Effect of Cell Therapy and Exercise Training in a Stroke Model, Considering the Cell Track by Molecular Image and Behavioral Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Isolation, Culture and Immunophenotypic Characterization of Human Bone Marrow Mesenchymal Stem Cells
2.2. Lentiviral Transduction of MSC
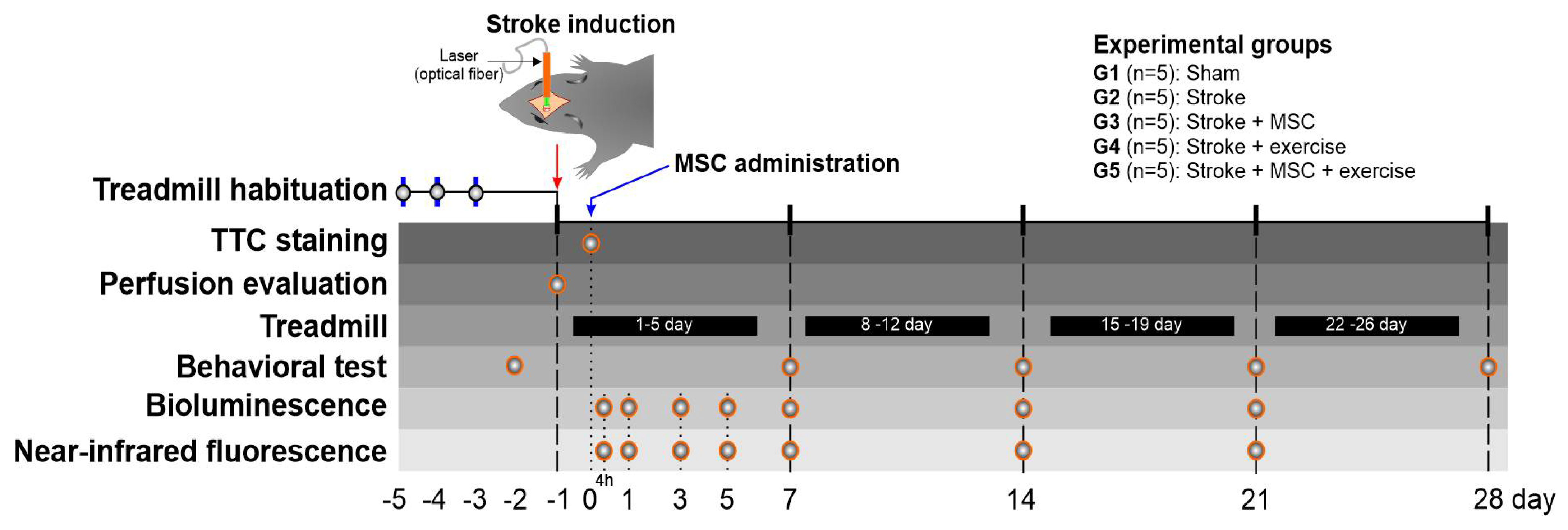
2.3. Nanoparticles Used in the MSC Homing Evaluation
2.4. Cell Labeling and the Internalization Evaluation of MSC Labeled with MNPs
2.5. Cellular Viability of MSC Labeled with MNP
2.6. Animals and Experimental Design
2.7. Treadmill Habituation Evaluation (Selection of the Best Running Animals for the Experiment)
2.8. Induction of Stroke through Photothrombosis
2.9. Focal Ischemic Lesion Induction Evaluation by Blood Perfusion and TTC Staining
2.10. MSC Administration
2.11. Treadmill Protocol—Exercise Training
2.12. Behavioral Analysis
2.13. MSC Homing after Implantation by Bioluminescence and Fluorescence Images
2.14. Statistical Analysis
3. Results
3.1. Evaluation of MNP Internalization into MSC and Their Viability
3.2. Evaluation of Focal Ischemic Brain Lesion Induction by Phototrombosis, Using Local Blood Perfusion Analysis and TTC Staining
3.3. Performance in Treadmill Training
3.4. Behavioral Evaluation by the Cylinder Test and the Spontaneous Locomotor Activity Test
3.5. Noninvasive Evaluation of Homing of MSCLuc Labeled with MNP by Molecular Images in the Stroke Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Morovatdar, N.; Avan, A.; Azarpazhooh, M.R.; Di Napoli, M.; Stranges, S.; Kapral, M.K.; Rezayat, A.A.; Shariatzadeh, A.; Abootalebi, S.; Mokhber, N.; et al. Secular trends of ischaemic heart disease, stroke, and dementia in high-income countries from 1990 to 2017: The Global Burden of Disease Study 2017. Neurol. Sci. 2021, 43, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, G.M.M.; Brant, L.C.C.; Polanczyk, C.A.; Biolo, A.; Nascimento, B.R.; Malta, D.C.; Souza, M.F.M.; Soares, G.P.; Xavier Junior, G.F.; Machline-Carrion, M.J.; et al. Cardiovascular Statistics—Brazil 2020. Arq. Bras. Cardiol. 2020, 115, 308–439. [Google Scholar] [CrossRef]
- Blank, I.A.; Fedorenko, E. Domain-General Brain Regions Do Not Track Linguistic Input as Closely as Language-Selective Regions. J. Neurosci. 2017, 37, 9999–10011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, W.; Shi, L.; Hu, B.; Hong, Y.; Zhang, H.; Li, X.; Zhang, Y. Mesenchymal Stem Cell-Based Therapy for Stroke: Current Understanding and Challenges. Front. Cell Neurosci. 2021, 15, 628940. [Google Scholar] [CrossRef]
- Jovin, T.G.; Chamorro, A.; Cobo, E.; de Miquel, M.A.; Molina, C.A.; Rovira, A.; San Román, L.; Serena, J.; Abilleira, S.; Ribó, M.; et al. Thrombectomy within 8 h after symptom onset in ischemic stroke. N. Engl. J. Med. 2015, 372, 2296–2306. [Google Scholar] [CrossRef] [Green Version]
