Towards a Customizable, SLA 3D-Printed Biliary Stent: Optimizing a Commercially Available Resin and Predicting Stent Behavior with Accurate In Silico Testing
Abstract
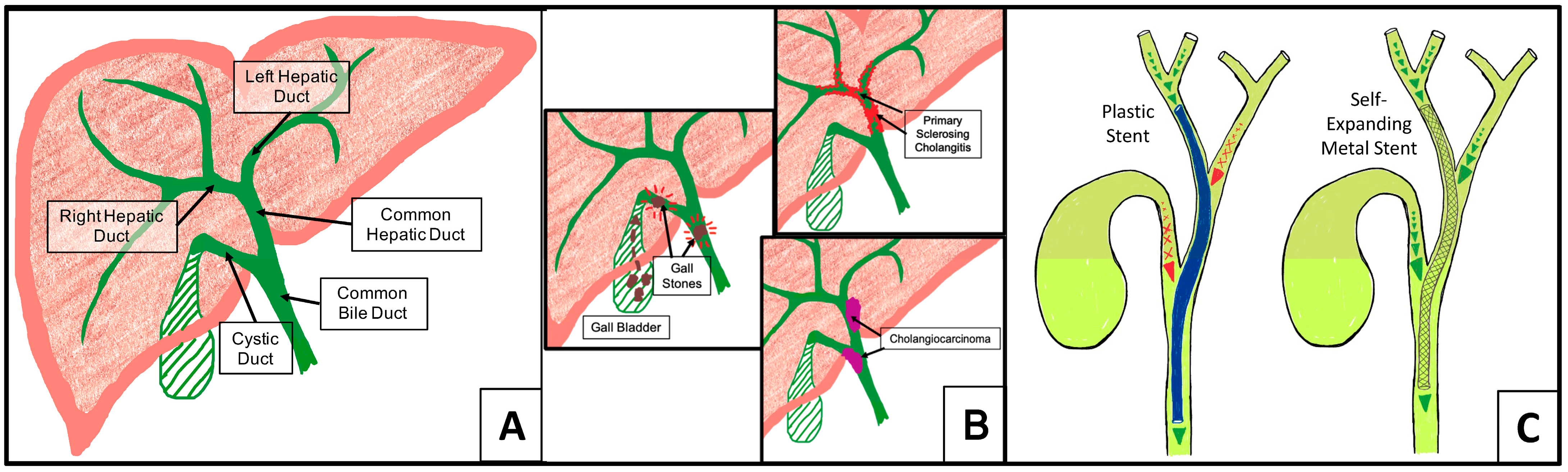
1. Introduction
2. Materials and Methods
2.1. Three-Dimensional Printing, Post-Processing, and Sterilization
2.2. Mechanical Characterization
2.3. Cytotoxicity Testing
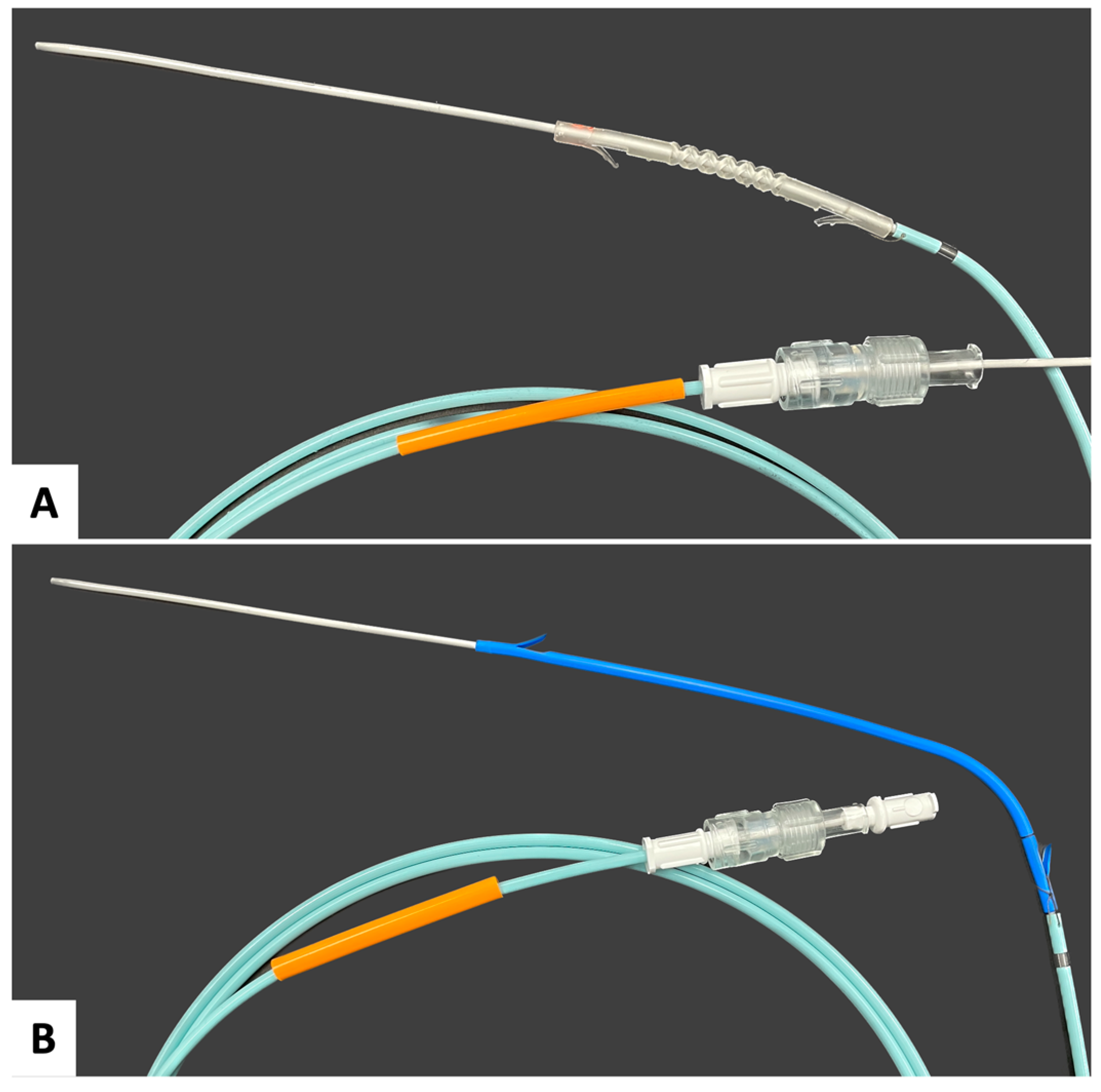
2.4. Biliary Stent Designs
2.5. Computational Fluid Dynamics (CFD) of Bile Flow with Biliary Stents
2.6. Optimization of FD Stent Printing Orientation
2.7. In Silico Stent 3-Point Bend Testing
2.8. Experimental Stent 3-Point Bend Testing
3. Results
3.1. Effects of Post-Processing Modifications and Sterilization on Formlabs Durable Polymer Mechanical Properties
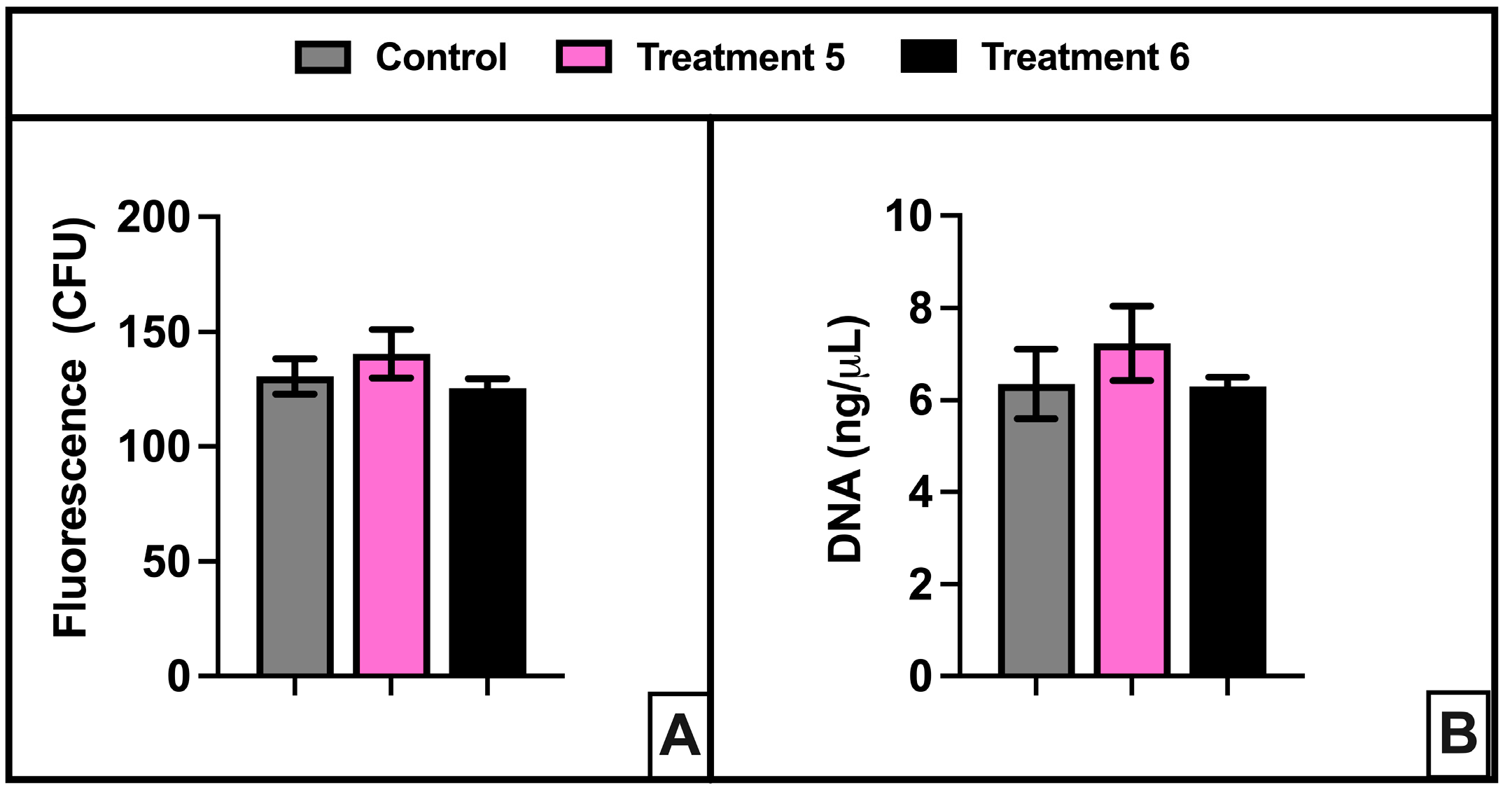
3.2. Cytotoxicity Testing of FD with Modified Post-Processing Parameters and Autoclave Sterilization
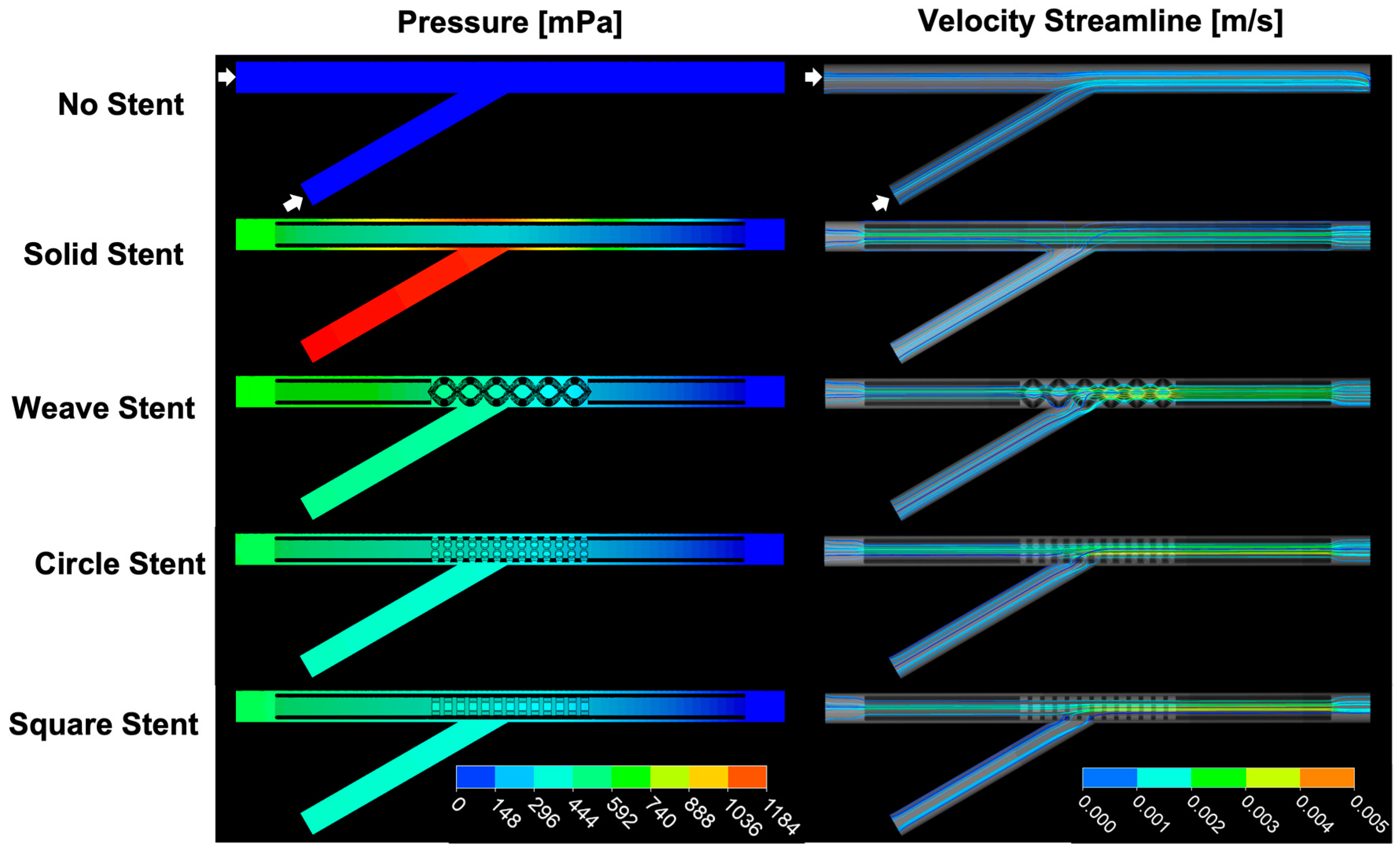
3.3. CFD Model of Bile Flow at an EHBD Juncture with and without Stents
3.4. Effects of Print Orientation on Print Platform
3.5. Accuracy of In Silico Stent 3-Point Bend Tests
3.6. In Silico Predicted Peak Stresses in FD-Treatment 6 Stents
4. Discussion
4.1. Commercial SLA Resin Feasibility
4.2. Design and Fabricate an SLA 3D-Printed Stent That Permits Bile Flow at a Duct Junction and Could Be Placed during ERCP
4.3. Accurate In Silico Stent 3-Point Bend Test
5. Conclusions
6. Patents
- Thomas, J. L.; Patel, S. G. Patmas Weave Stent. US D987,826 S, 30 May 2023.
- Thomas, J. L.; Patel, S. G. Patmas Weave Stent. EU 008 883 797-0001.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Banales, J.M.; Huebert, R.C.; Karlsen, T.; Strazzabosco, M.; LaRusso, N.F.; Gores, G.J. Cholangiocyte Pathobiology. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 269–281. [Google Scholar] [CrossRef] [PubMed]
- Chung, B.K.; Karlsen, T.H.; Folseraas, T. Cholangiocytes in the Pathogenesis of Primary Sclerosing Cholangitis and Development of Cholangiocarcinoma. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2018, 1864, 1390–1400. [Google Scholar] [CrossRef] [PubMed]
- Karlsen, T.H.; Folseraas, T.; Thorburn, D.; Vesterhus, M. Primary Sclerosing Cholangitis—A Comprehensive Review. J. Hepatol. 2017, 67, 1298–1323. [Google Scholar] [CrossRef] [PubMed]
- Ceci, L.; Han, Y.; Krutsinger, K.; Baiocchi, L.; Wu, N.; Kundu, D.; Kyritsi, K.; Zhou, T.; Gaudio, E.; Francis, H.; et al. Gallstone and Gallbladder Disease: Biliary Tract and Cholangiopathies. In Comprehensive Physiology; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2023; pp. 4909–4943. ISBN 978-0-470-65071-4. [Google Scholar]
