The Automatic Algorithm of the Auto-CPAP Device as a Tool for the Assessment of the Treatment Efficacy of CPAP in Patients with Moderate and Severe Obstructive Sleep Apnea Syndrome
Abstract
1. Introduction
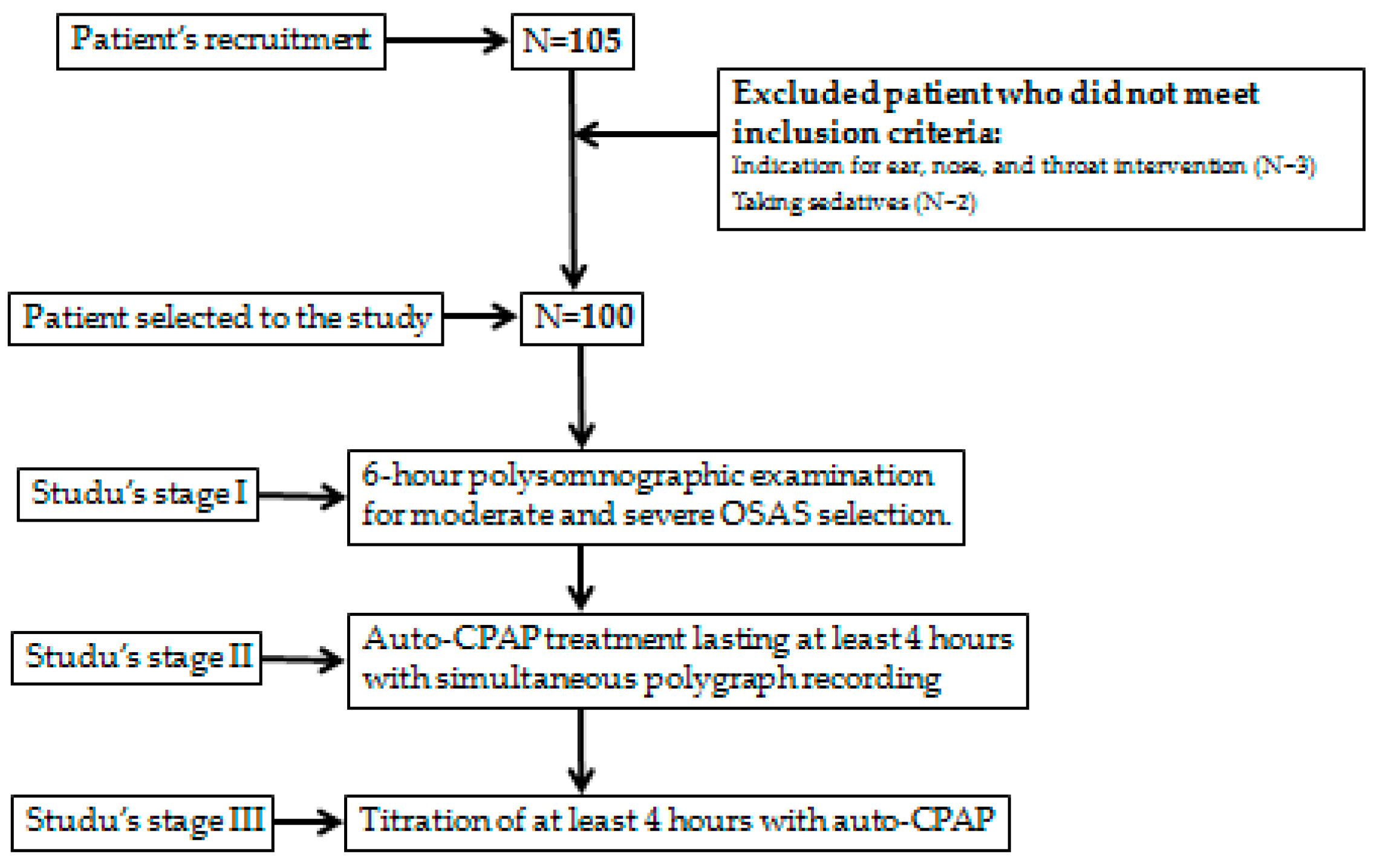
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Auto-CPAP Device Validation
2.4. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lyons, M.M.; Bhatt, N.Y.; Pack, A.I.; Magalang, U.J. Global burden of sleep-disordered breathing and its implications. Respirology 2020, 25, 690–702. [Google Scholar] [CrossRef]
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.L.; et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef]
- Kushida, C.A.; Littner, M.R.; Morgenthaler, T.; Alessi, C.A.; Bailey, D.; Coleman, J., Jr.; Friedman, L.; Hirshkowitz, M.; Kapen, S.; Kramer, M.; et al. Practice parameters for the indications for polysomnography and related procedures: An update for 2005. Sleep 2005, 28, 499–521. [Google Scholar] [CrossRef] [PubMed]
- Berry, R.B.; Brooks, R.; Gamaldo, C.; Harding, S.M.; Lloyd, R.M.; Quan, S.F.; Troester, M.T.; Vaughn, B.V. AASM Scoring Manual Updates for 2017 (Version 2.4). J. Clin. Sleep Med. 2017, 15, 665–666. [Google Scholar] [CrossRef] [PubMed]
- Epstein, L.J.; Kristo, D.; Strollo, P.J., Jr.; Friedman, N.; Malhotra, A.; Patil, S.P.; Ramar, K.; Rogers, R.; Schwab, R.J.; Weaver, E.M.; et al. Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J. Clin. Sleep Med. 2009, 15, 263–276. [Google Scholar]
- Liu, A.; Cardell, J.; Ariel, D.; Lamendola, C.; Abbasi, F.; Kim, S.H.; Holmes, T.H.; Tomasso, V.; Mojaddidi, H.; Grove, K.; et al. Abnormalities of Lipoprotein Concentrations in Obstructive Sleep Apnea Are Related to Insulin Resistance. Sleep 2015, 38, 793–799. [Google Scholar] [CrossRef]
