Comparison of Two Models to Estimate Deposition of Fungi and Bacteria in the Human Respiratory Tract
Abstract
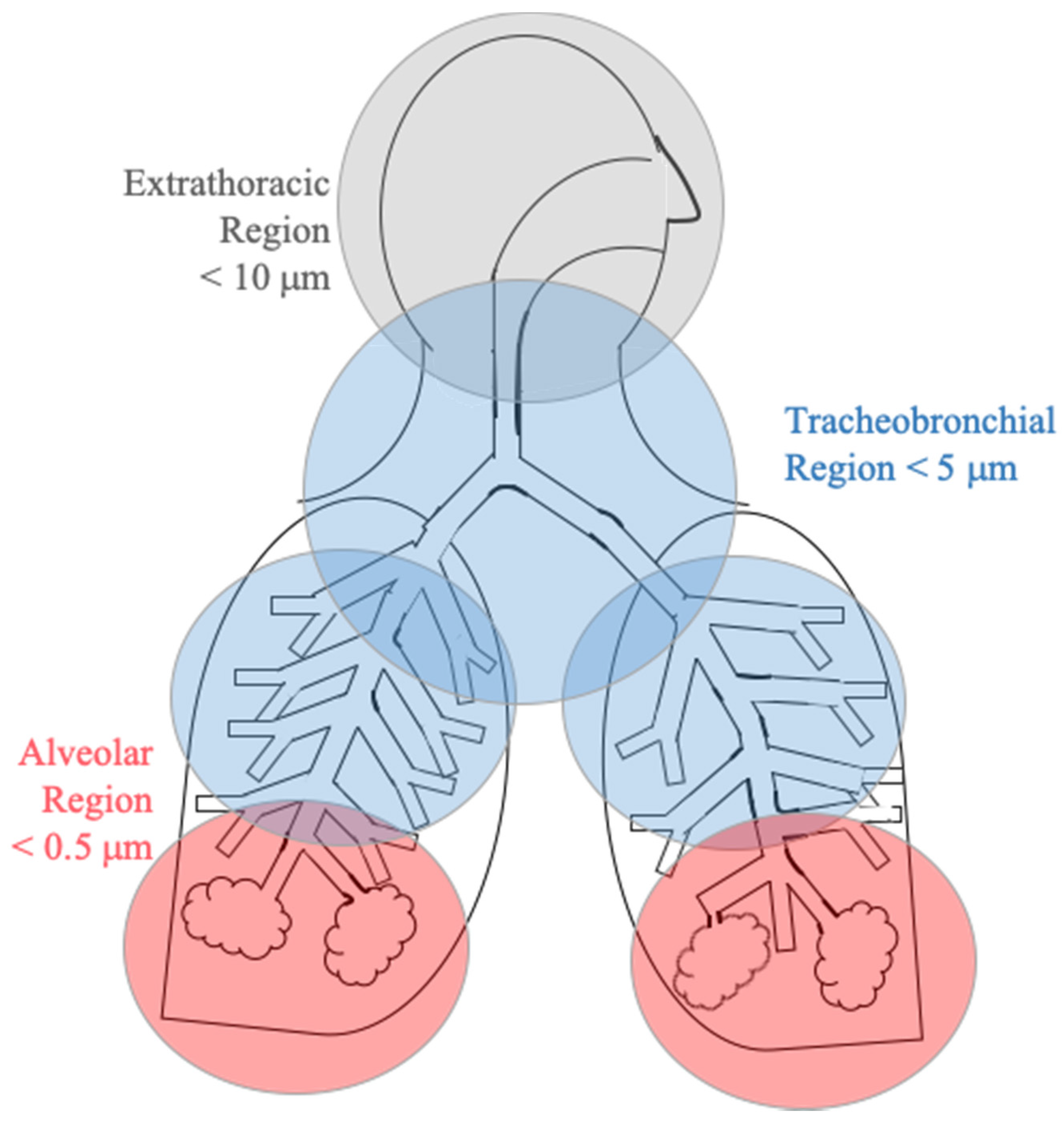
:1. Introduction
2. Experiments
2.1. Models Used
2.2. Model Input Parameters
2.3. Uncertainty Analysis
3. Results
3.1. Model Results
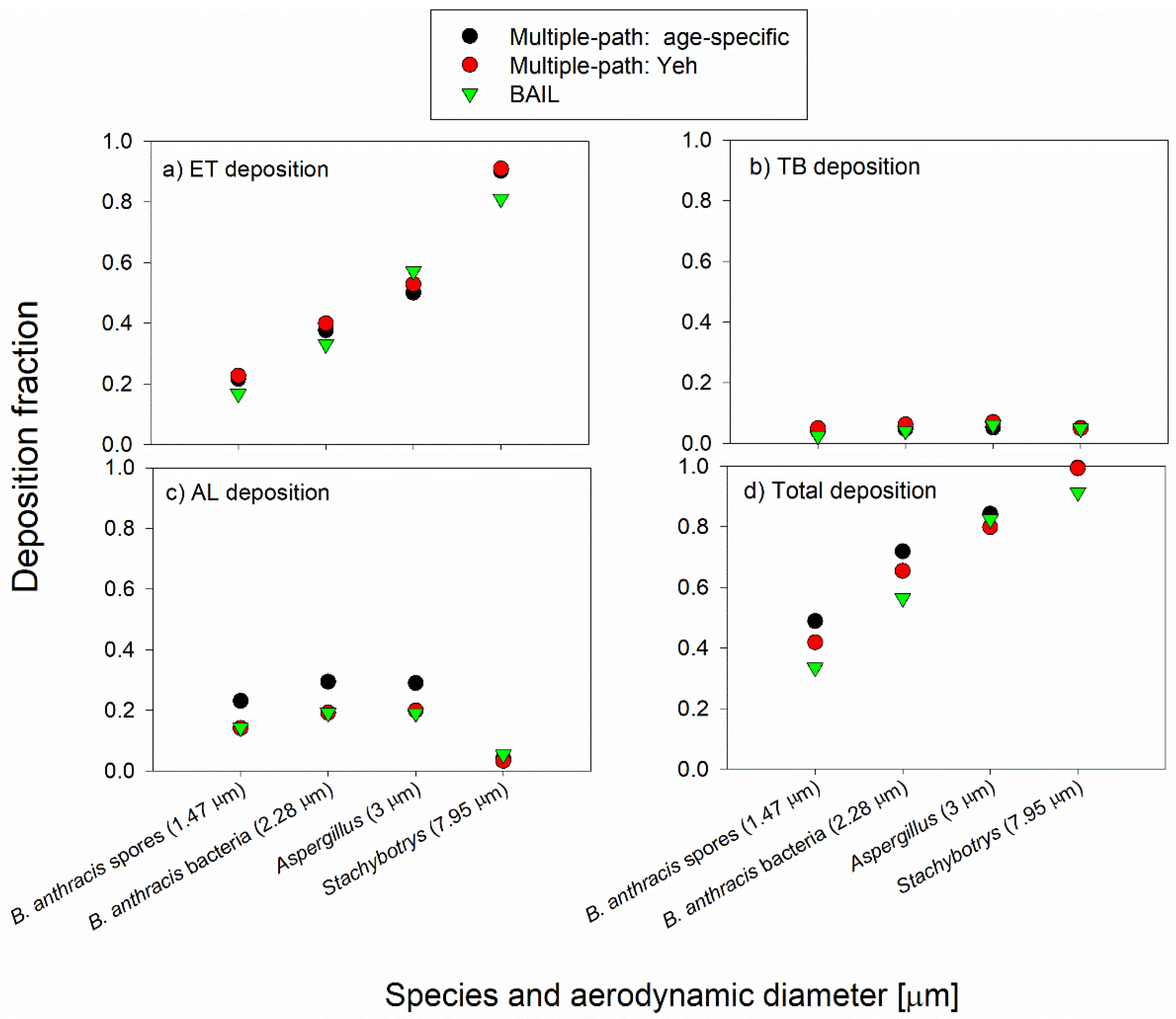
3.1.1. Default Case
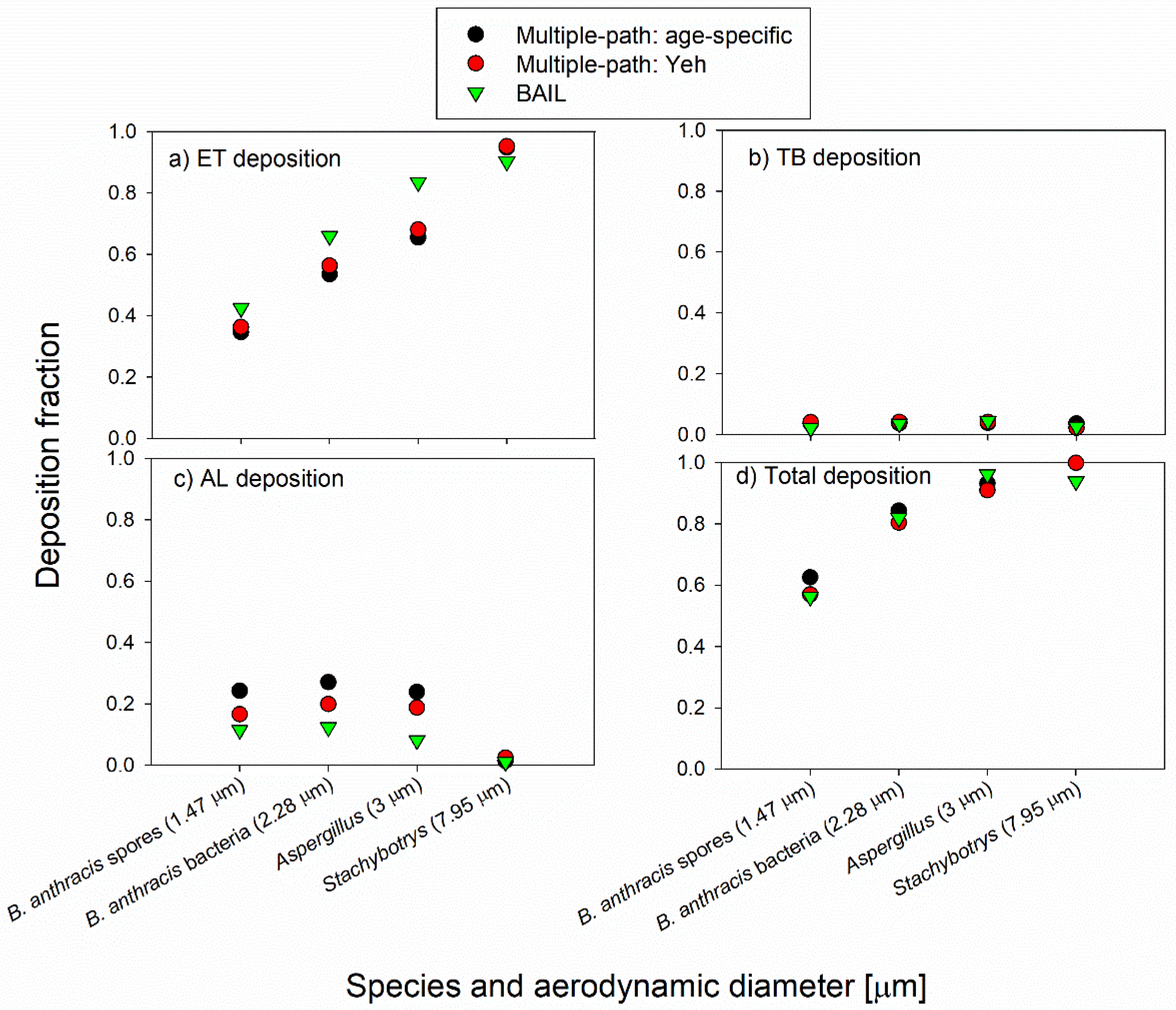
3.1.2. Light Exercise Case
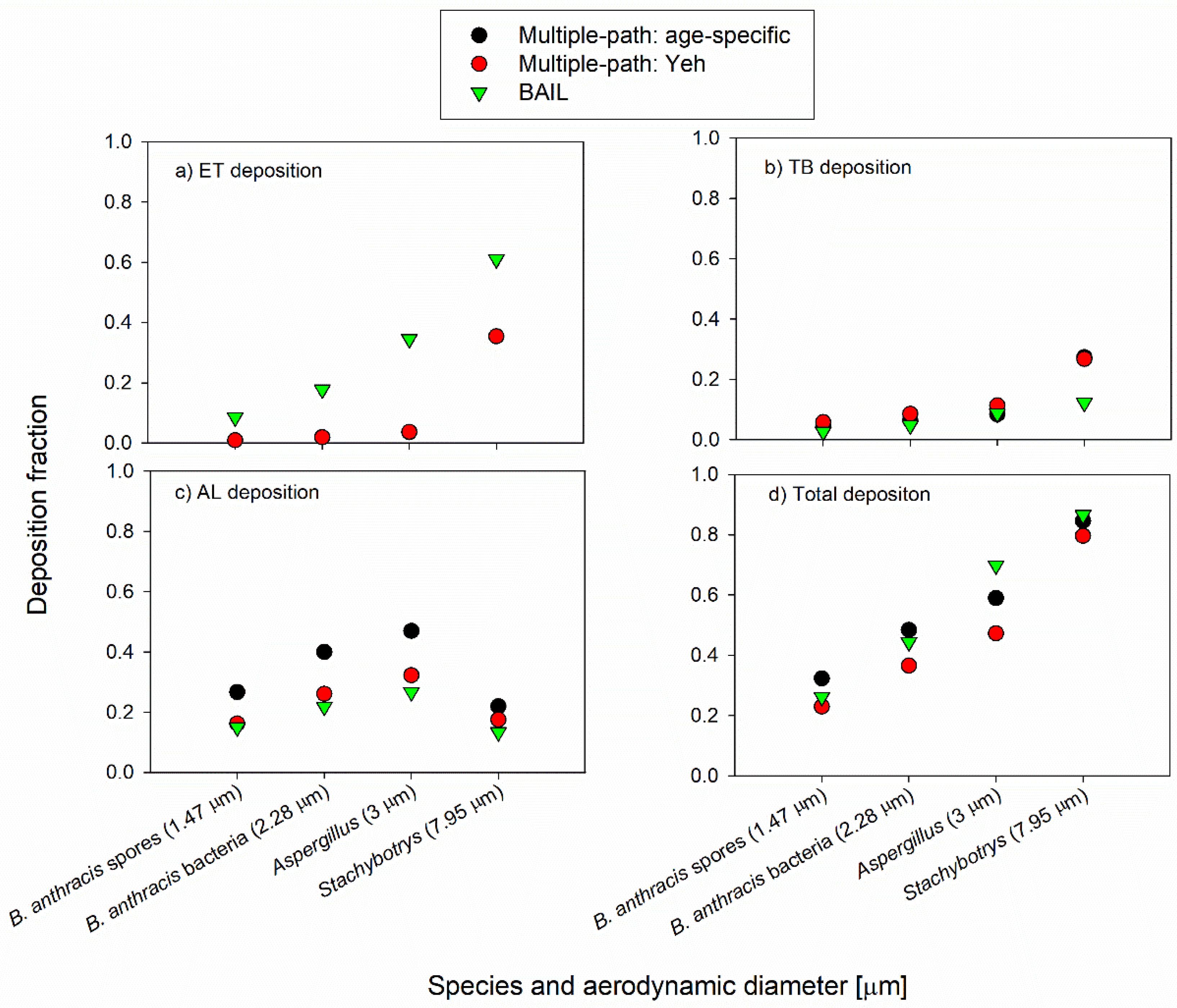
3.1.3. Mouth Breathing Case
3.2. Uncertainty Analysis
3.2.1. Effect of Changing FRC on the Deposition Fractions
3.2.2. Effect of Changing V on the Deposition Fractions
3.2.3. Effect of Changes in the Upper Respiratory Tract (URT) Volume on the Deposition Fractions
3.2.4. Effect of a Person’s Height on the Deposition Fractions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bünger, J.; Schappler-Scheele, B.; Hilgers, R.; Hallier, E. A 5-year follow-up study on respiratory disorders and lung function in workers exposed to organic dust from composting plants. Int. Arch. Occup. Environ. Health 2007, 80, 306–312. [Google Scholar] [CrossRef]
- Heldal, K.K.; Halstensen, A.S.; Thorn, J.; Diupesland, P.; Wouters, I.; Eduard, W.; Halstensen, T.S. Upper airway inflammation in waste handlers exposed to bioaerosols. Occup. Environ. Med. 2003, 60, 444–450. [Google Scholar] [CrossRef] [Green Version]
- Georgakopoulos, D.G.; Després, V.; Fröhlich-Nowoisky, J.; Psenner, R.; Ariya, P.A.; Pósfai, M.; Ahern, H.E.; Moffett, B.F.; Hill, T.C.J. Microbiology and atmospheric processes: Biological, physical and chemical characterization of aerosol particles. Biogeosciences 2009, 6, 721–737. [Google Scholar] [CrossRef] [Green Version]
