Sweet Syndrome Associated with Myelodysplastic Syndrome—A Review of a Multidisciplinary Approach
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Clinical Features
3.2. Diagnostic Criteria
3.3. Morphological Variants
3.4. Histopathology
3.5. Pathogenesis
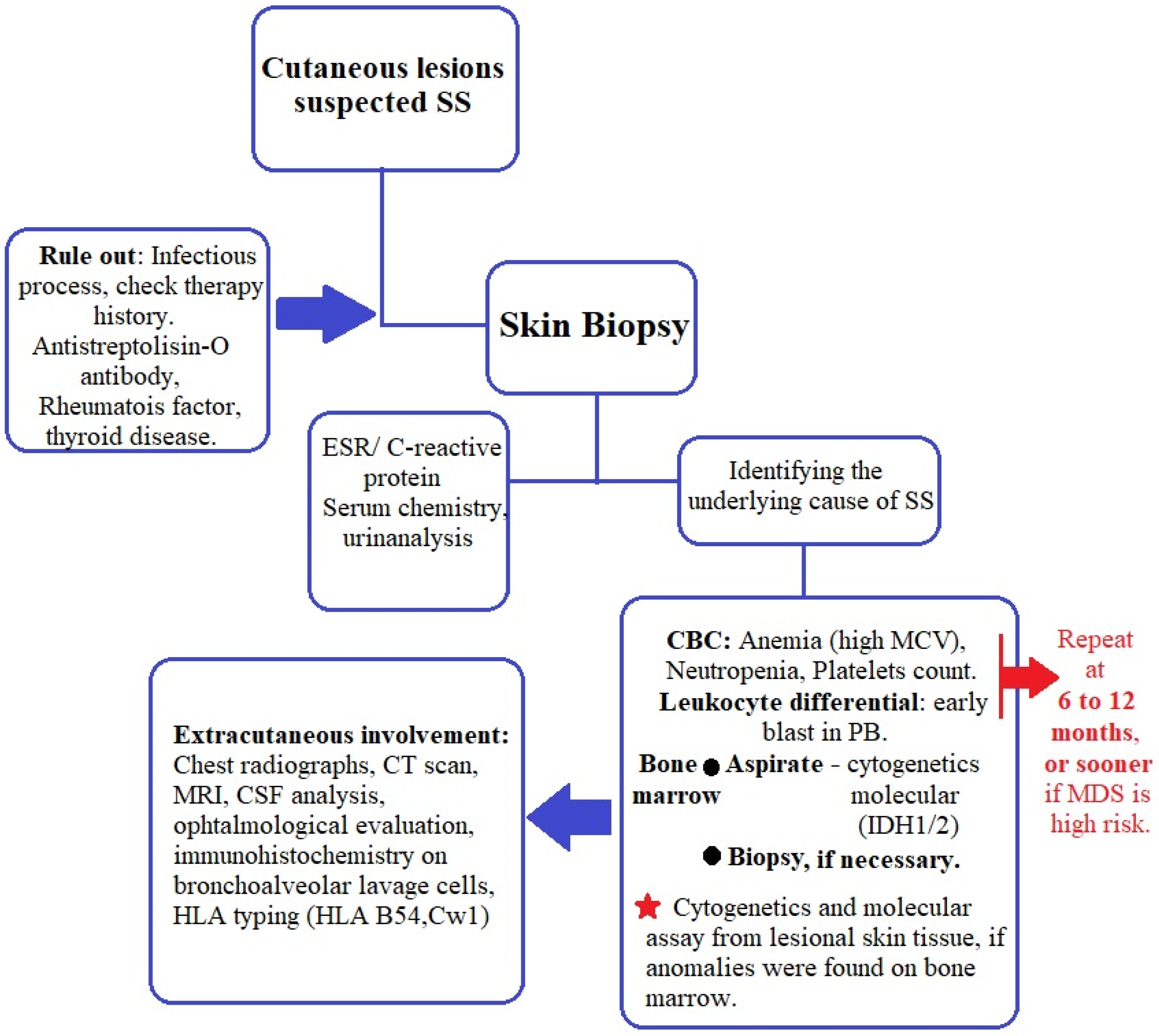
3.6. Laboratory
3.7. Cytogenetics and Molecular Assays
3.8. Treatment
4. Discussion
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Diamantino, F.D.E.R.; Raimundo, P.M.O.D.C.; Fidalgo, A.I.P.C. Síndrome de Sweet e policondrite recidivante reveladores de síndrome mielodisplásica. An. Bras. Dermatol. 2011, 86, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Kulasekararaj, A.G.; Kordasti, S.Y.; Basu, T.; Salisbury, J.; Mufti, G.J.; Du Vivier, A.W.P. Chronic relapsing remitting Sweet syndrome—A harbinger of myelodysplastic syndrome. Br. J. Haematol. 2015, 170, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Ai, M.; Yang, W.-B.; Li, X. Vital organ involvement in Sweet’s syndrome with myelodysplastic syndrome: A case report and literature review. Int. J. Dermatol. 2014, 54, 1303–1308. [Google Scholar] [CrossRef] [PubMed]
- Su, W.P.; Liu, H.N. Diagnostic criteria for Sweet’s syndrome. Cutis 1986, 37, 167–174. [Google Scholar]
- Merlant, M.; Lepelletier, C.; Battistella, M.; Vignon-Pennamen, M.-D.; Duriez, P.; Moguelet, P.; Brunet-Possenti, F.; Bagot, M.; Chasset, F.; Bouaziz, J.D. Acute myeloid leukemia and myelodysplastic syndrome–associated Sweet syndrome: A comparative multicenter retrospective study of 39 patients. J. Am. Acad. Dermatol. 2020, 84, 838–840. [Google Scholar] [CrossRef]
- Cohen, P.R. Sweet’s syndrome—A comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J. Rare Dis. 2007, 2, 34. [Google Scholar] [CrossRef]
- Cohen, P.R. Sweet’s syndrome and relapsing polychondritis: Is their appearance in the same patient a coincidental occurrence or a bona fide association of these conditions? Int. J. Dermatol. 2004, 43, 772–777. [Google Scholar] [CrossRef]
