Spatial Trueness Evaluation of 3D-Printed Dental Model Made of Photopolymer Resin: Use of Special Structurized Dental Model
Abstract
:1. Introduction
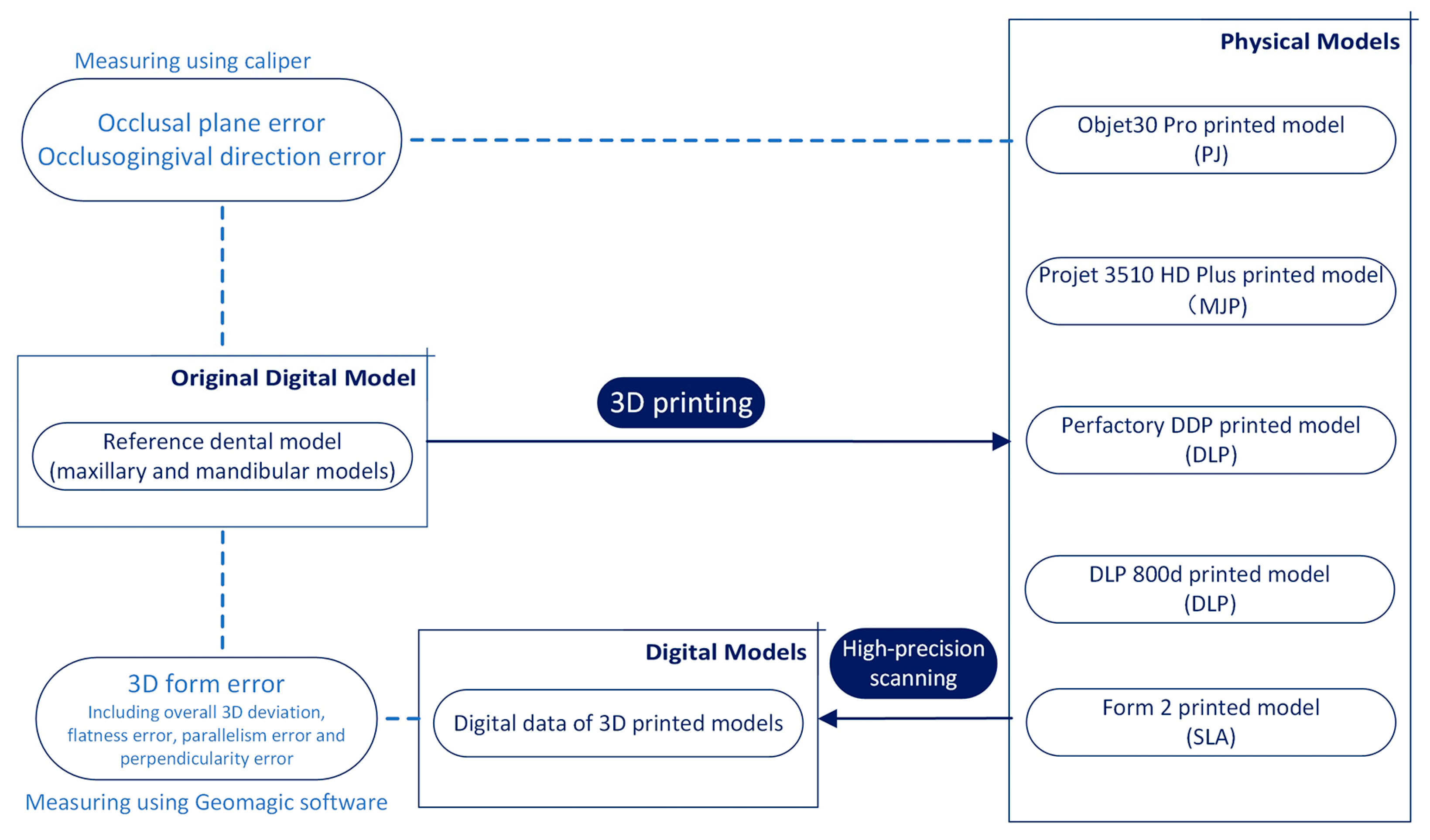
2. Materials and Methods
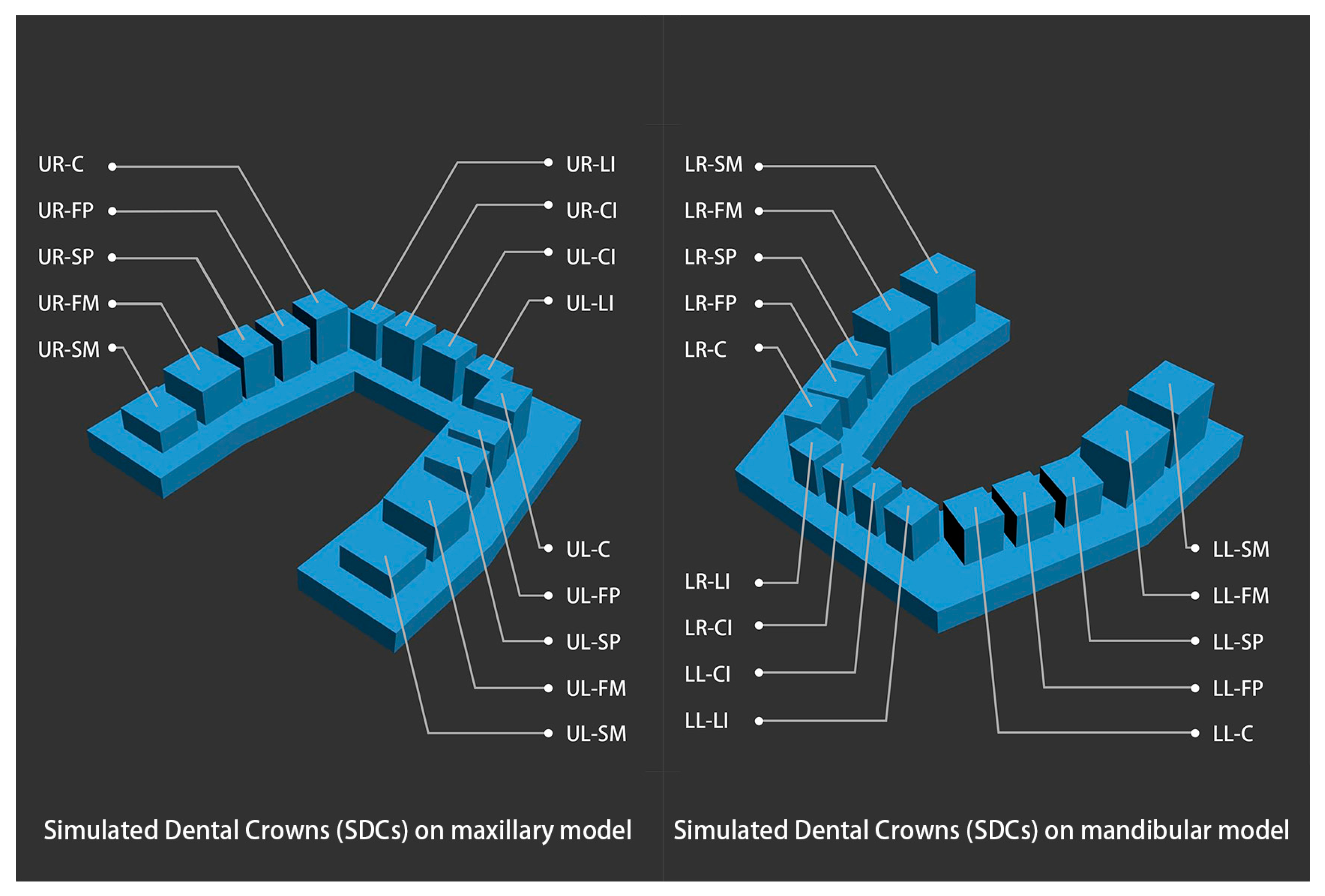
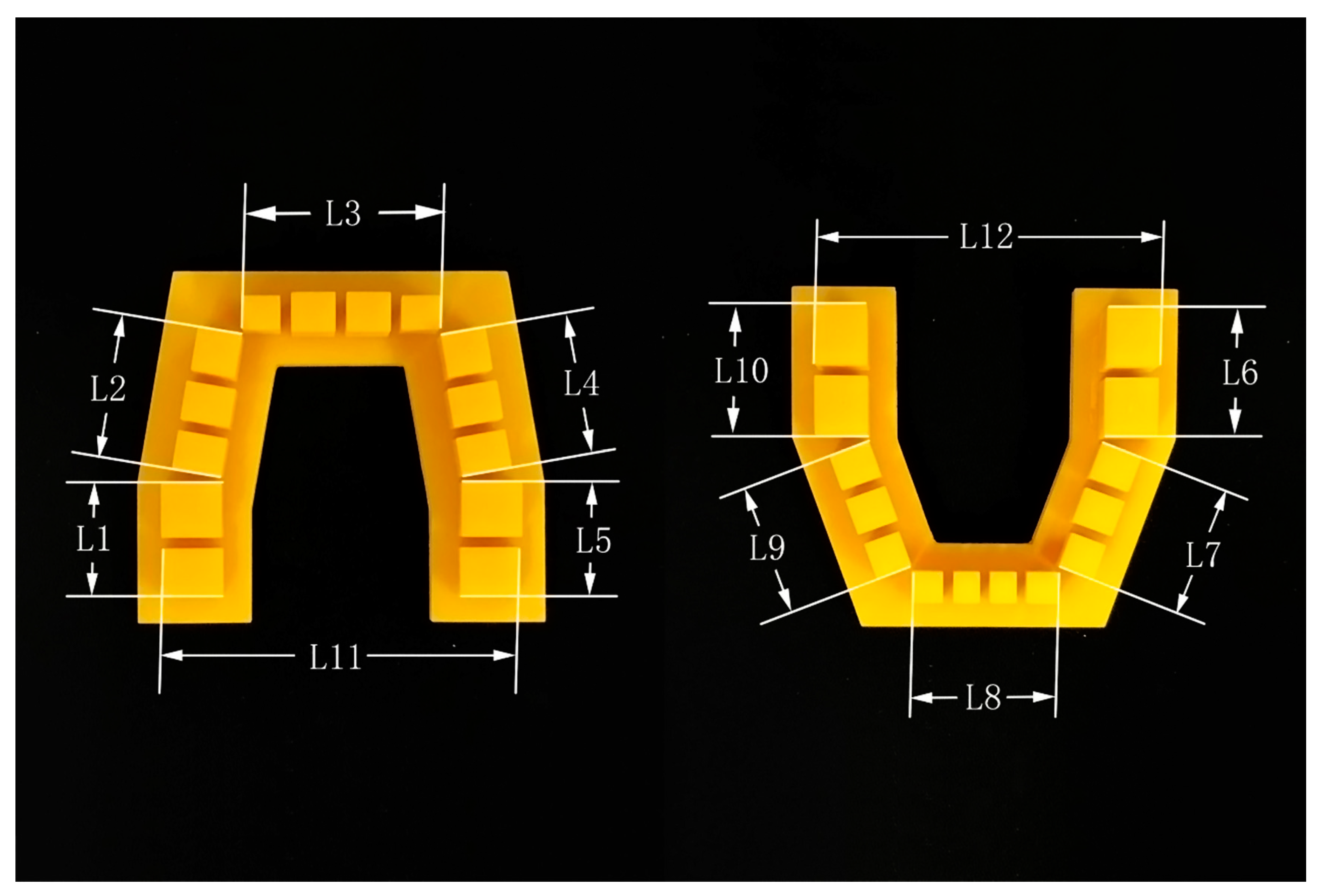
2.1. Establishment of the Structurized Dental Model
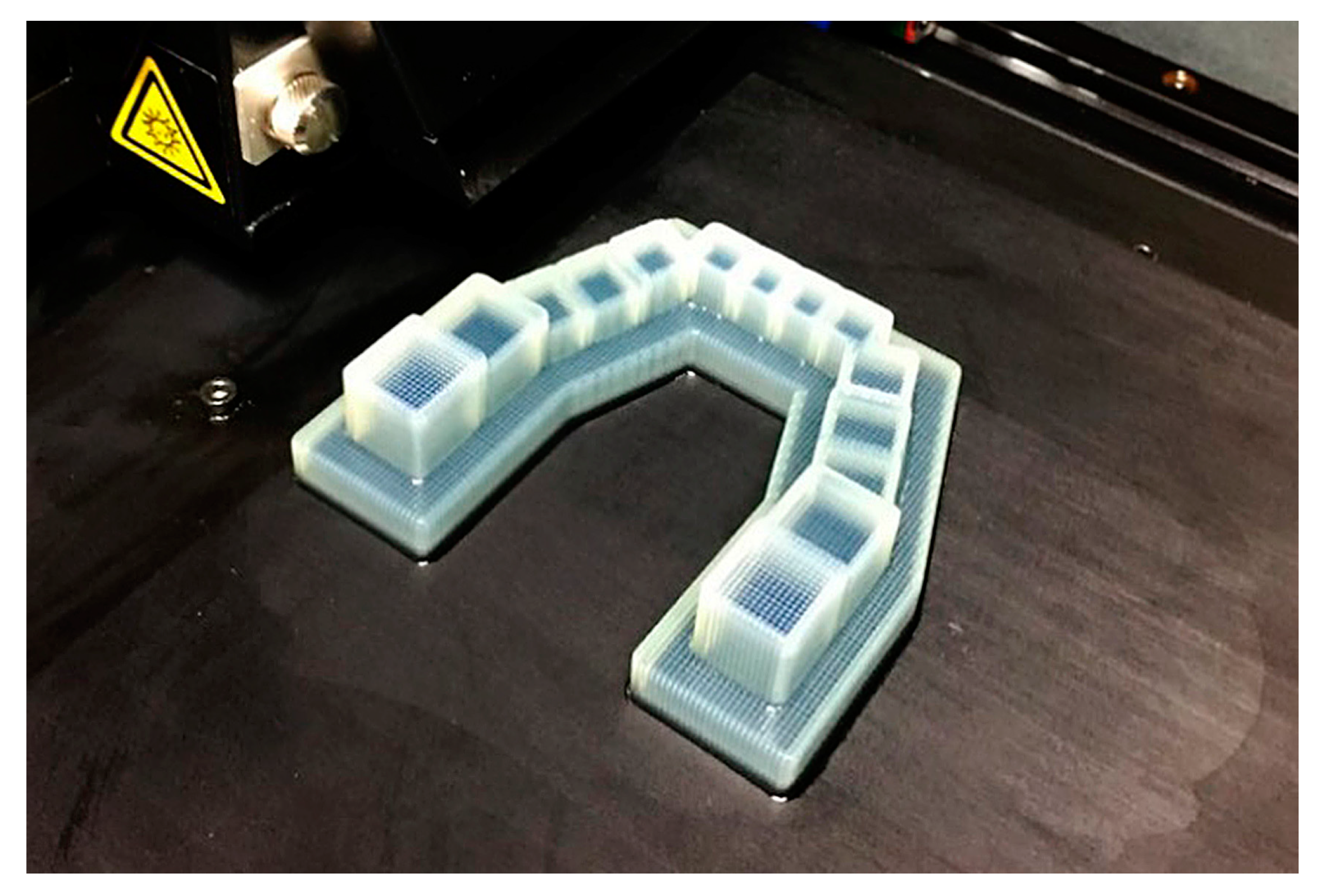
2.2. Fabrication of the 3D-Printed Structurized Dental Model
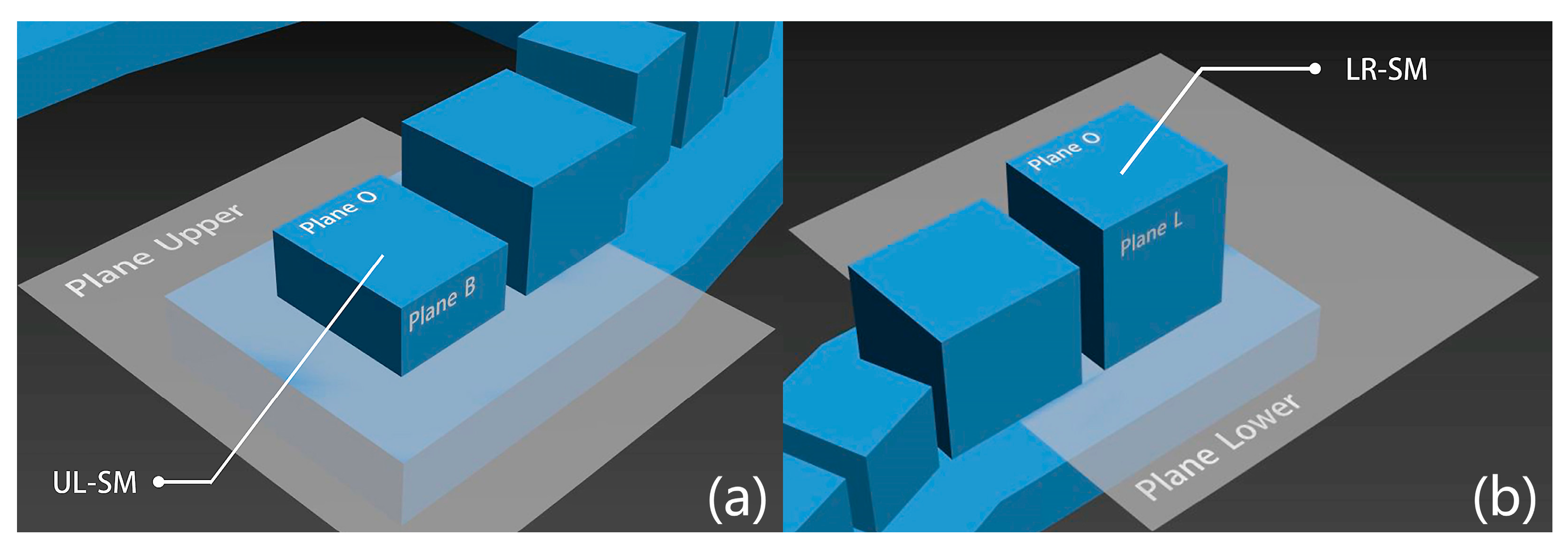
2.3. 3D Form Errors
2.4. Linear Dimensional Error
3. Results
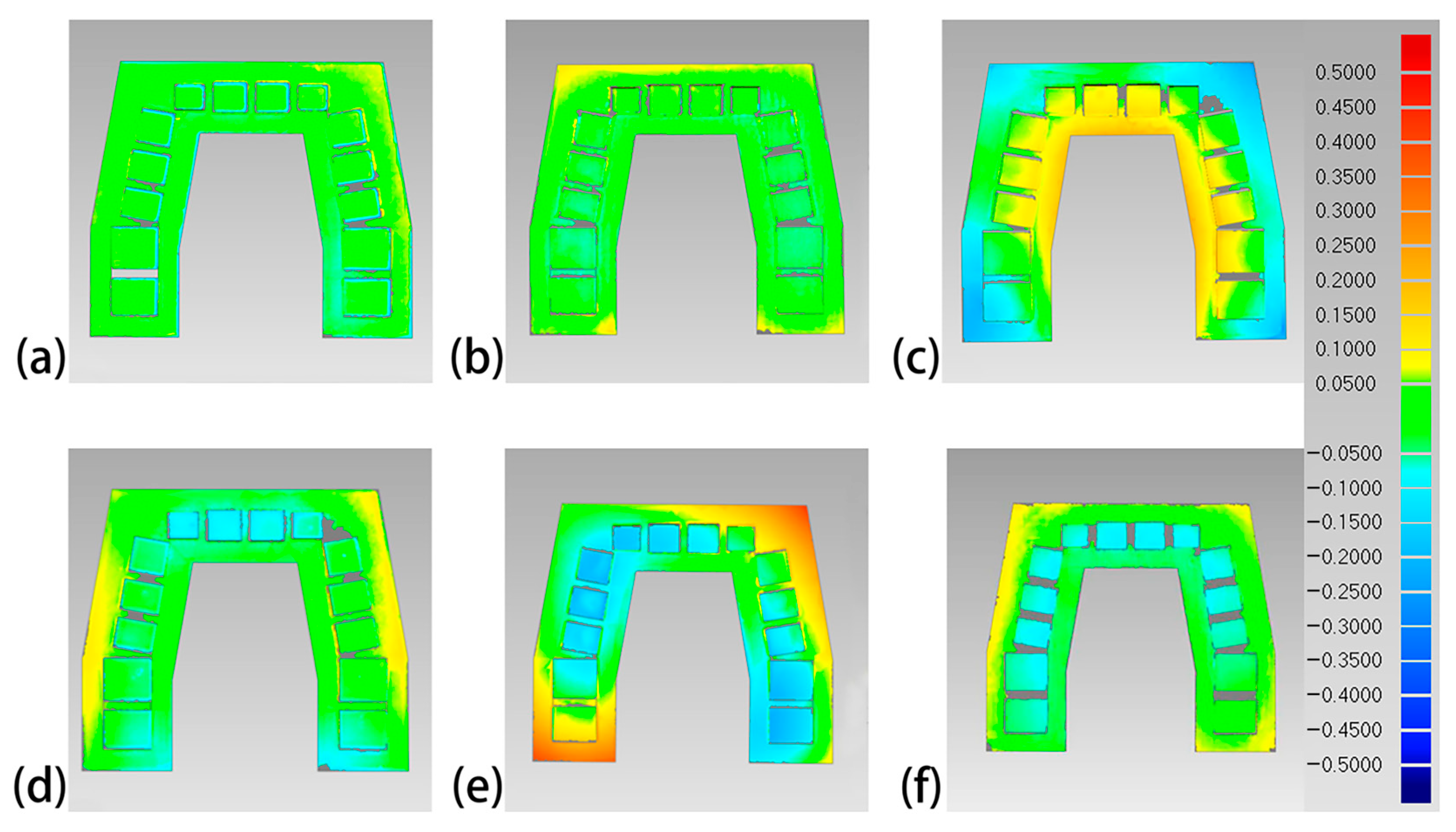
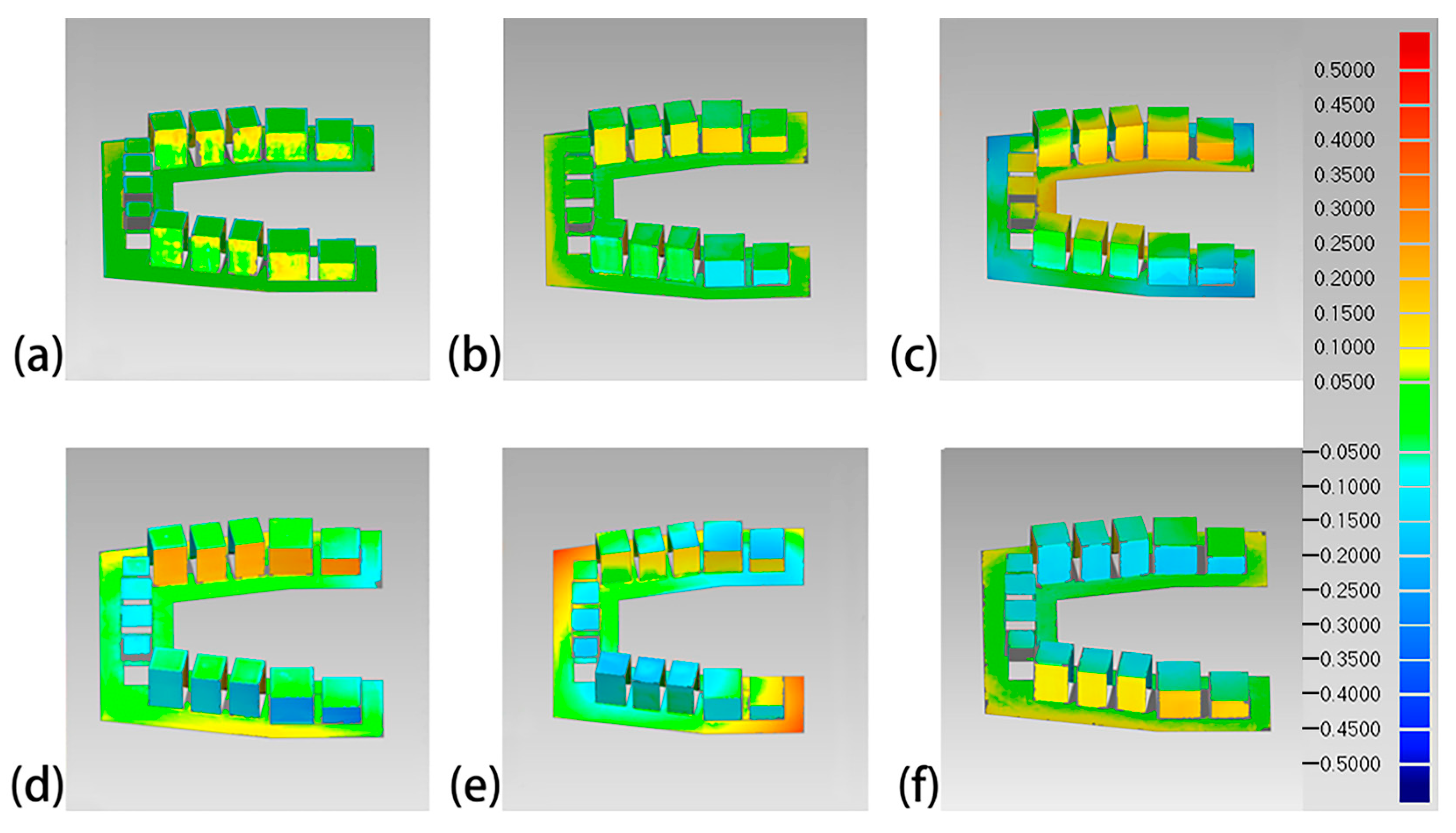
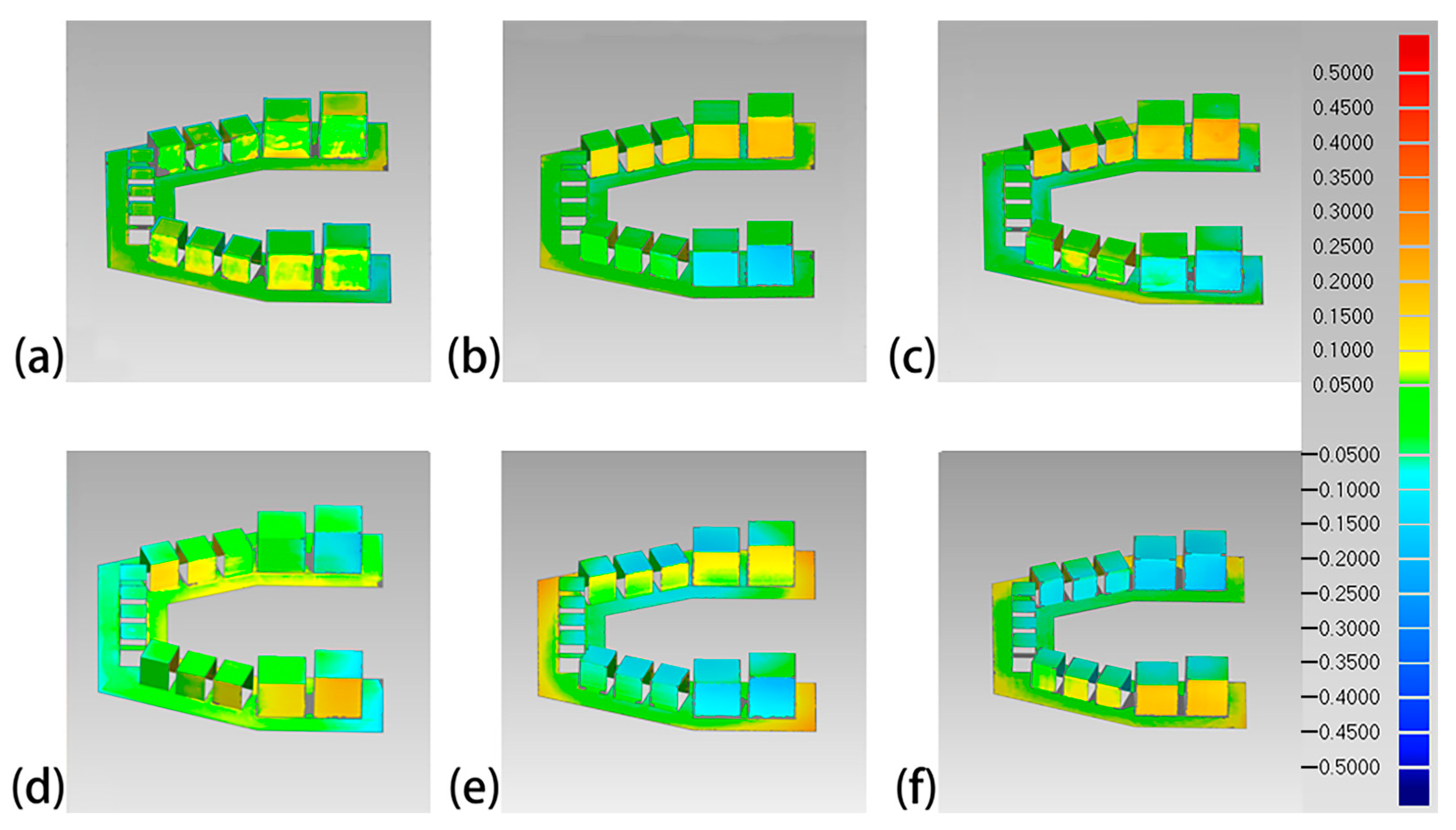
3.1. 3D Form Error
3.2. Linear Dimensional Error
4. Discussion
4.1. Diversity in Spatial Trueness Evaluation Results of Different Printers
4.2. Feasibility of Multi-Dimensional View of Spatial Trueness Offered by the Structurized Dental Model
4.3. Future Works to Optimize the Evaluation Process
