Conditions for a Meaningful Health Impact Assessment for Local Stakeholders: The Example of the Arve Valley in France
Abstract
1. Introduction
2. Methods
2.1. Stakeholder Involvement
2.2. Defining the Scope of the Health Impact Assessment (HIA)
2.3. Study Period and Study Area
2.4. Scenarios
- -
- ”Without anthropogenic pollution”, where none of the municipalities would exceed the concentrations observed in the less polluted rural municipalities. The threshold was fixed at the 5th percentile of the PM2.5 annual concentrations considering the whole surface of the municipality (i.e., 4.9 µg/m3).
- -
- “Decrease by 30%”, where all concentrations would be decreased by 30%.
- -
- “Decrease by 10%”, where all concentrations would be decreased by 10%.
- -
- “WHO Guidelines scenario“, where none of the municipalities would exceed the PM2.5 WHO guideline value of 10 µg/m3.
2.5. Exposure to PM2.5
- -
- “Whole area” approach: average of gridded-concentrations, weighted by the surface covered by each cell overlapping with the municipality.
- -
- “Inhabited areas” approach: average of gridded-concentrations, weighted by the surface excluding cells overlapping with natural spaces based on the 200 m resident’s location data.
- -
- “Population-weighted” approach: average of gridded-concentrations, weighted by the surface excluding cells overlapping with natural spaces based on the 200 m resident’s location data, and weighted by the population of the corresponding cell.
2.6. Choice of the Concentration–Response Function
2.7. Health Impact Equations
3. Results
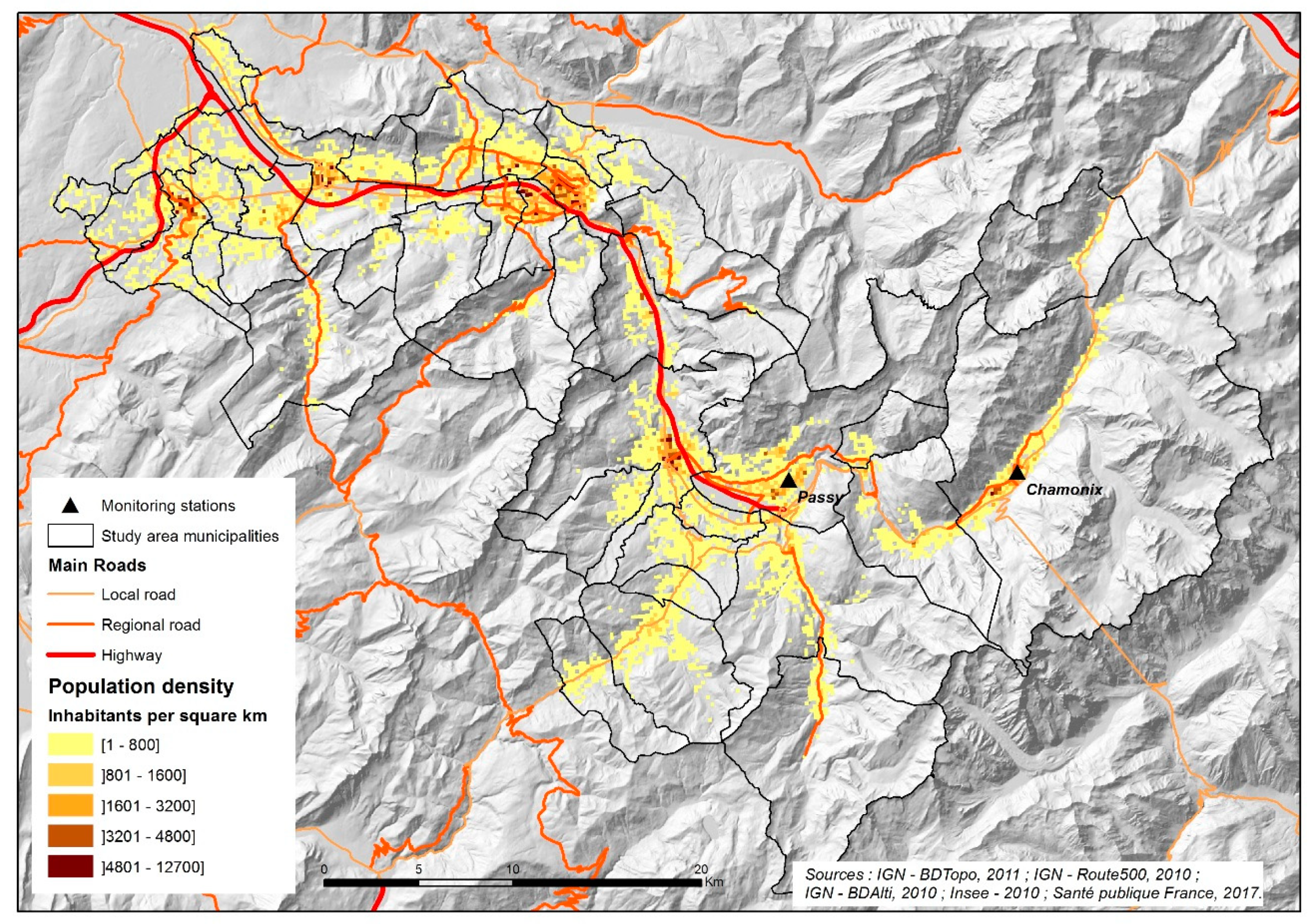
3.1. Main Characteristics of the Study Area
3.1.1. Population and Mortality
3.1.2. Exposure Assessment
3.2. Mortality Impacts of Chronic Exposure to PM2.5
3.3. Sensitivity Analyses
3.4. Communication of Results
4. Discussion
4.1. Summary and Relevance of the HIA Results in the Local Context
4.2. Limits and Uncertainties
4.3. Integration of the HIA in the PPA
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hoek, G.; Krishnan, R.M.; Beelen, R.; Peters, A.; Ostro, B.; Brunekreef, B.; Kaufman, J.D. Long-term air pollution exposure and cardio- respiratory mortality: A review. Environ. Health 2013, 12, 43. [Google Scholar] [PubMed]
