Functional Symmetry after Surgical Treatment of Pertrochanteric Fractures in the Elderly
Abstract
:1. Introduction
- quantify and draw inferences on observed differences in parameters related to hospital stay and surgery (length of a hospital stay, surgery duration),
- quantify and draw inferences on observed differences in functional status at three and six months,
- quantify and draw inferences on observed differences in health-related quality of life (HRQoL) at three and six months between the study intervention groups,
- quantify and draw inferences on observed differences in the symmetry assessment in selected parameters based on the X-rays.
2. Materials and Methods
2.1. Subjects
2.1.1. Comorbidities
2.1.2. Procedures Performed
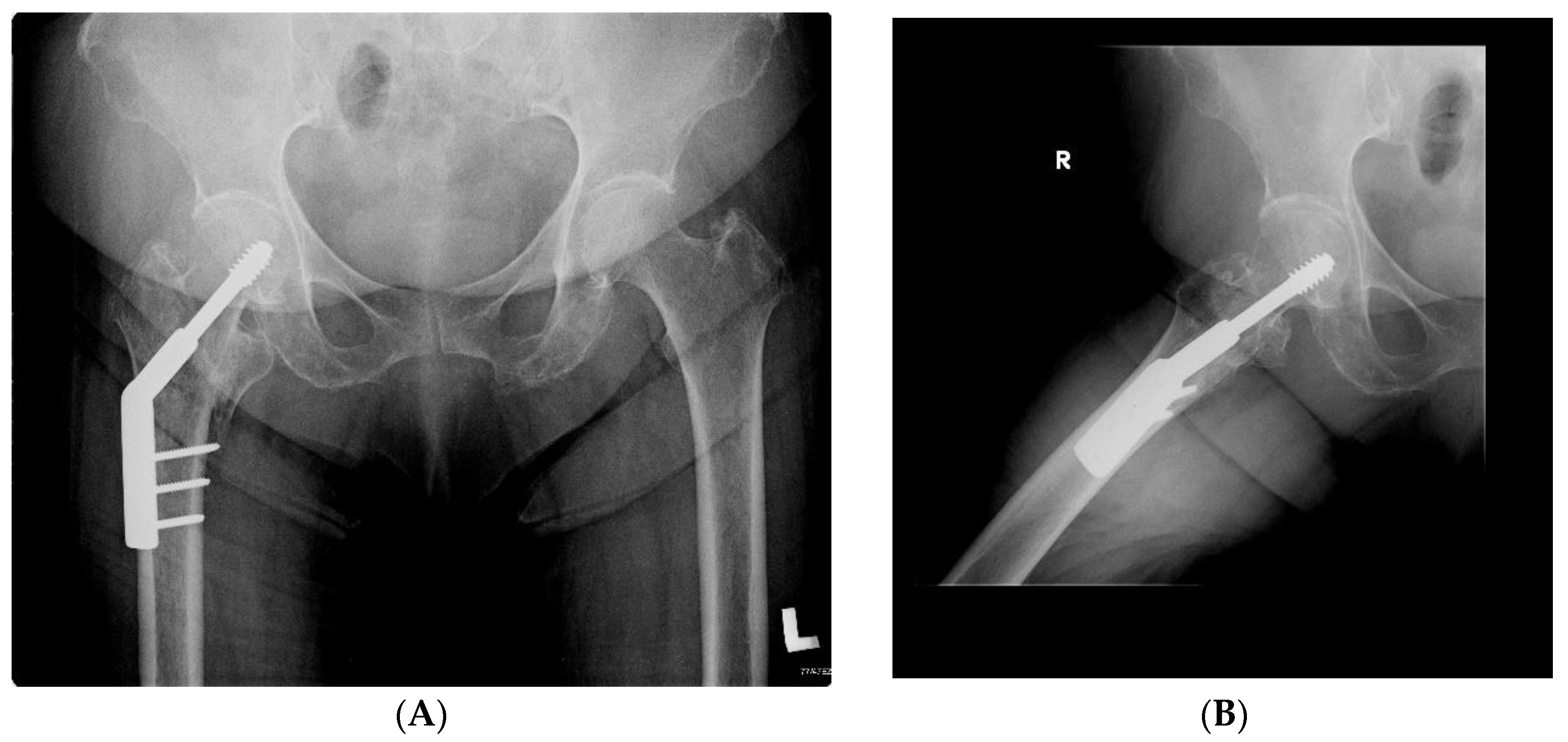
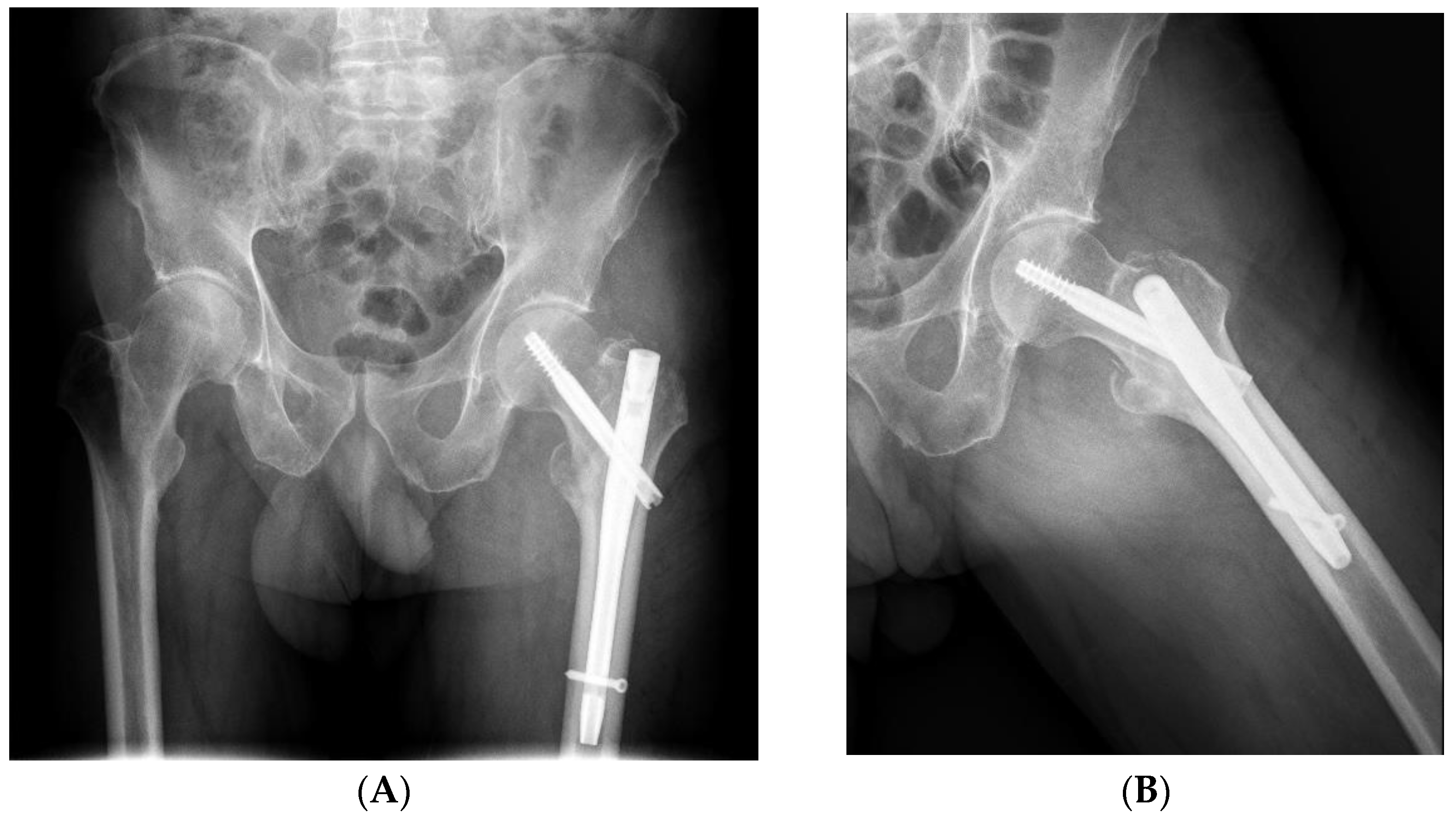
2.1.3. Types of Surgical Fixation
2.1.4. Study Group
2.2. Inclusion Criteria
- -
- Patients admitted for a hospital stay in the department of orthopaedics and traumatology of the motor organ in the period from 1 January 2015 to 31 December 2019 with the primary diagnosis of pertrochanteric fracture;
- -
- patients who underwent fixation of pertrochanteric fracture, performed by one/the same operator (operating surgeon—consultant);
- -
- type of fixation used: DHS screw plate or intramedullary Gamma nail;
- -
- type of fracture according to AO classification—A1, A2, A3;
- -
- aged 65+;
- -
- a minimum post-operative follow-up of six months.
