Abstract
The efficacy of corticosteroids (CS) for dry eye disease (DED) has been investigated in the clinical setting. The present study investigated whether topical CS application improves the clinical outcome at last follow-up compared to the baseline. The present study was conducted according to the PRISMA 2020. All the randomized clinical trials (RCTs), which investigated the efficacy of corticosteroids in the management of DED, were accessed. In September 2022, the following databases were accessed: Pubmed, Web of Science, Google Scholar, and Embase. The following data were extracted at baseline and at last follow-up: Ocular Surface Disease Index (OSDI), tear breakup time test (TBUT), Schirmer I test (SIT), and corneal staining. Data from 425 patients were retrieved. A total of 69.4% (295 of 425 patients) were women. CS were effective to improve SIT (p = 0.02) and corneal staining (p = 0.003) at the last follow-up of 10.0 ± 15.3 weeks. TBUT was greater in the CS than in the control group at the last follow-up (p = 0.002). Concluding, topical CS administration led to an increase of SIT and a reduction of corneal staining at a mean of 10 weeks follow-up in patients with DED. Compared to a control group, topical CS administration evidenced greater values of TBUT. Altogether, a good safety profile was witnessed in DED patients receiving CS. However, different safety profiles of different CS formulations were not investigated due to a lack of quantitative data. The exact dosing frequency, duration of therapy, and favorable potency of the CS are still under investigation. Future randomized, controlled trials with larger sample sizes are warranted to provide higher-quality evidence to establish the role of CS in DED.
1. Introduction
Dry eye disease (DED) is very common in adults, with prevalence rates up to 50% [1]. Symptoms of DED include ocular irritation, hyperemia, dryness, and visual disorders, which can significantly affect the patients’ quality of life [1,2]. DED is diagnosed clinically by various tests, including the Schirmer I test (SIT), tear breakup time (TBUT), and corneal and conjunctival staining [3]. In addition, self-reported questionnaires, such as the Ocular Surface Disease Index (OSDI), are used [4].
Generally, DED results from insufficient production or excessive evaporation of tears promoting ocular surface inflammation [5]. The exact etiology of DED is still largely unknown [6]. The instability of the tear film leads to a loss of its homeostatis, which subsequently causes ocular surface inflammation and neuro-sensory abnormalities [7]. The resulting oxidative and shear stress and corneal epithelial cell damage might trigger a vicious cycle of ocular surface disruption leading to further stimulation of the inflammatory cascade by initiating both innate and adaptive immune responses [7]. An increased activation of nuclear factor kB (NF-kB) and stress-related mitogen-activated protein kinases (MAPK) trigger the production of the pro-inflammatory cytokines interleukin 1α (IL-1α), IL-1ß, IL-6, IL-8, tumor necrosis factor-α (TNF-α), and matrix metalloproteinases (MMPs) 1, 3, and 9 by corneal epithelial cells [8]. Accordingly, these cytokines have been identified in the tear film of patients with DED [9]. Antigen-presenting cells are stimulated by these cytokines, leading to an activation of CD4+ helper T cell 1, helper T cell 17, and autoantibody-secreting B cells [10]. A chronic immune response with persisting signs and symptoms of DED might be initiated [7].
Tear substitutes are the most common treatment modality for mild and moderate forms of DED [11]. However, they do not address the underlying pathogenetic factors of DED, including ocular surface inflammation [12]. Although the efficacy of anti-inflammatory agents such as lifitegrast or cyclosporine for the treatment of DED has been shown, topical corticosteroids (CS) might offer possible advantages, including the early onset of effect [12]. CS halt the inflammatory cascade by inhibiting phospholipase A2, thus impeding the conversion of phospholipids to arachidonic acid [13]. Furthermore, CS form a corticosteroid–glucose receptor complex within the cell cytosol, which downregulates angiogenesis, oxidative stress, apoptosis, and the gene expression of pro-inflammatory cytokines [13]. Moreover, CS stabilize intra- and extracellular membranes and modulate the transcription factors in mast cell nuclei [14,15]. Nevertheless, CS have been implicated with potential side effects, such as cataract formation and intraocular pressure (IOP) elevation [16]. Approximately one third of the population are moderate steroid responders, with 5% responding with IOP spikes greater than 15 mmHg after 4–6 weeks of topical CS application [17]. Therefore, topical CS are only used for a short period of time. Prednisolone and dexamethasone are classified as moderate potency formulations [18], whereas commercially available low-potency CS eye drops include loteprednol etabonate, fluorometholone, and rimexolone [19]. The low potency CS are rapidly hydrolyzed into inactive metabolites with minimal or even no effect on IOP [20]. Moreover, long-term use of topical CS is presumed to depress the immune function of the ocular surface, and thus increasing the risk of infectious, especially herpetickeratitis [21].
The efficacy of topical CS application for DED has been investigated in the clinical setting [12,15,22,23,24,25,26,27,28,29]. However, a detailed review of the literature of this evidence is lacking. Therefore, this study investigated the efficacy and feasibility of CS for DED. We evaluated the improvement from baseline to last follow-up and we performed a meta-analysis comparing CS to other commonly used pharmacological treatments. Our hypothesis is that topical CS are an efficacious treatment for DED with comparable results to other commonly used pharmacological treatments. However, long-term side effects have to be evaluated.
2. Materials and Methods
2.1. Eligibility Criteria
All of the randomized clinical trials (RCTs) which evaluated the topical steroids application for DED were accessed. Only studies published in peer reviewed journals were eligible. According to the authors’ language capabilities, articles in English, German, Italian, French, and Spanish were eligible. Only articles with level I of evidence, according to the Oxford Centre of Evidence-Based Medicine [30], were included. Reviews, opinions, letters, and editorials were not considered. Animals, in vitro, biomechanics, computational, and cadaveric studies were not eligible. Studies which combined steroids with other treatments (e.g., hyaluronic acid, antibiotics, immunomodulators) were not considered, nor were those which reported data from steroids application and from the comparator group not separately. Only studies which reported quantitative data under the outcomes of interest were considered.
2.2. Search Strategy
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the 2020 PRISMA statement [31]. The PICOD algorithm was preliminarily pointed out:
- P (Population): DED;
- I (Intervention): isolated topical steroids application;
- C (Comparison): efficacy and safety;
- O (Outcomes): Ocular Surface Disease Index; tear breakup time test; Schirmer I test; corneal staining;
- D (Design): RCTs.
