Engineered Synthetic STxB for Enhanced Cytosolic Delivery
Abstract
:1. Introduction
2. Materials and Methods
2.1. UPLC-MS Analysis
2.2. Synthetic STxB Variant Syntheses
2.3. Cell Culture
2.4. Glycosphingolipid Depletion
2.5. Intracellular Trafficking Assay
2.6. Microscopy
2.7. Syntheses of Hydrophobic Moieties
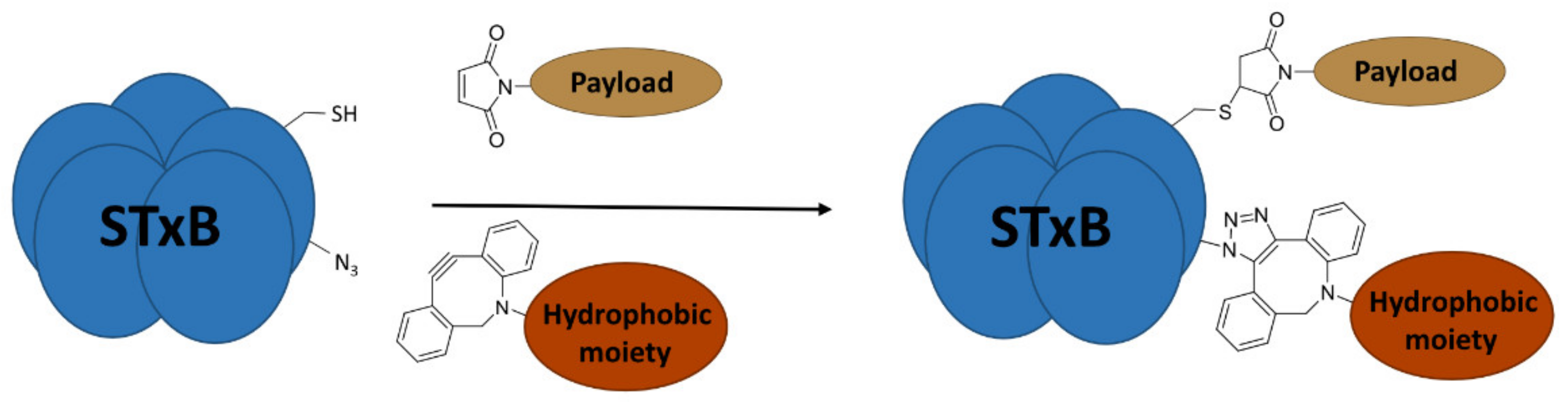
2.8. Double Conjugations
2.9. Concentration Assessment of the Double Conjugates
2.10. Size Exclusion Chromatography
2.11. Relative Quantification of Membrane Translocation to the Cytosol
2.12. Data Analysis and Figures
3. Results
3.1. Synthetic Double Variants of STxB
3.2. Hydrophobic Moieties
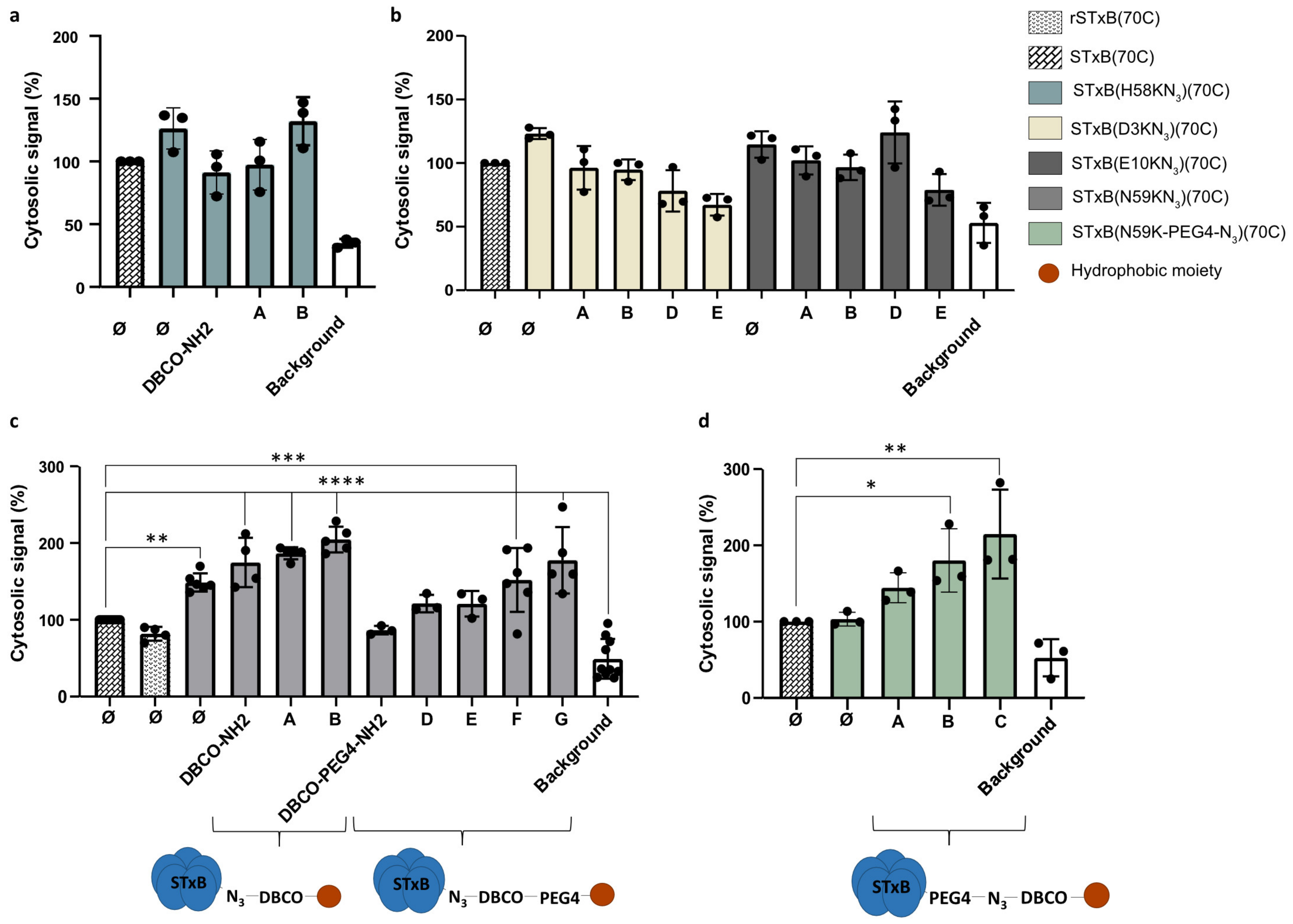
3.3. Membrane Translocation of Engineered STxB
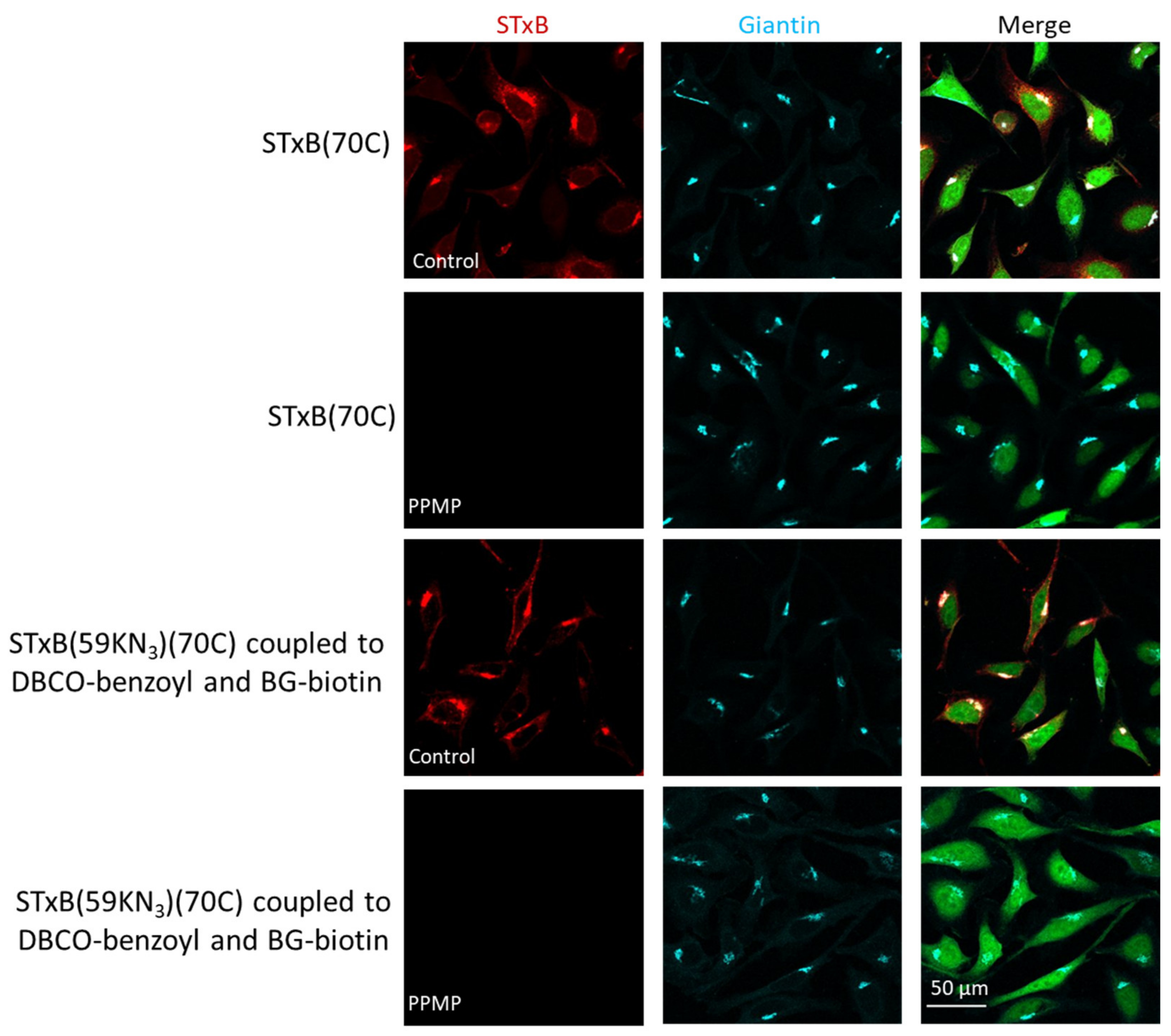
3.4. Gb3 Binding and Intracellular Trafficking
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vargason, A.M.; Anselmo, A.C.; Mitragotri, S. The Evolution of Commercial Drug Delivery Technologies. Nat. Biomed. Eng. 2021, 5, 951–967. [Google Scholar] [CrossRef]
- Varkouhi, A.K.; Scholte, M.; Storm, G.; Haisma, H.J. Endosomal Escape Pathways for Delivery of Biologicals. J. Control. Release 2011, 151, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Pei, D.; Buyanova, M. Overcoming Endosomal Entrapment in Drug Delivery. Bioconjug. Chem. 2019, 30, 273–283. [Google Scholar] [CrossRef]
