Design and Analysis of a Supine Ankle Rehabilitation Robot for Early Stroke Recovery
Abstract
1. Introduction
- (1)
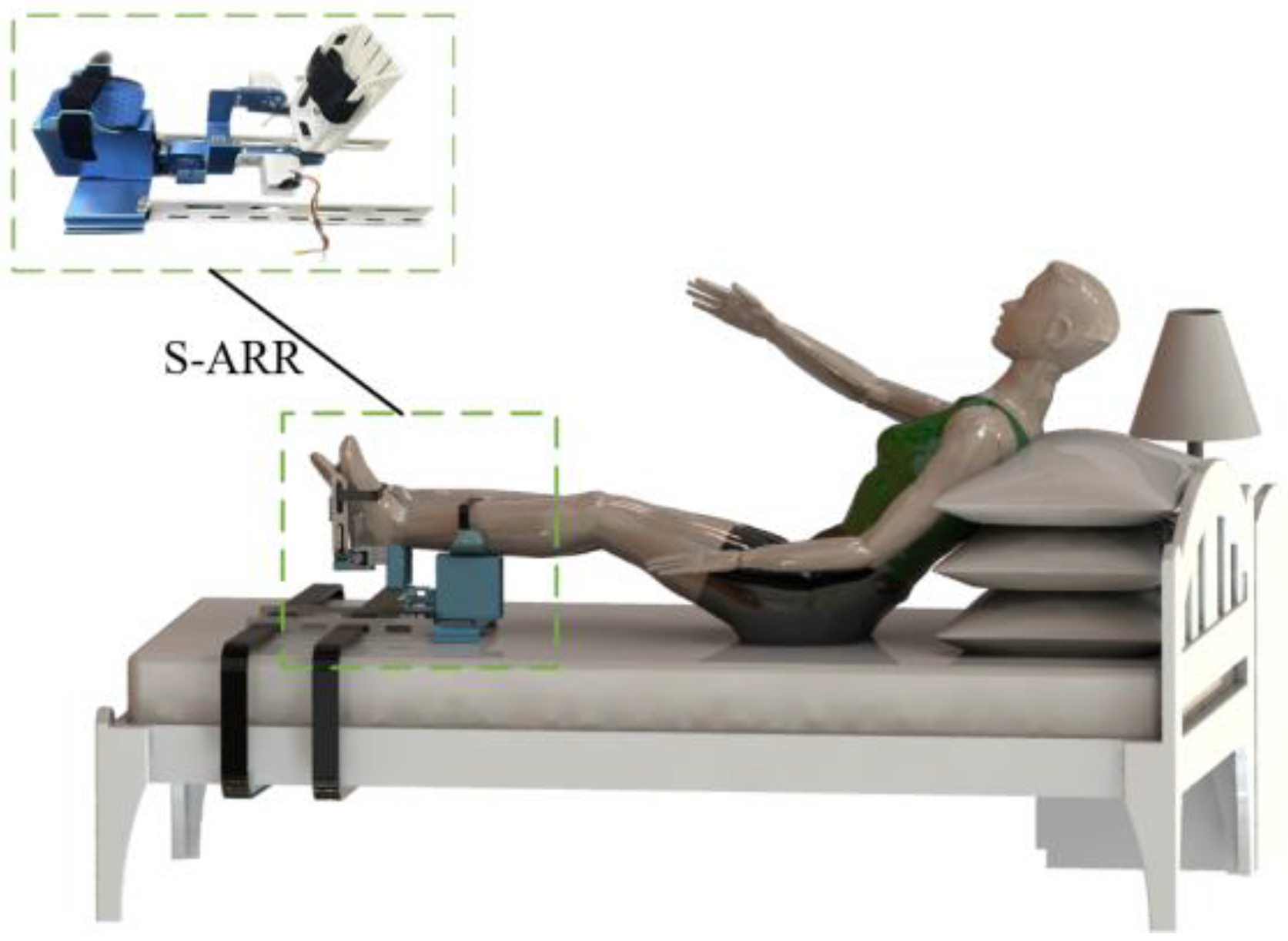
- Design a structurally simple, compact, and cost-effective supine ankle rehabilitation robot that can be conveniently moved and integrated with the patient’s bed for fixed positioning, enabling both seated and supine rehabilitation training.
- (2)
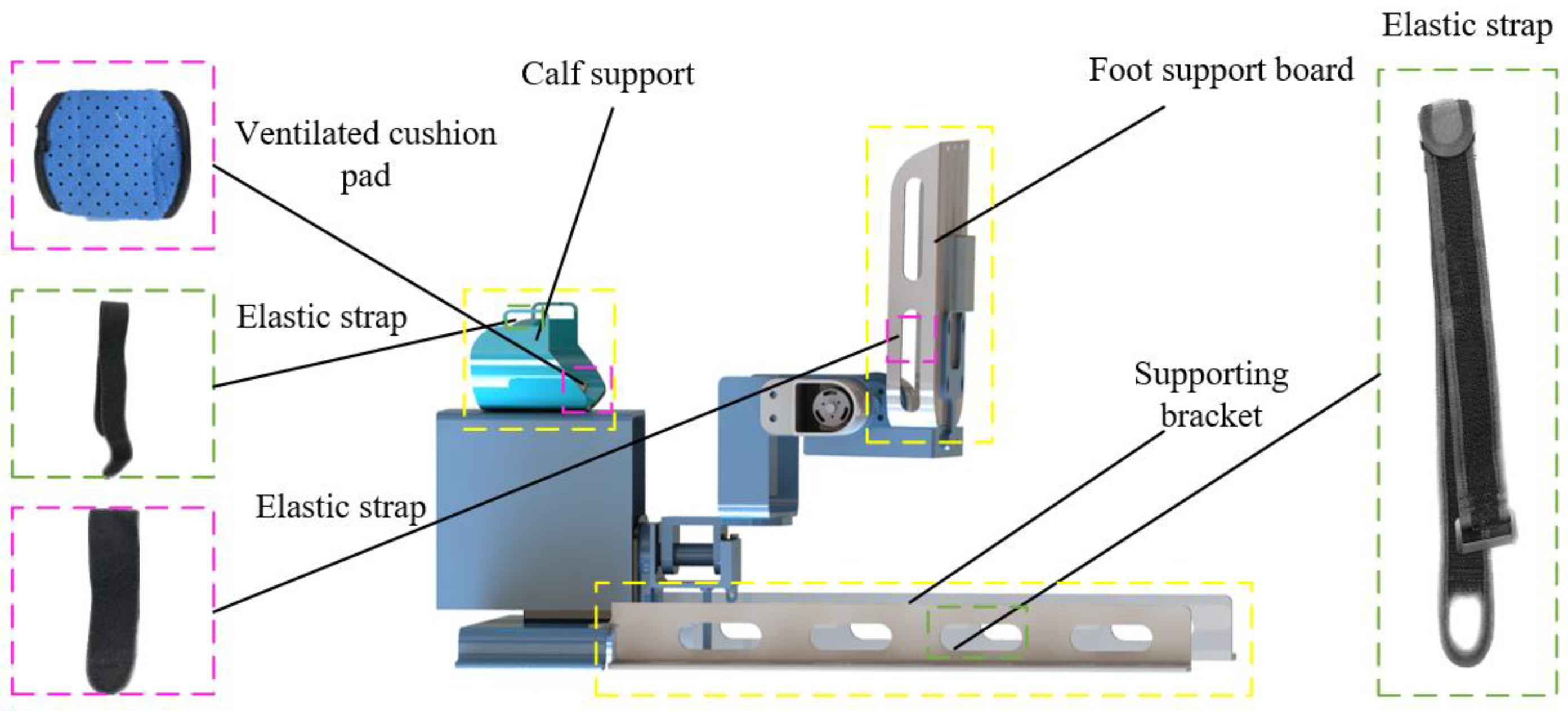
- Adjustable design: Considering the size differences among individuals, the robot can incorporate adjustable features. For example, the length and position of the lower leg can be adjustable, and different-sized footplates can be replaced to accommodate the needs of different individuals.
- (3)
- Functional variability: The robot has variable functional modules to adapt to different rehabilitation tasks and training requirements. For instance, the robot can adjust the range of motion limitation device to achieve different rehabilitation training goals.
