Symmetry Function in Trans-Tibial Amputees Gait Supplied with the New Concept of Affordable Dynamic Foot Prosthesis—Case Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Experimental Procedures
2.3. Data Analyses
2.4. Statistical Analyses
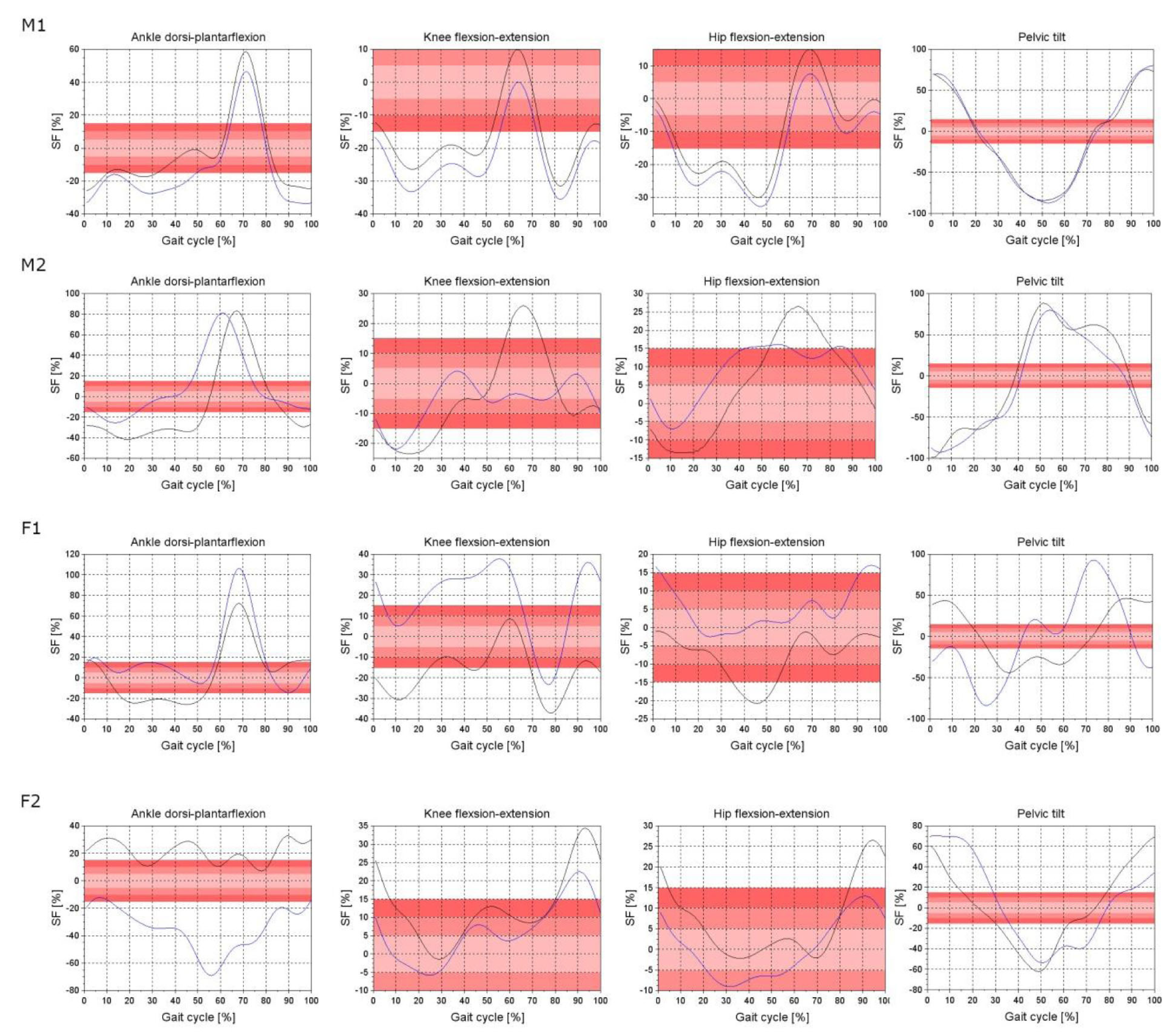
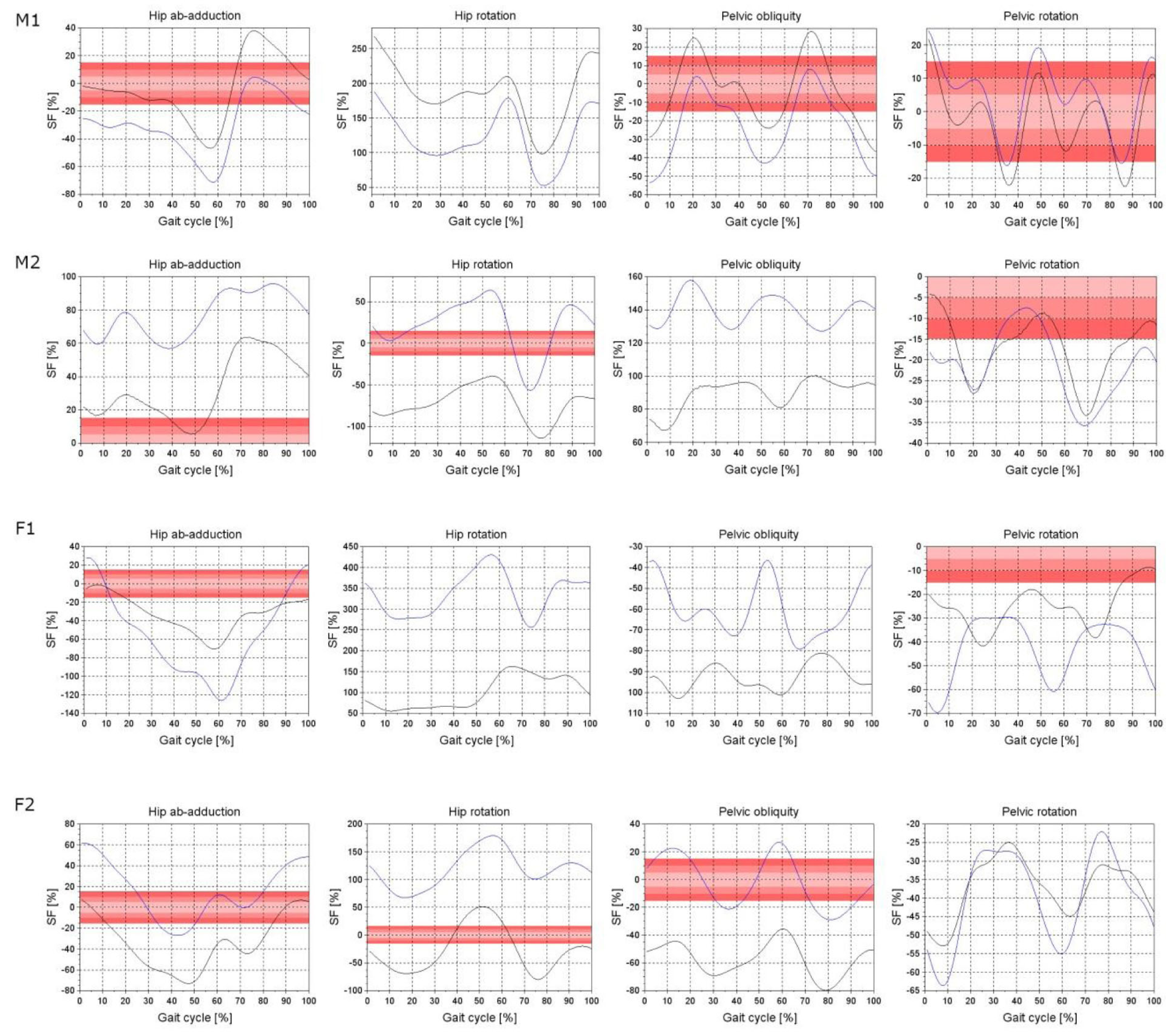
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pran, L.; Harnanan, D.; Baijoo, S.; Short, A.; Cave, C.; Maharaj, R.; Cawich, S.O.; Naraynsingh, V. Major lower limb amputations: Recognizing pitfalls. Cureus 2021, 13, e16972. [Google Scholar] [CrossRef]
- Spoden, M.; Nimptsch, U.; Mansky, T. Amputation rates of the lower limb by amputation level—Observational study using German national hospital discharge data from 2005 to 2015. BMC Health Serv. Res. 2019, 19, 8. [Google Scholar] [CrossRef]
- Eidmann, A.; Kamawal, Y.; Luedemann, M.; Raab, P.; Rudert, M.; Stratos, I. Demographics and etiology for lower extremity amputations—Experiences of an University Orthopaedic Center in Germany. Medicina 2023, 59, 200. [Google Scholar] [CrossRef]
- Available online: https://ezdrowie.gov.pl/portal/home/badania-i-dane/zdrowe-dane/zestawienia/informacje-o-liczbie-amputacji-konczyn (accessed on 11 March 2019).