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alghazzawi, T.F. Advancements in CAD/CAM technology: Options for practical implementation. J. Prosthodont. Res. 2016, 60, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Cheong, J.; Kim, S.; Park, W.; Kim, K. Accuracy of 3D printed dental casts for protective dental splints during general anesthesia. Rapid Prototyp. J. 2022, 28, 1374–1381. [Google Scholar] [CrossRef]
- Santoro, M.; Galkin, S.; Teredesai, M.; Nicolay, O.F.; Cangialosi, T.J. Comparison of measurements made on digital and plaster models. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Stevens, L.; Spratley, M.H. Accuracy of stopne, epoxy, and silve plate-acrylic models. Dent. Mater. 1987, 3, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, O.; Watts, D.C.; Sigusch, B.W.; Kuepper, H.; Guentsch, A. Marginal and internal fit of pressed lithium disilicate partial crowns in vitro: A three-dimensional analysis of accuracy and reproducibility. Dent. Mater. 2012, 28, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Fuh, J.Y.H.; Lu, L.; Tan, C.; Shen, Z.; Chew, S. Curing characteristics of acrylic photopolymer used in stereolithography process. Rapid Prototyp. J. 1999, 5, 27–34. [Google Scholar] [CrossRef]
- Narahara, H.; Tanaka, F.; Kishinami, T.; Igarashi, S.; Saito, K. Reaction heat effects on initial linear shrinkage and deformation in stereolithography. Rapid Prototyp. J. 1999, 5, 120–128. [Google Scholar] [CrossRef]
- Shin, S.; Lim, J.; Kang, Y.; Kim, J.; Shim, J.; Kim, J. Evaluation of the 3D Printing Accuracy of a Dental Model According to Its Internal Structure and Cross-Arch Plate Design: An In Vitro Study. Materials 2020, 13, 5433. [Google Scholar] [CrossRef]
- Moradi, M.; Karamimoghadam, M.; Meiabadi, S.; Casalino, G.; Ghaleeh, M.; Baby, B.; Ganapathi, H.; Jose, J.; Abdulla, M.S.; Tallon, P.; et al. Mathematical Modelling of Fused Deposition Modeling (FDM) 3D Printing of Poly Vinyl Alcohol Parts through Statistical Design of Experiments Approach. Mathematics 2023, 11, 3022. [Google Scholar] [CrossRef]
- Etemad-Shahidi, Y.; Qallandar, O.B.; Evenden, J.; Alifui-Segbaya, F.; Ahmed, K.E. Accuracy of 3-Dimensionally Printed Full-Arch Dental Models: A Systematic Review. J. Clin. Med. 2020, 9, 3357. [Google Scholar] [CrossRef] [PubMed]