- Haicheur, N.; Bismuth, E.; Bosset, S.; Adotevi, O.; Warnier, G.; Lacabanne, V.; Regnault, A.; Desaymard, C.; Amigorena, S.; Ricciardi-Castagnoli, P.; et al. The B Subunit of Shiga Toxin Fused to a Tumor Antigen Elicits CTL and Targets Dendritic Cells to Allow MHC Class I-Restricted Presentation of Peptides Derived from Exogenous Antigens. J. Immunol. Baltim. Md 1950 2000, 165, 3301–3308. [Google Scholar] [CrossRef] [PubMed]
- Nizard, M.; Roussel, H.; Diniz, M.O.; Karaki, S.; Tran, T.; Voron, T.; Dransart, E.; Sandoval, F.; Riquet, M.; Rance, B.; et al. Induction of Resident Memory T Cells Enhances the Efficacy of Cancer Vaccine. Nat. Commun. 2017, 8, 15221. [Google Scholar] [CrossRef]
- Thoreau, M.; Penny, H.L.; Tan, K.; Regnier, F.; Weiss, J.M.; Lee, B.; Johannes, L.; Dransart, E.; Le Bon, A.; Abastado, J.-P.; et al. Vaccine-Induced Tumor Regression Requires a Dynamic Cooperation between T Cells and Myeloid Cells at the Tumor Site. Oncotarget 2015, 6, 27832–27846. [Google Scholar] [CrossRef]
- Pere, H.; Montier, Y.; Bayry, J.; Quintin-Colonna, F.; Merillon, N.; Dransart, E.; Badoual, C.; Gey, A.; Ravel, P.; Marcheteau, E.; et al. A CCR4 Antagonist Combined with Vaccines Induces Antigen-Specific CD8+ T Cells and Tumor Immunity against Self Antigens. Blood 2011, 118, 4853–4862. [Google Scholar] [CrossRef]