- Mandal, J.; Brandl, H. Bioaerosols in Indoor Environment—A Review with Special Reference to Residential and Occupational Locations. Open Environ. Biol. Monit. J. 2011, 4, 83–96. [Google Scholar]
- Van Kampen, V.; Hoffmeyer, F.; Deckert, A.; Kendzia, B.; Casjens, S.; Neumann, H.D.; Buxtrup, M.; Willer, E.; Felten, C.; Schöneich, R.; et al. Effects of bioaerosol exposure on respiratory health in compost workers: A 13-year follow-up study. Occup. Environ. Med. 2016, 73, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Farokhi, A.; Heederik, D.; Smit, L.A.M. Respiratory health effects of exposure to low levels of airborne endotoxin—A systematic review. Environ. Health 2018, 17, 1–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garrett, M.H.; Rayment, P.R.; Hooper, M.A.; Abramson, M.J.; Hooper, B.M. Indoor airborne fungal spores, house dampness and associations with environmental factors and respiratory health in children. Clin. Exp. Allergy 1998, 28, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.H.; Ponikau, J.U.; Sherris, D.A.; Congdon, D.; Frigas, E.; Homburger, H.A.; Swanson, M.C.; Gleich, G.J.; Kita, H. Chronic rhinosinusitis: An enhanced immune response to ubiquitous airborne fungi. J. Allergy Clin. Immunol. 2004, 114, 1369–1375. [Google Scholar] [CrossRef]
- Vincent, M.; Corazza, F.; Chasseur, C.; Bladt, S.; Romano, M.; Huygen, K.; Denis, O.; Michel, O. Relationship between mold exposure, specific IgE sensitization, and clinical asthma: A case-control study. Ann. Allergy Asthma Immunol. 2018, 121, 333–339. [Google Scholar] [CrossRef]
- Richardson, M.; Bowyer, P.; Sabino, R. The human lung and Aspergillus: You are what you breathe in? Med. Mycol. 2019, 57, S145–S154. [Google Scholar] [CrossRef] [Green Version]
