Effects of Meteorological Factors on Asthma Hospital Visits in Haikou City, China
Abstract
:1. Introduction
2. Materials and Methods
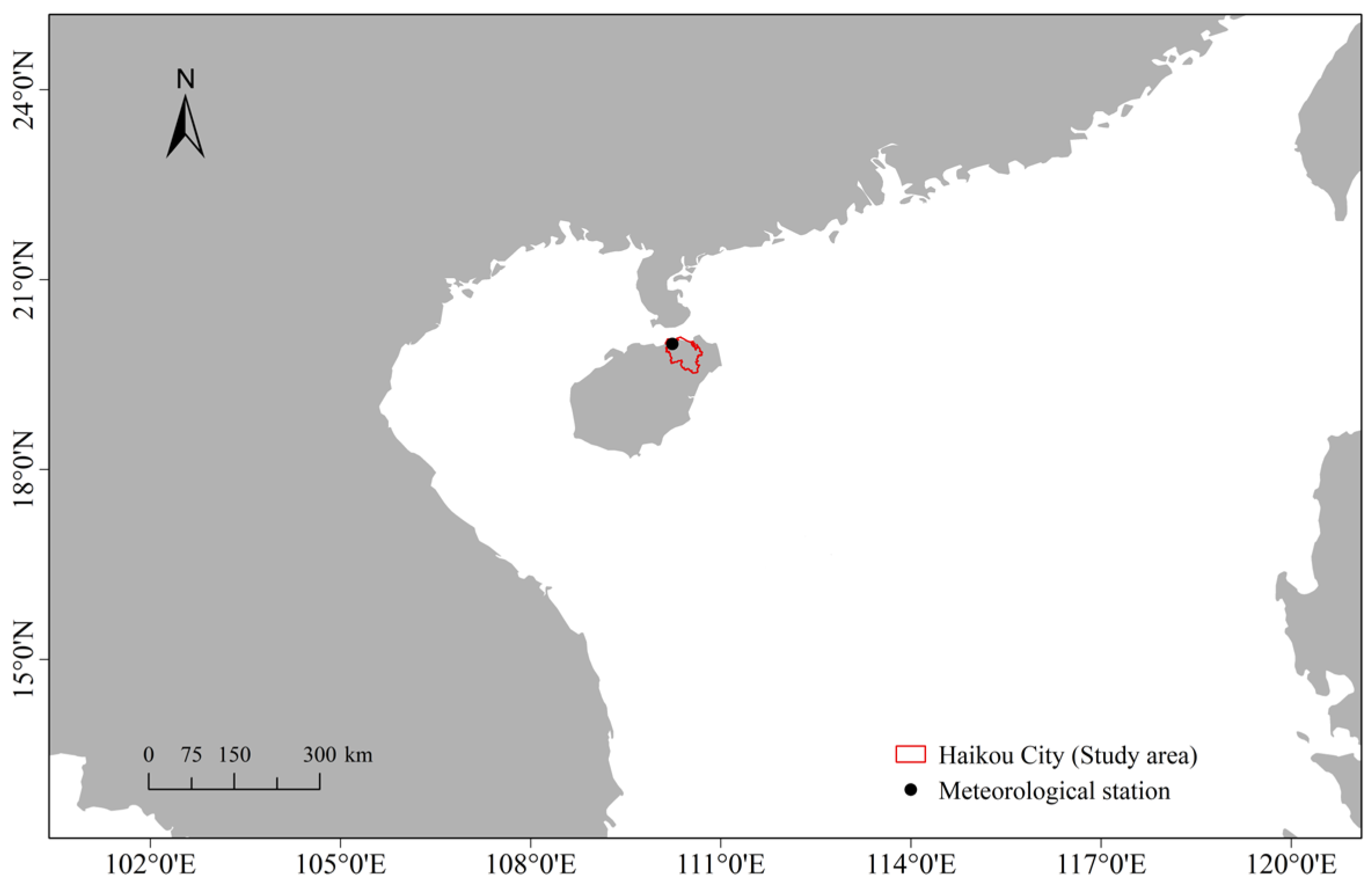
