The Early Days of Personal Solar Ultraviolet Dosimetry
Abstract
:1. Introduction
2. Fundamental Requirements of Personal Ultraviolet Dosimeters
- The dosimeter should be easy to handle and not impose restrictions on the activities of the wearers.
- In physical dosimeters, the output electrical signal should increase linearly with irradiance and have a wide dynamic range.
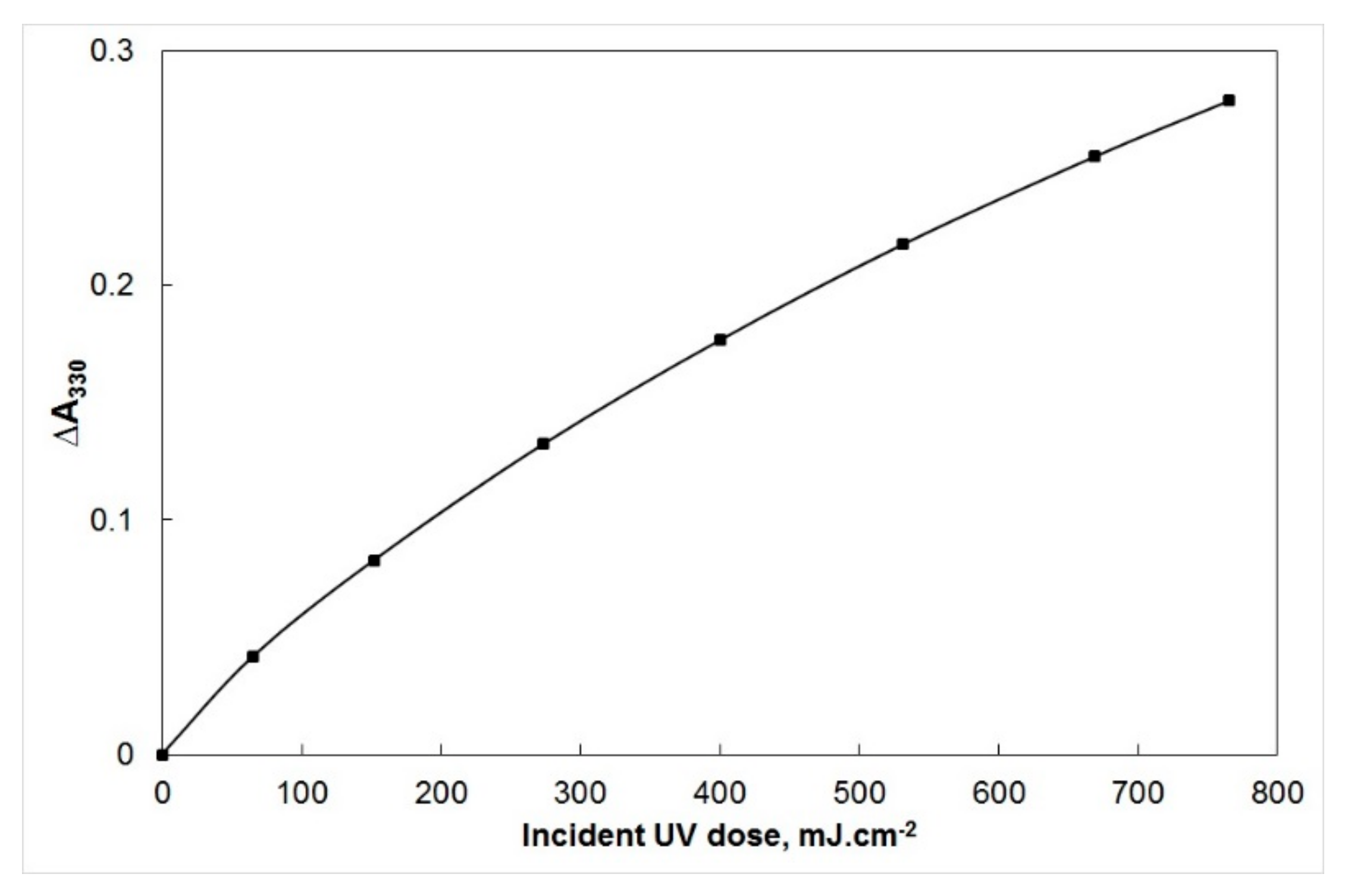
- In chemical or biological dosimeters, the change produced in the system should increase linearly with UV dose. If not, the dose response curve should at least be monotonic; that is, any given dosimeter response is the result of only one radiation dose.