In September 2022 PubMed, Web of Science, Google Scholar, and Embase were accessed using the Boolean operator AND/OR. No time constrains were used for the search. The following keywords were used in combination: xerophthalmus, dry eye disease, xeropthalmia, steroids, corticosteroids cortisone, cortisol, hydrocortisone, dexamethasone, prednisolone, fluorometholone, loteprednol, medrysone, management, therapy, Ocular Surface Disease Index; Tear breakup time test; TBUT; Schirmer I test, SIT; Corneal Staining.
2.3. Selection and Data Collection
Two authors (F.M. and J.P.) independently performed the database search. All of the resulting titles were screened and, if suitable, the abstract was accessed. The full-text of the abstracts which matched the topic were accessed. If the full-text was not available or not accessible, the article was excluded. A cross reference of the bibliography of the full-text articles were also screened for inclusion. Any disagreement was discussed and settled by consensus.
2.4. Data Items
Two authors (F.M. and J.P.) independently performed data extraction. The following data were extracted at baseline and at last follow-up: Disease Index (OSDI) [32], tear breakup time test (TBUT) [33], Schirmer I test (SIT) [34], and corneal staining [35]. The primary outcome of interest was to investigate whether CS application will improve the clinical outcome at last follow-up compared to the baseline. The secondary outcome of interest was to compare therapy with topical CS to a control group.
2.5. Methodological Quality Assessment
The assessment of the methodology quality among the included studies was performed by one author (J.P.). The Review Manger software (The Nordic Cochrane Collaboration, Copenhagen, Denmark) version 5.3 was used. The focus was on the following biases: selection, detection, performance, reporting, attrition, and other biases. To assess the publication risk of bias, the funnel plot of the most commonly reported outcome was performed.
2.6. Synthesis Methods
The statistical analysis was performed by one author (F.M.) following the guidelines in the Cochrane Handbook for Systematic Reviews of Interventions [9]. To assess the improvement from baseline to the last follow-up, the mean difference (MD), standard error (SE), T value, and the unpaired T-test were evaluated using the IBM SPSS software version 25. For the comparisons, the meta-analyses were conducted using the Review Manager software (The Nordic Cochrane Collaboration, Copenhagen, Denmark) version 5.3. Data were analyzed using the inverse variance and mean difference (MD) effect measure. The comparisons were performed with a fixed model effect as set up. Heterogeneity was assessed through the Higgins-I2 test. If I2 test > 50%, a random model effect was adopted. The confidence intervals (CI) were set at 95% in all comparisons. The overall effect was considered statistically significant if p < 0.05.
3. Results
3.1. Study Selection
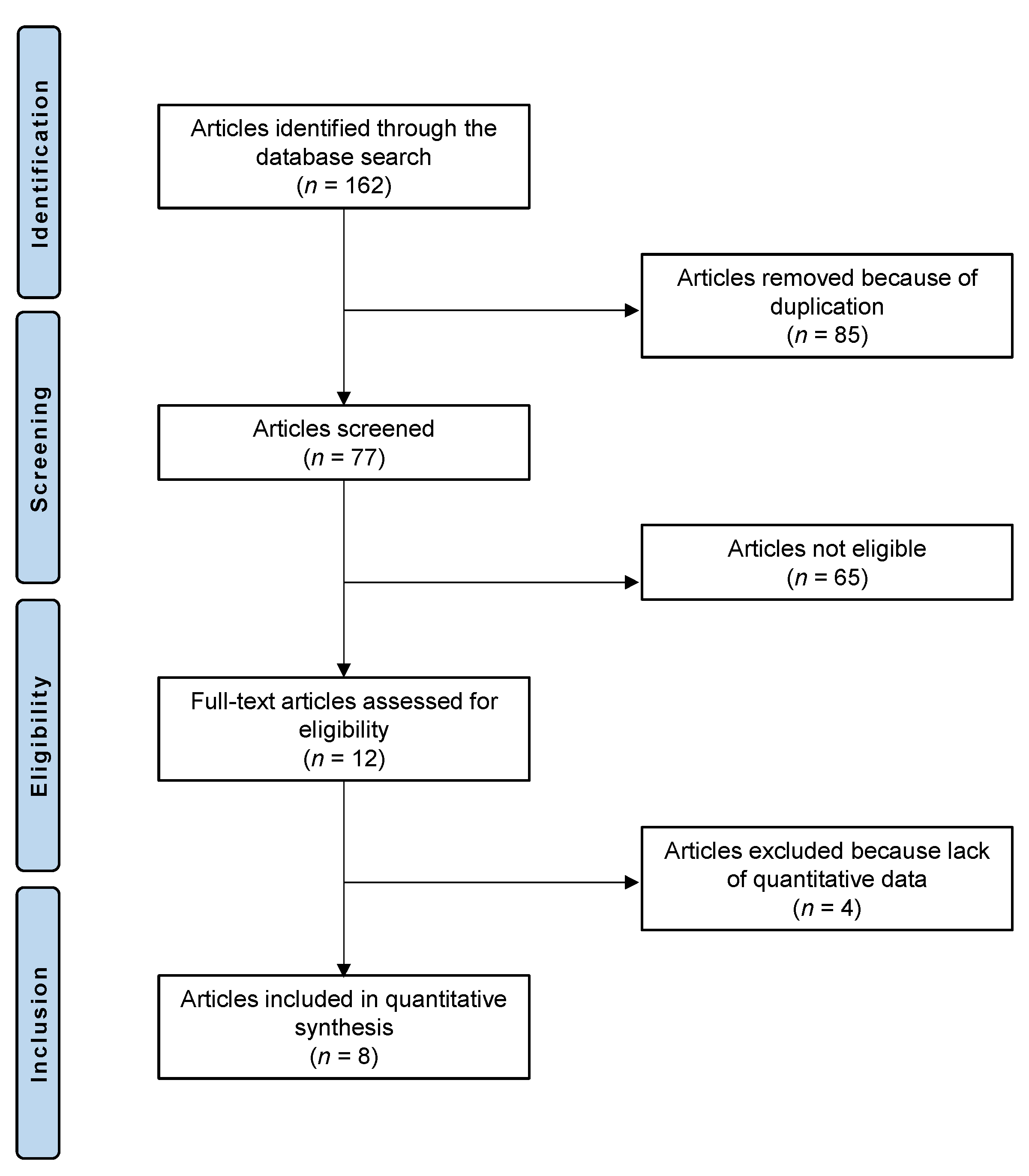
The literature search resulted in 162 RCTs which evaluated the effectiveness of acupuncture for DED. Of them, 85 were excluded because of redundancy. Another 65 articles were excluded because they did not match the eligibility criteria: type of study (n = 29), not focusing on the topic (n = 24), combining steroids with other treatments (n = 8), and language incompatibility (n = 4). Four further studies did not report quantitative data under the endpoints of interest. Finally, eight RCTs were eligible for analysis. The flow chart of the literature search is shown in Figure 1.
