Functional Orthodontic Treatment of Mandibular Condyle Fractures in Children and Adolescent Patients: An MRI Follow-Up
Abstract
1. Introduction
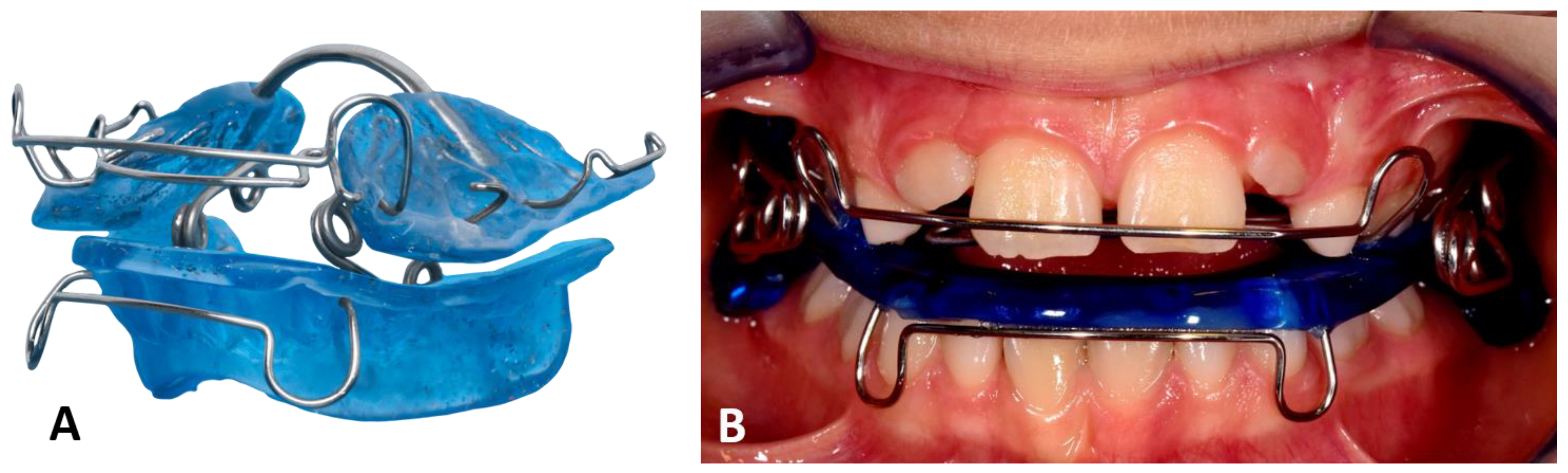
2. Patients and Methods
3. Results
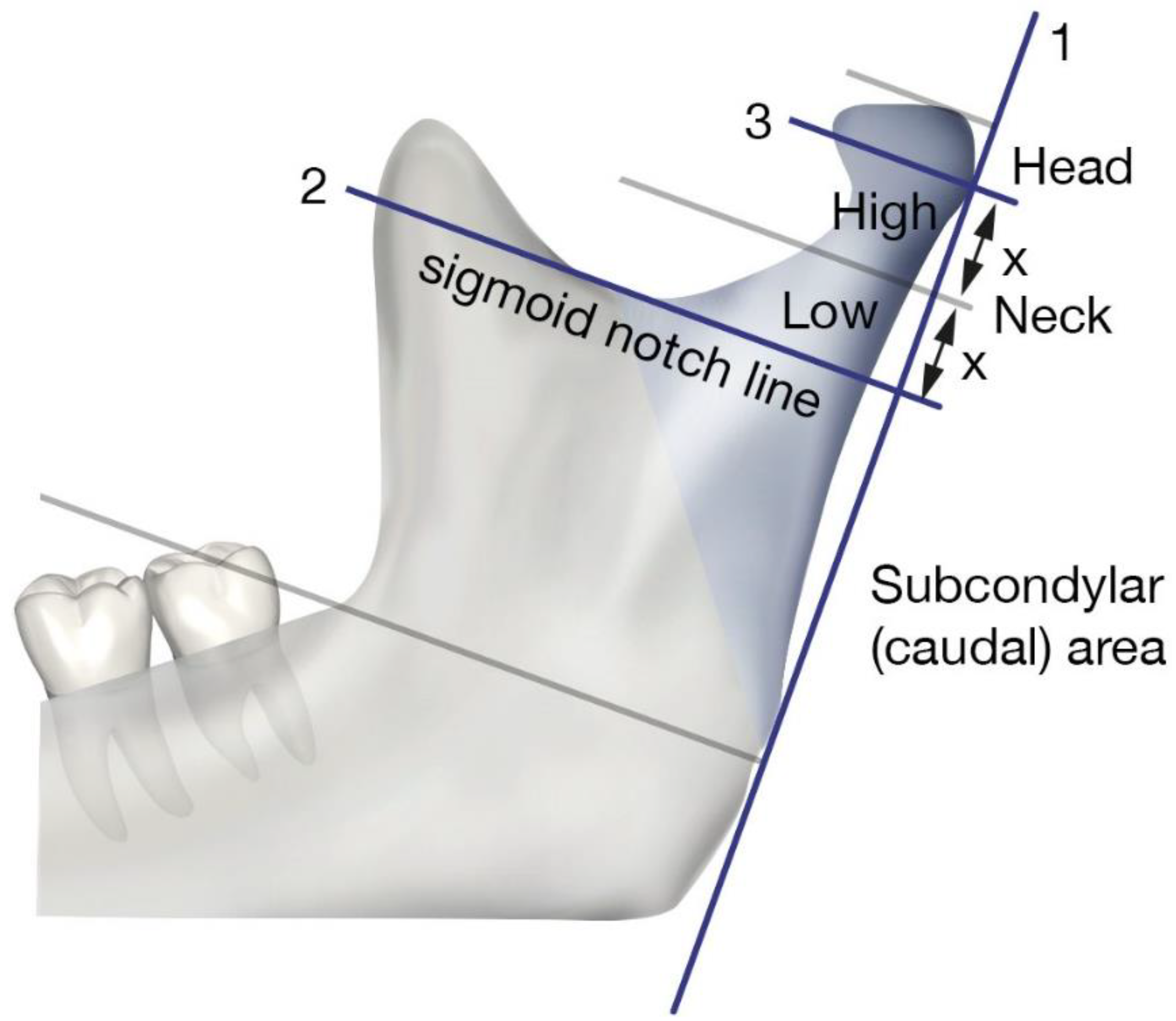
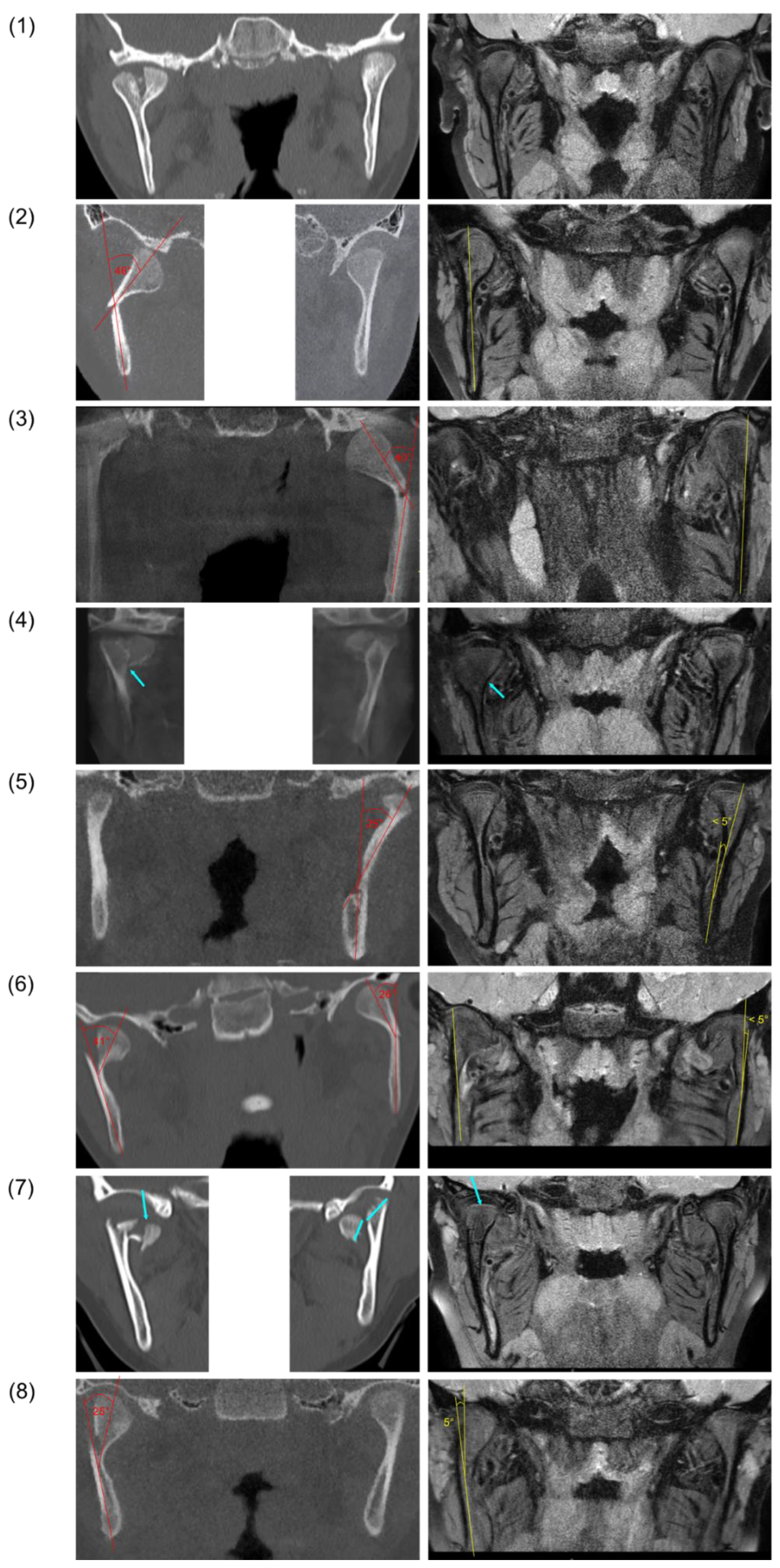
3.1. Patient Collective and Fracture Classification
3.2. Functional Findings
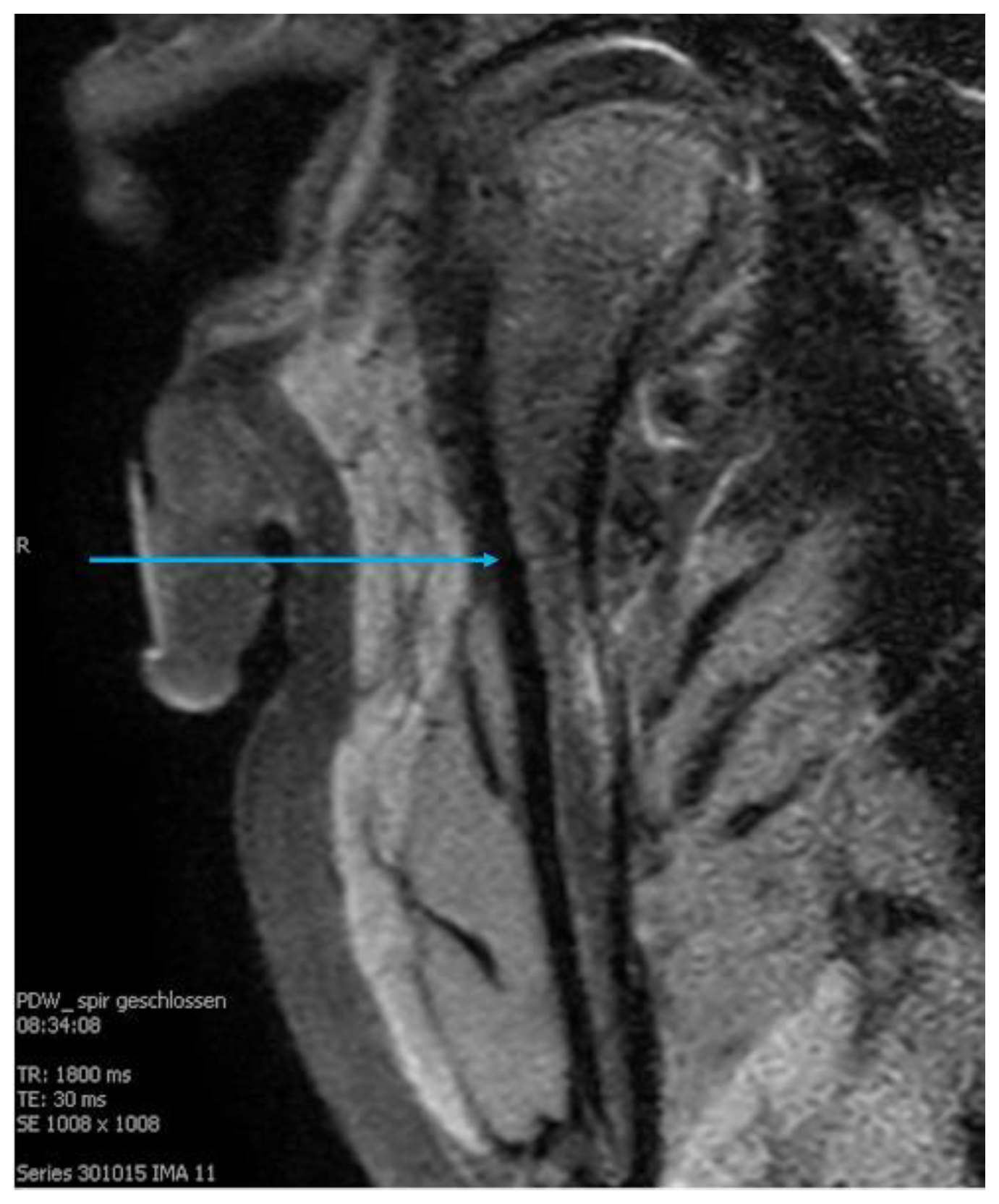
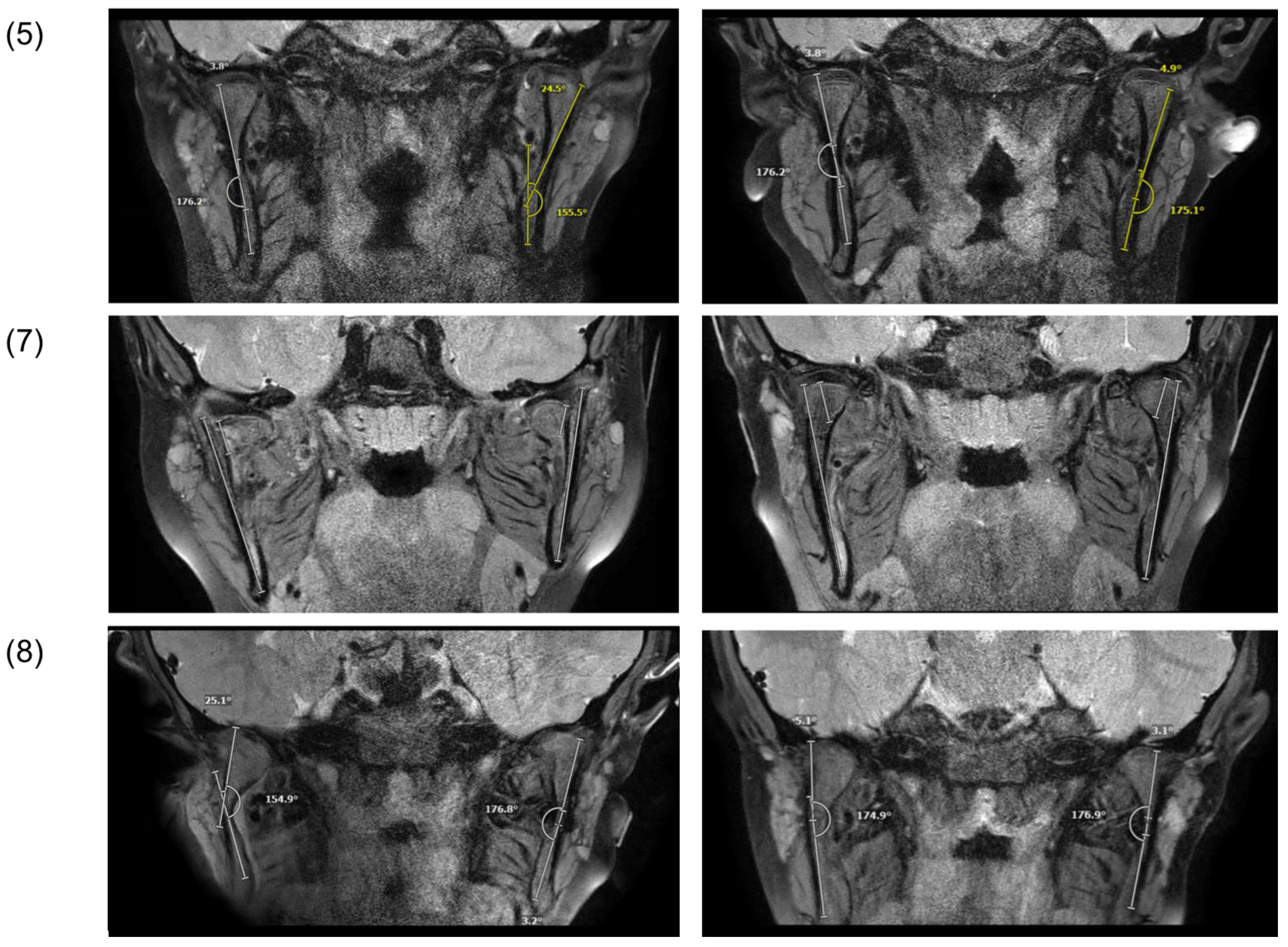
3.3. Radiological Findings
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Theologie-Lygidakis, N.; Chatzidimitriou, K.; Tzerbos, F.; Gouzioti, A.; Iatrou, I. Nonsurgical management of condylar fractures in children: A 15-year clinical retrospective study. J. Craniomaxillofac. Surg. 2016, 44, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Thoren, H.; Hallikainen, D.; Iizuka, T.; Lindqvist, C. Condylar process fractures in children: A follow-up study of fractures with total dislocation of the condyle from the glenoid fossa. J. Oral Maxillofac. Surg. 2001, 59, 768–773. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.M.; Bykowski, M.R.; Cray, J.J.; Naran, S.; Rottgers, S.A.; Shakir, S.; Vecchione, L.; Schuster, L.; Losee, J.E. 215 mandible fractures in 120 children: Demographics, treatment, outcomes, and early growth data. Plast. Reconstr. Surg. 2013, 131, 1348–1358. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R. Open versus closed reduction: Mandibular condylar fractures in children. Oral Maxillofac. Surg. 2012, 16, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Turvey, T.A. Midfacial fractures: A retrospective analysis of 593 cases. J. Oral Surg. 1977, 35, 887–891. [Google Scholar]
- Chang, S.; Yang, Y.; Liu, Y.; Wang, J.; Zhang, W.; Ma, Q. How Does the Remodeling Capacity of Children Affect the Morphologic Changes of Fractured Mandibular Condylar Processes After Conservative Treatment? J. Oral. Maxillofac. Surg. 2018, 76, 1279.e1271–1279.e1277. [Google Scholar] [CrossRef]
- Neff, A.; Chossegros, C.; Blanc, J.L.; Champsaur, P.; Cheynet, F.; Devauchelle, B.; Eckelt, U.; Ferri, J.; Gabrielli, M.F.; Guyot, L.; et al. Position paper from the IBRA Symposium on Surgery of the Head--the 2nd International Symposium for Condylar Fracture Osteosynthesis, Marseille, France 2012. J. Craniomaxillofac. Surg. 2014, 42, 1234–1249. [Google Scholar] [CrossRef]