- (4)
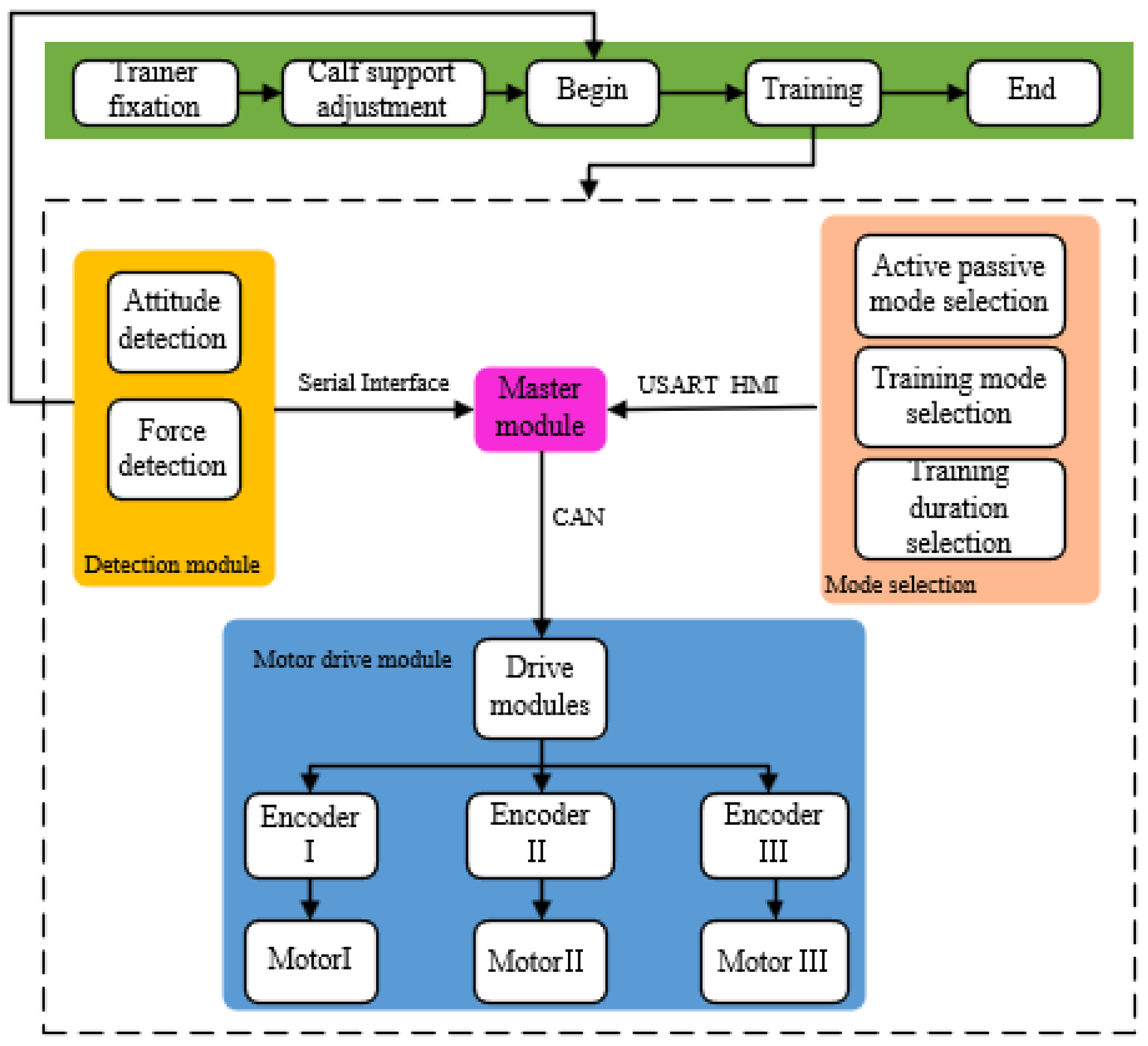
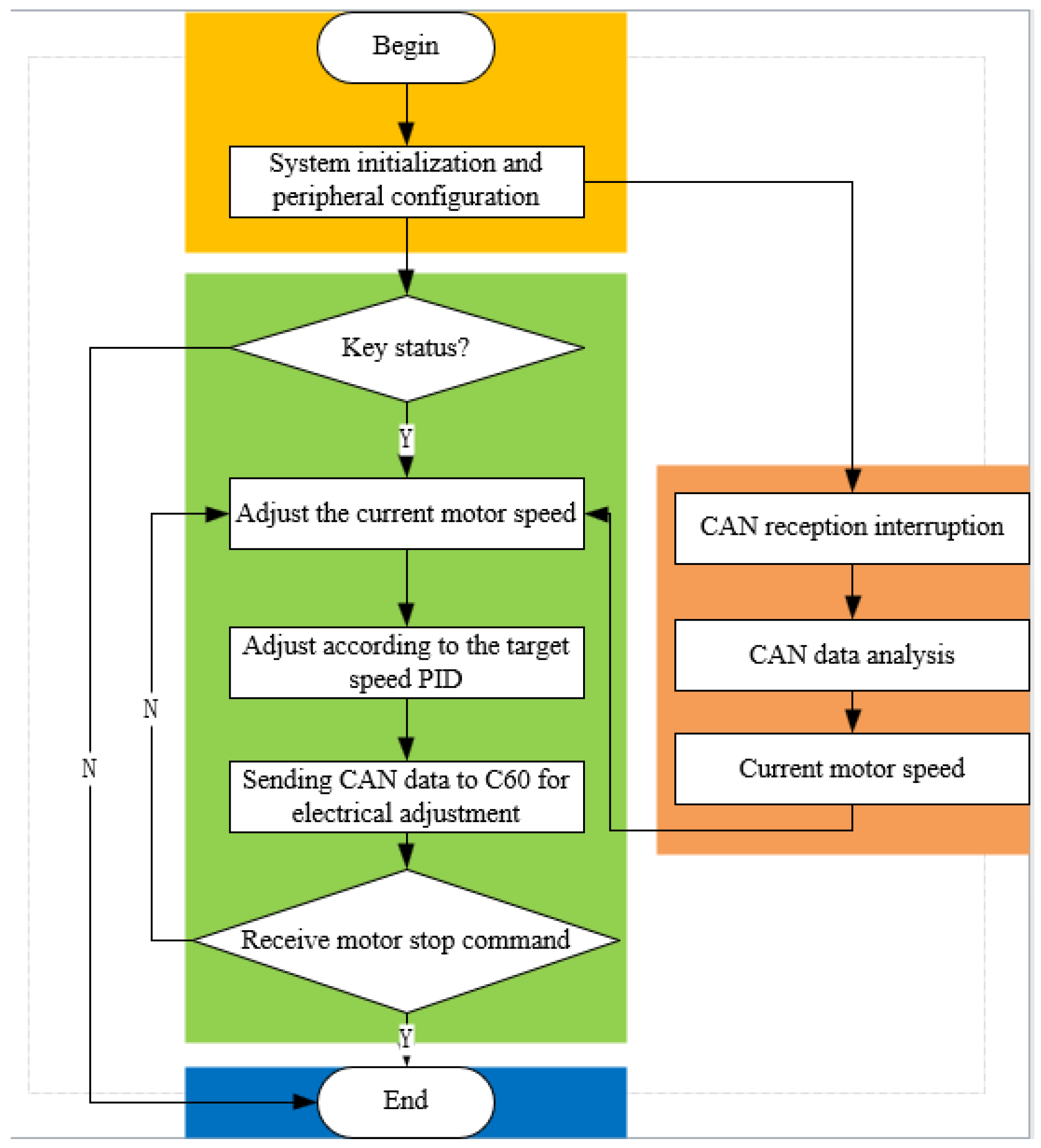
- The design includes a joint range of motion and rehabilitation motion experiment to restore ankle joint mobility. Additionally, a control system scheme for S-ARR is proposed to provide patients with more effective rehabilitation training.
