Synthesis of Cellulose-Based Hydrogel—Nanocomposites for Medical Applications
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Hydrogel
2.3. Y2O3 NPs Loaded to Hydrogels
2.4. Fourier Transform Infrared Spectroscopy (FTIR)
2.5. X-ray Powder Diffraction
2.6. Morphology
2.7. Antimicrobial Activity
2.8. Determination of Ultimate Tensile Strength, Young’s Modulus, and Percent of Elongation at Break
- -
- Fmax is the maximum force (N) needed to pull the sample apart.
- -
- A is the cross-sectional area (mm2), A = thickness × width.
- -
- Li is the initial length of the film sample.
- -
- L is the film elongation at the moment of rupture.
2.9. Measurement of Friction Coefficient
2.10. Swelling Percentage
3. Results and Discussion
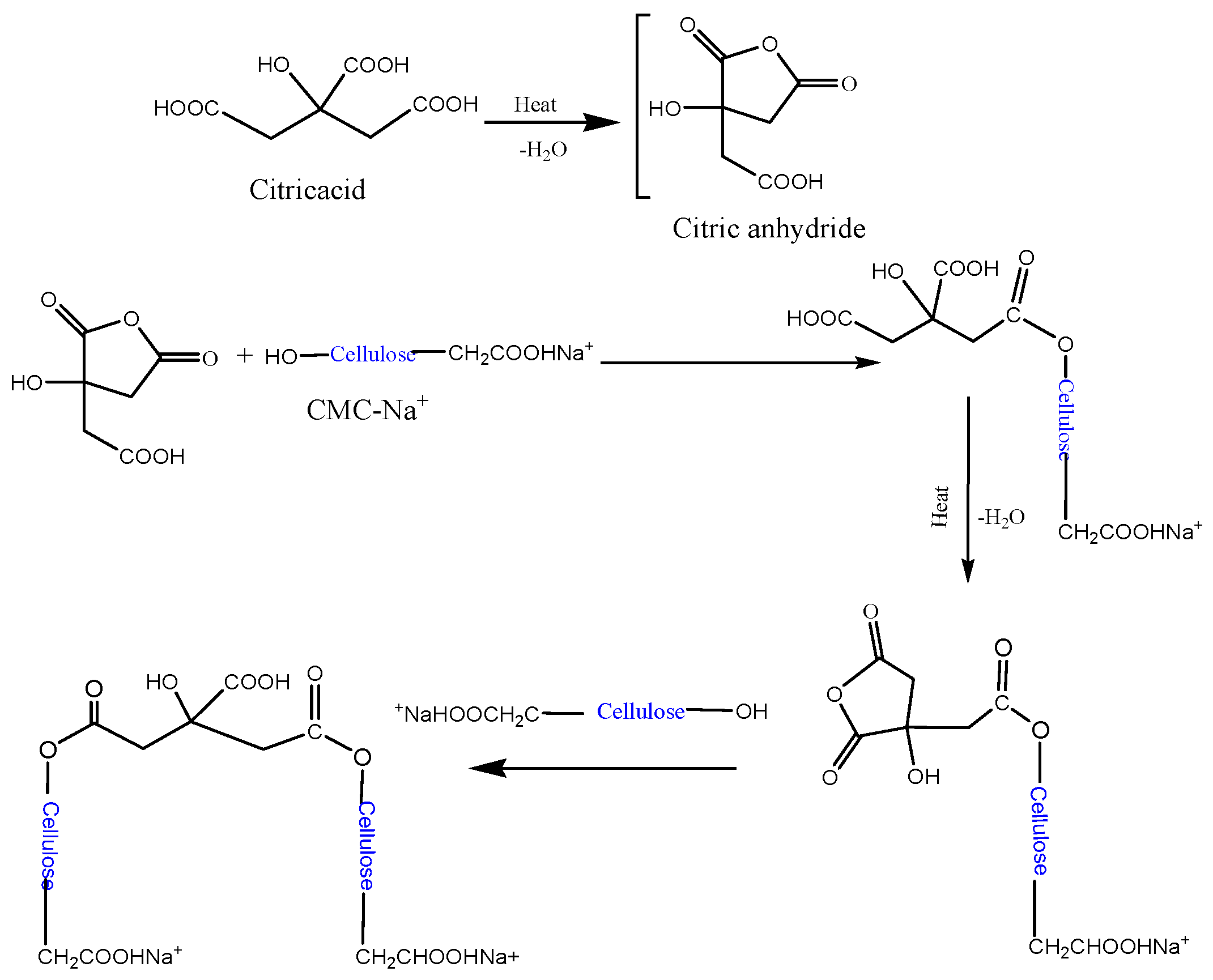
3.1. Formation Mechanism
3.2. FTIR Spectrum
3.3. X-ray Powder Diffraction (XRD)
3.4. Antimicrobial Activity
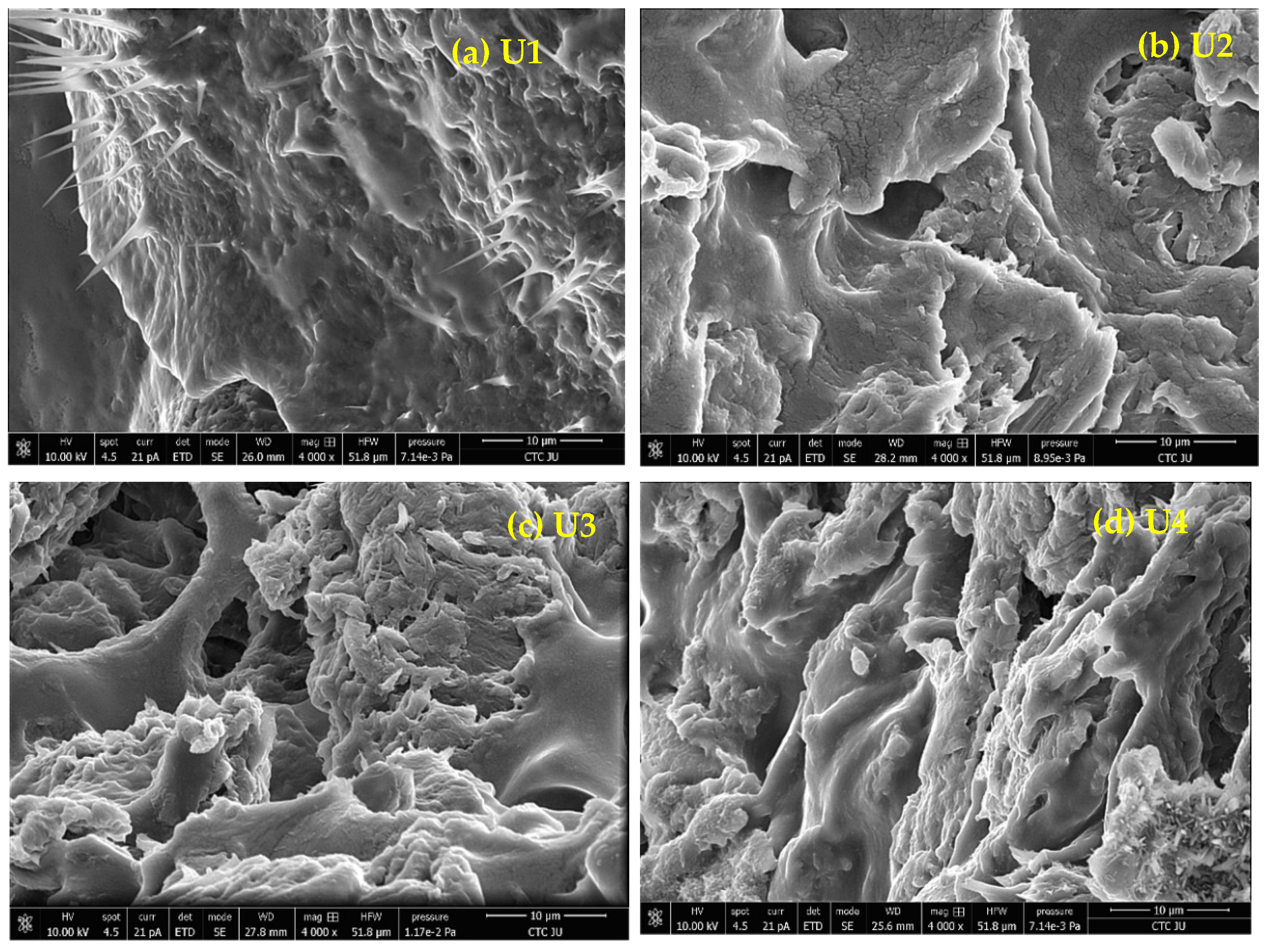
3.5. Morphology
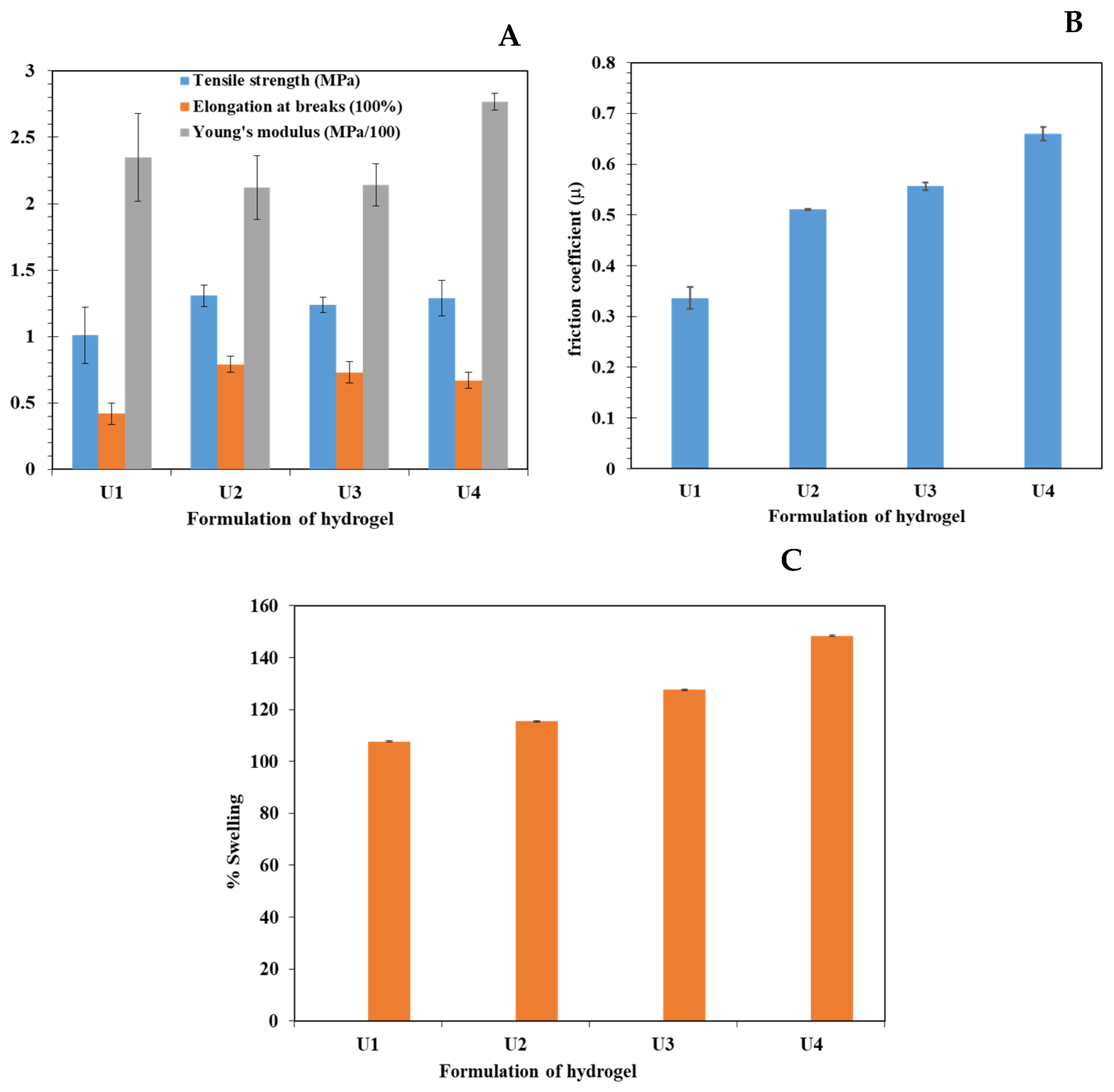
3.6. Mechanical Properties
3.7. Friction Coefficient
3.8. Swelling
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Annabi, N.; Zhang, Y.N.; Assmann, A.; Sani, E.S.; Cheng, G.; Lassaletta, A.D.; Vegh, A.; Dehghani, B.; Ruiz-Esparza, G.U.; Wang, X.; et al. Engineering a highly elastic human protein-based sealant for surgical applications. Sci. Transl. Med. 2017, 9, eaai7466. [Google Scholar] [CrossRef] [PubMed]
