Impact of Glucocorticoid Use in Oncology in the Immunotherapy Era
Abstract
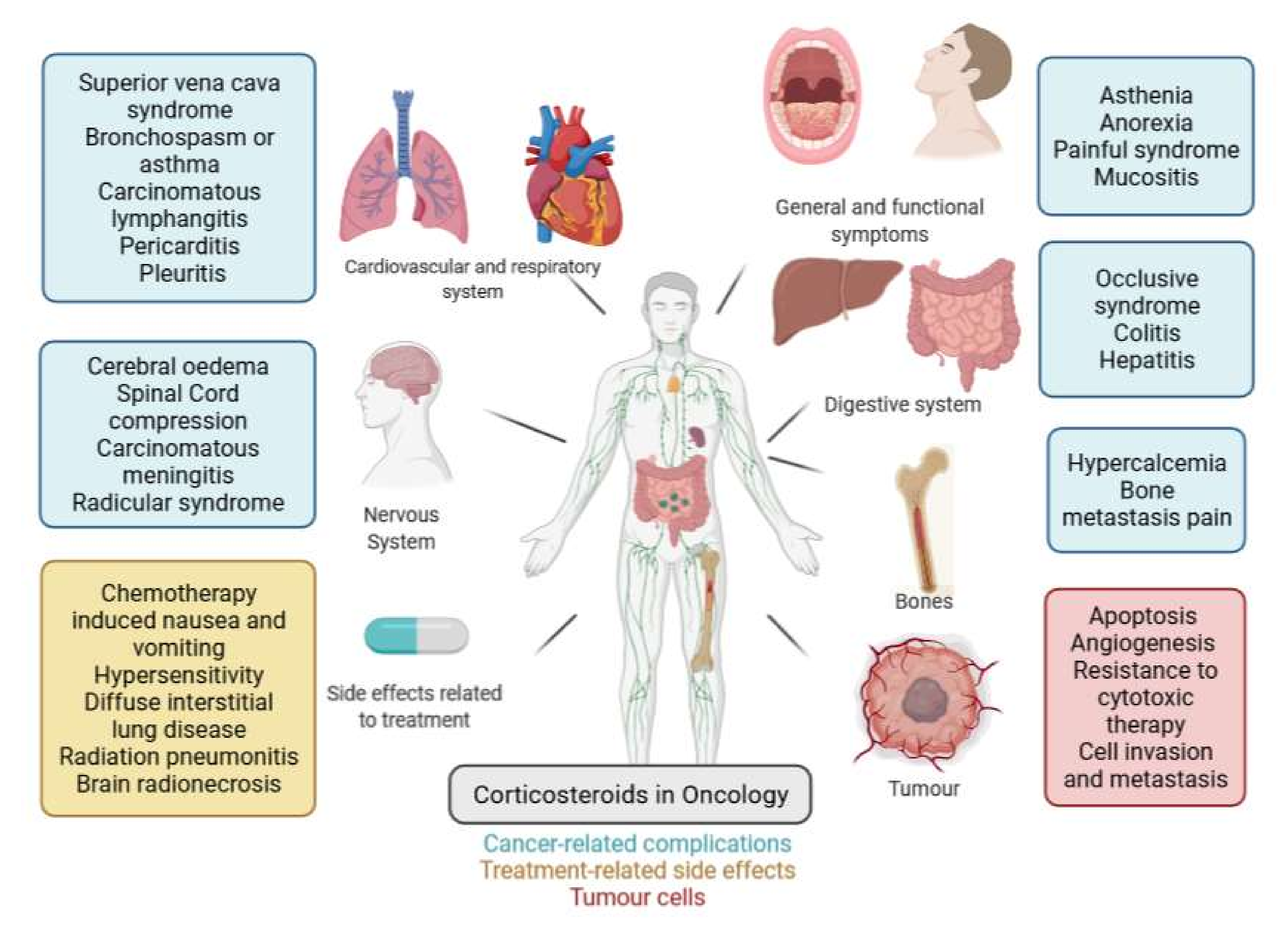
:1. Background: The Historical Role of Glucocorticoids in Cancer Treatment
1.1. Effect of Glucocorticoids on Tumour Cells: Pro- or Anti-Tumour?
1.2. Effect of Glucocorticoids on Cancer-Related Symptoms
1.3. Effect of Corticosteroids on Treatment Side Effects
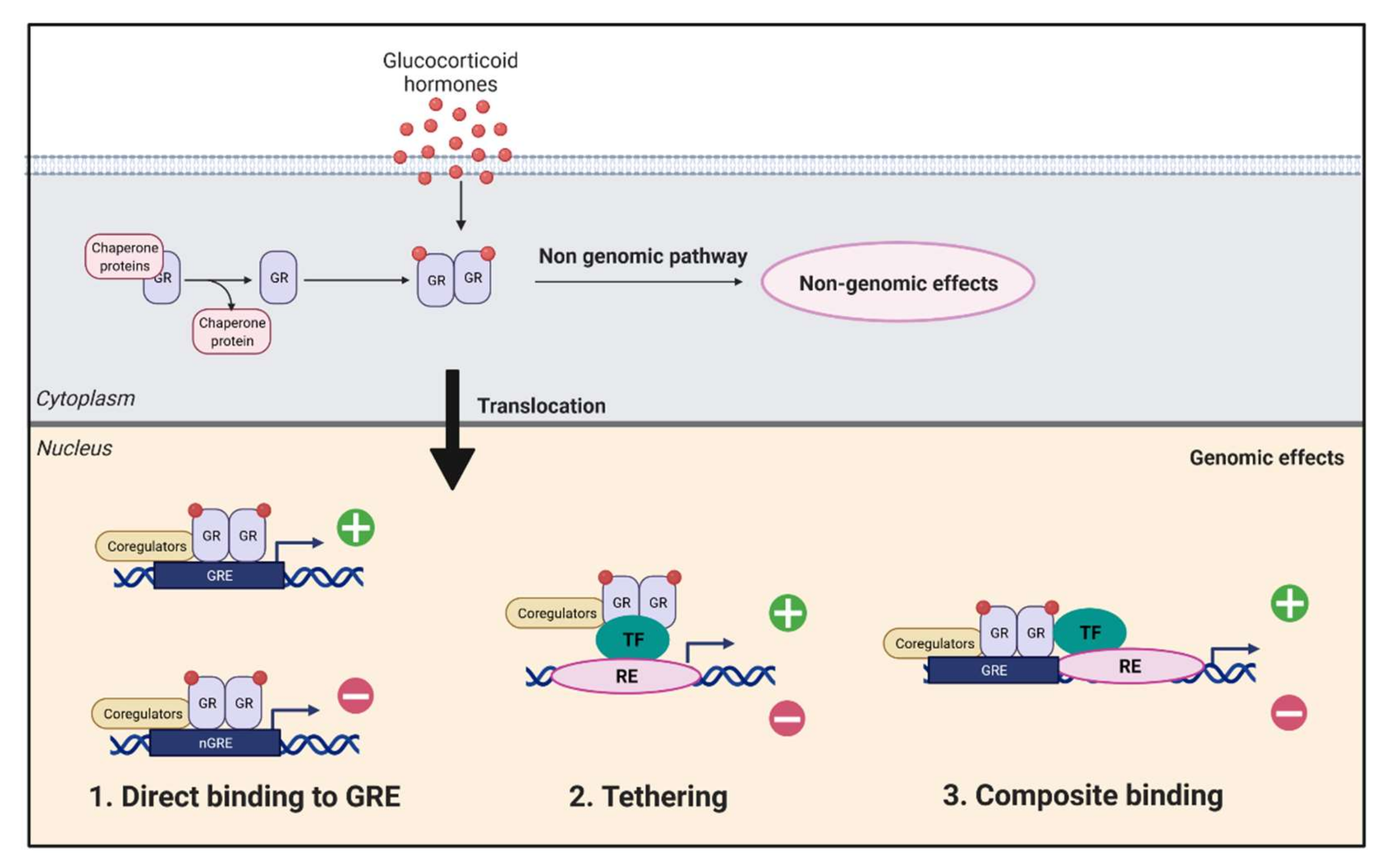
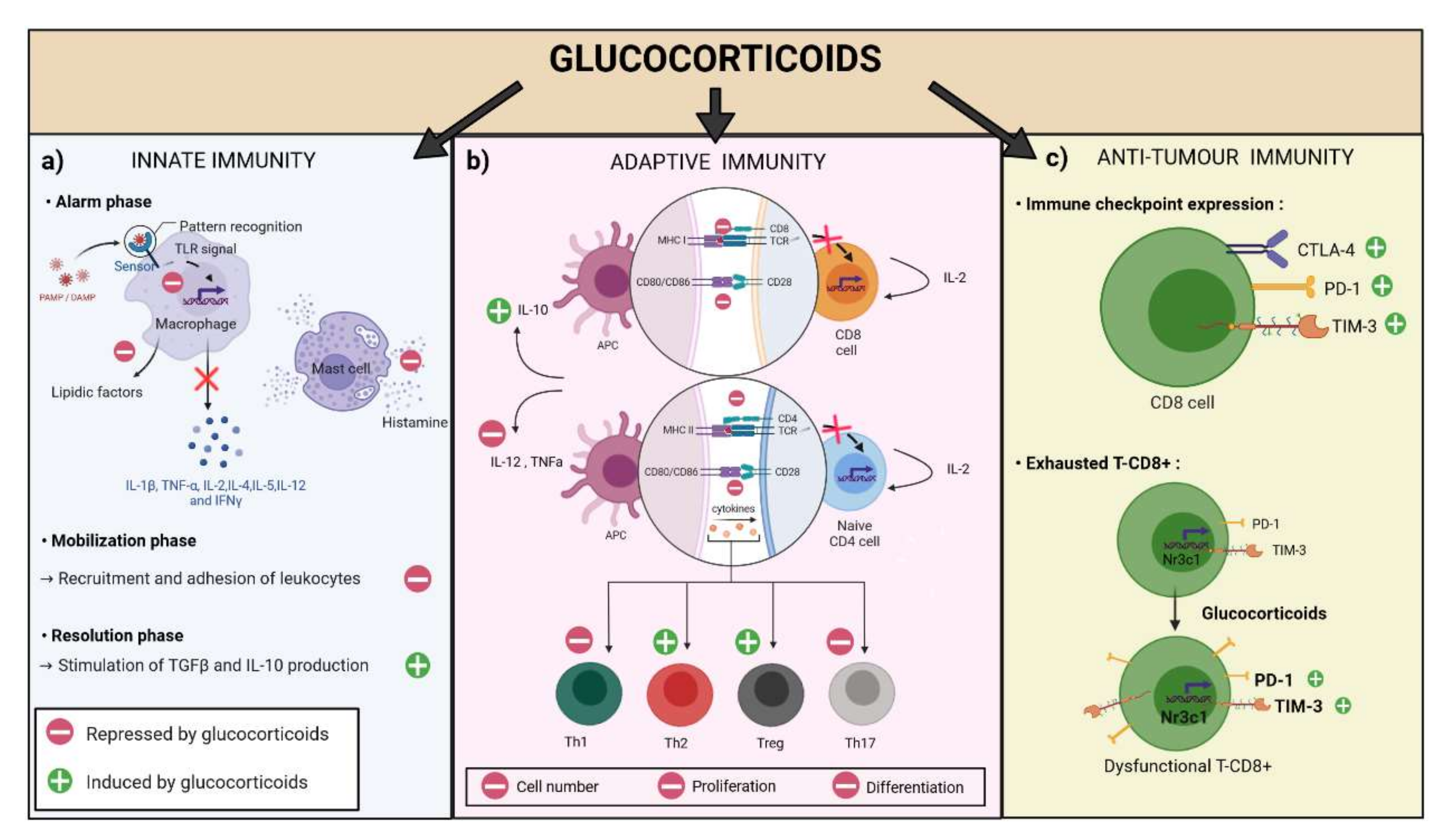
2. Effects of Glucocorticoids on the Immune System and the Immune Response in the Setting of Cancer
2.1. Effect of Glucocorticoids on Innate Immunity
2.2. Effect of Glucocorticoids on Adaptive Immunity
2.3. Effects of Glucocorticoids on Anti-Tumoral Immunity
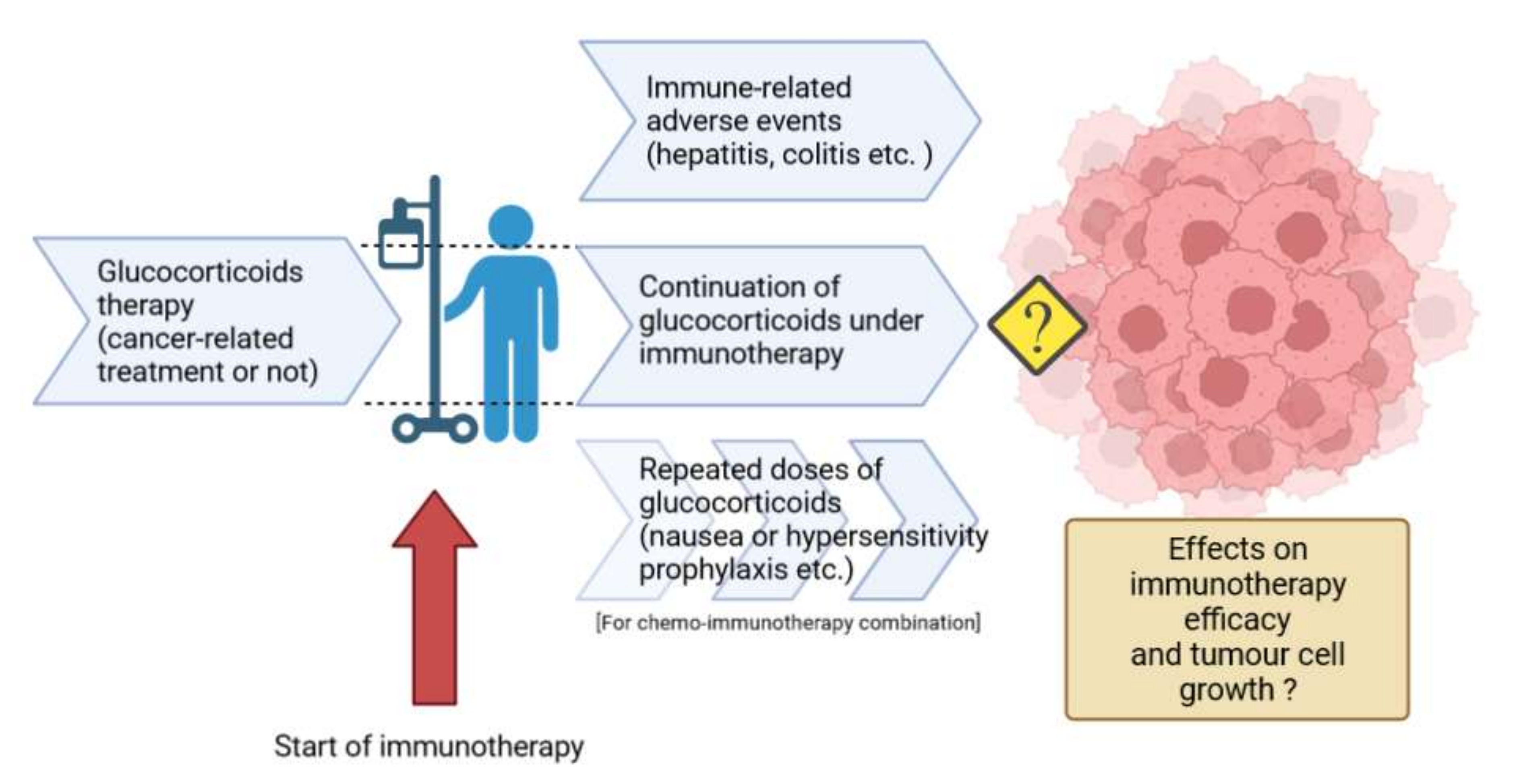
3. Challenges of Corticosteroid Use in the Immunotherapy Era
3.1. GCs to Manage Immune-Related Adverse Events Caused by Immunotherapy
3.2. Influence of Corticosteroids on the Efficacy of Immunotherapy
3.3. Role of Corticosteroids in Immunotherapy-Chemotherapy Associations
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pufall, M.A. Glucocorticoids and Cancer. Adv. Exp. Med. Biol. 2015, 872, 315–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Z.; Malone, M.H.; He, H.; McColl, K.S.; Distelhorst, C.W. Microarray Analysis Uncovers the Induction of the Proapoptotic BH3-Only Protein Bim in Multiple Models of Glucocorticoid-Induced Apoptosis. J. Biol. Chem. 2003, 278, 23861–23867. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Planey, S.L.; Litwack, G. Glucocorticoid-Induced Apoptosis in Lymphocytes. Biochem. Biophys. Res. Commun. 2000, 279, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Greenstein, S.; Ghias, K.; Krett, N.L.; Rosen, S.T. Mechanisms of Glucocorticoid-Mediated Apoptosis in Hematological Malignancies. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2002, 8, 1681–1694. [Google Scholar]
- Grugan, K.D.; Ma, C.; Singhal, S.; Krett, N.L.; Rosen, S.T. Dual Regulation of Glucocorticoid-Induced Leucine Zipper (GILZ) by the Glucocorticoid Receptor and the PI3-Kinase/AKT Pathways in Multiple Myeloma. J. Steroid Biochem. Mol. Biol. 2008, 110, 244–254. [Google Scholar] [CrossRef] [Green Version]
- Tissing, W.J.E.; den Boer, M.L.; Meijerink, J.P.P.; Menezes, R.X.; Swagemakers, S.; van der Spek, P.J.; Sallan, S.E.; Armstrong, S.A.; Pieters, R. Genomewide Identification of Prednisolone-Responsive Genes in Acute Lymphoblastic Leukemia Cells. Blood 2007, 109, 3929–3935. [Google Scholar] [CrossRef] [Green Version]
- Raab, M.S.; Podar, K.; Breitkreutz, I.; Richardson, P.G.; Anderson, K.C. Multiple Myeloma. Lancet 2009, 374, 324–339. [Google Scholar] [CrossRef]
- Real, P.J.; Tosello, V.; Palomero, T.; Castillo, M.; Hernando, E.; de Stanchina, E.; Sulis, M.L.; Barnes, K.; Sawai, C.; Homminga, I.; et al. Gamma-Secretase Inhibitors Reverse Glucocorticoid Resistance in T Cell Acute Lymphoblastic Leukemia. Nat. Med. 2009, 15, 50–58. [Google Scholar] [CrossRef] [Green Version]
- Wei, G.; Twomey, D.; Lamb, J.; Schlis, K.; Agarwal, J.; Stam, R.W.; Opferman, J.T.; Sallan, S.E.; den Boer, M.L.; Pieters, R.; et al. Gene Expression-Based Chemical Genomics Identifies Rapamycin as a Modulator of MCL1 and Glucocorticoid Resistance. Cancer Cell 2006, 10, 331–342. [Google Scholar] [CrossRef] [Green Version]
- Holleman, A.; Cheok, M.H.; den Boer, M.L.; Yang, W.; Veerman, A.J.P.; Kazemier, K.M.; Pei, D.; Cheng, C.; Pui, C.-H.; Relling, M.V.; et al. Gene-Expression Patterns in Drug-Resistant Acute Lymphoblastic Leukemia Cells and Response to Treatment. N. Engl. J. Med. 2004, 351, 533–542. [Google Scholar] [CrossRef]
- Keith, B.D. Systematic Review of the Clinical Effect of Glucocorticoids on Nonhematologic Malignancy. BMC Cancer 2008, 8, 84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rubenstein, N.M.; Guan, Y.; Woo, P.L.; Firestone, G.L. Glucocorticoid Down-Regulation of RhoA Is Required for the Steroid-Induced Organization of the Junctional Complex and Tight Junction Formation in Rat Mammary Epithelial Tumor Cells. J. Biol. Chem. 2003, 278, 10353–10360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, Y.; Izumi, K.; Li, Y.; Ishiguro, H.; Miyamoto, H. Contrary Regulation of Bladder Cancer Cell Proliferation and Invasion by Dexamethasone-Mediated Glucocorticoid Receptor Signals. Mol. Cancer Ther. 2012, 11, 2621–2632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Law, M.E.; Corsino, P.E.; Jahn, S.C.; Davis, B.J.; Chen, S.; Patel, B.; Pham, K.; Lu, J.; Sheppard, B.; Nørgaard, P.; et al. Glucocorticoids and Histone Deacetylase Inhibitors Cooperate to Block the Invasiveness of Basal-like Breast Cancer Cells through Novel Mechanisms. Oncogene 2013, 32, 1316–1329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Folkman, J.; Langer, R.; Linhardt, R.J.; Haudenschild, C.; Taylor, S. Angiogenesis Inhibition and Tumor Regression Caused by Heparin or a Heparin Fragment in the Presence of Cortisone. Science 1983, 221, 719–725. [Google Scholar] [CrossRef] [PubMed]
- Karmakar, S.; Jin, Y.; Nagaich, A.K. Interaction of Glucocorticoid Receptor (GR) with Estrogen Receptor (ER) α and Activator Protein 1 (AP1) in Dexamethasone-Mediated Interference of ERα Activity. J. Biol. Chem. 2013, 288, 24020–24034. [Google Scholar] [CrossRef] [Green Version]
- Sahu, B.; Laakso, M.; Pihlajamaa, P.; Ovaska, K.; Sinielnikov, I.; Hautaniemi, S.; Jänne, O.A. FoxA1 Specifies Unique Androgen and Glucocorticoid Receptor Binding Events in Prostate Cancer Cells. Cancer Res. 2013, 73, 1570–1580. [Google Scholar] [CrossRef] [Green Version]
- Lin, K.-T.; Wang, L.-H. New Dimension of Glucocorticoids in Cancer Treatment. Steroids 2016, 111, 84–88. [Google Scholar] [CrossRef] [Green Version]
- Lin, K.-T.; Yeh, Y.-M.; Chuang, C.-M.; Yang, S.Y.; Chang, J.-W.; Sun, S.-P.; Wang, Y.-S.; Chao, K.-C.; Wang, L.-H. Glucocorticoids Mediate Induction of MicroRNA-708 to Suppress Ovarian Cancer Metastasis through Targeting Rap1B. Nat. Commun. 2015, 6, 5917. [Google Scholar] [CrossRef] [Green Version]
- Volden, P.A.; Conzen, S.D. The Influence of Glucocorticoid Signaling on Tumor Progression. Brain. Behav. Immun. 2013, 30 (Suppl. S1), S26–S31. [Google Scholar] [CrossRef] [Green Version]
- Obradović, M.M.S.; Hamelin, B.; Manevski, N.; Couto, J.P.; Sethi, A.; Coissieux, M.-M.; Münst, S.; Okamoto, R.; Kohler, H.; Schmidt, A.; et al. Glucocorticoids Promote Breast Cancer Metastasis. Nature 2019, 567, 540–544. [Google Scholar] [CrossRef] [PubMed]
