Detection of Limbal Stem Cells Adhered to Melt Electrospun Silk Fibroin and Gelatin-Modified Polylactic Acid Scaffolds
Abstract
:1. Introduction
2. Materials and Methods
2.1. Post-Processing of Melt Electrospun PLA Scaffolds
2.2. PLA Feeder Cells and Limbal Stem Cells (LSCs) Culture
2.3. Scanning Electron Microscopy Analysis
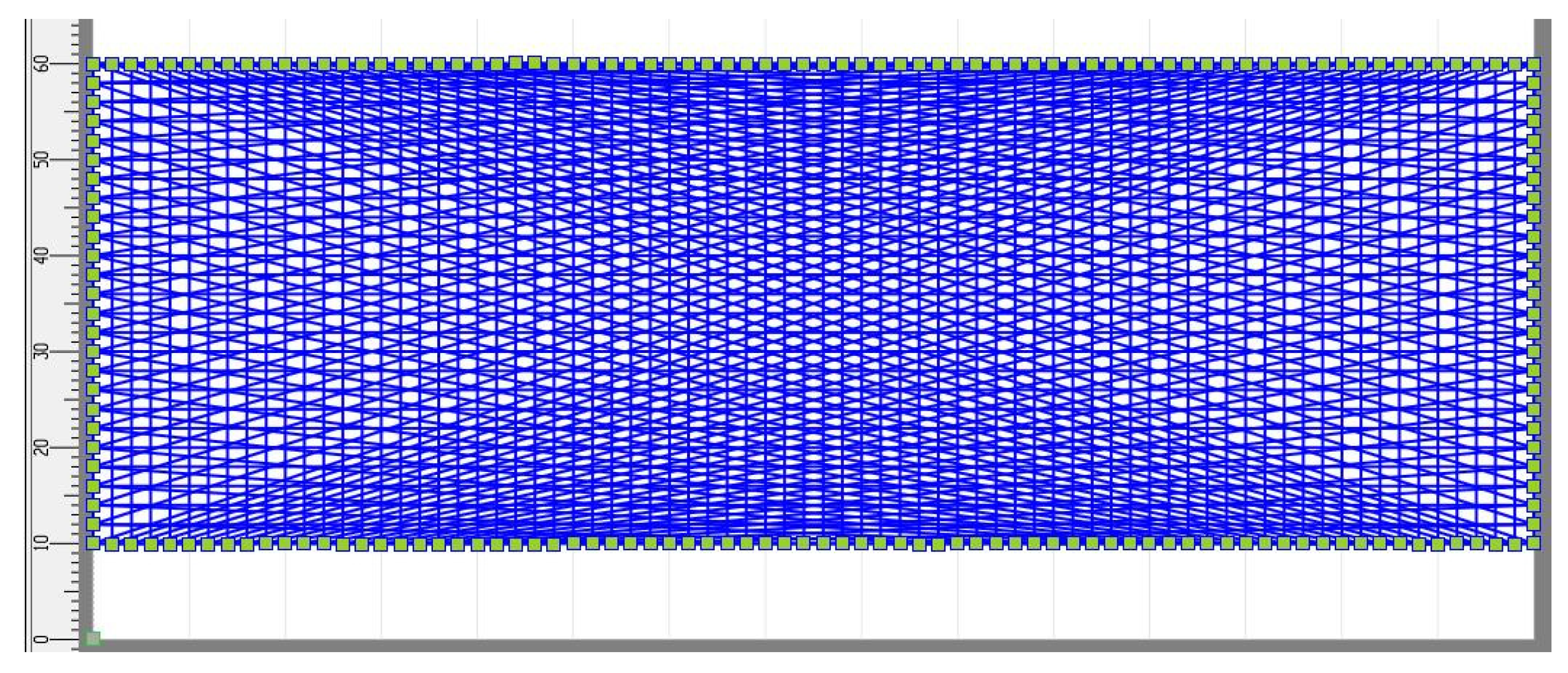
2.4. Total Porosity Calculation, Fiber Diameter, and Pore Area Measurement
2.5. Biodegradation of the Melt Electrospun Scaffolds
2.6. Absorption Ability of the Melt Electrospun Scaffolds
2.7. Scaffold Transparency Evaluation
2.8. Determining the Number of Viable LSCs Adhered to the Single PLA Scaffolds
2.9. Immunodetection of p63α and Cytokeratin 3 in the LSCs Using Flow Cytometry
2.10. The Detection of LSCs Adhered Onto the Modified PLA Scaffolds
2.11. Statistical Analysis
3. Results and Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pitts, D.G.; Kleinstein, R.N. Environmental vision: Interactions of the eye, vision, and the environment, Butterworth-Heinemann. MA 1993, 161–171. [Google Scholar]
- Van Buskirk, E.M. The anatomy of the limbus. Eye 1989, 3, 101–108. [Google Scholar] [CrossRef] [PubMed]
- WHO. Available online: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment (accessed on 28 October 2022).