- Varaprasad, K.; Raghavendra, G.M.; Jayaramudu, T.; Yallapu, M.M.; Sadiku, R. A mini review on hydrogels classification and recent developments in miscellaneous applications. Mater. Sci. Eng. C 2017, 79, 958–971. [Google Scholar] [CrossRef] [PubMed]
- Gaharwar, A.K.; Peppas, N.A.; Khademhosseini, A. Nanocomposite hydrogels for biomedical applications. Biotechnol. Bioeng. 2014, 111, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Dacrory, S.; Abou-Yousef, H.; Abou-Zeid, R.E.; Kamel, S.; Abdel-Aziz, M.S.; Elbadry, M. Preparation and characterization of eco-friendly carboxymethyl cellulose antimicrobial nanocomposite hydrogels. J. Renew. Mater. 2018, 6, 536–547. [Google Scholar] [CrossRef]
- Klemm, D.; Heublein, B.; Fink, H.P.; Bohn, A. Cellulose: Fascinating biopolymer and sustainable raw material. Angew. Chem. Int. Ed. 2005, 44, 3358–3393. [Google Scholar] [CrossRef]
- Wang, J.; Sun, Y.; Liu, X.; Kang, Y.; Cao, W.; Ye, J.; Gao, C. An antibacterial and anti-oxidant hydrogel containing hyperbranched poly-L-lysine and tea polyphenols accelerates healing of infected wound. Biomater. Adv. 2024, 157, 213755. [Google Scholar] [CrossRef]
- Chang, C.; Zhang, L. Cellulose-based hydrogels: Present status and application prospects. Carbohydr. Polym. 2011, 84, 40–53. [Google Scholar] [CrossRef]
- Tarawneh, O.; Hammad, A.M.; Mahfouz, H.A.; Hamadneh, L.; Hamed, R.; Hamadneh, I.; Al-Assi, A.R. Development of Mucoadhesive Cellulose Derivatives Based Films for the Treatment of Vaginal Candidiasis. Cellul. Chem. Technol. 2023, 57, 117–124. [Google Scholar] [CrossRef]