2.1. Study Area and Data Collection
2.2. Statistical Analysis
3. Results
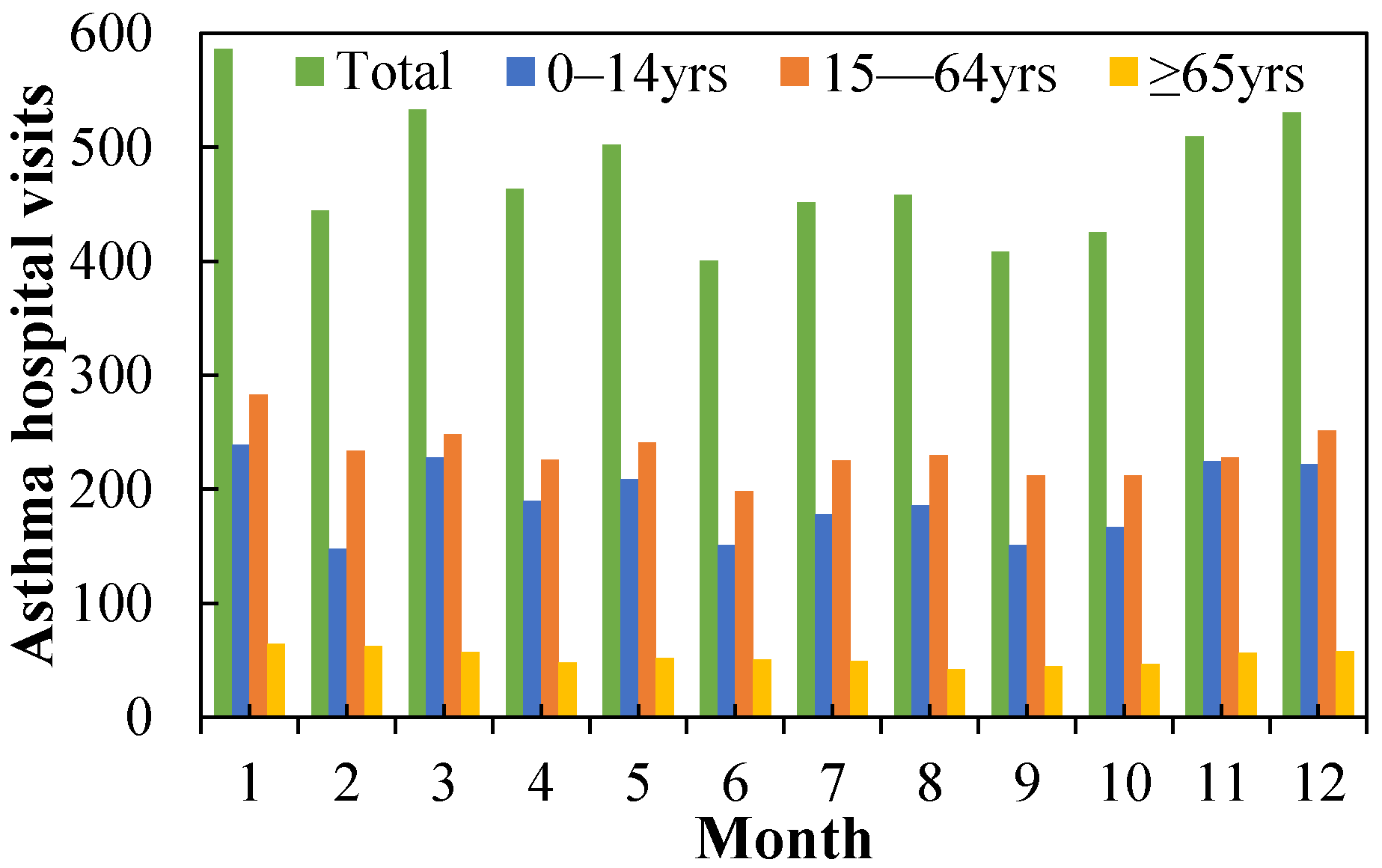
3.1. Descriptive Statistical Analysis