- Mikosz, C.A.; Brickley, D.R.; Sharkey, M.S.; Moran, T.W.; Conzen, S.D. Glucocorticoid Receptor-Mediated Protection from Apoptosis Is Associated with Induction of the Serine/Threonine Survival Kinase Gene, Sgk-1. J. Biol. Chem. 2001, 276, 16649–16654. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, W.; Chaudhuri, S.; Brickley, D.R.; Pang, D.; Karrison, T.; Conzen, S.D. Microarray Analysis Reveals Glucocorticoid-Regulated Survival Genes That Are Associated with Inhibition of Apoptosis in Breast Epithelial Cells. Cancer Res. 2004, 64, 1757–1764. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Münstedt, K.; Borces, D.; Bohlmann, M.K.; Zygmunt, M.; von Georgi, R. Glucocorticoid Administration in Antiemetic Therapy: Is It Safe? Cancer 2004, 101, 1696–1702. [Google Scholar] [CrossRef]
- Herr, I.; Ucur, E.; Herzer, K.; Okouoyo, S.; Ridder, R.; Krammer, P.H.; von Knebel Doeberitz, M.; Debatin, K.-M. Glucocorticoid Cotreatment Induces Apoptosis Resistance toward Cancer Therapy in Carcinomas. Cancer Res. 2003, 63, 3112–3120. [Google Scholar]
- Belova, L.; Delgado, B.; Kocherginsky, M.; Melhem, A.; Olopade, O.I.; Conzen, S.D. Glucocorticoid Receptor Expression in Breast Cancer Associates with Older Patient Age. Breast Cancer Res. Treat. 2009, 116, 441–447. [Google Scholar] [CrossRef] [Green Version]
- McNamara, K.M.; Kannai, A.; Sasano, H. Possible Roles for Glucocorticoid Signalling in Breast Cancer. Mol. Cell. Endocrinol. 2018, 466, 38–50. [Google Scholar] [CrossRef]
- Zhidkova, E.M.; Lylova, E.S.; Savinkova, A.V.; Mertsalov, S.A.; Kirsanov, K.I.; Belitsky, G.A.; Yakubovskaya, M.G.; Lesovaya, E.A. A Brief Overview of the Paradoxical Role of Glucocorticoids in Breast Cancer. Breast Cancer Basic Clin. Res. 2020, 14, 1178223420974667. [Google Scholar] [CrossRef]
- Paulsen, O.; Klepstad, P.; Rosland, J.H.; Aass, N.; Albert, E.; Fayers, P.; Kaasa, S. Efficacy of Methylprednisolone on Pain, Fatigue, and Appetite Loss in Patients with Advanced Cancer Using Opioids: A Randomized, Placebo-Controlled, Double-Blind Trial. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2014, 32, 3221–3228. [Google Scholar] [CrossRef]
- Yennurajalingam, S.; Frisbee-Hume, S.; Palmer, J.L.; Delgado-Guay, M.O.; Bull, J.; Phan, A.T.; Tannir, N.M.; Litton, J.K.; Reddy, A.; Hui, D.; et al. Reduction of Cancer-Related Fatigue with Dexamethasone: A Double-Blind, Randomized, Placebo-Controlled Trial in Patients with Advanced Cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2013, 31, 3076–3082. [Google Scholar] [CrossRef]
- Zimmermann, M.; Drings, P. Guidelines for therapy of pain in cancer patients. In Pain in the Cancer Patient; Recent Results in Cancer Research; Springer: Berlin/Heidelberg, Germany, 1984; Volume 89, pp. 1–12. [Google Scholar] [CrossRef]
- Chouahnia, K.; Luu, M.; Baba-Hamed, N.; Des Guetz, G. Bone metastases pain in the elderly. Rev. Med. Suisse 2009, 5, 1126, 1128, 1130, passim. [Google Scholar] [PubMed]
- Haywood, A.; Good, P.; Khan, S.; Leupp, A.; Jenkins-Marsh, S.; Rickett, K.; Hardy, J.R. Corticosteroids for the Management of Cancer-Related Pain in Adults. Cochrane Database Syst. Rev. 2015, 2015, CD010756. [Google Scholar] [CrossRef] [Green Version]
- Leppert, W.; Buss, T. The Role of Corticosteroids in the Treatment of Pain in Cancer Patients. Curr. Pain Headache Rep. 2012, 16, 307–313. [Google Scholar] [CrossRef] [Green Version]
- Lin, R.J.; Adelman, R.D.; Mehta, S.S. Dyspnea in Palliative Care: Expanding the Role of Corticosteroids. J. Palliat. Med. 2012, 15, 834–837. [Google Scholar] [CrossRef]
- Dudgeon, D.J.; Lertzman, M. Dyspnea in the Advanced Cancer Patient. J. Pain Symptom Manag. 1998, 16, 212–219. [Google Scholar] [CrossRef]
- Haywood, A.; Duc, J.; Good, P.; Khan, S.; Rickett, K.; Vayne-Bossert, P.; Hardy, J.R. Systemic Corticosteroids for the Management of Cancer-Related Breathlessness (Dyspnoea) in Adults. Cochrane Database Syst. Rev. 2019, 2, CD012704. [Google Scholar] [CrossRef] [Green Version]
- Hui, D.; Kilgore, K.; Frisbee-Hume, S.; Park, M.; Tsao, A.; Delgado Guay, M.; Lu, C.; William, W.; Pisters, K.; Eapen, G.; et al. Dexamethasone for Dyspnea in Cancer Patients: A Pilot Double-Blind, Randomized, Controlled Trial. J. Pain Symptom Manag. 2016, 52, 8–16.e1. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.S.; Shi, Q.; Williams, L.A.; Mao, L.; Cleeland, C.S.; Komaki, R.R.; Mobley, G.M.; Liao, Z. Inflammatory Cytokines Are Associated with the Development of Symptom Burden in Patients with NSCLC Undergoing Concurrent Chemoradiation Therapy. Brain. Behav. Immun. 2010, 24, 968–974. [Google Scholar] [CrossRef] [Green Version]
- Ryken, T.C.; McDermott, M.; Robinson, P.D.; Ammirati, M.; Andrews, D.W.; Asher, A.L.; Burri, S.H.; Cobbs, C.S.; Gaspar, L.E.; Kondziolka, D.; et al. The Role of Steroids in the Management of Brain Metastases: A Systematic Review and Evidence-Based Clinical Practice Guideline. J. Neurooncol. 2010, 96, 103–114. [Google Scholar] [CrossRef] [Green Version]
- Bollen, L.; Dijkstra, S.P.D.; Bartels, R.H.M.A.; de Graeff, A.; Poelma, D.L.H.; Brouwer, T.; Algra, P.R.; Kuijlen, J.M.A.; Minnema, M.C.; Nijboer, C.; et al. Clinical Management of Spinal Metastases-The Dutch National Guideline. Eur. J. Cancer 2018, 104, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Roth, P.; Happold, C.; Weller, M. Corticosteroid Use in Neuro-Oncology: An Update. Neuro-Oncol. Pract. 2015, 2, 6–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hardy, J.R.; Rees, E.; Ling, J.; Burman, R.; Feuer, D.; Broadley, K.; Stone, P. A Prospective Survey of the Use of Dexamethasone on a Palliative Care Unit. Palliat. Med. 2001, 15, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Nagpal, S.; Riess, J.; Wakelee, H. Treatment of Leptomeningeal Spread of NSCLC: A Continuing Challenge. Curr. Treat. Options Oncol. 2012, 13, 491–504. [Google Scholar] [CrossRef] [PubMed]
- Sodji, Q.; Kaminski, J.; Willey, C.; Kim, N.; Mourad, W.; Vender, J.; Dasher, B. Management of Metastatic Spinal Cord Compression. South. Med. J. 2017, 110, 586–593. [Google Scholar] [CrossRef]