- Abbasi, A.; Gupta, S.S.; Sabharwal, N.; Meghrajani, V.; Sharma, S.; Kamholz, S.; Kupfer, Y. A comprehensive review of obstructive sleep apnea. Sleep Sci. 2021, 14, 142–154. [Google Scholar] [CrossRef]
- Lal, C.; Weaver, T.E.; Bae, C.J.; Strohl, K.P. Excessive Daytime Sleepiness in Obstructive Sleep Apnea. Mechanisms and Clinical Management. Ann. Am. Thorac. Soc. 2021, 18, 757–768. [Google Scholar] [CrossRef]
- Stelmach-Mardas, M.; Brajer-Luftmann, B.; Kuśnierczak, M.; Batura-Gabryel, H.; Piorunek, T.; Mardas, M. Body Mass Index Reduction and Selected Cardiometabolic Risk Factors in Obstructive Sleep Apnea: Meta-Analysis. J. Clin. Med. 2021, 10, 1485. [Google Scholar] [CrossRef]
- Randerath, W.; Verbraecken, J.; de Raaff, C.A.L.; Hedner, J.; Herkenrath, S.; Hohenhorst, W.; Jakob, T.; Marrone, O.; Marklund, M.; McNicholas, W.T.; et al. European Respiratory Society guideline on non-CPAP therapies for obstructive sleep apnoea. Eur. Respir. Rev. 2021, 30, 210200. [Google Scholar] [CrossRef]
- Boyer, L.; Philippe, C.; Covali-Noroc, A.; Dalloz, M.-A.; Rouvel-Tallec, A.; Maillard, D.; Stoica, M.; d’Ortho, M.P. OSA treatment with CPAP: Randomized crossover study comparing tolerance and efficacy with and without humidification by ThermoSmart. Clin. Respir. J. 2019, 13, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Montserrat, J.M.; Ferrer, M.; Hernandez, L.; Farre, R.; Vilagut, G.; Navajas, D.; Badia, J.R.; Carrasco, E.; De Pablo, J.; Ballester, E.; et al. Effectiveness of CPAP treatment in daytime function in sleep apnea syndrome: A randomized controlled study with an optimized placebo. Am. J. Respir. Crit. Care Med. 2001, 164, 608–613. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, A.; Sakamoto, K.; Sato, K.; Nakashima, T.; Hashimoto, T.; Hara, H.; Nagura, M. Combination therapy for severe sleep apnea syndrome. Nihon Jibiinkoka Gakkai Kaiho 2005, 108, 787–793. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Patil, S.P.; Ayappa, I.A.; Caples, S.M.; Kimoff, R.J.; Patel, S.R.; Harrod, C.G. Treatment of Adult Obstructive Sleep Apnea with Positive Airway Pressure: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2019, 15, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Pływaczewski, R. Częstość i Nasilenie Zaburzeń Oddychania w Czasie snu Wśród Dorosłej Populacji Prawobrzeżnej Warszawy; Praca habilitacyjna; Instytut Gruźlicy i Chorób Płuc w Warszawie: Warsaw, Poland, 2003. [Google Scholar]
- Borsini, E.; Blanco, M.; Schonfeld, S.; Ernst, G.; Salvado, A. Performance of Epworth Sleepiness Scale and tiredness symptom used with simplified diagnostic tests for the identification of sleep apnea. Sleep Sci. 2019, 12, 287–294. [Google Scholar] [CrossRef]
- Wahba, N.; Sayeeduddin, S.; Diaz-Abad, M.; Scharf, S.M. The utility of current criteria for split-night polysomnography for predicting CPAP eligibility. Sleep Breath. 2019, 23, 729–734. [Google Scholar] [CrossRef]
- Corral, J.; Sánchez-Quiroga, M.Á.; Carmona-Bernal, C.; Sánchez-Armengol, Á.; de la Torre, A.S.; Durán-Cantolla, J.; Egea, C.J.; Salord, N.; Monasterio, C.; Terán, J.; et al. Spanish Sleep Network. Conventional Polysomnography Is Not Necessary for the Management of Most Patients with Suspected Obstructive Sleep Apnea. Noninferiority, Randomized Controlled Trial. Am. J. Respir. Crit. Care. Med. 2017, 196, 1181–1190. [Google Scholar] [CrossRef]
- Kotzian, S.T.; Schwarzinger, A.; Haider, S.; Saletu, B.; Spatt, J.; Saletu, M.T. Home polygraphic recording with telemedicine monitoring for diagnosis and treatment of sleep apnoea in stroke (HOPES Study): Study protocol for a single-blind, randomised controlled trial. BMJ Open 2018, 8, e018847. [Google Scholar] [CrossRef]
