Classification of Dystonia
Abstract
:1. Introduction
2. Definition of Dystonia
- Dystonia is a movement disorder characterized by sustained or intermittent muscle contractions causing abnormal and often repetitive, movements, postures, or both.
- Dystonic movements are typically patterned, twisting, and may be tremulous.
- Dystonia is often initiated or worsened by voluntary action and associated with overflow muscle activation.
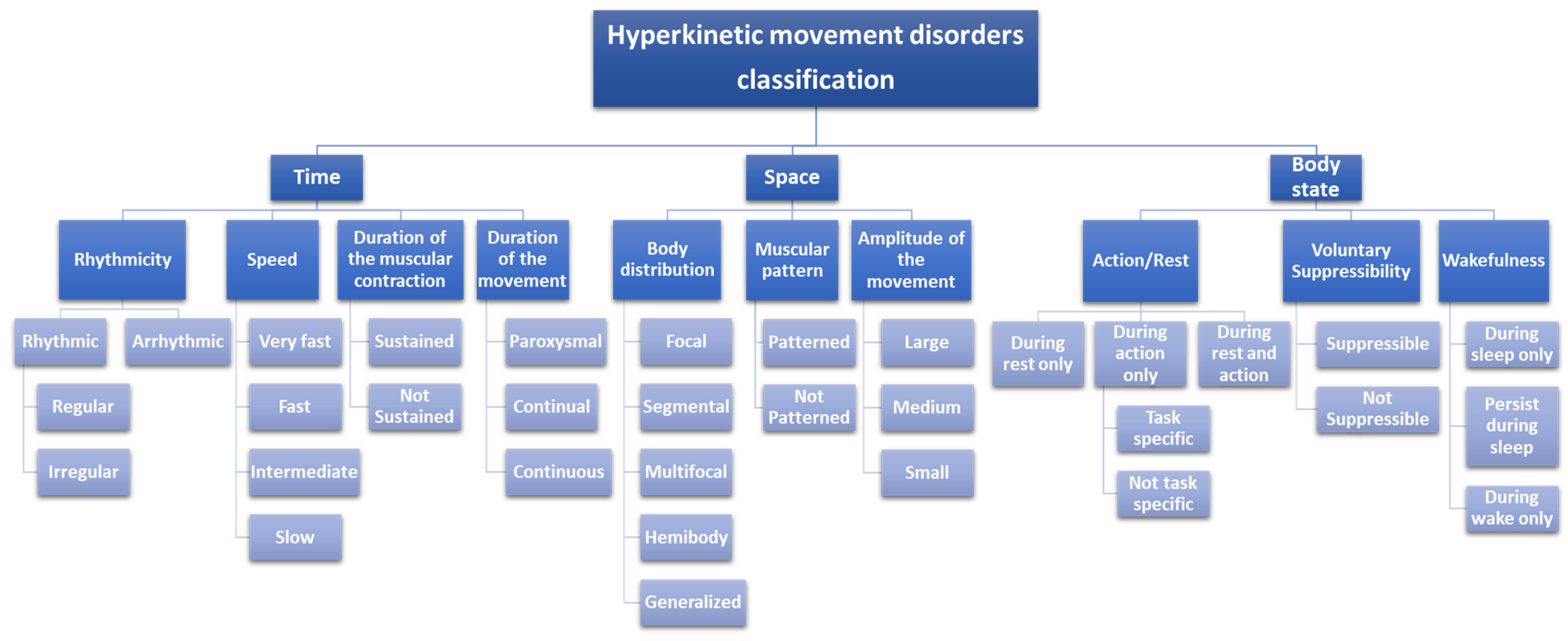
3. Phenomenological Spectrum
3.1. Time
3.1.1. Rhythmicity
3.1.2. Speed
3.1.3. Duration of the Muscular Contraction
3.1.4. Duration of the Movement
3.2. Space Distribution
3.2.1. Body Distribution
- Focal: 1 body part is affected
- Segmental: ≥2 contiguous body parts are affected
- Multifocal: ≥2 non-contiguous body parts are affected
- Hemidistonia: Ipsilateral arm and leg are involved
- Generalized: ≥3 body parts are affected, including the trunk and ≥2 other sites; with or without leg involvement
3.2.2. Muscular Pattern
3.2.3. Amplitude
3.3. Body State’s Impact
3.3.1. Action Rule
3.3.2. Suppressibility
3.3.3. Wakefulness
- Time: rhythmic; with intermediate speed; associated with non-sustained (intermittent) muscular contraction; with a continual duration (repeats over and over again without a sudden recurrence).
- Space: focal, patterned with a small amplitude.
- Body state: initiated or worsened by voluntary action, not suppressible, and present during wake only.
- Time: arrhythmic; with slow speed; associated with sustained muscular contraction; with a continuous duration (continue without stopping).
- Space: focal, patterned with a small amplitude.
- Body state: present during both rest and action, not suppressible and present during waking time only.
4. Classifications of Dystonia
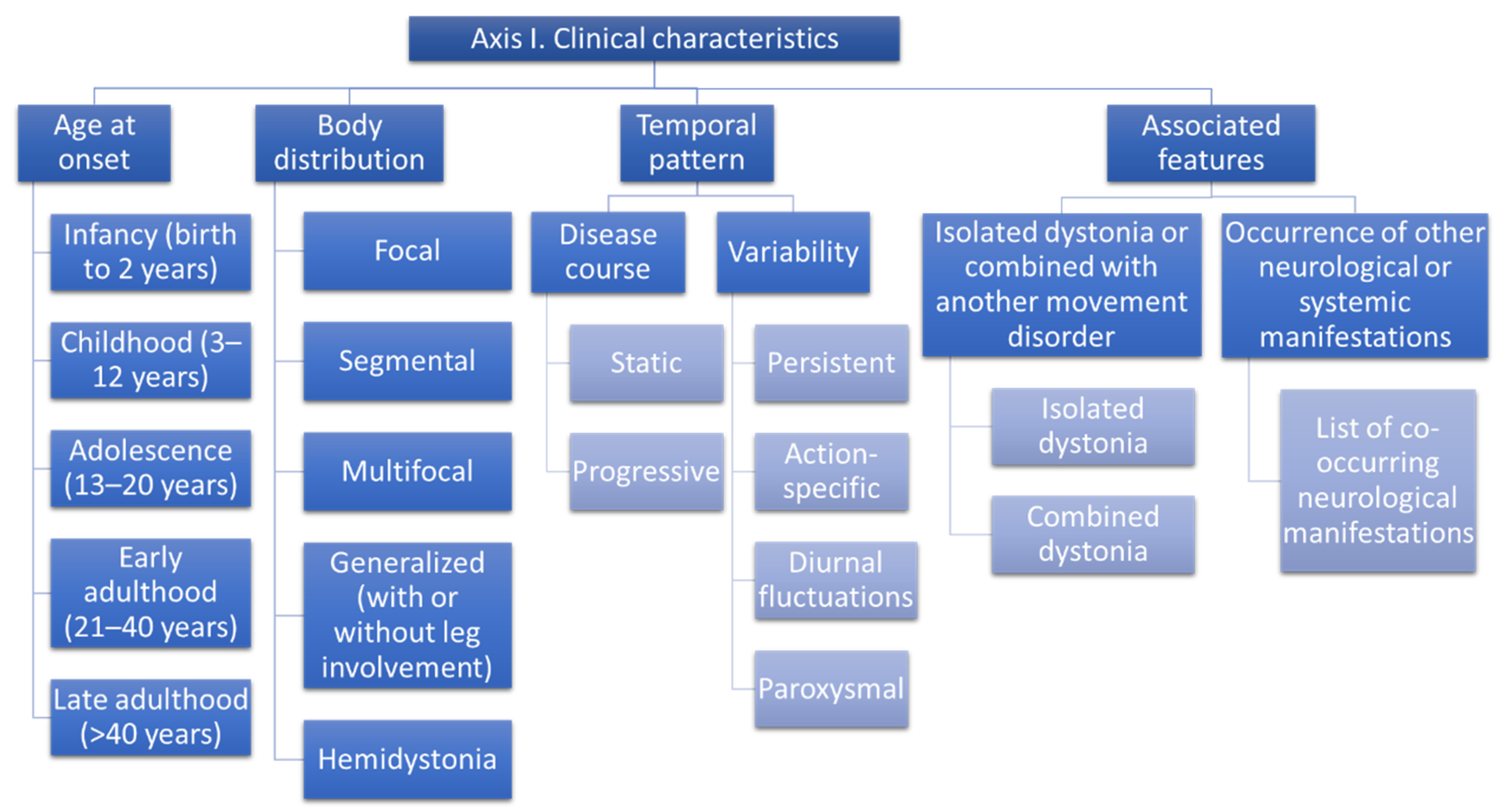
4.1. Axis I: Clinical Characteristics
4.1.1. Age at Onset
- Infancy (birth to 2 years)
- Childhood (3–12 years)
- Adolescence (13–20 years)
- Early adulthood (21–40 years)
- Late adulthood (>40 years)
4.1.2. Body Distribution
- Focal
- Segmental
- Multifocal
- Generalized
- Hemidystonia
4.1.3. Temporal Pattern
- Static
- Progressive
- Persistent
- Action-specific
- Diurnal fluctuations
- Paroxysmal
4.1.4. Associated Features
- Isolated dystonia: dystonia, associated or not with tremors that are the only additional movement disorder
- Combined dystonia: dystonia is combined with other movement disorders
- Complex dystonia: dystonia is accompanied by neurologic or systemic manifestations beyond movement disorders
4.2. Axis II: Etiology
4.2.1. Inherited Dystonia
4.2.2. Autosomal Dominant
4.2.3. Autosomal Recessive
4.2.4. X-Linked Recessive
4.2.5. X-Linked Dominant
4.2.6. Mitochondrial
4.2.7. Acquired Forms of Dystonia
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Albanese, A.; Bhatia, K.; Bressman, S.B.; DeLong, M.R.; Fahn, S.; Fung, V.S.; Hallett, M.; Jankovic, J.; Jinnah, H.A.; Klein, C. Phenomenology and classification of dystonia: A consensus update. Mov. Disord. 2013, 28, 863–873. [Google Scholar] [CrossRef] [Green Version]
- Elia, A.; Lalli, S.; Albanese, A. Differential diagnosis of dystonia. Eur. J. Neurol. 2010, 17, 1–8. [Google Scholar] [CrossRef]
- Fahn, S.; Eldridge, R. Definition of dystonia and classification of the dystonic states. Adv. Neurol. 1976, 14, 1–5. [Google Scholar]
- Fahn, S.; Marsden, C.D.; Calne, D.B. Classification and investigation of dystonia. Mov. Disord. 1987, 2, 332–358. [Google Scholar]
- Fahn, S.; Bressman, S.B.; Marsden, C.D. Classification of dystonia. Adv. Neurol. 1998, 78, 1–10. [Google Scholar] [CrossRef]
- Albanese, A.; Asmus, F.; Bhatia, K.P.; Elia, A.E.; Elibol, B.; Filippini, G.; Gasser, T.; Krauss, J.K.; Nardocci, N.; Newton, A.; et al. EFNS guidelines on diagnosis and treatment of primary dystonias. Eur. J. Neurol. 2011, 18, 5–18. [Google Scholar] [CrossRef]
- Fahn, S.; Jankovic, J.; Hallett, M. Principles and Practice of Movement Disorders; Elsevier Health Sciences: Oxford, UK, 2011. [Google Scholar]
- Albanese, A.; Jankovic, J. Hyperkinetic Movement Disorders; John Wiley & Sons: Hoboken, NJ, USA, 2012; p. 390. [Google Scholar]
- Bhatia, K.P.; Bain, P.; Bajaj, N.; Elble, R.J.; Hallett, M.; Louis, E.D.; Raethjen, J.; Stamelou, M.; Testa, C.M.; Deuschl, G.; et al. Consensus Statement on the classification of tremors. from the task force on tremor of the International Parkinson and Movement Disorder Society. Mov. Disord. Off. J. Mov. Disord. Soc. 2018, 33, 75–87. [Google Scholar] [CrossRef]
- Schneider, S.A.; Edwards, M.J.; Mir, P.; Cordivari, C.; Hooker, J.; Dickson, J.; Quinn, N.; Bhatia, K.P. Patients with adult-onset dystonic tremor resembling Parkinsonian tremor have scans without evidence of dopaminergic deficit (SWEDDs). Mov. Disord. 2007, 22, 2210–2215. [Google Scholar] [CrossRef]
- Albanese, A. The clinical expression of primary dystonia. J. Neurol. 2003, 250, 1145–1151. [Google Scholar] [CrossRef]
- Vercueil, L. Myoclonus and movement disorders. Neurophysiol. Clin. 2006, 36, 327–331. [Google Scholar] [CrossRef]
- Gatto, E.M.; Pardal, M.M.a.F.; Micheli, F.E. Unusual phenotypic expression of the DYT1 mutation. Parkinsonism Relat. Disord. 2003, 9, 277–279. [Google Scholar] [CrossRef]
- Chinnery, P.F.; Reading, P.J.; McCarthy, E.L.; Curtis, A.; Burn, D.J. Late-onset axial jerky dystonia due to the DYT1 deletion. Mov. Disord. 2002, 17, 196–198. [Google Scholar] [CrossRef]
- Leung, J.; Klein, C.; Friedman, J.; Vieregge, P.; Jacobs, H.; Doheny, D.; Kamm, C.; DeLeon, D.; Pramstaller, P.P.; Penney, J.B. Novel mutation in the TOR1A (DYT1) gene in atypical, early onset dystonia and polymorphisms in dystonia and early onset parkinsonism. Neurogenetics 2001, 3, 133–143. [Google Scholar] [CrossRef]
- Muller, B.; Hedrich, K.; Kock, N.; Dragasevic, N.; Svetel, M.; Garrels, J.; Landt, O.; Nitschke, M.; Pramstaller, P.P.; Reik, W.; et al. Evidence that paternal expression of the epsilon-sarcoglycan gene accounts for reduced penetrance in myoclonus-dystonia. Am. J. Hum. Genet. 2002, 71, 1303–1311. [Google Scholar] [CrossRef] [Green Version]
