Composite Score of Readiness (CSR) as a Data Reduction Technique for Monitoring the RTS Process in Footballers following ACL Reconstruction
Abstract
:1. Introduction
- The number of athletes who successfully return to pre-injury level of sport after ACL reconstruction is relatively low.
- Studies have reported that passing the RTS does not provide protection against graft rupture, and residual or undetected deficits in neuromuscular control are highly related to a second ACL injury.
- There are still no clear or validated guidelines about RTS testing after ACL reconstruction.
- This study analyzed how many tests should be included in the RTS test battery and which tests are most indicative for functional deficits related to ACL reconstruction.
2. Materials and Methods
2.1. Participants
- Group 1 (ACL) (n = 24)—after ACL rupture and reconstruction (involved leg—after ACL reconstruction, uninvolved leg—contralateral limb without ACL injury);
- Group 2 (MI) (n = 21)—after mild lower limb injury during the previous 2–3 years (involved leg—after mild injury, uninvolved leg—contralateral limb without injury);
- Group 3 (C) (n = 20)—controls without injuries (the left limb was the equivalent of the involved limb, and the right limb was the equivalent of the uninvolved limb).
2.2. Procedures
2.2.1. Functional Movement Screen Test (FMS)
2.2.2. Y-Balance Test (YBT)
2.2.3. Tuck Jump Assessment (TJA)
2.2.4. Isokinetic Test (IT)
2.2.5. Hop Test for Distance (HT)
2.2.6. Composite Score of Readiness (CSR)
- CSRA-H—for athletes after ACL reconstruction, relative to the group of athletes without injuries;
- CSRM-H—for athletes after mild lower limb injuries, relative to the group of athletes without injuries.
2.2.7. Statistical Analysis
3. Results
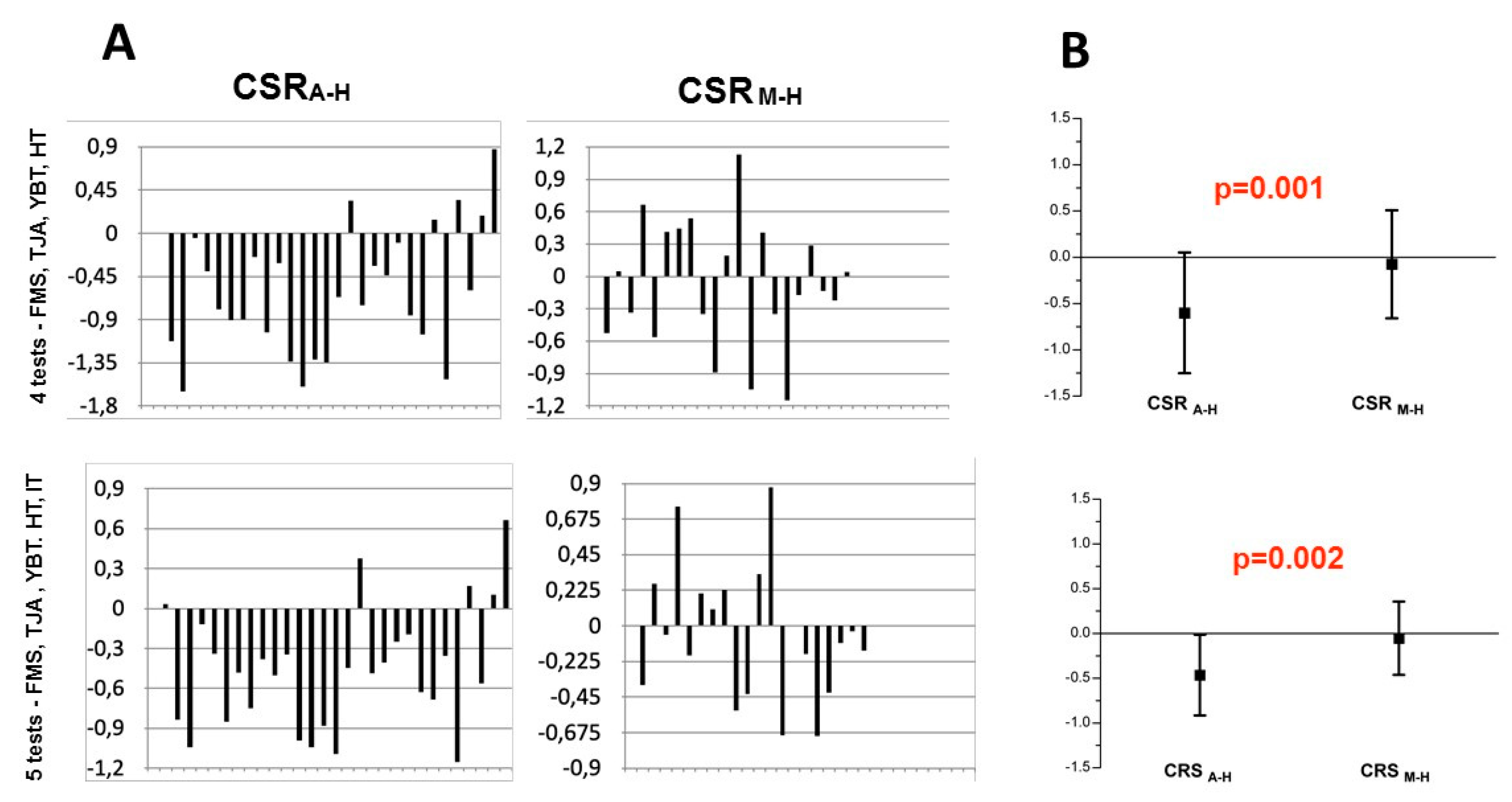
3.1. The Values of CSRA-H and CSRM-H in Individual Athletes and the Difference between CSRA-H and CSRM-H Indices
3.2. Multiple Regression Model
3.2.1. Multiple Regression Model When All Variables Were Included
3.2.2. Multiple Regression Model When Part of the Redundant Variables (H/Q Ratio) Were Excluded
3.2.3. Multiple Regression Model When All Redundant Variables (H/Q Ratio and IT for Extension) Were Excluded
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Gokeler, A.; Dingenen, B.; Hewett, T.E. Rehabilitation and Return to Sport Testing After Anterior Cruciate Ligament Reconstruction: Where Are We in 2022? Arthrosc. Sports Med. Rehabil. 2022, 4, e77–e82. [Google Scholar] [CrossRef] [PubMed]
- Myer, G.D.; Ford, K.R.; Hewett, T.E. Rationale and Clinical Techniques for Anterior Cruciate Ligament Injury Prevention Among Female Athletes. J. Athl. Train. 2004, 39, 352–364. [Google Scholar] [PubMed]
- Lai, C.C.H.; Ardern, C.L.; Feller, J.A.; Webster, K.E. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: A systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br. J. Sports Med. 2018, 52, 128–138. [Google Scholar] [CrossRef] [PubMed]