- The dosimeter should exhibit photoaddition; in other words, each wavelength acts independently, and the effect of polychromatic radiation is the sum of the effects of all wavelengths involved.
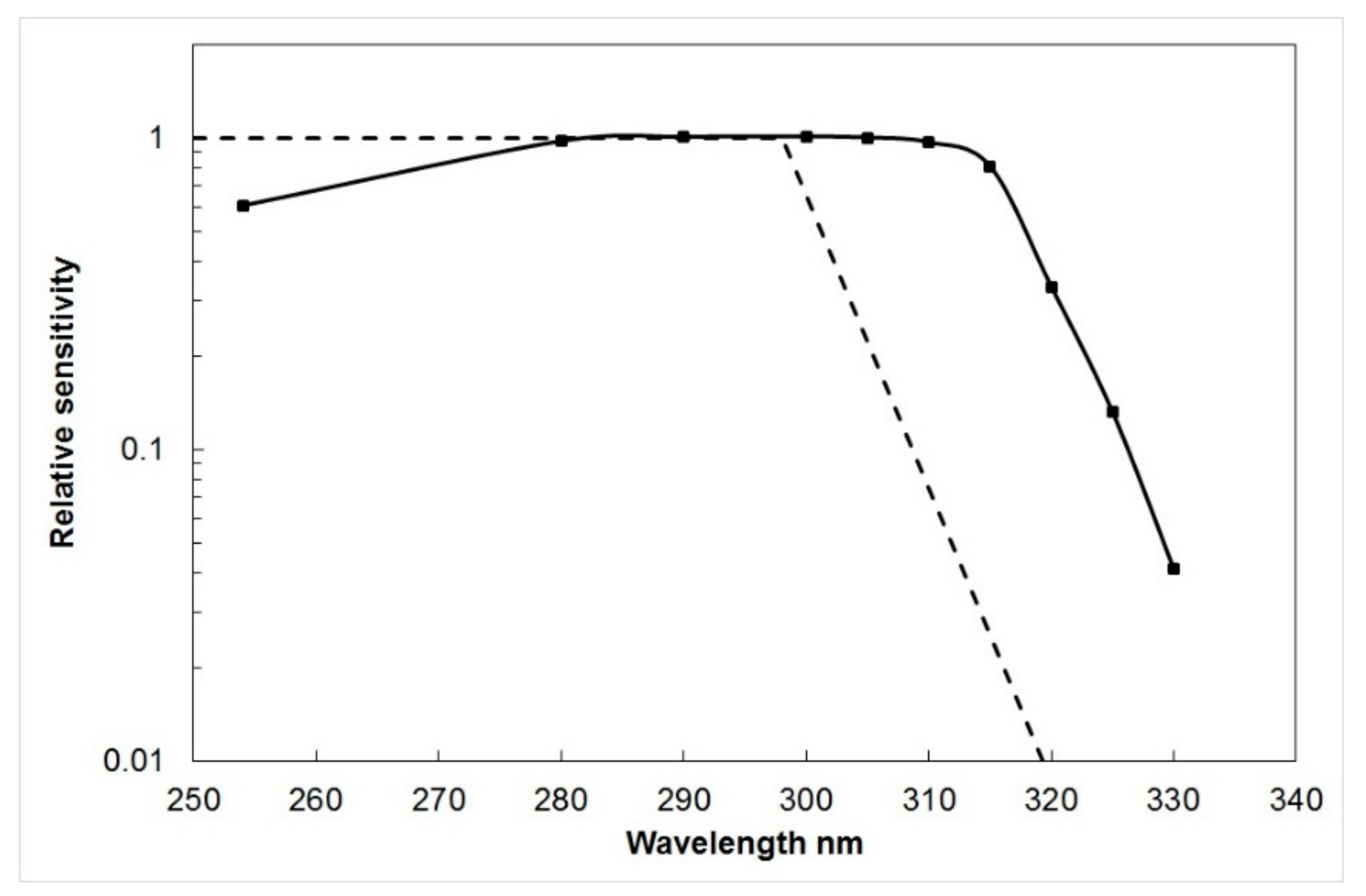
- The spectral sensitivity of the dosimeter should, ideally, match the action spectrum of the photobiological effect being monitored, most commonly erythema.
