Update on Statin Treatment in Patients with Neuropsychiatric Disorders
Abstract
:1. Introduction
2. Pharmacological Mechanism of Statins in Neuropsychiatric Disorders
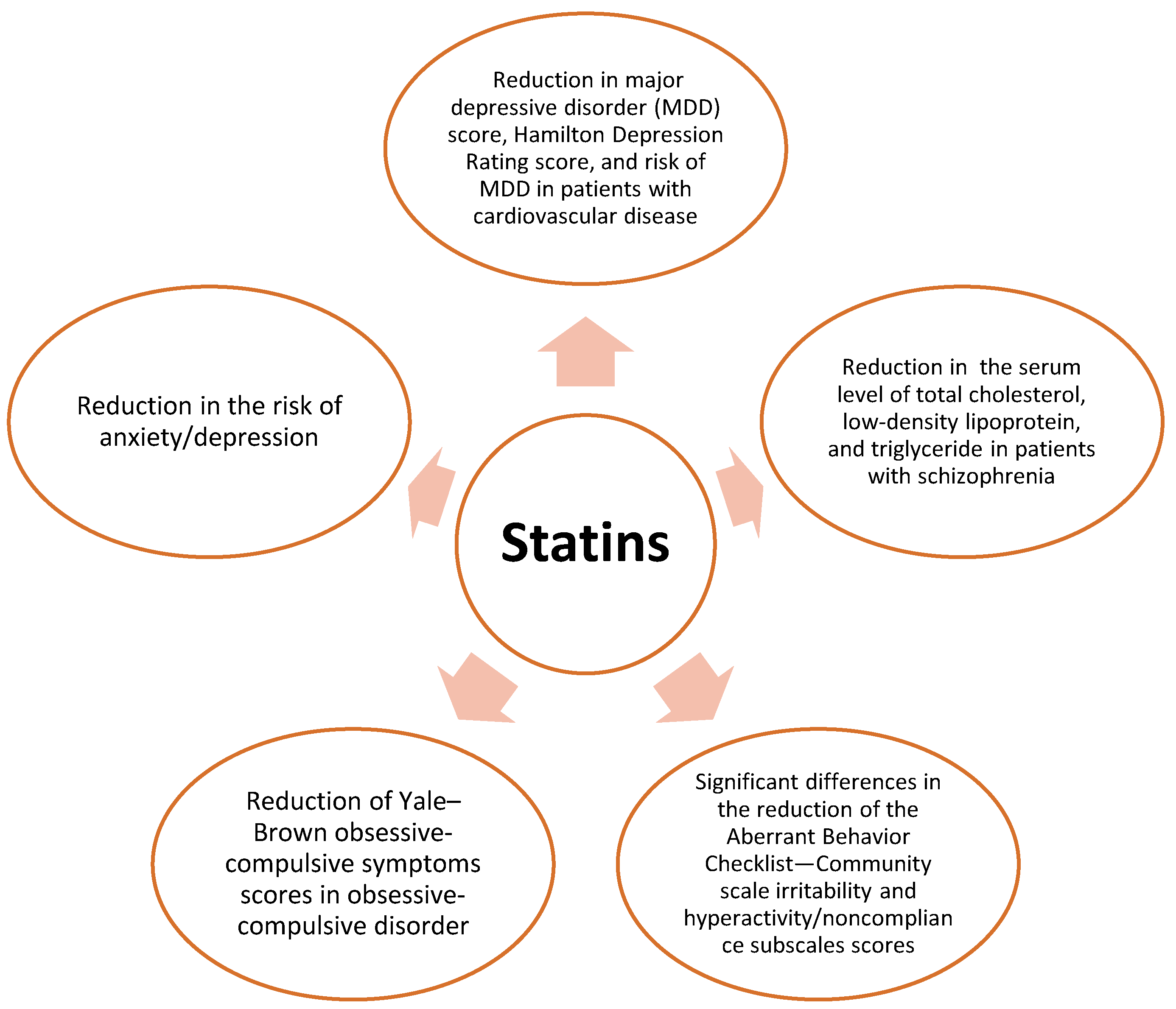
3. MDD and Statins
4. Schizophrenia and Statins
5. Anxiety Disorders and Statins
6. OCD and Statins
7. BD and Statins
7.1. BD Definition
7.2. Evidence from Clinical Trials
8. Delirium and Statins
8.1. Delirium Definition
8.2. Evidence from Clinical Trials
9. Autism and Statins
9.1. Autism Definition
9.2. Evidence from Clinical Trials
10. Potential Adverse Effects of Statins
11. Future Prospect
12. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- O’Neil, A.; Sanna, L.; Redlich, C.; Sanderson, K.; Jacka, F.; Williams, L.J.; Pasco, J.A.; Berk, M. The impact of statins on psychological wellbeing: A systematic review and meta-analysis. BMC Med. 2012, 10, 154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bellosta, S.; Bernini, F.; Paoletti, R.; Corsini, A. Non-lipid-related effects of statins. Ann. Med. 2000, 32, 164–176. [Google Scholar] [CrossRef]
- Sahebkar, A.; Watts, G.F. New therapies targeting apoB metabolism for high-risk patients with inherited dyslipidaemias: What can the clinician expect? Cardiovasc. Drugs Ther. 2013, 27, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Sahebkar, A.; Watts, G.F. New LDL-cholesterol lowering therapies: Pharmacology, clinical trials, and relevance to acute coronary syndromes. Clin. Ther. 2013, 35, 1082–1098. [Google Scholar] [CrossRef] [PubMed]
- Bahrami, A.; Parsamanesh, N.; Atkin, S.L.; Banach, M.; Sahebkar, A. Effect of statins on toll-like receptors: A new insight to pleiotropic effects. Pharmacol. Res. 2018, 135, 230–238. [Google Scholar] [CrossRef]
- Ferretti, G.; Bacchetti, T.; Sahebkar, A. Effect of statin therapy on paraoxonase-1 status: A systematic review and meta-analysis of 25 clinical trials. Prog. Lipid Res. 2015, 60, 50–73. [Google Scholar] [CrossRef]
- Gorabi, A.M.; Kiaie, N.; Pirro, M.; Bianconi, V.; Jamialahmadi, T.; Sahebkar, A. Effects of statins on the biological features of mesenchymal stem cells and therapeutic implications. Heart Fail. Rev. 2021, 26, 1259–1272. [Google Scholar] [CrossRef]
- Parizadeh, S.M.R.; Azarpazhooh, M.R.; Moohebati, M.; Nematy, M.; Ghayour-Mobarhan, M.; Tavallaie, S.; Rahsepar, A.A.; Amini, M.; Sahebkar, A.; Mohammadi, M.; et al. Simvastatin therapy reduces prooxidant-antioxidant balance: Results of a placebo-controlled cross-over trial. Lipids 2011, 46, 333–340. [Google Scholar] [CrossRef]
- Sahebkar, A.; Serban, C.; Mikhailidis, D.P.; Undas, A.; Lip, G.Y.H.; Muntner, P.; Bittner, V.; Ray, K.K.; Watts, G.F.; Hovingh, G.K.; et al. Association between statin use and plasma d-dimer levels: A systematic review and meta-analysis of randomised controlled trials. Thromb. Haemost. 2015, 114, 546–557. [Google Scholar]
- Vahedian-Azimi, A.; Mohammadi, S.M.; Beni, F.H.; Banach, M.; Guest, P.C.; Jamialahmadi, T.; Sahebkar, A. Improved COVID-19 ICU admission and mortality outcomes following treatment with statins: A systematic review and meta-analysis. Arch. Med. Sci. 2021, 17, 579. [Google Scholar] [CrossRef] [PubMed]
- Yildirir, A.; Muderrisoglu, H. Non-lipid effects of statins: Emerging new indications. Curr. Vasc. Pharmacol. 2004, 2, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-W.; Kang, H.-J.; Jhon, M.; Kim, J.-W.; Lee, J.-Y.; Walker, A.J.; Agustini, B.; Kim, J.M.; Berk, M. Statins and inflammation: New therapeutic opportunities in psychiatry. Front. Psychiatry 2019, 10, 103. [Google Scholar] [CrossRef] [Green Version]
- Hammond, T.R.; Marsh, S.E.; Stevens, B. Immune signaling in neurodegeneration. Immunity 2019, 50, 955–974. [Google Scholar] [CrossRef] [Green Version]
- Milenkovic, V.M.; Stanton, E.H.; Nothdurfter, C.; Rupprecht, R.; Wetzel, C.H. The role of chemokines in the pathophysiology of major depressive disorder. Int. J. Mol. Sci. 2019, 20, 2283. [Google Scholar] [CrossRef] [Green Version]
- Yan, Q. Neuroimmune imbalances and Yin-Yang dynamics in stress, anxiety, and depression. Psychoneuroimmunology 2018, 1781, 77–85. [Google Scholar]
- Young-Xu, Y.; Chan, K.A.; Liao, J.K.; Ravid, S.; Blatt, C.M. Long-term statin use and psychological well-being. J. Am. Coll. Cardiol. 2003, 42, 690–697. [Google Scholar] [CrossRef] [Green Version]
- Tajik-Esmaeeli, S.; Moazen-Zadeh, E.; Abbasi, N.; Shariat, S.V.; Rezaei, F.; Salehi, B.; Akhondzadeh, S. Simvastatin adjunct therapy for negative symptoms of schizophrenia: A randomized double-blind placebo-controlled trial. Int. Clin. Psychopharmacol. 2017, 32, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Zandi, P.; Sparks, D.; Khachaturian, A.; Tschanz, J.; Norton, M.; Steinberg, M.; Welsh-Bohmer, K.A.; Breitner, J.C.; Cache County Study investigators. Cache County Investigators Do statins reduce risk of incident dementia and Alzheimer’s disease. Arch. Gen. Psychiatry 2005, 62, 217–224. [Google Scholar] [CrossRef]
- Sparks, D.L.; Kryscio, R.J.; Sabbagh, M.N.; Connor, D.J.; Sparks, L.M.; Liebsack, C. Reduced risk of incident AD with elective statin use in a clinical trial cohort. Curr. Alzheimer Res. 2008, 5, 416–421. [Google Scholar] [CrossRef]
- Zissimopoulos, J.M.; Barthold, D.; Brinton, R.D.; Joyce, G. Sex and race differences in the association between statin use and the incidence of Alzheimer disease. JAMA Neurol. 2017, 74, 225–232. [Google Scholar] [CrossRef] [Green Version]