- Della Villa, F.; Hägglund, M.; Della Villa, S.; Ekstrand, J.; Waldén, M. High rate of second ACL injury following ACL reconstruction in male professional footballers: An updated longitudinal analysis from 118 players in the UEFA Elite Club Injury Study. Br. J. Sports Med. 2021, 55, 1350–1356. [Google Scholar] [CrossRef] [PubMed]
- Longstaffe, R.; Leiter, J.; Gurney-Dunlop, T.; McCormack, R.; MacDonald, P. Return to Play and Career Length After Anterior Cruciate Ligament Reconstruction Among Canadian Professional Football Players. Am. J. Sports Med. 2020, 48, 1682–1688. [Google Scholar] [CrossRef] [PubMed]
- Webster, K.E.; Hewett, T.E. What is the Evidence for and Validity of Return-to-Sport Testing after Anterior Cruciate Ligament Reconstruction Surgery? A Systematic Review and Meta-Analysis. Sports Med. 2019, 49, 917–929. [Google Scholar] [CrossRef]
- van Melick, N.; Pronk, Y.; der Sanden, M.N.V.; Rutten, S.; van Tienen, T.; Hoogeboom, T. Meeting movement quantity or quality return to sport criteria is associated with reduced second ACL injury rate. J. Orthop. Res. 2022, 40, 117–128. [Google Scholar] [CrossRef]
- van Melick, N.; Hoogeboom, T.J.; Pronk, Y.; Rutten, B.; Nijhuis-van der Sanden, M. Less than half of ACL-reconstructed athletes are cleared for return to play based on practice guideline criteria: Results from a prospective cohort study. Int. J. Sports Phys. Ther. 2020, 15, 1006–1018. [Google Scholar] [CrossRef]
- Kyritsis, P.; Bahr, R.; Landreau, P.; Miladi, R.; Witvrouw, E. Likelihood of ACL graft rupture: Not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br. J. Sports Med. 2016, 50, 946–951. [Google Scholar] [CrossRef]
- Losciale, J.M.; Zdeb, R.M.; Ledbetter, L.; Reiman, M.P.; Sell, T.C. The Association Between Passing Return-to-Sport Criteria and Second Anterior Cruciate Ligament Injury Risk: A Systematic Review with Meta-analysis. J. Orthop. Sports Phys. Ther. 2019, 49, 43–54. [Google Scholar] [CrossRef]
- Beischer, S.; Hamrin Senorski, E.; Thomeé, C.; Samuelsson, K.; Thomeé, R. Young athletes return too early to knee-strenuous sport, without acceptable knee function after anterior cruciate ligament reconstruction [published correction appears in Knee Surg Sports Traumatol Arthrosc. 2017 Nov 16]. Knee Surg. Sport. Traumatol. Arthrosc. 2018, 26, 1966–1974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gokeler, A.; Welling, W.; Zaffagnini, S.; Seil, R.; Padua, D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 192–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grindem, H.; Snyder-Mackler, L.; Moksnes, H.; Engebretsen, L.; Risberg, M.A. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: The Delaware-Oslo ACL cohort study. Br. J. Sports Med. 2016, 50, 804–808. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagelli, C.V.; Hewett, T.E. Should Return to Sport be Delayed Until 2 Years After Anterior Cruciate Ligament Reconstruction? Biological and Functional Considerations. Sports Med. 2017, 47, 221–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cronström, A.; Tengman, E.; Häger, C.K. Return to Sports: A Risky Business? A Systematic Review with Meta-Analysis of Risk Factors for Graft Rupture Following ACL Reconstruction. Sports Med. 2022, 53, 91–110. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Österberg, A.; Tagesson, S.; Gauffin, H.; Webster, K.E.; Kvist, J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br. J. Sports Med. 2014, 48, 1613–1619. [Google Scholar] [CrossRef] [Green Version]
- Ithurburn, M.P.; Paterno, M.V.; Ford, K.R.; Hewett, T.E.; Schmitt, L.C. Young Athletes with Quadriceps Femoris Strength Asymmetry at Return to Sport After Anterior Cruciate Ligament Reconstruction Demonstrate Asymmetric Single-Leg Drop-Landing Mechanics. Am. J. Sports Med. 2015, 43, 2727–2737. [Google Scholar] [CrossRef]
- Paterno, M.V.; Kiefer, A.W.; Bonnette, S.; Riley, M.A.; Schmitt, L.C.; Ford, K.R.; Myer, G.D.; Shockley, K.; Hewett, T.E. Prospectively identified deficits in sagittal plane hip-ankle coordination in female athletes who sustain a second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Clin. Biomech. 2015, 30, 1094–1101. [Google Scholar] [CrossRef] [Green Version]
- Schmitt, L.C.; Paterno, M.V.; Hewett, T.E. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J. Orthop. Sports Phys. Ther. 2012, 42, 750–759. [Google Scholar] [CrossRef] [Green Version]
- Paterno, M.V.; Schmitt, L.C.; Ford, K.R.; Rauh, M.J.; Myer, G.D.; Huang, B.; Hewett, T.E. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am. J. Sports Med. 2010, 38, 1968–1978. [Google Scholar] [CrossRef]
- Wasserstein, D.; Huston, L.J.; Nwosu, S.; Spindler, K.; Kaeding, C.; Parker, R.; Wright, R.; Andrish, J.; Marx, R.; Amendola, A.; et al. KOOS pain as a marker for significant knee pain two and six years after primary ACL reconstruction: A Multicenter Orthopaedic Outcomes Network (MOON) prospective longitudinal cohort study. Osteoarthr. Cartil. 2015, 23, 1674–1684. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ashigbi, E.Y.K.; Banzer, W.; Niederer, D. Return to Sport Tests’ Prognostic Value for Reinjury Risk after Anterior Cruciate Ligament Reconstruction: A Systematic Review. Med. Sci. Sports Exerc. 2020, 52, 1263–1271. [Google Scholar] [CrossRef] [PubMed]
- Wren, T.A.L.; Mueske, N.M.; Brophy, C.H.; Pace, J.L.; Katzel, M.J.; Edison, B.R.; Vandenberg, C.D.; Zaslow, T.L. Hop Distance Symmetry Does Not Indicate Normal Landing Biomechanics in Adolescent Athletes with Recent Anterior Cruciate Ligament Reconstruction. J. Orthop. Sports Phys. Ther. 2018, 48, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Ellman, M.B.; Sherman, S.L.; Forsythe, B.; LaPrade, R.F.; Cole, B.J.; Bach, B.R., Jr. Return to play following anterior cruciate ligament reconstruction. J. Am. Acad. Orthop. Surg. 2015, 23, 283–296. [Google Scholar] [CrossRef] [PubMed]