- The dosimeter response should be independent of temperature and humidity, exhibit no ‘dark effect’ (continuing response when radiation exposure is terminated), and be stable in long-term storage.
- The dosimeter should not require laborious processing, and it should be easy to convert the physical, chemical, or biological response to a measure of UV exposure dose.
- The cost per dosimeter should be low so that large scale monitoring is feasible.
3. The Birth of Polysulphone as a Dosimeter for Measuring Personal Solar UV Exposure
4. Calibration of Polysulphone Film as a UV Dosimeter
5. Using Polysulphone Film as a Personal UV Dosimeter
6. Pioneering Studies of Human Exposure to Solar UV
7. Applications of Polysulphone Film Dosimetry
Anatomical Distribution of Solar UV Radiation
8. Other Types of Personal UV Dosimeter
8.1. Plastic Films Incorporating Photosensitizing Drugs
8.2. Diazo Systems
8.3. Photosensitive Papers
8.4. Thermoluminescent Materials
8.5. Polycarbonate Plastic
8.6. Biological Systems
8.7. Electronic Dosimeters
9. Conclusions
Funding
Conflicts of Interest
References
- Davis, A.; Gordon, D.; Howell, G.V. Explosives Research and Development Establishment Reports; Nos. 141, 199 and 197; Ministry of Defence: New Delhi, India, 1975.
- Davis, A.; Deane, G.H.W.; Gordon, D.; Howell, G.V.; Ledbury, K.J. A worldwide programme for the continuous monitoring of solar UV radiation using polyphenylene oxide film. J. Appl. Polym. Sci. 1976, 20, 1165–1174. [Google Scholar] [CrossRef]
- Commission Internationale de l’Eclairage. Erythema Reference Action Spectrum and Standard Erythema Dose; CIE S007E-1998; CIE Central Bureau: Vienna, Austria, 1998. [Google Scholar]
- Davis, A.; Deane, G.; Disffey, B. Possible dosimeter for ultraviolet radiation. Nature 1976, 261, 169–170. [Google Scholar] [CrossRef] [PubMed]
- Pepper, M.G.; Diffey, B.L. Automatic read-out device for ultraviolet radiation polymer film dosimeters. Med. Bio. Eng. Comput. 1980, 18, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Diffey, B.L. Ultraviolet radiation dosimetry with polysulphone film. In Radiation Measurement in Photobiology; Diffey, B.L., Ed.; Academic Press: London, UK, 1989; pp. 135–139. [Google Scholar]
- Seckmeyer, G.; Bais, A.; Bernhard, G.; Blumthaler, M.; Booth, C.R.; Lantz, K.; McKenzie, R.L. Instruments to Measure Solar Ultraviolet Irradiance. Part 2: Broadband Instruments Measuring Erythemally Weighted Solar Irradiance; Global Atmosphere Watch, Report No. 164; World Meteorological Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Casal, G.R.; Borra, M.; Colosimo, A.; Colucci, M.; Militello, M.; Siani, A.M.; Sisto, R. Variability among polysulphone calibration curves. Phys. Med. Biol. 2006, 51, 4413–4427. [Google Scholar] [CrossRef]
- Gibbs, N.K.; Young, A.R.; Corbett, M.F. Personal solar UVR exposure: A method of increasing the reliability of measurements made with film badge dosimeters. Photodermatology 1984, 1, 133–136. [Google Scholar]