- Bach, F.; Larsen, B.H.; Rohde, K.; Børgesen, S.E.; Gjerris, F.; Bøge-Rasmussen, T.; Agerlin, N.; Rasmusson, B.; Stjernholm, P.; Sørensen, P.S. Metastatic Spinal Cord Compression. Occurrence, Symptoms, Clinical Presentations and Prognosis in 398 Patients with Spinal Cord Compression. Acta Neurochir. 1990, 107, 37–43. [Google Scholar] [CrossRef]
- Laval, G.; Marcelin-Benazech, B.; Guirimand, F.; Chauvenet, L.; Copel, L.; Durand, A.; Francois, E.; Gabolde, M.; Mariani, P.; Rebischung, C.; et al. Recommendations for Bowel Obstruction with Peritoneal Carcinomatosis. J. Pain Symptom Manag. 2014, 48, 75–91. [Google Scholar] [CrossRef]
- Desport, J.C.; Gory-Delabaere, G.; Blanc-Vincent, M.P.; Bachmann, P.; Béal, J.; Benamouzig, R.; Colomb, V.; Kere, D.; Melchior, J.C.; Nitenberg, G.; et al. Standards, Options and Recommendations for the Use of Appetite Stimulants in Oncology (2000). Br. J. Cancer 2003, 89 (Suppl. S1), S98–S100. [Google Scholar] [CrossRef] [Green Version]
- Miller, S.; McNutt, L.; McCann, M.-A.; McCorry, N. Use of Corticosteroids for Anorexia in Palliative Medicine: A Systematic Review. J. Palliat. Med. 2014, 17, 482–485. [Google Scholar] [CrossRef] [Green Version]
- Yennurajalingam, S.; Bruera, E. Role of Corticosteroids for Fatigue in Advanced Incurable Cancer: Is It a “wonder Drug” or “Deal with the Devil”. Curr. Opin. Support. Palliat. Care 2014, 8, 346–351. [Google Scholar] [CrossRef]
- Sturdza, A.; Millar, B.-A.; Bana, N.; Laperriere, N.; Pond, G.; Wong, R.K.S.; Bezjak, A. The Use and Toxicity of Steroids in the Management of Patients with Brain Metastases. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2008, 16, 1041–1048. [Google Scholar] [CrossRef] [PubMed]
- Grunberg, S.M. Antiemetic Activity of Corticosteroids in Patients Receiving Cancer Chemotherapy: Dosing, Efficacy, and Tolerability Analysis. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2007, 18, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Gupta, K.; Walton, R.; Kataria, S.P. Chemotherapy-Induced Nausea and Vomiting: Pathogenesis, Recommendations, and New Trends. Cancer Treat. Res. Commun. 2021, 26, 100278. [Google Scholar] [CrossRef] [PubMed]
- Van Ryckeghem, F. Corticosteroids, the Oldest Agent in the Prevention of Chemotherapy-Induced Nausea and Vomiting: What about the Guidelines? J. Transl. Intern. Med. 2016, 4, 46–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barnes, P.J. Anti-Inflammatory Actions of Glucocorticoids: Molecular Mechanisms. Clin. Sci. 1998, 94, 557–572. [Google Scholar] [CrossRef] [Green Version]
- Diakos, E.A.; Gallos, I.D.; El-Shunnar, S.; Clarke, M.; Kazi, R.; Mehanna, H. Dexamethasone Reduces Pain, Vomiting and Overall Complications Following Tonsillectomy in Adults: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Clin. Otolaryngol. Off. J. ENT-UK Off. J. Neth. Soc. Oto-Rhino-Laryngol. Cervico-Facial Surg. 2011, 36, 531–542. [Google Scholar] [CrossRef]
- Chu, C.-C.; Hsing, C.-H.; Shieh, J.-P.; Chien, C.-C.; Ho, C.-M.; Wang, J.-J. The Cellular Mechanisms of the Antiemetic Action of Dexamethasone and Related Glucocorticoids against Vomiting. Eur. J. Pharmacol. 2014, 722, 48–54. [Google Scholar] [CrossRef]
- Sapolsky, R.M.; Romero, L.M.; Munck, A.U. How Do Glucocorticoids Influence Stress Responses? Integrating Permissive, Suppressive, Stimulatory, and Preparative Actions. Endocr. Rev. 2000, 21, 55–89. [Google Scholar] [CrossRef] [Green Version]
- Santini, D.; Vincenzi, B.; Fossati, C.; D’Angelillo, R.M.; Patti, G.; Bianco, V.; Avvisati, G.; Tonini, G. Prevention of Delayed Emesis Induced by Moderately Emetogenic Chemotherapy in Patients with Acute Emesis: A Pilot Study with ACTH-Depot plus Tropisetron. Med. Oncol. 2001, 18, 131–135. [Google Scholar] [CrossRef]
- Mantovani, G.; Maccio, A.; Massa, E.; Lai, P.; Esu, S. Cisplatin Induces Serotonin Release from Human Peripheral Blood Mononuclear Cells of Cancer Patients and Methylprednisolone Inhibits This Effect. Oncol. Rep. 1997, 4, 1051–1053. [Google Scholar] [CrossRef]
- Williamson, J.D.; Sadofsky, L.R.; Hart, S.P. The Pathogenesis of Bleomycin-Induced Lung Injury in Animals and Its Applicability to Human Idiopathic Pulmonary Fibrosis. Exp. Lung Res. 2015, 41, 57–73. [Google Scholar] [CrossRef] [PubMed]
- Ter Heine, R.; van den Bosch, R.T.A.; Schaefer-Prokop, C.M.; Lankheet, N.a.G.; Beijnen, J.H.; Staaks, G.H.A.; van der Westerlaken, M.M.; Malingré, M.M.; van den Brand, J.J.G. Fatal Interstitial Lung Disease Associated with High Erlotinib and Metabolite Levels. A Case Report and a Review of the Literature. Lung Cancer 2012, 75, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Nishino, M.; Hatabu, H.; Hodi, F.S.; Ramaiya, N.H. Drug-Related Pneumonitis in the Era of Precision Cancer Therapy. JCO Precis. Oncol. 2017, 1, PO.17.00026. [Google Scholar] [CrossRef] [PubMed]
- Tarantino, P.; Modi, S.; Tolaney, S.M.; Cortés, J.; Hamilton, E.P.; Kim, S.-B.; Toi, M.; Andrè, F.; Curigliano, G. Interstitial Lung Disease Induced by Anti-ERBB2 Antibody-Drug Conjugates: A Review. JAMA Oncol. 2021, 7, 1873–1881. [Google Scholar] [CrossRef] [PubMed]
- Vahid, B.; Marik, P.E. Pulmonary Complications of Novel Antineoplastic Agents for Solid Tumors. Chest 2008, 133, 528–538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chow, E.; Meyer, R.M.; Ding, K.; Nabid, A.; Chabot, P.; Wong, P.; Ahmed, S.; Kuk, J.; Dar, A.R.; Mahmud, A.; et al. Dexamethasone in the Prophylaxis of Radiation-Induced Pain Flare after Palliative Radiotherapy for Bone Metastases: A Double-Blind, Randomised Placebo-Controlled, Phase 3 Trial. Lancet Oncol. 2015, 16, 1463–1472. [Google Scholar] [CrossRef]
- Liyanage, C.K.; Galappatthy, P.; Seneviratne, S.L. Corticosteroids in Management of Anaphylaxis; a Systematic Review of Evidence. Eur. Ann. Allergy Clin. Immunol. 2017, 49, 196–207. [Google Scholar] [CrossRef] [Green Version]
- Roselló, S.; Blasco, I.; García Fabregat, L.; Cervantes, A.; Jordan, K.; ESMO Guidelines Committee. Management of Infusion Reactions to Systemic Anticancer Therapy: ESMO Clinical Practice Guidelines. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2017, 28, iv100–iv118. [Google Scholar] [CrossRef]
- Syrigou, E.; Triantafyllou, O.; Makrilia, N.; Kaklamanos, I.; Kotanidou, A.; Manolopoulos, L.; Syrigos, K. Acute Hypersensitivity Reactions to Chemotherapy Agents: An Overview. Inflamm. Allergy Drug Targets 2010, 9, 206–213. [Google Scholar] [CrossRef]