- Ziegler-Graham, K.; MacKenzie, E.J.; Ephraim, P.L.; Travison, T.G.; Brookmeyer, R. Estimating the Prevalence of Limb Loss in the United States: 2005 to 2050. Arch. Phys. Med. Rehabil. 2008, 89, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Paradisi, F.; Delussu, A.S.; Brunelli, S.; Iosa, M.; Pellegrini, R.; Zenardi, D.; Traballesi, M. The conventional non-articulated SACH or a multiaxial prosthetic foot for hypomobile transtibial amputees? A clinical comparison on mobility, balance, and quality of life. Sci. World J. 2015, 2015, 261801. [Google Scholar] [CrossRef]
- Yang, J.R.; Yang, H.S.; Ahn, D.H.; Ahn, D.Y.; Sim, W.S.; Yang, H.E. Differences in gait patterns of unilateral transtibial amputees with two types of energy storing prosthetic feet. Ann. Rehabil. Med. 2018, 42, 609–616. [Google Scholar] [CrossRef]
- Hafner, B.J.; Sanders, J.E.; Czerniecki, J.; Fergason, J. Energy storage and return prostheses: Does patient perception correlate with biomechanical analysis? Clin. Biomech. 2002, 17, 325–344. [Google Scholar] [CrossRef]
- Chiriac, O.A.; Bucur, D. From conventional prosthetic feet to bionic feet. A review. In Proceedings of the International Conference of Mechatronics and Cyber-MixMechatronics—2020; Gheorghe, G.I., Ed.; Springer: Cham, Switzerland, 2020; pp. 130–138. [Google Scholar] [CrossRef]
- Jaegers, S.M.; Arendzen, J.H.; de Jongh, H.J. Prosthetic gait of unilateral transfemoral amputees: A kinematic study. Arch. Phys. Med. Rehabil. 1995, 76, 736–743. [Google Scholar] [CrossRef]
- Waters, R.L.; Mulroy, S. The energy expenditure of normal and pathologic gait. Gait Posture 1999, 9, 207–231. [Google Scholar] [CrossRef]
- Goujon-Pillet, H.; Sapin, E.; Fodé, P.; Lavaste, F. Three-dimensional motions of trunk and pelvis during transfemoral amputee gait. Arch. Phys. Med. Rehabil. 2008, 89, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Segal, A.D.; Orendurff, M.S.; Klute, G.K.; McDowell, M.L.; Pecoraro, J.A.; Shofer, J.; Czerniecki, J.M. Kinematic and kinetic comparisons of transfemoral amputee gait using C-Leg and Mauch SNS prosthetic knees. J. Rehabil. Res. Dev. 2006, 43, 857–870. [Google Scholar] [CrossRef]
- Donnelley, C.A.; von Kaeppler, E.P.; Hetherington, A.; Shirley, C.; Haonga, B.T.; Challa, S.T.; Andrysek, J.; Lutyens, E.M.; Mamseri, L.; Mwakasungula, G.; et al. Cost-effectiveness analysis of prosthesis provision for patients with transfemoral amputation in Tanzania. Prosthet. Orthot. Int. 2022, 46, 523–531. [Google Scholar] [CrossRef]
- McGimpsey, G.; Bradford, T.C. Limb Prosthetics Services and Devices. Critical Unmet Need: Market Analysis; Bioengineering Institute Center for Neuroprosthetics Worcester Polytechnic Institution: Worcester, MA, USA, 2008; pp. 1–35. [Google Scholar]