- Klein, C. Genetics in dystonia. Parkinsonism Relat. Disord. 2014, 20 (Suppl. 1), S137–S142. [Google Scholar] [CrossRef]
- Albanese, A.; Lalli, S. Is this dystonia? Mov. Disord. 2009, 24, 1725–1731. [Google Scholar] [CrossRef]
- Cardoso, F.; Seppi, K.; Mair, K.J.; Wenning, G.K.; Poewe, W. Seminar on choreas. Lancet Neurol. 2006, 5, 589–602. [Google Scholar] [CrossRef]
- Fahn, S.; Hening, W.; Bressman, S.; Burke, R.; Ilson, J.; Walters, A. Long-term usefulness of baclofen in the treatment of essential blepharospasm. Adv. Ophthalmic Plast. Reconstr. Surg. 1985, 4, 219–226. [Google Scholar]
- Cohen, L.G.; Hallett, M. Hand cramps: Clinical features and electromyographic patterns in a focal dystonia. Neurology 1988, 38, 1005. [Google Scholar] [CrossRef]
- Sitburana, O.; Wu, L.J.C.; Sheffield, J.K.; Davidson, A.; Jankovic, J. Motor overflow and mirror dystonia. Parkinsonism Relat. Disord. 2009, 15, 758–761. [Google Scholar] [CrossRef]
- Gömez-Wong, E.; Martí, M.J.; Cossu, G.; Fabregat, N.; Tolosa, E.S.; Valls-Solé, J. The ‘geste antagonistique’ induces transient modulation of the blink reflex in human patients with blepharospasm. Neurosci. Lett. 1998, 251, 125–128. [Google Scholar] [CrossRef]
- Greene, P.E.; Bressman, S. Exteroceptive and interoceptive stimuli in dystonia. Mov. Disord. 1998, 13, 549–551. [Google Scholar] [CrossRef]
- Hallett, M. Is dystonia a sensory disorder? Ann. Neurol. 1995, 38, 139–140. [Google Scholar] [CrossRef] [PubMed]
- Jahanshahi, M. Factors that ameliorate or aggravate spasmodic torticollis. J. Neurol. Neurosurg. Psychiatry 2000, 68, 227–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Müller, J.; Wissel, J.; Masuhr, F.; Ebersbach, G.; Wenning, G.K.; Poewe, W. Clinical characteristics of the geste antagoniste in cervical dystonia. J. Neurol. 2001, 248, 478–482. [Google Scholar] [CrossRef] [PubMed]
- Sanger, T.D. Pathophysiology of pediatric movement disorders. J. Child Neurol. 2003, 18 (Suppl. 1), S9–S24. [Google Scholar] [CrossRef]
- Barclay, C.L.; Lang, A.E. Dystonia in progressive supranuclear palsy. J. Neurol. Neurosurg. Psychiatry 1997, 62, 352–356. [Google Scholar] [CrossRef]
- Vanek, Z.; Jankovic, J. Dystonia in corticobasal degeneration. Mov. Disord. Off. J. Mov. Disord. Soc. 2001, 16, 252–257. [Google Scholar] [CrossRef]
- Mastrolilli, F.; Benvenga, A.; Di Biase, L.; Giambattistelli, F.; Trotta, L.; Salomone, G.; Quintiliani, L.; Landi, D.; Melgari, J.; Vernieri, F. An unusual cause of dementia: Essential diagnostic elements of corticobasal degeneration—A case report and review of the literature. Int. J. Alzheimer’s Dis. 2011, 2011, 536141. [Google Scholar] [CrossRef] [Green Version]
- Herzog, R.; Weissbach, A.; Bäumer, T.; Münchau, A. Complex dystonias: An update on diagnosis and care. J. Neural Transm. 2021, 128, 431–445. [Google Scholar] [CrossRef]
- Rosencrantz, R.; Schilsky, M. Wilson disease: Pathogenesis and clinical considerations in diagnosis and treatment. Semin. Liver Dis. 2011, 31, 245–259. [Google Scholar] [CrossRef] [PubMed]
- Zech, M.; Jech, R.; Boesch, S.; Škorvánek, M.; Weber, S.; Wagner, M.; Zhao, C.; Jochim, A.; Necpál, J.; Dincer, Y.; et al. Monogenic variants in dystonia: An exome-wide sequencing study. Lancet Neurol. 2020, 19, 908–918. [Google Scholar] [CrossRef]
- Wirth, T.; Tranchant, C.; Drouot, N.; Keren, B.; Mignot, C.; Cif, L.; Lefaucheur, R.; Lion-François, L.; Méneret, A.; Gras, D.; et al. Increased diagnostic yield in complex dystonia through exome sequencing. Parkinsonism Relat. Disord. 2020, 74, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Keller Sarmiento, I.J.; Mencacci, N.E. Genetic Dystonias: Update on Classification and New Genetic Discoveries. Curr. Neurol. Neurosci. Rep. 2021, 21, 8. [Google Scholar] [CrossRef] [PubMed]
- Vidailhet, M.; Méneret, A.; Roze, E. Dystonia: Genetics, phenomenology, and pathophysiology. Lancet Neurol. 2020, 19, 881–882. [Google Scholar] [CrossRef]
- Mencacci, N.E.; Reynolds, R.; Ruiz, S.G.; Vandrovcova, J.; Forabosco, P.; Sánchez-Ferrer, A.; Volpato, V.; Weale, M.E.; Bhatia, K.P.; Webber, C.; et al. Dystonia genes functionally converge in specific neurons and share neurobiology with psychiatric disorders. Brain 2020, 143, 2771–2787. [Google Scholar] [CrossRef]
- Marras, C.; Lang, A.; van de Warrenburg, B.P.; Sue, C.M.; Tabrizi, S.J.; Bertram, L.; Mercimek-Mahmutoglu, S.; Ebrahimi-Fakhari, D.; Warner, T.T.; Durr, A.; et al. Nomenclature of genetic movement disorders: Recommendations of the international Parkinson and movement disorder society task force. Mov. Disord. Off. J. Mov. Disord. Soc. 2016, 31, 436–457. [Google Scholar] [CrossRef]
- Ozelius, L.J.; Hewett, J.W.; Page, C.E.; Bressman, S.B.; Kramer, P.L.; Shalish, C.; de Leon, D.; Brin, M.F.; Raymond, D.; Corey, D.P.; et al. The early-onset torsion dystonia gene (DYT1) encodes an ATP-binding protein. Nat. Genet. 1997, 17, 40–48. [Google Scholar] [CrossRef]
- Kabakci, K.; Hedrich, K.; Leung, J.C.; Mitterer, M.; Vieregge, P.; Lencer, R.; Hagenah, J.; Garrels, J.; Witt, K.; Klostermann, F.; et al. Mutations in DYT1: Extension of the phenotypic and mutational spectrum. Neurology 2004, 62, 395–400. [Google Scholar] [CrossRef]
- Bressman, S.B.; Sabatti, C.; Raymond, D.; de Leon, D.; Klein, C.; Kramer, P.L.; Brin, M.F.; Fahn, S.; Breakefield, X.; Ozelius, L.J.; et al. The DYT1 phenotype and guidelines for diagnostic testing. Neurology 2000, 54, 1746–1752. [Google Scholar] [CrossRef]
- Artusi, C.A.; Dwivedi, A.; Romagnolo, A.; Bortolani, S.; Marsili, L.; Imbalzano, G.; Sturchio, A.; Keeling, E.G.; Zibetti, M.; Contarino, M.F.; et al. Differential response to pallidal deep brain stimulation among monogenic dystonias: Systematic review and meta-analysis. J. Neurol. Neurosurg. Psychiatry 2020, 91, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Leube, B.; Rudnicki, D.; Ratzlaff, T.; Kessler, K.R.; Benecke, R.; Auburger, G. Idiopathic torsion dystonia: Assignment of a gene to chromosome 18p in a German family with adult onset, autosomal dominant inheritance and purely focal distribution. Hum. Mol. Genet. 1996, 5, 1673–1677. [Google Scholar] [CrossRef] [Green Version]