- Mendez, A.A.; Samaniego, E.A.; Sheth, S.A.; Dandapat, S.; Hasan, D.M.; Limaye, K.S.; Hindman, B.J.; Derdeyn, C.P.; Ortega-Gutierrez, S. Update in the Early Management and Reperfusion Strategies of Patients with Acute Ischemic Stroke. Crit. Care Res. Pract. 2018, 2018, 9168731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, Y.; Yamamoto, Y.; Xiao, Z.; Ochiya, T. The Immunomodulatory Functions of Mesenchymal Stromal/Stem Cells Mediated via Paracrine Activity. J. Clin. Med. 2019, 8, 1025. [Google Scholar] [CrossRef] [Green Version]
- Maltman, D.J.; Hardy, S.A.; Przyborski, S.A. Role of mesenchymal stem cells in neurogenesis and nervous system repair. Neurochem. Int. 2011, 59, 347–356. [Google Scholar] [CrossRef]
- Nudo, R.J. Recovery after brain injury: Mechanisms and principles. Front. Hum. Neurosci. 2013, 7, 887. [Google Scholar] [CrossRef] [Green Version]
- Terashi, T.; Otsuka, S.; Takada, S.; Nakanishi, K.; Ueda, K.; Sumizono, M.; Kikuchi, K.; Sakakima, H. Neuroprotective effects of different frequency preconditioning exercise on neuronal apoptosis after focal brain ischemia in rats. Neurol. Res. 2019, 41, 510–518. [Google Scholar] [CrossRef]
- Di Raimondo, D.; Rizzo, G.; Musiari, G.; Tuttolomondo, A.; Pinto, A. Role of Regular Physical Activity in Neuroprotection against Acute Ischemia. Int. J. Mol. Sci. 2020, 21, 9086. [Google Scholar] [CrossRef] [PubMed]
- Marycz, K.; Mierzejewska, K.; Śmieszek, A.; Suszynska, E.; Malicka, I.; Kucia, M.; Ratajczak, M.Z. Endurance Exercise Mobilizes Developmentally Early Stem Cells into Peripheral Blood and Increases Their Number in Bone Marrow: Implications for Tissue Regeneration. Stem Cells Int. 2016, 2016, 5756901. [Google Scholar] [CrossRef] [Green Version]
- Nucci, M.P.; Filgueiras, I.S.; Ferreira, J.M.; de Oliveira, F.A.; Nucci, L.P.; Mamani, J.B.; Rego, G.N.A.; Gamarra, L.F. Stem cell homing, tracking and therapeutic efficiency evaluation for stroke treatment using nanoparticles: A systematic review. World J. Stem Cells 2020, 12, 381–405. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Lee, W.Y.; Wu, T.; Xu, J.; Zhang, K.; Hong Wong, D.S.; Li, R.; Li, G.; Bian, L. Near-infrared light-triggered release of small molecules for controlled differentiation and long-term tracking of stem cells in vivo using upconversion nanoparticles. Biomaterials 2016, 110, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Lin, S.; Huang, D.; Zhang, Y.; Li, C.; Wang, M.; Wang, Q. Revealing the Fate of Transplanted Stem Cells In Vivo with a Novel Optical Imaging Strategy. Small 2018, 14, 1702679. [Google Scholar] [CrossRef]
- Schaar, K.L.; Brenneman, M.M.; Savitz, S.I. Functional assessments in the rodent stroke model. Exp. Transl. Stroke Med. 2010, 2, 13. [Google Scholar] [CrossRef] [Green Version]