- Tarawneh, O.; Hamadneh, I.; Huwaitat, R.; Al-Assi, A.R.; El Madani, A. Characterization of Chlorhexidine-Impregnated Cellulose-Based Hydrogel Films Intended for the Treatment of Periodontitis. BioMed Res. Int. 2021, 9853977. [Google Scholar] [CrossRef]
- Nezhad-Mokhtari, P.; Akrami-Hasan-Kohal, M.; Ghorbani, M. An injectable chitosan-based hydrogel scaffold containing gold nanoparticles for tissue engineering applications. Int. J. Biol. Macromol. 2020, 154, 198–205. [Google Scholar] [CrossRef]
- Mahmoud, N.N.; Hikmat, S.; Ghith, D.A.; Hajeer, M.; Hamadneh, L.; Qattan, D.; Khalil, E.A. Gold nanoparticles loaded into polymeric hydrogel for wound healing in rats: Effect of nanoparticles’ shape and surface modification. Int. J. Pharm. 2019, 565, 174–186. [Google Scholar] [CrossRef] [PubMed]
- El Achaby, M.; El Miri, N.; Hannache, H.; Gmouh, S.; Ben Youcef, H.; Aboulkas, A. Production of cellulose nanocrystals from vine shoots and their use for the development of nanocomposite materials. Int. J. Biol. Macromol. 2018, 117, 592–600. [Google Scholar] [CrossRef] [PubMed]
- Janmohammadi, M.; Nazemi, Z.; Salehi, A.; Seyfoori, A.; John, J.V.; Nourbakhsh, M.S.; Akbari, M. Cellulose-based composite scaffolds for bone tissue engineering and localized drug delivery. Bioact. Mater. 2023, 20, 137–163. [Google Scholar] [CrossRef]
- Courtenay, J.C.; Johns, M.A.; Gale Beck, F.; Deneke, C.; Lanzoni, E.M.; Costa, C.A.; Scott, J.L.; Sharma, R.I. Surface-modified cellulose scaffolds for tissue engineering. Cellulose 2017, 24, 253–267. [Google Scholar] [CrossRef]