- Davies, G.J.; McCarty, E.; Provencher, M.; Manske, R.C. ACL Return to Sport Guidelines and Criteria. Curr. Rev. Musculoskelet. Med. 2017, 10, 307–314. [Google Scholar] [CrossRef] [Green Version]
- Turner, A.N.; Jones, B.; Stewart, P.; Bishop, C.; Parmar, N.; Chavda, S.; Read, P. Total score of athleticism: Holistic athlete profiling to enhance decision-making. Strength Cond. J. 2019, 41, 91–101. [Google Scholar] [CrossRef]
- Oleksy, Ł.; Mika, A.; Królikowska, A.; Kuchciak, M.; Stolarczyk, M.; Kielnar, R.; Racheniuk, H.; Szczegielniak, J.; Łuszczki, E.; Stolarczyk, A. Composite Score of Readiness (CSR) as Holistic Profiling of Functional Deficits in Footballers Following ACL Reconstruction. J. Clin. Med. 2021, 10, 3570. [Google Scholar] [CrossRef]
- Oleksy, Ł.; Mika, A.; Sulowska-Daszyk, I.; Szymczyk, D.; Kuchciak, M.; Stolarczyk, A.; Rojek, R.; Kielnar, R. Standard RTS criteria effectiveness verification using FMS, Y-balance and TJA in footballers following ACL reconstruction and mild lower limb injuries. Sci. Rep. 2021, 11, 1558. [Google Scholar] [CrossRef] [PubMed]
- Abourezk, M.N.; Ithurburn, M.P.; McNally, M.P.; Thoma, L.M.; Briggs, M.S.; Hewett, T.E.; Spindler, K.P.; Kaeding, C.C.; Schmitt, L.C. Hamstring Strength Asymmetry at 3 Years After Anterior Cruciate Ligament Reconstruction Alters Knee Mechanics During Gait and Jogging. Am. J. Sports Med. 2017, 45, 97–105. [Google Scholar] [CrossRef]
- Stecco, C.; Porzionato, A.; Lancerotto, L.; Stecco, A.; Macchi, V.; Day, J.A.; De Caro, R. Histological study of the deep fasciae of the limbs. J. Bodyw. Mov. Ther. 2008, 12, 225–230. [Google Scholar] [CrossRef]
- Myers, T. Anatomy Trains: Myofascial Meridians for Manual and Movement Therapists, 3rd ed.; Elsevier; Churchill Livingstone: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Snijders, C.J.; Vleeming, A.; Stoeckart, R. Transfer of lumbosacral load to iliac bones and legs. Part 1, 2. Clin. Biomech. 1993, 8, 295–301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pope, R.E. The common compensatory pattern: Its origin and relationship to the postural model. Am. Acad. Osteopath. J. 2003, 14, 19–40. [Google Scholar]
- Dingenen, B.; Gokeler, A. Optimization of the Return-to-Sport Paradigm After Anterior Cruciate Ligament Reconstruction: A Critical Step Back to Move Forward. Sports Med. 2017, 47, 1487–1500. [Google Scholar] [CrossRef]
- Grassi, A.; Quaglia, A.; Canata, G.L.; Zaffagnini, S. An update on the grading of muscle injuries: A narrative review from clinical to comprehensive systems. Joints 2016, 4, 39–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cook, G.; Burton, L.; Kiesel, K.; Rose, G.; Bryant, M.F. Functional Movement Systems: Screening, Assessment, Corrective Strategies; On Target Publications: Aptos, CA, USA, 2010. [Google Scholar]