- Dua, H.S.; Forrester, J.V. The corneoscleral limbus in human corneal epithelial wound healing. Am. J. Ophthalmol. 1990, 110, 646–656. [Google Scholar] [CrossRef] [PubMed]
- Meek, K. The cornea and sclera. In Collagen; Springer: Boston, MA, USA, 2008; pp. 359–396. [Google Scholar]
- Boulton, M.; Albon, J. Stem cells in the eye. Int. J. Biochem. Cell Biol. 2004, 36, 643–657. [Google Scholar] [CrossRef]
- Di Girolamo, N. Stem cells of the human cornea. Br. Med. Bull. 2011, 100, 191–207. [Google Scholar] [CrossRef]
- Le, Q.; Xu, J.; Deng, S.X. The diagnosis of limbal stem cell deficiency. Ocul. Surf. 2018, 16, 58–69. [Google Scholar] [CrossRef] [PubMed]
- Kruse, F.E. Stem cells and corneal epithelial regeneration. Eye 1994, 8, 170–183. [Google Scholar] [CrossRef]
- Singh, V.; Tiwari, A.; Kethiri, A.R.; Sangwan, V.S. Current perspectives of limbal-derived stem cells and its application in ocular surface regeneration and limbal stem cell transplantation. Stem Cells Transl. Med. 2021, 10, 1121–1128. [Google Scholar] [CrossRef]
- Chen, J.; Tseng, S. Corneal epithelial wound healing in partial limbal deficiency. Investig. Ophthalmol. Vis. Sci. 1990, 31, 1301–1314. [Google Scholar]
- Tsubota, K.; Satake, Y.; Kaido, M.; Shinozaki, N.; Shimmura, S.; Bissen-Miyajima, H.; Shimazaki, J. Treatment of severe ocular-surface disorders with corneal epithelial stem-cell transplantation. N. Engl. J. Med. 1999, 340, 1697–1703. [Google Scholar] [CrossRef]
- Rahman, I.; Said, D.; Maharajan, V.; Dua, H. Amniotic membrane in ophthalmology: Indications and limitations. Eye 2009, 23, 1954–1961. [Google Scholar] [CrossRef] [PubMed]
- Sanie-Jahromi, F.; Eghtedari, M.; Mirzaei, E.; Jalalpour, M.H.; Asvar, Z.; Nejabat, M.; Javidi-Azad, F. Propagation of limbal stem cells on polycaprolactone and polycaprolactone/gelatin fibrous scaffolds and transplantation in animal model. BioImpacts BI 2020, 10, 45. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.; Fang, J. Fundamentals of Electrospinning and Electrospun Nanofibers; DEStech Publications: Lancaster, PA, USA, 2017. [Google Scholar]
- Bubakir, M.M.; Li, H.; Barhoum, A.; Yang, W. Advances in Melt Electrospinning Technique; Springer: Cham/Zurich, Switzerland, 2018. [Google Scholar]
- Brown, T.D.; Dalton, P.D.; Hutmacher, D.W. Melt electrospinning today: An opportune time for an emerging polymer process. Prog. Polym. Sci. 2016, 56, 116–166. [Google Scholar] [CrossRef]
- Li, D.; Xia, Y. Electrospinning of nanofibers: Reinventing the wheel? Adv. Mater. 2004, 16, 1151–1170. [Google Scholar] [CrossRef]
- Włodarczyk-Biegun, M.K.; Villiou, M.; Koch, M.; Muth, C.; Wang, P.; Ott, J.; Del Campo, A. Melt Electrowriting of Graded Porous Scaffolds to Mimic the Matrix Structure of the Human Trabecular Meshwork. ACS Biomater. Sci. Eng. 2022, 8, 3899–3911. [Google Scholar] [CrossRef]