- Djonlagic, I.; Guo, M.; Matteis, P.; Carusona, A.; Stickgold, R.; Malhotra, A. First night of CPAP: Impact on memory consolidation attention and subjective experience. Sleep Med. 2015, 16, 697–702. [Google Scholar] [CrossRef]
- Cundrle, I.J.; Belehrad, M.; Jelinek, M.; Olson, L.J.; Ludka, O.; Sramek, V. The utility of perioperative polygraphy in the diagnosis of obstructive sleep apnea. Sleep Med. 2016, 25, 151–155. [Google Scholar] [CrossRef]
- Tedeschi, E.; Carratu, P.; Damiani, M.F.; Ventura, V.A.; Drigo, R.; Enzo, E.; Ferraresso, A.; Sasso, G.; Zambotto, F.M.; Resta, O. Home unattended portable monitoring and automatic CPAP titration in patients with high risk for moderate to severe obstructive sleep apnea. Respir. Care 2013, 58, 1178–1183. [Google Scholar] [CrossRef] [PubMed]
- Gagnadoux, F.; Pevernagie, D.; Jennum, P.; Lon, N.; Loiodice, C.; Tamisier, R.; van Mierlo, P.; Trzepizur, W.; Neddermann, M.; Machleit, A.; et al. Validation of the System One RemStar Auto A-Flex for Obstructive Sleep Apnea Treatment and Detection of Residual Apnea-Hypopnea Index: A European Randomized Trial. J. Clin. Sleep Med. 2017, 13, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Botokeky, E.; Freymond, N.; Gormand, F.; Le Cam, P.; Chatte, G.; Kuntz, J.; Liegeon, M.N.; Gaillot-Drevon, M.; Massardier-Pilonchery, A.; Fiquemont, A.; et al. Benefit of continuous positive airway pressure on work quality in patients with severe obstructive sleep apnea. Sleep Breath. 2019, 23, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Nigro, C.A.; Borsini, E.; Dibur, E.; Larrateguy, L.; Cazaux, A.; Elias, C.; de la Vega, M.; Berrozpe, C.; Maggi, S.; Grandval, S.; et al. Indication of CPAP without a sleep study in patients with high pretest probability of obstructive sleep apnea. Sleep Breath. 2020, 24, 1043–1050. [Google Scholar] [CrossRef]