- Patzelt, S.B.M.; Bishti, S.; Stampf, S.; Att, W. Accuracy of computer-aided design/computer-aided manufacturing–generated dental casts based on intraoral scanner data. J. Am. Dent. Assoc. 2014, 145, 1133–1140. [Google Scholar] [CrossRef]
- Cho, S.D.M.; Schaefer, O.D.; Thompson, G.A.D.M.; Guentsch, A.D.P.M. Comparison of accuracy and reproducibility of casts made by digital and conventional methods. J. Prosthet. Dent. 2015, 113, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Jin, S.J.; Jeong, I.D.; Kim, J.H.; Kim, W.C. Accuracy (trueness and precision) of dental models fabricated using additive manufacturing methods. Int. J. Comput. Dent. 2018, 21, 107–113. [Google Scholar]
- Jeong, Y.; Lee, W.; Lee, K. Accuracy evaluation of dental models manufactured by CAD/CAM milling method and 3D printing method. J. Adv. Prosthodont. 2018, 10, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.T. Accuracy of dental models fabricated by CAD/CAM milling method and 3D printing method. J. Oral Res. 2018, 7, 127–133. [Google Scholar] [CrossRef]
- Brown, G.B.; Currier, G.F.; Kadioglu, O.; Kierl, J.P. Accuracy of 3-dimensional printed dental models reconstructed from digital intraoral impressions. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Al-Imam, H.; Gram, M.; Benetti, A.R.; Gotfredsen, K. Accuracy of stereolithography additive casts used in a digital workflow. J. Prosthet. Dent. 2018, 119, 580–585. [Google Scholar]
- Choi, J.; Ahn, J.; Son, K.; Huh, J. Three-Dimensional Evaluation on Accuracy of Conventional and Milled Gypsum Models and 3D Printed Photopolymer Models. Materials 2019, 12, 3499. [Google Scholar] [CrossRef]
- Jin, S.J.; Kim, D.Y.; Kim, J.H.; Kim, W.C. Accuracy of Dental Replica Models Using Photopolymer Materials in Additive Manufacturing: In Vitro Three-Dimensional Evaluation. J. Prosthodont. 2019, 28, e557–e562. [Google Scholar] [CrossRef]
- Sim, J.-Y.; Jang, Y.; Kim, W.-C.; Kim, H.-Y.; Lee, D.-H. Comparing the accuracy (trueness and precision) of models of fixed dental prostheses fabricated by digital and conventional workflows. J. Prosthodont. Res. 2019, 63, 25–30. [Google Scholar] [CrossRef] [PubMed]
- ISO 5725-1:2023; Accuracy (Trueness and Precision) of Measurement Methods and Results-Part 1: General Principles and Definitions. International Organization for Standardization: Geneva, Switzerland, 2023.