- Pope, C.A.; Burnett, R.T.; Thurston, G.D.; Thun, M.J.; Calle, E.E.; Krewski, D.; Godleski, J.J. Cardiovascular Mortality and Long-Term Exposure to Particulate Air Pollution: Epidemiological Evidence of General Pathophysiological Pathways of Disease. Circulation 2004, 109, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Brook, R.D.; Rajagopalan, S.; Pope, C.A.; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A.; et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the american heart association. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef] [PubMed]
- Hoek, G.; Raaschou-Nielsen, O. Impact of fine particles in ambient air on lung cancer. Chin. J. Cancer 2014, 33, 197–203. [Google Scholar] [PubMed]
- Centre International de Recherche sur le Cancer. Les Gaz D’échappement des Moteurs Diesel Cancérogènes; Organisation Mondiale de la Santé: Lyon, France, 2012; pp. 1–3. [Google Scholar]
- Beelen, R.; Raaschou-Nielsen, O.; Stafoggia, M.; Andersen, Z.J.; Weinmayr, G.; Hoffmann, B.; Wolf, K.; Samoli, E.; Fischer, P.; Nieuwenhuijsen, M.; et al. Effects of long-term exposure to air pollution on natural-cause mortality: An analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet 2014, 383, 785–795. [Google Scholar] [PubMed]
- Pope, C.A.; Dockery, D.W. Health effects of fine particulate air pollution: Lines that connect. J. Air Waste Manag. Assoc. 2006, 56, 709–742. [Google Scholar] [CrossRef]
- WHO. Review of Evidence on Health Aspectes of Air Pollution—Revihaap Project; World Health Organisation: Copenhague, Danemark, 2013; pp. 1–309. [Google Scholar]
- WHO. Health Risks of Air Pollution in Europe—Hrapie Project—Recommandations for Concentration-Response Functions for Cost-Benefits Analysis of Particulate Matter, Ozone and Nitrogen Dioxide; WHO Regional Office for Europe: Copenhague, Danemark, 2013; pp. 1–60. [Google Scholar]
- Medina, S.; Ballester, F.; Chanel, O.; Declercq, C.; Pascal, M. Quantifying the health impacts of outdoor air pollution: Useful estimations for public health action. J. Epidemiol. Community Health 2013, 67, 480–483. [Google Scholar]
- Préfecture-de-Haute-Savoie. Plan. de Protection de L’atmosphère de la Vallée de l’Arve; Préfecture-de-Haute-Savoie: Annecy, France, 2012; pp. 1–69. [Google Scholar]
- Bonvalot, L.; Tuna, T.; Fagault, Y.; Jaffrezo, J.L.; Jacob, V.; Chevrier, F.; Bard, E. Estimating contributions from biomass burning, fossil fuel combustion, and biogenic carbon to carbonaceous aerosols in the Valley of Chamonix: A dual approach based on radiocarbon and levoglucosan. Atmos. Chem. Phys. 2016, 16, 13753–13772. [Google Scholar] [CrossRef]
- Judgment of the Court (Seventh Chamber) of 24 October 2019 6 European Commission v French Republic—Case C-636/18; Court of justice of the European Union: Luxembourg, 2019.