2.3. Exclusion Criteria
- -
- Patients who had a poor outcome due to comorbidities, who did not report to outpatient control;
- -
- a different type of fracture fixation was used;
- -
- multi-site musculoskeletal injuries;
- -
- pathological fracture (excluding osteoporosis).
2.4. Symmetry in the Length of Hospital Stay and Surgery Duration
- The length of hospital stay following the day of surgery admission (including the day of surgery)—days;
- The duration of the hospital stay after surgery (days);
- The duration of surgery (from anasthesia, including positioning and repositioning of the patient of the operating table)—min.
2.5. Functional Symmetry
2.6. Radiographic Analysis
- fracture union (full union vs. non-union present);
- symmetry of the neck-shaft angle (NSA)—operated femur and its opposite side (assessment for the presence of valgus or varus position);
- symmetry of the position of the neck screw in relation to the axis of the femoral neck (screw located on the axis or below the axis vs. located above the axis);
- the axis of the intramedullary nail in relation to the axis of the femur (evaluated in the anterior–posterior view: varus position—the distal part of the nail resting on the medial cortex; axial position—the axis of the nail coincides with the axis of the femoral shaft; valgus position—the distal part of the nail resting on the cortex layer of the femur on the lateral side);
- the minimum distance between the tip of the neck screw and the articular surface of the femoral head (arithmetic mean of the distance measured in the anterior–posterior and axial projection);
- the fracture/detachment of the lesser trochanter (X-ray of the hip after injury, before surgery);
- symmetry of the length of the operated limb (the difference in the height of the lesser trochanter position) shortening by >1 cm.
2.7. Statistical Analysis
3. Results
3.1. Symmetry in the Length of Hospital Stay and Surgery Duration
- In the DHS group: (31A1—eight cases, 31A2—28 cases);
- In the Gamma group: (31A1—five cases, 31A2—30 cases, 31A3—seven cases).
3.2. Symmetry in Functional Outcomes
3.3. Symmetry in Quality of Life
3.4. Symmetry/Assymetry in Radiographic Analysis
- DHS group: in 33 patients, the screw was located on the axis or below; in three patients, the screw was located above the axis,
- Gamma group: in 38 patients, the screw was located on the axis or below; in four patients, the screw was located above the axis.
4. Discussion
5. Conclusions
- There was a functional symmetry between the outcomes of surgical treatment of PFs in people treated with the dynamic hip screw and intramedullary gamma nail.
- There were no significant asymmetries in parameters regarding hospital stay and surgery between the DHS group and Gamma group.
- There were no significant asymmetries in parameters regarding functional status (motor function examined by assessing the performance of specific motor tasks), perceived pain, and quality of life at three and six months after surgery in both groups.