2. Materials and Methods
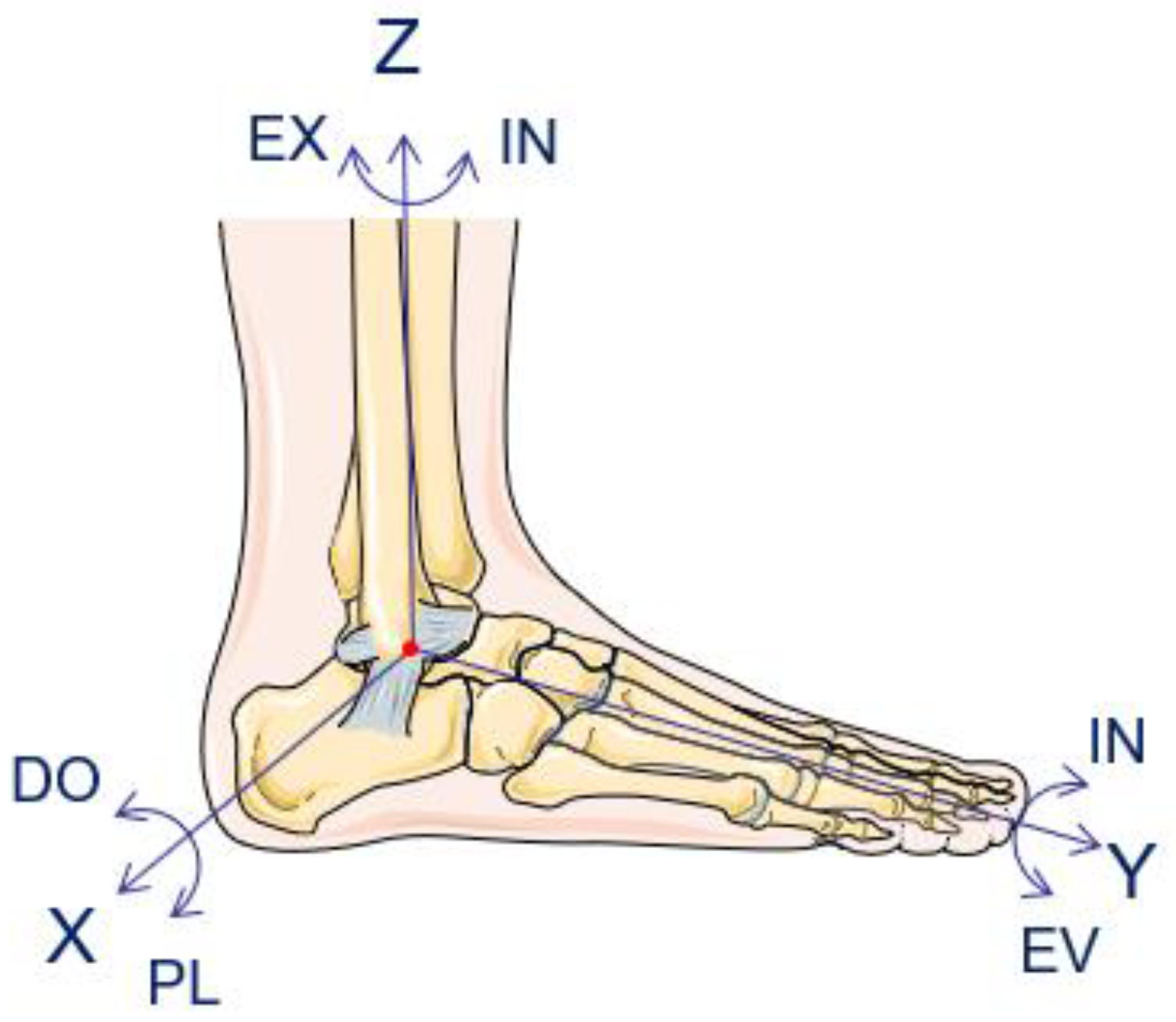
2.1. Analysis of Human Ankle Joint Movement Characteristics
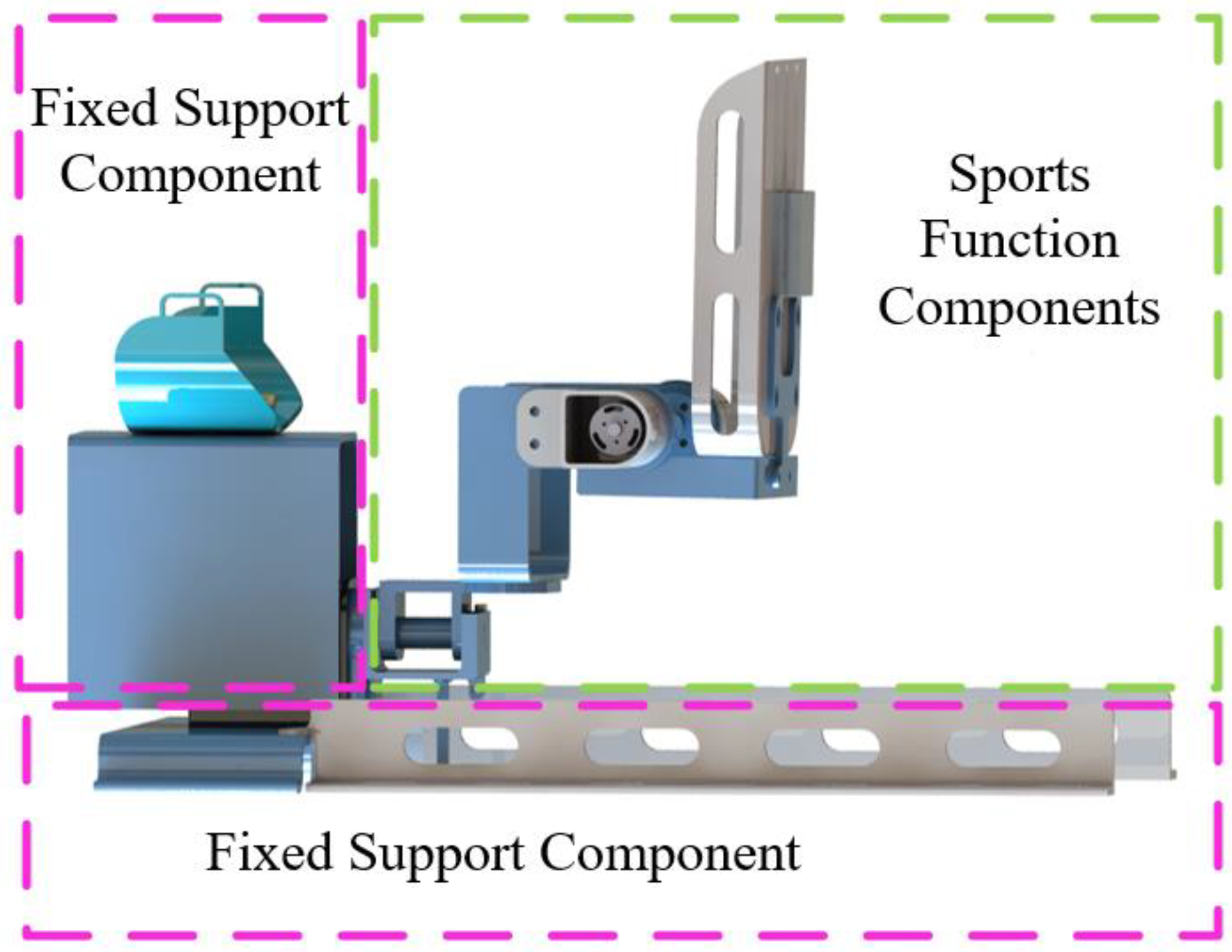
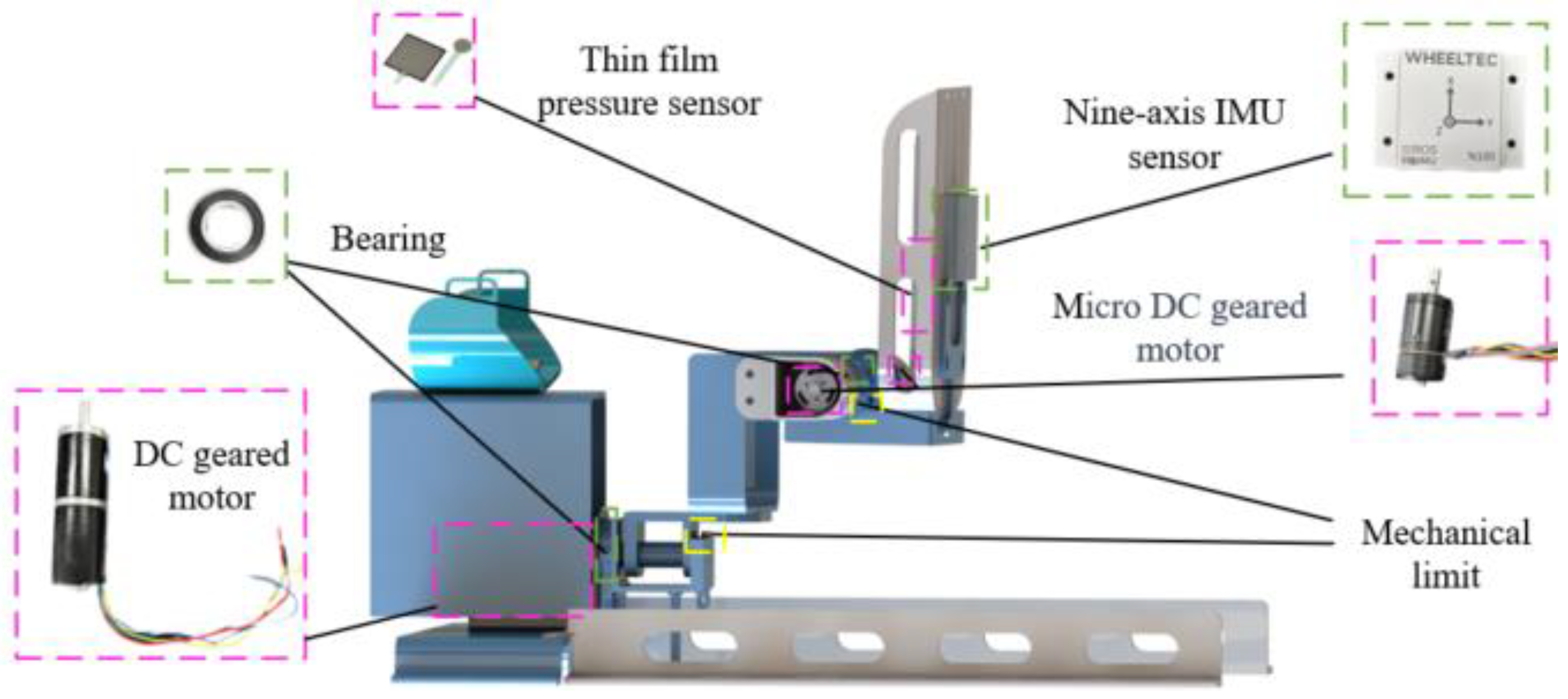
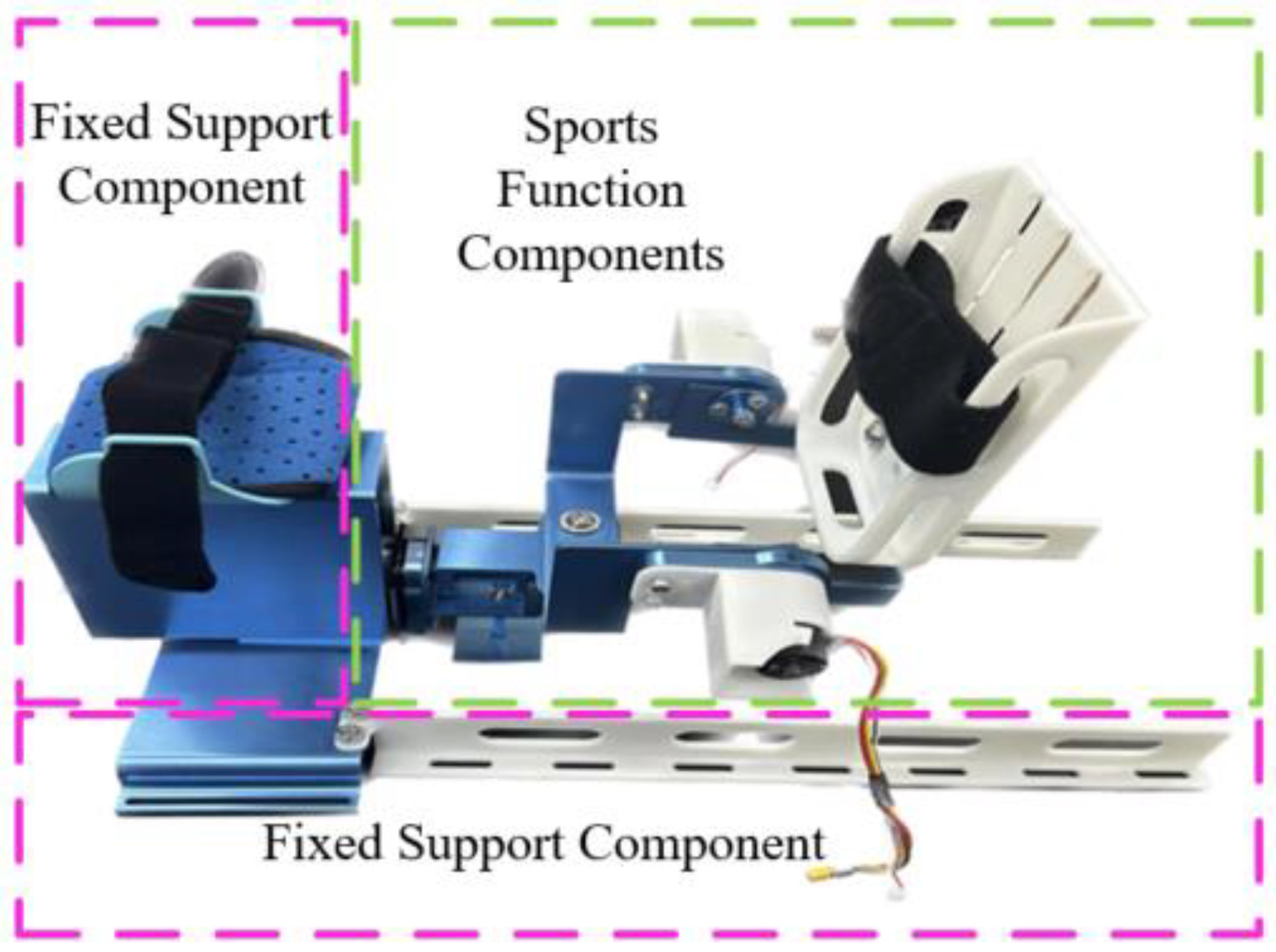
2.2. Mechanical Design
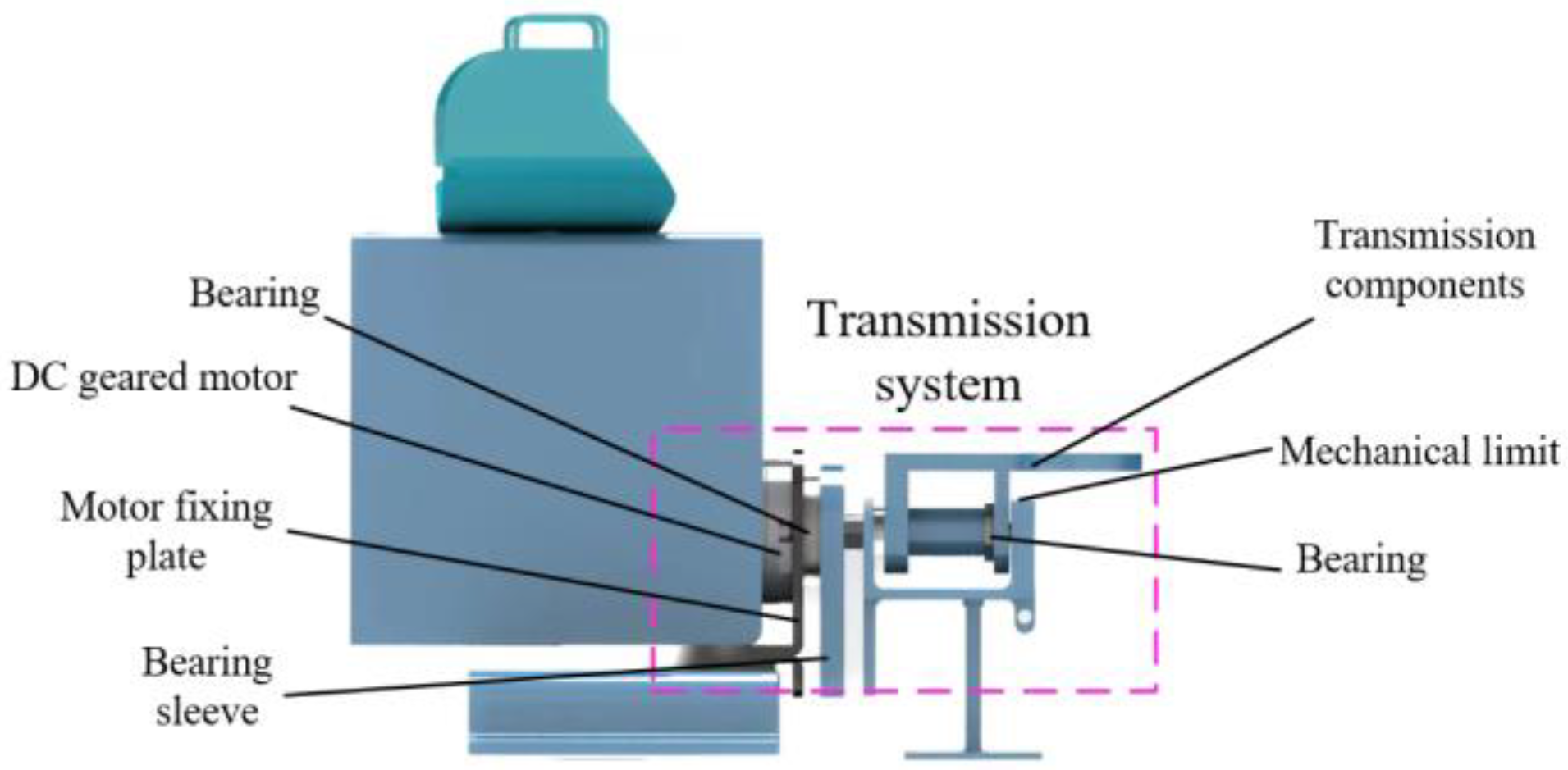
2.2.1. Motion Function Component Design
2.2.2. Fixed Support Component Design
2.2.3. Mechanical Limitation and Adjustable Structure Design
2.3. Procedure and Control System Design
3. Rehabilitation Robot Theoretical Foundations
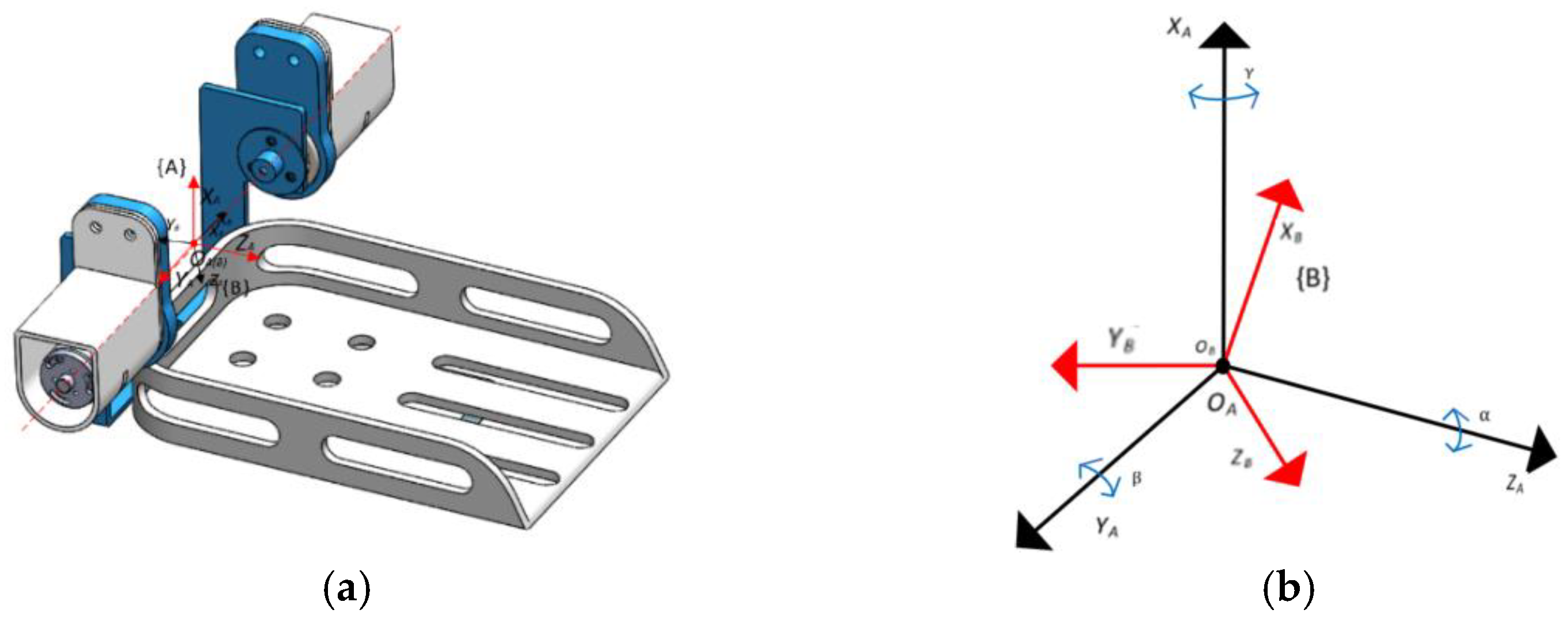
3.1. Kinematic Modeling
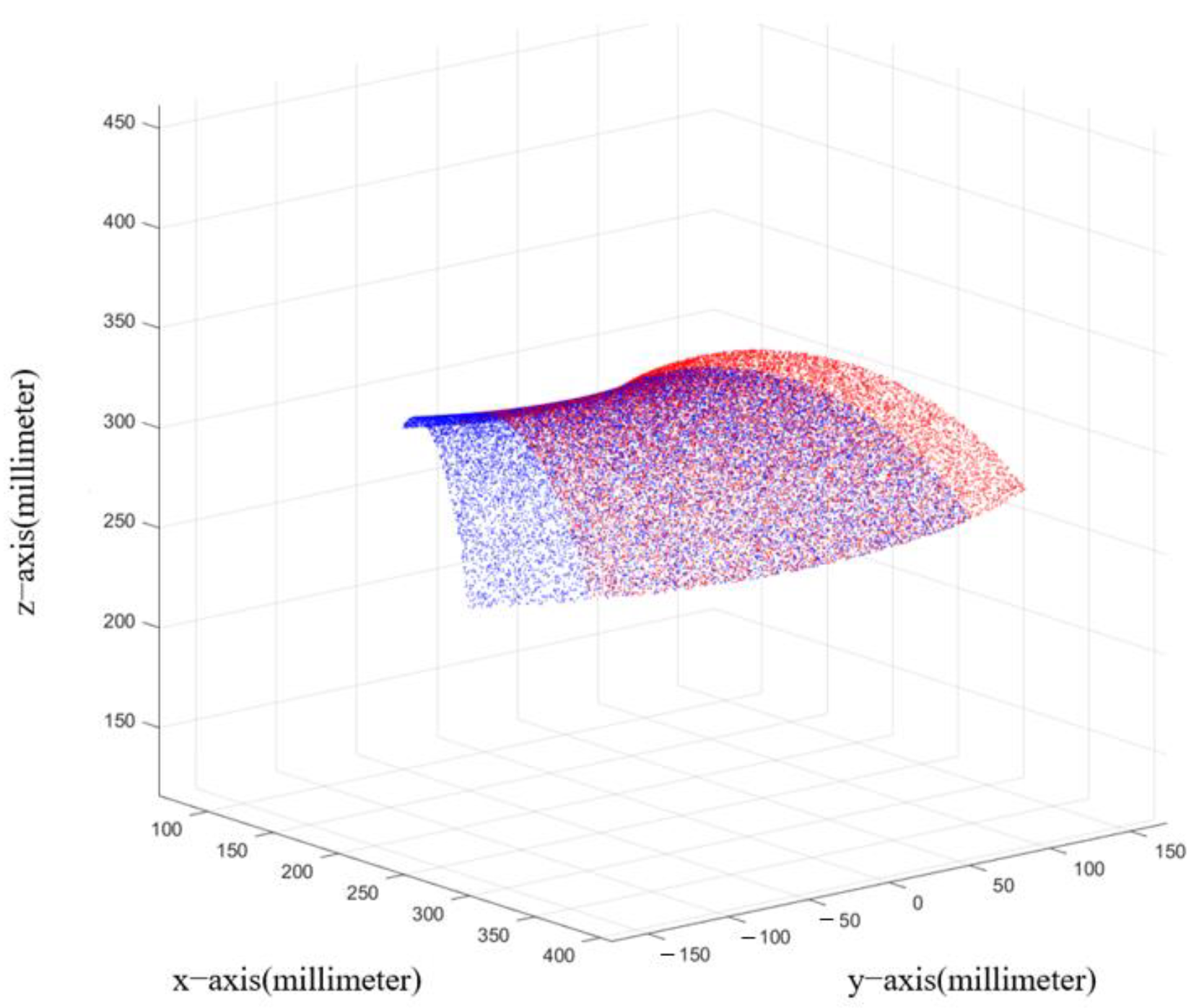
3.2. Workspace Analysis
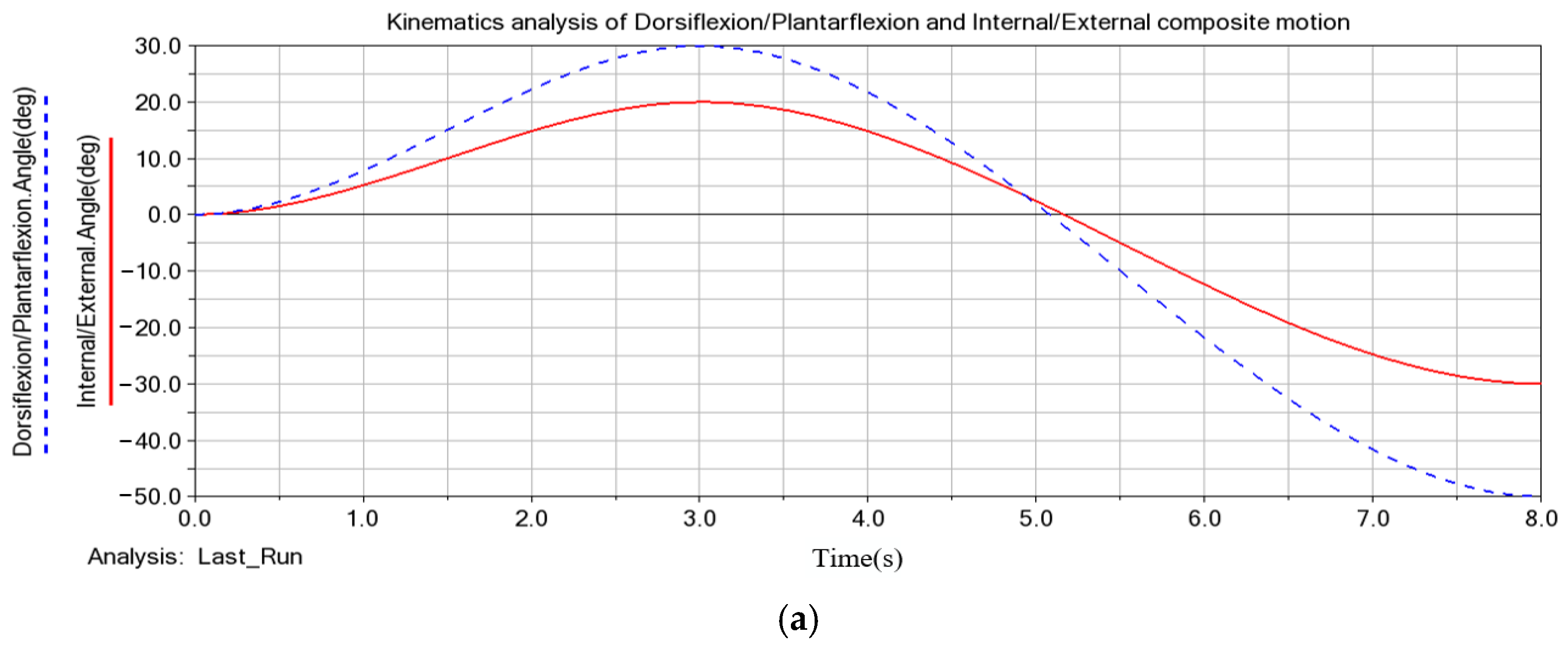
3.3. Robot Motion Performance Simulation
4. System Validation and Performance Analysis
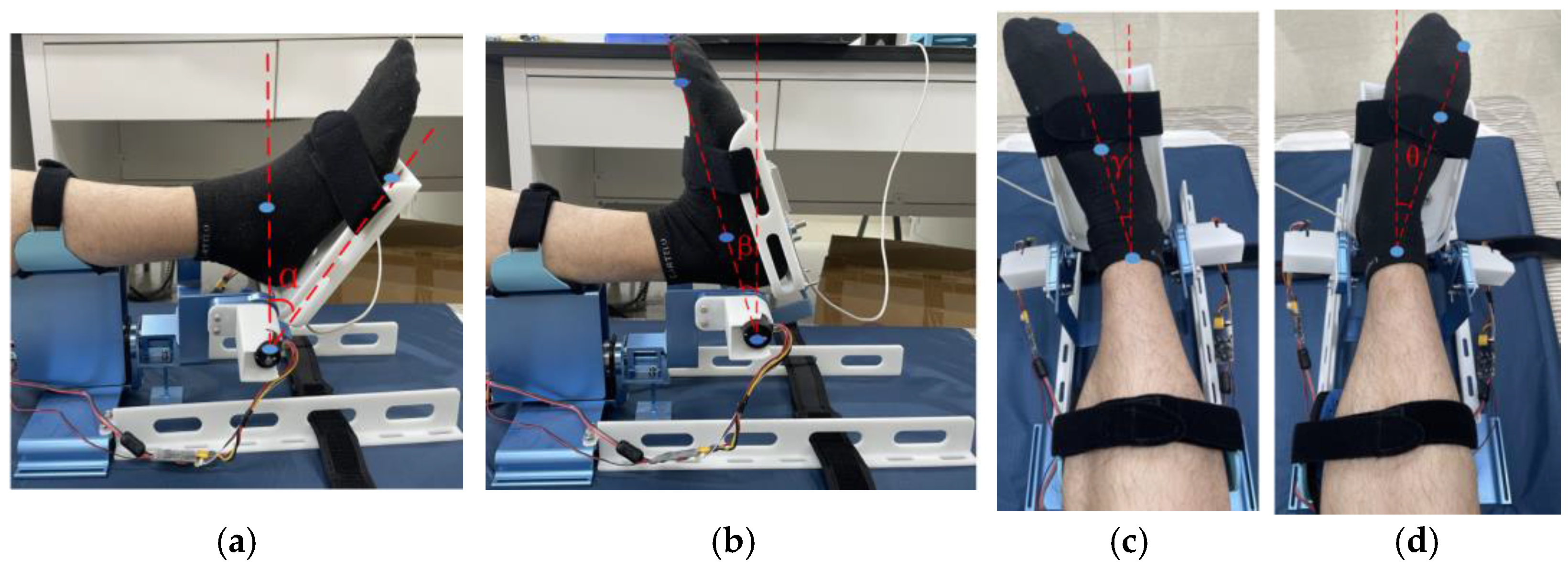
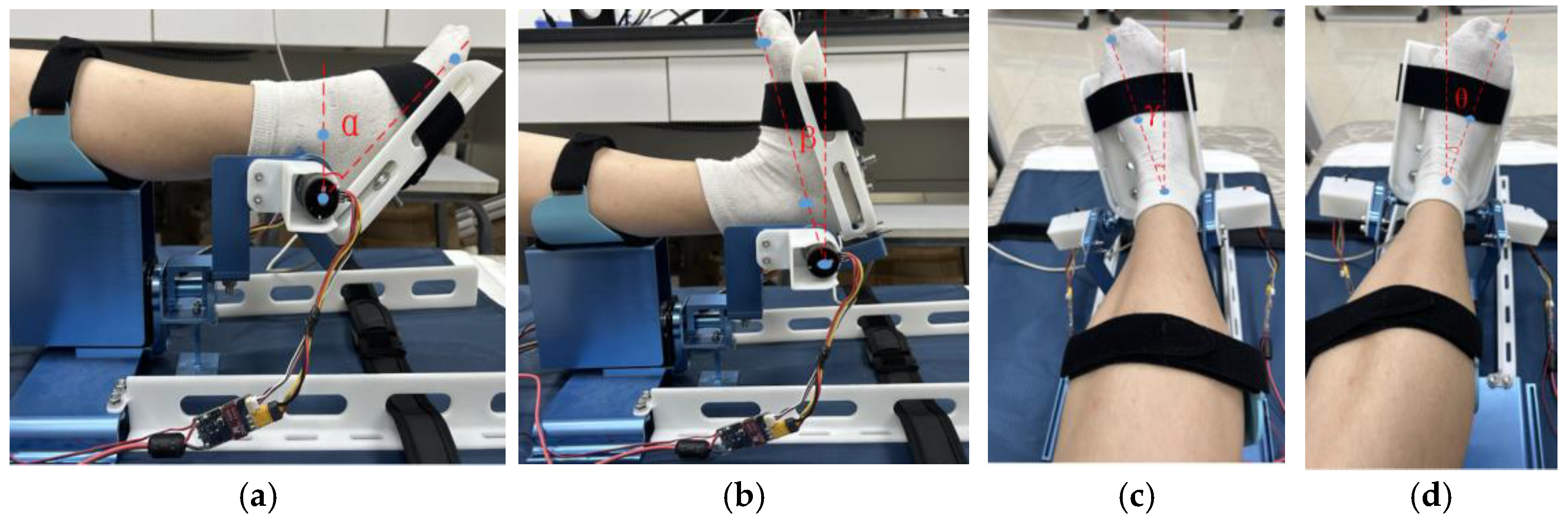
4.1. Joint Range of Motion Measurement Experiment
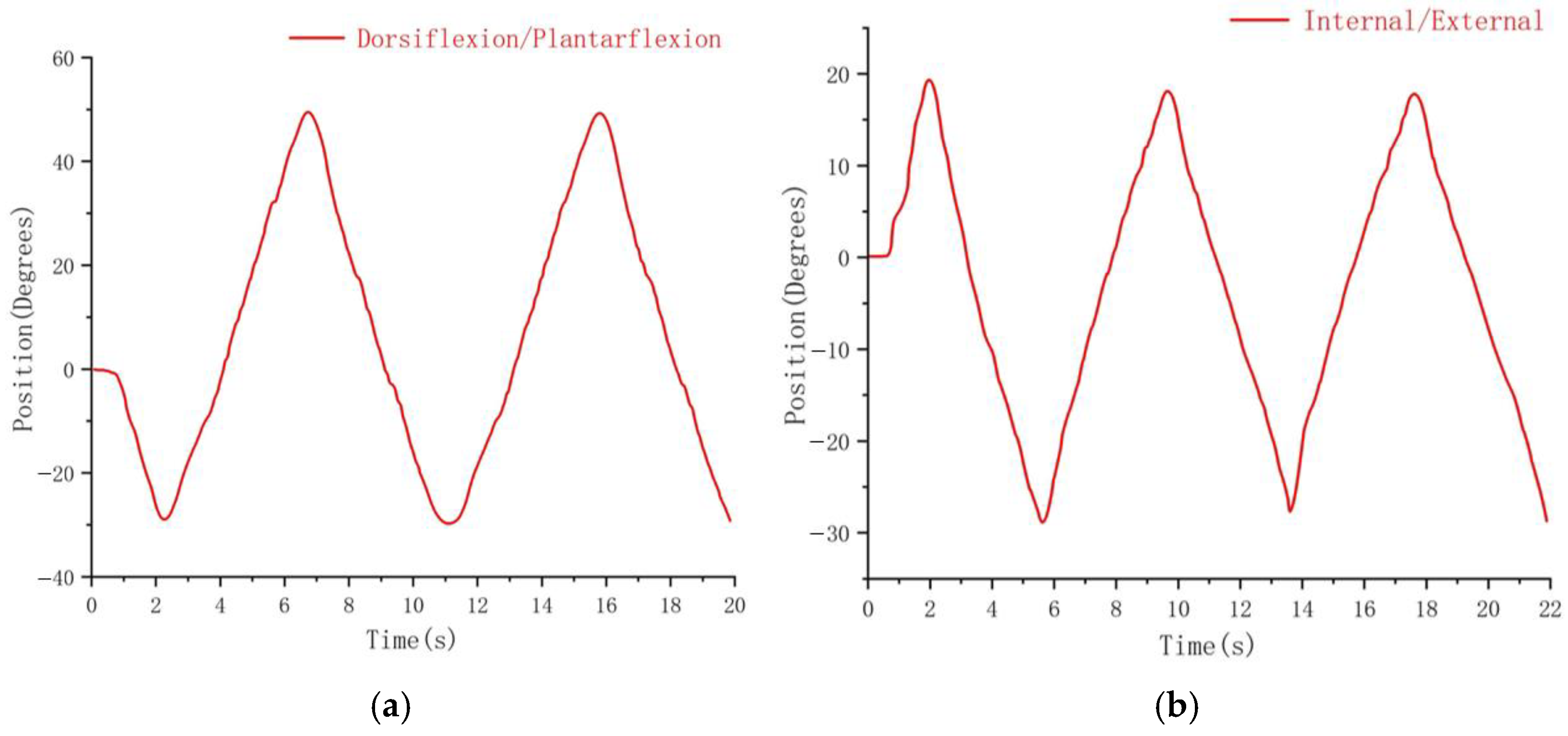
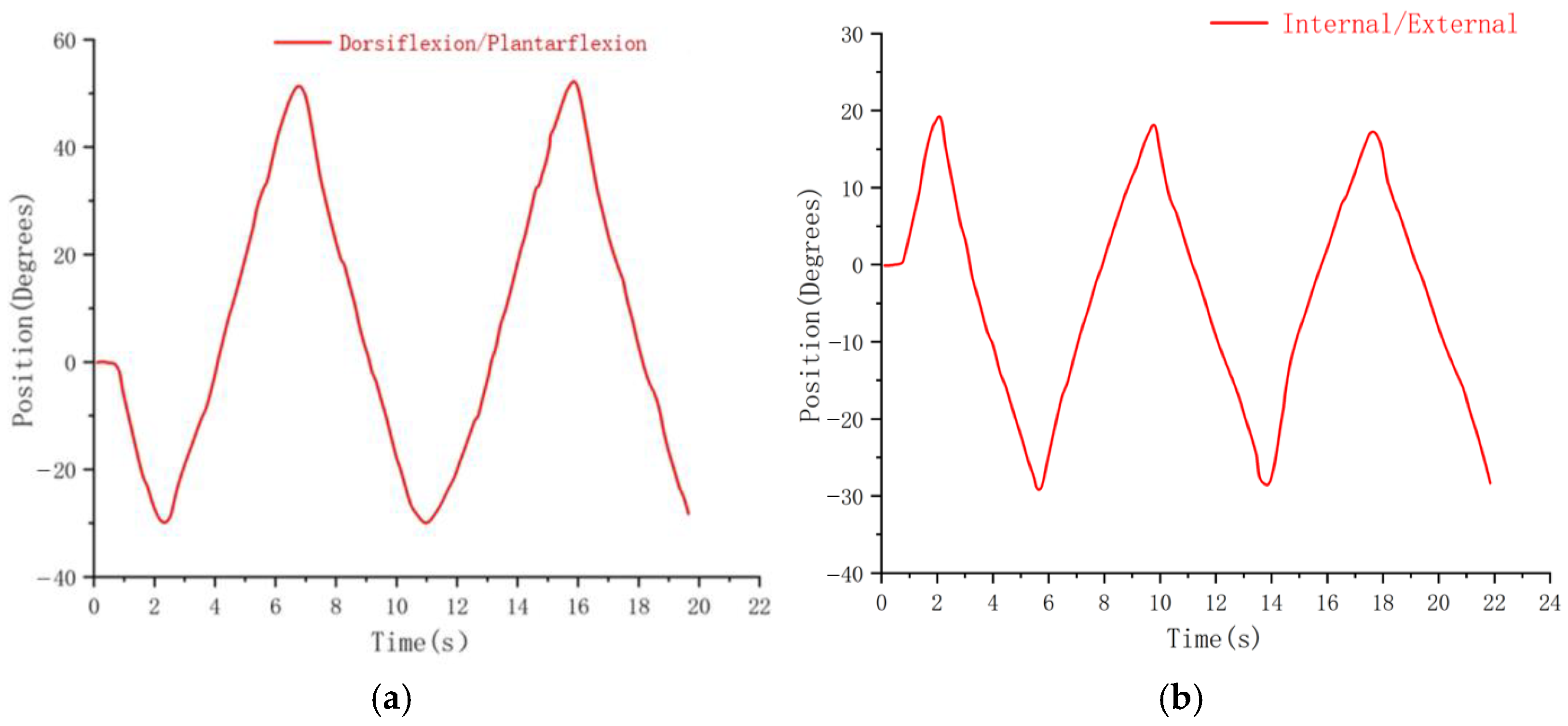
4.2. Rehabilitation Training Experiment
5. Conclusions and Future Work
- (1)
- The kinematic model of the robot was established, and simulation analysis was conducted on the ankle joint rotation angle, angular velocity, and angular acceleration curves. The simulation analysis of the S-ARR workspace demonstrated its ability to meet the training needs of patients. The analysis confirmed the rationality and feasibility of the mechanism design.
- (2)
- A prototype system was constructed, and joint range of motion measurement experiments were conducted. The results showed that the measured joint angles were slightly smaller than the preset values (approximately 2°). The fluctuations in the measured joint range of motion were within an acceptable range, indicating that the prototype could meet the rehabilitation requirements. The rehabilitation training experiments demonstrated the smooth operation of the robot, with the maximum angle slightly smaller than the specified angle, achieving satisfactory performance for supine rehabilitation training.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Hamidi, S. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef]