- Zamrini, E.; McGwin, G.; Roseman, J.M. Association between statin use and Alzheimer’s disease. Neuroepidemiology 2004, 23, 94–98. [Google Scholar] [CrossRef]
- Paoletti, R.; Bolego, C.; Cignarella, A. Lipid and non-lipid effects of statins. Atheroscler. Diet Drugs 2005, 170, 365–388. [Google Scholar]
- Mora, S.; Ridker, P.M. Justification for the Use of Statins in Primary Prevention: An Intervention Trial Evaluating Rosuvastatin (JUPITER)—Can C-reactive protein be used to target statin therapy in primary prevention? Am. J. Cardiol. 2006, 97, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Jašović-Gašić, M. Is treatment-resistance in psychiatric disorders a trap for polypharmacy? Psychiatr. Danub. 2015, 27, 1–313. [Google Scholar]
- Stertz, L.; Magalhães, P.V.S.; Kapczinski, F. Is bipolar disorder an inflammatory condition? The relevance of microglial activation. Curr. Opin. Psychiatry 2013, 26, 19–26. [Google Scholar] [CrossRef]
- Barger, S.W.; Basile, A.S. Activation of microglia by secreted amyloid precursor protein evokes release of glutamate by cystine exchange and attenuates synaptic function. J. Neurochem. 2001, 76, 846–854. [Google Scholar] [CrossRef]
- Takaki, J.; Fujimori, K.; Miura, M.; Suzuki, T.; Sekino, Y.; Sato, K. L-glutamate released from activated microglia downregulates astrocytic L-glutamate transporter expression in neuroinflammation: The ‘collusion’hypothesis for increased extracellular L-glutamate concentration in neuroinflammation. J. Neuroinflammation 2012, 9, 1–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Réus, G.Z.; Fries, G.R.; Stertz, L.; Badawy, M.; Passos, I.; Barichello, T.; Kapczinski, F.; Quevedo, J. The role of inflammation and microglial activation in the pathophysiology of psychiatric disorders. Neuroscience 2015, 300, 141–154. [Google Scholar] [CrossRef]
- Tanaka, M.; Tóth, F.; Polyák, H.; Szabó, Á.; Mándi, Y.; Vécsei, L. Immune Influencers in Action: Metabolites and Enzymes of the Tryptophan-Kynurenine Metabolic Pathway. Biomedicines 2021, 9, 734. [Google Scholar] [CrossRef]
- Link, A.; Ayadhi, T.; Böhm, M.; Nickenig, G. Rapid immunomodulation by rosuvastatin in patients with acute coronary syndrome. Eur. Heart J. 2006, 27, 2945–2955. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mayer, C.; Gruber, H.; Landl, E.; Pailer, S.; Scharnagl, H.; Truschnig-Wilders, M.; März, W. Rosuvastatin reduces interleukin-6-induced expression of C-reactive protein in human hepatocytes in a STAT3-and C/EBP-dependent fashion. Int. J. Clin. Pharmacol. Ther. 2007, 45, 319. [Google Scholar] [CrossRef] [PubMed]
- Williams, L.J.; Pasco, J.A.; Mohebbi, M.; Jacka, F.N.; Stuart, A.L.; Venugopal, K.; O’Neil, A.; Berk, M. Statin and aspirin use and the risk of mood disorders among men. Int. J. Neuropsychopharmacol. 2016, 19, 6. [Google Scholar] [CrossRef] [Green Version]
- Kohler, O.; Petersen, L.; Mors, O.; Gasse, C. Inflammation and depression: Combined use of selective serotonin reuptake inhibitors and NSAIDs or paracetamol and psychiatric outcomes. Brain Behav. 2015, 5, e00338. [Google Scholar] [CrossRef]
- Abbasi, S.-H.; Hosseini, F.; Modabbernia, A.; Ashrafi, M.; Akhondzadeh, S. Effect of celecoxib add-on treatment on symptoms and serum IL-6 concentrations in patients with major depressive disorder: Randomized double-blind placebo-controlled study. J. Affect. Disord. 2012, 141, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Muller, N.; Schwarz, M.J.; Dehning, S.; Douhe, A.; Cerovecki, A.; Goldstein-Miller, B.; Spellmann, I.; Hetzel, G.; Maino, K.; Kleindienst, N.; et al. The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: Results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine. Mol. Psychiatry 2006, 11, 680–684. [Google Scholar] [CrossRef]
- Raison, C.L.; Rutherford, R.E.; Woolwine, B.J.; Shuo, C.; Schettler, P.; Drake, D.F.; Haroon, E.; Miller, A.H. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: The role of baseline inflammatory biomarkers. JAMA Psychiatry 2013, 70, 31–41. [Google Scholar] [CrossRef]
- Dean, O.M.; Maes, M.; Ashton, M.; Berk, L.; Kanchanatawan, B.; Sughondhabirom, A.; Tangwongchai, S.; Ng, C.; Dowling, N.; Malhi, G.S.; et al. Protocol and rationale-the efficacy of minocycline as an adjunctive treatment for major depressive disorder: A double blind, randomised, placebo controlled trial. Clin. Psychopharmacol. Neurosci. 2014, 12, 180. [Google Scholar] [CrossRef] [Green Version]
- Berk, M.; Dean, O.M.; Cotton, S.M.; Jeavons, S.; Tanious, M.; Kohlmann, K.; Hewitt, K.; Moss, K.; Allwang, C.; Schapkaitz, I. The efficacy of adjunctive N-acetylcysteine in major depressive disorder: A double-blind, randomized, placebo-controlled trial. J. Clin. Psychiatry 2014, 75, 628. [Google Scholar] [CrossRef] [Green Version]
- Kohler, O.; Benros, M.E.; Nordentoft, M.; Farkouh, M.E.; Iyengar, R.L.; Mors, O.; Krogh, J. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: A systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry 2014, 71, 1381–1391. [Google Scholar] [CrossRef] [PubMed]
- Weitz-Schmidt, G. Statins as anti-inflammatory agents. Trends Pharmacol. Sci. 2002, 23, 482–487. [Google Scholar] [CrossRef]
- American Psychiatric Association. Practice Guideline for the Treatment of Patients with Major Depressive Disorder (3rd). 2009. Available online: http://psychiatryonline.org/guidelines.aspx (accessed on 1 October 2010).