- Elmunzer, B.J.; Maranki, J.L.; Gómez, V.; Tavakkoli, A.; Sauer, B.G.; Limketkai, B.N.; Brennan, E.A.; Attridge, E.M.; Brigham, T.J.; Wang, A.Y. ACG Clinical Guideline: Diagnosis and Management of Biliary Strictures. Am. J. Gastroenterol. 2023, 118, 405–426. [Google Scholar] [CrossRef] [PubMed]
- Dumonceau, J.-M.; Tringali, A.; Papanikolaou, I.; Blero, D.; Mangiavillano, B.; Schmidt, A.; Vanbiervliet, G.; Costamagna, G.; Devière, J.; García-Cano, J.; et al. Endoscopic Biliary Stenting: Indications, Choice of Stents, and Results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline—Updated October 2017. Endoscopy 2018, 50, 910–930. [Google Scholar] [CrossRef] [PubMed]
- Nakai, Y.; Isayama, H.; Wang, H.; Rerknimitr, R.; Khor, C.; Yasuda, I.; Kogure, H.; Moon, J.H.; Lau, J.; Lakhtakia, S.; et al. International Consensus Statements for Endoscopic Management of Distal Biliary Stricture. J. Gastroenterol. Hepatol. 2020, 35, 967–979. [Google Scholar] [CrossRef] [PubMed]
- Rushbrook, S.M.; Kendall, T.J.; Zen, Y.; Albazaz, R.; Manoharan, P.; Pereira, S.P.; Sturgess, R.; Davidson, B.R.; Malik, H.Z.; Manas, D.; et al. British Society of Gastroenterology Guidelines for the Diagnosis and Management of Cholangiocarcinoma. Gut 2024, 73, 16–46. [Google Scholar] [CrossRef] [PubMed]
- Chazouilleres, O.; Beuers, U.; Bergquist, A.; Karlsen, T.H.; Levy, C.; Samyn, M.; Schramm, C.; Trauner, M. EASL Clinical Practice Guidelines on Sclerosing Cholangitis. J. Hepatol. 2022, 77, 761–806. [Google Scholar] [CrossRef]
- Dinescu, B. The Perfect Biliary Plastic Stent: The Search Goes On. Ann. Gastroenterol. 2023, 36, 490–496. [Google Scholar] [CrossRef]
- Chiba, M.; Kato, M.; Kinoshita, Y.; Shimamoto, N.; Tomita, Y.; Abe, T.; Kawahara, Y.; Koyama, S.; Kanazawa, K.; Takakura, K.; et al. Best Period to Replace or Change Plastic Stents with Self-Expandable Metallic Stents Using Multivariate Competing Risk Regression Analysis. Sci. Rep. 2020, 10, 13080. [Google Scholar] [CrossRef]
- Emara, M.H.; Ahmed, M.H.; Mohammed, A.S.; Radwan, M.I.; Mahros, A.M. Biliary Stent Migration: Why, How, and What? Eur. J. Gastroenterol. Hepatol. 2021, 33, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Song, G.; Zhao, H.Q.; Liu, Q.; Fan, Z. A Review on Biodegradable Biliary Stents: Materials and Future Trends. Bioact. Mater. 2022, 17, 488–495. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Obando, J.V.; Bhatt, A.; Bucobo, J.C.; Chen, D.; Copland, A.P.; Das, K.K.; Girotra, M.; Kahn, A.; Krishnan, K.; et al. Biliary and Pancreatic Stents. iGIE 2023, 2, 240–253. [Google Scholar] [CrossRef]