- Winiarski, S.; Rutkowska-Kucharska, A.; Pozowski, A.; Aleksandrowicz, K. A new method of evaluating the symmetry of movement used to assess the gait of patients after unilateral total hip replacement. Appl. Bionics Biomech. 2019, 2019, 7863674. [Google Scholar] [CrossRef] [PubMed]
- Kowal, M.; Winiarski, S.; Gieysztor, E.; Kołcz, A.; Walewicz, K.; Borowicz, W.; Rutkowska-Kucharska, A.; Paprocka-Borowicz, M. Symmetry function in gait pattern analysis in patients after unilateral transfemoral amputation using a mechanical or microprocessor prosthetic knee. J. NeuroEng. Rehabil. 2021, 18, 9. [Google Scholar] [CrossRef]
- Winiarski, S.; Rutkowska-Kucharska, A.; Kowal, M. Symmetry function—An effective tool for evaluating the gait symmetry of trans-femoral amputees. Gait Posture 2021, 90, 9–15. [Google Scholar] [CrossRef]
- Kadaba, M.P.; Ramakrishnan, H.K.; Wootten, M.E. Measurement of lower extremity kinematics during level walking. J. Orthop. Res. 1990, 8, 383–392. [Google Scholar] [CrossRef]
- Davis, R.B.; Õunpuu, S.; Tyburski, D.; Gage James, R. A gait analysis data collection and reduction technique. Hum. Mov. Sci. 1991, 10, 575–587. [Google Scholar] [CrossRef]
- Fryzowicz, A.; Murawa, M.; Kabacinski, J.; Rzepnicka, A.; Dworak, L.B. Reference values of spatiotemporal parameters, joint angles, ground reaction forces, and plantar pressure distribution during normal gait in young women. Acta Bioeng. Biomech. 2018, 20, 9–57. [Google Scholar] [CrossRef]
- Pietraszewski, B.; Winiarski, S.; Jaroszczuk, S. Three-dimensional human gait pattern—Reference data for normal men. Acta Bioeng. Biomech. 2012, 4, 9–16. [Google Scholar]
- Rutkowska-Kucharska, A.; Kowal, M.; Winiarski, S. Relationship between asymmetry of gait and muscle torque in patients after unilateral transfemoral amputation. Appl. Bionics Biomech. 2018, 2018, 5190816. [Google Scholar] [CrossRef]
- Forczek, W.; Staszkiewicz, R. An evaluation of symmetry in the lower limb joints during the able-bodied gait of women and men. J. Hum. Kinet. 2012, 35, 47–57. [Google Scholar] [CrossRef]
- Loiret, I.; Villa, C.; Dauriac, B.; Bonnet, X.; Martinet, N.; Paysant, J.; Pillet, H. Are wearable insoles a validated tool for quantifying transfemoral amputee gait asymmetry? Prosthet. Orthot. Int. 2019, 43, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Adamczyk, P.G.; Kuo, A.D. Mechanisms of gait asymmetry due to push-off deficiency in unilateral amputees. IEEE Trans. Neural. Syst. Rehabil. Eng. 2015, 23, 776–785. [Google Scholar] [CrossRef]
- Schaarschmidt, M.; Lipfert, S.W.; Meier-Gratz, C.; Scholle, H.C.; Seyfarth, A. Functional gait asymmetry of unilateral transfemoral amputees. Hum. Mov. Sci. 2012, 31, 907–917. [Google Scholar] [CrossRef]