- Sandoval, F.; Terme, M.; Nizard, M.; Badoual, C.; Bureau, M.-F.; Freyburger, L.; Clement, O.; Marcheteau, E.; Gey, A.; Fraisse, G.; et al. Mucosal Imprinting of Vaccine-Induced CD8+ T Cells Is Crucial to Inhibit the Growth of Mucosal Tumors. Sci. Transl. Med. 2013, 5, 172ra20. [Google Scholar] [CrossRef]
- Badoual, C.; Hans, S.; Merillon, N.; Van Ryswick, C.; Ravel, P.; Benhamouda, N.; Levionnois, E.; Nizard, M.; Si-Mohamed, A.; Besnier, N.; et al. PD-1-Expressing Tumor-Infiltrating T Cells Are a Favorable Prognostic Biomarker in HPV-Associated Head and Neck Cancer. Cancer Res. 2013, 73, 128–138. [Google Scholar] [CrossRef]
- Adotevi, O.; Vingert, B.; Freyburger, L.; Shrikant, P.; Lone, Y.-C.; Quintin-Colonna, F.; Haicheur, N.; Amessou, M.; Herbelin, A.; Langlade-Demoyen, P.; et al. B Subunit of Shiga Toxin-Based Vaccines Synergize with Alpha-Galactosylceramide to Break Tolerance against Self Antigen and Elicit Antiviral Immunity. J. Immunol. Baltim. 2007, 179, 3371–3379. [Google Scholar] [CrossRef]
- Tartour, E.; Johannes, L. STxB as an Antigen Delivery Tool for Mucosal Vaccination. Toxins 2022, 14, 202. [Google Scholar] [CrossRef] [PubMed]