- Markus, H.S. Reducing disability after stroke. Int. J. Stroke 2022, 17, 249–250. [Google Scholar] [CrossRef]
- Grefkes, C.; Fink, G.R. Recovery from stroke: Current concepts and futures perspectives. Neurol. Res. Pract. 2020, 2, 17. [Google Scholar] [CrossRef]
- Gassert, R.; Dietz, V. Rehabilitation robots for the treatment of sensorimotor deficits: A neurophysiological perspective. J. NeuroEng. Rehabil. 2018, 15, 46. [Google Scholar] [CrossRef]
- Shi, M.; Yang, C.; Zhang, D. A novel human-machine collaboration model of an ankle joint rehabilitation robot driven by EEG signals. Math. Probl. Eng. 2021, 2021, 5564235. [Google Scholar] [CrossRef]
- Flansbjer, U.B.; Holmbck, A.M.; Downham, D.; Patten, C.; Lexell, J. Reliability of gait performance in men and women with hemiparesis after stroke. J. Rehabil. Med. 2005, 37, 75–82. [Google Scholar]
- Dao, M.D.; Tran, X.T.; Pham, D.P.; Ngo, Q.A.; Le, T.T.T. Study on the ankle rehabilitation device. Arch. Mech. Eng. 2022, 69, 147–163. [Google Scholar]
- Li, J.; Zuo, S.; Zhang, L.; Zhang, L.; Dong, M.; Zhang, Z.; Tao, C.; Ji, R. Mechanical design and performance analysis of a novel parallel robot for ankle rehabilitation. J. Mech. Robot. 2020, 12, 051007. [Google Scholar] [CrossRef]
- Jiang, J.; Min, Z.; Huang, Z.; Ma, X.; Chen, Y.; Yu, X. Research Status on Ankle Rehabilitation Robot. Recent Pat. Mech. Eng. 2019, 12, 104–124. [Google Scholar] [CrossRef]
- Engineering, J.H. Retracted: Design and Workspace Analysis of a Parallel Ankle Rehabilitation Robot (PARR). J. Healthc. Eng. 2021, 2021, 7345780. [Google Scholar] [CrossRef]