- Yang, L.; Dyer, P.S.; Carson, R.J.; Webster, J.B.; Foreman, K.B.; Bamberg, S.J.M. Utilization of a lower extremity ambulatory feedback system to reduce gait asymmetry in transtibial amputation gait. Gait Posture 2012, 36, 631–634. [Google Scholar] [CrossRef] [PubMed]
- Seth, M.; Coyle, P.C.; Pohlig, R.T.; Beisheim, E.H.; Horne, J.R.; Hicks, G.E.; Sions, J.M. Gait asymmetry is associated with performance-based physical function among adults with lower-limb amputation. Physiother. Theory Pract. 2022, 38, 3108–3118. [Google Scholar] [CrossRef]
- Gorwa, J.; Kabaciński, J.; Murawa, M.; Śpikowska-Pawelec, W.; Fryzowicz, A. Is the symmetry of classical ballet positions perfect. Med. Probl. Perform. Art. 2023; accepted. [Google Scholar]
| Subjects | Body Height [m] | Body Mass [kg] | Age [Years] | Cause | Time Since Amputation [Years] | Amputated Side | Socket Type | Prosthetic Foot |
|---|---|---|---|---|---|---|---|---|
| F1 | 1.70 | 92.0 | 20 | Congenital Malformation | birth defect | Right | Contact Shuttle Lock | SACH |
| F2 | 1.60 | 89.0 | 61 | Trauma | 57 | Left | Full contact | Pacifica LP 23 FS4-00-03 |
| M1 | 1.78 | 100.2 | 49 | Trauma | 4 | Left | Harmony E2 | Ottobock 1C64 Triton HD |
| M2 | 1.81 | 87.2 | 44 | Congenital Malformation | birth defect | Right | Full contact BOA system | Ottobock 1C60 Triton |
| Joint | Prosthesis | F1 | F2 | M1 | M2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5% | 10% | 15% | 5% | 10% | 15% | 5% | 10% | 15% | 5% | 10% | 15% | ||
| Ankle flexion extension | FP | 4 | 16 | 29 | 0 | 6 | 28 | 18 | 19 | 44 | 5 | 8 | 13 |
| DFP | 17 | 42 | 69 | 0 | 0 | 9 | 3 | 8 | 20 | 25 | 37 | 54 | |
| Knee flexion-extension | FP | 7 | 20 | 46 | 19 | 43 | 73 | 8 | 18 | 31 | 12 | 43 | 55 |
| DFP | 4 | 19 | 28 | 40 | 75 | 84 | 9 | 13 | 17 | 54 | 77 | 84 | |
| Hip flexion extension | FP | 39 | 72 | 80 | 57 | 71 | 80 | 25 | 41 | 56 | 17 | 38 | 73 |
| DFP | 60 | 78 | 88 | 35 | 85 | 100 | 20 | 43 | 51 | 19 | 39 | 74 | |
| Hip ab-adduction | FP | 9 | 14 | 17 | 10 | 24 | 27 | 16 | 34 | 53 | 0 | 11 | 17 |
| DFP | 4 | 8 | 12 | 16 | 17 | 39 | 17 | 21 | 24 | 0 | 0 | 0 | |
| Hip rotation | FP | 0 | 0 | 0 | 2 | 5 | 8 | 0 | 0 | 0 | 0 | 0 | 0 |
| DFP | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 14 | 20 | |
| Pelvic tilt | FP | 6 | 11 | 17 | 9 | 19 | 30 | 5 | 10 | 18 | 2 | 5 | 7 |
| DFP | 8 | 12 | 25 | 5 | 10 | 16 | 5 | 11 | 16 | 3 | 6 | 10 | |
| Pelvic obliquity | FP | 0 | 0 | 0 | 0 | 0 | 0 | 22 | 35 | 47 | 0 | 0 | 0 |
| DFP | 0 | 0 | 0 | 12 | 24 | 40 | 16 | 28 | 42 | 0 | 0 | 0 | |
| Pelvic rotation | FP | 0 | 8 | 15 | 0 | 0 | 0 | 43 | 62 | 81 | 3 | 16 | 47 |
| DFP | 0 | 0 | 0 | 0 | 0 | 0 | 20 | 61 | 78 | 0 | 13 | 23 | |
| Prosthesis | F1 | F2 | M1 | M2 | ||||
|---|---|---|---|---|---|---|---|---|
| ILE | ULE | ILE | ULE | ILE | ULE | ILE | ULE | |
| DFP | ||||||||
| SL [m] | 0.60 ± 0.02 | 0.65 b ± 0.02 | 0.56 a ± 0.03 | 0.46 ± 0.02 | 0.60 c ± 0.02 | 0.67 b,c ± 0.02 | 0.78 a ± 0.02 | 0.73 ± 0.02 |