- Yang, K.; Sun, W.; Cui, L.; Zou, Y.; Wen, C.; Zeng, R. Advances in Functional Coatings on Biliary Stents. Regen. Biomater. 2024, 11, rbae001. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-R.; Yang, S.W.; Kwon, C.-I.; Kim, K.S.; Park, S.H.; Jang, M.J.; Kim, G.H.; Sung, M.J.; Kim, G.; Son, J.S.; et al. Anti-Fibrotic and Anti-Stricture Effects of Biodegradable Biliary Stents Braided with Dexamethasone-Impregnated Sheath/Core Structured Monofilaments. Acta Biomater. 2024, 178, 137–146. [Google Scholar] [CrossRef]
- Xiao, J.-B.; Weng, J.-Y.; Hu, Y.-Y.; Deng, G.-L.; Wan, X.-J. Feasibility and Efficacy Evaluation of Metallic Biliary Stents Eluting Gemcitabine and Cisplatin for Extrahepatic Cholangiocarcinoma. World J. Gastroenterol. 2020, 26, 4589–4606. [Google Scholar] [CrossRef]
- Yun, D.; Kim, H.-O.; Son, H.Y.; Choi, Y.; Noh, I.; Lim, J.-W.; Kim, J.; Chun, H.; Park, G.; Lee, D.K.; et al. Stent Containing CD44-Targeting Polymeric Prodrug Nanoparticles That Release Paclitaxel and Gemcitabine in a Time Interval-Controlled Manner for Synergistic Human Biliary Cancer Therapy. J. Mater. Chem. B 2017, 5, 6317–6324. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Kang, D.H.; Jeong, Y.-I.; Chung, C.W.; Kim, C.H.; Kwak, T.W.; Lee, H.M. Preclinical Evaluation of Sorafenib-Eluting Stent for Suppression of Human Cholangiocarcinoma Cells. Int. J. Nanomed. 2013, 8, 1697–1711. [Google Scholar] [CrossRef] [PubMed]
- Shatzel, J. Drug Eluting Biliary Stents to Decrease Stent Failure Rates: A Review of the Literature. World J. Gastrointest. Endosc. 2016, 8, 77. [Google Scholar] [CrossRef]
- Jang, S.I.; Kim, J.-H.; You, J.W.; Rhee, K.; Lee, S.J.; Kim, H.G.; Han, J.; Shin, I.H.; Park, S.-H.; Lee, D.K. Efficacy of a Metallic Stent Covered with a Paclitaxel-Incorporated Membrane Versus a Covered Metal Stent for Malignant Biliary Obstruction: A Prospective Comparative Study. Dig. Dis. Sci. 2013, 58, 865–871. [Google Scholar] [CrossRef]
- Jang, S.I.; Lee, K.T.; Lee, S.H.; Kim, Y.-T.; Jeong, S.; Lee, D.H.; Choi, J.S.; Lee, D. Sa1342 Efficacy of a Paclitaxel-Eluting Biliary Metal Stent Incorporated with Sodium Caprate Versus a Covered Metal Stent in Malignant Biliary Obstruction: A Prospective Randomized Comparative Study. Gastrointest. Endosc. 2018, 87, AB223. [Google Scholar] [CrossRef]