- Farjadian, A.B.; Nabian, M.; Hartman, A.; Yen, S.C. Vi-RABT: A Platform-Based Robot for Ankle and Balance Assessment and Training. J. Med. Biol. Eng. 2018, 38, 556–572. [Google Scholar] [CrossRef]
- Cioi, D.; Kale, A.; Burdea, G.; Engsberg, J.; Janes, W.; Ross, S. Ankle control and strength training for children with cerebral palsy using the Rutgers ankle CP: A case study. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics (ICORR), ETH Zurich, Zurich, Switzerland, 27 June–1 July 2011; pp. 654–659. [Google Scholar]
- Lei, Y. Development of Ankle Rehabilitation Training Device and Evaluation of Rehabilitation Effect. Master’s Thesis, Dalian University of Technology, Dalian, China, 2021. [Google Scholar]
- Mayetin, U.; Kucuk, S. Design and Experimental Evaluation of a Low Cost, Portable, 3-DOF Wrist Rehabilitation Robot with High Physical Human–Robot Interaction. J. Intell. Robot. Syst. 2022, 106, 65. [Google Scholar] [CrossRef]
- Curcio, E.M.; Carbone, G. Mechatronic design of a robot for upper limb rehabilitation at home. J. Bionic Eng. 2021, 18, 857–871. [Google Scholar] [CrossRef]
- Reza, M.; Sally, E.; Catherine, C.; Anna, S.; Aseem, J.; Emmanuel, W.; Kevin, C. Robotically assisted ankle rehabilitation for pediatrics. In Proceedings of the 6th IEEE RAS/EMBS International Conference on Biomedical Robotics and Bio Mechatronics, Bio Rob 2016, Singapore, 26–29 June 2016; pp. 612–616. [Google Scholar]
- Kevin, C.; Reza, M.; Tyler, S.; Hadi, F.T.; Catherine, C.; Staci, K.; Justine, B.; Sara, A.; Manon, S.; Sarah, H.E. Pedbothome: Robotically-assisted ankle rehabilitation system for children with cerebral palsy. In Proceedings of the 16th IEEE International Conference on Rehabilitation Robotics, ICORR 2019, Toronto, ON, Canada, 24–28 June 2019; pp. 13–20. [Google Scholar]