- Bakker, J.; Weaver, T.E.; Parthasarathy, S.; Aloia, M.S. Adherence to CPAP: What Should We Be Aiming For, and How Can We Get There? Chest 2019, 155, 1272–1287. [Google Scholar] [CrossRef]
- Noseda, A.; Andre, S.; Potmans, V.; Kentos, M.; de Maertelaer, V.; Hoffmann, G. CPAP with algorithm-based versus titrated pressure: A randomized study. Sleep Med. 2009, 10, 988–992. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.Y.; Berry, R.B.; Goetting, M.G.; Staley, B.; Soto-Calderon, H.; Tsai, S.C.; Jasko, J.G.; Pack, A.I.; Kuna, S.T. Detection of upper airway status and respiratory events by a current generation positive airway pressure device. Sleep 2015, 38, 597–605. [Google Scholar] [CrossRef]
- Herkenrath, S.D.; Treml, M.; Anduleit, N.; Richter, K.; Pietzke-Calcagnile, A.; Schwaibold, M.; Schäfer, R.; Alshut, R.; Grimm, A.; Hagmeyer, L.; et al. Extended evaluation of the efficacy of a proactive forced oscillation technique-based auto-CPAP algorithm. Sleep Breath. 2020, 24, 825–833. [Google Scholar] [CrossRef]
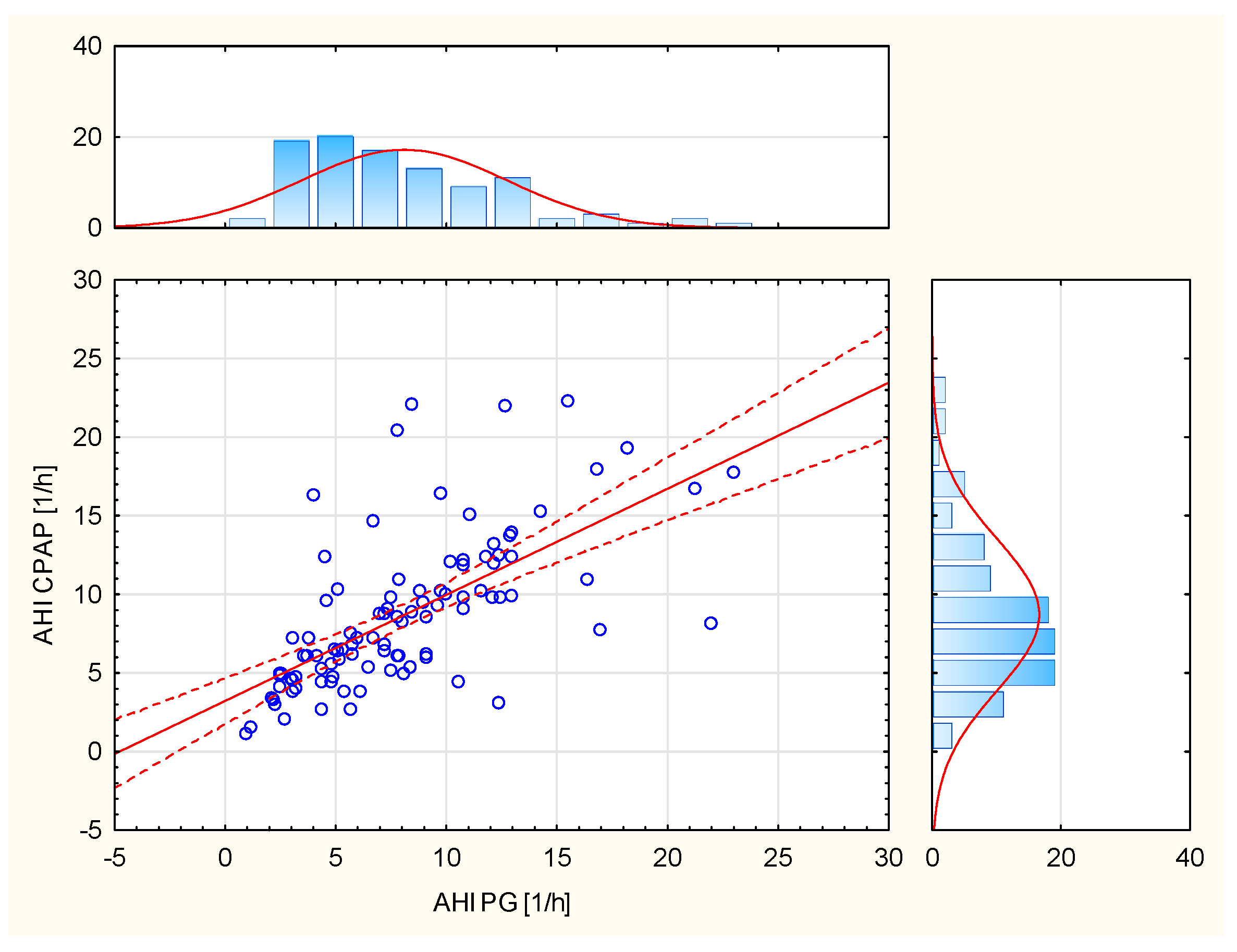


| Analyzed Variable | Mean | Minimum | Maximum | SD | Lower Quartile | Upper Quartile | Median | p-Value |
|---|---|---|---|---|---|---|---|---|
| AHI CPAP (1/h) | 8.6 | 1.1 | 22.3 | 4.8 | 4.9 | 10.9 | 7.6 | <0.0001 |
| AHI PG (1/h) | 8.3 | 1.0 | 23.0 | 4.6 | 4.5 | 10.8 | 7.5 | <0.0001 |
| ODI PG (1/h) | 9.4 | 2.1 | 39.3 | 6.2 | 5.8 | 10.7 | 7.9 | <0.0001 |
| Mean saturation PG (%) | 92.3 | 74.0 | 96.0 | 3.6 | 91.0 | 95.0 | 3.6 | <0.0001 |
| Lowest saturation PG (%) | 83.7 | 58.0 | 93.0 | 6.5 | 81.0 | 88.5 | 6.5 | <0.0001 |