- Trivedi, M.H.; Rush, A.J.; Wisniewski, S.R.; Nierenberg, A.A.; Warden, D.; Ritz, L.; Norquist, G.; Howland, R.H.; Lebowitz, B.; McGrath, P.J.; et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR* D: Implications for clinical practice. Am. J. Psychiatry 2006, 163, 28–40. [Google Scholar] [CrossRef]
- Benros, M.E.; Waltoft, B.L.; Nordentoft, M.; Ostergaard, S.D.; Eaton, W.W.; Krogh, J.; Mortensen, P.B. Autoimmune diseases and severe infections as risk factors for mood disorders: A nationwide study. JAMA Psychiatry 2013, 70, 812–820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muller, N. Immunology of major depression. Neuroimmunomodulation 2014, 21, 123–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wium-Andersen, M.K.; Orsted, D.D.; Nordestgaard, B.G. Association between elevated plasma fibrinogen and psychological distress, and depression in 73,367 individuals from the general population. Mol. Psychiatry 2013, 18, 854–855. [Google Scholar] [CrossRef] [PubMed]
- Salagre, E.; Fernandes, B.S.; Dodd, S.; Brownstein, D.J.; Berk, M. Statins for the treatment of depression: A meta-analysis of randomized, double-blind, placebo-controlled trials. J. Affect. Disord. 2016, 200, 235–242. [Google Scholar] [CrossRef]
- Kohler, O.; Gasse, C.; Petersen, L.; Ingstrup, K.G.; Nierenberg, A.A.; Mors, O.; Østergaard, S.D. The effect of concomitant treatment with SSRIs and statins: A population-based study. Am. J. Psychiatry 2016, 173, 807–815. [Google Scholar] [CrossRef]
- Santanello, N.C.; Barber, B.L.; Applegate, W.B.; Elam, J.; Curtis, C.; Hunninghake, D.B.; Gordon, D.J. Effect of pharmacologic lipid lowering on health-related quality of life in older persons: Results from the Cholesterol Reduction in Seniors Program (CRISP) Pilot Study. J. Am. Geriatr. Soc. 1997, 45, 8–14. [Google Scholar] [CrossRef]
- Hyyppa, M.T.; Kronholm, E.; Virtanen, A.; Leino, A.; Jula, A. Does simvastatin affect mood and steroid hormone levels in hypercholesterolemic men? A randomized double-blind trial. Psychoneuroendocrinology 2003, 28, 181–194. [Google Scholar] [CrossRef]
- Collins, R.; Reith, C.; Emberson, J.; Armitage, J.; Baigent, C.; Blackwell, L.; Blumenthal, R.; Danesh, J.; Smith, G.D.; DeMets, D.; et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet 2016, 388, 2532–2561. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Norris, S.L.; Gregg, E.W.; Cheng, Y.J.; Beckles, G.; Kahn, H.S. Depressive symptoms and mortality among persons with and without diabetes. Am. J. Epidemiol. 2005, 161, 652–660. [Google Scholar] [CrossRef] [Green Version]
- Otte, C.; Zhao, S.; Whooley, M.A. Statin use and risk of depression in patients with coronary heart disease: Longitudinal data from the heart and soul study. J. Clin. Psychiatry 2012, 73, 610–615. [Google Scholar] [CrossRef] [PubMed]
- Parsaik, A.K.; Singh, B.; Hassan, M.M.; Singh, K.; Mascarenhas, S.S.; Williams, M.D.; Lapid, M.I.; Richardson, J.W.; West, C.P.; Rummans, T.A. Statins use and risk of depression: A systematic review and meta-analysis. J. Affect. Disord. 2014, 160, 62–67. [Google Scholar] [CrossRef]
- Köhler-Forsberg, O.; Gasse, C.; Berk, M.; Østergaard, S.D. Do Statins Have Antidepressant Effects? CNS Drugs 2017, 31, 335–343. [Google Scholar] [CrossRef]
- Kessing, L.V.; Rytgaard, H.C.; Gerds, T.A.; Berk, M.; Ekstrøm, C.T.; Andersen, P.K. New drug candidates for depression—A nationwide population-based study. Acta Psychiatr. Scand. 2019, 139, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Köhler-Forsberg, O.; Gasse, C.; Petersen, L.; Nierenberg, A.A.; Mors, O.; Østergaard, S.D. Statin treatment and the risk of depression. J. Affect Disord. 2019, 246, 706–715. [Google Scholar] [CrossRef] [PubMed]
- Ghanizadeh, A.; Hedayati, A. Augmentation of fluoxetine with lovastatin for treating major depressive disorder, a randomized double-blind placebo controlled-clinical trial. Depress Anxiety 2013, 30, 1084–1088. [Google Scholar] [CrossRef] [PubMed]
- Haghighi, M.; Khodakarami, S.; Jahangard, L.; Ahmadpanah, M.; Bajoghli, H.; Holsboer-Trachsler, E.; Brand, S. In a randomized, double-blind clinical trial, adjuvant atorvastatin improved symptoms of depression and blood lipid values in patients suffering from severe major depressive disorder. J. Psychiatr. Res. 2014, 58, 109–114. [Google Scholar] [CrossRef]
- Gougol, A.; Zareh-Mohammadi, N.; Raheb, S.; Farokhnia, M.; Salimi, S.; Iranpour, N.; Yekehtaz, H.; Akhondzadeh, S. Simvastatin as an adjuvant therapy to fluoxetine in patients with moderate to severe major depression: A double-blind placebo-controlled trial. J. Psychopharmacol. 2015, 29, 575–581. [Google Scholar] [CrossRef]
- Abbasi, S.H.; Mohammadinejad, P.; Shahmansouri, N.; Salehiomran, A.; Beglar, A.A.; Zeinoddini, A.; Forghani, S.; Akhondzadeh, S. Simvastatin versus atorvastatin for improving mild to moderate depression in post-coronary artery bypass graft patients: A double-blind, placebo-controlled, randomized trial. J. Affect. Disord. 2015, 183, 149–155. [Google Scholar] [CrossRef]
- Quinn, A.L.; Dean, O.M.; Davey, C.G.; Kerr, M.; Harrigan, S.M.; Cotton, S.M.; Chanen, A.M.; Dodd, S.; Ratheesh, A.; Amminger, G.P.; et al. Youth Depression Alleviation-Augmentation with an anti-inflammatory agent (YoDA-A): Protocol and rationale for a placebo-controlled randomized trial of rosuvastatin and aspirin. Early Interv. Psychiatry 2018, 12, 45–54. [Google Scholar] [CrossRef] [Green Version]
- Redlich, C.; Berk, M.; Williams, L.J.; Sundquist, J.; Sundquist, K.; Li, X. Statin use and risk of depression: A Swedish national cohort study. BMC Psychiatry 2014, 14, 348. [Google Scholar] [CrossRef] [Green Version]
- Chuang, C.-S.; Yang, T.-Y.; Muo, C.-H.; Su, H.-L.; Sung, F.-C.; Kao, C.-H. Hyperlipidemia, statin use and the risk of developing depression: A nationwide retrospective cohort study. Gen. Hosp. Psychiatry 2014, 36, 497–501. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-M.; Stewart, R.; Kang, H.-J.; Bae, K.-Y.; Kim, S.-W.; Shin, I.-S.; Kim, J.T.; Park, M.S.; Cho, K.H.; Yoon, J.S. A prospective study of statin use and poststroke depression. J. Clin. Psychopharmacol. 2014, 34, 72–79. [Google Scholar] [CrossRef]
- Al Badarin, F.J.; Spertus, J.A.; Gosch, K.L.; Buchanan, D.M.; Chan, P.S. Initiation of statin therapy after acute myocardial infarction is not associated with worsening depressive symptoms: Insights from the Prospective Registry Evaluating Outcomes After Myocardial Infarctions: Events and Recovery (PREMIER) and Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status (TRIUMPH) registries. Am. Heart J. 2013, 166, 879–886. [Google Scholar]
- Glaus, J.; Vandeleur, C.L.; Lasserre, A.l.M.; Strippoli, M.-P.F.; Castelao, E.; Gholam-Rezaee, M.; Waeber, G.; Aubry, J.M.; Vollenweider, P.; Preisig, M. Aspirin and statin use and the subsequent development of depression in men and women: Results from a longitudinal population-based study. J. Affect. Disord. 2015, 182, 126–131. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.W.; Bae, K.Y.; Kim, J.M.; Shin, I.S.; Hong, Y.J.; Ahn, Y.; Jeong, M.H.; Berk, M.; Yoon, J.S. The use of statins for the treatment of depression in patients with acute coronary syndrome. Transl. Psychiatry 2015, 5, e620. [Google Scholar] [CrossRef] [Green Version]
- Dave, C.V.; Winterstein, A.G.; Park, H.; Cook, R.L.; Hartzema, A.G. Comparative risk of lipophilic and hydrophilic statins on incident depression: A retrospective cohort study. J. Affect. Disord. 2018, 238, 542–546. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Clinical Excellence (Great Britain). Psychosis and Schizophrenia in Adults: Treatment and Management; National Institute for Health and Clinical Excellence (NICE): London, UK; p. 2014.