- Prenesti, E.; Gosmaro, F. Trueness, precision and accuracy: A critical overview of the concepts as well as proposals for revision. Accredit. Qual. Assur. 2015, 20, 33–40. [Google Scholar] [CrossRef]
- Cuperus, A.M.R.; Harms, M.C.; Rangel, F.A.; Bronkhorst, E.M.; Schols, J.G.J.H.; Breuning, K.H. Dental models made with an intraoral scanner: A validation study. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Kasparova, M.; Grafova, L.; Dvorak, P.; Dostalova, T.; Prochazka, A.; Eliasova, H.; Prusa, J.; Kakawand, S. Possibility of reconstruction of dental plaster cast from 3D digital study models. Biomed. Eng. Online 2013, 12, 49. [Google Scholar] [CrossRef] [PubMed]
- Hazeveld, A.; Huddleston Slater, J.J.R.; Ren, Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Saleh, W.K.; Ariffin, E.; Sherriff, M.; Bister, D. Accuracy and reproducibility of linear measurements of resin, plaster, digital and printed study-models. J. Orthod. 2015, 42, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Camardella, L.T.; Vilella, O.D.V.; Breuning, H. Accuracy of printed dental models made with 2 prototype technologies and different designs of model bases. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1178–1187. [Google Scholar] [CrossRef] [PubMed]
- Rebong, R.E.; Stewart, K.T.; Utreja, A.; Ghoneima, A.A. Accuracy of three-dimensional dental resin models created by fused deposition modeling, stereolithography, and Polyjet prototype technologies: A comparative study. Angle Orthod. 2018, 88, 363–369. [Google Scholar] [CrossRef]
- Kim, S.Y.; Shin, Y.S.; Jung, H.D.; Hwang, C.J.; Baik, H.S.; Cha, J.Y. Precision and trueness of dental models manufactured with different 3-dimensional printing techniques. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 144–153. [Google Scholar] [CrossRef]
- Rungrojwittayakul, O.; Kan, J.Y.; Shiozaki, K.; Swamidass, R.S.; Lozada, J.L. Accuracy of 3D Printed Models Created by Two Technologies of Printers with Different Designs of Model Base. J. Prosthodont. 2019, 29, 124–128. [Google Scholar] [CrossRef]
- Sherman, S.L.; Kadioglu, O.; Currier, G.F.; Kierl, J.P.; Li, J. Accuracy of digital light processing printing of 3-dimensional dental models. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 422–428. [Google Scholar] [CrossRef]
- Hwang, Y.C.; Park, Y.S.; Kim, H.K.; Hong, Y.S.; Ahn, J.S.; Ryu, J.J. The Evaluation of Working Casts Prepared from Digital Impressions. Oper. Dent. 2013, 38, 655–662. [Google Scholar] [CrossRef]
- Wan Hassan, W.N.; Yusoff, Y.; Mardi, N.A. Comparison of reconstructed rapid prototyping models produced by 3-dimensional printing and conventional stone models with different degrees of crowding. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 209–218. [Google Scholar] [CrossRef]
- Keating, A.P.; Knox, J.; Bibb, R.; Zhurov, A.I. A Comparison of Plaster, Digital and Reconstructed Study Model Accuracy. J. Orthod. 2008, 35, 191–201. [Google Scholar] [CrossRef]
- Tahayeri, A.; Morgan, M.C.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef]
- Vyavahare, S.; Kumar, S.; Panghal, D. Experimental study of surface roughness, dimensional accuracy and time of fabrication of parts produced by fused deposition modelling. Rapid Prototyp. J. 2020, 26, 1535–1554. [Google Scholar] [CrossRef]
- Xiao, N.; Sun, Y.; Zhao, Y.; Wang, Y. A method to evaluate the trueness of reconstructed dental models made with photo-curing 3D printing technologies. J. Peking Univ. (Health Sci.) 2019, 51, 120–130. [Google Scholar]
- Ling, T.U.; Liang-Kui, L.; Yan-Jia, H.U. Study of teeth and dental arch in Hunan residents with normal permanent occlusion. China J. Mod. Med. 2003, 13, 62–64. [Google Scholar]
- Hui, P.; Haiyan, L.U. Measurement of permanent crown diameter of Han’s youth. J. Mod. Stomatol. 2003, 17, 57–59. [Google Scholar]
- Wang, H. The Measurement and statistics of Chinese dentition. Chin. J. Stomatol. 1959, 3, 149–155. [Google Scholar]
- Weng, X.; Yu, S.; Zhao, S.; Tang, R.; Wang, H.; Fan, J. Morphology of permanent teeth of the Han nationality. Chin. J. Conserv. Dent. 2007, 17, 75–77. [Google Scholar]
- Favero, C.S.; English, J.D.; Cozad, B.E.; Wirthlin, J.O.; Short, M.M.; Kasper, F.K. Effect of print layer height and printer type on the accuracy of 3-dimensional printed orthodontic models. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 557–565. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Chen, Y.W.; Alshawaf, B.; Kang, K.; Finkelman, M.; Chronopoulos, V.; Weber, H.P. Digital workflow: In vitro accuracy of 3D printed casts generated from complete-arch digital implant scans. J. Prosthet. Dent. 2020, 124, 589–593. [Google Scholar] [CrossRef]
- Park, J.M.; Jeon, J.; Koak, J.Y.; Kim, S.K.; Heo, S.J. Dimensional accuracy and surface characteristics of 3D-printed dental casts. J. Prosthet. Dent. 2020, 126, 427–437. [Google Scholar] [CrossRef]
- Zhang, Z.; Li, P.; Chu, F.; Shen, G. Influence of the three-dimensional printing technique and printing layer thickness on model accuracy. J. Orofac. Orthop./Fortschritte Kieferorthopadie 2019, 80, 194–204. [Google Scholar] [CrossRef]
- Dietrich, C.A.; Ender, A.; Baumgartner, S.; Mehl, A. A validation study of reconstructed rapid prototyping models produced by two technologies. Angle Orthod. 2017, 87, 782–787. [Google Scholar] [CrossRef]
- Mangano, F.G.; Admakin, O.; Bonacina, M.; Biaggini, F.; Lerner, H. Accuracy of 6 Desktop 3D Printers in Dentistry: A Comparative In Vitro Study. Eur. J. Prosthodont. Restor. Dent. 2020, 28, 75–85. [Google Scholar]
- Joda, T.; Matthisson, L.; Zitzmann, N.U. Impact of Aging on the Accuracy of 3D-Printed Dental Models: An In Vitro Investigation. J. Clin. Med. 2020, 9, 1436. [Google Scholar] [CrossRef]
- Bud, E.S.; Bocanet, V.I.; Muntean, M.H.; Vlasa, A.; Bucur, S.M.; Păcurar, M.; Dragomir, B.R.; Olteanu, C.D.; Bud, A. Accuracy of Three-Dimensional (3D) Printed Dental Digital Models Generated with Three Types of Resin Polymers by Extra-Oral Optical Scanning. J. Clin. Med. 2021, 10, 1908. [Google Scholar] [CrossRef]
- Nestler, N.; Wesemann, C.; Spies, B.C.; Beuer, F.; Bumann, A. Dimensional accuracy of extrusion- and photopolymerization-based 3D printers: Invitro study comparing printed casts. J. Prosthet. Dent. 2021, 125, 103–110. [Google Scholar] [CrossRef]
- Stansbury, J.W.; Idacavage, M.J. 3D printing with polymers: Challenges among expanding options and opportunities. Dent. Mater. 2016, 32, 54–64. [Google Scholar] [CrossRef]
- van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef]
- Ishida, Y.; Miyasaka, T. Dimensional accuracy of dental casting patterns created by 3D printers. Dent. Mater. J. 2016, 35, 250–256. [Google Scholar] [CrossRef]
- Park, M.E.; Shin, S.Y. Three-dimensional comparative study on the accuracy and reproducibility of dental casts fabricated by 3D printers. J. Prosthet. Dent. 2018, 119, 861. [Google Scholar] [CrossRef]
- Emir, F.; Ayyildiz, S. Accuracy evaluation of complete-arch models manufactured by three different 3D printing technologies: A three-dimensional analysis. J. Prosthodont. Res. 2021, 65, 365–370. [Google Scholar] [CrossRef]
- Ishida, Y.; Miura, D.; Miyasaka, T.; Shinya, A. Dimensional Accuracy of Dental Casting Patterns Fabricated Using Consumer 3D Printers. Polymers 2020, 12, 2244. [Google Scholar] [CrossRef]
- ISO 23298:2023; Dentistry-Test Methods for Machining Accuracy of Computer-Aided Milling Machines. International Organization for Standardization: Geneva, Switzerland, 2023.