- Challoner, A.V.J.; Corless, D.; Davis, A.; Deane, G.H.W.; Diffey, B.L.; Gupta, S.P.; Magnus, I.A. Personnel monitoring of exposure to ultraviolet radiation. Clin. Exp. Dermatol. 1976, 1, 175–179. [Google Scholar] [CrossRef]
- Leach, J.F.; McLeod, V.E.; Pingstone, A.R.; Davis, A.; Deane, G.H.W. Measurement of the ultraviolet doses received by office workers. Clin. Exp. Dermatol. 1978, 3, 77–79. [Google Scholar] [CrossRef]
- Diffey, B.L.; Larkö, O.; Swanbeck, G. UV-B doses received during different outdoor activities and UV-B treatment of psoriasis. Br. J. Dermatol. 1982, 106, 279–285. [Google Scholar] [CrossRef]
- Gies, H.P.; Herlihy, E.; Rivers, J. Personal dosimetry of solar UVB using polysulphone film. Proc. IRPA 8 Congr. Montr. 1992, 1, 791–794. [Google Scholar]
- Snellman, E.; Jansen, C.T.; Lauharanta, J.; Kolari, P. Solar ultraviolet (UV) radiation and UV doses received by patients during four-week climate therapy periods in the Canary Islands. Photodermatol. Photoimmunol. Photomed. 1992, 9, 40–43. [Google Scholar]
- Kimlin, M.G.; Parisi, A.V.; Wong, J.C.F. Quantification of personal solar UV exposure of outdoor workers, indoor workers and adolescents at two locations in Southeast Queensland. Photodermatol. Photoimmunol. Photomed. 1998, 14, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Holman, C.D.J.; Gibson, I.M.; Stephenson, M.; Armstrong, B.K. Ultraviolet irradiation of human body sites in relation to occupation and outdoor activity: Field studies using personal UVR dosimeters. Clin. Exp. Dermatol. 1983, 8, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Parisi, A.V.; Meldrum, L.R.; Kimlin, M.G.; Wong, J.C.F.; Aitken, J.; Mainstone, J.S. Evaluation of differences in ultraviolet exposure during weekend and weekday activities. Phys. Med. Biol. 2000, 45, 2253–2262. [Google Scholar] [CrossRef]
- Kimlin, M.G.; Wong, J.C.F.; Parisi, A.V. Simultaneous comparison of the personal UV exposure of two human groups at different altitudes. Health Phys. 1998, 74, 429–434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schothorst, A.A.; Slaper, H.; Schouten, R.; Suurmond, D. UVB doses in maintenance psoriasis phototherapy versus solar UVB exposure. Photodermatology 1985, 2, 213–220. [Google Scholar]
- Larkö, O.; Diffey, B.L. Natural UV-B radiation received by people with outdoor, indoor and mixed occupations and UV-B treatment of psoriasis. Clin. Exp. Dermatol. 1983, 8, 279–285. [Google Scholar] [CrossRef]
- Gies, H.P.; Roy, C.R.; Toomey, S.; MacLennan, R.; Watson, M. Solar UVR exposures of three groups of outdoor workers on the Sunshine Coast, Queensland. Photochem. Photobiol. 1995, 62, 1015–1021. [Google Scholar] [CrossRef]
- Slaper, H. Skin Cancer and UV Exposure: Investigations on the Estimation of Risks. PhD Thesis, University of Utrecht, Utrecht, The Netherlands, 1987. [Google Scholar]
- Webb, A.R. Solar ultraviolet radiation and vitamin D synthesis in man. PhD Thesis, University of Nottingham, Nottingham, UK, 1985. [Google Scholar]