- Roussel, I. Dans la vallée de l’Arve, une approche innovante de la gestion de la pollution atmosphérique. Pollut. Atmos. 2017, 231–232. [Google Scholar]
- Préfecture-de-Haute-Savoie. Enquête Publique—Plan de Protection de L’atmosphère (Projet); Préfecture de Haute Savoie: Annecy, France, 2011; pp. 1–399. [Google Scholar]
- Cassagne, E.P.; Martin, S.; Ségala, C. Suivi du Changement D’équipements et de L’évolution des Pratiques Liées à la Combustion de Biomasse Dans le Cadre de la Prime Air Bois de la Vallée de l’Arve; Agence de la transition écologique: Montrouge, France, 2018; pp. 1–110. [Google Scholar]
- SM3A. Le SM3A et la politique de l’air—Le fond air bois. Available online: http://www.riviere-arve.org/projets/fonds-chaleur-air-bois.htm (accessed on 2 March 2020).
- Pascal, M.; de Crouy Chanel, P.; Wagner, V.; Corso, M.; Tillier, C.; Bentayeb, M.; Blanchard, M.; Cochet, A.; Pascal, L.; Host, S.; et al. The mortality impacts of fine particles in France. Sci. Total Environ. 2016, 571, 416–425. [Google Scholar] [CrossRef]
- Pascal, M.; Yvon, J.-M.; Medina, S. Pollution Atmosphérique. Guide Pour la Réalisation D’une Évaluation Quantitative des Impacts sur la Santé (EQIS). EQIS Avec une Exposition Modélisée; Santé Publique France: Saint-Maurice, Switzerland, 2019; p. 92. [Google Scholar]
- Bhatia, R. Health Impact Assessment, a Guide for Practice; Human Impact Partners: Oakland, CA, USA, 2011; pp. 1–89. [Google Scholar]
- Pascal, M.; Corso, M.; Chanel, O.; Declercq, C.; Badaloni, C.; Cesaroni, G.; Henschel, S.; Meister, K.; Haluza, D.; Martin-Olmedo, P.; et al. Assessing the public health impacts of urban air pollution in 25 European cities: Results of the Aphekom project. Sci. Total Environ. 2013, 449, 390–400. [Google Scholar] [CrossRef] [PubMed]
- Bentayeb, M.; Stempfelet, M.; Wagner, V.; Zins, M.; Bonenfant, S.; Songeur, C.; Sanchez, O.; Rosso, A.; Brulfert, G.; Rios, I.; et al. Retrospective modeling outdoor air pollution at a fine spatial scale in France, 1989-2008. Atmos. Environ. 2014, 92, 267–279. [Google Scholar] [CrossRef]
- Bentayeb, M.; Wagner, V.; Stempfelet, M.; Zins, M.; Goldberg, M.; Pascal, M.; Larrieu, S.; Beaudeau, P.; Cassadou, S.; Eilstein, D.; et al. Association between long-term exposure to air pollution and mortality in France: A 25-year follow-up study. Environ. Int. 2015, 85, 5–14. [Google Scholar] [CrossRef]
- Beelen, R.; Stafoggia, M.; Raaschou-Nielsen, O.; Andersen, Z.J.; Xun, W.W.; Katsouyanni, K.; Dimakopoulou, K.; Brunekreef, B.; Weinmayr, G.; Hoffmann, B.; et al. Long-term Exposure to Air Pollution and Cardiovascular Mortality: An Analysis of 22 European Cohorts. Epidemiology 2014, 25, 368–378. [Google Scholar] [CrossRef] [PubMed]
- de Hoogh, K.; Wang, M.; Adam, M.; Badaloni, C.; Beelen, R.; Birk, M.; Cesaroni, G.; Cirach, M.; Declercq, C.; Dedele, A.; et al. Development of land use regression models for particle composition in twenty study areas in Europe. Environ. Sci. Technol. 2013, 47, 5778–5786. [Google Scholar] [CrossRef] [PubMed]
- Terrenoire, E.; Bessagnet, B.; Rouïl, L.; Tognet, F.; Pirovano, G.; Létinois, L.; Beauchamp, M.; Colette, A.; Thunis, P.; Amann, M.; et al. High-resolution air quality simulation over Europe with the chemistry transport model CHIMERE. Geosci. Model. Dev. 2015, 8, 21–42. [Google Scholar] [CrossRef]
- Soulhac, L.; Salizzoni, P.; Mejean, P.; Didier, D.; Rios, I. The model SIRANE for atmospheric urban pollutant dispersion; PART II, validation of the model on a real case study. Atmos. Environ. 2012, 49, 320–337. [Google Scholar] [CrossRef]
- Soulhac, L.; Salizzoni, P.; Cierco, F.X.; Perkins, R. The model SIRANE for atmospheric urban pollutant dispersion; part I, presentation of the model. Atmos. Environ. 2011, 45, 7379–7395. [Google Scholar] [CrossRef]