- Miller, B.J.; Culpepper, N.; Rapaport, M.H. C-reactive protein levels in schizophrenia: A review and meta-analysis. Clin. Schizophr. Relat. Psychoses 2014, 7, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Najjar, S.; Pearlman, D.M. Neuroinflammation and white matter pathology in schizophrenia: Systematic review. Schizophr. Res. 2015, 161, 102–112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, B.J.; Buckley, P.; Seabolt, W.; Mellor, A.; Kirkpatrick, B. Meta-analysis of cytokine alterations in schizophrenia: Clinical status and antipsychotic effects. Biol. Psychiatry 2011, 70, 663–671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keller, W.R.; Kum, L.M.; Wehring, H.J.; Koola, M.M.; Buchanan, R.W.; Kelly, D.L. A review of anti-inflammatory agents for symptoms of schizophrenia. J. Psychopharmacol. 2013, 27, 337–342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Berckel, B.N.; Bossong, M.G.; Boellaard, R.; Kloet, R.; Schuitemaker, A.; Caspers, E.; Luurtsema, G.; Windhorst, A.D.; Cahn, W.; Lammertsma, A.A.; et al. Microglia activation in recent-onset schizophrenia: A quantitative (R)-[11C] PK11195 positron emission tomography study. Biol. Psychiatry 2008, 64, 820–822. [Google Scholar] [CrossRef] [PubMed]
- Osborn, D.P.; Nazareth, I.; King, M.B. Physical activity, dietary habits and Coronary Heart Disease risk factor knowledge amongst people with severe mental illness. Soc. Psychiatry Psychiatr. Epidemiol. 2007, 42, 787–793. [Google Scholar] [CrossRef]
- Laursen, T.M.; Munk-Olsen, T.; Gasse, C. Chronic somatic comorbidity and excess mortality due to natural causes in persons with schizophrenia or bipolar affective disorder. PLoS ONE 2011, 6, e24597. [Google Scholar] [CrossRef] [Green Version]
- Olfson, M.; Marcus, S.C.; Corey-Lisle, P.; Tuomari, A.; Hines, P.; L’Italien, G.J. Hyperlipidemia following treatment with antipsychotic medications. Am. J. Psychiatry 2006, 163, 1821–1825. [Google Scholar] [CrossRef]
- Hsu, J.-H.; Chien, I.-C.; Lin, C.-H.; Chou, Y.-J.; Chou, P. Hyperlipidemia in patients with schizophrenia: A national population-based study. Gen. Hosp. Psychiatry 2012, 34, 360–367. [Google Scholar] [CrossRef]
- De, M.H.; Kalnicka, D.; Wampers, M.; Hanssens, L.; Van, D.E.; Scheen, A.; Peuskens, J. treatment with rosuvastatin for severe dyslipidemia in patients with schizophrenia and schizoaffective disorder. J. Clin. Psychiatry 2006, 67, 1889–1896. [Google Scholar]
- Ojala, K.; Repo-Tiihonen, E.; Tiihonen, J.; Niskanen, L. Statins are effective in treating dyslipidemia among psychiatric patients using second-generation antipsychotic agents. J. Psychopharmacol. 2008, 22, 33–38. [Google Scholar] [CrossRef]
- Chaudhry, I.B.; Husain, N.; Husain, M.O.; Hallak, J.; Drake, R.; Kazmi, A.; ur Rahman, R.; Hamirani, M.M.; Kiran, T.; Mehmood, N.; et al. Ondansetron and simvastatin added to treatment as usual in patients with schizophrenia: Study protocol for a randomized controlled trial. Trials 2013, 14, 101. [Google Scholar] [CrossRef]
- Mansi, I.; Frei, C.R.; Pugh, M.J.; Mortensen, E.M. Psychologic disorders and statin use: A propensity score-matched analysis. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2013, 33, 615–626. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghanizadeh, A.; Rezaee, Z.; Dehbozorgi, S.; Berk, M.; Akhondzadeh, S. Lovastatin for the adjunctive treatment of schizophrenia: A preliminary randomized double-blind placebo-controlled trial. Psychiatry Res. 2014, 219, 431–435. [Google Scholar] [CrossRef]
- Vincenzi, B.; Stock, S.; Borba, C.P.; Cleary, S.M.; Oppenheim, C.E.; Petruzzi, L.J.; Fan, X.; Copeland, P.M.; Freudenreich, O.; Cather, C.; et al. A randomized placebo-controlled pilot study of pravastatin as an adjunctive therapy in schizophrenia patients: Effect on inflammation, psychopathology, cognition and lipid metabolism. Schizophr. Res. 2014, 159, 395–403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osborn, D.; Burton, A.; Hunter, R.; Marston, L.; Atkins, L.; Barnes, T.; Blackburn, R.; Craig, T.; Gilbert, H.; Heinkel, S.; et al. Clinical and cost-effectiveness of an intervention for reducing cholesterol and cardiovascular risk for people with severe mental illness in English primary care: A cluster randomised controlled trial. Lancet Psychiatry 2018, 5, 145–154. [Google Scholar] [CrossRef] [Green Version]
- Nomura, I.; Kishi, T.; Ikuta, T.; Iwata, N. Statin add-on therapy in the antipsychotic treatment of schizophrenia: A meta-analysis. Psychiatry Res. 2018, 260, 41–47. [Google Scholar] [CrossRef]
- Çakici, N.; Van Beveren, N.; Judge-Hundal, G.; Koola, M.; Sommer, I. An update on the efficacy of anti-inflammatory agents for patients with schizophrenia: A meta-analysis. Psychol. Med. 2019, 49, 2307–2319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kato, T.; Monji, A.; Mizoguchi, Y.; Hashioka, S.; Horikawa, H.; Seki, Y.; Kasai, M.; Utsumi, H.; Kanba, S. Anti-Inflammatory properties of antipsychotics via microglia modulations: Are antipsychotics a ‘fire extinguisher’in the brain of schizophrenia? Mini Rev. Med. Chem. 2011, 11, 565–574. [Google Scholar] [CrossRef]
- Wang, Q.; Zengin, A.; Deng, C.; Li, Y.; Newell, K.A.; Yang, G.-Y.; Lu, Y.; Wilder-Smith, E.P.; Zhao, H.; Huang, X.F. High dose of simvastatin induces hyperlocomotive and anxiolytic-like activities: The association with the up-regulation of NMDA receptor binding in the rat brain. Exp. Neurol. 2009, 216, 132–138. [Google Scholar] [CrossRef]
- Yan, J.; Xu, Y.; Zhu, C.; Zhang, L.; Wu, A.; Yang, Y.; Xiong, Z.; Deng, C.; Huang, X.F.; Yenari, M.A.; et al. Simvastatin prevents dopaminergic neurodegeneration in experimental parkinsonian models: The association with anti-inflammatory responses. PLoS ONE 2011, 6, e20945. [Google Scholar] [CrossRef]
- Blake, G.J.; Ridker, P.M. Are statins anti-inflammatory? Trials 2000, 1, 161. [Google Scholar] [CrossRef] [Green Version]
- McFarland, A.; Davey, A.; Anoopkumar-Dukie, S. Statins reduce lipopolysaccharide-induced cytokine and inflammatory mediator release in an in vitro model of microglial-like cells. Mediat. Inflamm. 2017, 2017, 2582745. [Google Scholar] [CrossRef] [Green Version]
- Karmaus, P.W.; Shi, M.; Perl, S.; Biancotto, A.; Candia, J.; Cheung, F.; Kotliarov, Y.; Young, N.; Fessler, M.B.; CHI, Consortium. Effects of rosuvastatin on the immune system in healthy volunteers with normal serum cholesterol. JCI Insight 2019, 4, e131530. [Google Scholar] [CrossRef] [PubMed]
- Diamantis, E.; Kyriakos, G.; Victoria Quiles-Sanchez, L.; Farmaki, P.; Troupis, T. The anti-inflammatory effects of statins on coronary artery disease: An updated review of the literature. Curr. Cardiol. Rev. 2017, 13, 209–216. [Google Scholar] [CrossRef]
- McFarland, A.J.; Anoopkumar-Dukie, S.; Arora, D.S.; Grant, G.D.; McDermott, C.M.; Perkins, A.V.; Davey, A.K. Molecular mechanisms underlying the effects of statins in the central nervous system. Int. J. Mol. Sci. 2014, 15, 20607–20637. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Felger, J.C. Imaging the role of inflammation in mood and anxiety-related disorders. Curr. Neuropharmacol. 2018, 16, 533–558. [Google Scholar] [CrossRef]