- Knuschke, P.; Barth, J. Biologically weighted personal UV dosimetery. J. Photochem. Photobiol. 1996, 36, 77–83. [Google Scholar] [CrossRef]
- Herlihy, E.; Gies, H.P.; Roy, C.R.; Jones, M. Personal dosimetry of solar UVR for different outdoor activities. Photochem. Photobiol. 1994, 60, 288–294. [Google Scholar] [CrossRef]
- Diffey, B.L.; Roscoe, A.H. Exposure to solar ultraviolet radiation in flight. Aviat. Space Environ. Med. 1990, 61, 1032–1035. [Google Scholar]
- Corbett, M.F.; Hawk, J.L.M.; Herxheimer, A.; Magnus, I.A. Controlled therapeutic trials in polymorphic light eruption. Br. J. Dermatol. 1982, 107, 571–581. [Google Scholar] [CrossRef] [PubMed]
- Corbett, M.F.; Davis, A.; Magnus, I.A. Personnel radiation dosimetry in drug photosensitivity: Field studies of patients on phenothiazine therapy. Br. J. Dermatol. 1978, 98, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, F.S.; Lew, R.A.; Rouleau, L.J.; Thomson, M. Ultraviolet exposure to children from sunlight: A study using personal dosimetry. Photodermatol. Photoimmunol. Photomed. 1990, 7, 77–81. [Google Scholar]
- Melville, S.K.; Rosenthal, F.S.; Luckmann, R.; Lew, R.A. Quantitative ultraviolet skin exposure in children during selected outdoor activities. Photodermatol. Photoimmunol. Photomed. 1991, 8, 99–104. [Google Scholar]
- Diffey, B.L.; Gibson, C.J.; Haylock, R.; McKinlay, A.F. Outdoor ultraviolet exposure of children and adolescents. Br. J. Dermatol. 1996, 134, 1030–1034. [Google Scholar] [CrossRef]
- Diffey, B.L.; Gies, H.P. The confounding influence of sun exposure in melanoma. Lancet 1998, 351, 1101–1102. [Google Scholar] [CrossRef]
- Gies, H.P.; Roy, C.R.; Toomey, S.; MacLennan, R.; Watson, M. Solar UVR exposures of primary school children at three locations in Queensland. Photochem. Photobio. 1998, 68, 78–83. [Google Scholar] [CrossRef]
- Moise, A.F.; Büttner, P.G.; Harrison, S.L. Sun exposure at school. Photochem. Photobiol. 1999, 70, 269–274. [Google Scholar] [CrossRef]
- Moise, A.F.; Gies, H.P.; Harrison, S.L. Estimation of the annual solar UVR exposure dose of infants and small children in tropical Queensland, Australia. Photochem. Photobiol. 1999, 69, 457–463. [Google Scholar] [CrossRef]
- Moise, A.F.; Harrison, S.L.; Gies, H.P. Solar ultraviolet radiation exposure of infants and small children. Photodermatol. Photoimmunol. Photomed. 1999, 15, 109–114. [Google Scholar] [CrossRef]
- O’Riordan, D.L.; Stanton, W.R.; Eyeson-Annan, M.; Gies, P.; Roy, C. Correlations between reported and measured ultraviolet radiation exposure of mothers and young children. Photochem. Photobiol. 2000, 71, 60–64. [Google Scholar] [CrossRef]
- Parisi, A.V.; Meldrum, L.R.; Wong, J.C.F.; Aitken, J.; Fleming, R.A. Effect of childhood and adolescent ultraviolet exposures on cumulative exposure in South East Queensland schools. Photodermatol. Photoimmunol. Photomed. 2000, 16, 19–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diffey, B.L.; Larkö, O.; Meding, B.; Edeland, H.G.; Wester, U. Personal monitoring of exposure to ultraviolet radiation in the car manufacturing industry. Ann. Occup. Hyg. 1986, 30, 163–170. [Google Scholar] [PubMed]