- Choi, J.; Oh, N.; Kim, I.K. A follow-up study of condyle fracture in children. Int. J. Oral Maxillofac. Surg. 2005, 34, 851–858. [Google Scholar] [CrossRef]
- Ghasemzadeh, A.; Mundinger, G.S.; Swanson, E.W.; Utria, A.F.; Dorafshar, A.H. Treatment of Pediatric Condylar Fractures: A 20-Year Experience. Plast. Reconstr. Surg. 2015, 136, 1279–1288. [Google Scholar] [CrossRef]
- Vesnaver, A. Dislocated pediatric condyle fractures—Should conservative treatment always be the rule? J. Craniomaxillofac. Surg. 2020, 48, 933–941. [Google Scholar] [CrossRef]
- Strobl, H.; Emshoff, R.; Röthler, G. Conservative treatment of unilateral condylar fractures in children: A long-term clinical and radiologic follow-up of 55 patients. Int. J. Oral Maxillofac. Surg. 1999, 28, 95–98. [Google Scholar] [CrossRef]
- Eckelt, U.; Schneider, M.; Erasmus, F.; Gerlach, K.L.; Kuhlisch, E.; Loukota, R.; Rasse, M.; Schubert, J.; Terheyden, H. Open versus closed treatment of fractures of the mandibular condylar process-a prospective randomized multi-centre study. J. Craniomaxillofac. Surg. 2006, 34, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Kahl, B.; Gerlach, K.L. Functional treatment after condylar fractures with and without an activator. Fortschr. Kieferorthop. 1990, 51, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Kahl-Nieke, B.; Fischbach, R.; Gerlach, K.L. CT analysis of temporomandibular joint state in children 5 years after functional treatment of condylar fractures. Int. J. Oral Maxillofac. Surg. 1994, 23, 332–337. [Google Scholar] [CrossRef]
- Lund, K. Mandibular growth and remodelling processes after condylar fracture. A longitudinal roentgencephalometric study. Acta Odontol. Scand. Suppl. 1974, 32, 3–117. [Google Scholar]
- Zhao, Y.M.; Yang, J.; Bai, R.C.; Ge, L.H.; Zhang, Y. A retrospective study of using removable occlusal splint in the treatment of condylar fracture in children. J. Craniomaxillofac. Surg. 2014, 42, 1078–1082. [Google Scholar] [CrossRef]
- Liu, C.K.; Meng, F.W.; Tan, X.Y.; Xu, J.; Liu, H.W.; Liu, S.X.; Huang, H.T.; Yan, R.Z.; Hu, M.; Hu, K.J. Clinical and radiological outcomes after treatment of sagittal fracture of mandibular condyle (SFMC) by using occlusal splint in children. Br. J. Oral Maxillofac. Surg. 2014, 52, 144–148. [Google Scholar] [CrossRef]