- Lim, F.M.; Ruyi, F.; Goh, K.S.; Mok, Q.L.; Tan, B.H.J.; Toh, S.L.; Yu, H. Supine Gait Training Device for Stroke Rehabilitation–Design of a Compliant Ankle Orthosis. In Proceedings of the 15th International Conference on Biomedical Engineering, ICBME 2013, Singapore, 4–7 December 2013; pp. 512–515. [Google Scholar]
- Li, J.; Fang, Q.; Dong, M.; Rong, X.; Jiang, L.; Jiao, R. Reconfigurable Muscle Strength Training Robot with Multi-mode Training for 17 Joint Movements. J. Bionic Eng. 2023, 20, 212–224. [Google Scholar] [CrossRef]
- Tommaso, P.; Ciaran, O.; Lucas, G.; Tazzy, C.; Sarah, M.; Kristin, N.; Cameron, H.; David, L.; Sabrina, P.; Conor, W. Restoring arm function with a soft robotic wearable for individuals with amyotrophic lateral sclerosis. Sci. Transl. Med. 2023, 15, eadd1504. [Google Scholar]
- Panagiotis, P.; Zheng, W.; Kevin, C.G.; Robert, J.W.; Conor, J.W. Soft robotic glove for combined assistance and at-home rehabilitation. Robot. Auton. Syst. 2015, 73, 135–143. [Google Scholar]
- Zachary, Y.; Nicholas, K.; Christina, C.M.; Devon, R.; Shane, K.M.; Madison, B.E.; Richard, F.W.; Jacob, S.; Christoph, K. Design of a High-Speed Prosthetic Finger Driven by Peano-HASEL Actuators. Front. Robot. AI 2020, 7, 586216. [Google Scholar]
- Zhang, M.; Cao, J.; Zhu, G.; Miao, Q.; Zeng, X.; Xie, S. Reconfigurable workspace and torque capacity of a compliant ankle rehabilitation robot (CARR). Robot. Auton. Syst. 2017, 98, 213–221. [Google Scholar] [CrossRef]
- Gallagher, J.F.; Sivan, M.; Levesley, M. Making Best Use of Home-Based Rehabilitation Robots. Appl. Sci. 2022, 12, 1996. [Google Scholar] [CrossRef]
- Yu, H.; Zheng, S.; Wu, J.; Sun, L.; Chen, Y.; Zhang, S.; Qin, Z. A New Single-Leg Lower-Limb Rehabilitation Robot: Design, Analysis and Experimental Evaluation. Machines 2023, 11, 447. [Google Scholar] [CrossRef]
- Khan, M.A.; Saibene, M.; Das, R.; Brunner, I.; Puthusserypady, S. Emergence of flexible technology in developing advanced systems for post-stroke rehabilitation: A comprehensive review. J. Neural Eng. 2021, 18, 061003. [Google Scholar] [CrossRef] [PubMed]
