Gene Expression in MC3T3-E1 Cells Treated with Diclofenac and Methylprednisolone
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Culture
2.2. Cell Viability and Caspase Activity
2.3. RNA Extraction and RT-PCR
2.4. Gene Expression
2.5. Statistical Analysis
3. Results
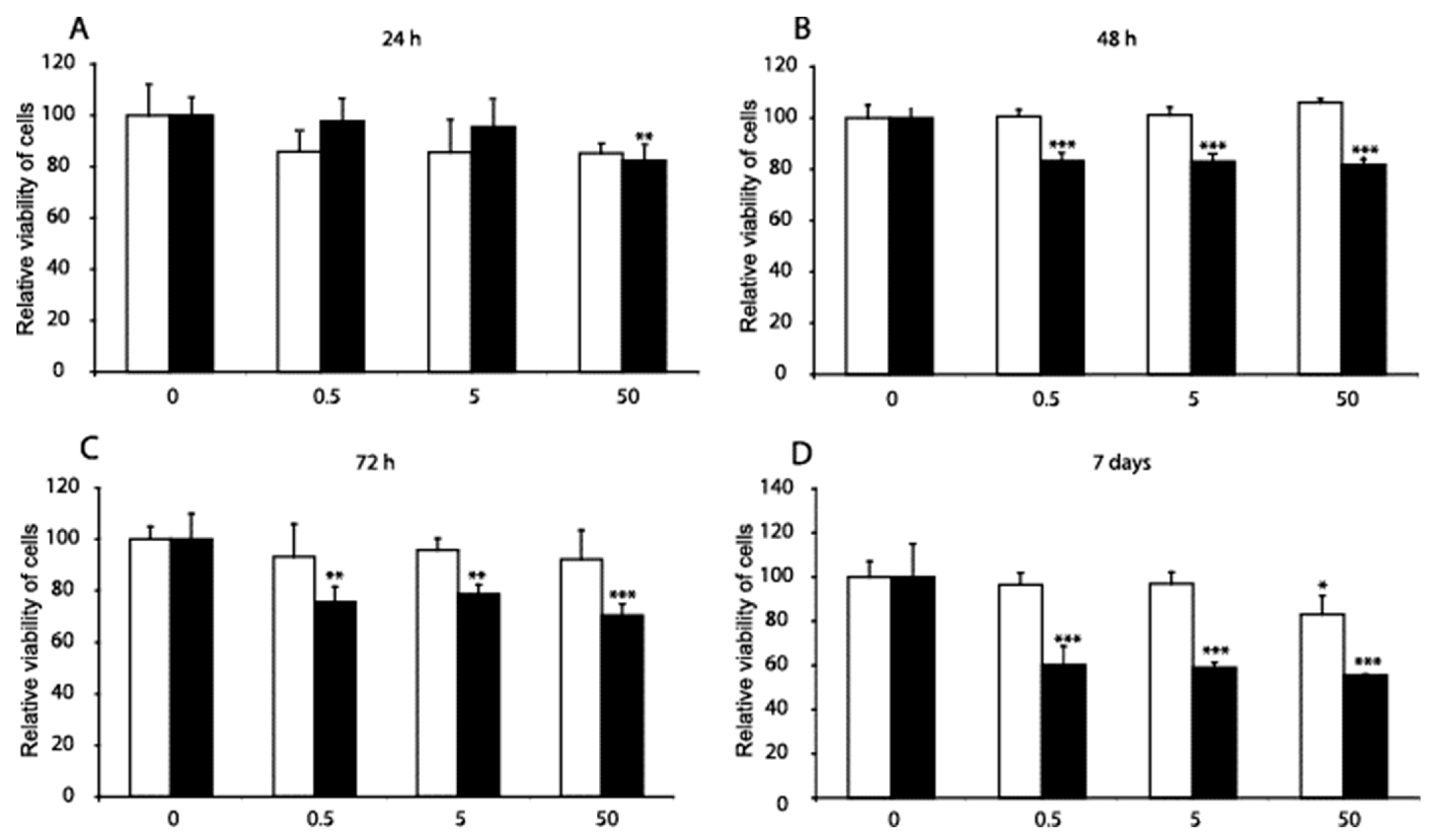
3.1. Cell Viability
3.2. Caspase
3.3. Gene Expression
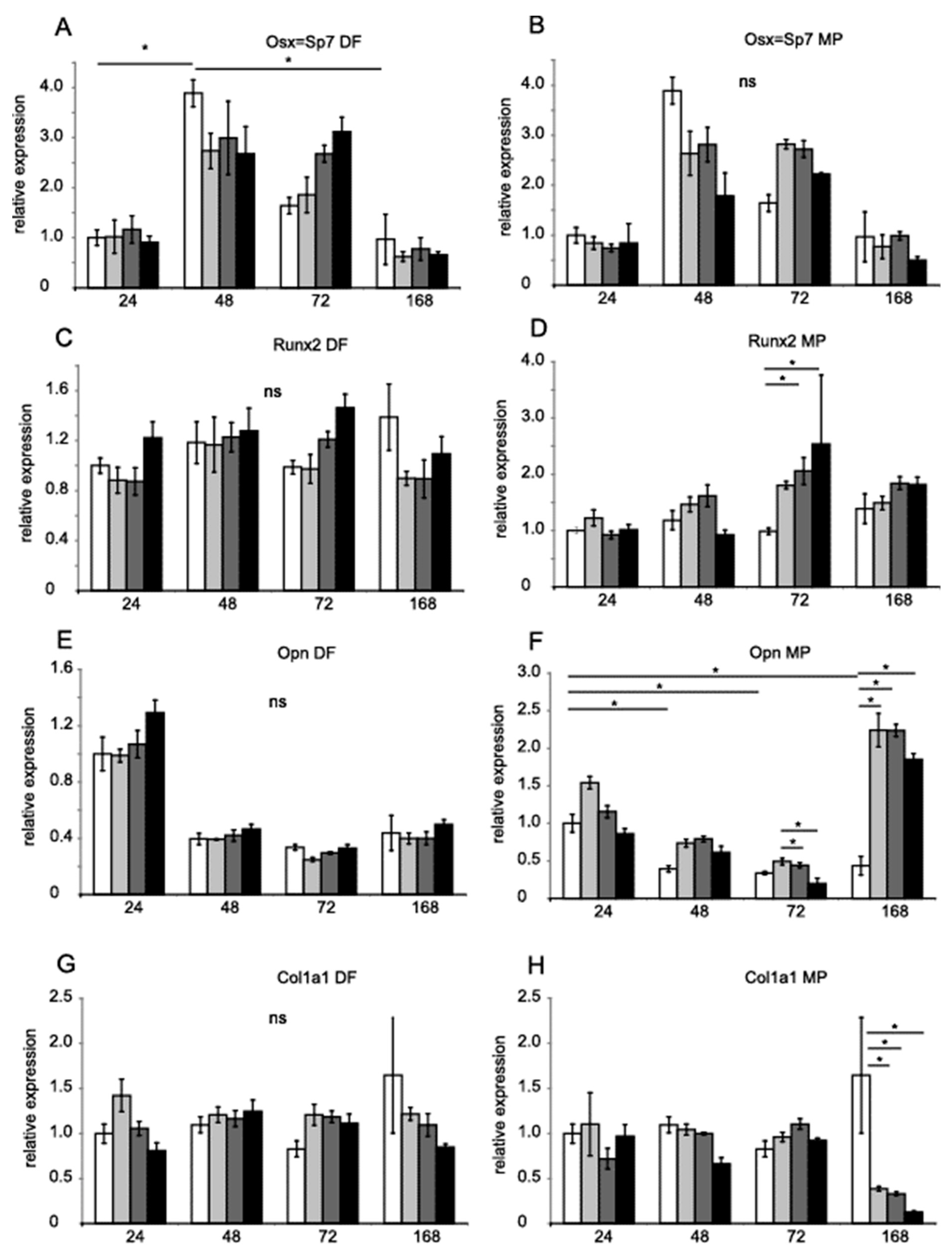
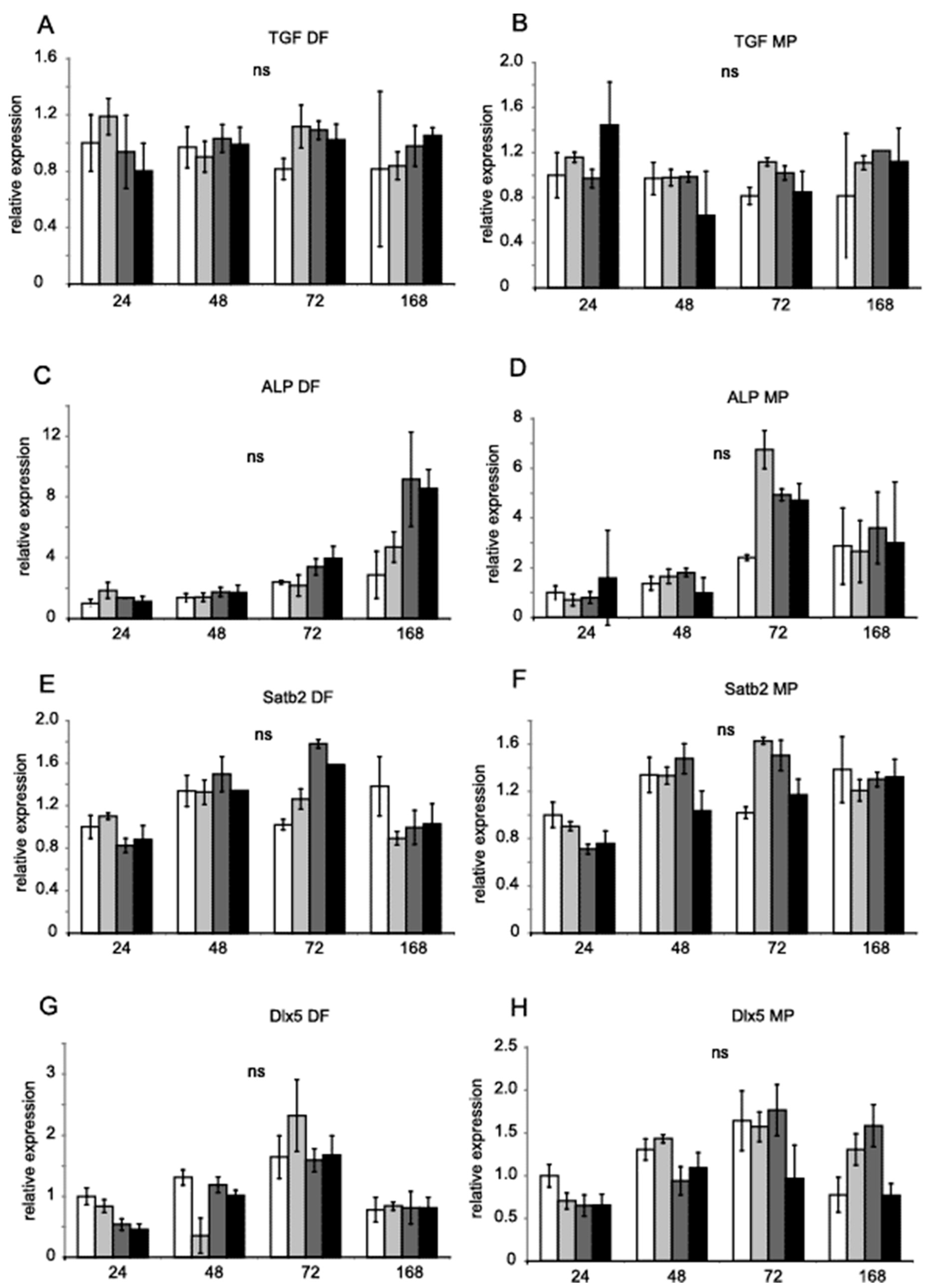
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gómez-Acebo, I.; Dierssen-Sotos, T.; de Pedro, M.; Pérez-Gómez, B.; Castaño-Vinyals, G.; Fernández-Villa, T.; Palazuelos-Calderón, C.; Amiano, P.; Etxeberria, J.; Benavente, Y.; et al. Epidemiology of Non-Steroidal Anti-Inflammatory Drugs Consumption in Spain. The MCC-Spain Study. BMC Public Health 2018, 18, 1134. [Google Scholar] [CrossRef]
- Felson, D.T.; Neogi, T. Emerging Treatment Models in Rheumatology: Challenges for Osteoarthritis Trials. Arthritis Rheumatol. 2018, 70, 1175–1181. [Google Scholar] [CrossRef] [Green Version]
- Hardy, R.S.; Zhou, H.; Seibel, M.J.; Cooper, M.S. Glucocorticoids and Bone: Consequences of Endogenous and Exogenous Excess and Replacement Therapy. 2018. Endocr. Rev. 2018, 39, 519–548. [Google Scholar] [CrossRef] [Green Version]
- Takahata, M.; Maher, J.R.; Juneja, S.C.; Inzana, J.; Xing, L.; Schwarz, E.M.; Berger, A.J.; Awad, H.A. Mechanisms of Bone Fragility in a Mouse Model of Glucocorticoid-Treated Rheumatoid Arthritis: Implications for Insufficiency Fracture Risk. Arthritis Rheum. 2012, 64, 3649–3659. [Google Scholar] [CrossRef] [Green Version]