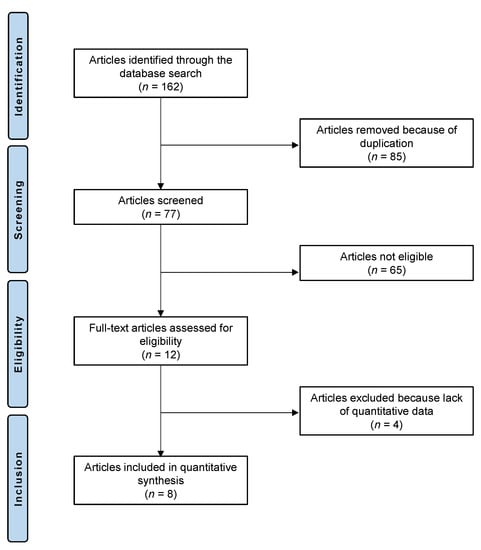
Figure 1.
Flow chart of the literature search.
3.2. Study Risk of Bias Assessment
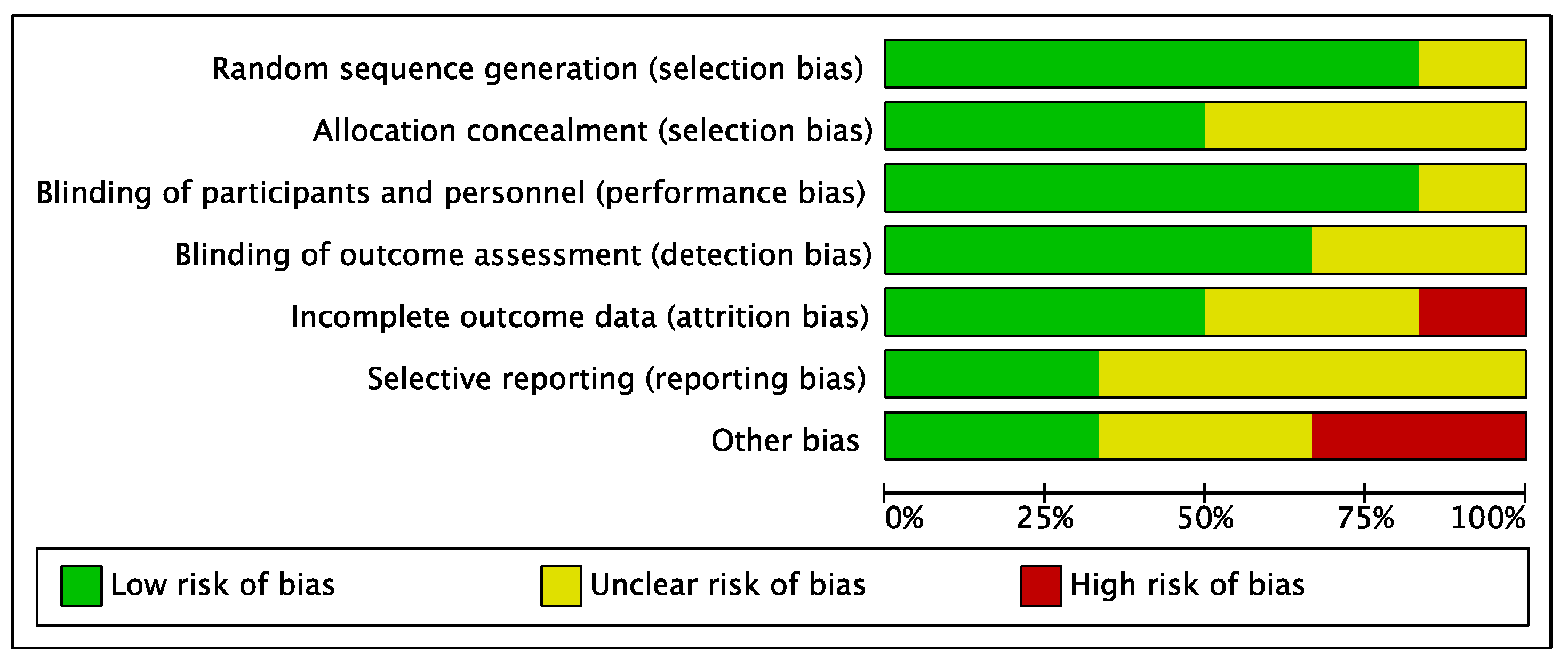
Given the randomized design of the included studies, the risk of selection bias was low. Similarly, the risk of performance, selection, and detection biases were low. The overall risks of attrition and reporting biases were low to moderate (Figure 2).
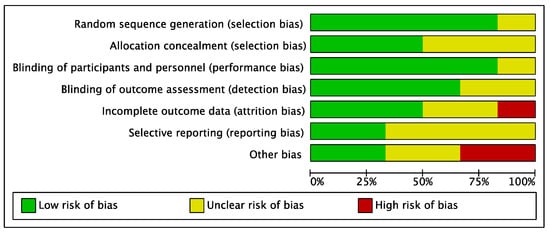
Figure 2.
Methodological quality assessment.
3.3. Study Characteristics and Results of Individual Studies
Data from 425 patients were retrieved. A total of 69.4% (295 of 425 patients) were women. The mean follow-up was 10.0 ± 15.3 weeks. The mean age was 56.4 ± 4.5 years. Baseline comparability between the placebo and active treatment was found in terms of TBUT (p = 0.1), OSDI (p = 0.2), SIT (p = 0.09), and corneal staining (p = 0.1). Generalities of the included studies are reported in Table 1.

Table 1.
Generalities and patient baseline of the included studies.