- ISO 1101:2017; Geometrical Product Specifications (GPS)-Geometrical Tolerancing-Tolerances of Form, Orientation, Location and Run-out. International Organization for Standardization: Geneva, Switzerland, 2017.
- Senthilkumaran, K.; Pandey, P.M.; Rao, P.V.M. Statistical modeling and minimization of form error in SLS prototyping. Rapid Prototyp. J. 2012, 18, 38–48. [Google Scholar] [CrossRef]
- Kumar, V.V.; Shirisha, A.; Ind, A.P. Geometrical Accuracy of Parts Produced by Rapid Prototyping Technique (Sls). Int. J. Adv. Mater. Manuf. Charact. 2013, 3, 447–450. [Google Scholar]
- Yoo, S.Y.; Kim, S.K.; Heo, S.J.; Koak, J.Y.; Kim, J.G. Dimensional Accuracy of Dental Models for Three-Unit Prostheses Fabricated by Various 3D Printing Technologies. Materials 2021, 14, 1550. [Google Scholar] [CrossRef]
- Han, J.; Ge, Y.; Mao, Y.; Wu, M. A study on the surface quality of the 3D printed parts caused by the scanning strategy. Rapid Prototyp. J. 2018, 25, 247–254. [Google Scholar] [CrossRef]
- Shankar Limaye, A.; Rosen, D.W. Compensation zone approach to avoid print-through errors in mask projection stereolithography builds. Rapid Prototyp. J. 2006, 12, 283–291. [Google Scholar] [CrossRef]
- Ciotti, M.; Campana, G.; Mele, M. A review of the accuracy of thermoplastic polymeric parts fabricated by additive manufacturing. Rapid Prototyp. J. 2022, 28, 358–389. [Google Scholar]
- Bagheri, A.; Jin, J. Photopolymerization in 3D Printing. ACS Appl. Polym. Mater. 2019, 1, 593–611. [Google Scholar] [CrossRef]
- Ligon, S.C.; Liska, R.; Stampfl, J.; Gurr, M.; Mülhaupt, R. Polymers for 3D Printing and Customized Additive Manufacturing. Chem. Rev. 2017, 117, 10212–10290. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Song, K.; Mo, H.; Li, J.; Pan, D.; Liang, Z. Progress on Photosensitive Resins for 3D Printing. J. Funct. Polym. 2015, 028, 102–108. [Google Scholar]
- Arnold, C.; Monsees, D.; Hey, J.; Schweyen, R. Surface Quality of 3D-Printed Models as a Function of Various Printing Parameters. Materials 2019, 12, 1970. [Google Scholar] [CrossRef]
- Osman, R.B.; Alharbi, N.; Wismeijer, D. Build Angle: Does It Influence the Accuracy of 3D-Printed Dental Restorations Using Digital Light-Processing Technology? Int. J. Prosthodont. 2017, 30, 182–188. [Google Scholar] [CrossRef]
- Unkovskiy, A.; Bui, H.B.; Schille, C.; Geis-Gerstorfer, J.; Huettig, F.; Spintzyk, S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent. Mater. 2018, 34, e324–e333. [Google Scholar] [CrossRef] [PubMed]
- Mostafavi, D.; Methani, M.M.; Cascón, W.P.; Zandinejad, A.; León, M.R. Influence of the Rinsing Post-Processing Procedures on the Manufacturing Accuracy of Vat-Polymerized Dental Model Material. J. Prosthodont. 2021, 30, 610–616. [Google Scholar] [CrossRef]
- Eman, S.; Abdulhadi, A.; Elke, V.D.C.; Constantinus, P.; Reinhilde, J. Evaluation of Dimensional Changes of 3D Printed Models After Sterilization: A Pilot Study. Open Dent. J. 2018, 12, 72–79. [Google Scholar]
- Bass, L.; Meisel, N.A.; Williams, C.B. Exploring variability of orientation and aging effects in material properties of multi-material jetting parts. Rapid Prototyp. J. 2016, 22, 826–834. [Google Scholar] [CrossRef]

| SDC | Maxillary Model | Mandibular Model | ||||
|---|---|---|---|---|---|---|
| Mesiodistal Diameter | Buccolingual Diameter | Crown Height | Mesiodistal Diameter | Buccolingual Diameter | Crown Height | |
| Central incisor | 8 | 7 | 10 | 5 | 6 | 8 |
| Lateral incisor | 7 | 6 | 9 | 6 | 6 | 8 |
| Canine | 8 | 8 | 11 | 7 | 7 | 8 |
| First premolar | 7 | 9 | 10 | 7 | 8 | 7 |