- Ersek, A.; Santo, A.I.; Vattakuzhi, Y.; George, S.; Clark, A.R.; Horwood, N.J. Strain Dependent Differences in Glucocorticoid-Induced Bone Loss between C57BL/6J and CD-1 Mice. Sci. Rep. 2016, 6, 36513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glowacki, M.; Ignys-O’Byrne, A.; Ignys, I.; Mankowski, P.; Melzer, P. Evaluation of Volume and Solitary Bone Cyst Remodeling Using Conventional Radiological Examination. Skeletal Radiol. 2010, 39, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Glowacki, M.; Ignys-O’Byrne, A.; Ignys, I.; Wroblewska, K. Limb Shortening in the Course of Solitary Bone Cyst Treatment—A Comparative Study. Skeletal Radiol. 2011, 40, 173–179. [Google Scholar] [CrossRef]
- Czarny-Ratajczak, M.; Bieganski, T.; Rogala, P.; Glowacki, M.; Trzeciak, T.; Kozlowski, K. New Intermediate Phenotype between MED and DD Caused by Compound Heterozygous Mutations in the DTDST Gene. Am. J. Med. Genet. A 2010, 152A, 3036–3042. [Google Scholar] [CrossRef]
- Ho, M.L.; Chang, J.K.; Chuang, L.Y.; Hsu, H.K.; Wang, G.J. Effects of Nonsteroidal Anti-Inflammatory Drugs and Prostaglandins on Osteoblastic Functions. Biochem. Pharm. 1999, 58, 983–990. [Google Scholar] [CrossRef] [PubMed]
- Manzano-Moreno, F.J.; Costela-Ruiz, V.J.; Melguizo-Rodríguez, L.; Illescas-Montes, R.; García-Martínez, O.; Ruiz, C.; Ramos-Torrecillas, J. Inhibition of VEGF Gene Expression in Osteoblast Cells by Different NSAIDs. Arch. Oral. Biol. 2018, 92, 75–78. [Google Scholar] [CrossRef]
- García-Martínez, O.; de Luna-Bertos, E.; Ramos-Torrecillas, J.; Manzano-Moreno, F.J.; Ruiz, C. Repercussions of NSAIDS Drugs on Bone Tissue: The Osteoblast. Life Sci. 2015, 123, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Datta, H.K.; Ng, W.F.; Walker, J.A.; Tuck, S.P.; Varanasi, S.S. The Cell Biology of Bone Metabolism. J. Clin. Pathol. 2008, 61, 577–587. [Google Scholar] [CrossRef]