- Vogelzangs, N.; Beekman, A.; De Jonge, P.; Penninx, B. Anxiety disorders and inflammation in a large adult cohort. Transl. Psychiatry 2013, 3, e249. [Google Scholar] [CrossRef] [Green Version]
- Quagliato, L.A.; Nardi, A.E. Cytokine alterations in panic disorder: A systematic review. J. Affect. Disord. 2018, 228, 91–96. [Google Scholar] [CrossRef]
- Hou, R.; Garner, M.; Holmes, C.; Osmond, C.; Teeling, J.; Lau, L.; Baldwin, D.S. Peripheral inflammatory cytokines and immune balance in Generalised Anxiety Disorder: Case-controlled study. Brain Behav. Immun. 2017, 62, 212–218. [Google Scholar] [CrossRef] [Green Version]
- Shrivastava, S.; Pucadyil, T.J.; Paila, Y.D.; Ganguly, S.; Chattopadhyay, A. Chronic cholesterol depletion using statin impairs the function and dynamics of human serotonin1A receptors. Biochemistry 2010, 49, 5426–5435. [Google Scholar] [CrossRef] [PubMed]
- Korhonen, M.J.; Pentti, J.; Hartikainen, J.; Kivimäki, M.; Vahtera, J. Somatic symptoms of anxiety and nonadherence to statin therapy. Int. J. Cardiol. 2016, 214, 493–499. [Google Scholar] [CrossRef]
- Huang, C.-I.; Lin, L.-C.; Tien, H.-C.; Que, J.; Ting, W.C.; Chen, P.-C.; Wu, H.M.; Ho, C.H.; Wang, J.J.; Wang, R.H.; et al. Hyperlipidemia and statins use for the risk of new-onset anxiety/depression in patients with head and neck cancer: A population-based study. PLoS ONE 2017, 12, e0174574. [Google Scholar] [CrossRef] [Green Version]
- Yeh, J.-J.; Syue, S.-H.; Lin, C.-L.; Hsu, C.Y.; Shae, Z.; Kao, C.-H. Effects of statins on anxiety and depression in patients with asthma-chronic obstructive pulmonary disease overlap syndrome. J. Affect. Disord. 2019, 253, 277–284. [Google Scholar] [CrossRef]
- Pemminati, S.; Colaco, M.N.; Patchava, D.; Shivaprakash, G.; Ullal, D.S.; Gopalakrishna, H.; Rathnakar, U.P.; Shenoy, A.K. Role of statins in animal models of anxiety in Normo-cholesterolemic rats. J. Pharm. Res. 2012, 5, 3764–3766. [Google Scholar]
- Thomas, J.M.; Varkey, J.; Augustine, B.B. Association between serum cholesterol, brain serotonin, and anxiety: A study in simvastatin administered experimental animals. Int. J. Nutr. Pharmacol. Neurol. Dis. 2014, 4, 69. [Google Scholar] [CrossRef]
- Stein, D.J. Obsessive-compulsive disorder. Lancet 2002, 360, 397–405. [Google Scholar] [CrossRef] [Green Version]
- Ravizza, L.; Barzega, G.; Bellino, S.; Bogetto, F.; Maina, G. Drug treatment of obsessive-compulsive disorder (OCD): Long-term trial with clomipramine and selective serotonin reuptake inhibitors (SSRIs). Psychopharmacol. Bull. 1996, 32, 167–173. [Google Scholar] [PubMed]
- Decloedt, E.H.; Stein, D.J. Current trends in drug treatment of obsessive–compulsive disorder. Neuropsychiatr. Dis. Treat. 2010, 6, 233. [Google Scholar] [CrossRef] [Green Version]
- Koo, M.-S.; Kim, E.-J.; Roh, D.; Kim, C.-H. Role of dopamine in the pathophysiology and treatment of obsessive–compulsive disorder. Expert Rev. Neurother. 2010, 10, 275–290. [Google Scholar] [CrossRef]
- Ting, J.T.; Feng, G. Glutamatergic synaptic dysfunction and obsessive-compulsive disorder. Curr. Chem. Genom. 2008, 2, 62. [Google Scholar] [CrossRef] [Green Version]
- Pallanti, S.; Quercioli, L. Treatment-refractory obsessive-compulsive disorder: Methodological issues, operational definitions and therapeutic lines. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2006, 30, 400–412. [Google Scholar] [CrossRef]
- Yang, J.-w.; Hu, Z.-p. Neuroprotective effects of atorvastatin against cerebral ischemia/reperfusion injury through the inhibition of endoplasmic reticulum stress. Neural Regen. Res. 2015, 10, 1239. [Google Scholar] [PubMed]
- Pathak, N.N.; Balaganur, V.; Lingaraju, M.C.; More, A.S.; Kant, V.; Kumar, D.; Kumar, D.; Tandan, S.K. Antihyperalgesic and anti-inflammatory effects of atorvastatin in chronic constriction injury-induced neuropathic pain in rats. Inflammation 2013, 36, 1468–1478. [Google Scholar] [CrossRef]
- Wang, Q.; Ting, W.L.; Yang, H.; Wong, P.T. High doses of simvastatin upregulate dopamine D1 and D2 receptor expression in the rat prefrontal cortex: Possible involvement of endothelial nitric oxide synthase. Br. J. Pharmacol. 2005, 144, 933. [Google Scholar] [CrossRef]
- Wang, Q.; Tang, X.N.; Wang, L.; Yenari, M.A.; Ying, W.; Goh, B.-C.; Lee, H.S.; Wilder-Smith, E.P.; Wong, P.T. Effects of high dose of simvastatin on levels of dopamine and its reuptake in prefrontal cortex and striatum among SD rats. Neurosci. Lett. 2006, 408, 189–193. [Google Scholar] [CrossRef]
- Guimaraes, F.; Beijamini, V.; Moreira, F.; Aguiar, D.; De Lucca, A. Role of nitric oxide in brain regions related to defensive reactions. Neurosci. Biobehav. Rev. 2005, 29, 1313–1322. [Google Scholar] [CrossRef] [PubMed]
- Umathe, S.; Bhutada, P.; Jain, N.; Mundhada, Y.; Borkar, S.; Dhumal, B. Role of nitric oxide in obsessive–compulsive behavior and its involvement in the anti-compulsive effect of paroxetine in mice. Nitric Oxide 2009, 21, 140–147. [Google Scholar] [CrossRef]
- Seker, F.; Kilic, U.; Caglayan, B.; Ethemoglu, M.; Caglayan, A.; Ekimci, N.; Demirci, S.; Dogan, A.; Oztezcan, S.; Sahin, F.; et al. HMG-CoA reductase inhibitor rosuvastatin improves abnormal brain electrical activity via mechanisms involving eNOS. Neuroscience 2015, 284, 349–359. [Google Scholar] [CrossRef]
- Lin, H.-C.; Kang, B.-H.; Wan, F.-J.; Huang, S.-T.; Tseng, C.-J. Reciprocal regulation of nitric oxide and glutamate in the nucleus tractus solitarii of rats. Eur. J. Pharmacol. 2000, 407, 83–89. [Google Scholar] [CrossRef]
- Serra, P.A.; Rocchitta, G.; Esposito, G.; Delogu, M.R.; Migheli, R.; Miele, E.; Desole, M.S.; Miele, M. A study on the role of nitric oxide and iron in 3-morpholino-sydnonimine-induced increases in dopamine release in the striatum of freely moving rats. Br. J. Pharmacol. 2001, 134, 275–282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahim, F.; Sayyah, M. Effects of atorvastatin on treatment-resistant obsessive-compulsive disorder: A double-blind randomized trial. Psychiatr. Pol. 2018, 52, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Akouchekian, S.; Omranifard, V.; Moshfegh, P.; Maracy, M.R.; Almasi, A. The Effect of Atorvastatin on Obsessive-compulsive Symptoms of Refractory Obsessive-compulsive Disorder (Add-on Therapy). Adv. Biomed. Res. 2018, 7, 90. [Google Scholar]
- While, A.; Keen, L. The effects of statins on mood: A review of the literature. Eur. J. Cardiovasc. Nurs. 2012, 11, 85–96. [Google Scholar] [CrossRef]
- Leppien, E.; Mulcahy, K.; Demler, T.L.; Trigoboff, E.; Opler, L. Effects of statins and cholesterol on patient aggression: Is there a connection? Innov. Clin. Neurosci. 2018, 15, 24. [Google Scholar]
- Tatley, M.; Savage, R. Psychiatric adverse reactions with statins, fibrates and ezetimibe. Drug Saf. 2007, 30, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Ling, Q.; Tejada-Simon, M.V. Statins and the brain: New perspective for old drugs. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2016, 66, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Armitage, J.; Collins, R.; Wallendszus, K.; Keech, A.; Lawson, A. Randomised placebo controlled trial of effect on mood of lowering cholesterol concentration. BMJ 1996, 313, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Lilly, S.M.; Mortensen, E.M.; Frei, C.R.; Pugh, M.J.; Mansi, I.A. Comparison of the risk of psychological and cognitive disorders between persistent and nonpersistent statin users. Am. J. Cardiol. 2014, 114, 1035–1039. [Google Scholar] [CrossRef] [Green Version]