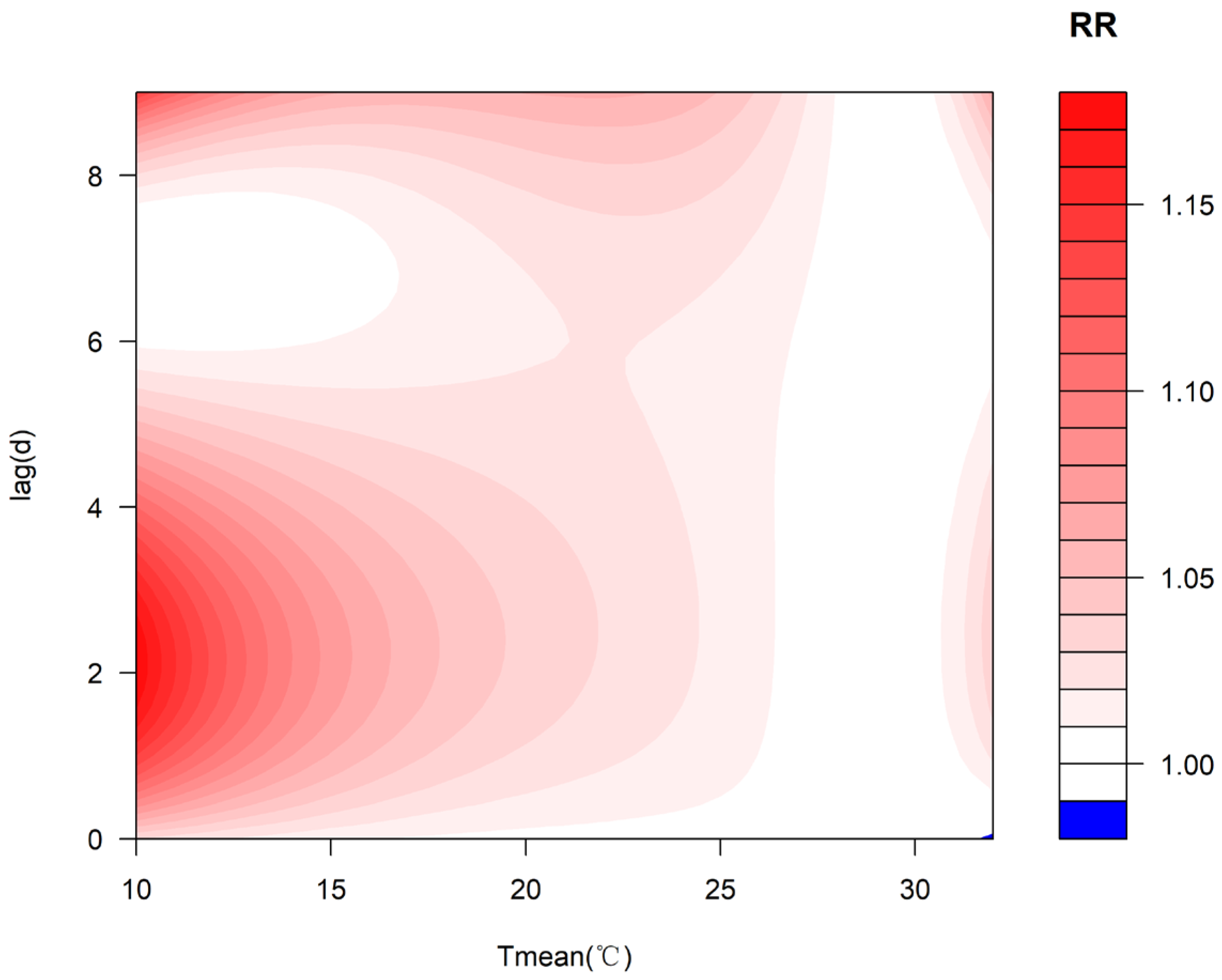
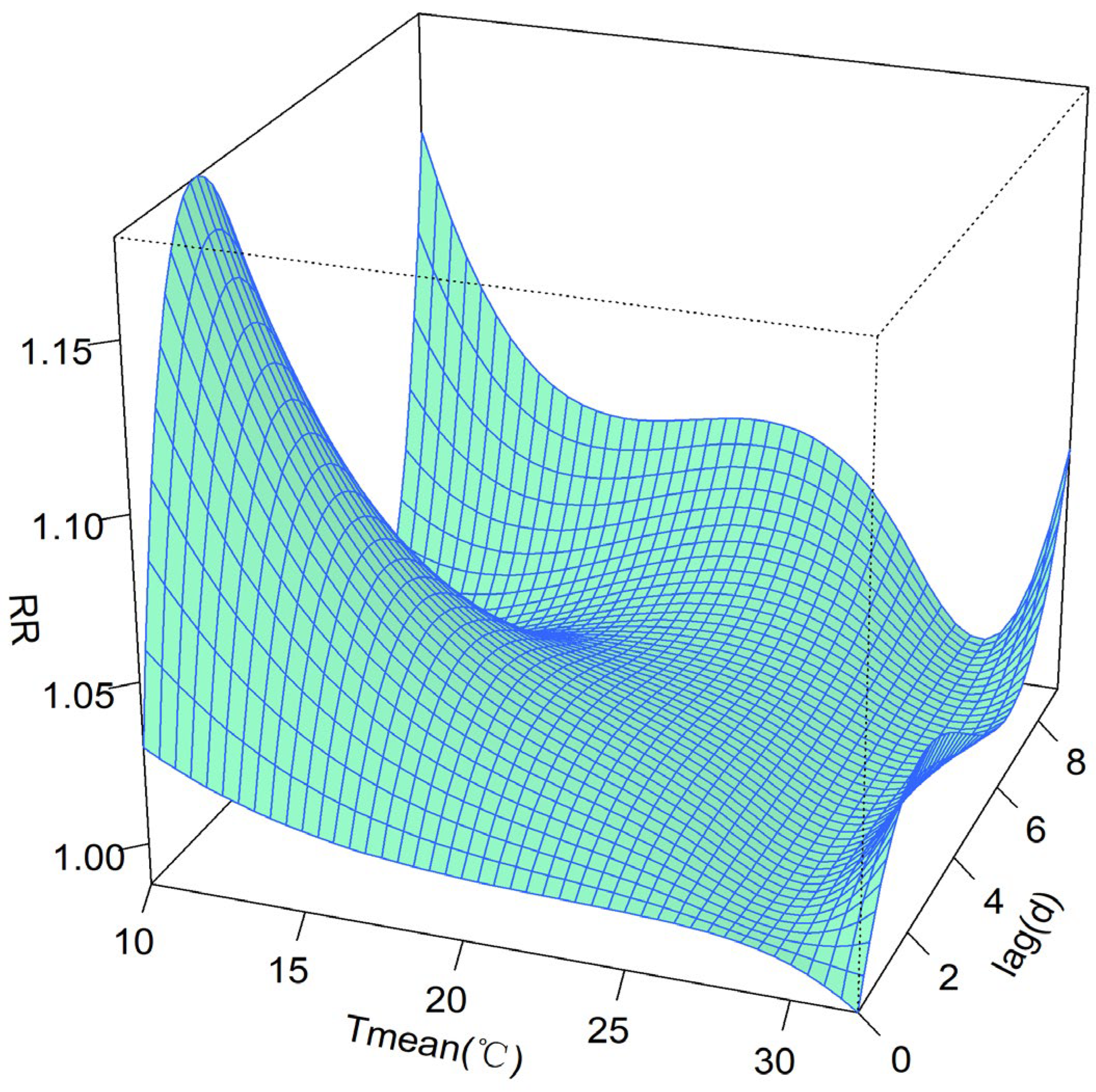
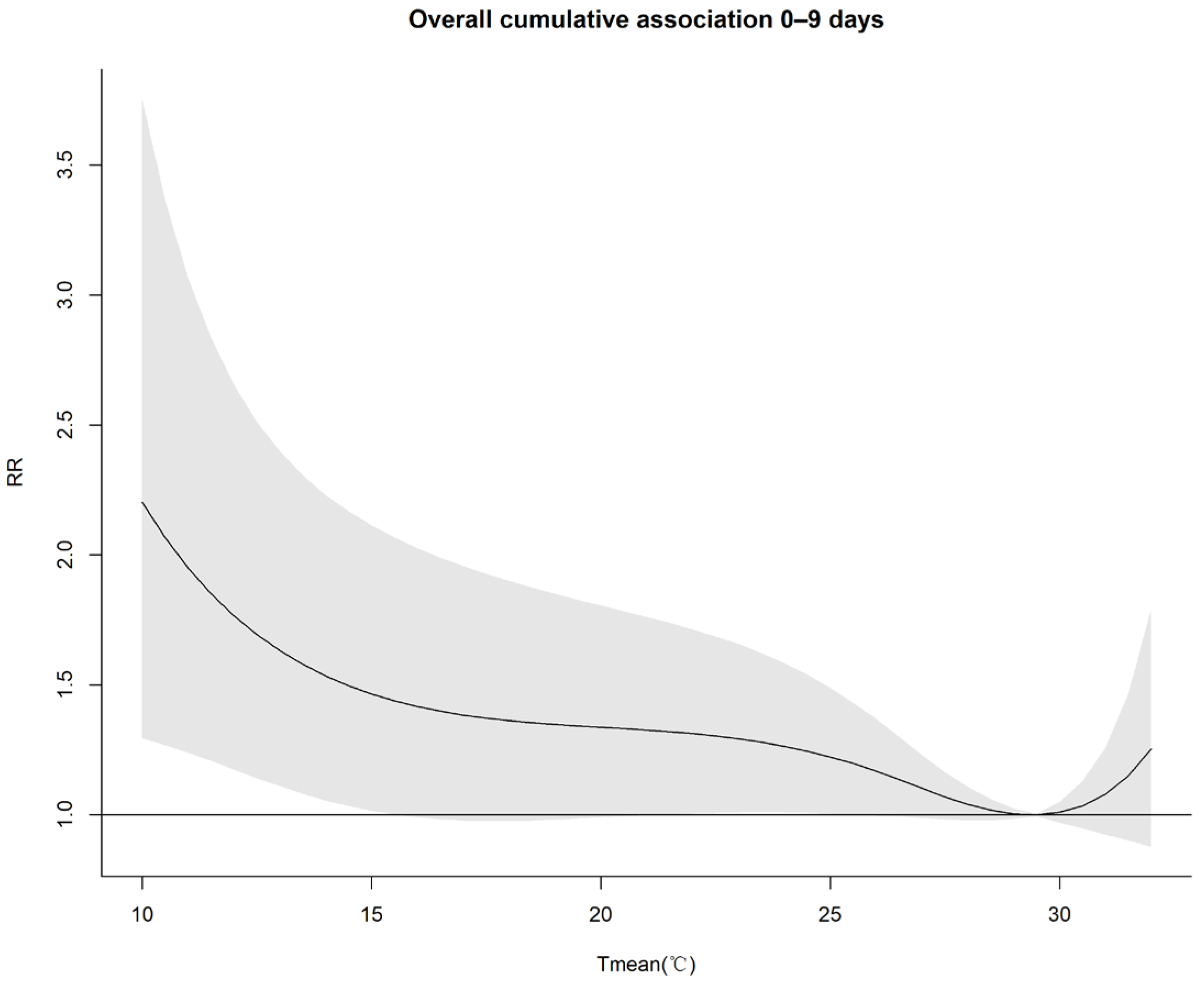
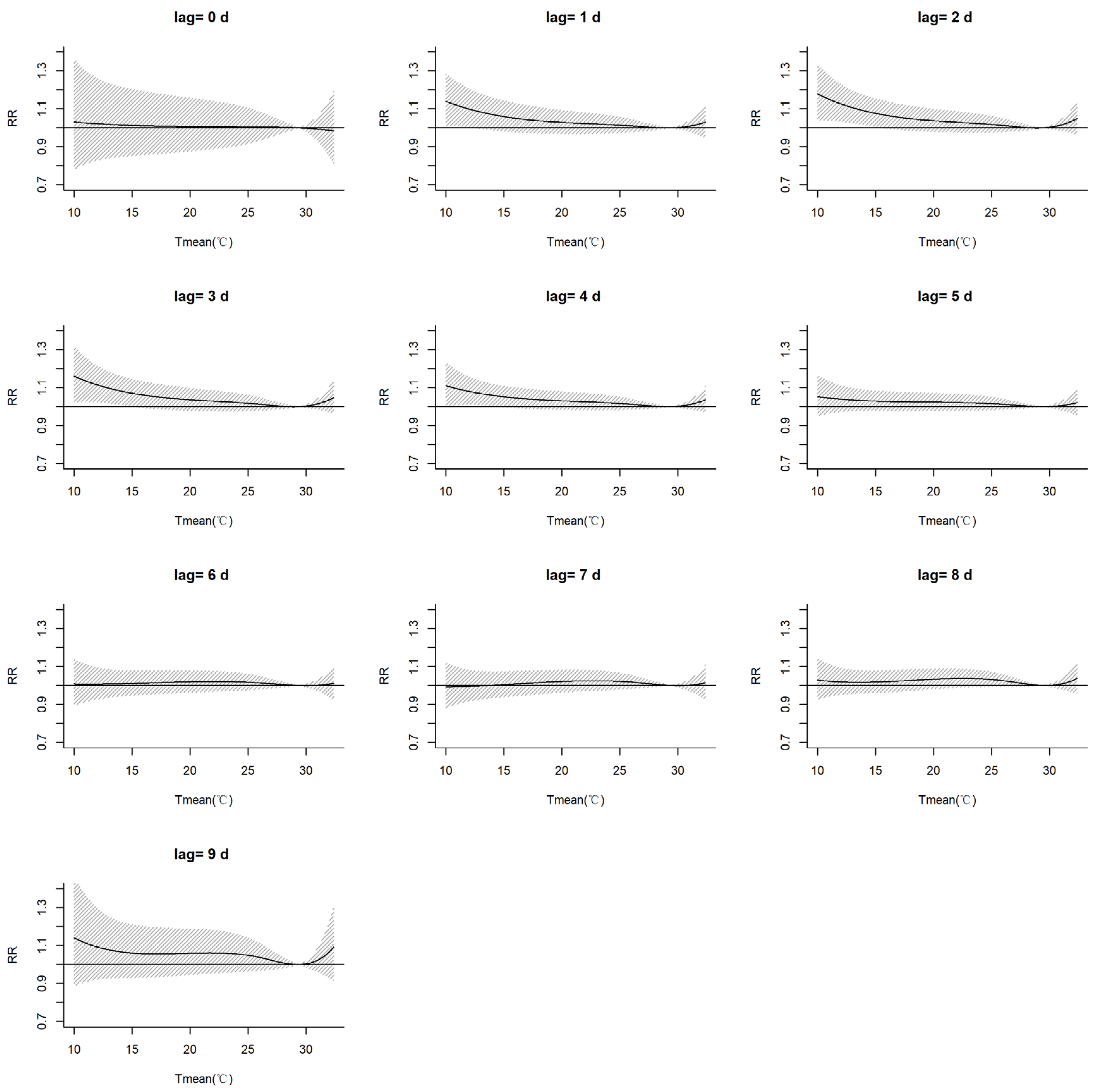