- There were no significant asymmetries in the radiographic image of the hip after the surgery of the pertrochanteric fracture and the hip on the opposite side.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Filipov, O. Epidemiology and social burden of the femoral neck fractures. J. IMAB 2014, 20, 516–518. [Google Scholar] [CrossRef] [Green Version]
- Gawrońska, K.; Lorkowski, J. Falls, Aging and Public Health—A Literature Review. Ortop. Traumatol. Rehabil. 2020, 22, 397–408. [Google Scholar] [CrossRef] [PubMed]
- Gawronska, K.; Lorkowski, J. Falls as One of the Atypical Presentations of COVID-19 in Older Population. Geriatr. Orthop. Surg. Rehabil. 2021, 12, 2151459321996619. [Google Scholar] [CrossRef] [PubMed]
- Anandasivam, N.S.; Russo, G.S.; Fischer, J.M.; Samuel, A.M.; Ondeck, N.T.; Swallow, M.S.; Chung, S.H.; Bohl, D.D.; Grauer, J.N. Analysis of Bony and Internal Organ Injuries Associated with 26,357 Adult Femoral Shaft Fractures and Their Impact on Mortality. Orthopedics 2017, 40, e506–e512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valentini, R.; Martino, M.; Piovan, G.; De Fabrizio, G.; Fancellu, G. Proximal cut-out in pertrochanteric femural fracture. Acta Biomed. 2014, 85, 144–151. [Google Scholar]
- Xu, B.Y.; Yan, S.; Low, L.L.; Vasanwala, F.F.; Low, S.G. Predictors of poor functional outcomes and mortality in patients with hip fracture: A systematic review. BMC Musculoskelet. Disord. 2019, 20, 568. [Google Scholar] [CrossRef]
- Huttunen, T.T.; Kannus, P.; Pihlajamäki, H.; Mattila, V.M. Pertrochanteric fracture of the femur in the Finnish National Hospital Discharge Register: Validity of procedural coding, external cause for injury and diagnosis. BMC Musculoskelet. Disord. 2014, 15, 98. [Google Scholar] [CrossRef] [Green Version]
- Deleanu, B.; Prejbeanu, R.; Tsiridis, E.; Vermesan, D.; Crisan, D.; Haragus, H.; Predescu, V.; Birsasteanu, F. Occult fractures of the proximal femur: Imaging diagnosis and management of 82 cases in a regional trauma center. World J. Emerg. Surg. 2015, 10, 55. [Google Scholar] [CrossRef] [Green Version]
- Meinberg, E.G.; Agel, J.; Roberts, C.S.; Karam, M.D.; Kellam, J.F. Fracture and Dislocation Classification Compendium. J. Ortopeda Trauma 2018, 32, S1–S170. [Google Scholar] [CrossRef]
- Young, L.; Uppal, H.S. Hip Fractures: Relevant Anatomy, Classification, and Biomechanics of Fracture and Fixation. Geriatr. Orthop. Surg. Rehabil. 2019, 10. [Google Scholar] [CrossRef] [Green Version]
- Saul, D.; Riekenberg, J.; Ammon, J.C.; Hoffmann, D.B.; Sehmisch, S. Hip Fractures: Therapy, Timing, and Complication Spectrum. Orthop. Surg. 2019, 11, 994–1002. [Google Scholar] [CrossRef] [PubMed]
- Selim, A.; Ponugoti, N.; Zain Naqvi, A.; Magill, H. Cephalo-medullary nailing versus dynamic hip screw with trochanteric stabilisation plate for the treatment of unstable per-trochanteric hip fractures: A meta-analysis. J. Orthop. Surg. Res. 2021, 16, 47. [Google Scholar] [CrossRef] [PubMed]
- Catania, P.; Passaretti, D.; Montemurro, G.; Ripanti, S.; Carbone, S.; Candela, V.; Carnovale, M.; Gumina, S.; Pallotta, F. Intramedullary nailing for pertrochanteric fractures of proximal femur: A consecutive series of 323 patients treated with two devices. J. Orthop. Surg. Res. 2019, 14, 449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lorkowski, J.; Wilk, R.; Pokorski, M. In Silico Evaluation of Treatment of Periprosthet-ic Fractures in Elderly Patients After Hip Arthroplasty. Adv. Exp. Med. Biol. 2021, 1289, 115–123. [Google Scholar]