- Kahl-Nieke, B.; Fischbach, R. Condylar restoration after early TMJ fractures and functional appliance therapy. Part I: Remodelling. J. Orofac. Orthop. 1998, 59, 150–162. [Google Scholar] [CrossRef]
- Kahl-Nieke, B.; Fischbach, R. A critical evaluation of the functional treatment of mandibular neck fractures in children. The results of a spiral computed tomographic follow-up. Fortschr. Kieferorthop. 1995, 56, 157–164. [Google Scholar] [CrossRef]
- Kahl, B.; Fischbach, R.; Gerlach, K.L. Temporomandibular joint morphology in children after treatment of condylar fractures with functional appliance therapy: A follow-up study us computed tomography. Dentomaxillofac. Radiol. 1995, 24, 37–45. [Google Scholar] [CrossRef]
- Dwivedi, A.N.; Tripathi, R.; Gupta, P.K.; Tripathi, S.; Garg, S. Magnetic resonance imaging evaluation of temporomandibular joint and associated soft tissue changes following acute condylar injury. J. Oral Maxillofac. Surg. 2012, 70, 2829–2834. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.R.; Vig, K.W.; Turvey, T.A. Early fracture of the mandibular condyles: Frequently an unsuspected cause of growth disturbances. Am. J. Orthod. 1980, 78, 1–24. [Google Scholar] [CrossRef]
- Wichelhaus, A.; Haas, R.; Sander, F.G.; Kreidler, J.F. The influence of the spring activator on the mobility of the lower jaw in traumatically injured patients. J. Orofac. Orthop. 1998, 59, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Nys, M.; Van Cleemput, T.; Dormaar, J.T.; Politis, C. Long-term Complications of Isolated and Combined Condylar Fractures: A Retrospective Study. Craniomaxillofacial Trauma Reconstr. 2022, 15, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; He, Y.; Lei, J.; Zhao, Y.; An, J.; Zhang, Y. Acute Intra-Articular Soft Tissue Injury as Seen on Magnetic Resonance Imaging and Its Association with Condylar Fracture Dislocation in Children. J. Oral Maxillofac. Surg. 2019, 77, 2503–2511. [Google Scholar] [CrossRef]
- Tripathi, R.; Sharma, N.; Dwivedi, A.N.; Kumar, S. Severity of Soft Tissue Injury Within the Temporomandibular Joint Following Condylar Fracture as Seen on Magnetic Resonance Imaging and Its Impact on Outcome of Functional Management. J. Oral Maxillofac. Surg. 2015, 73, 2371–2377. [Google Scholar] [CrossRef]