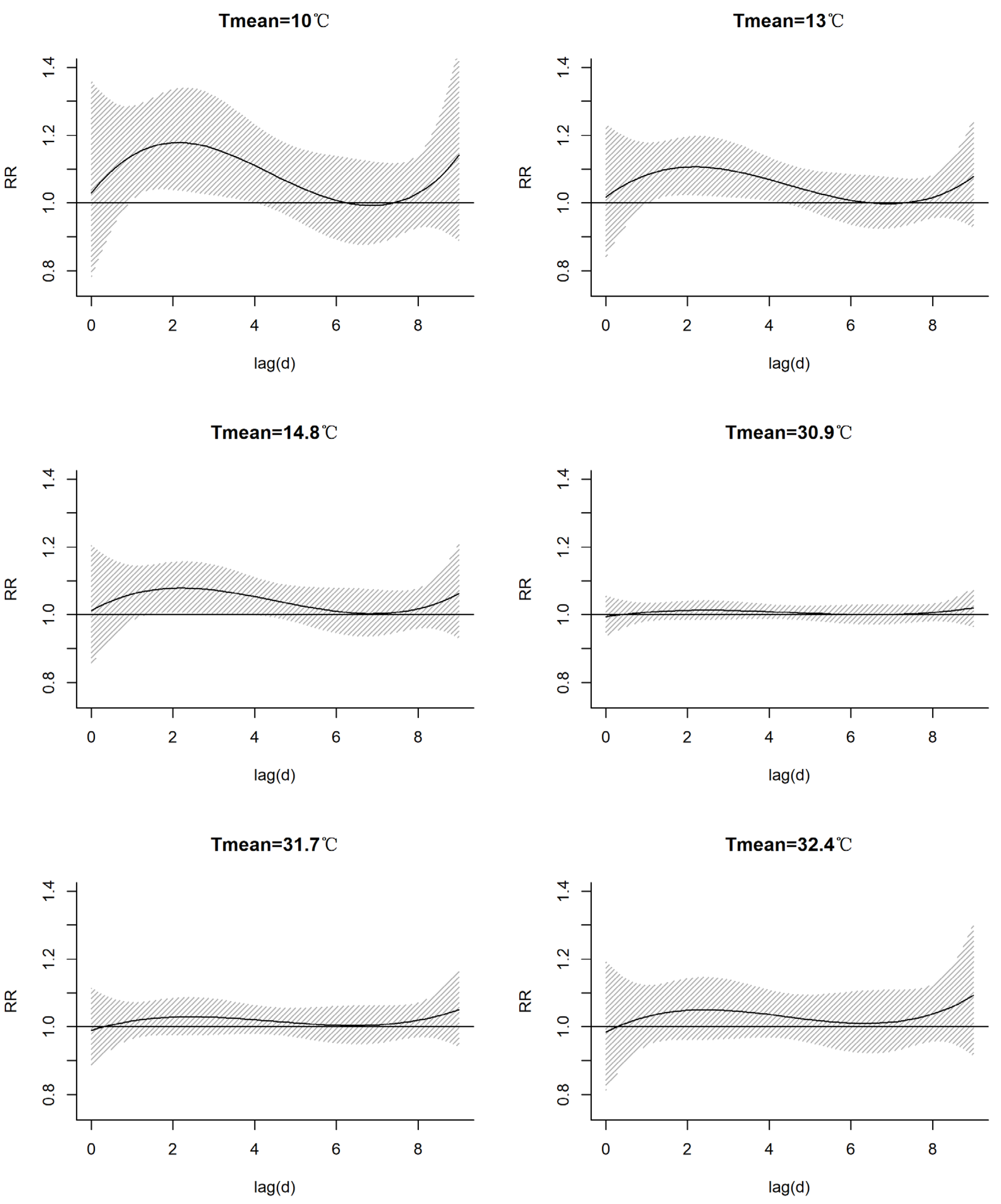
3.2. Exposure–Response Relationship between Temperature and Asthma Hospital Visits
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Global lnitiative for Asthma. Global Strategy for Asthma Management and Prevention. 2023. Available online: www.ginasthma.org (accessed on 23 June 2023).