- Borgström, F.; Karlsson, L.; Ortsäter, G.; Norton, N.; Halbout, P.; Cooper, C.; Lorentzon, M.; McCloskey, E.V.; Harvey, N.C.; Javaid, M.; et al. International Osteoporosis Foundation. Fragility fractures in Europe: Burden, management and opportunities. Arch. Osteoporos. 2020, 15, 59. [Google Scholar] [CrossRef] [Green Version]
- Sambrook, P.; Cooper, C. Osteoporosis. Lancet 2006, 367, 2010–2018, Erratum in Lancet 2006, 368, 28. [Google Scholar] [CrossRef]
- Khow, K.S.F.; Visvanathan, R. Falls In the Aging Population. Clin. Geriatr. Med. 2017, 33, 357–368. [Google Scholar] [CrossRef]
- Pascarella, R.; Fantasia, R.; Maresca, A.; Bettuzzi, C.; Amendola, L.; Violini, S.; Cuoghi, F.; Sangiovanni, P.; Cerbasi, S.; Boriani, S.; et al. How evolution of the nailing system improves results and reduces orthopedic complications: More than 2000 cases of trochanteric fractures treated with the Gamma Nail System. Musculoskelet. Surg. 2016, 100. [Google Scholar] [CrossRef]
- Smith, J.R.; Halliday, R.; Aquilina, A.L.; Morrison, R.J.; Yip, G.C.; McArthur, J.; Hull, P.; Gray, A.; Kelly, M.B.; Orthopaedic Trauma Society (OTS). Distal femoral fractures: The need to review the standard of care. Injury 2015, 46, 1084–1088. [Google Scholar] [CrossRef]
- Butt, M.S.; Krikler, S.J.; Ali, M.S. Displaced fractures of the distal femur in elderly patients. Operative versus non-operative treatment. J. Bone Jt. Surg. Br. 1996, 78, 110–114. [Google Scholar] [CrossRef] [Green Version]
- Hadeed, A.; Werntz, R.L.; Varacallo, M. External Fixation Principles and Overview. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Andrianne, Y.; Hinsenkamp, M. Historical review of the treatment of fractures. Contribution of the Belgian surgery to the origin and development of osteosynthesis. Rev. Med. Brux. 2011, 32, S30–S37. [Google Scholar] [PubMed]
- Norris, B.L.; Lang, G.; Russell, T.A.T.; Rothberg, D.L.; Ricci, W.M.; Borrelli, J., Jr. Absolute Versus Relative Fracture Fixation: Impact on Fracture Healing. J. Orthop. Trauma 2018, 1, S12–S16. [Google Scholar] [CrossRef]
- Kempf, A.; Grosse, G.; Taglang Favreul, E. Gamma nail in the treatment of closed trochanteric fractures. Results and indications of 121 cases. Orthop. Traumatol. Surg. Res. 2014, 100, 75–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saudan, M.; Lubbeke, A.; Sadowski, C.; Riand, N.; Stern, R.; Hoffmeyer, P. Pertrochanteric fractures; is there an advantage to an intramedullary nail? A randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J. Orthop. Trauma 2002, 16, 386–393. [Google Scholar] [CrossRef] [PubMed]
- Lindskog, D.M.; Braumgaertner, M.R. Unstable intertrochanteric hip fractures in the alderly. J. Am. Acad. Orthop. Surg. 2004, 12, 179–190. [Google Scholar] [CrossRef]
- Egol, A.K. Proximal Femur Fractures an Evidence-Based Approach to Evaluation and Management, 1st ed.; Springer: Berlin/Heidelberg, Germany, 2018; pp. 77–100. [Google Scholar]