- Tarawneh, O.; Al-Assi, A.R.; Hamed, R.; Sunoqrot, S.; Hasan, L.; Al-Sheikh, I.; Al-Qirim, R.; Alhusban, A.A.; Naser, W. Development and characterization of k-carrageenan platforms as periodontal intra-pocket films Trop. J. Pharm. Res. 2019, 18, 1791–1798. [Google Scholar] [CrossRef]
- Ahmed, A.Y.; Ayad, D.M.; Youssef, A.M.; Abdelaal, M.Y. Preparation and Evaluation of PANI/PVA/Cu Bionanocomposite Hydrogel via Green Route. Egypt. J. Chem. 2024, 67, 533–542. [Google Scholar] [CrossRef]
- Esser, V.M.; Elefson, D.E. Experiences with the Kirby-Bauer method of antibiotic susceptibility testing. Am. J. Clin. Pathol. 1970, 54, 193–198. [Google Scholar] [CrossRef]
- Salmon, J.H.; Rat, A.C.; Sellam, J.; Michel, M.; Eschard, J.P.; Guillemin, F.; Jolly, D.; Fautrel, B. Economic impact of lower-limb osteoarthritis worldwide: A systematic review of cost-of-illness studies. Osteoarthr. Cartil. 2016, 24, 1500–1508. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, M.J.; Ahamed, M.; Alrokayan, S.A.; Ramamoorthy, M.M.; Alaizeri, Z.M. High Surface Reactivity and Biocompatibility of Y2O3 NPs in Human MCF-7 Epithelial and HT-1080 Fibro-Blast Cells. Molecules 2020, 25, 1137. [Google Scholar] [CrossRef]
- Chawla, V.; Sharma, S.; Singh, Y. Yttrium Oxide Nanoparticle-Loaded, Self-Assembled Peptide Gel with Antibacterial, Anti-Inflammatory, and Proangiogenic Properties for Wound Healing. ACS Biomater. Sci. Eng. 2023, 9, 2647–2662. [Google Scholar] [CrossRef]