- Wang, W.; Luan, Z.; Shu, Z.; Xu, K.; Wang, T.; Liu, S.; Wu, X.; Liu, H.; Ye, S.; Dan, R.; et al. Biosynthetic Plastics as Tunable Elastic and Visible Stent with Shape-Memory to Treat Biliary Stricture. Adv. Sci. 2023, 10, 2303779. [Google Scholar] [CrossRef] [PubMed]
- Zeng, C.-H.; Liu, L.-L.; Zhu, H.-D.; Teng, G.-J. The Exploration of a Novel Biodegradable Drug-Eluting Biliary Stent: Preliminary Work. Cardiovasc. Interv. Radiol. 2021, 44, 1633–1642. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Yang, K.; Cheng, R.; Xiang, Y.; Yuan, T.; Cheng, Y.; Sarmento, B.; Cui, W. The Current Status of Biodegradable Stent to Treat Benign Luminal Disease. Mater. Today 2017, 20, 516–529. [Google Scholar] [CrossRef]
- Kim, J.H.; Ha, D.-H.; Han, E.S.; Choi, Y.; Koh, J.; Joo, I.; Kim, J.H.; Cho, D.-W.; Han, J.K. Feasibility and Safety of a Novel 3D-Printed Biodegradable Biliary Stent in an in Vivo Porcine Model: A Preliminary Study. Sci. Rep. 2022, 12, 15875. [Google Scholar] [CrossRef] [PubMed]
- Maieron, A.; Erhart, L.; Pramhofer, P.; Schöfl, R.; Spaun, G.; Steiner, E.; Wewalka, F.; Ziachehabi, A. Biodegradable Biliopancreatic Stents Could Help Conserve Health Care Resources during the COVID-19 Pandemic: An Observational Multicenter Study. Dig. Liver Dis. 2023, 55, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Plastic vs Biodegradable Pancreatic Stent in Post-ERCP Pancreatitis Prevention. Available online: https://www.clinicaltrials.gov/study/NCT05307861?term=NCT05307861&rank=1 (accessed on 1 June 2023).
- UNITY-B A Prospective, Multicentric, Single-Arm Study to Evaluate the Safety and Efficacy of the UNITY-B Biodegradable Balloon-Expandable Biliary Stent System in Subjects with Biliary Strictures. Available online: https://www.centerwatch.com/clinical-trials/listings/NCT04929821/unity-b-a-prospective-multicentric-single-arm-study-to-evaluate-the-safety-and-efficacy-of-the-unity-b-biodegradable-balloon-expandable-biliary-stent-system-in-subjects-with-biliary-strictures?phase=3&country=India&city=Hyderabad (accessed on 5 May 2024).
- ISO 10993; Biological Evaluation of Medical Devices. International Organization for Standardization: Geneva, Switzerland, 2018.
- ISO 13485; Medical Devices—Quality Management Systems—Requirements for Regulatory Purposes. International Organization for Standardization: Geneva, Switzerland, 2016.
- ISO 14971; Medical Devices—Application of Risk Management to Medical Devices. International Organization for Standardization: Geneva, Switzerland, 2019.