- Zanotti, K.M.; Markman, M. Prevention and Management of Antineoplastic-Induced Hypersensitivity Reactions. Drug Saf. 2001, 24, 767–779. [Google Scholar] [CrossRef]
- Gennari, A.; Salvadori, B.; Tognoni, A.; Conte, P.F. Rapid Intravenous Premedication with Dexamethasone Prevents Hypersensitivity Reactions to Paclitaxel. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 1996, 7, 978–979. [Google Scholar] [CrossRef] [PubMed]
- Hardy, J.; Haywood, A.; Rickett, K.; Sallnow, L.; Good, P. Practice Review: Evidence-Based Quality Use of Corticosteroids in the Palliative Care of Patients with Advanced Cancer. Palliat. Med. 2021, 35, 461–472. [Google Scholar] [CrossRef] [PubMed]
- Arlt, W.; Stewart, P.M. Adrenal Corticosteroid Biosynthesis, Metabolism, and Action. Endocrinol. Metab. Clin. N. Am. 2005, 34, 293–313, viii. [Google Scholar] [CrossRef] [PubMed]
- Auphan, N.; DiDonato, J.A.; Rosette, C.; Helmberg, A.; Karin, M. Immunosuppression by Glucocorticoids: Inhibition of NF-Kappa B Activity through Induction of I Kappa B Synthesis. Science 1995, 270, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Rhen, T.; Cidlowski, J.A. Antiinflammatory Action of Glucocorticoids--New Mechanisms for Old Drugs. N. Engl. J. Med. 2005, 353, 1711–1723. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jonat, C.; Rahmsdorf, H.J.; Park, K.K.; Cato, A.C.; Gebel, S.; Ponta, H.; Herrlich, P. Antitumor Promotion and Antiinflammation: Down-Modulation of AP-1 (Fos/Jun) Activity by Glucocorticoid Hormone. Cell 1990, 62, 1189–1204. [Google Scholar] [CrossRef]
- Oakley, R.H.; Cidlowski, J.A. The Biology of the Glucocorticoid Receptor: New Signaling Mechanisms in Health and Disease. J. Allergy Clin. Immunol. 2013, 132, 1033–1044. [Google Scholar] [CrossRef] [Green Version]
- Barrat, F.J.; Cua, D.J.; Boonstra, A.; Richards, D.F.; Crain, C.; Savelkoul, H.F.; de Waal-Malefyt, R.; Coffman, R.L.; Hawrylowicz, C.M.; O’Garra, A. In Vitro Generation of Interleukin 10-Producing Regulatory CD4(+) T Cells Is Induced by Immunosuppressive Drugs and Inhibited by T Helper Type 1 (Th1)- and Th2-Inducing Cytokines. J. Exp. Med. 2002, 195, 603–616. [Google Scholar] [CrossRef]
- Panettieri, R.A.; Schaafsma, D.; Amrani, Y.; Koziol-White, C.; Ostrom, R.; Tliba, O. Non-Genomic Effects of Glucocorticoids: An Updated View. Trends Pharmacol. Sci. 2019, 40, 38–49. [Google Scholar] [CrossRef]
- Miyata, M.; Lee, J.-Y.; Susuki-Miyata, S.; Wang, W.Y.; Xu, H.; Kai, H.; Kobayashi, K.S.; Flavell, R.A.; Li, J.-D. Glucocorticoids Suppress Inflammation via the Upregulation of Negative Regulator IRAK-M. Nat. Commun. 2015, 6, 6062. [Google Scholar] [CrossRef] [Green Version]
- Beaulieu, E.; Morand, E.F. Role of GILZ in Immune Regulation, Glucocorticoid Actions and Rheumatoid Arthritis. Nat. Rev. Rheumatol. 2011, 7, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Brattsand, R.; Linden, M. Cytokine Modulation by Glucocorticoids: Mechanisms and Actions in Cellular Studies. Aliment. Pharmacol. Ther. 1996, 10 (Suppl. S2), 81–90, discussion 91-92. [Google Scholar] [CrossRef]
- Grosman, N.; Jensen, S.M. Influence of Glucocorticoids on Histamine Release and 45calcium Uptake by Isolated Rat Mast Cells. Agents Actions 1984, 14, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Crocker, I.C.; Zhou, C.Y.; Bewtra, A.K.; Kreutner, W.; Townley, R.G. Glucocorticosteroids Inhibit Leukotriene Production. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 1997, 78, 497–505. [Google Scholar] [CrossRef]
- Lewis, G.D.; Campbell, W.B.; Johnson, A.R. Inhibition of Prostaglandin Synthesis by Glucocorticoids in Human Endothelial Cells. Endocrinology 1986, 119, 62–69. [Google Scholar] [CrossRef]
- Cronstein, B.N.; Kimmel, S.C.; Levin, R.I.; Martiniuk, F.; Weissmann, G. A Mechanism for the Antiinflammatory Effects of Corticosteroids: The Glucocorticoid Receptor Regulates Leukocyte Adhesion to Endothelial Cells and Expression of Endothelial-Leukocyte Adhesion Molecule 1 and Intercellular Adhesion Molecule 1. Proc. Natl. Acad. Sci. USA 1992, 89, 9991–9995. [Google Scholar] [CrossRef] [Green Version]
- Pitzalis, C.; Pipitone, N.; Perretti, M. Glucocorticoids and Leukocyte Adhesion. In Glucocorticoids; Goulding, N.J., Flower, R.J., Eds.; Milestones in Drug Therapy MDT; Birkhäuser: Basel, Switzerland, 2001; pp. 105–118. ISBN 9783034883481. [Google Scholar]
- Ehrchen, J.M.; Roth, J.; Barczyk-Kahlert, K. More Than Suppression: Glucocorticoid Action on Monocytes and Macrophages. Front. Immunol. 2019, 10, 2028. [Google Scholar] [CrossRef] [Green Version]
- Shapouri-Moghaddam, A.; Mohammadian, S.; Vazini, H.; Taghadosi, M.; Esmaeili, S.-A.; Mardani, F.; Seifi, B.; Mohammadi, A.; Afshari, J.T.; Sahebkar, A. Macrophage Plasticity, Polarization, and Function in Health and Disease. J. Cell. Physiol. 2018, 233, 6425–6440. [Google Scholar] [CrossRef]
- Iorgulescu, J.B.; Gokhale, P.C.; Speranza, M.C.; Eschle, B.K.; Poitras, M.J.; Wilkens, M.K.; Soroko, K.M.; Chhoeu, C.; Knott, A.; Gao, Y.; et al. Concurrent Dexamethasone Limits the Clinical Benefit of Immune Checkpoint Blockade in Glioblastoma. Clin. Cancer Res. 2021, 27, 276–287. [Google Scholar] [CrossRef]
- Larangé, A.; Antonios, D.; Pallardy, M.; Kerdine-Römer, S. Glucocorticoids Inhibit Dendritic Cell Maturation Induced by Toll-like Receptor 7 and Toll-like Receptor 8. J. Leukoc. Biol. 2012, 91, 105–117. [Google Scholar] [CrossRef]
- Scudeletti, M.; Lanza, L.; Contini, P.; Puppo, F.; Indiveri, F. Modulation of MHC Gene Expression by Glucocorticoid Hormones. Int. Arch. Allergy Immunol. 1992, 99, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Cain, D.W.; Cidlowski, J.A. Immune Regulation by Glucocorticoids. Nat. Rev. Immunol. 2017, 17, 233–247. [Google Scholar] [CrossRef] [PubMed]
- Tsitoura, D.C.; Rothman, P.B. Enhancement of MEK/ERK Signaling Promotes Glucocorticoid Resistance in CD4+ T Cells. J. Clin. Investig. 2004, 113, 619–627. [Google Scholar] [CrossRef] [PubMed]
- Gillis, S.; Crabtree, G.R.; Smith, K.A. Glucocorticoid-Induced Inhibition of T Cell Growth Factor Production: I. The Effect on Mitogen-Induced Lymphocyte Proliferation. J. Immunol. 1979, 123, 1624–1631. [Google Scholar] [PubMed]
- Elenkov, I.J. Glucocorticoids and the Th1/Th2 Balance. Ann. N. Y. Acad. Sci. 2004, 1024, 138–146. [Google Scholar] [CrossRef]