- Moriyama, A.; Takahashi, U.; Mizuno, Y.; Takahashi, J.; Horie, M.; Iwahashi, H. The truth of toxicity caused by yttrium oxide nanoparticles to yeast cells. J. Nanosci. Nanotechnol. 2019, 19, 5418–5425. [Google Scholar] [CrossRef] [PubMed]
- Haktaniyan, M.; Bradley, M. Polymers showing intrinsic antimicrobial activity. Chem. Soc. Rev. 2022, 51, 8584–8611. [Google Scholar] [CrossRef] [PubMed]


| Sample | S. auras ZOI (mm) | E. coli ZOI (mm) |
|---|---|---|
| U1 | 15.0 ± 0.1 | 12.0 ± 0.2 |
| U2 | 20.7 ± 0.1 | 18.0 ± 0.1 |
| U3 | 20.5 ± 0.2 | 20.7 ± 0.1 |
| U4 | 20.1 ± 0.1 | 20.5 ± 0.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Tarawneh, W.; Hamadneh, I.; Tarawneh, O.; Al Najdawi, A. Synthesis of Cellulose-Based Hydrogel—Nanocomposites for Medical Applications. Polymers 2024, 16, 2183. https://doi.org/10.3390/polym16152183
Al-Tarawneh W, Hamadneh I, Tarawneh O, Al Najdawi A. Synthesis of Cellulose-Based Hydrogel—Nanocomposites for Medical Applications. Polymers. 2024; 16(15):2183. https://doi.org/10.3390/polym16152183
Chicago/Turabian StyleAl-Tarawneh, Wala`a, Imad Hamadneh, Ola Tarawneh, and Ali Al Najdawi. 2024. "Synthesis of Cellulose-Based Hydrogel—Nanocomposites for Medical Applications" Polymers 16, no. 15: 2183. https://doi.org/10.3390/polym16152183
APA StyleAl-Tarawneh, W., Hamadneh, I., Tarawneh, O., & Al Najdawi, A. (2024). Synthesis of Cellulose-Based Hydrogel—Nanocomposites for Medical Applications. Polymers, 16(15), 2183. https://doi.org/10.3390/polym16152183