- Kaspar, D.; Hedrich, C.M.; Schmidt, C.; Liedert, A.; Claes, L.E.; Ignatius, A.A. Diclofenac Inhibits Proliferation and Matrix Formation of Osteoblast Cells. Unfallchirurg 2005, 108, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Hadjicharalambous, C.; Alpantaki, K.; Chatzinikolaidou, M. Effects of NSAIDs on Pre-Osteoblast Viability and Osteogenic Differentiation. Exp. Ther. Med. 2021, 22, 740. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.-K.; Li, C.-J.; Wu, S.-C.; Yeh, C.-H.; Chen, C.-H.; Fu, Y.-C.; Wang, G.-J.; Ho, M.-L. Effects of Anti-Inflammatory Drugs on Proliferation, Cytotoxicity and Osteogenesis in Bone Marrow Mesenchymal Stem Cells. Biochem. Pharm. 2007, 74, 1371–1382. [Google Scholar] [CrossRef] [PubMed]
- Gan, T.J. Diclofenac: An Update on Its Mechanism of Action and Safety Profile. Curr. Med. Res. Opin. 2010, 26, 1715–1731. [Google Scholar] [CrossRef]
- Chang, J.-K.; Li, C.-J.; Liao, H.-J.; Wang, C.-K.; Wang, G.-J.; Ho, M.-L. Anti-Inflammatory Drugs Suppress Proliferation and Induce Apoptosis through Altering Expressions of Cell Cycle Regulators and pro-Apoptotic Factors in Cultured Human Osteoblasts. Toxicology 2009, 258, 148–156. [Google Scholar] [CrossRef]
- Díaz-Rodríguez, L.; García-Martínez, O.; Morales, M.A.-; Rodríguez-Pérez, L.; Rubio-Ruiz, B.; Ruiz, C. Effects of Indomethacin, Nimesulide, and Diclofenac on Human MG-63 Osteosarcoma Cell Line. Biol. Res. Nurs. 2012, 14, 98–107. [Google Scholar] [CrossRef]