- Liberman, A.C.; Budziñski, M.L.; Sokn, C.; Gobbini, R.P.; Steininger, A.; Arzt, E. Regulatory and Mechanistic Actions of Glucocorticoids on T and Inflammatory Cells. Front. Endocrinol. 2018, 9, 235. [Google Scholar] [CrossRef]
- Karagiannidis, C.; Akdis, M.; Holopainen, P.; Woolley, N.J.; Hense, G.; Rückert, B.; Mantel, P.-Y.; Menz, G.; Akdis, C.A.; Blaser, K.; et al. Glucocorticoids Upregulate FOXP3 Expression and Regulatory T Cells in Asthma. J. Allergy Clin. Immunol. 2004, 114, 1425–1433. [Google Scholar] [CrossRef]
- Jones, S.A.; Perera, D.N.; Fan, H.; Russ, B.E.; Harris, J.; Morand, E.F. GILZ Regulates Th17 Responses and Restrains IL-17-Mediated Skin Inflammation. J. Autoimmun. 2015, 61, 73–80. [Google Scholar] [CrossRef]
- Yosef, N.; Shalek, A.K.; Gaublomme, J.T.; Jin, H.; Lee, Y.; Awasthi, A.; Wu, C.; Karwacz, K.; Xiao, S.; Jorgolli, M.; et al. Dynamic Regulatory Network Controlling TH17 Cell Differentiation. Nature 2013, 496, 461–468. [Google Scholar] [CrossRef]
- Dunn, G.P.; Old, L.J.; Schreiber, R.D. The Immunobiology of Cancer Immunosurveillance and Immunoediting. Immunity 2004, 21, 137–148. [Google Scholar] [CrossRef] [Green Version]
- Caplan, L.; Wolfe, F.; Russell, A.S.; Michaud, K. Corticosteroid Use in Rheumatoid Arthritis: Prevalence, Predictors, Correlates, and Outcomes. J. Rheumatol. 2007, 34, 696–705. [Google Scholar] [PubMed]
- Volmer, T.; Effenberger, T.; Trautner, C.; Buhl, R. Consequences of Long-Term Oral Corticosteroid Therapy and Its Side-Effects in Severe Asthma in Adults: A Focused Review of the Impact Data in the Literature. Eur. Respir. J. 2018, 52, 1800703. [Google Scholar] [CrossRef] [PubMed]
- Olnes, M.J.; Kotliarov, Y.; Biancotto, A.; Cheung, F.; Chen, J.; Shi, R.; Zhou, H.; Wang, E.; Tsang, J.S.; Nussenblatt, R.; et al. Effects of Systemically Administered Hydrocortisone on the Human Immunome. Sci. Rep. 2016, 6, 23002. [Google Scholar] [CrossRef] [Green Version]
- Gustafson, M.P.; Lin, Y.; New, K.C.; Bulur, P.A.; O’Neill, B.P.; Gastineau, D.A.; Dietz, A.B. Systemic Immune Suppression in Glioblastoma: The Interplay between CD14+HLA-DRlo/Neg Monocytes, Tumor Factors, and Dexamethasone. Neuro-Oncology 2010, 12, 631–644. [Google Scholar] [CrossRef] [Green Version]
- Chitadze, G.; Flüh, C.; Quabius, E.S.; Freitag-Wolf, S.; Peters, C.; Lettau, M.; Bhat, J.; Wesch, D.; Oberg, H.-H.; Luecke, S.; et al. In-Depth Immunophenotyping of Patients with Glioblastoma Multiforme: Impact of Steroid Treatment. Oncoimmunology 2017, 6, e1358839. [Google Scholar] [CrossRef] [PubMed]
- Aston, W.J.; Hope, D.E.; Cook, A.M.; Boon, L.; Dick, I.; Nowak, A.K.; Lake, R.A.; Lesterhuis, W.J. Dexamethasone Differentially Depletes Tumour and Peripheral Blood Lymphocytes and Can Impact the Efficacy of Chemotherapy/Checkpoint Blockade Combination Treatment. Oncoimmunology 2019, 8, e1641390. [Google Scholar] [CrossRef]
- Maxwell, R.; Luksik, A.; Garzon, T.; Hung, A.; Kim, E.; Wu, A.; Xia, Y.; Belcaid, Z.; Gorelick, N.; Choi, J.; et al. Contrasting Impact of Corticosteroids on Anti-PD-1 Immunotherapy Efficacy for Tumor Histologies Located within or Outside the Central Nervous System. OncoImmunology 2018, 7, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Giles, A.J.; Hutchinson, M.-K.N.D.; Sonnemann, H.M.; Jung, J.; Fecci, P.E.; Ratnam, N.M.; Zhang, W.; Song, H.; Bailey, R.; Davis, D.; et al. Dexamethasone-Induced Immunosuppression: Mechanisms and Implications for Immunotherapy. J. Immunother. Cancer 2018, 6, 51. [Google Scholar] [CrossRef]
- Xing, K.; Gu, B.; Zhang, P.; Wu, X. Dexamethasone Enhances Programmed Cell Death 1 (PD-1) Expression during T Cell Activation: An Insight into the Optimum Application of Glucocorticoids in Anti-Cancer Therapy. BMC Immunol. 2015, 16, 39. [Google Scholar] [CrossRef] [Green Version]
- Acharya, N.; Madi, A.; Zhang, H.; Klapholz, M.; Escobar, G.; Dulberg, S.; Christian, E.; Ferreira, M.; Dixon, K.O.; Fell, G.; et al. Endogenous Glucocorticoid Signaling Regulates CD8+ T Cell Differentiation and Development of Dysfunction in the Tumor Microenvironment. Immunity 2020, 53, 658–671.e6. [Google Scholar] [CrossRef]
- Sade-Feldman, M.; Yizhak, K.; Bjorgaard, S.L.; Ray, J.P.; de Boer, C.G.; Jenkins, R.W.; Lieb, D.J.; Chen, J.H.; Frederick, D.T.; Barzily-Rokni, M.; et al. Defining T Cell States Associated with Response to Checkpoint Immunotherapy in Melanoma. Cell 2018, 175, 998–1013.e20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keskin, D.B.; Anandappa, A.J.; Sun, J.; Tirosh, I.; Mathewson, N.D.; Li, S.; Oliveira, G.; Giobbie-Hurder, A.; Felt, K.; Gjini, E.; et al. Neoantigen Vaccine Generates Intratumoral T Cell Responses in Phase Ib Glioblastoma Trial. Nature 2019, 565, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Larkin, J.; Chiarion-Sileni, V.; Gonzalez, R.; Grob, J.-J.; Rutkowski, P.; Lao, C.D.; Cowey, C.L.; Schadendorf, D.; Wagstaff, J.; Dummer, R.; et al. Five-Year Survival with Combined Nivolumab and Ipilimumab in Advanced Melanoma. N. Engl. J. Med. 2019, 381, 1535–1546. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Powles, T.; Plimack, E.R.; Soulières, D.; Waddell, T.; Stus, V.; Gafanov, R.; Nosov, D.; Pouliot, F.; Melichar, B.; Vynnychenko, I.; et al. Pembrolizumab plus Axitinib versus Sunitinib Monotherapy as First-Line Treatment of Advanced Renal Cell Carcinoma (KEYNOTE-426): Extended Follow-up from a Randomised, Open-Label, Phase 3 Trial. Lancet Oncol. 2020, 21, 1563–1573. [Google Scholar] [CrossRef]
- Gadgeel, S.; Rodríguez-Abreu, D.; Speranza, G.; Esteban, E.; Felip, E.; Dómine, M.; Hui, R.; Hochmair, M.J.; Clingan, P.; Powell, S.F.; et al. Updated Analysis From KEYNOTE-189: Pembrolizumab or Placebo Plus Pemetrexed and Platinum for Previously Untreated Metastatic Nonsquamous Non-Small-Cell Lung Cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2020, 38, 1505–1517. [Google Scholar] [CrossRef] [PubMed]
- Pauken, K.E.; Dougan, M.; Rose, N.R.; Lichtman, A.H.; Sharpe, A.H. Adverse Events Following Cancer Immunotherapy: Obstacles and Opportunities. Trends Immunol. 2019, 40, 511–523. [Google Scholar] [CrossRef]
- Teraoka, S.; Fujimoto, D.; Morimoto, T.; Kawachi, H.; Ito, M.; Sato, Y.; Nagata, K.; Nakagawa, A.; Otsuka, K.; Uehara, K.; et al. Early Immune-Related Adverse Events and Association with Outcome in Advanced Non-Small Cell Lung Cancer Patients Treated with Nivolumab: A Prospective Cohort Study. J. Thorac. Oncol. Off. Publ. Int. Assoc. Study Lung Cancer 2017, 12, 1798–1805. [Google Scholar] [CrossRef] [Green Version]