- Knutsen, A.P.; Slavin, R.G. Allergic bronchopulmonary aspergillosis in asthma and cystic fibrosis. Clin. Dev. Immunol. 2011, 2011, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guarner, J.; Jernigan, J.A.; Shieh, W.J.; Tatti, K.; Flannagan, L.M.; Stephens, D.S.; Popovic, T.; Ashford, D.A.; Perkins, B.A.; Zaki, S.R. Pathology and pathogenesis of bioterrorism-related inhalational anthrax. Am. J. Pathol. 2003, 163, 701–709. [Google Scholar] [CrossRef] [Green Version]
- Guidi-Rontani, C. The alveolar macrophage: The Trojan horse of Bacillus anthracis. Trends Microbiol. 2002, 10, 405–409. [Google Scholar] [CrossRef]
- Druett, H.A.; Henderson, D.W.; Packman, L.; Peacock, S. Studies on respiratory infection: I. The influence of particle size on respiratory infection with anthrax spores. J. Hyg. (Lond.) 1953, 51, 359–371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, K.H.; Kabir, E.; Jahan, S.A. Airborne bioaerosols and their impact on human health. J. Environ. Sci. (China) 2018, 67, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Chan, T.L.; Lippmann, M. Experimental measurements and empirical modeling of the regional deposition of inhaled particles in humans. Am. Ind. Hygeine Assoc. 1980, 41, 399–408. [Google Scholar] [CrossRef]
- Heyder, J.; Gebhart, J.; Rudolf, G.; Schiller, C.F.; Stahlhofen, W. Deposition of particles in the human respiratory tract in the size range 0.005–15 μm. J. Aerosol Sci. 1986, 17, 811–825. [Google Scholar] [CrossRef]
- Dagenais, T.R.T.; Keller, N.P. Pathogenesis of Aspergillus fumigatus in invasive aspergillosis. Clin. Microbiol. Rev. 2009, 22, 447–465. [Google Scholar] [CrossRef] [Green Version]