- Karakawa, A.; Fukawa, Y.; Okazaki, M.; Takahashi, K.; Sano, T.; Amano, H.; Yamamoto, M.; Yamada, S. Diclofenac Sodium Inhibits NFkappaB Transcription in Osteoclasts. J. Dent. Res. 2009, 88, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Melguizo-Rodriguez, L.; Costela-Ruiz, V.J.; Manzano-Moreno, F.J.; Illescas-Montes, R.; Ramos-Torrecillas, J.; Garcia-Martinez, O.; Ruiz, C. Repercussion of Nonsteroidal Anti-Inflammatory Drugs on the Gene Expression of Human Osteoblasts. PeerJ 2018, 6, e5415. [Google Scholar] [CrossRef]
- Pountos, I.; Georgouli, T.; Calori, G.M.; Giannoudis, P.V. Do Nonsteroidal Anti-Inflammatory Drugs Affect Bone Healing? A Critical Analysis. Sci. World J. 2012, 2012, 606404. [Google Scholar] [CrossRef] [Green Version]
- Lehmann, T.P.; Wojtków, M.; Pruszyńska-Oszmałek, E.; Kołodziejski, P.; Pezowicz, C.; Trzaskowska, A.; Mielcarek, S.; Szybowicz, M.; Nowicka, A.B.; Nowicki, M.; et al. Trabecular Bone Remodelling in the Femur of C57BL/6J Mice Treated with Diclofenac in Combination with Treadmill Exercise. Acta Bioeng. Biomech. 2021, 23, 3–11. [Google Scholar] [CrossRef]
- Lehmann, T.P.; Juzwa, W.; Filipiak, K.; Sujka-Kordowska, P.; Zabel, M.; Gowacki, J.; Gowacki, M.; Jagodziski, P.P. Quantification of the Asymmetric Migration of the Lipophilic Dyes, DiO and DiD, in Homotypic Co-Cultures of Chondrosarcoma SW-1353 Cells. Mol. Med. Rep. 2016, 14, 4529–4536. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lehmann, T.P.; Filipiak, K.; Juzwa, W.; Sujka-Kordowska, P.; Jagodziński, P.P.; Zabel, M.; Głowacki, J.; Misterska, E.; Walczak, M.; Głowacki, M. Co-Culture of Human Nucleus Pulposus Cells with Multipotent Mesenchymal Stromal Cells from Human Bone Marrow Reveals Formation of Tunnelling Nanotubes. Mol. Med. Rep. 2014, 9, 574–582. [Google Scholar] [CrossRef] [Green Version]