- Hu, Y.; Cheng, J.; Jiang, F.; Liu, S.; Li, S.; Tan, J.; Yin, Y.; Tong, S. Season-stratified effects of meteorological factors on childhood asthma in Shanghai, China. Environ. Res. 2020, 191, 110115. [Google Scholar] [CrossRef]
- Asher, I.; Pearce, N. Global burden of asthma among children. Int. J. Tuberc. Lung Dis. 2014, 18, 1269–1278. [Google Scholar] [CrossRef]
- The National Cooperative Groupon Childhood Asthma; Institute of Environmental Health and Related Product Safety; Chinese Center for Disease Control and Prevention. Third nationwide survey of childhood asthma in urban areas of China. Chin. J. Pediatr. 2013, 51, 729–735. [Google Scholar] [CrossRef]
- Huang, K.; Yang, T.; Xu, J.; Yang, L.; Zhao, J.; Zhang, X.; Bai, C.; Kang, J.; Ran, P.; Shen, H.; et al. Prevalence, risk factors, and management of asthma in China: A national cross-sectional study. Lancet 2019, 394, 407–418. [Google Scholar] [CrossRef] [PubMed]
- The National Cooperative Groupon Childhood Asthma. A nationwide survey in China on prevalence of asthma in urban children. Chin. J. Pediatr. 2003, 41, 123–127. [Google Scholar]
- Newell, G.R., Jr.; Swafford, L.I. Epidemiology of asthma in children with particular reference to wind speed and wind direction. Pediatrics 1963, 31, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Carey, M.J.; Cordon, I. Asthma and climatic conditions: Experience from Bermuda, an isolated island community. Br. Med. J. 1986, 293, 843–844. [Google Scholar] [CrossRef] [PubMed]
- Rossi, O.V.; Kinnula, V.L.; Tienari, J.; Huhti, E. Association of severe asthma attacks with weather, pollen, and air pollutants. Thorax 1993, 48, 244–248. [Google Scholar] [CrossRef] [PubMed]
- Qasem, J.A.; Nasrallah, H.; Al-Khalaf, B.N.; Al-Sharifi, F.; Al-Sherafyee, A.; Almathkouri, S.A.; Al-Saraf, H. Meteorological factors, aeroallergens and asthma-related visits in Kuwait: A 12-month retrospective study. Ann. Saudi Med. 2008, 28, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Huang, C.; Hu, W.; Turner, L.R.; Su, H.; Tong, S. Extreme temperatures and emergency department admissions for childhood asthma in Brisbane, Australia. Occup. Environ. Med. 2013, 70, 730–735. [Google Scholar] [CrossRef] [PubMed]
- Jayawardene, W.P.; YoussefAgha, A.H.; Lohrmann, D.K.; El Afandi, G.S. Prediction of asthma exacerbations among children through integrating air pollution, upper atmosphere, and school health surveillances. Allergy Asthma Proc. 2013, 34, 1–8. [Google Scholar] [CrossRef]
- Zhang, Y.; Peng, L.; Kan, H.; Xu, J.; Chen, R.; Liu, Y.; Wang, W. Effects of meteorological factors on daily hospital admissions for asthma in adults: A time-series analysis. PLoS ONE 2014, 9, e102475. [Google Scholar] [CrossRef]
- Hervás, D.; Utrera, J.; Hervás-Masip, J.; Hervás, J.; García-Marcos, L. Can meteorological factors forecast asthma exacerbation in a paediatric population? Allergol. Immunopathol. 2015, 43, 32–36. [Google Scholar] [CrossRef]
- Da Silva, I.R.; Nedel, A.S.; Marques, J.R.Q.; Júnior, L.R.N. Excess of children’s outpatient consultations due to asthma and bronchitis and the association between meteorological variables in Canoas City, Southern Brazil. Int. J. Biometeorol. 2019, 63, 1517–1524. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Xu, Z.; Jiang, F.; Li, S.; Liu, S.; Wu, M.; Yan, C.; Tan, J.; Yu, G.; Hu, Y.; et al. Relative impact of meteorological factors and air pollutants on childhood allergic diseases in Shanghai, China. Sci. Total. Environ. 2019, 706, 135975. [Google Scholar] [CrossRef] [PubMed]
- Yousif, M.K.; Al Muhyi, A.-H.A. Impact of weather conditions on childhood admission for wheezy chest and bronchial asthma. Med. J. Islam. Repub. Iran. 2019, 33, 89. [Google Scholar]
- Zhao, Y.; Huang, Z.; Wang, S.; Hu, J.; Xiao, J.; Li, X.; Liu, T.; Zeng, W.; Guo, L.; Du, Q.; et al. Morbidity burden of respiratory diseases attributable to ambient temperature: A case study in a subtropical city in China. Environ. Health 2019, 18, 89. [Google Scholar] [CrossRef]
- Tikkakoski, A.P.; Tikkakoski, A.; Kivistö, J.E.; Huhtala, H.; Sipilä, K.; Karjalainen, J.; Kähönen, M.; Lehtimäki, L. Association of air humidity with incidence of exercise-induced bronchoconstriction in children. Pediatr. Pulmonol. 2019, 54, 1830–1836. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Liu, S.; Chen, Z.; Zu, B.; Zhao, Y. Effects of variations in meteorological factors on daily hospital visits for asthma: A time-series study. Environ. Res. 2020, 182, 109115. [Google Scholar] [CrossRef] [PubMed]
- Romaszko-Wojtowicz, A.; Cymes, I.; Dragańska, E.; Doboszyńska, A.; Romaszko, J.; Glińska-Lewczuk, K. Relationship between biometeorological factors and the number of hospitalizations due to asthma. Sci. Rep. 2020, 10, 9593. [Google Scholar] [CrossRef] [PubMed]