- Bressman, S.B.; Hunt, A.L.; Heiman, G.A.; Brin, M.F.; Burke, R.E.; Fahn, S.; Trugman, J.M.; de Leon, D.; Kramer, P.L.; Wilhelmsen, K.C.; et al. Exclusion of the DYT1 locus in a non-Jewish family with early-onset dystonia. Mov. Disord. Off. J. Mov. Disord. Soc. 1994, 9, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Bentivoglio, A.R.; Del Grosso, N.; Albanese, A.; Cassetta, E.; Tonali, P.; Frontali, M. Non-DYT1 dystonia in a large Italian family. J. Neurol. Neurosurg. Psychiatry 1997, 62, 357–360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Camargos, S.; Scholz, S.; Simon-Sanchez, J.; Paisan-Ruiz, C.; Lewis, P.; Hernandez, D.; Ding, J.; Gibbs, J.R.; Cookson, M.R.; Bras, J.; et al. DYT16, a novel young-onset dystonia-parkinsonism disorder: Identification of a segregating mutation in the stress-response protein PRKRA. Lancet Neurol. 2008, 7, 207–215. [Google Scholar] [CrossRef]
- Seibler, P.; Djarmati, A.; Langpap, B.; Hagenah, J.; Schmidt, A.; Bruggemann, N.; Siebner, H.; Jabusch, H.C.; Altenmuller, E.; Munchau, A.; et al. A heterozygous frameshift mutation in PRKRA (DYT16) associated with generalised dystonia in a German patient. Lancet Neurol. 2008, 7, 380–381. [Google Scholar] [CrossRef]
- Klein, C.; Lohmann, K.; Marras, C.; Münchau, A. Hereditary Dystonia Overview. In GeneReviews®; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Stephens, K., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993. [Google Scholar]
- Klein, C.; Fahn, S. Translation of Oppenheim’s 1911 paper on dystonia. Mov. Disord. Off. J. Mov. Disord. Soc. 2013, 28, 851–862. [Google Scholar] [CrossRef] [PubMed]
- Tadic, V.; Kasten, M.; Bruggemann, N.; Stiller, S.; Hagenah, J.; Klein, C. Dopa-responsive dystonia revisited: Diagnostic delay, residual signs, and nonmotor signs. Arch. Neurol. 2012, 69, 1558–1562. [Google Scholar] [CrossRef]
- Brashear, A.; Dobyns, W.B.; de Carvalho Aguiar, P.; Borg, M.; Frijns, C.J.; Gollamudi, S.; Green, A.; Guimaraes, J.; Haake, B.C.; Klein, C.; et al. The phenotypic spectrum of rapid-onset dystonia-parkinsonism (RDP) and mutations in the ATP1A3 gene. Brain 2007, 130, 828–835. [Google Scholar] [CrossRef] [Green Version]
- Rughani, A.I.; Lozano, A.M. Surgical treatment of myoclonus dystonia syndrome. Mov. Disord. Off. J. Mov. Disord. Soc. 2013, 28, 282–287. [Google Scholar] [CrossRef]
- Mencacci, N.E.; Rubio-Agusti, I.; Zdebik, A.; Asmus, F.; Ludtmann, M.H.; Ryten, M.; Plagnol, V.; Hauser, A.K.; Bandres-Ciga, S.; Bettencourt, C.; et al. A missense mutation in KCTD17 causes autosomal dominant myoclonus-dystonia. Am. J. Hum. Genet. 2015, 96, 938–947. [Google Scholar] [CrossRef] [Green Version]
- Todisco, M.; Gana, S.; Cosentino, G.; Errichiello, E.; Arceri, S.; Avenali, M.; Valente, E.M.; Alfonsi, E. KCTD17-related myoclonus-dystonia syndrome: Clinical and electrophysiological findings of a patient with atypical late onset. Parkinsonism Relat. Disord. 2020, 78, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Chinnery, P.F. Neuroferritinopathy. In GeneReviews®; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Stephens, K., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993. [Google Scholar]
- Van de Warrenburg, B.P.; van Gaalen, J.; Boesch, S.; Burgunder, J.M.; Dürr, A.; Giunti, P.; Klockgether, T.; Mariotti, C.; Pandolfo, M.; Riess, O. EFNS/ENS Consensus on the diagnosis and management of chronic ataxias in adulthood. Eur. J. Neurol. 2014, 21, 552–562. [Google Scholar] [CrossRef] [PubMed]
- Iizuka, R.; Hirayama, K.; Maehara, K.A. Dentato-rubro-pallido-luysian atrophy: A clinico-pathological study. J. Neurol. Neurosurg. Psychiatry 1984, 47, 1288–1298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hatano, T.; Okuma, Y.; Iijima, M.; Fujishima, K.; Goto, K.; Mizuno, Y. Cervical dystonia in dentatorubral-pallidoluysian atrophy. Acta Neurol. Scand. 2003, 108, 287–289. [Google Scholar] [CrossRef]
- Richards, R.I. Dynamic mutations: A decade of unstable expanded repeats in human genetic disease. Hum. Mol. Genet. 2001, 10, 2187–2194. [Google Scholar] [CrossRef] [Green Version]
- Becker, N.; Munhoz, R.P.; Raskin, S.; Werneck, L.C.; Teive, H.A. Non-choreic movement disorders as initial manifestations of Huntington’s disease. Arq. Neuro-Psiquiatr. 2007, 65, 402–405. [Google Scholar] [CrossRef] [Green Version]
- Van de Zande, N.A.; Massey, T.H.; McLauchlan, D.; Pryce Roberts, A.; Zutt, R.; Wardle, M.; Payne, G.C.; Clenaghan, C.; Tijssen, M.A.J.; Rosser, A.E.; et al. Clinical characterization of dystonia in adult patients with Huntington’s disease. Eur. J. Neurol. 2017, 24, 1140–1147. [Google Scholar] [CrossRef] [Green Version]
- De Castilhos, R.M.; Furtado, G.V.; Gheno, T.C.; Schaeffer, P.; Russo, A.; Barsottini, O.; Pedroso, J.L.; Salarini, D.Z.; Vargas, F.R.; de Lima, M.A.; et al. Spinocerebellar ataxias in Brazil--frequencies and modulating effects of related genes. Cerebellum 2014, 13, 17–28. [Google Scholar] [CrossRef]
- Jardim, L.B.; Pereira, M.L.; Silveira, I.; Ferro, A.; Sequeiros, J.; Giugliani, R. Neurologic findings in Machado-Joseph disease: Relation with disease duration, subtypes, and (CAG)n. Arch. Neurol. 2001, 58, 899–904. [Google Scholar] [CrossRef] [Green Version]
- Nunes, M.B.; Martinez, A.R.; Rezende, T.J.; Friedman, J.H.; Lopes-Cendes, I.; D’Abreu, A.; França, M.C., Jr. Dystonia in Machado-Joseph disease: Clinical profile, therapy and anatomical basis. Parkinsonism Relat. Disord. 2015, 21, 1441–1447. [Google Scholar] [CrossRef] [PubMed]
- Masters, C.L.; Richardson, E.P., Jr. Subacute spongiform encephalopathy (Creutzfeldt-Jakob disease). The nature and progression of spongiform change. Brain 1978, 101, 333–344. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, A.; Takei, K.; Enomoto, K.; Mitsui, T.; Nomura, K.; Iwasaki, S.; Maruki, T.; Shimazu, K. A case of Creutzfeldt-Jakob disease exhibiting athetosis in the early stage. No Shinkei 1999, 51, 887–890. [Google Scholar]