- Lehmann, T.P.; Głowacki, M.; Misterska, E.; Walczak, M.; Jagodziński, P.P.; Głowacki, J. Anti-Tuberculosis Drugs Decrease Viability and Stimulate the Expression of Chondrocyte Marker Genes in Human Nucleus Pulposus Cells. Mol. Med. Rep. 2014, 9, 316–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lehmann, T.P.; Jakub, G.; Harasymczuk, J.; Jagodziński, P.P. Transforming Growth Factor β Mediates Communication of Co-Cultured Human Nucleus Pulposus Cells and Mesenchymal Stem Cells. J. Orthop. Res. 2018, 36, 3023–3032. [Google Scholar] [CrossRef] [Green Version]
- Pfaffl, M.W.; Horgan, G.W.; Dempfle, L. Relative Expression Software Tool (REST) for Group-Wise Comparison and Statistical Analysis of Relative Expression Results in Real-Time PCR. Nucleic. Acids. Res. 2002, 30, e36. [Google Scholar] [CrossRef] [PubMed]
- Ortuno, M.J.; Susperregui, A.R.; Artigas, N.; Rosa, J.L.; Ventura, F. Osterix Induces Col1a1 Gene Expression through Binding to Sp1 Sites in the Bone Enhancer and Proximal Promoter Regions. Bone 2013, 52, 548–556. [Google Scholar] [CrossRef]
- Farshdousti Hagh, M.; Noruzinia, M.; Mortazavi, Y.; Soleimani, M.; Kaviani, S.; Abroun, S.; Dehghani Fard, A.; Mahmoodinia, M. Different Methylation Patterns of RUNX2, OSX, DLX5 and BSP in Osteoblastic Differentiation of Mesenchymal Stem Cells. Cell J. 2015, 17, 71–82. [Google Scholar] [CrossRef]
- Liu, Q.; Li, M.; Wang, S.; Xiao, Z.; Xiong, Y.; Wang, G. Recent Advances of Osterix Transcription Factor in Osteoblast Differentiation and Bone Formation. Front. Cell Dev. Biol. 2020, 8, 601224. [Google Scholar] [CrossRef]