- Kim, B.C.; Lee, Y.C.; Cha, H.S.; Lee, S.H. Characteristics of temporomandibular joint structures after mandibular condyle fractures revealed by magnetic resonance imaging. Maxillofac. Plast. Reconstr. Surg. 2016, 38, 24. [Google Scholar] [CrossRef]
- Stähli, C.; Eliades, T.; Papageorgiou, S.N. Functional appliance treatment for mandibular fractures: A systematic review with meta-analyses. J. Oral Rehabil. 2021, 48, 945–954. [Google Scholar] [CrossRef]
- Cornelius, C.P.; Neff, A.; Thieringer, F.; Kunz, C.; Smolka, W.; Reichert, T.; Audigé, L.; Prein, J. Unterkieferfrakturen nach AO-CMF-Trauma-Klassifikation. Der MKG-Chirurg. 2017, 10, 104–112. [Google Scholar] [CrossRef]
- Kaeppler, G. Einteilung von Unterkieferfrakturen nach der AO-CMF-Trauma-Klassifikation. Der MKG-Chirurg. 2017, 10, 127–133. [Google Scholar] [CrossRef]
- Neff, A.; Cornelius, C.-P.; Rasse, M.; Torre, D.D.; Audigé, L. The Comprehensive AOCMF Classification System: Condylar Process Fractures—Level 3 Tutorial. Craniomaxillofacial Trauma Reconstr. 2014, 7, S044–S058. [Google Scholar] [CrossRef] [PubMed]
- Sander, F. Rotationen des Unterkiefers durch den Federaktivator bei funktionellen Bewegungen. Prakt. Kieferorthop. 1990, 4, 183–188. [Google Scholar]
- Sander, F. Biomechanische Aspekte des Federaktivators wahrend des Nachtschlafes. Prakt. Kieferorthop. 1991, 5, 17–28. [Google Scholar]
- Kahl-Nieke, B.; Fischbach, R. Condylar restoration after early TMJ fractures and functional appliance therapy. Part II: Muscle evaluation. J. Orofac. Orthop. 1999, 60, 24–38. [Google Scholar] [CrossRef]
- Bumann, A.; Lotzmann, U.; Mah, J. TMJ Disorders and Orofacial Pain: The Role of Dentistry in a Multidisciplinary Diagnostic Approach; Thieme Medical Publishers: Stuttgart, Germany, 2002. [Google Scholar]
- Takaku, S.; Yoshida, M.; Sano, T.; Toyoda, T. Magnetic resonance images in patients with acute traumatic injury of the temporomandibular joint: A preliminary report. J. Craniomaxillofac. Surg. 1996, 24, 173–177. [Google Scholar] [CrossRef]
- Wang, P.; Yang, J.; Yu, Q. MR imaging assessment of temporomandibular joint soft tissue injuries in dislocated and nondislocated mandibular condylar fractures. AJNR Am. J. Neuroradiol. 2009, 30, 59–63. [Google Scholar] [CrossRef]