- Hrynevich, A.; Elçi, B.Ş.; Haigh, J.N.; McMaster, R.; Youssef, A.; Blum, C.; Blunk, T.; Hochleitner, G.; Groll, J.; Dalton, P.D. Dimension-based design of melt electrowritten scaffolds. Small 2018, 14, 1800232. [Google Scholar] [CrossRef]
- Saidy, N.T.; Shabab, T.; Bas, O.; Rojas-González, D.M.; Menne, M.; Henry, T.; Hutmacher, D.W.; Mela, P.; De-Juan-Pardo, E.M. Melt electrowriting of complex 3D anatomically relevant scaffolds. Front. Bioeng. Biotechnol. 2020, 8, 793. [Google Scholar] [CrossRef]
- Gao, Q.; Xie, J.; Salero, E.; Nuñez del Prado, Z.; Hutmacher, D.W.; Ye, J.; De Juan-Pardo, E.M.; Sabater, A.L.; Perez, V.L. Tissue engineering of corneal stroma via melt electrowriting. J. Tissue Eng. Regen. Med. 2021, 15, 841–851. [Google Scholar] [CrossRef]
- Bosworth, L.A.; Lanaro, M.; O’Loughlin, D.A.; D’Sa, R.A.; Woodruff, M.A.; Williams, R.L. Melt electro-written scaffolds with box-architecture support orthogonally oriented collagen. Biofabrication 2021, 14, 015015. [Google Scholar] [CrossRef]
- Wang, R.; Deng, S.; Wu, Y.; Wei, H.; Jing, G.; Zhang, B.; Liu, F.; Tian, H.; Chen, X.; Tian, W. Remodelling 3D printed GelMA-HA corneal scaffolds by cornea stromal cells. Colloid Interface Sci. Commun. 2022, 49, 100632. [Google Scholar] [CrossRef]
- Sharma, S.; Gupta, D.; Mohanty, S.; Jassal, M.; Agrawal, A.K.; Tandon, R. Surface-modified electrospun poly (ε-caprolactone) scaffold with improved optical transparency and bioactivity for damaged ocular surface reconstruction. Investig. Ophthalmol. Vis. Sci. 2014, 55, 899–907. [Google Scholar] [CrossRef]
- Kim, J.I.; Kim, J.Y.; Park, C.H. Fabrication of transparent hemispherical 3D nanofibrous scaffolds with radially aligned patterns via a novel electrospinning method. Sci. Rep. 2018, 8, 3424. [Google Scholar] [CrossRef] [Green Version]
- Xiao, Y.; Luo, H.; Tang, R.; Hou, J. Preparation and applications of electrospun optically transparent fibrous membrane. Polymers 2021, 13, 506. [Google Scholar] [CrossRef]
- Wu, M.; Wu, Y.; Liu, Z.; Liu, H. Optically transparent poly (methyl methacrylate) composite films reinforced with electrospun polyacrylonitrile nanofibers. J. Compos. Mater. 2012, 46, 2731–2738. [Google Scholar] [CrossRef]
- Tang, C.; Liu, H. Cellulose nanofiber reinforced poly (vinyl alcohol) composite film with high visible light transmittance. Compos. Part A Appl. Sci. Manuf. 2008, 39, 1638–1643. [Google Scholar] [CrossRef]
- Pawar, R.P.; Tekale, S.U.; Shisodia, S.U.; Totre, J.T.; Domb, A.J. Biomedical applications of poly (lactic acid). Recent Pat. Regen. Med. 2014, 4, 40–51. [Google Scholar] [CrossRef]
- Melke, J.; Midha, S.; Ghosh, S.; Ito, K.; Hofmann, S. Silk fibroin as biomaterial for bone tissue engineering. Acta Biomater. 2016, 31, 1–16. [Google Scholar] [CrossRef]
- Sun, W.; Gregory, D.A.; Tomeh, M.A.; Zhao, X. Silk fibroin as a functional biomaterial for tissue engineering. Int. J. Mol. Sci. 2021, 22, 1499. [Google Scholar] [CrossRef] [PubMed]