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional movement screening: The use of fundamental movements as an assessment of function—Part 2. Int. J. Sports Phys. Ther. 2014, 9, 549–563. [Google Scholar]
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional movement screening: The use of fundamental movements as an assessment of function—Part 1. Int. J. Sports Phys. Ther. 2014, 9, 396–409. [Google Scholar]
- Gribble, P.A.; Brigle, J.; Pietrosimone, B.G.; Pfile, K.R.; Webster, K.A. Intrarater reliability of the functional movement screen. J. Strength Cond. Res. 2013, 27, 978–981. [Google Scholar] [CrossRef]
- Smith, C.A.; Chimera, N.J.; Wright, N.J.; Warren, M. Interrater and intrarater reliability of the functional movement screen. J. Strength Cond. Res. 2013, 27, 982–987. [Google Scholar] [CrossRef] [Green Version]
- Chimera, N.J.; Smith, C.A.; Warren, M. Injury history, sex, and performance on the functional movement screen and Y balance test. J. Athl. Train. 2015, 50, 475–485. [Google Scholar] [CrossRef] [Green Version]
- Brumitt, J.; Nelson, K.; Duey, D.; Jeppson, M.; Hammer, L. Preseason Y Balance Test Scores are not Associated with Noncontact Time-Loss Lower Quadrant Injury in Male Collegiate Basketball Players. Sports 2018, 7, 4. [Google Scholar] [CrossRef] [Green Version]
- Shaffer, S.W.; Teyhen, D.S.; Lorenson, C.L.; Warren, R.L.; Koreerat, C.M.; Straseske, C.A.; Childs, J.D. Y-balance test: A reliability study involving multiple raters. Mil. Med. 2013, 178, 1264–1270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lininger, M.R.; Smith, C.A.; Chimera, N.J.; Hoog, P.; Warren, M. Tuck Jump Assessment: An Exploratory Factor Analysis in a College Age Population. J. Strength Cond. Res. 2017, 31, 653–659. [Google Scholar] [CrossRef] [PubMed]
- Herrington, L.; Myer, G.D.; Munro, A. Intra and inter-tester reliability of the tuck jump assessment. Phys. Ther. Sport. 2013, 14, 152–155. [Google Scholar] [CrossRef] [PubMed]
- Tiffreau, V.; Ledoux, I.; Eymard, B.; Thévenon, A.; Hogrel, J.Y. Isokinetic muscle testing for weak patients suffering from neuromuscular disorders: A reliability study. Neuromuscul. Disord. 2007, 17, 524–531. [Google Scholar] [CrossRef] [PubMed]
- Larsson, B.; Karlsson, S.; Eriksson, M.; Gerdle, B. Test-retest reliability of EMG and peak torque during repetitive maximum concentric knee extensions. J. Electromyogr. Kinesiol. 2003, 13, 281–287. [Google Scholar] [CrossRef]
- Ross, M.D.; Langford, B.; Whelan, P.J. Test-retest reliability of 4 single-leg horizontal hop tests. J. Strength Cond. Res. 2002, 16, 617–622. [Google Scholar]