- Watanabe-Tomita, Y.; Suzuki, A.; Oiso, Y.; Kozawa, O. Prostaglandin E1 Stimulates Interleukin-6 Secretion via Protein Kinase A in Osteoblast-like Cells. Cell Signal. 1997, 9, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Hakeda, Y.; Harada, S.; Matsumoto, T.; Tezuka, K.; Higashino, K.; Kodama, H.; Hashimoto-Goto, T.; Ogata, E.; Kumegawa, M. Prostaglandin F2 Alpha Stimulates Proliferation of Clonal Osteoblastic MC3T3-E1 Cells by up-Regulation of Insulin-like Growth Factor I Receptors. J. Biol. Chem. 1991, 266, 21044–21050. [Google Scholar] [CrossRef]
- Fang, M.A.; Noguchi, G.M.; McDougall, S. Prostaglandin E2 Induces Egr-1 MRNA in MC3T3-E1 Osteoblastic Cells by a Protein Kinase C-Dependent Pathway. Prostaglandins Leukot. Essent. Fat. Acids 1996, 54, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Suda, M.; Tanaka, K.; Sakuma, Y.; Yasoda, A.; Ozasa, A.; Fukata, J.; Tanaka, I.; Narumiya, S.; Nakao, K. Prostaglandin E(2) (PGE(2)) Induces the c-Fos and c-Jun Expressions via the EP(1) Subtype of PGE Receptor in Mouse Osteoblastic MC3T3-E1 Cells. Calcif. Tissue Int. 2000, 66, 217–223. [Google Scholar] [CrossRef]
- Suzuki, H.; Ohshima, N.; Tatei, K.; Taniguchi, T.; Sato, S.; Izumi, T. The Role of Autonomously Secreted PGE2 and Its Autocrine/Paracrine Effect on Bone Matrix Mineralization at the Different Stages of Differentiating MC3T3-E1 Cells. Biochem. Biophys. Res. Commun. 2020, 524, 929–935. [Google Scholar] [CrossRef] [PubMed]
- El-Sayed, M.G.A.; El-Komy, A.A.A.; Dalia, D.I.A.E. Evaluation of Teratogenic Potentials of Diclofenac in Pregnant Female Rats. Benha. Vet. Med. J. 2014, 26, 54–66. [Google Scholar]
- Siu, S.S.; Yeung, J.H.; Lau, T.K. A Study on Placental Transfer of Diclofenac in First Trimester of Human Pregnancy. Hum. Reprod. 2000, 15, 2423–2425. [Google Scholar] [CrossRef] [Green Version]
- Luppen, C.A.; Smith, E.; Spevak, L.; Boskey, A.L.; Frenkel, B. Bone Morphogenetic Protein-2 Restores Mineralization in Glucocorticoid-Inhibited MC3T3-E1 Osteoblast Cultures. J. Bone. Miner. Res. 2003, 18, 1186–1197. [Google Scholar] [CrossRef]