3.4. Efficacy of Steroids
CS were effective in reducing SIT (p = 0.02), corneal staining (p = 0.003). OSDI (p = 0.1) and TBUT (p = 0.2) did not evidence significant improvement at last follow-up. These results are shown in greater detail in Table 2.

Table 2.
Analysis of the improvement of TBUT (s), OSDI (points), SIT (mm), and corneal staining (points) from baseline to the last follow-up.
3.5. Meta-Analyses
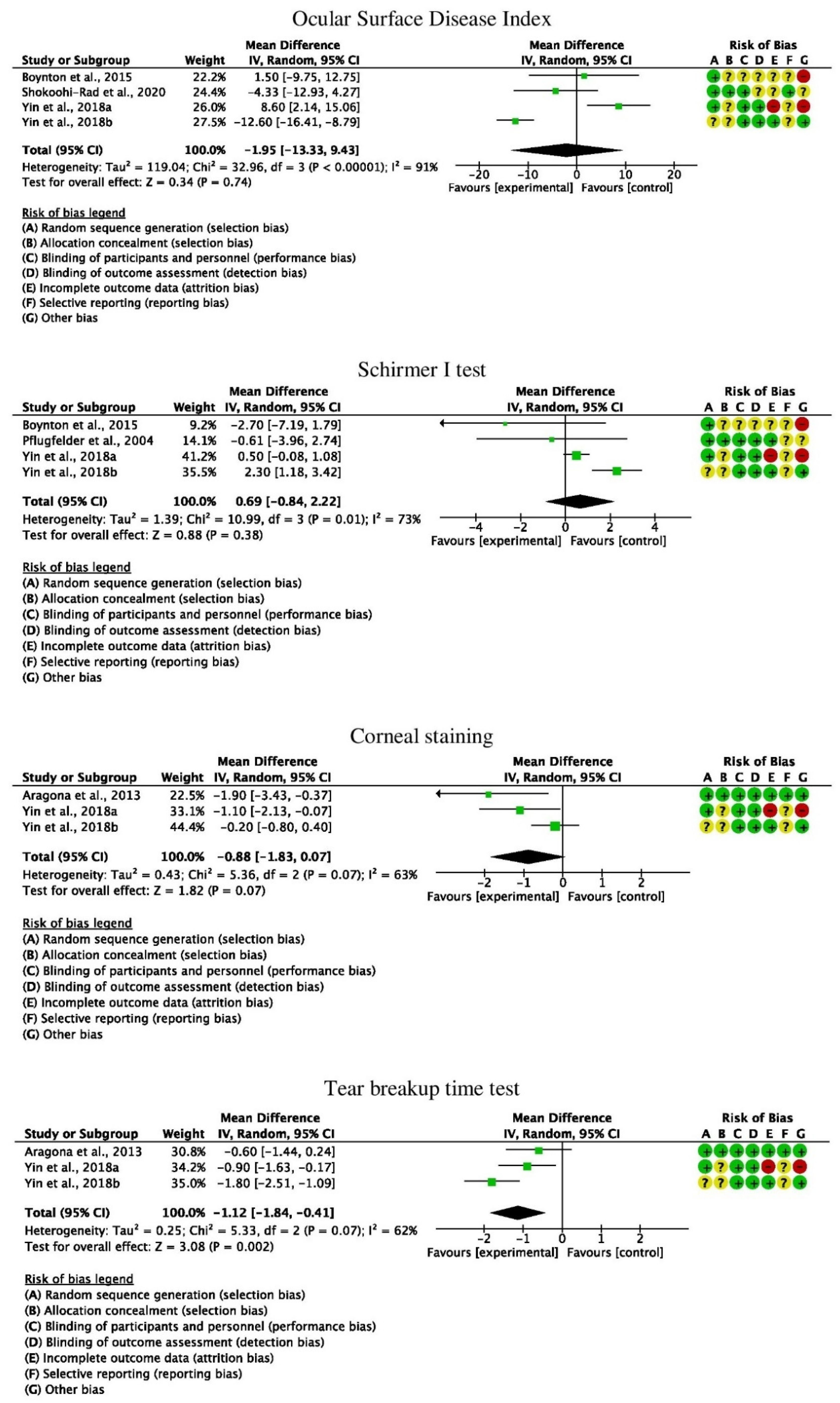
The meta-analyses demonstrated no superiority of topical steroids application compared to any of the considered control groups in OSDI, SIT and corneal staining. TBUT was greater in the CS than in the control group (p = 0.002) (Figure 3).
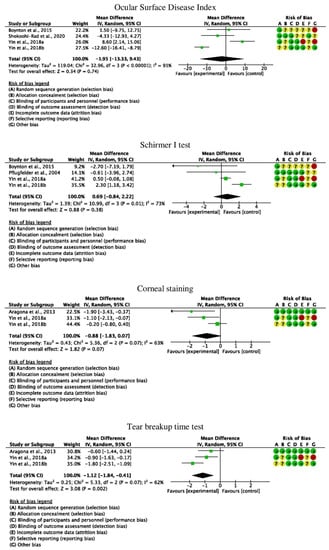
Figure 3.
Forest plots of the meta-analyses [12,15,22,23,29,36,37,38].
4. Discussion
According to the main findings of the present study, topical CS administration led to an increase of SIT and a reduction of corneal staining at a mean of 10 weeks follow-up in patients with DED. Compared to a control group, topical CS administration evidenced greater values of TBUT. Altogether, a good safety profile was witnessed in DED patients receiving CS.
To date, artificial tears are considered the first-line therapy in the management of DED [11]. However, the application of artificial tears does not address the underlying inflammatory causes of DED in patients with severe symptoms [12]. Inflammation is presumed to play a key pathogenic role for DED [39]. The efficacy of anti-inflammatory therapy, such as lifitegrast or cyclosporine, in DED has been reported previously [12]. CS are the most effective anti-inflammatory therapy for many chronic inflammatory diseases [40]. In ophthalmology, topical CS are approved for CS-responsive inflammatory conditions of the cornea, conjunctiva, and the anterior segment of the eye [29]. Previously, studies found that CS decrease the production of proinflammatory cytokines by the corneal and conjunctival epithelium [41]. CS have different propensities for side effects. Early generation CS, such as dexamethasone and prednisolone, have a strong side effect profile. In contrast, newer CS, such as loteprednol etabonate, show less risk of IOP elevation [42].