- Da Silva, H.R.; Mamani, J.B.; Nucci, M.P.; Nucci, L.P.; Kondo, A.T.; Fantacini, D.M.C.; de Souza, L.E.B.; Picanço-Castro, V.; Covas, D.T.; Kutner, J.M.; et al. Triple-modal imaging of stem-cells labeled with multimodal nanoparticles, applied in a stroke model. World J. Stem Cells 2019, 11, 100–123. [Google Scholar] [CrossRef]
- Souza, T.K.F.; Nucci, M.P.; Mamani, J.B.; da Silva, H.R.; Fantacini, D.M.C.; de Souza, L.E.B.; Picanço-Castro, V.; Covas, D.T.; Vidoto, E.L.; Tannús, A.; et al. Image and motor behavior for monitoring tumor growth in C6 glioma model. PLoS ONE 2018, 13, e0201453. [Google Scholar] [CrossRef] [Green Version]
- Oliveira, F.A.; Nucci, M.P.; Mamani, J.B.; Alves, A.H.; Rego, G.N.A.; Kondo, A.T.; Hamerschlak, N.; Junqueira, M.S.; de Souza, L.E.B.; Gamarra, L.F. Multimodal Tracking of Hematopoietic Stem Cells from Young and Old Mice Labeled with Magnetic–Fluorescent Nanoparticles and Their Grafting by Bioluminescence in a Bone Marrow Transplant Model. Biomedicines 2021, 9, 752. [Google Scholar] [CrossRef]
- Lindemann, A.; Lüdtke-Buzug, K.; Fräderich, B.M.; Gräfe, K.; Pries, R.; Wollenberg, B. Biological impact of superparamagnetic iron oxide nanoparticles for magnetic particle imaging of head and neck cancer cells. Int. J. Nanomed. 2014, 9, 5025–5040. [Google Scholar] [CrossRef] [Green Version]
- Dishman, R.K.; Armstrong, R.B.; Delp, M.D.; Graham, R.E.; Dunn, A.L. Open-field behavior is not related to treadmill performance in exercising rats. Physiol. Behav. 1988, 43, 541–546. [Google Scholar] [CrossRef]
- Ríos-Kristjánsson, J.G.; Rizo-Roca, D.; Kristjánsdóttir, K.M.; Núñez-Espinosa, C.A.; Torrella, J.R.; Pagès, T.; Viscor, G. A three-criteria performance score for rats exercising on a running treadmill. PLoS ONE 2019, 14, e0219167. [Google Scholar] [CrossRef] [PubMed]
- Paxinos, G.; Watson, C. The Rat Brain in Stereotaxic Coordinates: Compact; Elsevier Science: Cambridge, MA, USA, 2017. [Google Scholar]
- Li, P.; Gan, Y.; Sun, B.L.; Zhang, F.; Lu, B.; Gao, Y.; Liang, W.; Thomson, A.W.; Chen, J.; Hu, X. Adoptive regulatory T-cell therapy protects against cerebral ischemia. Ann. Neurol. 2013, 74, 458–471. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Liu, H.; Zhang, H.; Ye, Q.; Wang, J.; Yang, B.; Mao, L.; Zhu, W.; Leak, R.K.; Xiao, B.; et al. ST2/IL-33-Dependent Microglial Response Limits Acute Ischemic Brain Injury. J. Neurosci. 2017, 37, 4692–4704. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, H.; Nucci, M.P.; Mamani, J.B.; Mendez-Otero, R.; Nucci, L.P.; Tannus, A.; Gamarra, L.F. Evaluation of temperature induction in focal ischemic thermocoagulation model. PLoS ONE 2018, 13, e0200135. [Google Scholar] [CrossRef] [Green Version]