- Hwang, P.W.; Horton, J.A. Variable Osteogenic Performance of MC3T3-E1 Subclones Impacts Their Utility as Models of Osteoblast Biology. Sci. Rep. 2019, 9, 8299. [Google Scholar] [CrossRef] [Green Version]
- Xu, D.; Gao, Y.; Hu, N.; Wu, L.; Chen, Q. MiR-365 Ameliorates Dexamethasone-Induced Suppression of Osteogenesis in MC3T3-E1 Cells by Targeting HDAC4. Int. J. Mol. Sci. 2017, 18, 977. [Google Scholar] [CrossRef]

| Gene | Assay Catalogue Number | Sequence ID |
|---|---|---|
| Osx | 4351372 | Mm04933803_m1 |
| Runx2 | 4331182 | Mm00501584_m1 |
| Opn/Spp1 | 4331182 | Mm00436767_m1 |
| Col1a1 | 4331182 | Mm00801666_g1 |
| Tgfb1 | 4331182 | Mm01178820_m1 |
| Alp | 4331182 | Mm00475834_m1 |
| Satb2 | 4331182 | Mm00507331_m1 |
| Dlx5 | 4331182 | Mm00438430_m1 |
| Hprt | 4331182 | Mm03024075_m1 |
| B2m | 4331182 | Mm00437764_m1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lehmann, T.P.; Iwańczyk-Skalska, E.; Harasymczuk, J.; Jagodziński, P.P.; Głowacki, M. Gene Expression in MC3T3-E1 Cells Treated with Diclofenac and Methylprednisolone. Genes 2023, 14, 184. https://doi.org/10.3390/genes14010184
Lehmann TP, Iwańczyk-Skalska E, Harasymczuk J, Jagodziński PP, Głowacki M. Gene Expression in MC3T3-E1 Cells Treated with Diclofenac and Methylprednisolone. Genes. 2023; 14(1):184. https://doi.org/10.3390/genes14010184
Chicago/Turabian StyleLehmann, Tomasz P., Ewa Iwańczyk-Skalska, Jerzy Harasymczuk, Paweł P. Jagodziński, and Maciej Głowacki. 2023. "Gene Expression in MC3T3-E1 Cells Treated with Diclofenac and Methylprednisolone" Genes 14, no. 1: 184. https://doi.org/10.3390/genes14010184