- Shehade, S.A.; Roberts, P.J.; Diffey, B.L.; Foulds, I.S. Photodermatitis due to spot welding. Br. J. Dermatol. 1987, 117, 117–119. [Google Scholar] [CrossRef]
- Barth, C.; Knuschke, P.; Barth, J. UV-Strahlenbelastung in der Umgebung von Schweißarbeitsplätzen. Zeitschrift für die gesamte Hygiene und ihre Grenzgebiete 1990, 36, 654–655. [Google Scholar]
- Tenkate, T.D.; Collins, M.J. Personal ultraviolet radiation exposure of workers in a welding environment. Am. Indust. Hyg. Assoc. J. 1997, 58, 33–38. [Google Scholar] [CrossRef]
- Jekler, J.; Diffey, B.L.; Larkö, O. Ultraviolet radiation dosimetry in phototherapy for atopic dermatitis. J. Am. Acad. Dermatol. 1990, 23, 49–51. [Google Scholar] [CrossRef]
- Larkö, O.; Diffey, B.L. Occupational exposure to ultraviolet radiation in dermatology departments. Br. J. Dermatol. 1986, 114, 479–484. [Google Scholar] [CrossRef]
- Corless, D.; Gupta, S.P.; Switala, S.; Barragry, J.M.; Boucher, B.J.; Cohen, R.D.; Diffey, B.L. Response of Plasma-25-hydroxyvitamin D to ultraviolet irradiation in long-stay geriatric patients. Lancet 1978, 312, 649–651. [Google Scholar] [CrossRef]
- Toss, G.; Andersson, R.; Diffey, B.L.; Fall, P.A.; Larkö, O.; Larsson, L. Oral vitamin D and ultraviolet radiation for the prevention of vitamin D deficiency in the elderly. Acta Med. Scand. 1982, 212, 157–161. [Google Scholar] [CrossRef]
- Chuck, A.; Todd, J.; Diffey, B.L. Subliminal ultraviolet-B irradiation for the prevention of vitamin D deficiency in the elderly: A feasibility study. Photodermatol. Photoimmunol. Photomed. 2001, 17, 168–171. [Google Scholar] [CrossRef] [PubMed]
- Wright, C.; Reeder, A.I. Youth solar ultraviolet radiation exposure, concurrent activities and sun-protective practices: A review. Photochem. Photobiol. 2005, 81, 1331–1342. [Google Scholar] [CrossRef] [PubMed]
- Schmalwieser, A.W.; Siani, A.M. Review on nonoccupational personal solar UV exposure measurements. Photochem. Photobiol. 2018, 94, 900–915. [Google Scholar] [CrossRef]
- Diffey, B.L.; Kerwin, M.; Davis, A. The anatomical distribution of sunlight. Br. J. Dermatol. 1977, 97, 407–410. [Google Scholar] [CrossRef]
- Diffey, B.L.; Tate, T.J.; Davis, A. Solar dosimetry of the face: The relationship of natural ultraviolet radiation exposure to basal cell carcinoma localisation. Phys. Med. Biol. 1979, 24, 931–939. [Google Scholar] [CrossRef]
- Airey, D.K.; Wong, J.C.F.; Fleming, R.A. A comparison of human- and headform based measurements of solar ultraviolet B dose. Photodermatol. Photoimmunol. Photomed. 1995, 11, 155–158. [Google Scholar] [CrossRef]
- Kimlin, M.G.; Parisi, A.V.; Wong, J.C.F. The facial distribution of erythemal ultraviolet in south-east Queensland. Phys. Med. Biol. 1998, 43, 231–240. [Google Scholar] [CrossRef]
- Rosenthal, F.S.; Safran, M.; Taylor, H.R. The ocular dose of ultraviolet radiation from sunlight exposure. Photochem. Photobiol. 1985, 42, 163–171. [Google Scholar] [CrossRef]