Kallab et al. investigated the efficacy and safety of preservative-free hydrocortisone 0.335% either for 12 days four times daily followed by 2 days twice daily (intense treatment group) or for 8 days three times daily followed by 3 days twice daily instillation (standard treatment group). They included 60 DED patients with a mean age of 51 years. OSDI significantly decreased in both treatment groups. The treatment effect remained significant 2 weeks after the treatment phase, indicating a prolonged effect of the hydrocortisone treatment. The absence of changes in IOP suggested a good safety profile of hydrocortisone [12]. The reduced likelihood for side effects was attributed to the less pronounced penetration through the ocular surface by CS formulations such as hydrocortisone [12,43]. Moreover, the authors strongly recommend the use of preservative-free CS formulations to avoid toxic side effects and to allow for a high tolerability on the ocular surface [12]. No cataract formation was witnessed. However, with a follow-up of only 4 weeks, long-term data regarding cataract formation are missing [12]. Shokoohi-Rad et al. evaluated the efficacy of a preoperative dose of betamethasone acetate 0.1% compared to placebo on DED after cataract surgery. Sixty-two patients with a mean age of 69.2 years were included. No significant effect of a preoperative betamethasone acetate instillation on postoperative DED indices, including OSDI, was reported in their study [23]. However, in the study by Shokoohi-Rad et al., only two measurements for the evaluation of DED were used: the meniscometry test and OSDI questionnaire [23]. Therefore, no conclusions can be drawn on other relevant parameters, such as the SIT or TBUT score. The authors conclude that betamethasone acetate 0.1% has no effect over placebo in DED after cataract surgery. However, this conclusion should be interpreted with caution, as the effect on the TBUT or SIT scores has not been assessed [23]. In addition, DED after cataract surgery has a different pathogenesis and is not primarily based on the inflammatory component. Rather, DED after cataract surgery has been shown to be attributable to a series of factors, including prolonged use of antibiotic–steroid eye drops, decreased mucin production from the conjunctiva following the incision, decreased corneal sensation because of the surgical incision disrupting the cornea–lacrimal gland loop, decreased TBUT due to the surface irregularity at the incision site, and the exposure to light from the operating microscope [44,45].
Rolando et al. included patients with DED from Sjögren’s syndrome (SS) and compared the treatment with cortisol phosphate 0.3% eye drops to cortisol phosphate 0.3% in a hyaluronic acid vehicle. No changes in IOP were witnessed. Furthermore, no cases of cataract formation were observed. The formula with the hyaluronic acid vehicle proved to be more effective, with a significant improvement of corneal and conjunctival staining at 7 days compared to baseline in comparison with the cortisol phosphate 0.3% group. However, it should be considered that the cortisol phosphate 0.3% eye drops contained preservatives with low levels of direct toxicity on histology of the tissues [46]. Therefore, the preservatives might be a confounding factor and hypothetically contribute to the difference witnessed between the two groups [22]. Nevertheless, the authors argue that the combination of cortisol phosphate associated with hyaluronic acid creates a compound between the steroid and the polymer, which is a hydrophilic mucoadhesive drug. In this drug, cortisol and hyaluronic acid are linked through hydrogen bonds, which enable the drug to bind the epithelial corneal mucin, leading to a long permanence of the CS on the ocular surface [22]. Pinto-Fraga et al. assessed the efficacy of topical fluorometholone 0.1% compared to polyvinyl alcohol in 40 DED patients. After a follow-up of 3 weeks, greater improvements of corneal and conjunctival staining, hyperemia, and TBUT were witnessed in the fluorometholone compared to the polyvinyl alcohol group. No significant IOP changes occurred [15]. In addition, an increase in the best corrected visual acuity was witnessed in the fluorometholone group, which can be attributed to the positive correlation between corneal epithelial damage and visual acuity [47]. Interestingly, the authors found the 0.1% fluorometholone therapy to prevent an ocular surface worsening in DED patients exposed to desiccating stress. Therefore, Pinto-Fraga et al. suggest this treatment to be occasionally administered to patients who are anticipating adverse environmental conditions, including air-conditioned vehicles, etc. Especially, the treatment could be used to avoid exacerbation periods rather than in the long-term [15]. Aragona et al. evaluated the efficacy of clobetasone butyrate eyedrops in patients with DED associated with SS. Forty patients were included in the RCT. A significant improvement of corneal and conjunctival staining at last follow-up compared to baseline occurred in patients treated with topical clobetasone butyrate. No severe adverse events, including no cases of IOP elevation or cataract formation, were witnessed [36]. Yin et al. investigated the efficacy of loteprednol etabonate 0.5% ophthalmic suspension in two groups of 21 patients each with DED, with or without association to graft-versus-host-disease (GVHD), respectively. Similar to the inflammation cascade described above, DED in GVHD is mediated by T cells and cytokines [48]. The authors concluded a less favorable efficacy of loteprednol etabonate 0.5% in patients with ocular GVHD [38]. This lower efficacy in the GVHD group is attributed to different baseline characteristics between the two groups, possibly including cellular and molecular markers of inflammation. In addition, chronic ocular GVHD is characterized by lacrimal tissue destruction and fibrosis, which might not be reversible by topical CS treatment at an advanced stage [38]. Similarly, Boynton et al. analyzed the efficacy of loteprednol etabonate 0.5% compared with cyclosporine A in the management of DED associated with GVHD. In both groups, similar changes in OSDI, SIT, corneal staining, and TBUT occurred without relevant complications, such as IOP elevation [37]. However, as ocular hypertension is a common complication in patients with ocular GVHD, the long-term application of topical CS has to be considered with caution [49]. In a study by Pflugfelder et al., 66 patients were randomized to receive either topical loteprednol etabonate 0.5% or only the vehicle of loteprednol etabonate ophthalmic suspension. Loteprednol etabonate led to significant higher improvement in inferior tarsal and nasal bulbar conjunctival hyperemia at 2-week follow-up and in nasal bulbar hyperemia at 4-week follow-up than the vehicle [29]. The authors suggest that patients with greater degrees of ocular surface inflammation show a greater likelihood for a clinical response to loteprednol. Moreover, no toxic effects nor cases of IOP elevation due to the therapy with topical loteprednol were evidenced [29]. Interestingly, both loteprednol and its vehicle contained a preservative (benzalkonium chloride), which is known to cause corneal epithelial toxicity [50]. However, a clinical improvement in conjunctival hyperemia was witnessed at 2 weeks, while the improvement was less impressive at 4 weeks [29].