- FDA Technical Considerations for Additive Manufactured Medical Devices. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/technical-considerations-additive-manufactured-medical-devices (accessed on 5 October 2023).
- FDA 3D Printing of Medical Devices. Available online: https://www.fda.gov/medical-devices/products-and-medical-procedures/3d-printing-medical-devices (accessed on 5 October 2023).
- Boyer, C.J.; Boktor, M.; Samant, H.; White, L.A.; Wang, Y.; Ballard, D.H.; Huebert, R.C.; Woerner, J.E.; Ghali, G.E.; Alexander, J.S. 3D Printing for Bio-Synthetic Biliary Stents. Bioengineering 2019, 6, 16. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Won, D.-S.; Park, S.; Park, Y.; Kim, J.W.; Han, G.; Na, Y.; Kang, M.-H.; Kim, S.B.; Kang, H.; et al. 3D-Printed Versatile Biliary Stents with Nanoengineered Surface for Anti-Hyperplasia and Antibiofilm Formation. Bioact. Mater. 2024, 37, 172–190. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.A.; Rajabi, M.; Sudhir Sali, S. Additive Manufacturing Potential for Medical Devices and Technology. Curr. Opin. Chem. Eng. 2020, 28, 127–133. [Google Scholar] [CrossRef]
- Bao, Y.; Paunović, N.; Leroux, J. Challenges and Opportunities in 3D Printing of Biodegradable Medical Devices by Emerging Photopolymerization Techniques. Adv. Funct. Mater. 2022, 32, 2109864. [Google Scholar] [CrossRef]
- Levato, R.; Dudaryeva, O.; Garciamendez-Mijares, C.E.; Kirkpatrick, B.E.; Rizzo, R.; Schimelman, J.; Anseth, K.S.; Chen, S.; Zenobi-Wong, M.; Zhang, Y.S. Light-Based Vat-Polymerization Bioprinting. Nat. Rev. Methods Prim. 2023, 3, 47. [Google Scholar] [CrossRef]
- Kim, G.-T.; Go, H.-B.; Yu, J.-H.; Yang, S.-Y.; Kim, K.-M.; Choi, S.-H.; Kwon, J.-S. Cytotoxicity, Colour Stability and Dimensional Accuracy of 3D Printing Resin with Three Different Photoinitiators. Polymers 2022, 14, 979. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, A.; Jin, J. Photopolymerization in 3D Printing. ACS Appl. Polym. Mater. 2019, 1, 593–611. [Google Scholar] [CrossRef]
- Stansbury, J.W. Curing Dental Resins and Composites by Photopolymerization. J. Esthet. Restor. Dent. 2000, 12, 300–308. [Google Scholar] [CrossRef] [PubMed]
- 3D Systems Dental Materials. Available online: https://www.3dsystems.com/materials/dental (accessed on 2 May 2024).
- Liqcreate Dental. Available online: https://www.liqcreate.com/products/#dental (accessed on 2 May 2024).
- Formlabs High-Accuracy 3D Printing Materials for Dental Labs and Practices. Available online: https://dental.formlabs.com/materials/ (accessed on 2 May 2024).