- Gies, P.; Roy, C.; Elliott, G. The anatomical distribution of solar UVR with emphasis on the eye. In Proceedings of the Seventh International Congress of the International Radiation Protection Association; Pergamon Press: Sydney, Australia, 1988; pp. 341–344. [Google Scholar]
- Lindgren, G.; Diffey, B.L.; Larkö, O. Basal cell carcinoma of the eyelids and solar ultraviolet radiation exposure. Br. J. Ophthalmol. 1998, 82, 1412–1415. [Google Scholar] [CrossRef]
- Keck, G.; Kasper, I.; Schauberger, G.; Cabaj, A. Biological effects of UV-irradiation of horses with artificial UV-sources. In Human Exposure to Ultraviolet Radiation: Risk and Regulations; Passchier, W.F., Bosnjakovic, B.F.M., Eds.; Elsevier: Amsterdam, The Netherlands, 1987; pp. 71–76. [Google Scholar]
- Diffey, B.L.; Davis, A.; Johnson, M.; Harrington, T.R. A dosimeter for long wave ultraviolet radiation. Br. J. Dermatol. 1977, 97, 127–130. [Google Scholar] [CrossRef]
- Diffey, B.L.; Davis, A. A new dosimeter for the measurement of natural ultraviolet radiation in the study of photodermatoses and drug photosensitivity. Phys. Med. Biol. 1978, 23, 318–323. [Google Scholar] [CrossRef] [PubMed]
- Tate, T.J.; Diffey, B.L.; Davis, A. An ultraviolet radiation dosimeter based on the photosensitising drug nalidixic acid. Photochem. Photobiol. 1980, 31, 27–30. [Google Scholar] [CrossRef]
- Diffey, B.L.; Oliver, I.; Davis, A. A personal dosimeter for quantifying the biologically-effective sunlight exposure of patients receiving benoxaprofen. Phys. Med. Biol. 1982, 27, 1507–1513. [Google Scholar] [CrossRef] [PubMed]
- Moseley, H.; Diffey, B.L.; Marks, J.M.; Mackie, R.M. Personal solar UV-A doses received by patients undergoing oral psoralen photochemotherapy for psoriasis. Br. J. Dermatol. 1981, 105, 573–577. [Google Scholar] [CrossRef]
- Jackson, S.A. A film badge dosimeter for UVA radiation. J. Biomed. Eng. 1980, 2, 63–64. [Google Scholar] [CrossRef]
- Moseley, H.; Robertson, J.; O’Donoghue, J. The suitability of diazochrome KBL film for UV dosimetry. Phys. Med. Biol. 1984, 29, 679–685. [Google Scholar] [CrossRef]
- Zweig, A.; Henderson, W.A., Jr. A photochemical mid-ultraviolet dosimeter for practical use as a sunburn dosimeter. Photochem. Photobiol. 1976, 24, 543–549. [Google Scholar] [CrossRef]
- Fanselow, D.L.; Pathak, M.A.; Crone, M.A.; Ersfield, D.A.; Raber, P.B.; Trancik, R.J.; Dahl, M.V. Reusable ultraviolet monitors: Design, characteristics and efficacy. J. Am. Acad. Dermatol. 1983, 9, 714–724. [Google Scholar] [CrossRef]
- Moseley, H.; Mackie, R.M.; Ferguson, J. The suitability of Suncheck patches and Tanscan cards for monitoring the sunburning effectiveness of sunlight. Br. J. Dermatol. 1993, 128, 75–78. [Google Scholar] [CrossRef]
- Noha, A.M.; Amina, Y.M.; Mahata, R.H.; Bradley, D.A. Investigation of some commercial TLD chips/discs as UV dosimeters. Rad. Phys. Chem. 2001, 61, 497–499. [Google Scholar] [CrossRef]