- Benedek, A.; Móricz, K.; Jurányi, Z.; Gigler, G.; Lévay, G.; Hársing, L.G., Jr.; Mátyus, P.; Szénási, G.; Albert, M. Use of TTC staining for the evaluation of tissue injury in the early phases of reperfusion after focal cerebral ischemia in rats. Brain Res. 2006, 1116, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Schallert, T. Behavioral tests for preclinical intervention assessment. NeuroRx 2006, 3, 497–504. [Google Scholar] [CrossRef]
- Verma, V.K.; Kamaraju, S.R.; Kancherla, R.; Kona, L.K.; Beevi, S.S.; Debnath, T.; Usha, S.P.; Vadapalli, R.; Arbab, A.S.; Chelluri, L.K. Fluorescent magnetic iron oxide nanoparticles for cardiac precursor cell selection from stromal vascular fraction and optimization for magnetic resonance imaging. Int. J. Nanomed. 2015, 10, 711–726. [Google Scholar] [CrossRef] [Green Version]
- Karimi, M.A.; Lee, E.; Bachmann, M.H.; Salicioni, A.M.; Behrens, E.M.; Kambayashi, T.; Baldwin, C.L. Measuring Cytotoxicity by Bioluminescence Imaging Outperforms the Standard Chromium-51 Release Assay. PLoS ONE 2014, 9, e89357. [Google Scholar] [CrossRef]
- Sibov, T.T.; Pavon, L.F.; Miyaki, L.A.; Mamani, J.B.; Nucci, L.P.; Alvarim, L.T.; Silveira, P.H.; Marti, L.C.; Gamarra, L. Umbilical cord mesenchymal stem cells labeled with multimodal iron oxide nanoparticles with fluorescent and magnetic properties: Application for in vivo cell tracking. Int. J. Nanomed. 2014, 9, 337–350. [Google Scholar] [CrossRef] [Green Version]
- Labat-gest, V.; Tomasi, S. Photothrombotic ischemia: A minimally invasive and reproducible photochemical cortical lesion model for mouse stroke studies. J. Vis. Exp. 2013, 50370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jolkkonen, J.; Jokivarsi, K.; Laitinen, T.; Gröhn, O. Subacute hemorrhage and resolution of edema in Rose Bengal stroke model in rats coincides with improved sensorimotor functions. Neurosci. Lett. 2007, 428, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Nucci, L.P.; Silva, H.R.; Giampaoli, V.; Mamani, J.B.; Nucci, M.P.; Gamarra, L.F. Stem cells labeled with superparamagnetic iron oxide nanoparticles in a preclinical model of cerebral ischemia: A systematic review with meta-analysis. Stem Cell Res. Ther. 2015, 6, 27. [Google Scholar] [CrossRef] [Green Version]
- Morishita, S.; Hokamura, K.; Yoshikawa, A.; Agata, N.; Tsutsui, Y.; Umemura, K.; Kumada, T. Different exercises can modulate the differentiation/maturation of neural stem/progenitor cells after photochemically induced focal cerebral infarction. Brain Behav. 2020, 10, e01535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boltze, J.; Modo, M.M.; Mays, R.W.; Taguchi, A.; Jolkkonen, J.; Savitz, S.I. Stem Cells as an Emerging Paradigm in Stroke 4: Advancing and Accelerating Preclinical Research. Stroke 2019, 50, 3299–3306. [Google Scholar] [CrossRef] [PubMed]