- Karaki, S.; Blanc, C.; Tran, T.; Galy-Fauroux, I.; Mougel, A.; Dransart, E.; Anson, M.; Tanchot, C.; Paolini, L.; Gruel, N.; et al. CXCR6 Deficiency Impairs Cancer Vaccine Efficacy and CD8+ Resident Memory T-Cell Recruitment in Head and Neck and Lung Tumors. J. Immunother. Cancer 2021, 9, e001948. [Google Scholar] [CrossRef]
- Lucchino, M.; Billet, A.; Bai, S.-K.; Dransart, E.; Hadjerci, J.; Schmidt, F.; Wunder, C.; Johannes, L. Absolute Quantification of Drug Vector Delivery to the Cytosol. Angew. Chem. Int. Ed Engl. 2021, 60, 14824–14830. [Google Scholar] [CrossRef] [PubMed]
- Han, X.; Bushweller, J.H.; Cafiso, D.S.; Tamm, L.K. Membrane Structure and Fusion-Triggering Conformational Change of the Fusion Domain from Influenza Hemagglutinin. Nat. Struct. Biol. 2001, 8, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Lönn, P.; Kacsinta, A.D.; Cui, X.-S.; Hamil, A.S.; Kaulich, M.; Gogoi, K.; Dowdy, S.F. Enhancing Endosomal Escape for Intracellular Delivery of Macromolecular Biologic Therapeutics. Sci. Rep. 2016, 6, 32301. [Google Scholar] [CrossRef]
- Enhanced Intracellular Delivery Using Arginine-Rich Peptides by the Addition of Penetration Accelerating Sequences (Pas)—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/19465072/ (accessed on 9 November 2022).