- Kockum, B.; Heijne, A.I. Hop performance and leg muscle power in athletes: Reliability of a test battery. Phys. Ther. Sport 2015, 16, 222–227. [Google Scholar] [CrossRef]
- Munro, A.G.; Herrington, L.C. Between-session reliability of four hop tests and the agility T-test. J. Strength Cond. Res. 2011, 25, 1470–1477. [Google Scholar] [CrossRef]
- Webster, K.E.; Feller, J.A. Who Passes Return-to-Sport Tests, and Which Tests Are Most Strongly Associated with Return to Play After Anterior Cruciate Ligament Reconstruction? Orthop. J. Sports Med. 2020, 8, 2325967120969425. [Google Scholar] [CrossRef]
- Hewett, T.E.; Webster, K.E.; Hurd, W.J. Systematic Selection of Key Logistic Regression Variables for Risk Prediction Analyses: A Five-Factor Maximum Model. Clin. J. Sport Med. 2019, 29, 78–85. [Google Scholar] [CrossRef]
- Abrams, G.D.; Harris, J.D.; Gupta, A.K.; McCormick, F.M.; Bush-Joseph, C.A.; Verma, N.N.; Cole, B.J.; Bach, B.R. Functional Performance Testing After Anterior Cruciate Ligament Reconstruction: A Systematic Review. Orthop. J. Sports Med. 2014, 2, 2325967113518305. [Google Scholar] [CrossRef] [PubMed]
- Larsen, J.B.; Farup, J.; Lind, M.; Dalgas, U. Muscle strength and functional performance is markedly impaired at the recommended time point for sport return after anterior cruciate ligament reconstruction in recreational athletes. Hum. Mov. Sci. 2015, 39, 73–87. [Google Scholar] [CrossRef] [PubMed]
- Thomeé, R.; Kaplan, Y.; Kvist, J.; Myklebust, G.; Risberg, M.A.; Theisen, D.; Tsepis, E.; Werner, S.; Wondrasch, B.; Witvrouw, E. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1798–1805. [Google Scholar] [CrossRef] [Green Version]
- Undheim, M.B.; Cosgrave, C.; King, E.; Strike, S.; Marshall, B.; Falvey, É.; Franklyn-Miller, A. Isokinetic muscle strength and readiness to return to sport following anterior cruciate ligament reconstruction: Is there an association? A systematic review and a protocol recommendation. Br. J. Sports Med. 2015, 49, 1305–1310. [Google Scholar] [CrossRef] [PubMed]
- Kuenze, C.; Hertel, J.; Saliba, S.; Diduch, D.R.; Weltman, A.; Hart, J.M. Clinical thresholds for quadriceps assessment after anterior cruciate ligament reconstruction. J. Sport Rehabil. 2015, 24, 36–46. [Google Scholar] [CrossRef]
- Thomeé, R.; Neeter, C.; Gustavsson, A.; Thomeé, P.; Augustsson, J.; Eriksson, B.; Karlsson, J. Variability in leg muscle power and hop performance after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 1143–1151. [Google Scholar] [CrossRef]
- Hewett, T.E.; Myer, G.D.; Zazulak, B.T. Hamstrings to quadriceps peak torque ratios diverge between sexes with increasing isokinetic angular velocity. J. Sci. Med. Sport 2008, 11, 452–459. [Google Scholar] [CrossRef] [Green Version]
- Paterno, M.V.; Rauh, M.J.; Schmitt, L.C.; Ford, K.R.; Hewett, T.E. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin. J. Sport Med. 2012, 22, 116–121. [Google Scholar] [CrossRef]