- Freeman-Keller, M.; Kim, Y.; Cronin, H.; Richards, A.; Gibney, G.; Weber, J.S. Nivolumab in Resected and Unresectable Metastatic Melanoma: Characteristics of Immune-Related Adverse Events and Association with Outcomes. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2016, 22, 886–894. [Google Scholar] [CrossRef] [Green Version]
- Johnson, D.B.; Friedman, D.L.; Berry, E.; Decker, I.; Ye, F.; Zhao, S.; Morgans, A.K.; Puzanov, I.; Sosman, J.A.; Lovly, C.M. Survivorship in Immune Therapy: Assessing Chronic Immune Toxicities, Health Outcomes, and Functional Status among Long-Term Ipilimumab Survivors at a Single Referral Center. Cancer Immunol. Res. 2015, 3, 464–469. [Google Scholar] [CrossRef] [Green Version]
- Voskens, C.J.; Goldinger, S.M.; Loquai, C.; Robert, C.; Kaehler, K.C.; Berking, C.; Bergmann, T.; Bockmeyer, C.L.; Eigentler, T.; Fluck, M.; et al. The Price of Tumor Control: An Analysis of Rare Side Effects of Anti-CTLA-4 Therapy in Metastatic Melanoma from the Ipilimumab Network. PLoS ONE 2013, 8, e53745. [Google Scholar] [CrossRef] [Green Version]
- Xu, C.; Chen, Y.-P.; Du, X.-J.; Liu, J.-Q.; Huang, C.-L.; Chen, L.; Zhou, G.-Q.; Li, W.-F.; Mao, Y.-P.; Hsu, C.; et al. Comparative Safety of Immune Checkpoint Inhibitors in Cancer: Systematic Review and Network Meta-Analysis. BMJ 2018, 363, k4226. [Google Scholar] [CrossRef] [PubMed]
- Osorio, J.C.; Ni, A.; Chaft, J.E.; Pollina, R.; Kasler, M.K.; Stephens, D.; Rodriguez, C.; Cambridge, L.; Rizvi, H.; Wolchok, J.D.; et al. Antibody-Mediated Thyroid Dysfunction during T-Cell Checkpoint Blockade in Patients with Non-Small-Cell Lung Cancer. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2017, 28, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Hasan Ali, O.; Diem, S.; Markert, E.; Jochum, W.; Kerl, K.; French, L.E.; Speiser, D.E.; Früh, M.; Flatz, L. Characterization of Nivolumab-Associated Skin Reactions in Patients with Metastatic Non-Small Cell Lung Cancer. Oncoimmunology 2016, 5, e1231292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, P.-F.; Chen, Y.; Song, S.-Y.; Wang, T.-J.; Ji, W.-J.; Li, S.-W.; Liu, N.; Yan, C.-X. Immune-Related Adverse Events Associated with Anti-PD-1/PD-L1 Treatment for Malignancies: A Meta-Analysis. Front. Pharmacol. 2017, 8, 730. [Google Scholar] [CrossRef]
- Wang, D.Y.; Salem, J.-E.; Cohen, J.V.; Chandra, S.; Menzer, C.; Ye, F.; Zhao, S.; Das, S.; Beckermann, K.E.; Ha, L.; et al. Fatal Toxic Effects Associated With Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. JAMA Oncol. 2018, 4, 1721–1728. [Google Scholar] [CrossRef] [Green Version]
- Galon, J.; Franchimont, D.; Hiroi, N.; Frey, G.; Boettner, A.; Ehrhart-Bornstein, M.; O’Shea, J.J.; Chrousos, G.P.; Bornstein, S.R. Gene Profiling Reveals Unknown Enhancing and Suppressive Actions of Glucocorticoids on Immune Cells. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2002, 16, 61–71. [Google Scholar] [CrossRef] [Green Version]
- Strehl, C.; Ehlers, L.; Gaber, T.; Buttgereit, F. Glucocorticoids-All-Rounders Tackling the Versatile Players of the Immune System. Front. Immunol. 2019, 10, 1744. [Google Scholar] [CrossRef] [Green Version]
- Brahmer, J.R.; Lacchetti, C.; Schneider, B.J.; Atkins, M.B.; Brassil, K.J.; Caterino, J.M.; Chau, I.; Ernstoff, M.S.; Gardner, J.M.; Ginex, P.; et al. Management of Immune-Related Adverse Events in Patients Treated with Immune Checkpoint Inhibitor Therapy: American Society of Clinical Oncology Clinical Practice Guideline. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2018, 36, 1714–1768. [Google Scholar] [CrossRef]
- Thompson, J.A.; Schneider, B.J.; Brahmer, J.; Andrews, S.; Armand, P.; Bhatia, S.; Budde, L.E.; Costa, L.; Davies, M.; Dunnington, D.; et al. Management of Immunotherapy-Related Toxicities, Version 1.2019. J. Natl. Compr. Cancer Netw. 2019, 17, 255–289. [Google Scholar] [CrossRef] [Green Version]
- Haanen, J.B.a.G.; Carbonnel, F.; Robert, C.; Kerr, K.M.; Peters, S.; Larkin, J.; Jordan, K.; ESMO Guidelines Committee. Management of Toxicities from Immunotherapy: ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2017, 28, iv119–iv142. [Google Scholar] [CrossRef]
- Puzanov, I.; Diab, A.; Abdallah, K.; Bingham, C.O.; Brogdon, C.; Dadu, R.; Hamad, L.; Kim, S.; Lacouture, M.E.; LeBoeuf, N.R.; et al. Managing Toxicities Associated with Immune Checkpoint Inhibitors: Consensus Recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J. Immunother. Cancer 2017, 5, 95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michot, J.M.; Bigenwald, C.; Champiat, S.; Collins, M.; Carbonnel, F.; Postel-Vinay, S.; Berdelou, A.; Varga, A.; Bahleda, R.; Hollebecque, A.; et al. Immune-Related Adverse Events with Immune Checkpoint Blockade: A Comprehensive Review. Eur. J. Cancer 2016, 54, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Weber, J.S.; Dummer, R.; de Pril, V.; Lebbé, C.; Hodi, F.S.; MDX010-20 Investigators. Patterns of Onset and Resolution of Immune-Related Adverse Events of Special Interest with Ipilimumab: Detailed Safety Analysis from a Phase 3 Trial in Patients with Advanced Melanoma. Cancer 2013, 119, 1675–1682. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Beattie, J.A.; Fuentes, P.; Rizvi, H.; Egger, J.V.; Kern, J.A.; Leung, D.Y.M.; Lacouture, M.E.; Kris, M.G.; Gambarin, M.; et al. Beyond Steroids: Immunosuppressants in Steroid-Refractory or Resistant Immune-Related Adverse Events. J. Thorac. Oncol. Off. Publ. Int. Assoc. Study Lung Cancer 2021, 16, 1759–1764. [Google Scholar] [CrossRef]
- Abu-Sbeih, H.; Ali, F.S.; Wang, X.; Mallepally, N.; Chen, E.; Altan, M.; Bresalier, R.S.; Charabaty, A.; Dadu, R.; Jazaeri, A.; et al. Early Introduction of Selective Immunosuppressive Therapy Associated with Favorable Clinical Outcomes in Patients with Immune Checkpoint Inhibitor-Induced Colitis. J. Immunother. Cancer 2019, 7, 93. [Google Scholar] [CrossRef] [PubMed]
- Arbour, K.C.; Mezquita, L.; Long, N.; Rizvi, H.; Auclin, E.; Ni, A.; Martínez-Bernal, G.; Ferrara, R.; Lai, W.V.; Hendriks, L.E.L.; et al. Impact of Baseline Steroids on Efficacy of Programmed Cell Death-1 and Programmed Death-Ligand 1 Blockade in Patients With Non-Small-Cell Lung Cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2018, 36, 2872–2878. [Google Scholar] [CrossRef]