- Maltete, D.; Guyant-Marechal, L.; Gerardin, E.; Laquerriere, A.; Martinaud, O.; Mihout, B.; Hannequin, D. Hemidystonia as initial manifestation of sporadic Creutzfeldt-Jakob disease. Eur. J. Neurol. 2006, 13, 667–668. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Contreras, M.; Baker, M.C.; Finch, N.A.; Nicholson, A.; Wojtas, A.; Wszolek, Z.K.; Ross, O.A.; Dickson, D.W.; Rademakers, R. Genetic screening and functional characterization of PDGFRB mutations associated with basal ganglia calcification of unknown etiology. Hum. Mutat. 2014, 35, 964–971. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Legati, A.; Giovannini, D.; Nicolas, G.; López-Sánchez, U.; Quintáns, B.; Oliveira, J.R.; Sears, R.L.; Ramos, E.M.; Spiteri, E.; Sobrido, M.J.; et al. Mutations in XPR1 cause primary familial brain calcification associated with altered phosphate export. Nat. Genet. 2015, 47, 579–581. [Google Scholar] [CrossRef] [PubMed]
- Lange, L.M.; Junker, J.; Loens, S.; Baumann, H.; Olschewski, L.; Schaake, S.; Madoev, H.; Petkovic, S.; Kuhnke, N.; Kasten, M.; et al. Genotype-Phenotype Relations for Isolated Dystonia Genes: MDSGene Systematic Review. Mov. Disord. Off. J. Mov. Disord. Soc. 2021, 36, 1086–1103. [Google Scholar] [CrossRef] [PubMed]
- Steel, D.; Zech, M.; Zhao, C.; Barwick, K.E.S.; Burke, D.; Demailly, D.; Kumar, K.R.; Zorzi, G.; Nardocci, N.; Kaiyrzhanov, R.; et al. Loss-of-Function Variants in HOPS Complex Genes VPS16 and VPS41 Cause Early Onset Dystonia Associated with Lysosomal Abnormalities. Ann. Neurol. 2020, 88, 867–877. [Google Scholar] [CrossRef] [PubMed]
- Monfrini, E.; Zech, M.; Steel, D.; Kurian, M.A.; Winkelmann, J.; Di Fonzo, A. HOPS-associated neurological disorders (HOPSANDs): Linking endolysosomal dysfunction to the pathogenesis of dystonia. Brain 2021, 144, 2610–2615. [Google Scholar] [CrossRef]
- Kuipers, D.J.S.; Mandemakers, W.; Lu, C.S.; Olgiati, S.; Breedveld, G.J.; Fevga, C.; Tadic, V.; Carecchio, M.; Osterman, B.; Sagi-Dain, L.; et al. EIF2AK2 Missense Variants Associated with Early Onset Generalized Dystonia. Ann. Neurol. 2021, 89, 485–497. [Google Scholar] [CrossRef]
- Magrinelli, F.; Moualek, D.; Tazir, M.; Ali Pacha, L.; Verghese, A.; Bhatia, K.P.; Maroofian, R.; Houlden, H. Heterozygous EIF2AK2 variant causes adolescence-onset generalized dystonia partially responsive to DBS. Mov. Disord. Clin. Pract. 2021. [Google Scholar] [CrossRef]
- Ebrahimi-Fakhari, D.; Van Karnebeek, C.; Munchau, A. Movement Disorders in Treatable Inborn Errors of Metabolism. Mov. Disord. Off. J. Mov. Disord. Soc. 2019, 34, 598–613. [Google Scholar] [CrossRef] [PubMed]
- Svetel, M.; Kozic, D.; Stefanova, E.; Semnic, R.; Dragasevic, N.; Kostic, V.S. Dystonia in Wilson’s disease. Mov. Disord. Off. J. Mov. Disord. Soc. 2001, 16, 719–723. [Google Scholar] [CrossRef] [PubMed]
- Gregory, A.; Hayflick, S. Neurodegeneration with Brain Iron Accumulation Disorders Overview. In GeneReviews®; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Stephens, K., Amemiya, A., Eds.; University of Washington: Seattle, MA, USA, 2019. [Google Scholar]
- Miyajima, H.; Hosoi, Y. Aceruloplasminemia. In GeneReviews®; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Stephens, K., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993. [Google Scholar]
- Ahlskog, J.E. Parkin and PINK1 parkinsonism may represent nigral mitochondrial cytopathies distinct from Lewy body Parkinson’s disease. Parkinsonism Relat. Disord. 2009, 15, 721–727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valente, E.M.; Abou-Sleiman, P.M.; Caputo, V.; Muqit, M.M.; Harvey, K.; Gispert, S.; Ali, Z.; Del Turco, D.; Bentivoglio, A.R.; Healy, D.G.; et al. Hereditary early-onset Parkinson’s disease caused by mutations in PINK1. Science 2004, 304, 1158–1160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brüggemann, N.; Spiegler, J.; Hellenbroich, Y.; Opladen, T.; Schneider, S.A.; Stephani, U.; Boor, R.; Gillessen-Kaesbach, G.; Sperner, J.; Klein, C. Beneficial prenatal levodopa therapy in autosomal recessive guanosine triphosphate cyclohydrolase 1 deficiency. Arch. Neurol. 2012, 69, 1071–1075. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Himmelreich, N.; Montioli, R.; Bertoldi, M.; Carducci, C.; Leuzzi, V.; Gemperle, C.; Berner, T.; Hyland, K.; Thöny, B.; Hoffmann, G.F.; et al. Aromatic amino acid decarboxylase deficiency: Molecular and metabolic basis and therapeutic outlook. Mol. Genet. Metab. 2019, 127, 12–22. [Google Scholar] [CrossRef]
- Vanier, M.T. Niemann-Pick disease type C. Orphanet J. Rare Dis. 2010, 5, 16. [Google Scholar] [CrossRef] [Green Version]
- Koens, L.H.; Kuiper, A.; Coenen, M.A.; Elting, J.W.; de Vries, J.J.; Engelen, M.; Koelman, J.H.; van Spronsen, F.J.; Spikman, J.M.; de Koning, T.J.; et al. Ataxia, dystonia and myoclonus in adult patients with Niemann-Pick type C. Orphanet J. Rare Dis. 2016, 11, 121. [Google Scholar] [CrossRef] [Green Version]
- Mitchison, H.M.; Hofmann, S.L.; Becerra, C.H.; Munroe, P.B.; Lake, B.D.; Crow, Y.J.; Stephenson, J.B.; Williams, R.E.; Hofman, I.L.; Taschner, P.E.; et al. Mutations in the palmitoyl-protein thioesterase gene (PPT.; CLN1) causing juvenile neuronal ceroid lipofuscinosis with granular osmiophilic deposits. Hum. Mol. Genet. 1998, 7, 291–297. [Google Scholar] [CrossRef] [Green Version]
- Yıldırım, M.; Köse, E.; Keçeli, A.M.; Balasar, Ö.; Şimşek, N. Status dystonicus associated with CLN8 disease. Brain Dev. 2020, 43, 571–575. [Google Scholar] [CrossRef] [PubMed]
- Arash-Kaps, L.; Komlosi, K.; Seegräber, M.; Diederich, S.; Paschke, E.; Amraoui, Y.; Beblo, S.; Dieckmann, A.; Smitka, M.; Hennermann, J.B. The Clinical and Molecular Spectrum of GM1 Gangliosidosis. J. Pediatr. 2019, 215, 152–157.e3. [Google Scholar] [CrossRef] [PubMed]