- Meng, W.; Liu, Q.; Zhou, Z.; Ai, Q. Active interaction control applied to a lower limb rehabilitation robot by using EMG recognition and impedance model. Ind. Robot-Int. J. Robot. Res. Appl. 2014, 41, 465–479. [Google Scholar] [CrossRef]
- Sheng, B.; Tang, L.; Moosman, O.M.; Deng, C.; Xie, S.; Zhang, Y. Development of a biological signal-based evaluator for robot-assisted upper-limb rehabilitation: A pilot study. Australas. Phys. Eng. Sci. Med. 2019, 42, 789–801. [Google Scholar] [PubMed]
- Zhou, J.; Yang, S.; Xue, Q. Lower limb rehabilitation exoskeleton robot: A review. Adv. Mech. Eng. 2021, 13, 16878140211011862. [Google Scholar] [CrossRef]
- Bernhardt, J.; Indredavik, B.; Langhorne, P. When Should Rehabilitation Begin after Stroke? Int. J. Stroke 2013, 8, 5–7. [Google Scholar] [CrossRef]
- Coleman, E.R.; Moudgal, R.; Lang, K.; Hyacinth, H.I.; Awosika, O.O.; Kissela, B.M.; Feng, W.W. Early Rehabilitation After Stroke: A Narrative Review. Curr. Atheroscler. Rep. 2017, 19, 59. [Google Scholar]
- Sun, Z.; Wang, C.; Wei, J.; Xia, J.; Wang, T.; Liu, Q.; Duan, L.; Wang, Y.; Long, J. Kinematics and Dynamics Analysis of a Novel Ankle Rehabilitation Robot. In Proceedings of the 2019 IEEE 9th Annual International Conference on CYBER Technology in Automation, Control, and Intelligent Systems (CYBER), Suzhou, China, 29 July–2 August 2019; pp. 1404–1409. [Google Scholar]







| Features | S-ARR | vi-RABT | Device [7] | CARR | Trainer [13] |
|---|---|---|---|---|---|
| Type | Platform-based | Platform-based | Platform-based | Platform-based | Platform-based |
| Size | Little | Little | Moderate | Moderate | Moderate |
| Single foot/ Double foot | Single | Single | Single | Single | Double |
| Driving method | Motor drive | Motor drive | Motor drive | Flexible drive | Motor drive |
| Posture | Sitting and lying | Sitting | Sitting | Sitting | Lying |