- Otaki, H.; Kido, H.; Hiratsuka, A.; Fukuda, A.Y.; Takeuchi, N. Estimation of UV radiation dose using CaF2:Tb407 as a thermoluminescence dosimeter. J. Mater. Sci. Lett. 1994, 13, 1267–1269. [Google Scholar] [CrossRef]
- Justus, B.L.; Huston, A.L. Ultraviolet dosimetry using thermoluminescence of semiconductor-doped Vycor glass. Appl. Phys. Lett. 1995, 67, 1179–1181. [Google Scholar] [CrossRef]
- Wong, C.F.; Fleming, R.; Carter, S.J. A new dosimeter for ultraviolet B radiation. Photochem. Photobiol. 1989, 50, 611–615. [Google Scholar] [CrossRef]
- Sydenham, M.M.; Collins, M.J.; Hirst, L.W. The effectiveness of poly(allyl diglycol carbonate) (CR-39) for low-dose solar ultraviolet dosimetry. Photochem. Photobiol. 1994, 59, 58–65. [Google Scholar]
- Rontó, G.; Gáspár, S.; Bérces, A. Phage T7 in biological UV dose measurement. J. Photochem. Photobiol. 1992, 12, 285–294. [Google Scholar] [CrossRef]
- Rontó, G.; Gáspár, S.; Gróf, P.; Bérces, A.; Gugolya, Z. Ultraviolet dosimetry in outdoor measurements based on bacteriophage T7 as a biosensor. Photochem. Photobiol. 1994, 59, 209–214. [Google Scholar] [CrossRef]
- Quintern, L.E.; Furusawa, Y.; Fukutsu, K.; Holtschmidt, H. Characterization and application of UV detector spore films: The sensitivity curve of a new detector system provides good similarity to the action spectrum for UV-induced erythema in human skin. J. Photochem. Photobiol. 1997, 37, 158–166. [Google Scholar] [CrossRef]
- Diffey, B.L.; Saunders, P.J. Behaviour outdoors and its effect on personal ultraviolet exposure rate measured using a portable datalogging dosimeter. Photochem. Photobiol. 1995, 61, 615–618. [Google Scholar] [CrossRef]
- Heydenreich, J.; Wulf, H.C. Miniature personal electronic UVR dosimeter with erythema response and time-stamped readings in a wristwatch. Photochem. Photobiol. 2005, 81, 1138–1144. [Google Scholar] [CrossRef]
- Allen, M.; McKenzie, R. Enhanced UV exposure on a ski-field compared with exposures at sea level. Photochem. Photobiol. Sci. 2005, 4, 429–437. [Google Scholar] [CrossRef]
- Naggar, S.A.; Gustat, H.; Magister, H.; Rochlitzer, R. An electronic personal UV-B-dosimeter. J. Photochem. Photobiol. B Biol. 1995, 31, 83–86. [Google Scholar] [CrossRef]
- Thieden, E. Sun exposure behaviour among subgroups of the Danish population. Dan. Med. Bull. 2008, 55, 47–68. [Google Scholar] [PubMed]


© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diffey, B. The Early Days of Personal Solar Ultraviolet Dosimetry. Atmosphere 2020, 11, 125. https://doi.org/10.3390/atmos11020125
Diffey B. The Early Days of Personal Solar Ultraviolet Dosimetry. Atmosphere. 2020; 11(2):125. https://doi.org/10.3390/atmos11020125
Chicago/Turabian StyleDiffey, Brian. 2020. "The Early Days of Personal Solar Ultraviolet Dosimetry" Atmosphere 11, no. 2: 125. https://doi.org/10.3390/atmos11020125
APA StyleDiffey, B. (2020). The Early Days of Personal Solar Ultraviolet Dosimetry. Atmosphere, 11(2), 125. https://doi.org/10.3390/atmos11020125