- Hayes, J.F.; Lundin, A.; Wicks, S.; Lewis, G.; Wong, I.C.; Osborn, D.P.; Dalman, C. Association of hydroxylmethyl glutaryl coenzyme A reductase inhibitors, L-Type calcium channel antagonists, and biguanides with rates of psychiatric hospitalization and self-harm in individuals with serious mental illness. JAMA Psychiatry 2019, 76, 382–390. [Google Scholar] [CrossRef] [Green Version]
- Berk, M.; Kapczinski, F.; Andreazza, A.C.; Dean, O.; Giorlando, F.; Maes, M.; Yücel, M.; Gama, C.S.; Dodd, S.; Dean, B.; et al. Pathways underlying neuroprogression in bipolar disorder: Focus on inflammation, oxidative stress and neurotrophic factors. Neurosci. Biobehav. Rev. 2011, 35, 804–817. [Google Scholar] [CrossRef]
- Leboyer, M.; Soreca, I.; Scott, J.; Frye, M.; Henry, C.; Tamouza, R.; Kupfer, D.J. Can bipolar disorder be viewed as a multi-system inflammatory disease? J. Affect. Disord. 2012, 141, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Pfaffenseller, B.; Fries, G.R.; Wollenhaupt-Aguiar, B.; Colpo, G.D.; Stertz, L.; Panizzutti, B.; Magalhaes, P.V.; Kapczinski, F. Neurotrophins, inflammation and oxidative stress as illness activity biomarkers in bipolar disorder. Expert Rev. Neurother. 2013, 13, 827–842. [Google Scholar] [CrossRef] [PubMed]
- Ghanizadeh, A.; Berk, M. Molecular hydrogen: An overview of its neurobiological effects and therapeutic potential for bipolar disorder and schizophrenia. Med Gas Res. 2013, 3, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghanizadeh, A.; OmraniSigaroodi, M.; Javadpour, A.; Dabbaghmanesh, M.H.; Shafiee, S. Lovastatin as an adjuvant to lithium for treating manic phase of bipolar disorder: A 4-week, randomized, double-blind, placebo-controlled clinical trial. Depress. Res. Treat. 2014, 2014, 730505. [Google Scholar] [CrossRef] [PubMed]
- Soh, J.F.; Almadani, A.; Beaulieu, S.; Rajji, T.; Mulsant, B.H.; Su, C.-L.; Renaud, S.; Mucsi, I.; Torres-Platas, S.G.; Levinson, A.; et al. The effect of atorvastatin on cognition and mood in bipolar disorder and unipolar depression patients: A secondary analysis of a randomized controlled trial. J. Affect. Disord. 2020, 262, 149–154. [Google Scholar]
- Gildengers, A.; Tatsuoka, C.; Bialko, C.; Cassidy, K.A.; Dines, P.; Emanuel, J.; Al Jurdi, R.K.; Gyulai, L.; Mulsant, B.H.; Young, R.C.; et al. Correlates of disability in depressed older adults with bipolar disorder. Cut. Edge Psychiatry Pract. 2013, 2013, 332. [Google Scholar]
- Sajatovic, M.; Strejilevich, S.A.; Gildengers, A.G.; Dols, A.; Al Jurdi, R.K.; Forester, B.P.; Kessing, L.V.; Beyer, J.; Manes, F.; Rej, S.; et al. A report on older-age bipolar disorder from the International Society for Bipolar Disorders Task Force. Bipolar Disord. 2015, 17, 689–704. [Google Scholar] [CrossRef]
- Nadkarni, N.K.; Perera, S.; Hanlon, J.T.; Lopez, O.; Newman, A.B.; Aizenstein, H.; Elam, M.; Harris, T.B.; Kritchevsky, S.; Yaffe, K.; et al. Statins and brain integrity in older adults: Secondary analysis of the Health ABC study. Alzheimer’s Dement. 2015, 11, 1202–1211. [Google Scholar] [CrossRef] [Green Version]
- Rej, S.; Schulte, S.W.; Rajji, T.K.; Gildengers, A.G.; Miranda, D.; Menon, M.; Butters, M.A.; Mulsant, B.H. Statins and cognition in late-life bipolar disorder. Int. J. Geriatr. Psychiatry 2018, 33, 1355–1360. [Google Scholar] [CrossRef]
- Casarin, A.; McAuley, D.F.; Alce, T.M.; Zhao, X.; Ely, E.W.; Jackson, J.C.; McDowell, C.; Agus, A.; Murphy, L.; Page, V.J. Evaluating early administration of the hydroxymethylglutaryl-CoA reductase inhibitor simvastatin in the prevention and treatment of delirium in critically ill ventilated patients (MoDUS trial): Study protocol for a randomized controlled trial. Trials 2015, 16, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Ely, E.; Gautam, S.; Margolin, R.; Francis, J.; May, L.; Speroff, T.; Truman, B.; Dittus, R.; Bernard, G.; Inouye, S. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001, 27, 1892–1900. [Google Scholar] [CrossRef]
- Cerejeira, J.; Firmino, H.; Vaz-Serra, A.; Mukaetova-Ladinska, E.B. The neuroinflammatory hypothesis of delirium. Acta Neuropathol. 2010, 119, 737–754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cunningham, C. Systemic Inflammation and Delirium: Important Co-Factors in the Progression of Dementia. Biochem. Soc. Trans. 2011, 39, 945–953. [Google Scholar] [CrossRef] [PubMed]
- Ritter, C.; Tomasi, C.D.; Dal-Pizzol, F.; Pinto, B.B.; Dyson, A.; de Miranda, A.S.; Comim, C.M.; Soares, M.; Teixeira, A.L.; Quevedo, J.; et al. Inflammation biomarkers and delirium in critically ill patients. Crit. Care 2014, 18, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Cape, E.; Hall, R.J.; van Munster, B.C.; de Vries, A.; Howie, S.E.; Pearson, A.; Middleton, S.D.; Gillies, F.; Armstrong, I.R.; White, T.O.; et al. Cerebrospinal fluid markers of neuroinflammation in delirium: A role for interleukin-1β in delirium after hip fracture. J. Psychosom. Res. 2014, 77, 219–225. [Google Scholar] [CrossRef] [Green Version]
- Needham, D.M.; Colantuoni, E.; Dinglas, V.D.; Hough, C.L.; Wozniak, A.W.; Jackson, J.C.; Morris, P.E.; Mendez-Tellez, P.A.; Ely, E.W.; Hopkins, R.O. Rosuvastatin versus placebo for delirium in intensive care and subsequent cognitive impairment in patients with sepsis-associated acute respiratory distress syndrome: An ancillary study to a randomised controlled trial. Lancet Respir. Med. 2016, 4, 203–212. [Google Scholar] [CrossRef] [Green Version]
- Alexandre, P.C.; Reis, P.A.; Joana, D.; de JOliveira, F.M.; Pamplona, F.A.; Siqueira, L.D.; Neto, H.C.; Bozza, F.A. Atorvastatin and simvastatin protects cognitive impairment in an animal model of sepsis. Crit. Care 2013, 17, 1–59. [Google Scholar] [CrossRef] [Green Version]
- Katznelson, R.; Djaiani, G.N.; Borger, M.A.; Friedman, Z.; Abbey, S.E.; Fedorko, L.; Karski, J.; Mitsakakis, N.; Carroll, J.; Beattie, W.S. Preoperative use of statins is associated with reduced early delirium rates after cardiac surgery. Anesthesiol. J. Am. Soc. Anesthesiol. 2009, 110, 67–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Katznelson, R.; Djaiani, G.; Mitsakakis, N.; Lindsay, T.F.; Tait, G.; Friedman, Z.; Wasowicz, M.; Beattie, W.S. Delirium following vascular surgery: Increased incidence with preoperative β-blocker administration. Can. J. Anesth./J. Can. D’anesthésie 2009, 56, 793. [Google Scholar] [CrossRef] [Green Version]
- Morandi, A.; Hughes, C.G.; Thompson, J.L.; Pandharipande, P.P.; Shintani, A.K.; Vasilevskis, E.E.; Han, J.H.; Jackson, J.C.; Laskowitz, D.T.; Bernard, G.R.; et al. Statins and delirium during critical illness: A multicenter, prospective cohort study. Crit. Care Med. 2014, 42, 1899. [Google Scholar] [CrossRef]
- Page, V.J.; Davis, D.; Zhao, X.B.; Norton, S.; Casarin, A.; Brown, T.; Ely, E.W.; McAuley, D.F. Statin use and risk of delirium in the critically ill. Am. J. Respir. Crit. Care Med. 2014, 189, 666–673. [Google Scholar] [CrossRef] [Green Version]