- pro3Dure Dental Polymers. Available online: https://www.pro3dure.com/en/products/dental/polymers/ (accessed on 2 May 2024).
- Biocompatible 3D Resins. Available online: https://www.3dresyns.com/collections/ultra-safe-biocompatible-3d-resins (accessed on 2 May 2024).
- Guttridge, C.; Shannon, A.; O’Sullivan, A.; O’Sullivan, K.J.; O’Sullivan, L.W. Biocompatible 3D Printing Resins for Medical Applications: A Review of Marketed Intended Use, Biocompatibility Certification, and Post-Processing Guidance. Ann. 3d Print. Med. 2022, 5, 100044. [Google Scholar] [CrossRef]
- ASTM D1708-06a; Standard Test Method for Tensile Properties of Plastics by Use of Microtensile Specimens. ANSI: Washington, DC, USA, 2010.
- ANSI/AAMI/ISO 10993-12: 2007; Biological Evaluation of Medical Devices. Part 12. Sample Preparation and Reference Material. Association for the Advancement of Medical Instrumentation: Arlington, VA, USA, 2007.
- Thomas, J.; Patel, S. Patmas Weave Stent. D987826, 30 May 2023. [Google Scholar]
- Al-Atabi, M.; Ooi, R.C.; Luo, X.Y.; Chin, S.B.; Bird, N.C. Computational Analysis of the Flow of Bile in Human Cystic Duct. Med. Eng. Phys. 2012, 34, 1177–1183. [Google Scholar] [CrossRef] [PubMed]
- Boyer, J.L. Bile Formation and Secretion. In Comprehensive Physiology; Terjung, R., Ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2013; p. c120027. ISBN 978-0-470-65071-4. [Google Scholar]
- Reinhart, W.H.; Näf, G.; Werth, B. Viscosity of Human Bile Sampled from the Common Bile Duct. Clin. Hemorheol. Microcirc. 2010, 44, 177–182. [Google Scholar] [CrossRef]
- Luo, X.; Li, W.; Bird, N.; Chin, S.B.; Hill, N.; Johnson, A.G. On the Mechanical Behavior of the Human Biliary System. World J. Gastroenterol. 2007, 13, 1384. [Google Scholar] [CrossRef] [PubMed]
- National Center for Health Statistics: Body Measurements. Available online: https://www.cdc.gov/nchs/fastats/body-measurements.htm (accessed on 25 July 2020).
- ASTM D790; Standard Test Methods for Flexural Properties of Unreinforced and Reinforced Plastics and Electrical Insulating Materials. ASTM: West Conshohocken, PA, USA, 2017.
- ASTM F2606-08(2021); ASTM Standard Guide for Three-Point Bending of Balloon-Expandable Vascular Stents and Stent Systems. ASTM: West Conshohocken, PA, USA, 2021.
- Biomed Durable Resin. Available online: https://formlabs.com/store/materials/biomed-durable-resin/ (accessed on 1 March 2024).
- Baghaei, M.; Kavian, M.; Ghodsi, S.; Razavi, S.E. Numerical Investigation of Bile Secretion and Pressure Rise in Obstructed Human Common Bile Duct. J. Appl. Fluid Mech. 2021, 14, 275–286. [Google Scholar] [CrossRef]
- Huang, H.; Zhang, B.; Zhong, J.; Han, G.; Zhang, J.; Zhou, H.; Mao, T.; Liu, Y. The Behavior between Fluid and Structure from Coupling System of Bile, Bile Duct, and Polydioxanone Biliary Stent: A Numerical Method. Med. Eng. Phys. 2023, 113, 103966. [Google Scholar] [CrossRef]
- Beltrán, M.A.; Beltrán, A.A. Common Bile Duct Pressure in Patients with and without Cholelithiasis: A Case-control Study. J. Hepato. Biliary Pancreat. 2021, 28, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Gregg, J.A.; Carr-Locke, D.L. Endoscopic Pancreatic and Biliary Manometry in Pancreatic, Biliary, and Papillary Disease, and after Endoscopic Sphincterotomy and Surgical Sphincteroplasty. Gut 1984, 25, 1247–1254. [Google Scholar] [CrossRef] [PubMed]
- Csendes, A.; Kruse, A.; Funch-Jensen, P.; Øster, M.J.; Ørnsholt, J.; Amdrup, E. Pressure Measurements in the Biliary and Pancreatic Duct Systems in Controls and in Patients with Gallstones, Previous Cholecystectomy, or Common Bile Duct Stones. Gastroenterology 1979, 77, 1203–1210. [Google Scholar] [CrossRef]
- Kuchumov, A.G.; Nyashin, Y.I.; Samarcev, V.A.; Gavrilov, V.A. Modelling of the Pathological Bile Flow in the Duct with a Calculus. Acta Bioeng. Biomech. 2013, 15, 9–17. [Google Scholar] [CrossRef]
- Jüngst, D. Mucin and Phospholipids Determine Viscosity of Gallbladder Bile in Patients with Gallstones. World J. Gastroenterol. 2001, 7, 203. [Google Scholar] [CrossRef] [PubMed]
- Klasztorny, M.; Nycz, D.; Labuda, R. Modelling, Simulation and Experimental Validation of Bend Tests on GFRP Laminate Beam and Plate Specimens. Compos. Struct. 2018, 184, 604–612. [Google Scholar] [CrossRef]
- Seifoori, S.; Mirzaei, M.; Afjoland, H. Experimental and FE Analysis for Accurate Measurement of Deflection in CFRP and GFRP Laminates under Bending. Measurement 2020, 153, 107445. [Google Scholar] [CrossRef]
- Thomas, J.; Patel, S.; Troop, L.; Guru, R.; Faist, N.; Bellott, B.J.; Esterlen, B.A. 3D Printed Model of Extrahepatic Biliary Ducts for Biliary Stent Testing. Materials 2020, 13, 4788. [Google Scholar] [CrossRef] [PubMed]
- Formlabs Resin Family: Tough and Durable. Available online: https://formlabs.com/materials/tough-durable/ (accessed on 7 December 2019).