- Heyder, J.; Blanchard, J.D.; Feldman, H.A.; Brain, J.D. Convective mixing in human respiratory tract—Estimates with aerosol boli. J. Appl. Physiol. 1988, 64, 1273–1278. [Google Scholar] [CrossRef]
- Hofmann, W. Modelling inhaled particle deposition in the human lung-A review. J. Aerosol Sci. 2011, 42, 693–724. [Google Scholar] [CrossRef]
- Islam, M.S.; Paul, G.; Ong, H.X.; Young, P.M.; Gu, Y.T.; Saha, S.C. A review of respiratory anatomical development, air flow characterization and particle deposition. Int. J. Environ. Res. Public Health 2020, 17, 380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- International Commission on Radiological Protection. Human Respiratory Tract Model for Radiological Protection. Ann. ICRP 1994, 24, 1–493. [Google Scholar] [CrossRef]
- Guha, S.; Hariharan, P.; Myers, M.R. Enhancement of ICRP’s lung deposition model for pathogenic bioaerosols. Aerosol Sci. Technol. 2014, 48, 1226–1235. [Google Scholar] [CrossRef]
- Anjilvel, S.; Asgharian, B. A multiple-path model of particle deposition in the rat lung. Fundam. Appl. Toxicol. 1995, 28, 41–50. [Google Scholar] [CrossRef] [Green Version]
- Asgharian, B.; Hofmann, W.; Bergmann, R. Particle deposition in a multiple-path model of the human lung. Aerosol Sci. Technol. 2001, 34, 332–339. [Google Scholar] [CrossRef]
- Yeh, H.-C.; Schum, G.M. Models of Human Lung Airways and Their Application to Inhaled Particle Deposition. Bull. Math. Biol. 1980, 42, 461–480. [Google Scholar] [CrossRef]
- Shelton, B.G.; Kirkland, K.H.; Flanders, W.D.; Morris, G.K. Profiles of airborne fungi in buildings and outdoor environments in the United States. Appl. Environ. Microbiol. 2002, 68, 1743–1753. [Google Scholar] [CrossRef] [Green Version]