- Niessner, A.; Steiner, S.; Speidl, W.S.; Pleiner, J.; Seidinger, D.; Maurer, G.; Goronzy, J.J.; Weyand, C.M.; Kopp, C.W.; Huber, K.; et al. Simvastatin suppresses endotoxin-induced upregulation of toll-like receptors 4 and 2 in vivo. Atherosclerosis 2006, 189, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Lynch, J.R.; Song, P.; Yang, H.-J.; Yates, R.B.; Mace, B.; Warner, D.S.; Guyton, J.R.; Laskowitz, D.T. Simvastatin and atorvastatin improve behavioral outcome, reduce hippocampal degeneration, and improve cerebral blood flow after experimental traumatic brain injury. Exp. Neurol. 2007, 206, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Page, V.J.; Casarin, A.; Ely, E.W.; Zhao, X.B.; McDowell, C.; Murphy, L.; McAuley, D.F. Evaluation of early administration of simvastatin in the prevention and treatment of delirium in critically ill patients undergoing mechanical ventilation (MoDUS): A randomised, double-blind, placebo-controlled trial. Lancet Respir. Med. 2017, 5, 727–737. [Google Scholar] [CrossRef] [Green Version]
- Lee, D.-S.; Lee, M.Y.; Park, C.-M.; Kim, D.-I.; Kim, Y.-W.; Park, Y.-J. Preoperative statins are associated with a reduced risk of postoperative delirium following vascular surgery. PLoS ONE 2018, 13, e0192841. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vallabhajosyula, S.; Kanmanthareddy, A.; Erwin, P.J.; Esterbrooks, D.J.; Morrow, L.E. Role of statins in delirium prevention in critical ill and cardiac surgery patients: A systematic review and meta-analysis. J. Crit. Care 2017, 37, 189–196. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Pub: Washington, DC, USA; London, UK, 2013. [Google Scholar]
- van der Most, P.J.; Dolga, A.M.; Nijholt, I.M.; Luiten, P.G.; Eisel, U.L. Statins: Mechanisms of neuroprotection. Prog. Neurobiol. 2009, 88, 64–75. [Google Scholar] [CrossRef] [PubMed]
- Wang, H. Lipid rafts: A signaling platform linking cholesterol metabolism to synaptic deficits in autism spectrum disorders. Front. Behav. Neurosci. 2014, 8, 104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Young, A.M.; Chakrabarti, B.; Roberts, D.; Lai, M.-C.; Suckling, J.; Baron-Cohen, S. From molecules to neural morphology: Understanding neuroinflammation in autism spectrum condition. Mol. Autism 2016, 7, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rossignol, D.A.; Frye, R.E. Evidence linking oxidative stress, mitochondrial dysfunction, and inflammation in the brain of individuals with autism. Front. Physiol. 2014, 5, 150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Estes, M.L.; McAllister, A.K. Immune mediators in the brain and peripheral tissues in autism spectrum disorder. Nat. Rev. Neurosci. 2015, 16, 469–486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moazen-Zadeh, E.; Shirzad, F.; Karkhaneh-Yousefi, M.-A.; Khezri, R.; Mohammadi, M.-R.; Akhondzadeh, S. Simvastatin as an adjunctive therapy to risperidone in treatment of autism: A randomized, double-blind, placebo-controlled clinical trial. J. Child Adolesc. Psychopharmacol. 2018, 28, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Stivaros, S.; Garg, S.; Tziraki, M.; Cai, Y.; Thomas, O.; Mellor, J.; Morris, A.A.; Jim, C.; Szumanska-Ryt, K.; Parkes, L.M.; et al. Randomised controlled trial of simvastatin treatment for autism in young children with neurofibromatosis type 1 (SANTA). Mol. Autism 2018, 9, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Johnson, M.H.; Griffin, R.; Gergely Csibra, H.H.; Farroni, T.; de Haan, M.; Tucker, L.A.; BARON–COHEN, S.I.; Richards, J. The emergence of the social brain network: Evidence from typical and atypical development. Dev. Psychopathol. 2005, 17, 599. [Google Scholar] [CrossRef] [Green Version]
- Ramkumar, S.; Raghunath, A.; Raghunath, S. Statin therapy: Review of safety and potential side effects. Acta Cardiol. Sin. 2016, 32, 631. [Google Scholar] [PubMed]
- Pedro-Botet, J.; Núñez-Cortés, J.M.; Flores, J.; Rius, J. Muscle symptoms related with statin therapy in general practice. Atherosclerosis 2015, 241, e197. [Google Scholar] [CrossRef]
- Buettner, C.; Burstein, R. Association of statin use and risk for severe headache or migraine by serum vitamin D status: A cross-sectional population-based study. Cephalalgia 2015, 35, 757–766. [Google Scholar] [CrossRef] [PubMed]
- Vesza, Z.; Pires, C.; da Silva, P.M. Statin-related lichenoid dermatosis: An uncommon adverse reaction to a common treatment. Eur. J. Case Rep. Intern. Med. 2018, 5, 844. [Google Scholar] [CrossRef]
- Smith, I.B.; Schmidt, R.; Mansi, I. Are Statins Associated with Upper Gastrointestinal Symptoms? Gastroenterology 2017, 152, S305. [Google Scholar] [CrossRef]
- Schultz, B.G.; Patten, D.K.; Berlau, D.J. The role of statins in both cognitive impairment and protection against dementia: A tale of two mechanisms. Transl. Neurodegener. 2018, 7, 5. [Google Scholar] [CrossRef]
- Ott, B.R.; Daiello, L.A.; Dahabreh, I.J.; Springate, B.A.; Bixby, K.; Murali, M.; Trikalinos, T.A. Do statins impair cognition? A systematic review and meta-analysis of randomized controlled trials. J. Gen. Intern. Med. 2015, 30, 348–358. [Google Scholar] [CrossRef] [Green Version]
- Thompson, P.D.; Panza, G.; Zaleski, A.; Taylor, B. Statin-associated side effects. J. Am. Coll. Cardiol. 2016, 67, 2395–2410. [Google Scholar] [CrossRef] [PubMed]
- Muldoon, M.F.; Barger, S.D.; Ryan, C.M.; Flory, J.D.; Lehoczky, J.P.; Matthews, K.A.; Manuck, S.B. Effects of lovastatin on cognitive function and psychological well-being. Am. J. Med. 2000, 108, 538–546. [Google Scholar] [CrossRef]
- Stewart, R.A.; Sharples, K.J.; North, F.M.; Menkes, D.B.; Baker, J.; Simes, J. Long-term assessment of psychological well-being in a randomized placebo-controlled trial of cholesterol reduction with pravastatin. Arch. Intern. Med. 2000, 160, 3144–3152. [Google Scholar] [CrossRef] [Green Version]
- Olson, M.B.; Kelsey, S.F.; Matthews, K.A.; Bairey Merz, C.N.; Eteiba, W.; McGorray, S.P.; Cornell, C.E.; Vido, D.A.; Muldoon, M.F. Lipid-lowering medication use and aggression scores in women: A report from the NHLBI-sponsored WISE study. J. Women’s Health 2008, 17, 187–194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agostini, J.V.; Tinetti, M.E.; Han, L.; McAvay, G.; Foody, J.M.; Concato, J. Effects of statin use on muscle strength, cognition, and depressive symptoms in older adults. J. Am. Geriatr. Soc. 2007, 55, 420–425. [Google Scholar] [CrossRef]
- Tuccori, M.; Lapi, F.; Testi, A.; Coli, D.; Moretti, U.; Vannacci, A.; Motola, D.; Salvo, F.; Rivolta, A.L.; Blandizzi, C.; et al. Statin-associated psychiatric adverse events. Drug Saf. 2008, 31, 1115–1123. [Google Scholar] [CrossRef] [PubMed]
- Kamel, N.S.; Gammack, J.K. Insomnia in the elderly: Cause, approach, and treatment. Am. J. Med. 2006, 119, 463–469. [Google Scholar] [CrossRef]
| Disease | Statin Type | No. of Patients | Study Design | Dosage/Duration | Main Outcomes | References |
|---|---|---|---|---|---|---|
| Coronary artery bypass graft | Simvastatin and atorvastatin | 46 | Double-blind RCT | 20 mg/day for 6 weeks | Simvastatin tended to improve depressive symptoms earlier and more effectively than did atorvastatin | [60] |
| MDD | Atorvastatin | 60 | Double-blind RCT | 20 mg/day for 12 weeks | Adjuvant atorvastatin favorably affect symptoms of MDD among patients with severe MDD | [58] |