- Panta, G.; Richardson, A.K.; Shaw, I.C. Effectiveness of Autoclaving in Sterilizing Reusable Medical Devices in Healthcare Facilities. J. Infect. Dev. Ctries 2019, 13, 858–864. [Google Scholar] [CrossRef]
- Rutala, W.A.; Weber, D.J. Disinfection and Sterilization in Health Care Facilities. Infect. Dis. Clin. N. Am. 2021, 35, 575–607. [Google Scholar] [CrossRef]
- US FDA Sterilization for Medical Devices. Available online: https://www.fda.gov/medical-devices/general-hospital-devices-and-supplies/sterilization-medical-devices#:~:text=Medical%20devices%20are%20sterilized%20in,acid%2C%20and%20nitrogen%20dioxide) (accessed on 17 April 2021).
- Bayarsaikhan, E.; Lim, J.-H.; Shin, S.-H.; Park, K.-H.; Park, Y.-B.; Lee, J.-H.; Kim, J.-E. Effects of Postcuring Temperature on the Mechanical Properties and Biocompatibility of Three-Dimensional Printed Dental Resin Material. Polymers 2021, 13, 1180. [Google Scholar] [CrossRef] [PubMed]
- Tipnis, N.P.; Burgess, D.J. Sterilization of Implantable Polymer-Based Medical Devices: A Review. Int. J. Pharm. 2018, 544, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Anastasio, R.; Peerbooms, W.; Cardinaels, R.; Van Breemen, L.C.A. Characterization of Ultraviolet-Cured Methacrylate Networks: From Photopolymerization to Ultimate Mechanical Properties. Macromolecules 2019, 52, 9220–9231. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Cao, S.; Msallem, B.; Kunz, C.; Brantner, P.; Honigmann, P.; Thieringer, F.M. Effects of Steam Sterilization on 3D Printed Biocompatible Resin Materials for Surgical Guides—An Accuracy Assessment Study. J. Clin. Med. 2020, 9, 1506. [Google Scholar] [CrossRef] [PubMed]
- Guerra, A.J.; Cano, P.; Rabionet, M.; Puig, T.; Ciurana, J. Effects of Different Sterilization Processes on the Properties of a Novel 3D-Printed Polycaprolactone Stent. Polym. Adv. Technol. 2018, 29, 2327–2335. [Google Scholar] [CrossRef]
- BioMed Durable Resin V1/V1.1 (Compliance and Technical Documents). Available online: https://support.formlabs.com/s/article/BioMed-Durable-Resin-V1-Compliance-and-technical-documents?language=en_US (accessed on 13 August 2023).
- Formlabs Safety Data Sheet Durable Resin. Available online: https://asset.dynamism.com/media/catalog/product/pdf/Formlabs_Durable_v2_SDS.pdf (accessed on 4 May 2023).
- Qumseya, B.J.; Jamil, L.H.; Elmunzer, B.J.; Riaz, A.; Ceppa, E.P.; Thosani, N.C.; Buxbaum, J.L.; Storm, A.C.; Sawhney, M.S.; Pawa, S.; et al. ASGE Guideline on the Role of Endoscopy in the Management of Malignant Hilar Obstruction. Gastrointest. Endosc. 2021, 94, 222–234.e22. [Google Scholar] [CrossRef] [PubMed]
- Adler; Byrne Endoscopic Stenting for Malignant Biliary Obstruction. Available online: https://www.uptodate.com/contents/endoscopic-stenting-for-malignant-biliary-obstruction (accessed on 8 May 2024).
- Herczeg, C.K.; Song, J. Sterilization of Polymeric Implants: Challenges and Opportunities. ACS Appl. Bio Mater. 2022, 5, 5077–5088. [Google Scholar] [CrossRef] [PubMed]