- Martino, G.; Pluchino, S. The therapeutic potential of neural stem cells. Nat. Rev. Neurosci. 2006, 7, 395–406. [Google Scholar] [CrossRef]
- Xiong, X.Y.; Liu, L.; Yang, Q.W. Functions and mechanisms of microglia/macrophages in neuroinflammation and neurogenesis after stroke. Prog. Neurobiol. 2016, 142, 23–44. [Google Scholar] [CrossRef]
- Emmons, R.; Niemiro, G.M.; De Lisio, M. Exercise as an Adjuvant Therapy for Hematopoietic Stem Cell Mobilization. Stem Cells Int. 2016, 2016, 7131359. [Google Scholar] [CrossRef] [Green Version]
- Le Blanc, K.; Mougiakakos, D. Multipotent mesenchymal stromal cells and the innate immune system. Nat. Rev. Immunol. 2012, 12, 383–396. [Google Scholar] [CrossRef]
- Nauta, A.J.; Fibbe, W.E. Immunomodulatory properties of mesenchymal stromal cells. Blood 2007, 110, 3499–3506. [Google Scholar] [CrossRef] [Green Version]
- English, K. Mechanisms of mesenchymal stromal cell immunomodulation. Immunol. Cell Biol. 2013, 91, 19–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crigler, L.; Robey, R.C.; Asawachaicharn, A.; Gaupp, D.; Phinney, D.G. Human mesenchymal stem cell subpopulations express a variety of neuro-regulatory molecules and promote neuronal cell survival and neuritogenesis. Exp. Neurol. 2006, 198, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Bhasin, A.; Srivastava, M.V.P.; Kumaran, S.S.; Mohanty, S.; Bhatia, R.; Bose, S.; Gaikwad, S.; Garg, A.; Airan, B. Autologous Mesenchymal Stem Cells in Chronic Stroke. Cerebrovasc. Dis. Extra 2011, 1, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Kiyose, R.; Sasaki, M.; Kataoka-Sasaki, Y.; Nakazaki, M.; Nagahama, H.; Magota, H.; Oka, S.; Ukai, R.; Takemura, M.; Yokoyama, T.; et al. Intravenous Infusion of Mesenchymal Stem Cells Enhances Therapeutic Efficacy of Reperfusion Therapy in Cerebral Ischemia. World Neurosurg. 2021, 149, e160–e169. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.-X.; Yuan, M.-Z.; Cheng, L.; Lin, L.-Z.; Du, H.-W.; Chen, R.-H.; Liu, N. Treadmill exercise enhances therapeutic potency of transplanted bone mesenchymal stem cells in cerebral ischemic rats via anti-apoptotic effects. BMC Neurosci. 2015, 16, 56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmidt, A.; Wellmann, J.; Schilling, M.; Strecker, J.K.; Sommer, C.; Schäbitz, W.R.; Diederich, K.; Minnerup, J. Meta-analysis of the efficacy of different training strategies in animal models of ischemic stroke. Stroke 2014, 45, 239–247. [Google Scholar] [CrossRef] [Green Version]
- Pin-Barre, C.; Constans, A.; Brisswalter, J.; Pellegrino, C.; Laurin, J. Effects of High- Versus Moderate-Intensity Training on Neuroplasticity and Functional Recovery After Focal Ischemia. Stroke 2017, 48, 2855–2864. [Google Scholar] [CrossRef] [Green Version]