- Scott, S.C.; Pennell, N.A. Early Use of Systemic Corticosteroids in Patients with Advanced NSCLC Treated with Nivolumab. J. Thorac. Oncol. Off. Publ. Int. Assoc. Study Lung Cancer 2018, 13, 1771–1775. [Google Scholar] [CrossRef] [Green Version]
- Chasset, F.; Pages, C.; Biard, L.; Roux, J.; Sidina, I.; Madelaine, I.; Basset-Seguin, N.; Viguier, M.; Madjlessi-EzrA, N.; Schneider, P.; et al. Single-Center Study under a French Temporary Authorization for Use (TAU) Protocol for Ipilimumab in Metastatic Melanoma: Negative Impact of Baseline Corticosteroids. Eur. J. Dermatol. 2015, 25, 36–44. [Google Scholar] [CrossRef]
- Garant, A.; Guilbault, C.; Ekmekjian, T.; Greenwald, Z.; Murgoi, P.; Vuong, T. Concomitant Use of Corticosteroids and Immune Checkpoint Inhibitors in Patients with Hematologic or Solid Neoplasms: A Systematic Review. Crit. Rev. Oncol. Hematol. 2017, 120, 86–92. [Google Scholar] [CrossRef]
- Weber, J.S.; Hodi, F.S.; Wolchok, J.D.; Topalian, S.L.; Schadendorf, D.; Larkin, J.; Sznol, M.; Long, G.V.; Li, H.; Waxman, I.M.; et al. Safety Profile of Nivolumab Monotherapy: A Pooled Analysis of Patients With Advanced Melanoma. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2017, 35, 785–792. [Google Scholar] [CrossRef]
- Albiges, L.; Negrier, S.; Dalban, C.; Chevreau, C.; Gravis, G.; Oudard, S.; Laguerre, B.; Barthelemy, P.; Borchiellini, D.; Gross-Goupil, M.; et al. Safety and Efficacy of Nivolumab in Metastatic Renal Cell Carcinoma (MRCC): Final Analysis from the NIVOREN GETUG AFU 26 Study. J. Clin. Oncol. 2019, 37, 542. [Google Scholar] [CrossRef]
- Lefort, F.; Dalban, C.; Gross-Goupil, M.; Laguerre, B.; Barthelemy, P.; Sarradin, V.; Chanez, B.; Negrier, S.; Geoffrois, L.; Gillon, P.; et al. Impact of Corticosteroids on Nivolumab Activity in Metastatic Clear Cell Renal Cell Carcinoma. Ann. Oncol. 2019, 30, v391. [Google Scholar] [CrossRef]
- Horvat, T.Z.; Adel, N.G.; Dang, T.-O.; Momtaz, P.; Postow, M.A.; Callahan, M.K.; Carvajal, R.D.; Dickson, M.A.; D’Angelo, S.P.; Woo, K.M.; et al. Immune-Related Adverse Events, Need for Systemic Immunosuppression, and Effects on Survival and Time to Treatment Failure in Patients With Melanoma Treated With Ipilimumab at Memorial Sloan Kettering Cancer Center. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015, 33, 3193–3198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Downey, S.G.; Klapper, J.A.; Smith, F.O.; Yang, J.C.; Sherry, R.M.; Royal, R.E.; Kammula, U.S.; Hughes, M.S.; Allen, T.E.; Levy, C.L.; et al. Prognostic Factors Related to Clinical Response in Patients with Metastatic Melanoma Treated by CTL-Associated Antigen-4 Blockade. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2007, 13, 6681–6688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aldea, M.; Orillard, E.; Mansi, L.; Marabelle, A.; Scotte, F.; Lambotte, O.; Michot, J.-M. How to Manage Patients with Corticosteroids in Oncology in the Era of Immunotherapy? Eur. J. Cancer 2020, 141, 239–251. [Google Scholar] [CrossRef]
- Fucà, G.; Galli, G.; Poggi, M.; Lo Russo, G.; Proto, C.; Imbimbo, M.; Ferrara, R.; Zilembo, N.; Ganzinelli, M.; Sica, A.; et al. Modulation of Peripheral Blood Immune Cells by Early Use of Steroids and Its Association with Clinical Outcomes in Patients with Metastatic Non-Small Cell Lung Cancer Treated with Immune Checkpoint Inhibitors. ESMO Open 2019, 4, e000457. [Google Scholar] [CrossRef] [Green Version]
- Petrelli, F.; Signorelli, D.; Ghidini, M.; Ghidini, A.; Pizzutilo, E.G.; Ruggieri, L.; Cabiddu, M.; Borgonovo, K.; Dognini, G.; Brighenti, M.; et al. Association of Steroids Use with Survival in Patients Treated with Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. Cancers 2020, 12, 546. [Google Scholar] [CrossRef] [Green Version]
- Ricciuti, B.; Dahlberg, S.E.; Adeni, A.; Sholl, L.M.; Nishino, M.; Awad, M.M. Immune Checkpoint Inhibitor Outcomes for Patients With Non-Small-Cell Lung Cancer Receiving Baseline Corticosteroids for Palliative Versus Nonpalliative Indications. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2019, 37, 1927–1934. [Google Scholar] [CrossRef]
- Toi, Y.; Sugawara, S.; Kawashima, Y.; Aiba, T.; Kawana, S.; Saito, R.; Tsurumi, K.; Suzuki, K.; Shimizu, H.; Sugisaka, J.; et al. Association of Immune-Related Adverse Events with Clinical Benefit in Patients with Advanced Non-Small-Cell Lung Cancer Treated with Nivolumab. Oncologist 2018, 23, 1358–1365. [Google Scholar] [CrossRef] [Green Version]
- Attia, P.; Phan, G.Q.; Maker, A.V.; Robinson, M.R.; Quezado, M.M.; Yang, J.C.; Sherry, R.M.; Topalian, S.L.; Kammula, U.S.; Royal, R.E.; et al. Autoimmunity Correlates with Tumor Regression in Patients with Metastatic Melanoma Treated with Anti-Cytotoxic T-Lymphocyte Antigen-4. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2005, 23, 6043–6053. [Google Scholar] [CrossRef] [Green Version]
- Verzoni, E.; Cartenì, G.; Cortesi, E.; Giannarelli, D.; De Giglio, A.; Sabbatini, R.; Buti, S.; Rossetti, S.; Cognetti, F.; Rastelli, F.; et al. Real-World Efficacy and Safety of Nivolumab in Previously-Treated Metastatic Renal Cell Carcinoma, and Association between Immune-Related Adverse Events and Survival: The Italian Expanded Access Program. J. Immunother. Cancer 2019, 7, 99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Jong, W.K.; Mulders, A.C.M.; Westendorp, W.; Becker, A. Exceptional Response of Brain Metastases to Short Course Nivolumab While on High-Dose Steroids. Neth. J. Med. 2019, 77, 338–340. [Google Scholar] [PubMed]
- Faje, A.T.; Lawrence, D.; Flaherty, K.; Freedman, C.; Fadden, R.; Rubin, K.; Cohen, J.; Sullivan, R.J. High-Dose Glucocorticoids for the Treatment of Ipilimumab-Induced Hypophysitis Is Associated with Reduced Survival in Patients with Melanoma. Cancer 2018, 124, 3706–3714. [Google Scholar] [CrossRef] [Green Version]