- Pan, R.; Wang, X.; Yi, W.; Wei, Q.; Gao, J.; Xu, Z.; Duan, J.; He, Y.; Tang, C.; Liu, X.; et al. Interactions between climate factors and air quality index for improved childhood asthma self-management. Sci. Total. Environ. 2020, 723, 137804. [Google Scholar] [CrossRef]
- Wei, Q.; Zhong, L.; Gao, J.; Yi, W.; Pan, R.; Gao, J.; Duan, J.; Xu, Z.; He, Y.; Liu, X.; et al. Diurnal temperature range and childhood asthma in Hefei, China: Does temperature modify the association? Sci. Total. Environ. 2020, 724, 138206. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; He, Y.; Tang, C.; Wei, Q.; Xu, Z.; Yi, W.; Pan, R.; Gao, J.; Duan, J.; Su, H. Association between cold spells and childhood asthma in Hefei, an analysis based on different definitions and characteristics. Environ. Res. 2021, 195, 110738. [Google Scholar] [CrossRef] [PubMed]
- Lei, X.; Liu, L.; Chen, R.; Liu, C.; Hong, J.; Cao, L.; Lu, Y.; Dong, X.; Chen, X.; Qiu, X.; et al. Temperature changes between neighboring days and childhood asthma: A seasonal analysis in Shanghai, China. Int. J. Biometeorol. 2021, 65, 827–836. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Yang, T.; Huang, S.; Li, H.; Lei, J.; Xue, X.; Gao, Y.; Jiang, Y.; Liu, C.; Kan, H.; et al. Cold temperature and sudden temperature drop as novel risk factors of asthma exacerbation: A longitudinal study in 18 Chinese cities. Sci. Total. Environ. 2022, 814, 151959. [Google Scholar] [CrossRef] [PubMed]
- Deng, S.; Han, A.; Jin, S.; Wang, S.; Zheng, J.; Jalaludin, B.B.; Hajat, S.; Liang, W.; Huang, C. Effect of extreme temperatures on asthma hospital visits: Modification by event characteristics and healthy behaviors. Environ. Res. 2023, 226, 115679. [Google Scholar] [CrossRef] [PubMed]
- D’amato, G.; Vitale, C.; De Martino, A.; Viegi, G.; Lanza, M.; Molino, A.; Sanduzzi, A.; Vatrella, A.; Annesi-Maesano, I.; D’amato, M. Effects on asthma and respiratory allergy of Climate change and air pollution. Multidiscip. Respir. Med. 2015, 10, 39. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.-Y.; Ding, H.; Jiang, L.-N.; Chen, S.-W.; Zheng, J.-P.; Qiu, M.; Zhou, Y.-X.; Chen, Q.; Guan, W.-J. Association between Air Pollutants and Asthma Emergency Room Visits and Hospital Admissions in Time Series Studies: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0138146. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Glonek, G.; Hansen, A.; Williams, S.; Tuke, J.; Salter, A.; Bi, P. The effects of air pollution on asthma hospital admissions in Adelaide, South Australia, 2003–2013: Time-series and case–crossover analyses. Clin. Exp. Allergy 2016, 46, 1416–1430. [Google Scholar] [CrossRef]
- Orellano, P.; Quaranta, N.; Reynoso, J.; Balbi, B.; Vasquez, J. Effect of outdoor air pollution on asthma exacerbations in children and adults: Systematic review and multilevel meta-analysis. PLoS ONE 2017, 12, e0174050. [Google Scholar] [CrossRef]
- Klabuschnig, A.; Göiz, M.; Horak, F.; Jäger, S.; Machalek, A.; Popow, C.; Haschke, F.; Skoda-Türk, R. Influence of aerobiology and weather on symptoms in children with asthma. Respiration 1981, 42, 52–60. [Google Scholar] [CrossRef]
- Erbas, B.; Akram, M.; Dharmage, S.C.; Tham, R.; Dennekamp, M.; Newbigin, E.; Taylor, P.; Tang, M.L.K.; Abramson, M.J. The role of seasonal grass pollen on childhood asthma emergency department presentations. Clin. Exp. Allergy 2012, 42, 799–805. [Google Scholar] [CrossRef]
- Johnston, N.W. Asthma exacerbations. 1: Epidemiology. Thorax 2006, 61, 722–728. [Google Scholar] [CrossRef] [PubMed]
- Erbas, B.; Dharmage, S.C.; Tang, M.L.; Akram, M.; Allen, K.J.; Vicendese, D.; Davies, J.M.; Hyndman, R.J.; Newbigin, E.J.; Taylor, P.E.; et al. Do human rhinovirus infections and food allergy modify grass pollen–induced asthma hospital admissions in children? J. Allergy Clin. Immunol. 2015, 136, 1118–1120.e2. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.; Yu, I.T.-S.; Tse, L.A.; Chan, E.Y.; Wong, T.W.; Tian, L. Greater temperature variation within a day associated with increased emergency hospital admissions for asthma. Sci. Total. Environ. 2015, 505, 508–513. [Google Scholar] [CrossRef] [PubMed]
- Lam, H.C.-Y.; Li, A.M.; Chan, E.Y.-Y.; Goggins, W.B. The short-term association between asthma hospitalisations, ambient temperature, other meteorological factors and air pollutants in Hong Kong: A time-series study. Thorax 2016, 71, 1097–1109. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Crooks, J.L.; Davies, J.M.; Khan, A.F.; Hu, W.; Tong, S. The association between ambient temperature and childhood asthma: A systematic review. Int. J. Biometeorol. 2018, 62, 471–481. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Distributed lag non-linear models. Stat. Med. 2010, 29, 2224–2234. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A. Distributed Lag Linear and Non-Linear Models in R: The Package DLNM. J. Stat. Softw. 2011, 43, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Jiang, F.; Peng, L.; Zhang, J.; Geng, F.; Xu, J.; Zhen, C.; Shen, X.; Tong, S. The Association between Cold Spells and Pediatric Outpatient Visits for Asthma in Shanghai, China. PLoS ONE 2012, 7, e42232. [Google Scholar] [CrossRef]