- Evans, M.A.; Lim, R.; Kim, H.A.; Chu, H.X.; Gardiner-Mann, C.V.; Taylor, K.W.E.; Chan, C.T.; Brait, V.H.; Lee, S.; Dinh, Q.N.; et al. Acute or Delayed Systemic Administration of Human Amnion Epithelial Cells Improves Outcomes in Experimental Stroke. Stroke 2018, 49, 700–709. [Google Scholar] [CrossRef]
- Corbett, D.; Carmichael, S.T.; Murphy, T.H.; Jones, T.A.; Schwab, M.E.; Jolkkonen, J.; Clarkson, A.N.; Dancause, N.; Weiloch, T.; Johansen-Berg, H.; et al. Enhancing the alignment of the preclinical and clinical stroke recovery research pipeline: Consensus-based core recommendations from the Stroke Recovery and Rehabilitation Roundtable translational working group. Int. J. Stroke 2017, 12, 462–471. [Google Scholar] [CrossRef]
- Chen, P.J.; Kang, Y.D.; Lin, C.H.; Chen, S.Y.; Hsieh, C.H.; Chen, Y.Y.; Chiang, C.W.; Lee, W.; Hsu, C.Y.; Liao, L.D.; et al. Multitheragnostic Multi-GNRs Crystal-Seeded Magnetic Nanoseaurchin for Enhanced In Vivo Mesenchymal-Stem-Cell Homing, Multimodal Imaging, and Stroke Therapy. Adv. Mater. 2015, 27, 6488–6495. [Google Scholar] [CrossRef]
- Zhang, F.; Duan, X.; Lu, L.; Zhang, X.; Chen, M.; Mao, J.; Cao, M.; Shen, J. In Vivo Long-Term Tracking of Neural Stem Cells Transplanted into an Acute Ischemic Stroke model with Reporter Gene-Based Bimodal MR and Optical Imaging. Cell Transpl. 2017, 26, 1648–1662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, S.; Yoon, H.Y.; Jang, H.J.; Song, S.; Kim, W.; Park, J.; Lee, K.E.; Jeon, S.; Lee, S.; Lim, D.-K.; et al. Dual-Modal Imaging-Guided Precise Tracking of Bioorthogonally Labeled Mesenchymal Stem Cells in Mouse Brain Stroke. ACS Nano 2019, 13, 10991–11007. [Google Scholar] [CrossRef] [PubMed]
- Jasmin; de Souza, G.T.; Louzada, R.A.; Rosado-de-Castro, P.H.; Mendez-Otero, R.; Campos de Carvalho, A.C. Tracking stem cells with superparamagnetic iron oxide nanoparticles: Perspectives and considerations. Int. J. Nanomed. 2017, 12, 779–793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ravoori, M.K.; Margalit, O.; Singh, S.; Kim, S.-H.; Wei, W.; Menter, D.G.; DuBois, R.N.; Kundra, V. Magnetic Resonance Imaging and Bioluminescence Imaging for Evaluating Tumor Burden in Orthotopic Colon Cancer. Sci. Rep. 2019, 9, 6100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, J.; Hou, S.; Ding, H.; Liu, Z.; Song, M.; Qin, X.; Wang, X.; Yu, M.; Sun, Z.; Liu, J.; et al. In Vivo Tracking of Systemically Administered Allogeneic Bone Marrow Mesenchymal Stem Cells in Normal Rats through Bioluminescence Imaging. Stem Cells Int. 2016, 2016, 3970942. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strohschein, K.; Radojewski, P.; Winkler, T.; Duda, G.N.; Perka, C.; von Roth, P. In Vivo Bioluminescence Imaging—A Suitable Method to Track Mesenchymal Stromal Cells in a Skeletal Muscle Trauma. Open Orthop. J. 2015, 9, 262–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Samakova, A.; Gazova, A.; Sabova, N.; Valaskova, S.; Jurikova, M.; Kyselovic, J. The PI3k/Akt pathway is associated with angiogenesis, oxidative stress and survival of mesenchymal stem cells in pathophysiologic condition in ischemia. Physiol. Res. 2019, 68, S131–S138. [Google Scholar] [CrossRef] [PubMed]