Three further RCTs investigating the efficacy of CS in DED are registered on https://clinicaltrials.gov (accessed on 4 September 2022). A RCT (NCT04711642) is planned to be conducted by the Fundación Oftalmológica Los Andes in Chile to evaluate the efficacy of a topical CS combined with antibiotic (tobramycin 0.3% and dexamethasone acetate 0.1%) on DED prior to and after cataract surgery. MMP9 is used as a parameter to diagnose ocular surface dysfunction. Recruitment of 100 patients has not started yet. Another registered RCT (NCT04498468) sponsored by the Johns Hopkins University, Maryland, USA, compares the efficacy of a CS intracanalicular insert releasing dexamethasone for up to 30 days to a sham comparator. Recruitment of an estimated patient enrolment of 85 patients has started.
Between studies, both the CS groups and the control groups were variable, and may impact the reliability of the results of the present meta-analysis. The efficacy of CS was compared to placebo in the studies by Aragona et al. [36] and Shokoohi-Rad et al. [23], to topical polyvinyl alcohol in the study by Pinto-Fraga [15], or to cyclosporine A in the study by Boynton et al. [37]. Yin et al. used artificial tears as a comparator [38]. Kallab et al. compared the efficacy of two different treatment protocols (standard and intense protocol) of hydrocortisone 0.335% [12]. Rolando et al. compared the efficacy of cortisol phosphate 0.3% eye drops to cortisol phosphate 0.3% in a hyaluronic acid vehicle as a control group [22]. Given the lack of quantitative data available for inclusion in the literature, no further subgroup investigations regarding different CS formulations were possible in the present meta-analysis. Furthermore, no subgroup investigations concerning different control groups was possible. Active treatments, such as cyclosporine A, and inert substances, such as placebo, were included as control groups, which might limit the reliability of the results of the present study. Moreover, no subgroup investigations in terms of formulations containing preservative versus preservative-free eye drops were possible. Additionally, the heterogeneous length of the follow-up might limit the reliability of our results. Moreover, it remains unclear whether the parameters investigated in this study, especially corneal staining, were evaluated identically, given the different investigators and implementation options. Given the lack of quantitative data, the different steroids (e.g., hydrocortisone, betamethasone, fluorometholone) and related concentration and administration protocols were not analyzed separately. Future long-term investigations are required to overcome these limitations and compare different CS with related concentration and administration protocols in a clinical setting. Therefore, the most indicated therapeutical algorithm should be identified and defined by future larger cohort level I studies. Given these limitations, results from the present study must be interpreted with caution. The current literature would benefit from high-quality clinical trials on a large scale. Future high-quality studies are needed to confirm the role of CS in patients with DED.
5. Conclusions
Topical CS administration led to an increase of SIT and a reduction of corneal staining at a mean of 10 weeks follow-up in patients with DED. Compared to a control group, topical CS administration evidenced greater values of TBUT. Altogether, a good safety profile was witnessed in DED patients receiving CS. However, different safety profiles of different CS formulations were not investigated due to a lack of quantitative data. The exact dosing frequency, duration of therapy, and favorable potency of the CS are still under investigation. Future randomized, controlled trials with larger sample sizes are warranted to provide higher-quality evidence to establish the role of CS in DED.
Author Contributions
Conceptualization, F.M. and J.P.; methodology, F.M. and N.M.; validation, M.F., P.W. and A.B.; formal analysis, F.M. and J.P.; writing—original draft preparation, J.P.; writing—review and editing, F.M., N.M. and P.W.; visualization, F.M.; supervision, F.M. and N.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Craig, J.P.; Nichols, K.K.; Akpek, E.K.; Caffery, B.; Dua, H.S.; Joo, C.-K.; Liu, Z.; Nelson, J.D.; Nichols, J.J.; Tsubota, K.; et al. TFOS DEWS II Definition and Classification Report. Ocul. Surf. 2017, 15, 276–283. [Google Scholar] [CrossRef]
- Miljanović, B.; Dana, R.; Sullivan, D.A.; Schaumberg, D.A. Impact of Dry Eye Syndrome on Vision-Related Quality of Life. Am. J. Ophthalmol. 2007, 143, 409–415.e2. [Google Scholar] [CrossRef]
- Smith, J.; Nichols, K.K.; Baldwin, E.K. Current patterns in the use of diagnostic tests in dry eye evaluation. Cornea 2008, 27, 656–662. [Google Scholar] [CrossRef]
- Yang, Y.-J.; Lee, W.-Y.; Kim, Y.-J.; Hong, Y.-P. A Meta-Analysis of the Efficacy of Hyaluronic Acid Eye Drops for the Treatment of Dry Eye Syndrome. Int. J. Environ. Res. Public Health 2021, 18, 2383. [Google Scholar] [CrossRef] [PubMed]
- Galor, A.; Levitt, R.C.; Felix, E.R.; Sarantopoulos, C.D. Understanding the true burden of dry eye disease. Expert Rev. Ophthalmol. 2015, 10, 403–405. [Google Scholar] [CrossRef]