- Son, J.-Y.; Bell, M.L.; Lee, J.-T. The impact of heat, cold, and heat waves on hospital admissions in eight cities in Korea. Int. J. Biometeorol. 2014, 58, 1893–1903. [Google Scholar] [CrossRef] [PubMed]
- Belachew, A.B.; Rantala, A.K.; Jaakkola, M.S.; Hugg, T.T.; Ruuhela, R.; Kukkonen, J.; Jaakkola, J.J.K. Effect of cold winters on the risk of new asthma: A case-crossover study in Finland. Occup. Environ. Med. 2023, 80, 702–705. [Google Scholar] [CrossRef] [PubMed]
- Fang, J.; Song, J.; Wu, R.; Xie, Y.; Xu, X.; Zeng, Y.; Zhu, Y.; Wang, T.; Yuan, N.; Xu, H.; et al. Association between ambient temperature and childhood respiratory hospital visits in Beijing, China: A time-series study (2013–2017). Environ. Sci. Pollut. Res. Int. 2021, 28, 29445–29454. [Google Scholar] [CrossRef]
- Konstantinoudis, G.; Minelli, C.; Lam, H.C.Y.; Fuertes, E.; Ballester, J.; Davies, B.; Vicedo-Cabrera, A.M.; Gasparrini, A.; Blangiardo, M. Asthma hospitalisations and heat exposure in England: A case–crossover study during 2002–2019. Thorax 2023, 78, 875–881. [Google Scholar] [CrossRef]
- O’lenick, C.R.; Winquist, A.; Chang, H.H.; Kramer, M.R.; Mulholland, J.A.; Grundstein, A.; Sarnat, S.E. Evaluation of individual and area-level factors as modifiers of the association between warm-season temperature and pediatric asthma morbidity in Atlanta, GA. Environ. Res. 2017, 156, 132–144. [Google Scholar] [CrossRef]
- Li, S.; Baker, P.J.; Jalaludin, B.B.; Guo, Y.; Marks, G.B.; Denison, L.S.; Williams, G.M. Are children׳s asthmatic symptoms related to ambient temperature? A panel study in Australia. Environ. Res. 2014, 133, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Lam, H.C.Y.; Hajat, S.; Chan, E.Y.Y.; Goggins, W.B. Different sensitivities to ambient temperature between first- and re-admission childhood asthma cases in Hong Kong—A time series study. Environ. Res. 2019, 170, 487–492. [Google Scholar] [CrossRef] [PubMed]
- Hayes, D., Jr.; Collins, P.B.; Khosravi, M.; Lin, R.-L.; Lee, L.-Y. Bronchoconstriction Triggered by Breathing Hot Humid Air in Patients with Asthma: Role of cholinergic reflex. Am. J. Respir. Crit. Care Med. 2012, 185, 1190–1196. [Google Scholar] [CrossRef]
- Intergovernmental Panel on Climate Change (IPCC). Climate Change 2021—The Physical Science Basis: Working Group I Contribution to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Cambridge University Press: Cambridge, UK, 2023; pp. 1517–1520. [Google Scholar] [CrossRef]
| Min. | 1st Qu. | Median | Mean | 3rd Qu. | Max. | Std. Dev. | |
|---|---|---|---|---|---|---|---|
| Meteorological factors | |||||||
| Prs | 984.9 | 999.2 | 1003.7 | 1003.9 | 1008.2 | 1019.6 | 6.2 |
| Pmax | 989.7 | 1001 | 1005.9 | 1005.9 | 1010.4 | 1022 | 6.4 |
| Pmin | 980 | 997 | 1002 | 1002.0 | 1006 | 1018 | 6.3 |
| Tmean | 10.0 | 22.1 | 26.2 | 25.1 | 28.3 | 32.4 | 4.3 |
| Tmax | 11.6 | 25.1 | 29.8 | 28.7 | 32.7 | 38.9 | 5.3 |
| Tmin | 7 | 20.2 | 23.8 | 22.6 | 25.5 | 28.8 | 3.9 |
| RH | 42 | 77 | 82 | 81.4 | 86.5 | 99 | 7.7 |
| R | 0 | 0 | 0 | 5.5 | 2 | 266.6 | 19.1 |
| WS | 0.7 | 2.3 | 2.8 | 2.9 | 3.4 | 10.4 | 0.9 |
| Air pollutants | |||||||
| AQI | 13 | 29 | 37 | 41.2 | 48.5 | 150 | 18.4 |
| PM2.5 | 4 | 11 | 15 | 18.2 | 22 | 73 | 11.1 |
| PM10 | 8 | 23 | 30 | 34.0 | 42 | 109 | 15.5 |
| SO2 | 3 | 4 | 5 | 5.6 | 6 | 16 | 1.9 |
| NO2 | 3 | 9 | 12 | 12.6 | 15 | 39 | 4.7 |
| CO | 0.3 | 0.5 | 0.6 | 0.6 | 0.7 | 1.2 | 0.1 |
| O3 | 0 | 51 | 68 | 72.7 | 88.5 | 215 | 30.6 |
| Daily asthma hospital visits | |||||||
| Total | 0 | 8.5 | 15 | 15.7 | 21 | 45 | 9.4 |
| 0–14 yrs | 0 | 1 | 4 | 6.3 | 10 | 27 | 6.4 |
| 15–64 yrs | 0 | 4 | 7 | 7.6 | 11 | 26 | 4.6 |
| ≥65 yrs | 0 | 0 | 1 | 1.7 | 3 | 10 | 1.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Yang, J.; Chen, S.; Zhang, M.; Zhang, J. Effects of Meteorological Factors on Asthma Hospital Visits in Haikou City, China. Atmosphere 2024, 15, 328. https://doi.org/10.3390/atmos15030328
Zhang Y, Yang J, Chen S, Zhang M, Zhang J. Effects of Meteorological Factors on Asthma Hospital Visits in Haikou City, China. Atmosphere. 2024; 15(3):328. https://doi.org/10.3390/atmos15030328
Chicago/Turabian StyleZhang, Yajie, Jing Yang, Shengbei Chen, Mingjie Zhang, and Jinghong Zhang. 2024. "Effects of Meteorological Factors on Asthma Hospital Visits in Haikou City, China" Atmosphere 15, no. 3: 328. https://doi.org/10.3390/atmos15030328