- Meek, D.; Wolfe, L.S.; Andermann, E.; Andermann, F. Juvenile progressive dystonia: A new phenotype of GM2 gangliosidosis. Ann. Neurol. 1984, 15, 348–352. [Google Scholar] [CrossRef] [PubMed]
- van Rappard, D.F.; Boelens, J.J.; Wolf, N.I. Metachromatic leukodystrophy: Disease spectrum and approaches for treatment. Best Prac. Res. Clin. Endocrinol. Metab. 2015, 29, 261–273. [Google Scholar] [CrossRef] [PubMed]
- Carson, N.A.; Dent, C.E.; Field, C.M.; Gaull, G.E. Homocystinuria: Clinical and pathological review of ten cases. J. Pediatr. 1965, 66, 565–583. [Google Scholar] [CrossRef]
- Biery, B.J.; Stein, D.E.; Morton, D.H.; Goodman, S.I. Gene structure and mutations of glutaryl-coenzyme A dehydrogenase: Impaired association of enzyme subunits that is due to an A421V substitution causes glutaric acidemia type I in the Amish. Am. J. Hum. Genet. 1996, 59, 1006–1011. [Google Scholar]
- Kölker, S.; Burgard, P.; Sauer, S.W.; Okun, J.G. Current concepts in organic acidurias: Understanding intra- and extracerebral disease manifestation. J. Inherit. Metab. Dis. 2013, 36, 635–644. [Google Scholar] [CrossRef]
- Cossée, M.; Dürr, A.; Schmitt, M.; Dahl, N.; Trouillas, P.; Allinson, P.; Kostrzewa, M.; Nivelon-Chevallier, A.; Gustavson, K.H.; Kohlschütter, A.; et al. Friedreich’s ataxia: Point mutations and clinical presentation of compound heterozygotes. Ann. Neurol. 1999, 45, 200–206. [Google Scholar] [CrossRef]
- Davidson, C.S. The Metabolic Basis of Inherited Disease; Stanbury, J.B., Wyngaarden, B.J., Fredrickson, D.S., Goldstein, J.L., Brown, M.S., Eds.; McGraw-Hill: New York, NY, USA, 1983; pp. 1563–1577. [Google Scholar]
- Darras, B.T.; Ampola, M.G.; Dietz, W.H.; Gilmore, H.E. Intermittent dystonia in Hartnup disease. Pediatric Neurol. 1989, 5, 118–120. [Google Scholar] [CrossRef]
- Kim, M.; Kim, A.R.; Park, J.; Kim, J.S.; Ahn, J.H.; Park, W.Y.; Kim, N.K.D.; Lee, C.; Kim, N.S.; Cho, J.W.; et al. Clinical characteristics of ataxia-telangiectasia presenting dystonia as a main manifestation. Clin. Neurol. Neurosurg. 2020, 199, 106267. [Google Scholar] [CrossRef]
- Van Os, N.J.H.; Hensiek, A.; van Gaalen, J.; Taylor, A.M.R.; van Deuren, M.; Weemaes, C.M.R.; Willemsen, M.; van de Warrenburg, B.P.C. Trajectories of motor abnormalities in milder phenotypes of ataxia telangiectasia. Neurology 2019, 92, e19–e29. [Google Scholar] [CrossRef] [PubMed]
- Levy, A.; Lang, A.E. Ataxia-telangiectasia: A review of movement disorders, clinical features, and genotype correlations. Mov. Disord. Off. J. Mov. Disord. Soc. 2018, 33, 1238–1247. [Google Scholar] [CrossRef] [PubMed]
- Campuzano, V.; Montermini, L.; Moltò, M.D.; Pianese, L.; Cossée, M.; Cavalcanti, F.; Monros, E.; Rodius, F.; Duclos, F.; Monticelli, A.; et al. Friedreich’s ataxia: Autosomal recessive disease caused by an intronic GAA triplet repeat expansion. Science 1996, 271, 1423–1427. [Google Scholar] [CrossRef] [PubMed]
- Rampoldi, L.; Danek, A.; Monaco, A.P. Clinical features and molecular bases of neuroacanthocytosis. J. Mol. Med. 2002, 80, 475–491. [Google Scholar] [CrossRef] [PubMed]
- Danek, A.; Jung, H.H.; Melone, M.A.; Rampoldi, L.; Broccoli, V.; Walker, R.H. Neuroacanthocytosis: New developments in a neglected group of dementing disorders. J. Neurol. Sci. 2005, 229–230, 171–186. [Google Scholar] [CrossRef] [PubMed]
- Paviour, D.C.; Revesz, T.; Holton, J.L.; Evans, A.; Olsson, J.E.; Lees, A.J. Neuronal intranuclear inclusion disease: Report on a case originally diagnosed as dopa-responsive dystonia with Lewy bodies. Mov. Disord. Off. J. Mov. Disord. Soc. 2005, 20, 1345–1349. [Google Scholar] [CrossRef] [PubMed]
- Kish, S.J.; Gilbert, J.J.; Chang, L.J.; Mirchandani, L.; Shannak, K.; Hornykiewicz, O. Brain neurotransmitter abnormalities in neuronal intranuclear inclusion body disorder. Ann. Neurol. 1985, 17, 405–407. [Google Scholar] [CrossRef] [PubMed]
- Goutières, F.; Mikol, J.; Aicardi, J. Neuronal intranuclear inclusion disease in a child: Diagnosis by rectal biopsy. Ann. Neurol. 1990, 27, 103–106. [Google Scholar] [CrossRef] [PubMed]
- Garen, P.D.; Powers, J.M.; Young, G.F.; Lee, V. Neuronal intranuclear hyaline inclusion disease in a nine year old. Acta Neuropathol. 1986, 70, 327–332. [Google Scholar] [CrossRef]
- Schaefer, S.M.; Szekely, A.M.; Moeller, J.J.; Tinaz, S. Hereditary spastic paraplegia presenting as limb dystonia with a rare SPG7 mutation. Neurol. Clin. Pract. 2018, 8, e49–e50. [Google Scholar] [CrossRef]
- Pfeffer, G.; Gorman, G.S.; Griffin, H.; Kurzawa-Akanbi, M.; Blakely, E.L.; Wilson, I.; Sitarz, K.; Moore, D.; Murphy, J.L.; Alston, C.L.; et al. Mutations in the SPG7 gene cause chronic progressive external ophthalmoplegia through disordered mitochondrial DNA maintenance. Brain 2014, 137, 1323–1336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daoud, H.; Papadima, E.M.; Ouled Amar Bencheikh, B.; Katsila, T.; Dionne-Laporte, A.; Spiegelman, D.; Dion, P.A.; Patrinos, G.P.; Orrù, S.; Rouleau, G.A. Identification of a novel homozygous SPG7 mutation by whole exome sequencing in a Greek family with a complicated form of hereditary spastic paraplegia. Eur. J. Med. Genet. 2015, 58, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Marcotulli, C.; Leonardi, L.; Tessa, A.; De Negris, A.M.; Cornia, R.; Pierallini, A.; Haggiag, S.; Pierelli, F.; Santorelli, F.M.; Casali, C. Early-onset optic neuropathy as initial clinical presentation in SPG7. J. Neurol. 2014, 261, 1820–1821. [Google Scholar] [CrossRef]
- Roxburgh, R.H.; Marquis-Nicholson, R.; Ashton, F.; George, A.M.; Lea, R.A.; Eccles, D.; Mossman, S.; Bird, T.; van Gassen, K.L.; Kamsteeg, E.J.; et al. The p.Ala510Val mutation in the SPG7 (paraplegin) gene is the most common mutation causing adult onset neurogenetic disease in patients of British ancestry. J. Neurol. 2013, 260, 1286–1294. [Google Scholar] [CrossRef] [PubMed]