- Schaumberg, D.A.; Buring, J.E.; Sullivan, D.A.; Dana, M.R. Hormone Replacement Therapy and Dry Eye Syndrome. JAMA 2001, 286, 2114–2119. [Google Scholar] [CrossRef]
- Rhee, M.K.; Mah, F.S. Inflammation in Dry Eye Disease: How Do We Break the Cycle? Ophthalmology. Ophthalmology 2017, 124, S14–S19. [Google Scholar] [CrossRef] [PubMed]
- Li, D.-Q.; Chen, Z.; Song, X.J.; Luo, L.; Pflugfelder, S.C. Stimulation of Matrix Metalloproteinases by Hyperosmolarity via a JNK Pathway in Human Corneal Epithelial Cells. Investig. Opthalmol. Vis. Sci. 2004, 45, 4302–4311. [Google Scholar] [CrossRef]
- Luo, L.; Li, D.-Q.; Doshi, A.; Farley, W.; Corrales, R.M.; Pflugfelder, S.C. Experimental Dry Eye Stimulates Production of Inflammatory Cytokines and MMP-9 and Activates MAPK Signaling Pathways on the Ocular Surface. Investig. Opthalmol. Vis. Sci. 2004, 45, 4293–4301. [Google Scholar] [CrossRef]
- Stern, M.E.; Gao, J.; Siemasko, K.F.; Beuerman, R.W.; Pflugfelder, S.C. The role of the lacrimal functional unit in the pathophysiology of dry eye. Exp. Eye Res. 2004, 78, 409–416. [Google Scholar] [CrossRef]
- Yavuz, B.; Pehlivan, S.B.; Ünlü, N. An Overview on Dry Eye Treatment: Approaches for Cyclosporin a Delivery. Sci. World J. 2012, 2012, 194848. [Google Scholar] [CrossRef] [PubMed]
- Kallab, M.; Szegedi, S.; Hommer, N.; Stegmann, H.; Kaya, S.; Werkmeister, R.M.; Schmidl, D.; Schmetterer, L.; Garhöfer, G. Topical Low Dose Preservative-Free Hydrocortisone Reduces Signs and Symptoms in Patients with Chronic Dry Eye: A Randomized Clinical Trial. Adv. Ther. 2019, 37, 329–341. [Google Scholar] [CrossRef]
- Rhen, T.; Cidlowski, J.A. Antiinflammatory Action of Glucocorticoids—New Mechanisms for Old Drugs. N. Engl. J. Med. 2005, 353, 1711–1723. [Google Scholar] [CrossRef] [PubMed]
- Comstock, T.L.; Decory, H.H. Advances in corticosteroid therapy for ocular inflammation: Loteprednol etabonate. Int. J. Inflam. 2012, 2012, 789623. [Google Scholar] [CrossRef] [PubMed]
- Pinto-Fraga, J.; López-Miguel, A.; González-García, M.J.; Fernández, I.; de la Rosa, A.L.; Enríquez-De-Salamanca, A.; Stern, M.E.; Calonge, M. Topical Fluorometholone Protects the Ocular Surface of Dry Eye Patients from Desiccating Stress: A Randomized Controlled Clinical Trial. Ophthalmology 2016, 123, 141–153. [Google Scholar] [CrossRef] [PubMed]
- Bielory, B.P.; O’Brien, T.P.; Bielory, L. Management of seasonal allergic conjunctivitis: Guide to therapy. Acta Ophthalmol. 2012, 90, 399–407. [Google Scholar] [CrossRef]
- Tripathi, R.C.; Parapuram, S.K.; Tripathi, B.J.; Zhong, Y.; Chalam, K. Corticosteroids and Glaucoma Risk. Drugs Aging 1999, 15, 439–450. [Google Scholar] [CrossRef]
- Gaballa, S.A.; Kompella, U.B.; Elgarhy, O.; Alqahtani, A.M.; Pierscionek, B.; Alany, R.G.; Abdelkader, H. Corticosteroids in ophthalmology: Drug delivery innovations, pharmacology, clinical applications, and future perspectives. Drug Deliv. Transl. Res. 2021, 11, 866–893. [Google Scholar] [CrossRef]
- Shokoohi-Rad, S.; Daneshvar, R.; Jafarian-Shahri, M.; Rajaee, P. Comparison between Betamethasone, Fluorometholone and Loteprednol Etabonate on intraocular pressure in patients after keratorefractive surgery. J. Curr. Ophthalmol. 2018, 30, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Pavesio, C.E.; DeCory, H.H. Treatment of ocular inflammatory conditions with loteprednol etabonate. Br. J. Ophthalmol. 2008, 92, 455–459. [Google Scholar] [CrossRef]
- Srinivasan, M.; Mascarenhas, J.; Rajaraman, R.; Ravindran, M.; Lalitha, P.; Glidden, D.; Ray, K.J.; Hong, K.C.; Oldenburg, C.E.; Lee, S.M.; et al. The steroids for corneal ulcers trial: Study design and baseline characteristics. Arch. Ophthalmol. 2012, 130, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Rolando, M.; Vagge, A. Safety and Efficacy of Cortisol Phosphate in Hyaluronic Acid Vehicle in the Treatment of Dry Eye in Sjogren Syndrome. J. Ocul. Pharmacol. Ther. 2017, 33, 383–390. [Google Scholar] [CrossRef]
- Javaheri, S.Z.H.; Shokoohi-Rad, S.; Malekabad, F.Z.; Khakshoor, H.; Daluee, M.K. Effects of preoperative doses of betamethasone acetate 0.1% on dry eye control after cataract surgery. Indian J. Ophthalmol. 2020, 68, 450–454. [Google Scholar] [CrossRef] [PubMed]
- Avunduk, A.M.; Avunduk, M.C.; Varnell, E.D.; E Kaufman, H. The comparison of efficacies of topical corticosteroids and nonsteroidal anti-inflammatory drops on dry eye patients: A clinical and immunocytochemical study. Am. J. Ophthalmol. 2003, 136, 593–602. [Google Scholar] [CrossRef]
- Mencucci, R.; Boccalini, C.; Caputo, R.; Favuzza, E. Effect of a hyaluronic acid and carboxymethylcellulose ophthalmic solution on ocular comfort and tear-film instability after cataract surgery. J. Cataract Refract. Surg. 2015, 41, 1699–1704. [Google Scholar] [CrossRef]
- Lin, T.; Gong, L. Topical fluorometholone treatment for ocular dryness in patients with Sjögren syndrome: A randomized clinical trial in China. Medicine (Baltimore). Medicine 2015, 94, e551. [Google Scholar] [CrossRef]
- Aragona, P.; Aguennouz, M.; Rania, L.; Postorino, E.; Sommario, M.S.; Roszkowska, A.M.; De Pasquale, M.G.; Pisani, A.; Puzzolo, D. Matrix Metalloproteinase 9 and Transglutaminase 2 Expression at the Ocular Surface in Patients with Different Forms of Dry Eye Disease. Ophthalmology 2015, 122, 62–71. [Google Scholar] [CrossRef]