- Rydberg, H.A.; Matson, M.; Amand, H.L.; Esbjörner, E.K.; Nordén, B. Effects of Tryptophan Content and Backbone Spacing on the Uptake Efficiency of Cell-Penetrating Peptides. Biochemistry 2012, 51, 5531–5539. [Google Scholar] [CrossRef] [PubMed]
- Billet, A.; Hadjerci, J.; Tran, T.; Kessler, P.; Ulmer, J.; Mourier, G.; Ghazarian, M.; Gonzalez, A.; Thai, R.; Urquia, P.; et al. A Synthetic Delivery Vector for Mucosal Vaccination; Institut Curie: Paris, France, 2023; submitted. [Google Scholar]
- Philpott, D.; Ebel, F. E. coli: Shiga Toxin Methods and Protocols; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2003; ISBN 978-1-59259-316-3. [Google Scholar]
- Schindelin, J.; Arganda-Carreras, I.; Frise, E.; Kaynig, V.; Longair, M.; Pietzsch, T.; Preibisch, S.; Rueden, C.; Saalfeld, S.; Schmid, B.; et al. Fiji: An Open-Source Platform for Biological-Image Analysis. Nat. Methods 2012, 9, 676–682. [Google Scholar] [CrossRef]
- Viel, T.; Dransart, E.; Nemati, F.; Henry, E.; Thézé, B.; Decaudin, D.; Lewandowski, D.; Boisgard, R.; Johannes, L.; Tavitian, B. In Vivo Tumor Targeting by the B-Subunit of Shiga Toxin. Mol. Imaging 2008, 7, 239–247. [Google Scholar] [CrossRef]
- Janssen, K.-P.; Vignjevic, D.; Boisgard, R.; Falguières, T.; Bousquet, G.; Decaudin, D.; Dollé, F.; Louvard, D.; Tavitian, B.; Robine, S.; et al. In Vivo Tumor Targeting Using a Novel Intestinal Pathogen-Based Delivery Approach. Cancer Res. 2006, 66, 7230–7236. [Google Scholar] [CrossRef]
- Biodistribution and Tumor Targeting of Indium and Iodine-Labeled Shiga Toxin B-Subunit | Bentham Science. Available online: http://www.eurekaselect.com/article/38358 (accessed on 10 November 2022).
- Lamblet, M.; Delord, B.; Johannes, L.; van Effenterre, D.; Bassereau, P. Key Role of Receptor Density in Colloid/Cell Specific Interaction: A Quantitative Biomimetic Study on Giant Vesicles. Eur. Phys. J. E Soft Matter 2008, 26, 205–216. [Google Scholar] [CrossRef]
- Haicheur, N.; Benchetrit, F.; Amessou, M.; Leclerc, C.; Falguières, T.; Fayolle, C.; Bismuth, E.; Fridman, W.H.; Johannes, L.; Tartour, E. The B Subunit of Shiga Toxin Coupled to Full-Size Antigenic Protein Elicits Humoral and Cell-Mediated Immune Responses Associated with a Th1-Dominant Polarization. Int. Immunol. 2003, 15, 1161–1171. [Google Scholar] [CrossRef]
- Garcia-Castillo, M.D.; Tran, T.; Bobard, A.; Renard, H.-F.; Rathjen, S.J.; Dransart, E.; Stechmann, B.; Lamaze, C.; Lord, M.; Cintrat, J.-C.; et al. Retrograde Transport Is Not Required for Cytosolic Translocation of the B-Subunit of Shiga Toxin. J. Cell Sci. 2015, 128, 2373–2387. [Google Scholar] [CrossRef]
- Jacewicz, M.; Clausen, H.; Nudelman, E.; Donohue-Rolfe, A.; Keusch, G.T. Pathogenesis of Shigella Diarrhea. XI. Isolation of a Shigella Toxin-Binding Glycolipid from Rabbit Jejunum and HeLa Cells and Its Identification as Globotriaosylceramide. J. Exp. Med. 1986, 163, 1391–1404. [Google Scholar] [CrossRef]
- Johannes, L.; Römer, W. Shiga Toxins--from Cell Biology to Biomedical Applications. Nat. Rev. Microbiol. 2010, 8, 105–116. [Google Scholar] [CrossRef] [PubMed]