- Fryar, C.D.C.; Gu, Q.; Ogden, C.L.; Flegal, K.M.; McDowell, M.A.; Fryar, C.D.C.; Ogden, C.L.; Flegal, K.M. Anthropometric Reference Data for Children and Adults: United States, 2003–2006. Vital Heal. Stat. 2010, 11, 2007–2010. [Google Scholar]
- Domsch, K.D.; Gams, W.; Anderson, T.-H. Compendium of Soil Fungi; Academic Press: London, UK, 1980. [Google Scholar]
- Spencer, R.C. Bacillus anthracis. J. Clin. Pathol. 2003, 56, 182–187. [Google Scholar] [CrossRef] [Green Version]
- Lamb, D.; Verlinde, J. Physics and Chemistry of Clouds; Cambridge University Press: Cambridge, UK, 2011; ISBN 9780521899109. [Google Scholar]
- Tian, L.; Ahmadi, G.; Wang, Z.; Hopke, P.K. Transport and deposition of ellipsoidal fibers in low Reynolds number flows. J. Aerosol Sci. 2012, 45, 1–18. [Google Scholar] [CrossRef]
- Sudakin, D.L. Stachybotrys chartarum: Current knowledge of its role in disease. MedGenMed Medscape Gen. Med. 2000, 2, E11. [Google Scholar]
- Islam, Z.; Harkema, J.R.; Pestka, J.J. Satratoxin G from the black mold Stachybotrys chartarum evokes olfactory sensory neuron loss and inflammation in the murine nose and brain. Environ. Health Perspect. 2006, 114, 1099–1107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carey, S.A.; Plopper, C.G.; Hyde, D.M.; Islam, Z.; Pestka, J.J.; Harkema, J.R. Satratoxin-G from the Black Mold Stachybotrys chartarum Induces Rhinitis and Apoptosis of Olfactory Sensory Neurons in the Nasal Airways of Rhesus Monkeys. Toxicol. Pathol. 2012, 40, 887–898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CDC Inhalation Anthrax. Available online: https://www.cdc.gov/anthrax/basics/types/inhalation.html (accessed on 19 May 2020).