- Sheppard, J.D.; Donnenfeld, E.D.; Holland, E.J.; Slonim, C.B.; Solomon, R.; Solomon, K.D.; McDonald, M.B.; Perry, H.D.; Lane, S.S.; Pflugfelder, S.C.; et al. Effect of Loteprednol Etabonate 0.5% on Initiation of Dry Eye Treatment with Topical Cyclosporine 0.05%. Eye Contact Lens 2014, 40, 289–296. [Google Scholar] [CrossRef]
- Pflugfelder, S.C.; Maskin, S.L.; Anderson, B.; Chodosh, J.; Holland, E.J.; de Paiva, C.; Bartels, S.P.; Micuda, T.; Proskin, H.M.; Vogel, R. A randomized, double-masked, placebo-controlled, multicenter comparison of loteprednol etabonate ophthalmic suspension, 0.5%, and placebo for treatment of keratoconjunctivitis sicca in patients with delayed tear clearance. Am. J. Ophthalmol. 2004, 138, 444–457. [Google Scholar] [CrossRef]
- Howick, J.C.I.; Glasziou, P.; Greenhalgh, T.; Carl, H.; Liberati, A.; Moschetti, I.; Phillips, B.; Thornton, H.; Goddard, O.; Hodgkinson, M. The 2011 Oxford CEBM Levels of Evidence; Oxford Centre for Evidence-Based Medicine: Oxford, UK, 2011; Available online: https://wwwcebmnet/indexaspx?o=5653 (accessed on 5 September 2022).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Walt, J.R.M.; Stern, K. Evaluating the functional impact of dry eye: The Ocular Surface Disease Index. Drug Inf. J. 1997, 31, 1436. [Google Scholar]
- Cho, P.; Leung, L.; Lam, A.; Choi, A. Tear break-up time: Clinical procedures and their effects. Ophthalmic. Physiol. Opt. 1998, 18, 319–324. [Google Scholar] [CrossRef]
- Cho, P.; Yap, M. Schirmer test. I. A review. Optom. Vis. Sci. 1993, 70, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Bron, A.J.; Evans, V.E.; Smith, J.A. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea 2003, 22, 640–650. [Google Scholar] [CrossRef] [PubMed]
- Aragona, P.; Spinella, R.; Rania, L.; Postorino, E.; Sommario, M.S.; Roszkowska, A.M.; Puzzolo, D. Safety and Efficacy of 0.1% Clobetasone Butyrate Eyedrops in the Treatment of Dry Eye in Sjögren Syndrome. Eur. J. Ophthalmol. 2013, 23, 368–376. [Google Scholar] [CrossRef] [PubMed]
- Boynton, G.E.; Raoof, D.; Niziol, L.M.; Hussain, M.; Mian, S. Prospective Randomized Trial Comparing Efficacy of Topical Loteprednol Etabonate 0.5% Versus Cyclosporine-A 0.05% for Treatment of Dry Eye Syndrome Following Hematopoietic Stem Cell Transplantation. Cornea 2015, 34, 725–732. [Google Scholar] [CrossRef]
- Yin, J.; Kheirkhah, A.; Dohlman, T.; Saboo, U.; Dana, R. Reduced Efficacy of Low-dose Topical Steroids in Dry Eye Disease Associated with Graft-versus-Host Disease. Am. J. Ophthalmol. 2018, 190, 17–23. [Google Scholar] [CrossRef]
- Tuan, H.-I.; Chi, S.-C.; Kang, Y.-N. An Updated Systematic Review with Meta-Analysis of Randomized Trials on Topical Cyclosporin A For Dry-Eye Disease. Drug Des. Dev. Ther. 2020, 14, 265–274. [Google Scholar] [CrossRef]
- Barnes, P.J. How corticosteroids control inflammation: Quintiles Prize Lecture 2005. Br. J. Pharmacol. 2006, 148, 245–254. [Google Scholar] [CrossRef]
- Solomon, A.; Rosenblatt, M.; Li, D.Q.; Liu, Z.; Monroy, D.; Ji, Z.; Lokeshwar, B.L.; Pflugfelder, S.C. Doxycycline inhibition of interleukin-1 in the corneal epithelium. Inves. Ophthalmol. Vis. Sci. 2000, 41, 2544–2557. [Google Scholar] [CrossRef]
- Pleyer, U.; Ursell, P.G.; Rama, P. Intraocular Pressure Effects of Common Topical Steroids for Post-Cataract Inflammation: Are They All the Same? Ophthalmol. Ther. 2013, 2, 55–72. [Google Scholar] [CrossRef] [PubMed]
- Sheppard, J.D.; Comstock, T.L.; Cavet, M.E. Impact of the Topical Ophthalmic Corticosteroid Loteprednol Etabonate on Intraocular Pressure. Adv. Ther. 2016, 33, 532–552. [Google Scholar] [CrossRef] [PubMed]
- Li, X.-M.; Hu, L.; Hu, J.; Wang, W. Investigation of Dry Eye Disease and Analysis of the Pathogenic Factors in Patients after Cataract Surgery. Cornea 2007, 26 (Suppl. 1), S16–S20. [Google Scholar] [CrossRef]
- Sutu, C.; Fukuoka, H.; Afshari, N.A. Mechanisms and management of dry eye in cataract surgery patients. Curr. Opin. Ophthalmol. 2016, 27, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Soni, M.; Burdock, G.; Taylor, S.; Greenberg, N. Safety assessment of propyl paraben: A review of the published literature. Food Chem. Toxicol. 2001, 39, 513–532. [Google Scholar] [CrossRef]
- Kaido, M.; Kawashima, M.; Shigeno, Y.; Yamada, Y.; Tsubota, K. Randomized Controlled Study to Investigate the Effect of Topical Diquafosol Tetrasodium on Corneal Sensitivity in Short Tear Break-Up Time Dry Eye. Adv. Ther. 2018, 35, 697–706. [Google Scholar] [CrossRef] [PubMed]
- Shikari, H.; Antin, J.H.; Dana, R. Ocular Graft-versus-Host Disease: A Review. Surv. Ophthalmol. 2013, 58, 233–251. [Google Scholar] [CrossRef]
- Saboo, U.S.; Amparo, F.; Shikari, H.; Dana, R. Prevalence of ocular hypertension and glaucoma in patients with chronic ocular graft-versus-host disease. Graefes Arch. Clin. Exp. Ophthalmol. 2016, 254, 923–928. [Google Scholar] [CrossRef]
- Ichijima, H.; Petroll, W.M.; Jester, J.V.; Cavanagh, H.D. Confocal microscopic studies of living rabbit cornea treated with benzalkonium chloride. Cornea 1992, 11, 221–225. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).