- Dahlström, L.; Kahnberg, K.E.; Lindahl, L. 15 years follow-up on condylar fractures. Int. J. Oral Maxillofac. Surg. 1989, 18, 18–23. [Google Scholar] [CrossRef]
- Zhou, H.H.; Lv, K.; Yang, R.T.; Li, Z.; Li, Z.B. Extracapsular Condylar Fractures Treated Conservatively in Children: Mechanism of Bone Remodelling. J. Craniofac. Surg. 2021, 32, 1440–1444. [Google Scholar] [CrossRef] [PubMed]
- Du, C.; Xu, B.; Zhu, Y.; Zhu, M. Radiographic evaluation in three dimensions of condylar fractures with closed treatment in children and adolescents. J. Craniomaxillofac. Surg. 2021, 49, 830–836. [Google Scholar] [CrossRef]
- Nørholt, S.E.; Krishnan, V.; Sindet-Pedersen, S.; Jensen, I. Pediatric condylar fractures: A long-term follow-up study of 55 patients. J. Oral Maxillofac. Surg. 1993, 51, 1302–1310. [Google Scholar] [CrossRef]
- Köhler, J.A. Diagnostik und Therapie der Kieferfrakturen: Mit 405 Abb. u. 213 Skizzen; Hüthig: Heidelberg, Germany, 1951. [Google Scholar]
- Wassmund, M. Frakturen und Luxationen des Gesichtsschädels: Unter Berücksichtigung der Komplikationen des Hirnschädels: Ihre Klinik und Therapie: Praktisches Lehrbuch; H. Meusser: Berlin, Germany, 1927. [Google Scholar]
- Reichenbach, E. The problem of bone fracture surgery in the region of the facial bones. Dtsch. Zahnarztl. Z. 1953, 17, 376–399. [Google Scholar] [PubMed]
- Lindahl, L. Condylar fractures of the mandible. I. Classification and relation to age, occlusion, and concomitant injuries of teeth and teeth-supporting structures, and fractures of the mandibular body. Int. J. Oral Surg. 1977, 6, 12–21. [Google Scholar] [CrossRef]
- Spiessl, B.; Kieferköpfchenfrakturen, S.K.G.-U. Spezielle Frakturen-und Luxationslehre. Band l/1: Gesichtsschädel ed; Thieme Medical Publishers: Stuttgart, Germany, 1972. (In German) [Google Scholar]
- Loukota, R.A.; Eckelt, U.; De Bont, L.; Rasse, M. Subclassification of fractures of the condylar process of the mandible. Br. J. Oral Maxillofac. Surg. 2005, 43, 72–73. [Google Scholar] [CrossRef] [PubMed]
- Staderini, E.; Patini, R.; Tepedino, M.; Gasparini, G.; Zimbalatti, M.A.; Marradi, F.; Gallenzi, P. Radiographic Assessment of Pediatric Condylar Fractures after Conservative Treatment with Functional Appliances-A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 9204. [Google Scholar] [CrossRef] [PubMed]