- Brooks, N.W.; Duckett, R.A.; Ward, I.M. Investigation into Double Yield Points in Polyethylene. Polymer 1992, 33, 1872–1880. [Google Scholar] [CrossRef]
- Patlazhan, S.; Remond, Y. Structural Mechanics of Semicrystalline Polymers Prior to the Yield Point: A Review. J. Mater. Sci. 2012, 47, 6749–6767. [Google Scholar] [CrossRef]
- Seguela, R.; Rietsch, F. Double Yield Point in Polyethylene under Tensile Loading. J. Mater. Sci. Lett. 1990, 9, 46–47. [Google Scholar] [CrossRef]

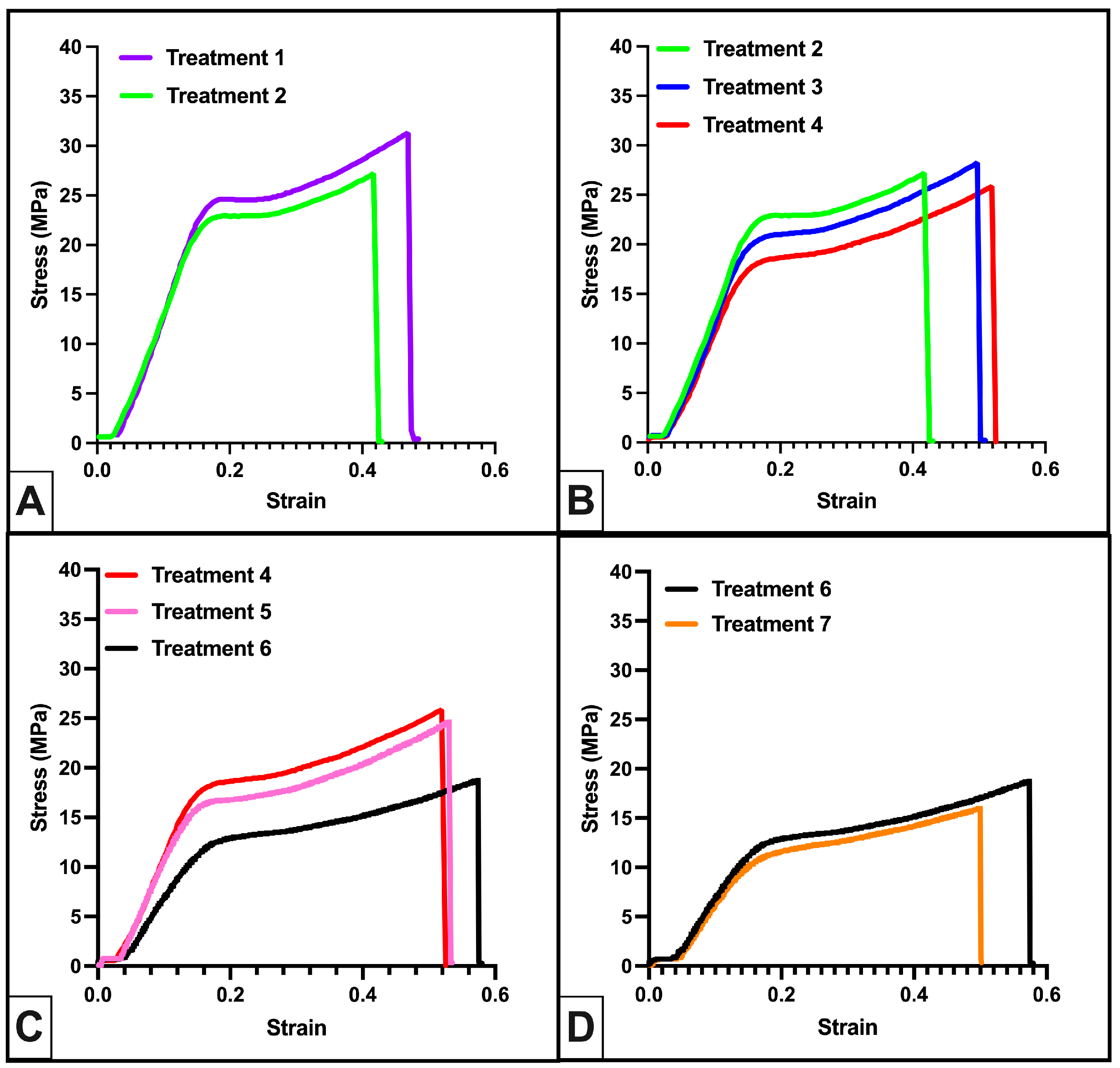

| Treatment | IPA Wash (min) | Air Dry (min) | UV Post-Cure Time (min) | UV Post-Cure Temperature (°C) | Autoclave Cycle | Autoclave Time (min) |
|---|---|---|---|---|---|---|
| 1 | 20 | 30–60 | 60 | 60 | - | - |
| 2 | 20 | 30–60 | 60 | 60 | gravity | 60 |
| 3 | 20 | 30–60 | 60 | 50 | gravity | 60 |
| 4 | 20 | 30–60 | 60 | 40 | gravity | 60 |
| 5 | 20 | 30–60 | 10 | 40 | gravity | 60 |
| 6 | 60 | 30–60 | 10 | 40 | gravity | 60 |
| 7 | 60 | 30–60 | 10 | 40 | gravity | 30 |
| Treatment | Elastic Modulus (MPa) | Yield Stress (MPa) | Peak Stress (MPa) |
|---|---|---|---|
| 1 | 191.38 ± 8.72 | 21.43 ± 1.28 | 34.37 ± 3.76 |
| 2 | 177 ± 10.67 | 19.51 ± 1.32 | 27.64 ± 2.19 |
| 3 | 185.7 ± 10.77 | 17.97 ± 1.08 | 26.93 ± 2.83 |
| 4 | 161.57 ± 12.16 | 16.63 ± 1.42 | 25.77 ± 2.08 |
| 5 | 148.99 ± 11.09 | 14.00 ± 0.66 | 22.81 ± 1.11 |
| 6 | 104.89 ± 12.6 | 12.06 ± 0.38 | 18.95 ± 2.01 |
| 7 | 108.38 ± 8.81 | 9.96 ± 0.79 | 18.37 ± 1.71 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cordista, V.; Patel, S.; Lawson, R.; Lee, G.; Verheyen, M.; Westbrook, A.; Shelton, N.; Sapkota, P.; Zabala Valencia, I.; Gaddam, C.; et al. Towards a Customizable, SLA 3D-Printed Biliary Stent: Optimizing a Commercially Available Resin and Predicting Stent Behavior with Accurate In Silico Testing. Polymers 2024, 16, 1978. https://doi.org/10.3390/polym16141978
Cordista V, Patel S, Lawson R, Lee G, Verheyen M, Westbrook A, Shelton N, Sapkota P, Zabala Valencia I, Gaddam C, et al. Towards a Customizable, SLA 3D-Printed Biliary Stent: Optimizing a Commercially Available Resin and Predicting Stent Behavior with Accurate In Silico Testing. Polymers. 2024; 16(14):1978. https://doi.org/10.3390/polym16141978
Chicago/Turabian StyleCordista, Victoria, Sagar Patel, Rebecca Lawson, Gunhee Lee, Morgan Verheyen, Ainsley Westbrook, Nathan Shelton, Prakriti Sapkota, Isabella Zabala Valencia, Cynthia Gaddam, and et al. 2024. "Towards a Customizable, SLA 3D-Printed Biliary Stent: Optimizing a Commercially Available Resin and Predicting Stent Behavior with Accurate In Silico Testing" Polymers 16, no. 14: 1978. https://doi.org/10.3390/polym16141978
APA StyleCordista, V., Patel, S., Lawson, R., Lee, G., Verheyen, M., Westbrook, A., Shelton, N., Sapkota, P., Zabala Valencia, I., Gaddam, C., & Thomas, J. (2024). Towards a Customizable, SLA 3D-Printed Biliary Stent: Optimizing a Commercially Available Resin and Predicting Stent Behavior with Accurate In Silico Testing. Polymers, 16(14), 1978. https://doi.org/10.3390/polym16141978