| Group 1 | Group 2 | Group 3 | |
|---|---|---|---|
| Number of subjects (n) | 24 | 21 | 20 |
| Height (cm) | 175 ± 4 | 177 ± 6 | 178 ± 6 |
| Weight (kg) | 77.3 ± 7.6 | 74.3 ± 9.1 | 75.8 ± 8.8 |
| Age | 22.7 ± 3.6 | 20.5 ± 3.7 | 23.1 ± 2.8 |
| CSRA-H | B | SE (B) | p | r | Tolerance | CSRM-H | B | SE (B) | p | r | Tolerance |
|---|---|---|---|---|---|---|---|---|---|---|---|
| FMS | 0.139 | 0.019 | 0.000 | 0.883 | 0.335 | FMS | 0.107 | 0.035 | 0.022 | 0.780 | 0.621 |
| YBT IL | 0.384 | 0.023 | 0.000 | 0.972 | 0.218 | YBT IL | 0.231 | 0.059 | 0.008 | 0.844 | 0.216 |
| YBT UL | 0.249 | 0.023 | 0.000 | 0.937 | 0.215 | YBT UL | 0.338 | 0.056 | 0.000 | 0.926 | 0.246 |
| TJA | 0.040 | 0.014 | 0.011 | 0.595 | 0.607 | TJA | 0.186 | 0.059 | 0.019 | 0.789 | 0.219 |
| IT Ext IL | 0.022 | 0.031 | 0.484 | 0.181 | 0.127 | IT Ext IL | −0.161 | 0.456 | 0.736 | −0.142 | −0.009 |
| IT Ext UL | 0.295 | 0.075 | 0.001 | 0.709 | 0.021 | IT Ext UL | 0.113 | 0.132 | 0.421 | 0.332 | 0.023 |
| IT Flx IL | 0.150 | 0.021 | 0.000 | 0.879 | 0.274 | IT Flx IL | 0.427 | 0.392 | 0.318 | 0.406 | 0.030 |
| IT Flx UL | −0.060 | 0.062 | 0.345 | −0.243 | 0.031 | IT Flx UL | 0.035 | 0.187 | 0.857 | 0.076 | 0.005 |
| IT H/Q IL | −0.008 | 0.035 | 0.811 | −0.062 | 0.098 | IT H/Q IL | −0.127 | 0.304 | 0.689 | −0.168 | 0.008 |
| IT HQ UL | 0.229 | 0.055 | 0.000 | 0.728 | 0.039 | IT HQ UL | 0.176 | 0.105 | 0.144 | 0.564 | 0.069 |
| HT SI | 0.123 | 0.021 | 0.000 | 0.828 | 0.263 | HT SI | 0.152 | 0.051 | 0.025 | 0.770 | 0.291 |
| HT IL | 0.099 | 0.031 | 0.006 | 0.629 | 0.121 | HT IL | 0.130 | 0.068 | 0.106 | 0.612 | 0.162 |
| HT UL | 0.192 | 0.028 | 0.000 | 0.865 | 0.146 | HT UL | 0.125 | 0.081 | 0.174 | 0.531 | 0.115 |
| R2 = 0.996; SE = 0.264; p < 0.000 | R2 = 0.985; SE = 0.051; p < 0.000 | ||||||||||
| CSRA-H | B | SE (B) | p | r | Tolerance | CSRM-H | B | SE (B) | p | r | Tolerance |
|---|---|---|---|---|---|---|---|---|---|---|---|
| FMS | 0.122 | 0.024 | 0.000 | 0.772 | 0.388 | FMS | 0.118 | 0.036 | 0.011 | 0.756 | 0.649 |
| YBT IL | 0.367 | 0.030 | 0.000 | 0.945 | 0.246 | YBT IL | 0.268 | 0.056 | 0.001 | 0.858 | 0.264 |
| YBT UL | 0.265 | 0.032 | 0.000 | 0.893 | 0.221 | YBT UL | 0.320 | 0.056 | 0.000 | 0.894 | 0.265 |
| TJA | 0.032 | 0.019 | 0.019 | 0.383 | 0.623 | TJA | 0.122 | 0.0475 | 0.032 | 0.673 | 0.377 |
| IT Ext IL | 0.050 | 0.024 | 0.050 | 0.454 | 0.393 | IT Ext IL | 0.007 | 0.087 | 0.933 | 0.030 | 0.110 |
| IT Ext UL | −0.003 | 0.031 | 0.923 | −0.023 | 0.238 | IT Ext UL | −0.051 | 0.085 | 0.560 | −0.209 | 0.116 |
| IT Flx IL | 0.158 | 0.024 | 0.000 | 0.843 | 0.384 | IT Flx IL | 0.200 | 0.068 | 0.018 | 0.721 | 0.184 |
| IT Flx UL | 0.171 | 0.035 | 0.000 | 0.764 | 0.186 | IT Flx UL | 0.325 | 0.075 | 0.002 | 0.836 | 0.150 |
| HT SI | 0.116 | 0.023 | 0.000 | 0.772 | 0.423 | HT SI | 0.120 | 0.044 | 0.027 | 0.688 | 0.425 |