| StP [%GC] | 58.8 ± 2.3 | 60.8 ± 4.3 | 60.1 ± 2.9 | 61.9 ± 1.6 | 62.3 ± 0.6 | 67.5 b ± 0.5 | 57.6 ± 1.9 | 60.6 c ± 2.3 |
| SwP [%GC] | 41.2 ± 2.3 | 39.2 c ± 4.3 | 39.9 ± 2.9 | 38.1 ± 1.6 | 37.7 a ± 0.6 | 32.5 ± 0.5 | 42.4 ± 1.9 | 39.4 ± 2.3 |
| FP | ||||||||
| SL [m] | 0.58 ± 0.03 | 0.72 b,d ± 0.02 | 0.62 a,d ± 0.02 | 0.49 d ± 0.02 | 0.55 ± 0.02 | 0.63 b ± 0.03 | 0.81 a ± 0.03 | 0.74 ± 0.02 |
| StP [%GC] | 59.4 ± 1.1 | 64.1 b,d ± 1.3 | 61.5 ± 1.2 | 61.1 ± 0.8 | 63.1 ± 0.9 | 68.0 b ± 1.0 | 58.6 ± 0.8 | 58.1 ± 1.0 |
| SwP [%GC] | 40.6 a ± 1.1 | 35.9 ± 1.3 | 38.5 ± 1.2 | 38.9 ± 0.8 | 36.9 a ± 0.9 | 32.0 ± 1.0 | 41.4 ± 0.8 | 41.9 d± 1.0 |
| Prosthesis | F1 | F2 | M1 | M2 | ||||
|---|---|---|---|---|---|---|---|---|
| ILE | ULE | ILE | ULE | ILE | ULE | ILE | ULE | |
| DFP | ||||||||
| AF [°] | 4.2 a ± 1.0 | −16.2 ± 1.8 | −3.7 ± 0.6 | −1.6 b ± 0.9 | 0.1 a ± 0.9 | −6.0 ± 1.5 | −4.5 a ± 0.4 | −19.1 ± 1.7 |
| KF [°] | 23.4 a,c ± 1.7 | 6.5 ± 1.7 | −1.3 a ± 1.1 | −5.7 ± 1.4 | −5.0 ± 0.9 | 6.8 b,c ± 1.1 | 7.2 a,c ± 0.7 | 5.8 c ± 1.2 |
| HF [°] | 14.1 c ± 2.1 | 13.9 c ± 1.5 | −8.5 ± 0.9 | −5.7 b c ± 0.7 | −4.1 ± 1.0 | 5.9 b,c ± 1.2 | 0.8 a,c ± 0.8 | −6.5 c ± 1.0 |
| HA [°] | −3.3 c ± 0.9 | 8.4 b,c ± 1.4 | 2.7 a,c ± 1.1 | 1.6 ± 0.7 | −0.5 ± 0.9 | 1.4 b ± 0.8 | −2.7 a,c ± 0.7 | −10.8 ± 0.7 |
| HR [°] | 17.3 a ± 2.0 | 3.7 ± 0.9 | −6.8 ± 1.1 | −4.1 c ± 1.4 | −14.3 c ± 0.8 | −9.5 b ± 1.4 | −11.9 ± 1.2 | 6.3 b ± 1.6 |
| PO [°] | −7.4 ± 0.6 | −1.6 b ± 0.4 | −3.3 a,c ± 0.6 | −4.4 ± 0.5 | −2.8 ± 0.5 | −2.2 b ± 0.5 | 1.1 a,c ± 0.4 | −7.2 ± 0.6 |
| PT [°] | 16.2 c ± 1.1 | 16.4 c ± 1.1 | 9.1 c ± 0.8 | 9.6 b, c ± 1.0 | 10.8 ± 0.7 | 10.8 ± 0.7 | 11.2 c ± 0.5 | 11.3 c ± 0.6 |
| PR [°] | −19.7 ± 2.2 | −6.2 b,c ± 1.6 | −17.5 ± 1.4 | −5.6 b ± 2.0 | −9.7 a,c ± 2.1 | −10.9 ± 1.4 | −12.7 ± 1.1 | −8.3 b ± 1.4 |
| FP | ||||||||
| AF [°] | 5.1 a,d ± 1.0 | −4.3 d ± 3.6 | 7.8 a,d ± 0.9 | 2.0 d ± 1.9 | 1.2 a,d ± 1.0 | −8.0 ± 5.9 | −0.5 a,d ± 0.7 | −13.3 d ± 2.8 |
| KF [°] | 4.8 ± 3.5 | 12.3 b,d ± 1.7 | 7.2 a,d ± 2.1 | 1.7 d ± 1.8 | −3.0 d ± 2.1 | 2.9 b ± 15.2 | −4.8 ± 1.1 | −1.6 b ± 1.2 |
| HF [°] | −8.3 ± 2.6 | −2.6 b ± 0.8 | −7.8 a,d ± 1.4 | −8.3 ± 0.9 | −3.9 ± 0.8 | 3.4 b ± 8.2 | −8.8 a ± 1.4 | −14.0 ± 1.2 |
| HA [°] | −9.0 ± 1.0 | −1.5 b ± 0.9 | 0.9 ± 1.7 | 4.2 b,d ± 1.2 | 0.1 a,d ± 0.9 | −1.3 ± 7.3 | −6.6 a ± 0.9 | −10.8 ± 0.8 |
| HR [°] | 24.7 a,d ± 6.8 | 3.4 ± 1.2 | 0.9 a,d ± 1.7 | −22.1 ± 8.3 | −17.4 ± 2.8 | −6.5 b,d ± 12.0 | 18.7 d ± 1.3 | 18.7 d ± 2.7 |
| PO [°] | −7.4 ± 0.7 | 0.3 b,d ± 0.4 | −4.3 ± 0.5 | −1.7 b,d ± 0.3 | −2.4 ± 0.5 | −2.4 ± 0.3 | −0.3 a ± 0.6 | −6.2 d ± 0.6 |
| PT [°] | 4.2 ± 1.2 | 3.9 ± 0.9 | 6.2 ± 0.8 | 6.0 ± 0.6 | 10.8 ± 0.7 | 10.8 ± 0.6 | 8.8 ± 0.8 | 8.8 ± 0.7 |