- Opzoomer, J.W.; Sosnowska, D.; Anstee, J.E.; Spicer, J.F.; Arnold, J.N. Cytotoxic Chemotherapy as an Immune Stimulus: A Molecular Perspective on Turning Up the Immunological Heat on Cancer. Front. Immunol. 2019, 10, 1654. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galluzzi, L.; Buqué, A.; Kepp, O.; Zitvogel, L.; Kroemer, G. Immunological Effects of Conventional Chemotherapy and Targeted Anticancer Agents. Cancer Cell 2015, 28, 690–714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scurr, M.; Pembroke, T.; Bloom, A.; Roberts, D.; Thomson, A.; Smart, K.; Bridgeman, H.; Adams, R.; Brewster, A.; Jones, R.; et al. Low-Dose Cyclophosphamide Induces Antitumor T-Cell Responses, Which Associate with Survival in Metastatic Colorectal Cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2017, 23, 6771–6780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vincent, J.; Mignot, G.; Chalmin, F.; Ladoire, S.; Bruchard, M.; Chevriaux, A.; Martin, F.; Apetoh, L.; Rébé, C.; Ghiringhelli, F. 5-Fluorouracil Selectively Kills Tumor-Associated Myeloid-Derived Suppressor Cells Resulting in Enhanced T Cell-Dependent Antitumor Immunity. Cancer Res. 2010, 70, 3052–3061. [Google Scholar] [CrossRef] [Green Version]
- Alizadeh, D.; Trad, M.; Hanke, N.T.; Larmonier, C.B.; Janikashvili, N.; Bonnotte, B.; Katsanis, E.; Larmonier, N. Doxorubicin Eliminates Myeloid-Derived Suppressor Cells and Enhances the Efficacy of Adoptive T-Cell Transfer in Breast Cancer. Cancer Res. 2014, 74, 104–118. [Google Scholar] [CrossRef] [Green Version]
- Voorwerk, L.; Slagter, M.; Horlings, H.M.; Sikorska, K.; van de Vijver, K.K.; de Maaker, M.; Nederlof, I.; Kluin, R.J.C.; Warren, S.; Ong, S.; et al. Immune Induction Strategies in Metastatic Triple-Negative Breast Cancer to Enhance the Sensitivity to PD-1 Blockade: The TONIC Trial. Nat. Med. 2019, 25, 920–928. [Google Scholar] [CrossRef]
- Sistigu, A.; Yamazaki, T.; Vacchelli, E.; Chaba, K.; Enot, D.P.; Adam, J.; Vitale, I.; Goubar, A.; Baracco, E.E.; Remédios, C.; et al. Cancer Cell-Autonomous Contribution of Type I Interferon Signaling to the Efficacy of Chemotherapy. Nat. Med. 2014, 20, 1301–1309. [Google Scholar] [CrossRef]
- Tesniere, A.; Schlemmer, F.; Boige, V.; Kepp, O.; Martins, I.; Ghiringhelli, F.; Aymeric, L.; Michaud, M.; Apetoh, L.; Barault, L.; et al. Immunogenic Death of Colon Cancer Cells Treated with Oxaliplatin. Oncogene 2010, 29, 482–491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paz-Ares, L.; Vicente, D.; Tafreshi, A.; Robinson, A.; Soto Parra, H.; Mazières, J.; Hermes, B.; Cicin, I.; Medgyasszay, B.; Rodríguez-Cid, J.; et al. A Randomized, Placebo-Controlled Trial of Pembrolizumab Plus Chemotherapy in Patients With Metastatic Squamous NSCLC: Protocol-Specified Final Analysis of KEYNOTE-407. J. Thorac. Oncol. Off. Publ. Int. Assoc. Study Lung Cancer 2020, 15, 1657–1669. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.-M.; Shen, L.; Shah, M.A.; Enzinger, P.; Adenis, A.; Doi, T.; Kojima, T.; Metges, J.-P.; Li, Z.; Kim, S.-B.; et al. Pembrolizumab plus Chemotherapy versus Chemotherapy Alone for First-Line Treatment of Advanced Oesophageal Cancer (KEYNOTE-590): A Randomised, Placebo-Controlled, Phase 3 Study. Lancet 2021, 398, 759–771. [Google Scholar] [CrossRef]
- Schmid, P.; Cortes, J.; Pusztai, L.; McArthur, H.; Kümmel, S.; Bergh, J.; Denkert, C.; Park, Y.H.; Hui, R.; Harbeck, N.; et al. Pembrolizumab for Early Triple-Negative Breast Cancer. N. Engl. J. Med. 2020, 382, 810–821. [Google Scholar] [CrossRef] [PubMed]
- Cortes, J.; Cescon, D.W.; Rugo, H.S.; Nowecki, Z.; Im, S.-A.; Yusof, M.M.; Gallardo, C.; Lipatov, O.; Barrios, C.H.; Holgado, E.; et al. Pembrolizumab plus Chemotherapy versus Placebo plus Chemotherapy for Previously Untreated Locally Recurrent Inoperable or Metastatic Triple-Negative Breast Cancer (KEYNOTE-355): A Randomised, Placebo-Controlled, Double-Blind, Phase 3 Clinical Trial. Lancet 2020, 396, 1817–1828. [Google Scholar] [CrossRef]
- Schmid, P.; Rugo, H.S.; Adams, S.; Schneeweiss, A.; Barrios, C.H.; Iwata, H.; Diéras, V.; Henschel, V.; Molinero, L.; Chui, S.Y.; et al. Atezolizumab plus Nab-Paclitaxel as First-Line Treatment for Unresectable, Locally Advanced or Metastatic Triple-Negative Breast Cancer (IMpassion130): Updated Efficacy Results from a Randomised, Double-Blind, Placebo-Controlled, Phase 3 Trial. Lancet Oncol. 2020, 21, 44–59. [Google Scholar] [CrossRef]
- Miles, D.; Gligorov, J.; André, F.; Cameron, D.; Schneeweiss, A.; Barrios, C.; Xu, B.; Wardley, A.; Kaen, D.; Andrade, L.; et al. Primary Results from IMpassion131, a Double-Blind, Placebo-Controlled, Randomised Phase III Trial of First-Line Paclitaxel with or without Atezolizumab for Unresectable Locally Advanced/Metastatic Triple-Negative Breast Cancer. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2021, 32, 994–1004. [Google Scholar] [CrossRef]
- Lansinger, O.M.; Biedermann, S.; He, Z.; Colevas, A.D. Do Steroids Matter? A Retrospective Review of Premedication for Taxane Chemotherapy and Hypersensitivity Reactions. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2021, 39, JCO2101200. [Google Scholar] [CrossRef]
- Paz-Ares, L.; Luft, A.; Vicente, D.; Tafreshi, A.; Gümüş, M.; Mazières, J.; Hermes, B.; Çay Şenler, F.; Csőszi, T.; Fülöp, A.; et al. Pembrolizumab plus Chemotherapy for Squamous Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 379, 2040–2051. [Google Scholar] [CrossRef]
| Pathways | Targets | Effects | Tumour Types |
|---|---|---|---|
| Apoptosis | Bcl2 miR-17~9 ROS (reactive oxygen species) | Increased | Haemopathic malignancies |
| BIM, BAX, BAK TXNIP, GILZ miR-708 | Decreased | Haemopathic malignancies and solid tumours | |
| Proliferation | AP1, Nf-κB c-MYC | Decreased | Haemopathic malignancies and solid tumours |
| Invasion/migration | SGK1 Selectins E-cadherin | Decreased | Solid tumours |
| RhoA MMP2/9 IL-6 | Decreased | Solid tumours | |
| Angiogenesis | VEGF/IL-8 | Decreased | Solid tumours |
| Resistance to cytotoxic therapy | SGK1 MKP1 (DUSP1) IκBα | Increased | Solid tumours |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kalfeist, L.; Galland, L.; Ledys, F.; Ghiringhelli, F.; Limagne, E.; Ladoire, S. Impact of Glucocorticoid Use in Oncology in the Immunotherapy Era. Cells 2022, 11, 770. https://doi.org/10.3390/cells11050770
Kalfeist L, Galland L, Ledys F, Ghiringhelli F, Limagne E, Ladoire S. Impact of Glucocorticoid Use in Oncology in the Immunotherapy Era. Cells. 2022; 11(5):770. https://doi.org/10.3390/cells11050770
Chicago/Turabian StyleKalfeist, Laura, Loïck Galland, Fanny Ledys, François Ghiringhelli, Emeric Limagne, and Sylvain Ladoire. 2022. "Impact of Glucocorticoid Use in Oncology in the Immunotherapy Era" Cells 11, no. 5: 770. https://doi.org/10.3390/cells11050770