| Usage patterns | Combining with the bed | Fixed Position | Fixed seat | Fixed Position | Combining with the bed |
| Mobility | Easy | Easy | Harder | Harder | Easy |
| Motion | Angle Range (°) |
|---|---|
| Internal | 0~20 |
| External | 0~30 |
| Dorsiflexion | 0~30 |
| Plantarflexion | 0~50 |
| Inversion | 0~40 |
| Eversion | 0~30 |
| ID | Gender | Age | Height | Weight |
|---|---|---|---|---|
| 1 | Male | 25 | 175 cm | 60 kg |
| 2 | Female | 25 | 160 cm | 42 kg |
| 3 | Male | 26 | 180 cm | 65 kg |
| Angle | 1 | 2 | 3 | 4 | 5 | Mean |
|---|---|---|---|---|---|---|
| α | 49.5 | 49.7 | 49.2 | 48.8 | 49.3 | 49.3 |
| β | 29.4 | 28.7 | 29.6 | 28.8 | 29.6 | 29.2 |
| γ | 19.8 | 19.6 | 19.2 | 18.5 | 19.4 | 19.3 |
| θ | 28.8 | 29.7 | 28.9 | 29.0 | 29.3 | 29.1 |
| Angle | 1 | 2 | 3 | 4 | 5 | Mean |
|---|---|---|---|---|---|---|
| α | 48.7 | 49.3 | 49.4 | 48.6 | 48.5 | 48.9 |
| β | 28.4 | 29.2 | 28.5 | 28.9 | 29.5 | 28.9 |
| γ | 19.2 | 18.7 | 18.5 | 18.3 | 19.0 | 18.7 |
| θ | 28.4 | 29.0 | 28.6 | 28.3 | 28.5 | 28.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meng, Q.; Liu, G.; Xu, X.; Meng, Q.; Yu, H. Design and Analysis of a Supine Ankle Rehabilitation Robot for Early Stroke Recovery. Machines 2023, 11, 787. https://doi.org/10.3390/machines11080787
Meng Q, Liu G, Xu X, Meng Q, Yu H. Design and Analysis of a Supine Ankle Rehabilitation Robot for Early Stroke Recovery. Machines. 2023; 11(8):787. https://doi.org/10.3390/machines11080787
Chicago/Turabian StyleMeng, Qingyun, Guanxin Liu, Xin Xu, Qiaoling Meng, and Hongliu Yu. 2023. "Design and Analysis of a Supine Ankle Rehabilitation Robot for Early Stroke Recovery" Machines 11, no. 8: 787. https://doi.org/10.3390/machines11080787
APA StyleMeng, Q., Liu, G., Xu, X., Meng, Q., & Yu, H. (2023). Design and Analysis of a Supine Ankle Rehabilitation Robot for Early Stroke Recovery. Machines, 11(8), 787. https://doi.org/10.3390/machines11080787