- Bartrand, T.A.; Weir, M.H.; Haas, C.N. Dose-response models for inhalation of Bacillus anthracis spores: Interspecies comparisons. Risk Anal. 2008, 28, 1115–1124. [Google Scholar] [CrossRef] [PubMed]
- Reponen, T. Aerodynamic Diameters and Respiratory Deposition Estimates of Viable Fungal Particles in Mold Problem Dwellings. Aerosol Sci. Technol. 1995, 22, 11–23. [Google Scholar] [CrossRef]
- Stahlhofen, W.; Rudolf, G.; James, A.C. Intercomparison of Experimental Regional Aerosol Deposition Data. J. Aerosol Med. Depos. Clear. Eff. Lung 1989, 2, 285–308. [Google Scholar] [CrossRef]
- Cho, S.H.; Seo, S.C.; Schmechel, D.; Grinshpun, S.A.; Reponen, T. Aerodynamic characteristics and respiratory deposition of fungal fragments. Atmos. Environ. 2005, 39, 5454–5465. [Google Scholar] [CrossRef]
- Birchall, A.; Bailey, M.R.; James, A.C. LUDEP: A lung dose evaluation program. Radiat. Prot. Dosim. 1991, 38, 167–174. [Google Scholar] [CrossRef]
- Thomas, R.J. Particle size and pathogenicity in the respiratory tract. Virulence 2013, 4, 847–858. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, C.S.; Hu, S.C. Regional deposition of inhaled particles in human lungs; comparison between men and women. J. Appl. Physiol. 1998, 84, 1834–1844. [Google Scholar] [CrossRef]
- Mainelis, G.; Willeke, K.; Baron, P.; Reponen, T.; Grinshpun, S.A.; Górny, R.L.; Trakumas, S. Electrical charges on airborne microorganisms. J. Aerosol Sci. 2001, 32, 1087–1110. [Google Scholar] [CrossRef]
- Ali, M.; Reddy, R.N.; Mazumder, M.K. Electrostatic charge effect on respirable aerosol particle deposition in a cadaver based throat cast replica. J. Electrostat. 2008, 66, 401–406. [Google Scholar] [CrossRef]
- Prodi, V.; Mularoni, A. Electrostatic Lung Deposition Experiments. Ann. Occup. Hyg. 1985, 29, 229–240. [Google Scholar] [PubMed]
- Saini, D.; Gunamgari, J.; Zulaloglu, C.; Sims, R.A.; Mazumder, M.K. Effect of electrostatic charge and size distributions on respirable aerosol deposition in lung model. Conf. Rec. IAS Annu. Meet. IEEE Ind. Appl. Soc. 2004, 2, 948–952. [Google Scholar]
- Reponen, T.; Willeke, K.; Ulevicius, V.; Reponen, A.; Grinshpun, S.A. Effect of relative humidity on the aerodynamic diameter and respiratory deposition of fungal spores. Atmos. Environ. 1996, 30, 3967–3974. [Google Scholar] [CrossRef]
- Zhen, H.; Han, T.; Fennell, D.E.; Mainelis, G. A systematic comparison of four bioaerosol generators: Affect on culturability and cell membrane integrity when aerosolizing Escherichia coli bacteria. J. Aerosol Sci. 2014, 70, 67–79. [Google Scholar] [CrossRef]
- Ferron, G.A.; Oberdorster, G.; Henneberg, R. Estimation of the Deposition of Aerosolized Drugs in the Human Respiratory Tract Due to Hygroscopic Growth. J. Aerosol Med. 1989, 2, 271–284. [Google Scholar] [CrossRef]
- Broday, D.M.; Georgopoulos, P.G. Growth and deposition of hygroscopic particulate matter in the human lungs. Aerosol Sci. Technol. 2001, 34, 144–159. [Google Scholar] [CrossRef]