- Van Gassen, K.L.; van der Heijden, C.D.; de Bot, S.T.; den Dunnen, W.F.; van den Berg, L.H.; Verschuuren-Bemelmans, C.C.; Kremer, H.P.; Veldink, J.H.; Kamsteeg, E.J.; Scheffer, H.; et al. Genotype-phenotype correlations in spastic paraplegia type 7: A study in a large Dutch cohort. Brain 2012, 135, 2994–3004. [Google Scholar] [CrossRef]
- Sjogren, T.; Larsson, T. Oligophrenia in combination with congenital ichthyosis and spastic disorders; a clinical and genetic study. Acta Psychiatr. Neurol. Scand. Suppl. 1957, 113, 1–112. [Google Scholar] [PubMed]
- Cubo, E.; Goetz, C.G. Dystonia secondary to Sjogren-Larsson syndrome. Neurology 2000, 55, 1236–1237. [Google Scholar] [CrossRef]
- Zeng, W.Q.; Al-Yamani, E.; Acierno, J.S., Jr.; Slaugenhaupt, S.; Gillis, T.; MacDonald, M.E.; Ozand, P.T.; Gusella, J.F. Biotin-responsive basal ganglia disease maps to 2q36.3 and is due to mutations in SLC19A3. Am. J. Hum. Genet. 2005, 77, 16–26. [Google Scholar] [CrossRef] [Green Version]
- Charlesworth, G.; Angelova, P.R.; Bartolomé-Robledo, F.; Ryten, M.; Trabzuni, D.; Stamelou, M.; Abramov, A.Y.; Bhatia, K.P.; Wood, N.W. Mutations in HPCA cause autosomal-recessive primary isolated dystonia. Am. J. Hum. Genet. 2015, 96, 657–665. [Google Scholar] [CrossRef] [Green Version]
- Zech, M.; Kumar, K.R.; Reining, S.; Reunert, J.; Tchan, M.; Riley, L.G.; Drew, A.P.; Adam, R.J.; Berutti, R.; Biskup, S.; et al. Biallelic AOPEP Loss-of-Function Variants Cause Progressive Dystonia with Prominent Limb Involvement. Mov. Disord. Off. J. Mov. Disord. Soc. 2021, 37, 137–141. [Google Scholar] [CrossRef]
- Lee, L.V.; Rivera, C.; Teleg, R.A.; Dantes, M.B.; Pasco, P.M.; Jamora, R.D.; Arancillo, J.; Villareal-Jordan, R.F.; Rosales, R.L.; Demaisip, C.; et al. The unique phenomenology of sex-linked dystonia parkinsonism (XDP, DYT3, “Lubag”). Int. J. Neurosci. 2011, 121 (Suppl. 1), 3–11. [Google Scholar] [CrossRef] [PubMed]
- Balint, B.; Mencacci, N.E.; Valente, E.M.; Pisani, A.; Rothwell, J.; Jankovic, J.; Vidailhet, M.; Bhatia, K.P. Dystonia. Nat. Rev. Dis. Primers 2018, 4, 25. [Google Scholar] [CrossRef] [PubMed]
- Nanagiri, A.; Shabbir, N. Lesch Nyhan Syndrome. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK556079/ (accessed on 15 January 2022).
- Fu, R.; Sutcliffe, D.; Zhao, H.; Huang, X.; Schretlen, D.J.; Benkovic, S.; Jinnah, H.A. Clinical severity in Lesch-Nyhan disease: The role of residual enzyme and compensatory pathways. Mol. Genet. Metab. 2015, 114, 55–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jin, H.; May, M.; Tranebjaerg, L.; Kendall, E.; Fontan, G.; Jackson, J.; Subramony, S.H.; Arena, F.; Lubs, H.; Smith, S.; et al. A novel X-linked gene, DDP, shows mutations in families with deafness (DFN-1), dystonia, mental deficiency and blindness. Nat. Genet. 1996, 14, 177–180. [Google Scholar] [CrossRef]
- Ha, A.D.; Parratt, K.L.; Rendtorff, N.D.; Lodahl, M.; Ng, K.; Rowe, D.B.; Sue, C.M.; Hayes, M.W.; Tranebjaerg, L.; Fung, V.S. The phenotypic spectrum of dystonia in Mohr-Tranebjaerg syndrome. Mov. Disord. Off. J. Mov. Disord. Soc. 2012, 27, 1034–1040. [Google Scholar] [CrossRef]
- Amir, R.E.; Van den Veyver, I.B.; Wan, M.; Tran, C.Q.; Francke, U.; Zoghbi, H.Y. Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nat. Genet. 1999, 23, 185–188. [Google Scholar] [CrossRef]
- Lake, N.J.; Compton, A.G.; Rahman, S.; Thorburn, D.R. Leigh syndrome: One disorder, more than 75 monogenic causes. Ann. Neurol. 2016, 79, 190–203. [Google Scholar] [CrossRef]
- Tranchant, C.; Anheim, M. Movement disorders in mitochondrial diseases. Rev. Neurol. 2016, 172, 524–529. [Google Scholar] [CrossRef]
- Yu-Wai-Man, P.; Turnbull, D.M.; Chinnery, P.F. Leber hereditary optic neuropathy. J. Med. Genet. 2002, 39, 162–169. [Google Scholar] [CrossRef]
- Nikoskelainen, E.K.; Marttila, R.J.; Huoponen, K.; Juvonen, V.; Lamminen, T.; Sonninen, P.; Savontaus, M.L. Leber’s “plus”: Neurological abnormalities in patients with Leber’s hereditary optic neuropathy. J. Neurol. Neurosurg. Psychiatry 1995, 59, 160–164. [Google Scholar] [CrossRef] [Green Version]
- Dressler, D. Nonprimary dystonias. Handb. Clin. Neurol. 2011, 100, 513–538. [Google Scholar] [CrossRef] [PubMed]
- Michael-Asalu, A.; Taylor, G.; Campbell, H.; Lelea, L.L.; Kirby, R.S. Cerebral Palsy: Diagnosis, Epidemiology, Genetics, and Clinical Update. Adv. Pediatrics 2019, 66, 189–208. [Google Scholar] [CrossRef] [PubMed]
- Chuang, C.; Fahn, S.; Frucht, S.J. The natural history and treatment of acquired hemidystonia: Report of 33 cases and review of the literature. J. Neurol. Neurosurg. Psychiatry 2002, 72, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Cammarota, A.; Gershanik, O.S.; Garcia, S.; Lera, G. Cervical dystonia due to spinal cord ependymoma: Involvement of cervical cord segments in the pathogenesis of dystonia. Mov. Disord. Off. J. Mov. Disord. Soc. 1995, 10, 500–503. [Google Scholar] [CrossRef] [PubMed]
- Jinnah, H.A. The Dystonias. Continuum 2019, 25, 976–1000. [Google Scholar] [CrossRef] [PubMed]
- De Keyser, J. Subtypes and localization of dopamine receptors in human brain. Neurochem. Int. 1993, 22, 83–93. [Google Scholar] [CrossRef]
- Marano, M.; di Biase, L.; Salomone, G.; Di Santo, A.; Montiroli, A.; Di Lazzaro, V. The Clinical Course of a Drug-induced Acute Dystonic Reaction in the Emergency Room. Tremor Other Hyperkinetic Mov. 2016, 6, 436. [Google Scholar] [CrossRef]
- Choi, I.S.; Cheon, H.Y. Delayed movement disorders after carbon monoxide poisoning. Eur. Neurol. 1999, 42, 141–144. [Google Scholar] [CrossRef]
- Moulick, A.; Sengupta, P.; Banerjee, S.; Basu, D. Oromandibular dystonia and persistent psychiatric symptoms in extra-pontine myelinolysis. J. Assoc. Physicians India 2008, 56, 259–261. [Google Scholar] [PubMed]
- Shah, I.; Chudgar, P. Progressive multifocal leukoencephalopathy (PML) presenting as intractable dystonia in an HIV-infected child. J. Trop. Pediatrics 2005, 51, 380–382. [Google Scholar] [CrossRef] [Green Version]
- Angelini, L.; Rumi, V.; Nardocci, N.; Combi, M.L.; Bruzzone, M.G.; Pellegrini, G. Hemidystonia symptomatic of primary antiphospholipid syndrome in childhood. Mov. Disord. Off. J. Mov. Disord. Soc. 1993, 8, 383–386. [Google Scholar] [CrossRef] [PubMed]