| PR [°] | −19.6 ± 1.4 | −11.5 b ± 2.8 | −18.5 ± 3.4 | −6.6 b ± 2.4 | −11.3 ± 1.8 | −9.9 b ± 1.4 | −12.4 ± 0.8 | −8.9 b ± 1.1 |
| Prosthesis | F1 | F2 | M1 | M2 | ||||
|---|---|---|---|---|---|---|---|---|
| ILE | ULE | ILE | ULE | ILE | ULE | ILE | ULE | |
| DFP | ||||||||
| AF [°] | 18.2 ± 0.8 | 18.8 ± 0.8 | 9.4 ± 0.3 | 20.0 b ± 0.9 | 17.2 c ± 0.5 | 19.8 b,c ± 0.6 | 13.5 a ± 0.3 | 11.4 ± 1.2 |
| KF [°] | 57.7 c ± 2.7 | 66.2 b ± 1.6 | 60.2 a ± 1.2 | 55.1 ± 1.6 | 56.4 ± 2.3 | 70.5 b ± 1.1 | 64.4 ± 0.9 | 67.6 b,c ± 1.1 |
| HF [°] | 58.2 a,c ± 1.2 | 52.5 ± 1.3 | 41.4 a ± 1.3 | 36.0 c ± 1.1 | 37.2 ± 0.8 | 40.9 b ± 1.3 | 46.3 a,c ± 0.8 | 42.6 c ± 1.0 |
| HA [°] | 12.5 c ± 0.9 | 17.1 b,c ± 0.9 | 14.9 a,c ± 1.0 | 11.2 ± 1.0 | 8.5 ± 0.7 | 11.0 b ± 0.6 | 5.5 a,c ± 0.6 | −0.7 ± 1.1 |
| HR [°] | 29.5 a ± 2.7 | 26.2 c ± 1.8 | 1.8 ± 0.7 | 5.7 b,c ± 0.9 | 2.4 ± 1.0 | 9.3 b ± 2.2 | −2.2 ± 0.8 | 21.7 b ± 1.2 |
| PO [°] | 1.4 c ± 0.5 | 7.2 b ± 0.5 | 4.9 a,c ± 0.9 | 3.2 ± 0.5 | 1.9 ± 0.3 | 3.0 b,c ± 0.4 | 7.3 b,c ± 0.6 | −1.0 ± 0.6 |
| PT [°] | 20.9 c ± 0.8 | 21.2 c ± 0.8 | 12.8 c ± 0.7 | 12.2 c ± 0.7 | 14.7 ± 0.5 | 14.6 ± 0.6 | 13.8 c ± 0.8 | 14.7 b,c ± 0.5 |
| PR [°] | 6.7 ± 1.4 | 20.7 b ± 2.8 | 4.5 ± 1.7 | 17.6 b ± 1.3 | 11.0 a ± 1.4 | 9.5 ± 1.8 | 8.0 ± 1.4 | 12.2 b,c ± 1.2 |
| FP | ||||||||
| AF [°] | 20.8 d ± 1.0 | 25.5 b,d ± 1.1 | 27.3 a,d ± 1.2 | 23.7 d ± 1.8 | 16.2 ± 0.9 | 18.9 b ± 1.1 | 13.2 ± 0.5 | 21.2 b,d ± 1.1 |
| KF [°] | 51.6 ± 2.6 | 63.6 b ± 2.5 | 61.3 a ± 0.9 | 55.8 ± 1.7 | 55.3 ± 1.8 | 66.8 b ± 17.1 | 64.7 a ± 2.1 | 52.2 ± 1.4 |
| HF [°] | 34.8 ± 1.4 | 34.7 d ± 1.1 | 39.6 a ± 0.8 | 29.7 ± 1.3 | 37.3 ± 0.6 | 40.4 b ± 3.8 | 41.3 a ± 1.2 | 38.4 ± 0.5 |
| HA [°] | 9.5 ± 0.9 | 11.5 b ± 0.3 | 10.8 ± 1.0 | 13.2 b,d ± 1.4 | 9.0 ± 0.9 | 10.1 b ± 2.9 | 3.3 a ± 0.6 | 0.4 d ± 1.0 |
| HR [°] | 35.1 a,d ± 10.2 | 16.8 ± 0.8 | 17.5 a,d ± 1.5 | −7.9 ± 3.0 | 4.4 d ± 2.3 | 12.2 b,d ± 14.0 | 34.2 a,d ± 1.8 | 29.4 d ± 1.5 |
| PO [°] | 0.0 ± 0.8 | 7.6 b ± 0.6 | 1.7 ± 0.6 | 4.2 b,d ± 0.5 | 2.2 d ± 0.3 | 2.6 b ± 0.5 | 6.4 a ± 0.5 | 1.0 d ± 0.9 |
| PT [°] | 9.9 ± 1.0 | 9.4 ± 1.2 | 9.5 ± 0.6 | 9.1 ± 0.6 | 15.1 ± 0.7 | 14.9 ± 0.6 | 12.1 ± 0.9 | 12.7 ± 0.5 |
| PR [°] | 11.6 d ± 1.6 | 20.0 b ± 2.9 | 7.4 d ± 2.7 | 20.2 b,d ± 3.2 | 10.6 ± 1.5 | 11.3 d ± 1.6 | 8.7 ± 1.3 | 11.5 b ± 0.7 |
| Prosthesis | F1 | F2 | M1 | M2 | ||||
|---|---|---|---|---|---|---|---|---|
| ILE | ULE | ILE | ULE | ILE | ULE | ILE | ULE | |
| DFP | ||||||||
| AF [°] | 14.0 ± 0.5 | 34.9 b,c ± 1.4 | 13.1 ± 0.7 | 21.7 b ± 1.4 | 17.0 c ± 0.6 | 25.9 b ± 1.3 | 17.9 c ± 0.4 | 30.6 b ± 2.1 |
| KF [°] | 34.3 ± 2.8 | 59.6 b,c ± 2.4 | 61.5 c ± 1.7 | 60.8 c ± 2.4 | 61.3 ± 2.3 | 63.7 ± 1.0 | 57.3 ± 1.4 | 61.8 b,c ± 1.6 |
| HF [°] | 44.1 a ± 2.1 | 38.6 ± 2.1 | 49.9 a,c ± 1.7 | 41.7 c ± 0.9 | 41.4 a ± 1.0 | 35.0 ± 1.9 | 45.5 ± 1.1 | 49.0 ± 1.2 |