- Hoque, M.E.; Nuge, T.; Yeow, T.K.; Nordin, N.; Prasad, R. Gelatin based scaffolds for tissue engineering—A review. Polym. Res. J. 2015, 9, 15. [Google Scholar]
- Lukin, I.; Erezuma, I.; Maeso, L.; Zarate, J.; Desimone, M.F.; Al-Tel, T.H.; Dolatshahi-Pirouz, A.; Orive, G. Progress in Gelatin as Biomaterial for Tissue Engineering. Pharmaceutics 2022, 14, 1177. [Google Scholar] [CrossRef] [PubMed]
- Promnil, S.; Ruksakulpiwat, C.; Numpaisal, P.-o.; Ruksakulpiwat, Y. Electrospun poly (lactic acid) and silk fibroin based nanofibrous scaffold for meniscus tissue engineering. Polymers 2022, 14, 2435. [Google Scholar] [CrossRef]
- Pezeshki-Modaress, M.; Zandi, M.; Rajabi, S. Tailoring the gelatin/chitosan electrospun scaffold for application in skin tissue engineering: An in vitro study. Prog. Biomater. 2018, 7, 207–218. [Google Scholar] [CrossRef]
- Wu, J.; Zheng, A.; Liu, Y.; Jiao, D.; Zeng, D.; Wang, X.; Cao, L.; Jiang, X. Enhanced bone regeneration of the silk fibroin electrospun scaffolds through the modification of the graphene oxide functionalized by BMP-2 peptide. Int. J. Nanomed. 2019, 14, 733. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xue, C.; Zhu, H.; Tan, D.; Ren, H.; Gu, X.; Zhao, Y.; Zhang, P.; Sun, Z.; Yang, Y.; Gu, J. Electrospun silk fibroin-based neural scaffold for bridging a long sciatic nerve gap in dogs. J. Tissue Eng. Regen. Med. 2018, 12, e1143–e1153. [Google Scholar] [CrossRef]
- Fu, W.; Liu, Z.; Feng, B.; Hu, R.; He, X.; Wang, H.; Yin, M.; Huang, H.; Zhang, H.; Wang, W. Electrospun gelatin/PCL and collagen/PLCL scaffolds for vascular tissue engineering. Int. J. Nanomed. 2014, 9, 2335. [Google Scholar] [CrossRef] [PubMed]
- Tominac Trcin, M.; Dekaris, I.; Mijović, B.; Bujić, M.; Zdraveva, E.; Dolenec, T.; Pauk-Gulić, M.; Primorac, D.; Crnjac, J.; Špoljarić, B. Synthetic vs natural scaffolds for human limbal stem cells. Croat. Med. J. 2015, 56, 246–256. [Google Scholar] [CrossRef]
- Balan, K.K.; Sivanesan, V.; Moorthy, N.; Budhhan, D.; Jeyaseelan, S.; Sundaramoorthy, S. Effect of thickness of mat and testing parameters on tensile strength variability of electrospun nanofibrous mat. Mater. Today Proc. 2016, 3, 1320–1329. [Google Scholar] [CrossRef]
- Dias, J.R.; Sousa, A.; Augusto, A.; Bártolo, P.J.; Granja, P.L. Electrospun polycaprolactone (PCL) degradation: An in vitro and in vivo study. Polymers 2022, 14, 3397. [Google Scholar] [CrossRef]
- Guo, Z.; Yang, C.; Zhou, Z.; Chen, S.; Li, F. Characterization of biodegradable poly (lactic acid) porous scaffolds prepared using selective enzymatic degradation for tissue engineering. RSC Adv. 2017, 7, 34063–34070. [Google Scholar] [CrossRef]
- Shahverdi, M.; Seifi, S.; Akbari, A.; Mohammadi, K.; Shamloo, A.; Movahhedy, M.R. Melt electrowriting of PLA, PCL, and composite PLA/PCL scaffolds for tissue engineering application. Sci. Rep. 2022, 12, 19935. [Google Scholar] [CrossRef]