- Lorkowski, J.; Kolaszyńska, O.; Pokorski, M. Artificial Intelligence and Precision Medicine: A Perspective. Adv. Exp. Med. Biol. 2021. [Google Scholar] [CrossRef]
- Harris, W.H. Traumatic Arthritis of the Hip after Dislocation and Acetabular Fractures: Treatment by Mold Arthroplasty an end-result study using a new method of results evaluation. J. Bone Jt. Surg. Am. 1969, 51, 737–755. [Google Scholar] [CrossRef]
- Babhulkar, S. Unstable trochanteric fractures: Issues and avoiding pitfalls. Injury 2017, 48, 803–818. [Google Scholar] [CrossRef]
- Hopp, S.; Wirbel, R.; Ojodu, I.; Pizanis, A.; Pohlemann, T.; Fleischer, J. Does the implant make the difference ?—Prospective comparison of two different proximal femur nails. Acta Orthop. Belg. 2016, 82, 319–331. [Google Scholar]
- Zhang, H.; Zeng, X.; Zhang, N.; Zeng, D.; Xu, P.; Zhang, L.; Chen, D.; Yu, W.; Zhang, X. INTERTAN nail versus proximal femoral nail antirotation-Asia for intertrochanteric femur fractures in elderly patients with primary osteoporosis. J. Int. Med. Res. 2017, 45, 1297–1309. [Google Scholar] [CrossRef] [Green Version]
- Brooks, R. EuroQol: The current state of play. Health Policy 1996, 37, 53–72. [Google Scholar] [CrossRef]
- Griffin, X.L.; Parsons, N.; Achten, J.; Fernandez, M.; Costa, M.L. Recovery of health-related quality of life in a United Kingdom hip fracture population. The Warwick Hip Trauma Evaluation-a prospective cohort study. Bone Jt. J. 2015, 97-B, 372–382. [Google Scholar] [CrossRef] [PubMed]
- Parsons, N.; Griffin, X.L.; Achten, J.; Costa, M.L. Outcome assessment after hip fracture: Is EQ-5D the answer? Bone Jt. Res. 2014, 3, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Selim, A.A.H.A.; Beder, F.K.; Algeaidy, I.T.; Farhat, A.S.; Diab, N.M.; Barakat, A.S. Management of unstable pertrochanteric fractures, evaluation of forgotten treatment options. SICOT J. 2020, 6, 21. [Google Scholar] [CrossRef] [PubMed]
- Mao, W.; Ni, H.; Li, L.; He, Y.; Chen, X.; Tang, H.; Dong, Y. Comparison of Baumgaertner and Chang reduction quality criteria for the assessment of trochanteric fractures. Bone Jt. Res. 2019, 8, 502–550. [Google Scholar] [CrossRef] [PubMed]
- Griffin, X.L.; Costa, M.L.; Phelps, E.; Parsons, N.; Dritsaki, M.; Png, M.E.; Achten, J.; Tutton, E.; Lerner, R.; McGibbon, A.; et al. Retrograde intramedullary nail fixation compared with fixed-angle plate fixation for fracture of the distal femur: The TrAFFix feasibility RCT. Health Technol Assess. 2019, 23, 1–132. [Google Scholar] [CrossRef] [PubMed]
- Lovejoy, C.O. The origin of man. Science 1981, 211, 341–350. [Google Scholar] [CrossRef]
- Coren, S.; Porac, C. Fifty centuries of right-handedness: The historical record. Science 1977, 198, 631–632. [Google Scholar] [CrossRef]
- Rogers, L.J.; Vallortigara, G.; Andrew, R. Divided Brains: The Biology and Behaviour of Brain Asymmetries, 1st ed.; Cambridge UP: Cambridge, UK, 2013. [Google Scholar]
- Lemon, R.N. Descending pathways in motor control. Annu. Rev. Neurosci. 2008, 31, 195–218. [Google Scholar] [CrossRef] [Green Version]
- Versace, E.; Vallortigara, G. Forelimb preferences in human beings and other species: Multiple models for testing hypotheses on lateralization. Front. Psychol. 2015, 6, 233. [Google Scholar] [CrossRef] [Green Version]