| MDD | Lovastatin | 68 | Double-blind RCT | 30 mg/day for 6 weeks | Treatment group was more effective than placebo group in reduction of MDD score | [57] |
| Moderate to severe MDD | Simvastatin | 48 | Double-blind RCT | 20 mg/day for 6 weeks | Simvastatin showed early improvement and response rates with more reductions in HDR scores compared to the placebo group | [59] |
| Youth MDD | Rosuvastatin | 85 | Triple-blind RCT | 10 mg/day for 12 weeks | Aspirin and rosuvastatin can be considered as new adjunctive treatment options for youth MDD | [61] |
| Disease | Statin Type | No. of Patients | Study Design | Dosage/Duration | Main Outcomes | References |
|---|---|---|---|---|---|---|
| Schizophrenia | Simvastatin | 66 | Double-blind RCT | 40 mg daily/8 weeks | Reduction of negative symptoms of schizophrenia | [17] |
| Schizophrenia and Schizoaffective Disorder | Rosuvastatin | 100 | RCT | Unknown/3 months | Reduction of TC, LDL, and TG | [79] |
| Schizophrenia, bipolar psychosis, organic psychosis | Statins including atorvastatin (n = 20), fluvastatin (n = 2), rosuvastatin (n = 2), or simvastatin (n = 4) | 28 | Retrospective, single-center study | Atorvastatin (19 ± 8.5 mg/day), fluvastatin (80 mg/day), rosuvastatin (10 mg/day), and simvastatin (10–20 mg/day)/14–54 days | Reduction of TC, LDL, and TG. | [80] |
| Schizophrenia | Simvastatin | 216 | Two-center double-blind RCT | 20 mg once daily giving rise to 40 mg once daily after 4 weeks/26 weeks | Improvement in symptoms of schizophrenia, no serious side-effects | [81] |
| Psychologic disorders | Statins including simvastatin, atorvastatin, pravastatin, rosuvastatin, fluvastatin, or lovastatin | 46,249 | Retrospective, cohort study | Unknown | A similar risk of developing psychologic disorders | [82] |
| Schizophrenia | Lovastatin | 36 | Double-blind mdd | 20 mg daily/8 weeks | No changes in the PANSS score | [83] |
| Schizophrenia | Pravastatin | 60 | Pilot RCT | 40 mg daily/12 weeks | Reduction of cholesterol and LDL, no changes in cognition and psychiatric scores | [84] |
| Schizophrenia, BD, psychosis | Statins | 47 out of 144 recruited patients | Cluster RCT | Unknown/12 months | No reduction in TC | [85] |
| Disease | Statin Type | No. of Patients | Study Design | Dosage/Duration | Main Outcomes | References |
|---|---|---|---|---|---|---|
| Anxiety and nonadherence to statin therapy | Unknown | 1924 | Prospective cohort study | Not defined | Frequent occurrence of somatic symptoms of anxiety but not psychological symptoms was found to be associated with future nonadherence to statin therapy | [101] |
| New-onset anxiety/depression in patients with head and neck cancer | Unknown | 1632 | A matched longitudinal cohort study | Not defined | Statins use for head and neck cancer patients with hyperlipidemia could decrease the risk of anxiety/depression | [102] |
| Anxiety and depression in patients with asthma-chronic obstructive pulmonary disease overlap syndrome | Unknown | 9139 | Retrospective cohort study | Not defined | The incidences of anxiety and depression were relatively low among users of statins | [103] |
| Disease | Statin Type | No. of Patients | Study Design | Dosage/Duration | Main Outcomes | References |
|---|---|---|---|---|---|---|
| OCD | Atorvastatin | 26 | Double-blind RCT | 10 mg daily/12 weeks | Reduction of Y-BOCS scores | [121] |
| OCD | Atorvastatin | 64 | Double-blind RCT | 40 mg daily/1 year | Reduction of Y-BOCS scores | [122] |
| Disease | Statin Type | No. of Patients | Study Design | Dosage/Duration | Main Outcomes | References |
|---|---|---|---|---|---|---|
| BD and MDD | Atorvastatin | 60 | Double-blinded, placebo-controlled RCT | Atorvastatin 20 mg/day for the 12-week duration of the study. | No significantly different between atorvastatin and placebo groups in MDD relapse or mania relapse or any mood episode relapse | [135] |
| BD | Unknown | 143 | Cross-sectional | Unknown | Statin use is not independently associated with cognitive impairment in older patients with bipolar disease | [139] |
| BD | Lovastatin | 45 | Double-blinded, placebo-controlled RCT | Started with the dose of 10 mg/day, then titrated up to 30 mg/day during one week for 4 weeks | No significant difference between groups in exacerbation or decrease the symptoms of mania in patients with BD | [134] |
| Psychologically healthy | Simvastatin | 621 | RCT | 20 mg or 40 mg or followed up at an average of 152 weeks | No significant differences in the use of psychotropic medication or in reports of symptoms possibly related to mood | [127] |
| Disease | Statin Type | No. of Patients | Study Design | Dosage/Duration | Main Outcomes | References |
|---|---|---|---|---|---|---|
| Delirium | Rosuvastatin | 272 | Multi-center RCT | 40 mg loading dose with 20 mg daily/up to 28 days | No changes in delirium incidence and cognitive impairment | [146] |
| Delirium | Simvastatin | 142 | Double-blind RCT | 80 mg daily/up to 28 days | No reduction in delirium incidence and coma | [154] |
| Delirium | Preoperative statins | 1132 | Retrospective, single-center study | Unknown | A decrease in delirium incidence | [155] |
| Disease | Statin Type | No. of Patients | Study Design | Dosage/Duration | Main Outcomes | References |
|---|---|---|---|---|---|---|
| Autism | Simvastatin | 66 | Double-blind RCT | Children <10 years: 20 mg/day Children >10 years: 40 mg/day for 10 weeks | Significant differences in change of the ABC-C scale irritability and hyperactivity/noncompliance. No significant difference in lethargy/social withdrawal, stereotypic behavior, and inappropriate speech subscale | [163] |
| Neurofibromatosis Type 1-Autism | Simvastatin | 26 | A single-site triple-blind (clinician, family, assessor) placebo-controlled RCT | Simvastatin or placebo in liquid preparation at 0.5 mg/kg in a single daily dose, then increased to 1 mg/kg/day to a maximum of 30 mg/day for 12 weeks | No significant difference in clinical response. Multiparametric imaging suggests possible simvastatin effects in brain areas previously associated with NF1 pathophysiology and the social brain network | [164] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Avan, R.; Sahebnasagh, A.; Hashemi, J.; Monajati, M.; Faramarzi, F.; Henney, N.C.; Montecucco, F.; Jamialahmadi, T.; Sahebkar, A. Update on Statin Treatment in Patients with Neuropsychiatric Disorders. Life 2021, 11, 1365. https://doi.org/10.3390/life11121365
Avan R, Sahebnasagh A, Hashemi J, Monajati M, Faramarzi F, Henney NC, Montecucco F, Jamialahmadi T, Sahebkar A. Update on Statin Treatment in Patients with Neuropsychiatric Disorders. Life. 2021; 11(12):1365. https://doi.org/10.3390/life11121365
Chicago/Turabian StyleAvan, Razieh, Adeleh Sahebnasagh, Javad Hashemi, Mahila Monajati, Fatemeh Faramarzi, Neil C. Henney, Fabrizio Montecucco, Tannaz Jamialahmadi, and Amirhossein Sahebkar. 2021. "Update on Statin Treatment in Patients with Neuropsychiatric Disorders" Life 11, no. 12: 1365. https://doi.org/10.3390/life11121365
APA StyleAvan, R., Sahebnasagh, A., Hashemi, J., Monajati, M., Faramarzi, F., Henney, N. C., Montecucco, F., Jamialahmadi, T., & Sahebkar, A. (2021). Update on Statin Treatment in Patients with Neuropsychiatric Disorders. Life, 11(12), 1365. https://doi.org/10.3390/life11121365