- Carey, I.M.; Atkinson, R.W.; Kent, A.J.; Van Staa, T.; Cook, D.G.; Anderson, H.R. Mortality associations with long-term exposure to outdoor air pollution in a national English cohort. Am. J. Respir. Crit. Care Med. 2013, 187, 1226–1233. [Google Scholar] [CrossRef]
- Cesaroni, G.; Badaloni, C.; Gariazzo, C.; Stafoggia, M.; Sozzi, R.; Davoli, M.; Forastiere, F. Long-term exposure to urban air pollution and mortality in a cohort of more than a million adults in Rome. Environ. Health Perspect. 2013, 121, 324–331. [Google Scholar] [CrossRef]
- Pascal, M.; de Crouy Chanel, P.; Wagner, V.; Yvon, J.M.; Saura, C. Impact de L’exposition Chronique aux Particules Fines sur la Mortalité Dans la Vallée de L’ARVE; Santé Publique France: Saint-Maurice, Switzerland, 2017; p. 41. [Google Scholar]
- Pascal, M.; De Crouy Chanel, P.; Corso, M.; Medina, S.; Wagner, V.; Goria, S.; Beaudeau, P.; Bentayeb, M.; Le Tertre, A.; Ung, A.; et al. Impacts de L’exposition Chronique aux Particules Fines sur la Mortalité‚ en France Continentale et Analyse des Gains en Santé‚ de Plusieurs Scénarii de Réduction de la Pollution Atmosphérique; Santé Publique France: Saint-Maurice, Switzerland, 2016; pp. 1–161. [Google Scholar]
- Atmo-Air-Rhône-Alpes. Indicateurs Air Santé: Identification des Points de Cumul de Facteurs de Défaveur Environnementaux, Socio-Économiques et Sanitaires; Atmo-Air-Rhône-Alpes: Lyon, France, 2019; pp. 1–14. [Google Scholar]
- Naeher, L.P.; Brauer, M.; Lipsett, M.; Zelikoff, J.T.; Simpson, C.D.; Koenig, J.Q.; Smith, K.R. Woodsmoke health effects: A review. Inhal. Toxicol. 2007, 19, 67–106. [Google Scholar] [CrossRef] [PubMed]
- Boman, B.C.; Forsberg, A.B.; Järvholm, B.G. Adverse health effects from ambient air pollution in relation to residential wood combustion in modern society. Scand. J. Work Environ. Health 2003, 29, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Organisation Mondiale de la Sant. Review of Evidence on Health Aspects of Air Pollution—Revihaap Project Technical Report; Organisation Mondiale de la Sant: Copenhague, Danemark, 2013; pp. 1–302. [Google Scholar]




| Characteristics | Value | Source |
|---|---|---|
| Number of municipalities | 41 | Plan de protection de l’atmosphère |
| Total area | 1224 km2 | Insee (2013) |
| Area classified as natural space | 1016 km2 | Insee (2013) |
| Population | 154,718 inhabitants | Insee (2012–2013) |
| Population aged 30 years and over | 97,937 inhabitants | Insee (2012–2013) |
| All-cause mortality rate (30 years and over) | 1030 deaths per 100,000 inhabitants | CépiDC (2012–2013) |
| Life expectancy at 30 | 53 years | Average for all municipalities (2012–2013) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pascal, M.; Yvon, J.-M.; Corso, M.; Blanchard, M.; De Crouy-Chanel, P.; Medina, S. Conditions for a Meaningful Health Impact Assessment for Local Stakeholders: The Example of the Arve Valley in France. Atmosphere 2020, 11, 566. https://doi.org/10.3390/atmos11060566
Pascal M, Yvon J-M, Corso M, Blanchard M, De Crouy-Chanel P, Medina S. Conditions for a Meaningful Health Impact Assessment for Local Stakeholders: The Example of the Arve Valley in France. Atmosphere. 2020; 11(6):566. https://doi.org/10.3390/atmos11060566
Chicago/Turabian StylePascal, Mathilde, Jean-Marc Yvon, Magali Corso, Myriam Blanchard, Perrine De Crouy-Chanel, and Sylvia Medina. 2020. "Conditions for a Meaningful Health Impact Assessment for Local Stakeholders: The Example of the Arve Valley in France" Atmosphere 11, no. 6: 566. https://doi.org/10.3390/atmos11060566
APA StylePascal, M., Yvon, J.-M., Corso, M., Blanchard, M., De Crouy-Chanel, P., & Medina, S. (2020). Conditions for a Meaningful Health Impact Assessment for Local Stakeholders: The Example of the Arve Valley in France. Atmosphere, 11(6), 566. https://doi.org/10.3390/atmos11060566