- Fahn, S.; Williams, D.T. Psychogenic dystonia. Adv. Neurol. 1988, 50, 431–455. [Google Scholar] [PubMed]
- Oppenheim, H. About a rare spasm disease of childhood and young age (Dysbasia lordotica progressiva, dystonia musculorum deformans). Neurol. Cent. 1911, 30, 1090–1107. [Google Scholar]
- Schramm, A.; Classen, J.; Reiners, K.; Naumann, M. Characteristics of sensory trick-like manoeuvres in jaw-opening dystonia. Mov. Disord. 2007, 22, 430–433. [Google Scholar] [CrossRef] [PubMed]
- Dressler, D. Botulinum toxin for treatment of dystonia. Eur. J. Neurol. 2010, 17, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Engstrom, P.F.; Arnoult, J.B.; Mazow, M.L.; Prager, T.C.; Wilkins, R.B.; Byrd, W.A.; Hofmann, R.J. Effectiveness of botulinum toxin therapy for essential blepharospasm. Ophthalmology 1987, 94, 971–975. [Google Scholar] [CrossRef]
- Albanese, A.; Colosimo, C.; Carretta, D.; Dickmann, A.; Bentivoglio, A.R.; Tonali, P. Botulinum toxin as a treatment for blepharospasm, spasmodic torticollis and hemifacial spasm. Eur. Neurol. 1992, 32, 112–117. [Google Scholar] [CrossRef]
- Ababneh, O.H.; Cetinkaya, A.; Kulwin, D.R. Long-term efficacy and safety of botulinum toxin A injections to treat blepharospasm and hemifacial spasm. Clin. Exp. Ophthalmol. 2014, 42, 254–261. [Google Scholar] [CrossRef]
- Kessler, K.R.; Skutta, M.; Benecke, R.; Group, G.D.S. Long-term treatment of cervical dystonia with botulinum toxin A: Efficacy, safety, and antibody frequency. J. Neurol. 1999, 246, 265–274. [Google Scholar] [CrossRef]
- Behari, M. Botulinum toxin in the treatment of writer’s cramp. J. Assoc. Physicians India 1999, 47, 694–698. [Google Scholar]
- Turjanski, N.; Pirtosek, Z.; Quirk, J.; Anderson, T.; Rivest, J.; Marsden, C.; Lees, A. Botulinum toxin in the treatment of writer’s cramp. Clin. Neuropharmacol. 1996, 19, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Schuele, S.; Jabusch, H.-C.; Lederman, R.J.; Altenmüller, E. Botulinum toxin injections in the treatment of musician’s dystonia. Neurology 2005, 64, 341–343. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, D.M.; Aminoff, M.J.; Olney, R.K. Botulinum toxin therapy for limb dystonias. Neurology 1992, 42, 627. [Google Scholar] [CrossRef] [PubMed]
- Pullman, S.L.; Greene, P.; Fahn, S.; Pedersen, S.F. Approach to the treatment of limb disorders with botulinum toxin A: Experience with 187 patients. Arch. Neurol. 1996, 53, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Quirk, J.; Sheean, G.; Marsden, C.; Lees, A. Treatment of nonoccupational limb and trunk dystonia with botulinum toxin. Mov. Disord. Off. J. Mov. Disord. Soc. 1996, 11, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Bonanni, L.; Thomas, A.; Varanese, S.; Scorrano, V.; Onofrj, M. Botulinum toxin treatment of lateral axial dystonia in Parkinsonism. Mov. Disord. Off. J. Mov. Disord. Soc. 2007, 22, 2097–2103. [Google Scholar] [CrossRef]
- di Biase, L.; Fasano, A. Low-frequency deep brain stimulation for Parkinson’s disease: Great expectation or false hope? Mov. Disord. 2016, 31, 962–967. [Google Scholar] [CrossRef]
- Kern, D.S.; Picillo, M.; Thompson, J.A.; Sammartino, F.; di Biase, L.; Munhoz, R.P.; Fasano, A. Interleaving Stimulation in Parkinson’s Disease, Tremor, and Dystonia. Stereotact. Funct. Neurosurg. 2018, 96, 379–391. [Google Scholar] [CrossRef]
- Benabid, A.L.; Chabardes, S.; Mitrofanis, J.; Pollak, P. Deep brain stimulation of the subthalamic nucleus for the treatment of Parkinson’s disease. Lancet Neurol. 2009, 8, 67–81. [Google Scholar] [CrossRef]
- Krack, P.; Batir, A.; Van Blercom, N.; Chabardes, S.; Fraix, V.; Ardouin, C.; Koudsie, A.; Limousin, P.D.; Benazzouz, A.; LeBas, J.F.; et al. Five-year follow-up of bilateral stimulation of the subthalamic nucleus in advanced Parkinson’s disease. N. Engl. J. Med. 2003, 349, 1925–1934. [Google Scholar] [CrossRef] [Green Version]
- Sandoe, C.; Krishna, V.; Basha, D.; Sammartino, F.; Tatsch, J.; Picillo, M.; di Biase, L.; Poon, Y.Y.; Hamani, C.; Reddy, D.; et al. Predictors of deep brain stimulation outcome in tremor patients. Brain Stimul. 2018, 11, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Benabid, A.L.; Pollak, P.; Gervason, C.; Hoffmann, D.; Gao, D.M.; Hommel, M.; Perret, J.E.; de Rougemont, J. Long-term suppression of tremor by chronic stimulation of the ventral intermediate thalamic nucleus. Lancet 1991, 337, 403–406. [Google Scholar] [CrossRef]
- Koller, W.C.; Lyons, K.E.; Wilkinson, S.B.; Troster, A.I.; Pahwa, R. Long-term safety and efficacy of unilateral deep brain stimulation of the thalamus in essential tremor. Mov. Disord. 2001, 16, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Di Biase, L.; Munhoz, R.P. Deep brain stimulation for the treatment of hyperkinetic movement disorders. Expert Rev. Neurother. 2016, 16, 1067–1078. [Google Scholar] [CrossRef] [PubMed]
- Mehrkens, J.H.; Botzel, K.; Steude, U.; Zeitler, K.; Schnitzler, A.; Sturm, V.; Voges, J. Long-term efficacy and safety of chronic globus pallidus internus stimulation in different types of primary dystonia. Stereotact. Funct. Neurosurg. 2009, 87, 8–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cif, L.; El Fertit, H.; Vayssiere, N.; Hemm, S. Treatment of dystonic syndromes by chronic electrical stimulation of the internal globus pallidus. J. Neurosurg. Sci. 2003, 47, 52. [Google Scholar]
- Kupsch, A.; Benecke, R.; Muller, J.; Trottenberg, T.; Schneider, G.H.; Poewe, W.; Eisner, W.; Wolters, A.; Muller, J.U.; Deuschl, G.; et al. Pallidal deep-brain stimulation in primary generalized or segmental dystonia. N. Engl. J. Med. 2006, 355, 1978–1990. [Google Scholar] [CrossRef] [Green Version]
- Vidailhet, M.; Vercueil, L.; Houeto, J.L.; Krystkowiak, P.; Benabid, A.L.; Cornu, P.; Lagrange, C.; Du Montcel, S.T.; Dormont, D.; Grand, S.; et al. Bilateral deep-brain stimulation of the globus pallidus in primary generalized dystonia. N. Engl. J. Med. 2005, 352, 459–467. [Google Scholar] [CrossRef] [Green Version]