- Pina, D.G.; Gómez, J.; Villar, E.; Johannes, L.; Shnyrov, V.L. Thermodynamic Analysis of the Structural Stability of the Shiga Toxin B-Subunit. Biochemistry 2003, 42, 9498–9506. [Google Scholar] [CrossRef] [PubMed]
- Pina, D.G.; Gómez, J.; England, P.; Craescu, C.T.; Johannes, L.; Shnyrov, V.L. Characterization of the Non-Native Trifluoroethanol-Induced Intermediate Conformational State of the Shiga Toxin B-Subunit. Biochimie 2006, 88, 1199–1207. [Google Scholar] [CrossRef]
- Pina, D.G.; Johannes, L.; Castanho, M.A.R.B. Shiga Toxin B-Subunit Sequential Binding to Its Natural Receptor in Lipid Membranes. Biochim. Biophys. Acta 2007, 1768, 628–636. [Google Scholar] [CrossRef]
- Mix, K.A.; Lomax, J.E.; Raines, R.T. Cytosolic Delivery of Proteins by Bioreversible Esterification. J. Am. Chem. Soc. 2017, 139, 14396–14398. [Google Scholar] [CrossRef]
- Ressler, V.T.; Mix, K.A.; Raines, R.T. Esterification Delivers a Functional Enzyme into a Human Cell. ACS Chem. Biol. 2019, 14, 599–602. [Google Scholar] [CrossRef]
- Tran, T.; Blanc, C.; Granier, C.; Saldmann, A.; Tanchot, C.; Tartour, E. Therapeutic Cancer Vaccine: Building the Future from Lessons of the Past. Semin. Immunopathol. 2019, 41, 69–85. [Google Scholar] [CrossRef]

| STxB Variant | Positions of the Azide (Red) and Extra Cysteine (Orange) | Azide—Membrane Distance (Å) | Fmoc Synthesis yield (%) | Oxidation and Folding Yield (%) | Overall Yield (%) | Retrograde Trafficking |
|---|---|---|---|---|---|---|
| STxB(70C) |  | _ | 43 | 28 | 12.0 | Functional |
| STxB(D3KN3)(70C) |  | 14 | 54 | 25 | 13.5 | Functional |
| STxB(E10KN3)(70C) |  | 20 | 52 | 21 | 10.9 | Functional |
| STxB(H58KN3)(70C) | 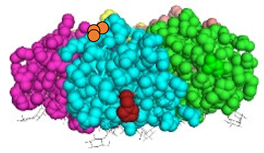 | 10 | 47 | 23 | 10.8 | Functional |
| STxB(N59KN3)(70C) | 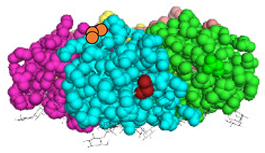 | 11 | 51 | 19 | 9.7 | Functional |
| STxB(N59K-PEG4-N3)(70C) |  | 0 | 47 | 31 | 14.6 | Functional |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hadjerci, J.; Billet, A.; Kessler, P.; Mourier, G.; Ghazarian, M.; Gonzalez, A.; Wunder, C.; Mabrouk, N.; Tartour, E.; Servent, D.; et al. Engineered Synthetic STxB for Enhanced Cytosolic Delivery. Cells 2023, 12, 1291. https://doi.org/10.3390/cells12091291
Hadjerci J, Billet A, Kessler P, Mourier G, Ghazarian M, Gonzalez A, Wunder C, Mabrouk N, Tartour E, Servent D, et al. Engineered Synthetic STxB for Enhanced Cytosolic Delivery. Cells. 2023; 12(9):1291. https://doi.org/10.3390/cells12091291
Chicago/Turabian StyleHadjerci, Justine, Anne Billet, Pascal Kessler, Gilles Mourier, Marine Ghazarian, Anthony Gonzalez, Christian Wunder, Nesrine Mabrouk, Eric Tartour, Denis Servent, and et al. 2023. "Engineered Synthetic STxB for Enhanced Cytosolic Delivery" Cells 12, no. 9: 1291. https://doi.org/10.3390/cells12091291
APA StyleHadjerci, J., Billet, A., Kessler, P., Mourier, G., Ghazarian, M., Gonzalez, A., Wunder, C., Mabrouk, N., Tartour, E., Servent, D., & Johannes, L. (2023). Engineered Synthetic STxB for Enhanced Cytosolic Delivery. Cells, 12(9), 1291. https://doi.org/10.3390/cells12091291