- Rogers, L.J.; Vallortigara, G. When and Why Did Brains Break Symmetry? Symmetry 2015, 7, 2181–2194. [Google Scholar] [CrossRef] [Green Version]
- Vallortigara, G.; Versace, E. Laterality at the Neural, Cognitive, and Behavioral Levels. In APA Handbook of Comparative Psychology: Vol. 1. Basic Concepts, Methods, Neural Substrate, and Behavior; American Psychological Association: Washington, DC, USA, 2017; pp. 557–577. [Google Scholar]
- Vallortigara, G.; Rogers, L.J. Survival with an asymmetrical brain: Advantages and disadvantages of cerebral lateralization. Behav. Brain Sci. 2005, 28, 575–588. [Google Scholar] [CrossRef] [PubMed]
- Vallortigara, G.; Rogers, L.J.; Bisazza, A. Possible evolutionary origins of cognitive brain lateralization. Brain Res. Rev. 1999, 30, 164–175. [Google Scholar] [CrossRef]
- Vallortigara, G. Comparative neuropsychology of the dual brain: A stroll through left and right animals’ perceptual worlds. Brain Lang. 2000, 73, 189–219. [Google Scholar] [CrossRef]
- Struchtrup, H. Entropy and the Second Law of Thermodynamics-The Nonequilibrium Perspective. Entropy 2020, 22, 793. [Google Scholar] [CrossRef] [PubMed]
- Andrew, R.J. (Ed.) Neural and Behavioural Plasticity: The Use of the Domestic Chicken as a Model; Oxford University Press: Oxford, UK, 1991. [Google Scholar]
- Vallortigara, G.; Cozzutti, C.; Tommasi, L.; Rogers, L.J. How birds use their eyes: Opposite left-right specialisation for the lateral and frontal visual hemifield in the domestic chick. Curr. Biol. 2001, 11, 29–33. [Google Scholar] [CrossRef] [Green Version]
- Jozet-Alves, C.; Viblanc, V.A.; Romagny, S.; Dacher, M.; Healy, S.D.; Dickel, L. Visual lateralization is task and age dependent in cuttlefish, Sepia officinalis. Anim. Behav. 2012, 83, 1313–1318. [Google Scholar] [CrossRef]
- Romano, D.; Benelli, G.; Kavallieratos, N.G.; Athanassiou, C.G.; Canale, A.; Stefanini, C. Beetle-robot hybrid interaction: Sex, lateralization and mating experience modulate behavioural responses to robotic cues in the larger grain borer Prostephanus truncatus (Horn). Biol. Cybern. 2020, 114, 473–483. [Google Scholar] [CrossRef]
- Ciszkiewicz, A.; Lorkowski, J.; Milewski, G. A novel planning solution for semi-autonomous aspiration of Baker’s cysts. Int. J. Med. Robot. 2018, 14. [Google Scholar] [CrossRef]
- Frasnelli, E.; Vallortigara, G. Individual-Level and Population-Level Lateralization: Two Sides of the Same Coin. Symmetry 2018, 10, 739. [Google Scholar] [CrossRef]
- Romano, D.; Kavallieratos, N.G.; Athanassiou, C.G.; Stefanini, C.; Canale, A.; Benelli, G. Impact of geographical origin and rearing medium on mating success and lateralization in the rice weevil, Sitophilus oryzae (L.) (Coleoptera: Curculionidae). J. Stored Prod. Res. 2016, 69, 106–112. [Google Scholar] [CrossRef]
- Guyer, P.; Landolt, M.; Keller, H.; Eberle, C. The Gamma Nail in per- and intertrochanteric femoral fractures-alternative or supplement to the dynamic hip screw? A prospective randomized study of 100 patients with per- and intertrochanteric femoral fractures in the surgical clinic of the City Hospital of Triemli, Zurich, September 1989–June 1990. Aktuelle Traumatol. 1991, 21, 242–249. [Google Scholar] [PubMed]