- Koenig, K.; Hermanns, S.; Ellerkmann, J.; Saralidze, K.; Langensiepen, F.; Seide, G. The effect of additives and process parameters on the pilot-scale manufacturing of polylactic acid sub-microfibers by melt electrospinning. Text. Res. J. 2020, 90, 1948–1961. [Google Scholar] [CrossRef]
- Chen, Y.-P.; Liu, H.-Y.; Liu, Y.-W.; Lee, T.-Y.; Liu, S.-J. Determination of electrospinning parameters’ strength in Poly (D, L)-lactide-co-glycolide micro/nanofiber diameter tailoring. J. Nanomater. 2019, 2019, 2626085. [Google Scholar] [CrossRef]
- Youssef, A.; Hrynevich, A.; Fladeland, L.; Balles, A.; Groll, J.; Dalton, P.D.; Zabler, S. The impact of melt electrowritten scaffold design on porosity determined by x-ray microtomography. Tissue Eng. Part C Methods 2019, 25, 367–379. [Google Scholar] [CrossRef] [Green Version]
- Ginzberg, M.B.; Kafri, R.; Kirschner, M. On being the right (cell) size. Science 2015, 348, 1245075. [Google Scholar] [CrossRef] [PubMed]
- Romano, A.C.; Espana, E.M.; Yoo, S.H.; Budak, M.T.; Wolosin, J.M.; Tseng, S.C. Different cell sizes in human limbal and central corneal basal epithelia measured by confocal microscopy and flow cytometry. Investig. Ophthalmol. Vis. Sci. 2003, 44, 5125–5129. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Lian, M.; Wu, Q.; Qiao, Z.; Sun, B.; Dai, K. Effect of Pore Size on Cell Behavior Using Melt Electrowritten Scaffolds. Front. Bioeng. Biotechnol. 2021, 9, 495. [Google Scholar] [CrossRef]
- Zhang, J.; Yin, H.-M.; Hsiao, B.S.; Zhong, G.-J.; Li, Z.-M. Biodegradable poly (lactic acid)/hydroxyl apatite 3D porous scaffolds using high-pressure molding and salt leaching. J. Mater. Sci. 2014, 49, 1648–1658. [Google Scholar] [CrossRef]
- Kishore, V.; Alapan, Y.; Iyer, R.; Mclay, R.; Gurkan, U.A. Application of hydrogels in ocular tissue engineering. In Gels Handbook: Fundamentals, Properties and Applications Volume 2: Applications of Hydrogels in Regenerative Medicine; World Scientific: Singapore, 2016; pp. 137–164. [Google Scholar]
- Ratner, B.D.; Castner, D.G. Surface Modification of Polymeric Biomaterials; Springer: New York, NY, USA, 1997. [Google Scholar]
- Mahdavi, S.S.; Abdekhodaie, M.J.; Mashayekhan, S.; Baradaran-Rafii, A.; Djalilian, A.R. Bioengineering approaches for corneal regenerative medicine. Tissue Eng. Regen. Med. 2020, 17, 567–593. [Google Scholar] [CrossRef]
- Echeverria Molina, M.I.; Malollari, K.G.; Komvopoulos, K. Design challenges in polymeric scaffolds for tissue engineering. Front. Bioeng. Biotechnol. 2021, 9, 617141. [Google Scholar] [CrossRef]
- Kumar, P.; Pandit, A.; Zeugolis, D.I. Progress in corneal stromal repair: From tissue grafts and biomaterials to modular supramolecular tissue-like assemblies. Adv. Mater. 2016, 28, 5381–5399. [Google Scholar] [CrossRef]
- Bernardo, M.P.; da Silva, B.C.; Hamouda, A.E.; de Toledo, M.A.; Schalla, C.; Rütten, S.; Goetzke, R.; Mattoso, L.H.; Zenke, M.; Sechi, A. PLA/Hydroxyapatite scaffolds exhibit in vitro immunological inertness and promote robust osteogenic differentiation of human mesenchymal stem cells without osteogenic stimuli. Sci. Rep. 2022, 12, 2333. [Google Scholar] [CrossRef]