- Giovanni, A.; Capone, F.; di Biase, L.; Ferreri, F.; Florio, L.; Guerra, A.; Marano, M.; Paolucci, M.; Ranieri, F.; Salomone, G.; et al. Oscillatory Activities in Neurological Disorders of Elderly: Biomarkers to Target for Neuromodulation. Front. Aging Neurosci. 2017, 9, 189. [Google Scholar] [CrossRef]
- Assenza, G.; Capone, F.; di Biase, L.; Ferreri, F.; Florio, L.; Guerra, A.; Marano, M.; Paolucci, M.; Ranieri, F.; Salomone, G.; et al. Corrigendum: Oscillatory Activities in Neurological Disorders of Elderly: Biomarkers to Target for Neuromodulation. Front. Aging Neurosci. 2017, 9, 252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Little, S.; Pogosyan, A.; Neal, S.; Zavala, B.; Zrinzo, L.; Hariz, M.; Foltynie, T.; Limousin, P.; Ashkan, K.; FitzGerald, J.; et al. Adaptive deep brain stimulation in advanced Parkinson disease. Ann. Neurol. 2013, 74, 449–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Little, S.; Pogosyan, A.; Neal, S.; Zrinzo, L.; Hariz, M.; Foltynie, T.; Limousin, P.; Brown, P. Controlling Parkinson’s disease with adaptive deep brain stimulation. JoVE 2014, 89, 51403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tinkhauser, G.; Pogosyan, A.; Debove, I.; Nowacki, A.; Shah, S.A.; Seidel, K.; Tan, H.; Brittain, J.S.; Petermann, K.; di Biase, L.; et al. Directional local field potentials: A tool to optimize deep brain stimulation. Mov. Disord. Off. J. Mov. Disord. Soc. 2018, 33, 159–164. [Google Scholar] [CrossRef]
- Pina-Fuentes, D.; Beudel, M.; Little, S.; van Zijl, J.; Elting, J.W.; Oterdoom, D.L.M.; van Egmond, M.E.; van Dijk, J.M.C.; Tijssen, M.A.J. Toward adaptive deep brain stimulation for dystonia. Neurosurg. Focus 2018, 45, E3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Year | Reference |
|---|---|
| 1976 | (Fahn and Eldridge) [3] |
| 1987 | (Fahn, Marsden et al.) [4] |
| 1998 | (Fahn, Marsden et al.) [5] |
| 2011 | (Albanese, Asmus et al.) [6] |
| 2013 | (Albanese, Bhatia et al.) [1] |
| Autosomal Dominant | |
| Disease | OMIM Code |
| - Oppenheim dystonia (DYT-TOR1A) | #128100 |
| - Childhood and adult onset-familial cranial limb dystonia (DYT-THAP1) | #602629 |
| - Dopa-responsive dystonia (DYT/PARK-GCH1) | #128230 |
| - Rapid-onset dystonia–parkinsonism (DYT/PARK-ATP1A3) | #128235 |
| - Myoclonus–dystonia (DYT-SGCE) | #159900 |
| - Neuroferritinopathy (NBIA/CHOREA-FTL) | #606159 |
| - Dentatorubral-pallidoluysian atrophy | #125370 |
| - Huntington’s disease | #143100 |
| - Machado–Joseph disease (SCA-ATXN3) | #109150 |
| - Creutzfeldt–Jakob disease | #123400 |
| - Primary Familial Brain Calcification | #213600 |
| - Myclonic-dystonia 26 (DYT-26) | #616398 |
| - Dystonia-28 (DYT-KMT2B) | #617284 |
| - Dystonia-30 (DYT-30) | #619291 |
| - Dystonia-33 (DYT-33) | #619687 |
| Autosomal recessive: | |
| - Wilson disease | #277900 |
| - Neurodegeneration with brain iron accumulation type 1 (NBIA/DYT-PANK2) | #234200 |
| - Neurodegeneration with brain iron accumulation type 2, infantile neuroaxonal dystrophy (NBIA/DYT/PARK-PLA2G6) | #610217 |
| - Aceruloplasminemia (NBIA/DYT/PARK-C) | #604290 |
| - Fatty acid hydroxylase-associated neurodegeneration (FAHN) (HSP/NBIA-FA2H) | #612319 |
| - Early-onset parkinsonism (PARK-Parkin) (PARK-PINK1) | #608309 |
| - Aromatic-L-amino acid decarboxylase (DYT-DDC) | #608643 |
| - Early-onset dystonia with parkinsonism (DYT-PRKRA) | #612067 |
| - Niemann–Pick type C | #257220 |
| - Juvenile neuronal ceroid-lipofuscinosis (Batten disease) | #204200 |
| - GM1 gangliosidosis (DYT/PARK-GLB1) type III, chronic/adult form | #230500 |
| - GM2 gangliosidosis | #272750 |
| - Metachromatic leukodystrophy | #250100 |
| - Homocystinuria | #277400 |
| - Glutaric acidemia (DYT/CHOR-GCDH) | #231670 |
| - Methylmalonic aciduria (DYT/CHOR-MUT) | #251000 |
| - Hartnup disease | #234500 |
| - Ataxia telangiectasia | #208900 |
| - Friedreich ataxia | #229300 |
| - Neuroacanthocytosis | #200150 |
| - Dopa-responsive dystonia (DYT/PARK-TH) | #605407 |
| - Neuronal intranuclear hyaline inclusion disease | #603472 |
| - Hereditary spastic paraplegia (HSP-SPG7) | #607259 |
| - Sjögren–Larsson syndrome (ichthyosis, spasticity, intellectual disability) | #270200 |
| - Biotin-responsive basal ganglia disease (DYT-SLC19A3) | #607483 |
| - Dystonia musculorum deformans 2 (DYT-HPCA) | #224500 |
| - Zech-boesch syndrom (DYT-31) | #619565 |
| X-linked recessive: | |
| - Dystonia-parkinsonism or Lubag syndrome (DYT/PARK-TAF1) | #314250 |
| - Lesch- Nyhan syndrome (DYT/CHOR-HPRT) | #300322 |
| - Mohr-Tranebjaerg syndrome (Deafness–dystonia syndrome) (DYT-TIMM8A) | #304700 |
| X-linked dominant | |
| - Rett syndrome | #312750 |
| Mitochondrial | |
| - Leigh syndrome | #256000 |
| - Leber’s hereditary ocular neuropathy plus dystonia (DYT-mt-ND6) | #500001 |
| Perinatal Brain Injury: |
|
| Brain Injury: |
|
| Vascular: |
|
| Neoplastic and paraneoplastic: |
|
| Drug: |
|
| Toxic: |
|
| Metabolic: |
|
| Encephalitis, infections, and post infections: |
|
| Autoimmune: |
|
| Immune encephalopathy: |
|
| Psychogenic (functional) dystonia |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
di Biase, L.; Di Santo, A.; Caminiti, M.L.; Pecoraro, P.M.; Di Lazzaro, V. Classification of Dystonia. Life 2022, 12, 206. https://doi.org/10.3390/life12020206
di Biase L, Di Santo A, Caminiti ML, Pecoraro PM, Di Lazzaro V. Classification of Dystonia. Life. 2022; 12(2):206. https://doi.org/10.3390/life12020206
Chicago/Turabian Styledi Biase, Lazzaro, Alessandro Di Santo, Maria Letizia Caminiti, Pasquale Maria Pecoraro, and Vincenzo Di Lazzaro. 2022. "Classification of Dystonia" Life 12, no. 2: 206. https://doi.org/10.3390/life12020206
APA Styledi Biase, L., Di Santo, A., Caminiti, M. L., Pecoraro, P. M., & Di Lazzaro, V. (2022). Classification of Dystonia. Life, 12(2), 206. https://doi.org/10.3390/life12020206