilicate glass, and calcium fluorosilicate glass Liquid: Urethane dimethacrylate, tricyclodecane dimethanol dimethacrylate, tetramethyl-xylylen diurethane dimethacrylate, polyethylene glycol 400 dimethacrylate, Ivocerin, and hydroxyperoxide | Ivoclar Vivadent, Schaan, Liechtenstein | Z0054T |
| AdperTM Easy One | 2 HEMA, Bis-GMA, Methacrylated 85010 phosphoric esters, 1,6 hexaneddiol dimethacrylate, Methacrylate functionalized polyalkenoic acid (vitrebond copolymer), dispersed bonbed silica fillers 7 nm, ethanol, water, camphorquinone, stabilizers. pH = 2.4 | 3M ESPE, Seefeld, Germany | 6744628 |
| Materials | Mean ± Standard Deviation (µm) | Mean ± Standard Deviation (MPa) |
|---|---|---|
| Group 1 (LC-CENT) | 0.27 ± 0.04 a | 58.17 ± 8.38 a |
| Group 2 (SC-CENT) | 0.17 ± 0.04 b | 86.32 ± 15.37 b |
| Group 3 (COMP) | 0.18 ± 0.06 b | 83.78 ± 16.65 b |
| Group 4 (DYRA) | 0.22 ± 0.1 b | 61.21 ± 9.82 a |
| Group 5 (LINER) | 0.18 ± 0.07 b | 41.75 ± 10.05 c |
| Group 6 (FUJI) | 0.33 ± 0.1 c | 48.17 ± 6.24 d |
| Group 7 (NOVA) | 0.26 ± 0.07 a | 57.83 ± 22.98 a,d |
| Materials | Mean ± Standard Deviation (MPa) | |
|---|---|---|
| Group 1 (LC-CENT) | 13.25 ± 4.4 B | F = 2.873 p = 0.015 * |
| Group 2 (SC-CENT) | 12.50 ± 5.05 B | |
| Group 3 (COMP) | 16.50 ± 7.73 A | |
| Group 4 (DYRA) | 16.36 ± 4.64 A | |
| Group 5 (LINER) | 11.98 ± 5.01 B | |
| Group 6 (FUJI) | 11.17 ± 3.0 B | |
| Group 7 (NOVA) | 9.88 ± 1.87 C |
| Materials | Group 1 (LC-CENT) | Group 2 (SC-CENT) | |
|---|---|---|---|
| Mean ± Standard Deviation (MPa) | p Values | ||
| Group 3 (COMP) | 20.00 ± 3.09 a | 23.69 ± 6.68 a | p = 0.131 |
| Group 4 (DYRA) | 17.23 ± 2.53 a,b | 20.09 ± 5.59 a,b | p = 0.156 |
| Group 5 (LINER) | 15.24 ± 2.20 b,c | 17.39 ± 2.94 a,b | p = 0.081 |
| Group 6 (FUJI) | 11.52 ± 2.65 c | 16.26 ± 5.09 b | p = 0.018 * |
| Group 7 (NOVA) | 12.79 ± 4.99 c | 21.72 ± 3.95 a,b | p = 0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaptan, A.; Oznurhan, F.; Candan, M. In Vitro Comparison of Surface Roughness, Flexural, and Microtensile Strength of Various Glass-Ionomer-Based Materials and a New Alkasite Restorative Material. Polymers 2023, 15, 650. https://doi.org/10.3390/polym15030650
Kaptan A, Oznurhan F, Candan M. In Vitro Comparison of Surface Roughness, Flexural, and Microtensile Strength of Various Glass-Ionomer-Based Materials and a New Alkasite Restorative Material. Polymers. 2023; 15(3):650. https://doi.org/10.3390/polym15030650
Chicago/Turabian StyleKaptan, Alper, Fatih Oznurhan, and Merve Candan. 2023. "In Vitro Comparison of Surface Roughness, Flexural, and Microtensile Strength of Various Glass-Ionomer-Based Materials and a New Alkasite Restorative Material" Polymers 15, no. 3: 650. https://doi.org/10.3390/polym15030650
APA StyleKaptan, A., Oznurhan, F., & Candan, M. (2023). In Vitro Comparison of Surface Roughness, Flexural, and Microtensile Strength of Various Glass-Ionomer-Based Materials and a New Alkasite Restorative Material. Polymers, 15(3), 650. https://doi.org/10.3390/polym15030650