- Ahearne, M.; Fernández-Pérez, J.; Masterton, S.; Madden, P.W.; Bhattacharjee, P. Designing scaffolds for corneal regeneration. Adv. Funct. Mater. 2020, 30, 1908996. [Google Scholar] [CrossRef]
- Di Iorio, E.; Ferrari, S.; Fasolo, A.; Böhm, E.; Ponzin, D.; Barbaro, V. Techniques for culture and assessment of limbal stem cell grafts. Ocul. Surf. 2010, 8, 146–153. [Google Scholar] [CrossRef]
- Rama, P.; Matuska, S.; Paganoni, G.; Spinelli, A.; De Luca, M.; Pellegrini, G. Limbal stem-cell therapy and long-term corneal regeneration. N. Engl. J. Med. 2010, 363, 147–155. [Google Scholar] [CrossRef]
- Schlötzer-Schrehardt, U.; Kruse, F.E. Identification and characterization of limbal stem cells. Exp. Eye Res. 2005, 81, 247–264. [Google Scholar] [CrossRef]
- Donate, R.; Monzón, M.; Alemán-Domínguez, M.E. Additive manufacturing of PLA-based scaffolds intended for bone regeneration and strategies to improve their biological properties. e-Polymers 2020, 20, 571–599. [Google Scholar] [CrossRef]
- Hunter, S.R. Cellular Attachment on Poly (Lactic Acid) for Use in Tissue Engineering. Master’s Thesis, Western Michigan University, Kalamazoo, MI, USA, 2020. [Google Scholar]
- Ashwin, B.; Abinaya, B.; Prasith, T.; Chandran, S.V.; Yadav, L.R.; Vairamani, M.; Patil, S.; Selvamurugan, N. 3D-poly (lactic acid) scaffolds coated with gelatin and mucic acid for bone tissue engineering. Int. J. Biol. Macromol. 2020, 162, 523–532. [Google Scholar] [CrossRef]
- Swetha, S.; Balagangadharan, K.; Lavanya, K.; Selvamurugan, N. Three-dimensional-poly (lactic acid) scaffolds coated with gelatin/magnesium-doped nano-hydroxyapatite for bone tissue engineering. Biotechnol. J. 2021, 16, 2100282. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, S.F.; Mehrabi, M.; Ehterami, A.; Gharravi, A.M.; Bitaraf, F.S.; Salehi, M. In-vitro and in-vivo studies of PLA/PCL/gelatin composite scaffold containing ascorbic acid for bone regeneration. J. Drug Deliv. Sci. Technol. 2021, 61, 102077. [Google Scholar] [CrossRef]
- Nooeaid, P.; Chuysinuan, P.; Pengsuk, C.; Dechtrirat, D.; Lirdprapamongkol, K.; Techasakul, S.; Svasti, J. Polylactic acid microparticles embedded porous gelatin scaffolds with multifunctional properties for soft tissue engineering. J. Sci. Adv. Mater. Devices 2020, 5, 337–345. [Google Scholar] [CrossRef]
- Chen, H.; Zhang, H.; Shen, Y.; Dai, X.; Wang, X.; Deng, K.; Long, X.; Liu, L.; Zhang, X.; Li, Y. Instant in-situ tissue repair by biodegradable PLA/Gelatin nanofibrous membrane using a 3D printed handheld electrospinning device. Front. Bioeng. Biotechnol. 2021, 9, 684105. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, P.; Ramachandran, C.; Sefat, F.; Mariappan, I.; Johnson, C.; McKean, R.; Hannah, M.; Sangwan, V.S.; Claeyssens, F.; Ryan, A.J. Simplifying corneal surface regeneration using a biodegradable synthetic membrane and limbal tissue explants. Biomaterials 2013, 34, 5088–5106. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, C.; Deshpande, P.; Ortega, I.; Sefat, F.; McKean, R.; Srivastava, M.; MacNeil, S.; Basu, S.; Sangwan, V.S. Proof-of-concept study of electrospun PLGA membrane in the treatment of limbal stem cell deficiency. BMJ Open Ophthalmol. 2021, 6, e000762. [Google Scholar] [CrossRef]
- Baradaran-Rafii, A.; Biazar, E.; Heidari-Keshel, S. Cellular response of limbal stem cells on PHBV/gelatin nanofibrous scaffold for ocular epithelial regeneration. Int. J. Polym. Mater. Polym. Biomater. 2015, 64, 879–887. [Google Scholar] [CrossRef]
- Tominac Trcin, M.; Zdraveva, E.; Dolenec, T.; Vrgoč Zimić, I.; Bujić Mihica, M.; Batarilo, I.; Dekaris, I.; Blažević, V.; Slivac, I.; Holjevac Grgurić, T. Poly (ε-caprolactone) titanium dioxide and cefuroxime antimicrobial scaffolds for cultivation of human limbal stem cells. Polymers 2020, 12, 1758. [Google Scholar] [CrossRef]


















| Scaffold | LSC Sample 1 | LSC Sample 2 | LSC Sample 3 | |||
|---|---|---|---|---|---|---|
| No. of Cells | % of Cells Viability | No. of Cells | % of Cells Viability | No. of Cells | % of Cells Viability | |
| PLA | 1.1 × 106 | 98 | 1.2 × 106 | 99 | 1.05 × 106 | 99 |
| PLA/silk fibroin | 2.7 × 106 | 98 | 2.9 × 106 | 98 | 2.2 × 106 | 99 |
| PLA/gelatin | 1.9 × 106 | 98 | 2.3 × 106 | 98 | 1.75 × 106 | 99 |
| Scaffold | LSC Sample 1 | LSC Sample 2 | LSC Sample 3 | |
|---|---|---|---|---|
| % p63 + LSCs | PLA | 97.3 | 93.7 | 73.0 |
| PLA/silk fibroin | 98.7 | 90.5 | 71.6 | |
| PLA/gelatin | 98.2 | 92.9 | 74.7 | |
| % CK3 + LSCs | PLA | 33.1 | 41.0 | 17.2 |
| PLA/silk fibroin | 32.9 | 42.7 | 19.8 | |
| PLA/gelatin | 35.3 | 40.1 | 20.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zdraveva, E.; Bendelja, K.; Bočkor, L.; Dolenec, T.; Mijović, B. Detection of Limbal Stem Cells Adhered to Melt Electrospun Silk Fibroin and Gelatin-Modified Polylactic Acid Scaffolds. Polymers 2023, 15, 777. https://doi.org/10.3390/polym15030777
Zdraveva E, Bendelja K, Bočkor L, Dolenec T, Mijović B. Detection of Limbal Stem Cells Adhered to Melt Electrospun Silk Fibroin and Gelatin-Modified Polylactic Acid Scaffolds. Polymers. 2023; 15(3):777. https://doi.org/10.3390/polym15030777
Chicago/Turabian StyleZdraveva, Emilija, Krešo Bendelja, Luka Bočkor, Tamara Dolenec, and Budimir Mijović. 2023. "Detection of Limbal Stem Cells Adhered to Melt Electrospun Silk Fibroin and Gelatin-Modified Polylactic Acid Scaffolds" Polymers 15, no. 3: 777. https://doi.org/10.3390/polym15030777
APA StyleZdraveva, E., Bendelja, K., Bočkor, L., Dolenec, T., & Mijović, B. (2023). Detection of Limbal Stem Cells Adhered to Melt Electrospun Silk Fibroin and Gelatin-Modified Polylactic Acid Scaffolds. Polymers, 15(3), 777. https://doi.org/10.3390/polym15030777