| HT IL | 0.099 | 0.039 | 0.022 | 0.518 | 0.147 | HT IL | 0.147 | 0.069 | 0.068 | 0.596 | 0.174 |
| HT UL | 0.184 | 0.037 | 0.000 | 0.762 | 0.160 | HT UL | 0.085 | 0.069 | 0.253 | 0.399 | 0.176 |
| R2 = 0.993; SE = 0.036; p < 0.000 | R2 = 0.983; SE = 0.054; p < 0.000 | ||||||||||
| CSRA-H | B | SE (B) | p | r | Tolerance | CSRM-H | B | SE (B) | p | r | Tolerance |
|---|---|---|---|---|---|---|---|---|---|---|---|
| FMS | 0.139 | 0.024 | 0.000 | 0.793 | 0.452 | FMS | 0.122 | 0.031 | 0.022 | 0.779 | 0.771 |
| YBT IL | 0.388 | 0.03 | 0.000 | 0.942 | 0.272 | YBT IL | 0.281 | 0.050 | 0.000 | 0.870 | 0.295 |
| YBT UL | 0.237 | 0.030 | 0.000 | 0.871 | 0.292 | YBT UL | 0.312 | 0.047 | 0.000 | 0.902 | 0.336 |
| TJA | 0.026 | 0.020 | 0.023 | 0.281 | 0.653 | TJA | 0.120 | 0.042 | 0.017 | 0.669 | 0.418 |
| IT Flx IL | 0.157 | 0.026 | 0.000 | 0.810 | 0.401 | IT Flx IL | 0.185 | 0.051 | 0.005 | 0.748 | 0.277 |
| IT Flx UL | 0.186 | 0.025 | 0.345 | 0.863 | 0.438 | IT Flx UL | 0.301 | 0.054 | 0.000 | 0.866 | 0.248 |
| HT SI | 0.128 | 0.023 | 0.000 | 0.780 | 0.489 | HT SI | 0.111 | 0.030 | 0.004 | 0.753 | 0.790 |
| HT IL | 0.105 | 0.04 | 0.024 | 0.489 | 0.148 | HT IL | 0.162 | 0.063 | 0.028 | 0.629 | 0.186 |
| HT UL | 0.177 | 0.040 | 0.000 | 0.706 | 0.163 | HT UL | 0.061 | 0.057 | 0.312 | 0.318 | 0.225 |
| R2 = 0.992; SE = 0.039; p < 0.000 | R2 = 0.985; SE = 0.050; p < 0.000 | ||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oleksy, Ł.; Mika, A.; Kielnar, R.; Szczudło, M.; Racheniuk, H.; Adamska, O.; Rzepko, M.; Królikowska, A.; Reichert, P.; Prill, R.; et al. Composite Score of Readiness (CSR) as a Data Reduction Technique for Monitoring the RTS Process in Footballers following ACL Reconstruction. Symmetry 2023, 15, 298. https://doi.org/10.3390/sym15020298
Oleksy Ł, Mika A, Kielnar R, Szczudło M, Racheniuk H, Adamska O, Rzepko M, Królikowska A, Reichert P, Prill R, et al. Composite Score of Readiness (CSR) as a Data Reduction Technique for Monitoring the RTS Process in Footballers following ACL Reconstruction. Symmetry. 2023; 15(2):298. https://doi.org/10.3390/sym15020298
Chicago/Turabian StyleOleksy, Łukasz, Anna Mika, Renata Kielnar, Miłosz Szczudło, Henryk Racheniuk, Olga Adamska, Marian Rzepko, Aleksandra Królikowska, Paweł Reichert, Robert Prill, and et al. 2023. "Composite Score of Readiness (CSR) as a Data Reduction Technique for Monitoring the RTS Process in Footballers following ACL Reconstruction" Symmetry 15, no. 2: 298. https://doi.org/10.3390/sym15020298
APA StyleOleksy, Ł., Mika, A., Kielnar, R., Szczudło, M., Racheniuk, H., Adamska, O., Rzepko, M., Królikowska, A., Reichert, P., Prill, R., & Stolarczyk, A. (2023). Composite Score of Readiness (CSR) as a Data Reduction Technique for Monitoring the RTS Process in Footballers following ACL Reconstruction. Symmetry, 15(2), 298. https://doi.org/10.3390/sym15020298