- Hotz, R.P. Functional jaw orthopedics in the treatment of condylar fractures. Am. J. Orthod. 1978, 73, 365–377. [Google Scholar] [CrossRef]
- Eberhardt, K.; Sahm, G. CT morphology and function of the temporomandibular joint following conservative functional treatment of temporomandibular joint fractures. Radiologe 1990, 30, 541–546. [Google Scholar]
- Moss, M.L. The functional matrix hypothesis revisited. 3. The genomic thesis. Am. J. Orthod. Dentofacial Orthop. 1997, 112, 338–342. [Google Scholar] [CrossRef]
- Moss, M.L. The functional matrix hypothesis revisited. 4. The epigenetic antithesis and the resolving synthesis. Am. J. Orthod. Dentofacial Orthop. 1997, 112, 410–417. [Google Scholar] [CrossRef]
- Moss, M.L. The functional matrix hypothesis revisited. 1. The role of mechanotransduction. Am. J. Orthod. Dentofacial Orthop. 1997, 112, 8–11. [Google Scholar] [CrossRef]
- Moss, M.L. The functional matrix hypothesis revisited. 2. The role of an osseous connected cellular network. Am. J. Orthod. Dentofacial Orthop. 1997, 112, 221–226. [Google Scholar] [CrossRef]
- Lindahl, L.; Hollender, L. Condylar fractures of the mandible. II. a radiographic study of remodeling processes in the temporomandibular joint. Int. J. Oral Surg. 1977, 6, 153–165. [Google Scholar] [CrossRef]
- Li, Z.; Zhang, W.; Li, Z.B.; Li, J.R. Mechanism in favorable prognosis of pediatric condylar fractures managed by closed procedures: An experimental study in growing rats. Dent. Traumatol. 2010, 26, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.A.; Louvrier, A.; Colletti, G.; Wolford, L.M.; Biglioli, F.; Ragaey, M.; Meyer, C.; Ellis, E., 3rd. Does the surgical approach for treating mandibular condylar fractures affect the rate of seventh cranial nerve injuries? A systematic review and meta-analysis based on a new classification for surgical approaches. J. Craniomaxillofac. Surg. 2018, 46, 398–412. [Google Scholar] [CrossRef] [PubMed]
- Berner, T.; Essig, H.; Schumann, P.; Blumer, M.; Lanzer, M.; Rücker, M.; Gander, T. Closed versus open treatment of mandibular condylar process fractures: A meta-analysis of retrospective and prospective studies. J. Craniomaxillofac. Surg. 2015, 43, 1404–1408. [Google Scholar] [CrossRef] [PubMed]