| HA [°] | 15.8 a ± 1.2 | 8.7 ± 1.8 | 12.2 a,c ± 1.2 | 9.6 ± 0.6 | 9.0 ± 1.3 | 9.6 ± 0.7 | 8.2 ± 0.9 | 10.1 b ± 1.1 |
| HR [°] | 12.2 ± 2.5 | 22.5 b,c ± 2.0 | 8.6 ± 1.3 | 9.8 ± 1.0 | 16.7 ± 1.3 | 18.8 b ± 2.4 | 9.7 ± 1.2 | 15.4 b,c ± 1.7 |
| PO [°] | 8.8 c ± 0.7 | 8.8 c ± 0.5 | 8.3 a,c ± 1.0 | 7.6 c ± 0.6 | 4.8 ± 0.6 | 5.2 b ± 0.6 | 6.2 ± 0.5 | 6.3 ± 0.9 |
| PT [°] | 4.6 ± 1.0 | 4.8 ± 1.2 | 3.7 a ± 0.9 | 2.7 ± 0.6 | 3.9 ± 0.6 | 3.7 ± 0.6 | 2.6 ± 0.7 | 3.4 b ± 0.5 |
| PR [°] | 26.4 ± 2.5 | 26.9 ± 2.8 | 22.0 ± 2.0 | 23.2 ± 2.2 | 20.7 ± 2.7 | 20.4 ± 2.3 | 20.7 ± 1.8 | 20.5 ± 2.3 |
| FP | ||||||||
| AF [°] | 15.6 d ± 0.5 | 29.7 b ± 3.7 | 19.6 d ± 1.5 | 21.6 b ± 2.1 | 15.0 ± 1.8 | 26.9 b ± 5.1 | 13.6 ± 0.9 | 34.5 b,d ± 2.9 |
| KF [°] | 46.8 d ± 1.5 | 51.3 b ± 4.1 | 54.1 ± 2.2 | 54.2 ± 3.2 | 58.3 ± 2.8 | 64.0 b ± 2.2 | 69.6 a,d ± 2.5 | 53.8 ± 2.2 |
| HF [°] | 43.1 a ± 2.0 | 37.3 ± 1.7 | 47.4 a ± 1.9 | 38.0 ± 1.7 | 41.2 a ± 0.7 | 37.0 ± 4.8 | 50.1 d ± 2.2 | 52.4 d ± 1.4 |
| HA [°] | 18.5 a,d ± 1.6 | 13.0 d ± 0.9 | 9.9 ± 1.1 | 9.0 ± 1.0 | 8.9 ± 0.9 | 11.5 b,d ± 4.5 | 9.9 d ± 1.1 | 11.2 b,d ± 1.6 |
| HR [°] | 10.4 d ± 3.8 | 13.4 b ± 1.4 | 16.6 a,d ± 1.1 | 14.2 d ± 6.2 | 21.8 a,d ± 5.0 | 18.7 ± 3.0 | 15.6 a,d ± 2.3 | 10.7 ± 2.2 |
| PO [°] | 7.4 ± 1.0 | 7.3 ± 0.7 | 6.0 ± 0.9 | 5.9 ± 0.7 | 4.6 ± 0.5 | 5.0 b ± 0.5 | 6.8 d ± 0.9 | 7.2 d ± 1.2 |
| PT [°] | 5.8 d ± 0.9 | 5.5 d ± 0.7 | 3.4 ± 0.5 | 3.1 d ± 0.6 | 4.3 ± 0.7 | 4.1 ± 0.6 | 3.4 d ± 0.6 | 3.8 b,d ± 0.5 |
| PR [°] | 31.2 d ± 1.8 | 31.5 d ± 3.5 | 25.9 d ± 2.9 | 26.9 d ± 5.0 | 21.9 ± 1.9 | 21.2 ± 2.5 | 21.1 ± 1.6 | 20.4 ± 1.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murawa, M.; Otworowski, J.; But, S.; Kabacinski, J.; Kubaszewski, L.; Gramala, A. Symmetry Function in Trans-Tibial Amputees Gait Supplied with the New Concept of Affordable Dynamic Foot Prosthesis—Case Study. Symmetry 2023, 15, 1595. https://doi.org/10.3390/sym15081595
Murawa M, Otworowski J, But S, Kabacinski J, Kubaszewski L, Gramala A. Symmetry Function in Trans-Tibial Amputees Gait Supplied with the New Concept of Affordable Dynamic Foot Prosthesis—Case Study. Symmetry. 2023; 15(8):1595. https://doi.org/10.3390/sym15081595
Chicago/Turabian StyleMurawa, Michal, Jakub Otworowski, Sebastian But, Jaroslaw Kabacinski, Lukasz Kubaszewski, and Adam Gramala. 2023. "Symmetry Function in Trans-Tibial Amputees Gait Supplied with the New Concept of Affordable Dynamic Foot Prosthesis—Case Study" Symmetry 15, no. 8: 1595. https://doi.org/10.3390/sym15081595
APA StyleMurawa, M., Otworowski, J., But, S., Kabacinski, J., Kubaszewski, L., & Gramala, A. (2023). Symmetry Function in Trans-Tibial Amputees Gait Supplied with the New Concept of Affordable Dynamic Foot Prosthesis—Case Study. Symmetry, 15(8), 1595. https://doi.org/10.3390/sym15081595