| Second premolar | 7 | 9 | 10 | 7 | 8 | 7 |
| First molar | 10 | 11 | 8 | 11 | 10 | 10 |
| Second molar | 9 | 11 | 5 | 11 | 10 | 12 |
| 3D Printer Name | Manufacturer | Printing Technology | Printing Materials | Layer Thickness (μm) | XY Resolution (μm) |
|---|---|---|---|---|---|
| Objet30 Pro | Stratasys (Eden Grasslands, MN, USA) | Polyjet | VeroClear light-curing resin | 16 | 42 |
| Projet 3510 HD Plus | 3D systems (Rockhill, SC, USA) | Multijet | VisiJet EX200 light-curing resin | 16 | 34 |
| Perfactory DDP | EnvisionTEC (Mar, Ruhr, Germany) | DLP | E-model light light-curing resin | 50 | 60 |
| DLP 800d | Han’s laser (Shenzhen, Guangdong, China) | DLP | T-MOG-522 light-curing resin | 50 | 75 |
| Form2 | Formlabs (Somerville, MA, USA) | SLA | Dental Model light-curing resin | 50 | 140 |
| Form3 | Formlabs (Somerville, MA, USA) | SLA | Dental Model light-curing resin | 50 | 85 |
| Overall 3D Deviation | |||
|---|---|---|---|
| Maxillary Model | Mandibular Model | Overall Value | |
| Objet30 Pro | 47 | 43 | 45 |
| Projet 3510 HD Plus | 55 | 72 | 64 |
| Perfactory DDP | 97 | 92 | 95 |
| DLP 800d | 98 | 72 | 85 |
| Form2 | 102 | 79 | 91 |
| Form3 | 74 | 87 | 80 |
| Flatness Error (mm) | Parallelism Error (°) | Perpendicularity Error (°) | |
|---|---|---|---|
| Objet30 Pro | 0.190 ± 0.059 | 0.138 ± 0.068 | 0.265 ± 0.191 |
| Projet 3510 HD Plus | 0.081 ± 0.024 | 0.141 ± 0.071 | 0.095 ± 0.070 |
| Perfactory DDP | 0.074 ± 0.023 | 0.434 ± 0.244 | 0.478 ± 0.273 |
| DLP 800d | 0.075 ± 0.019 | 0.262 ± 0.090 | 0.214 ± 0.161 |
| Form2 | 0.076 ± 0.020 | 0.453 ± 0.237 | 0.568 ± 0.183 |
| Form3 | 0.061 ± 0.019 | 0.270 ± 0.094 | 0.151 ± 0.122 |
| Flatness Error of Horizontal Planes | Flatness Error of Vertical Planes | |
|---|---|---|
| Objet30 Pro | 0.250 | 0.161 |
| Projet 3510 HD Plus | 0.081 | 0.081 |
| Perfactory DDP | 0.056 | 0.083 |
| DLP 800d | 0.068 | 0.079 |
| Form2 | 0.065 | 0.081 |
| Form3 | 0.042 | 0.071 |
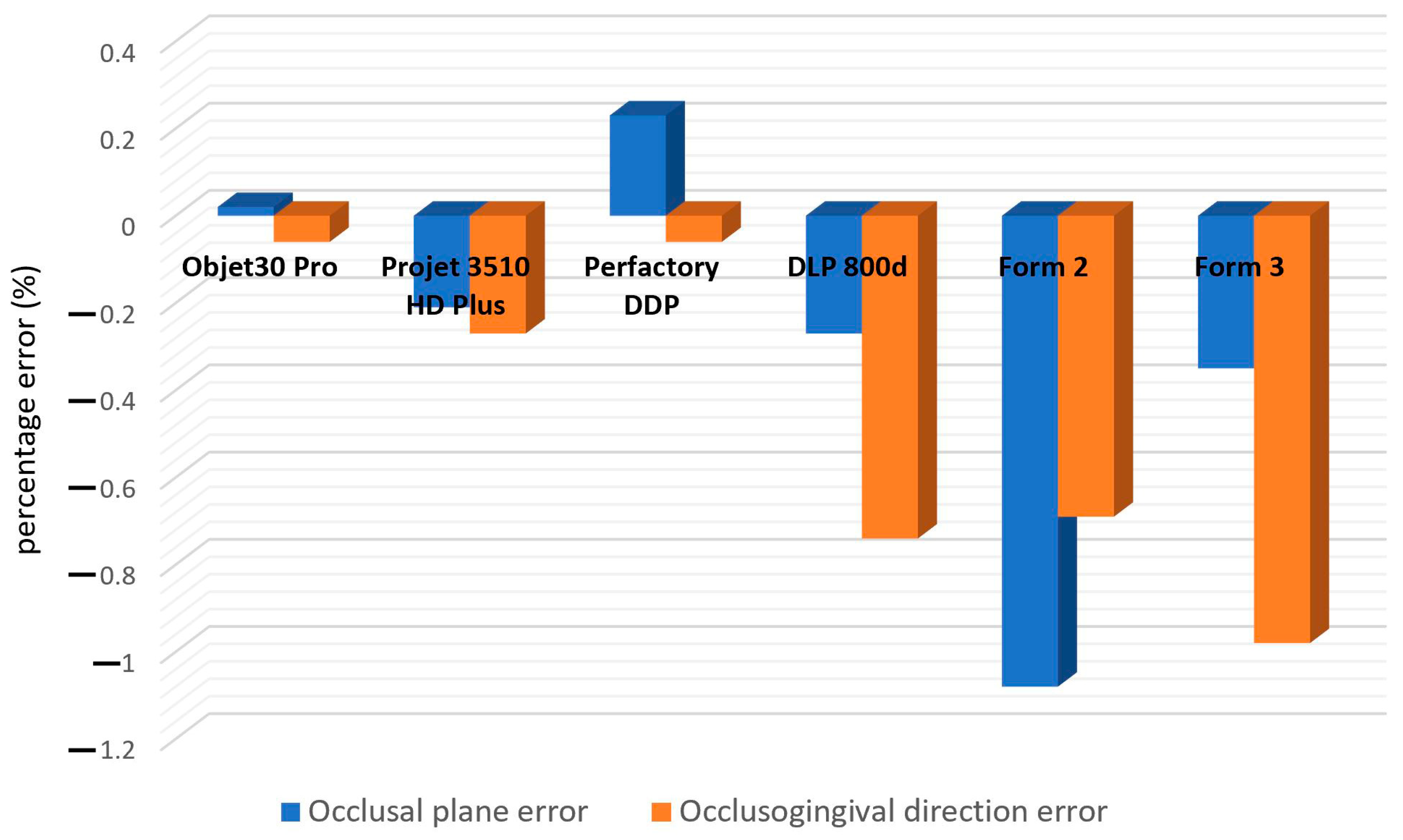
| Occlusal Plane Error | Occlusogingival Direction Error | |
|---|---|---|
| Objet30 Pro | 0.02 ± 0.36 * | −0.06 ± 0.09 |
| Projet 3510 HD Plus | −0.21 ± 0.30 | −0.27 ± 0.14 |
| Perfactory DDP | 0.23 ± 0.36 | −0.06 ± 0.15 |
| DLP 800d | −0.27 ± 0.24 | −0.74 ± 0.11 |
| Form2 | −1.08 ± 0.38 | −0.69 ± 0.19 |
| Form3 | −0.35 ± 0.15 | −0.98 ± 0.14 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wen, A.; Xiao, N.; Zhu, Y.; Gao, Z.; Qin, Q.; Shan, S.; Li, W.; Sun, Y.; Wang, Y.; Zhao, Y. Spatial Trueness Evaluation of 3D-Printed Dental Model Made of Photopolymer Resin: Use of Special Structurized Dental Model. Polymers 2024, 16, 1083. https://doi.org/10.3390/polym16081083
Wen A, Xiao N, Zhu Y, Gao Z, Qin Q, Shan S, Li W, Sun Y, Wang Y, Zhao Y. Spatial Trueness Evaluation of 3D-Printed Dental Model Made of Photopolymer Resin: Use of Special Structurized Dental Model. Polymers. 2024; 16(8):1083. https://doi.org/10.3390/polym16081083
Chicago/Turabian StyleWen, Aonan, Ning Xiao, Yujia Zhu, Zixiang Gao, Qingzhao Qin, Shenyao Shan, Wenbo Li, Yuchun Sun, Yong Wang, and Yijiao Zhao. 2024. "Spatial Trueness Evaluation of 3D-Printed Dental Model Made of Photopolymer Resin: Use of Special Structurized Dental Model" Polymers 16, no. 8: 1083. https://doi.org/10.3390/polym16081083
APA StyleWen, A., Xiao, N., Zhu, Y., Gao, Z., Qin, Q., Shan, S., Li, W., Sun, Y., Wang, Y., & Zhao, Y. (2024). Spatial Trueness Evaluation of 3D-Printed Dental Model Made of Photopolymer Resin: Use of Special Structurized Dental Model. Polymers, 16(8), 1083. https://doi.org/10.3390/polym16081083