- Asim, M.A.; Ahmed, W.; Ibrahim, M.W.; Ali Bukhari, S.G.; Khan, M.N. Assessment of complications of the open treatment of mandibular condylar fractures. J. Pak. Med. Assoc. 2021, 71, 1689–1692. [Google Scholar] [CrossRef] [PubMed]
- Skroch, L.; Fischer, I.; Meisgeier, A.; Kozolka, F.; Apitzsch, J.; Neff, A. Condylar remodeling after osteosynthesis of fractures of the condylar head or close to the temporomandibular joint. J. Craniomaxillofac. Surg. 2020, 48, 413–420. [Google Scholar] [CrossRef]
- Zhou, H.H.; Lv, K.; Yang, R.T.; Li, Z.; Li, Z.B. Restoration of Ramus Height in Child Patients with Extracapsular Condylar Fractures: Is This Mission Almost Impossible to Accomplish? J. Craniofac. Surg. 2021, 32, e293–e296. [Google Scholar] [CrossRef]
- Leake, D.; Doykos, J., 3rd; Habal, M.B.; Murray, J.E. Long-term follow-up of fractures of the mandibular condyle in children. Plast. Reconstr. Surg. 1971, 47, 127–131. [Google Scholar] [CrossRef]
| Case | Sex | Age at Trauma | Type of Trauma/Etiology | Fracture Side | Type of Fracture AO-CMF | Specific Level 3 Condylar Process System Code [30] | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Location | Fragmentation | Vertical Apposition | Sidewards Displacement | Angulation | Displacement Head Fragment/Fossa | Displacement Caudal Fragment/Fossa | Distortion of Head | Loss of Ramus Height | Angulation in ° | Height Loss in mm | ||||||
| (1) | M | 7 years, 5 months | Bicycle | Right | Condylar head fracture | M | 0 | 0 | - | - | 1, a | - | 0 | 0 | - | 0 mm |
| (2) | M | 5 years, 6 months | Bicycle | Right | Low condylar neck fracture | - | 0 | - | 1 | 2, m | 1, a, m | 0 | 0 | 1 | 46° | 3.2 mm |
| (3) | M | 14 years, 9 months | Fall | Left | Low condylar neck fracture | - | 0 | - | 0 | 1, m | 1, m | 0 | 0 | 1 | 40° | 5 mm |
| (4) | F | 7 years, 3 months | Scooter | Bilateral | Right: condylar head fracture | M | 0 | 0 | - | - | 0 | - | 0 | 0 | - | 0 mm |
| Left: condylar head fracture | M | 1 | 0 | - | - | 0 | - | 0 | 0 | - | 0 mm | |||||
| (5) | M | 10 years, 7 months | Play | Left | Subcondylar fracture | - | 0 | - | 1 | 1, l | 1 | 0 | 0 | 1 | 25° | 4.5 mm |