| [Fe] (µg Fe/mL) | MTT (%) Mean ± SD | BLI (%) Mean ± SD | n |
|---|---|---|---|
| [0] | 99.875 ± 0.629 | 100 | 4 |
| [50] | 97.600 ± 0.589 | 96.925 ± 0.822 | 4 |
| Group | Blood Perfusion Mean ± SD | n |
|---|---|---|
| G2 | 72.15 ± 2.22 | 5 |
| G3 | 73.14 ± 2.60 | 5 |
| G4 | 72.76 ± 2.36 | 5 |
| G5 | 71.60 ± 2.16 | 5 |
| ANOVA Test | |||||
|---|---|---|---|---|---|
| Cases | Sum of Squares | df | Mean Square | F | p |
| Groups | 6.88 | 3 | 2.29 | 0.419 | 0.742 |
| Residuals | 87.54 | 16 | 5.47 | ||
| Week | Maximum Speed Mean ± SD (m Per Min) | N | |
|---|---|---|---|
| G4 | G5 | ||
| 1 | 12.60 ± 1.67 | 13.00 ± 2.24 | 10 |
| 2 | 16.40 ± 1.67 | 17.80 ± 3.03 | 10 |
| 3 | 14.60 ± 2.79 | 19.00 ± 2.45 | 10 |
| 4 | 16.00 ± 2.00 | 18.60 ± 2.88 | 10 |
| ANOVA Test | |||||
|---|---|---|---|---|---|
| Cases | Sum of Squares | df | Mean Square | F | p |
| Weeks | 137.800 | 3 | 45.933 | 8.006 | <0.001 |
| Groups | 48.400 | 1 | 48.400 | 8.436 | 0.007 |
| Week * Group | 22.200 | 3 | 7.400 | 1.290 | 0.295 |
| Residuals | 183.600 | 32 | 5.737 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nucci, M.P.; Oliveira, F.A.; Ferreira, J.M.; Pinto, Y.O.; Alves, A.H.; Mamani, J.B.; Nucci, L.P.; Valle, N.M.E.; Gamarra, L.F. Effect of Cell Therapy and Exercise Training in a Stroke Model, Considering the Cell Track by Molecular Image and Behavioral Analysis. Cells 2022, 11, 485. https://doi.org/10.3390/cells11030485
Nucci MP, Oliveira FA, Ferreira JM, Pinto YO, Alves AH, Mamani JB, Nucci LP, Valle NME, Gamarra LF. Effect of Cell Therapy and Exercise Training in a Stroke Model, Considering the Cell Track by Molecular Image and Behavioral Analysis. Cells. 2022; 11(3):485. https://doi.org/10.3390/cells11030485
Chicago/Turabian StyleNucci, Mariana P., Fernando A. Oliveira, João M. Ferreira, Yolanda O. Pinto, Arielly H. Alves, Javier B. Mamani, Leopoldo P. Nucci, Nicole M. E. Valle, and Lionel F. Gamarra. 2022. "Effect of Cell Therapy and Exercise Training in a Stroke Model, Considering the Cell Track by Molecular Image and Behavioral Analysis" Cells 11, no. 3: 485. https://doi.org/10.3390/cells11030485
APA StyleNucci, M. P., Oliveira, F. A., Ferreira, J. M., Pinto, Y. O., Alves, A. H., Mamani, J. B., Nucci, L. P., Valle, N. M. E., & Gamarra, L. F. (2022). Effect of Cell Therapy and Exercise Training in a Stroke Model, Considering the Cell Track by Molecular Image and Behavioral Analysis. Cells, 11(3), 485. https://doi.org/10.3390/cells11030485