| Analyzed Variable | R Spearman | p-Value |
|---|---|---|
| AHI CPAP and AHI PG | 0.7193 | <0.0001 |
| AHI CPAP and ODI PG | 0.4435 | <0.0001 |
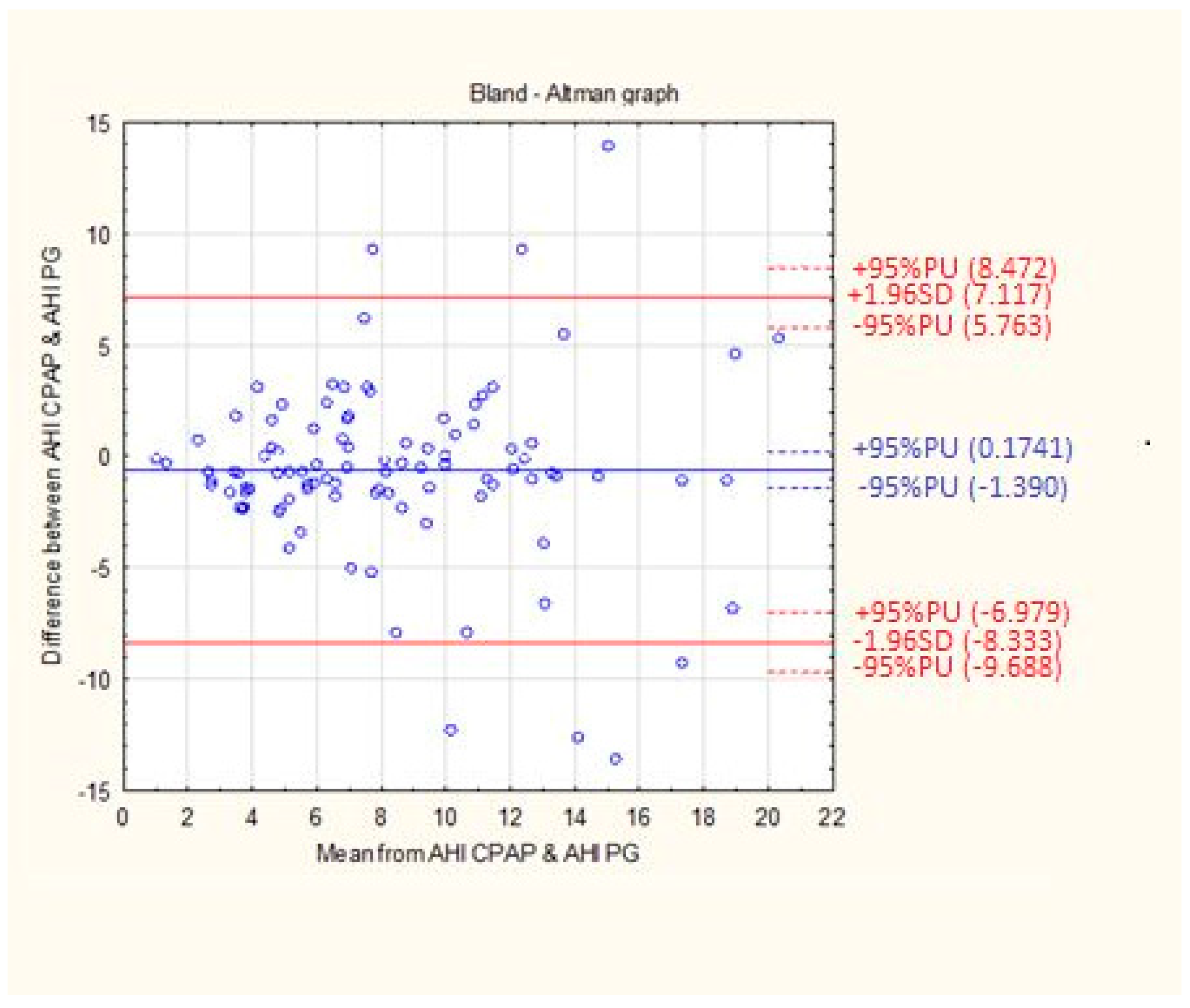
| Analyzed Variable | Mean Difference | SD | Standard Error |
|---|---|---|---|
| Difference between AHI CPAP and AHI PG | 0.6080 | 3.94 | 0.39 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brajer-Luftmann, B.; Trafas, T.; Mardas, M.; Stelmach-Mardas, M.; Batura-Gabryel, H.; Piorunek, T. The Automatic Algorithm of the Auto-CPAP Device as a Tool for the Assessment of the Treatment Efficacy of CPAP in Patients with Moderate and Severe Obstructive Sleep Apnea Syndrome. Life 2022, 12, 1357. https://doi.org/10.3390/life12091357
Brajer-Luftmann B, Trafas T, Mardas M, Stelmach-Mardas M, Batura-Gabryel H, Piorunek T. The Automatic Algorithm of the Auto-CPAP Device as a Tool for the Assessment of the Treatment Efficacy of CPAP in Patients with Moderate and Severe Obstructive Sleep Apnea Syndrome. Life. 2022; 12(9):1357. https://doi.org/10.3390/life12091357
Chicago/Turabian StyleBrajer-Luftmann, Beata, Tomasz Trafas, Marcin Mardas, Marta Stelmach-Mardas, Halina Batura-Gabryel, and Tomasz Piorunek. 2022. "The Automatic Algorithm of the Auto-CPAP Device as a Tool for the Assessment of the Treatment Efficacy of CPAP in Patients with Moderate and Severe Obstructive Sleep Apnea Syndrome" Life 12, no. 9: 1357. https://doi.org/10.3390/life12091357
APA StyleBrajer-Luftmann, B., Trafas, T., Mardas, M., Stelmach-Mardas, M., Batura-Gabryel, H., & Piorunek, T. (2022). The Automatic Algorithm of the Auto-CPAP Device as a Tool for the Assessment of the Treatment Efficacy of CPAP in Patients with Moderate and Severe Obstructive Sleep Apnea Syndrome. Life, 12(9), 1357. https://doi.org/10.3390/life12091357