| (6) | F | 8 years, 10 months | Play | Bilateral | Right: high condylar neck fracture | - | 0 | - | 1 | 1, m | 0 | 0 | 0 | 1 | 41° | 4 mm |
| Left: low condylar neck fracture | - | 0 | - | 0 | 1, m | 0 | 0 | 0 | 1 | 26° | 2 mm | |||||
| (7) | M | 8 years, 6 months | Bicycle | Bilateral | Right: condylar head fracture | P | 1 | 2 | - | - | 1, a | - | 1 | 1 | - | 5.5 mm |
| Left: condylar head fracture | P | 2 | 1 | - | - | 1, a, m | - | 1 | 1 | - | 9 mm | |||||
| (8) | M | 5 years, 7 months | Fall | Right | Subcondylar fracture | - | 0 | - | 1 | 1, m | 0 | 0 | 0 | 1 | 25° | 3 mm |
| Sign | No. Patients (t0) | No. Patients (t1) | % (t1) |
|---|---|---|---|
| Reduced range of mouth opening | 8/8 | 0/8 | 0 |
| Reduced range of lateral movement | 8/8 | 0/8 | 0 |
| Reduced range of protrusion | 8/8 | 0/8 | 0 |
| Arthralgia | 7/8 | 0/8 | 0 |
| Myalgia | 2/8 | 0/8 | 0 |
| Joint sounds (clicking or crepitation) | 2/8 | 2/8 | 25.0 |
| Mandibular midline deviation during mouth opening | 8/8 | 6/8 | 75.0 |
| Mandibular midline deviation in centric occlusion | 8/8 | 6/8 | 75.0 |
| Alteration to occlusal relationship (crossbite or open bite) | 4/8 | 0/8 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sabbagh, H.; Nikolova, T.; Kakoschke, S.C.; Wichelhaus, A.; Kakoschke, T.K. Functional Orthodontic Treatment of Mandibular Condyle Fractures in Children and Adolescent Patients: An MRI Follow-Up. Life 2022, 12, 1596. https://doi.org/10.3390/life12101596
Sabbagh H, Nikolova T, Kakoschke SC, Wichelhaus A, Kakoschke TK. Functional Orthodontic Treatment of Mandibular Condyle Fractures in Children and Adolescent Patients: An MRI Follow-Up. Life. 2022; 12(10):1596. https://doi.org/10.3390/life12101596
Chicago/Turabian StyleSabbagh, Hisham, Trayana Nikolova, Sara Carina Kakoschke, Andrea Wichelhaus, and Tamara Katharina Kakoschke. 2022. "Functional Orthodontic Treatment of Mandibular Condyle Fractures in Children and Adolescent Patients: An MRI Follow-Up" Life 12, no. 10: 1596. https://doi.org/10.3390/life12101596
APA StyleSabbagh, H., Nikolova, T., Kakoschke, S. C., Wichelhaus, A., & Kakoschke, T. K. (2022). Functional Orthodontic Treatment of Mandibular Condyle Fractures in Children and Adolescent Patients: An MRI Follow-Up. Life, 12(10), 1596. https://doi.org/10.3390/life12101596