- Harapan, H.; Itoh, N.; Yufika, A.; Winardi, W.; Keam, S.; Te, H.; Megawati, D.; Hayati, Z.; Wagner, A.L.; Mudatsir, M. Coronavirus disease 2019 (COVID-19): A literature review. J. Infect. Public Health 2020, 13, 667–673. [Google Scholar] [CrossRef]
- Lindsley, W.G.; Pearce, T.A.; Hudnall, J.B.; Davis, K.A.; Davis, S.M.; Fisher, M.A.; Khakoo, R.; Palmer, J.E.; Clark, K.E.; Celik, I.; et al. Quantity and size distribution of cough-generated aerosol particles produced by influenza patients during and after illness. J. Occup. Environ. Hyg. 2012, 9, 443–449. [Google Scholar] [CrossRef]
- Cox, C.S.W.; Christopher, M. Bioaerosols Handbook; CRC Press: Boca Raton, FL, USA, 1995. [Google Scholar]
| Model Input Parameter | Value |
|---|---|
| Functional Residual Capacity (FRC) | 3075.75 mL |
| Upper Respiratory Tract (URT) volume | 48.2 mL |
| Tidal volume, sitting | 568.33 mL |
| Tidal volume, light exercise | 1122.88 mL |
| Breathing frequency | 12 breaths/minute for default and mouth-breathing cases 14 breaths/minute for light exercise case |
| Inhalation time fraction | 50% |
| Species | Shape and Approximate Dimensions (µm) | Aerodynamic Diameter (µm), Oblate | Aerodynamic Diameter (µm), Prolate | Average Aerodynamic Diameter (µm) |
|---|---|---|---|---|
| Bacillus anthracis spores | Ellipsoid; 0.5 × 0.5 × 1 | 1.39 | 1.55 | 1.47 |
| Bacillus anthracis cells | Long rod; 1.25 × 6.5 | 2.14 | 2.41 | 2.28 |
| Aspergillus clavatus | Spherical; 3 | 3 | 3 | 3 |
| Stachybotrys chartarum | Ellipsoid; 3 × 3 × 5 | 7.66 | 8.34 | 8 |
| Region | Tidal Volume | Functional Residual Capacity | ||||||
|---|---|---|---|---|---|---|---|---|
| −20% | Average | +20% | −20% | Average | +20% | |||
| B. anthracis spores | Default | ET | 0.1970 | 0.2165 | 0.2620 | 0.2130 | 0.2165 | 0.2190 |
| TB | 0.0414 | 0.0407 | 0.0386 | 0.0399 | 0.0407 | 0.0415 | ||
| AL | 0.1982 | 0.2312 | 0.2280 | 0.2557 | 0.2312 | 0.2087 | ||
| Total | 0.4366 | 0.4884 | 0.5285 | 0.5086 | 0.4884 | 0.4691 | ||
| Light Exercise | ET | 0.2980 | 0.3460 | 0.3895 | 0.9990 | 0.3460 | 0.3485 | |
| TB | 0.0377 | 0.0370 | 0.0366 | 0.0376 | 0.0370 | 0.0368 | ||
| AL | 0.2467 | 0.2421 | 0.2327 | 0.2524 | 0.2421 | 0.2307 | ||
| Total | 0.5823 | 0.6254 | 0.6587 | 0.6335 | 0.6254 | 0.6160 | ||
| Mouth Breathing | ET | 0.0095 | 0.0095 | 0.0095 | 0.0095 | 0.0095 | 0.0095 | |
| TB | 0.0478 | 0.0469 | 0.0465 | 0.0460 | 0.0469 | 0.0478 | ||
| AL | 0.2355 | 0.2666 | 0.2859 | 0.2948 | 0.2666 | 0.2406 | ||
| Total | 0.2928 | 0.3230 | 0.3419 | 0.3503 | 0.3230 | 0.2979 | ||
| B. anthracis bacteria | Default | ET | 0.3315 | 0.3765 | 0.4160 | 0.3705 | 0.3765 | 0.3820 |
| TB | 0.0521 | 0.0473 | 0.0439 | 0.0458 | 0.0473 | 0.0487 | ||
| AL | 0.2783 | 0.2944 | 0.2975 | 0.3184 | 0.2944 | 0.2710 | ||
| Total | 0.6618 | 0.7182 | 0.7574 | 0.7346 | 0.7182 | 0.7017 | ||
| Light Exercise | ET | 0.4805 | 0.5350 | 0.5810 | 0.5315 | 0.5350 | 0.5390 | |
| TB | 0.0399 | 0.0374 | 0.0361 | 0.0388 | 0.0374 | 0.0369 | ||
| AL | 0.2879 | 0.2706 | 0.2506 | 0.2778 | 0.2706 | 0.2613 | ||