- Gjertsen, J.E.; Baste, V.; Fevang, J.M.; Furnes, O.; Engesæter, B. Quality of life following hip fractures: Results from the Norwegian hip fracture register. BMC Musculoskel. Disord. 2016, 17, 265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peeters, C.M.; Visser, E.; Van de Ree, C.L.; Gosens, T.; Den Oudsten, B.L.; De Vries, J. Quality of life after hip fracture in the elderly: A systematic literature review. Injury 2016, 47, 1369–1382. [Google Scholar] [CrossRef]
- Cheng, Y.X.; Sheng, X. Optimal surgical methods to treat intertrochanteric fracture: A Bayesian network meta-analysis based on 36 randomized controlled trials. J. Orthop. Surg. Res. 2020, 15, 402. [Google Scholar] [CrossRef]
- Hong, C.C.; Nashi, N.; Makandura, M.C.; Tan, J.H.; Peter, L.; Murphy, D. The long and short of cephalomedullary nails in the treatment of osteoporotic pertrochanteric fracture. Singap. Med. J. 2017, 58, 85–91. [Google Scholar] [CrossRef] [Green Version]
- Tsai, S.W.; Lin, C.J.; Tzeng, Y.H.; Lin, C.C.; Huang, C.K.; Chang, M.C.; Chiang, C.C. Risk factors for cut-out failure of Gamma3 nails in treating unstable intertrochanteric fractures: An analysis of 176 patients. J. Chin. Med. Assoc. 2017, 80, 587–594. [Google Scholar] [CrossRef]

| DHS Group | Gamma Group | p | |
|---|---|---|---|
| Time from admission to surgery (days) | 3.18 ± 1.85 | 3.38 ± 1.70 | 0.57 |
| Time from surgery to discharge (days) | 4.96 ± 2.86 | 4.31 ± 2.22 | 0.21 |
| Intra-operative time (min) | 52.56 ± 15.32 | 54.33 ± 19.48 | 0.62 |
| DHS Group | Gamma Group | p | |
|---|---|---|---|
| HHS 3-month follow-up | 67.43 ± 7.07 | 68.33 ± 6.01 | 0.54 |
| HHS 6-month follow-up | 78.36± 5.52 | 79.03 ± 5.18 | 0.58 |
| DHS Group | Gamma Group | p | |
|---|---|---|---|
| VAS (pain) 3-month follow-up | 3.72 ± 1.03 | 3.66 ± 0.93 | 0.80 |
| VAS (pain) 6-month follow-up | 2.44 ± 0.94 | 2.21 ± 0.98 | 0.29 |
| DHS Group | Gamma Group | p | |
|---|---|---|---|
| 3 months post-operatively | 0.59 ± 0.12 | 0.60 ± 0.11 | 0.73 |
| 6 months post-operatively | 0.64 ± 0.09 | 0.63 ± 0.09 | 0.58 |
| VAS 3 months post-operatively | 55.55 ± 7.45 | 56.69 ± 5.84 | 0.45 |
| VAS 6 months post-operatively | 61.97 ± 9.24 | 62.61 ± 7.60 | 0.73 |
| DHS Group | Gamma Group | p | |
|---|---|---|---|
| NSA—non-operated side (degrees) | 131.61 ± 2.47 | 130.76 ± 1.90 | 0.09 |
| NSA—operated side (degrees) | 133.22 ± 3.07 | 132.07 ± 2.87 | 0.09 |
| NSA difference between the operated and the opposite side (degrees) | 2.36 ± 2.11 | 2.17 ± 2.18 | 0.69 |
| The minimum distance between the tip of the neck screw and the articular surface of the femoral head (millimeters) | 14.96 ± 5.39 | 10.33 ± 3.40 | 0.00 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gawronska, K.; Lorkowski, J. Functional Symmetry after Surgical Treatment of Pertrochanteric Fractures in the Elderly. Symmetry 2022, 14, 393. https://doi.org/10.3390/sym14020393
Gawronska K, Lorkowski J. Functional Symmetry after Surgical Treatment of Pertrochanteric Fractures in the Elderly. Symmetry. 2022; 14(2):393. https://doi.org/10.3390/sym14020393
Chicago/Turabian StyleGawronska, Karolina, and Jacek Lorkowski. 2022. "Functional Symmetry after Surgical Treatment of Pertrochanteric Fractures in the Elderly" Symmetry 14, no. 2: 393. https://doi.org/10.3390/sym14020393