| Total | 0.8082 | 0.8430 | 0.8677 | 0.8480 | 0.8430 | 0.8372 | ||
| Mouth Breathing | ET | 0.0180 | 0.0195 | 0.0210 | 0.0195 | 0.0195 | 0.0195 | |
| TB | 0.0671 | 0.0643 | 0.0628 | 0.0622 | 0.0643 | 0.0662 | ||
| AL | 0.3583 | 0.4000 | 0.4253 | 0.4325 | 0.4000 | 0.3683 | ||
| Total | 0.4434 | 0.4838 | 0.5091 | 0.5142 | 0.4838 | 0.4540 | ||
| Aspergillus clavatus | Default | ET | 0.4530 | 0.5010 | 0.5420 | 0.4940 | 0.5010 | 0.5080 |
| TB | 0.0593 | 0.0521 | 0.0470 | 0.0506 | 0.0521 | 0.0537 | ||
| AL | 0.2841 | 0.2900 | 0.2849 | 0.3090 | 0.2900 | 0.2708 | ||
| Total | 0.7964 | 0.8431 | 0.8739 | 0.8536 | 0.8431 | 0.8325 | ||
| Light Exercise | ET | 0.6050 | 0.6550 | 0.6950 | 0.6510 | 0.6550 | 0.6580 | |
| TB | 0.0413 | 0.0385 | 0.0374 | 0.0417 | 0.0385 | 0.0371 | ||
| AL | 0.2638 | 0.2386 | 0.2145 | 0.2419 | 0.2386 | 0.2334 | ||
| Total | 0.9101 | 0.9321 | 0.9469 | 0.9346 | 0.9321 | 0.9285 | ||
| Mouth Breathing | ET | 0.0330 | 0.0360 | 0.0400 | 0.0360 | 0.0360 | 0.0360 | |
| TB | 0.0887 | 0.0843 | 0.0819 | 0.0819 | 0.0843 | 0.0869 | ||
| AL | 0.4248 | 0.4693 | 0.4960 | 0.5000 | 0.4693 | 0.4382 | ||
| Total | 0.5465 | 0.5896 | 0.6179 | 0.6179 | 0.5896 | 0.5611 | ||
| Stachybotrys chartarum | Default | ET | 0.8825 | 0.9025 | 0.9165 | 0.9000 | 0.9025 | 0.9045 |
| TB | 0.0589 | 0.0509 | 0.0462 | 0.0560 | 0.0509 | 0.0480 | ||
| AL | 0.0487 | 0.0412 | 0.0335 | 0.0391 | 0.0412 | 0.0413 | ||
| Total | 0.9901 | 0.9946 | 0.9962 | 0.9951 | 0.9946 | 0.9938 | ||
| Light Exercise | ET | 0.9360 | 0.9485 | 0.9575 | 0.9485 | 0.9485 | 0.9495 | |
| TB | 0.0408 | 0.0366 | 0.0329 | 0.0406 | 0.0366 | 0.0332 | ||
| AL | 0.0217 | 0.0138 | 0.0088 | 0.0106 | 0.0138 | 0.0163 | ||
| Total | 0.9985 | 0.9988 | 0.9992 | 0.9997 | 0.9988 | 0.9990 | ||
| Mouth Breathing | ET | 0.3260 | 0.3540 | 0.3770 | 0.3540 | 0.3540 | 0.3540 | |
| TB | 0.2645 | 0.2732 | 0.2881 | 0.3004 | 0.2732 | 0.2576 | ||
| AL | 0.2170 | 0.2189 | 0.2067 | 0.2077 | 0.2189 | 0.2195 | ||
| Total | 0.8075 | 0.8462 | 0.8718 | 0.8621 | 0.8462 | 0.8311 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sagona, J.A.; Secondo, L.E.; Mainelis, G. Comparison of Two Models to Estimate Deposition of Fungi and Bacteria in the Human Respiratory Tract. Atmosphere 2020, 11, 561. https://doi.org/10.3390/atmos11060561
Sagona JA, Secondo LE, Mainelis G. Comparison of Two Models to Estimate Deposition of Fungi and Bacteria in the Human Respiratory Tract. Atmosphere. 2020; 11(6):561. https://doi.org/10.3390/atmos11060561
Chicago/Turabian StyleSagona, Jessica A., Lynn E. Secondo, and Gediminas Mainelis. 2020. "Comparison of Two Models to Estimate Deposition of Fungi and Bacteria in the Human Respiratory Tract" Atmosphere 11, no. 6: 561. https://doi.org/10.3390/atmos11060561
APA StyleSagona, J. A., Secondo, L. E., & Mainelis, G. (2020). Comparison of Two Models to Estimate Deposition of Fungi and Bacteria in the Human Respiratory Tract. Atmosphere, 11(6), 561. https://doi.org/10.3390/atmos11060561