- Miranda, C.V.D.R.; Filgueiras, F.D.M.; Obadia, D.L.; Gripp, A.C.; Alves, M.D.F.S.G. Síndrome de Sweet associada a linfoma de Hodgkin: Relato de caso. An. Bras. Dermatol. 2011, 86, 1016–1018. [Google Scholar] [CrossRef]
- Kakaletsis, N.; Kaiafa, G.; Savopoulos, C.; Iliadis, F.; Perifanis, V.; Tzalokostas, V.; Grekou, A.; Giannouli, A.; Hatzitolios, A.I. Initially Lymphocytic Sweet’s Syndrome in Male Patients with Myelodysplasia: A Distinguished Clinicopathological Entity? Case Report and Systematic Review of the Literature. Acta Haematol. 2014, 132, 220–225. [Google Scholar] [CrossRef]
- Maller, B.; Bigness, A.; Moiño, D.; Greene, J. Sweet’s syndrome associated with hematological malignancies. Leuk. Res. 2020, 99, 106461. [Google Scholar] [CrossRef]
- Dotson, J.L.; Yehuda, L. Myelodysplastic Syndrome—StatPearls—NCBI Bookshelf; StatPearls: Treasure Island, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK534126/ (accessed on 4 January 2023).
- Rochet, N.M.; Chavan, R.N.; Cappel, M.A.; Wada, D.A.; Gibson, L.E. Sweet syndrome: Clinical presentation, associations, and response to treatment in 77 patients. J. Am. Acad. Dermatol. 2013, 69, 557–564. [Google Scholar] [CrossRef] [PubMed]
- Heath, M.; Ortega-Loayza, A.G. Insights Into the Pathogenesis of Sweet’s Syndrome. Front. Immunol. 2019, 10, 414. [Google Scholar] [CrossRef]
- Cohen, P.R. Neutrophilic Dermatoses: A review of current treatment options. Am. J. Clin. Dermatol. 2009, 10, 301–312. [Google Scholar] [CrossRef] [PubMed]
- Mizes, A.; Khosravi, H.; Bordelon, J.; Kazlouskaya, V.; Karunamurthy, A.; Ho, J.; James, A.; Patton, T. Sweet syndrome with pulmonary involvement in a patient with myelodysplastic syndrome. Dermatol. Online J. 2020, 26. [Google Scholar] [CrossRef]
- Li, B.; Ma, Z.; Xu, X.; Yin, J.; Wang, X.; Ren, J.; Wang, S.; Yang, J.; Ma, T.; Zhang, Q.; et al. Multi-organ Involvement of Sweet’s Syndrome: A Case Report and Literature Review. Intern. Med. 2015, 54, 339–343. [Google Scholar] [CrossRef][Green Version]
- Astudillo, L.; Sailler, L.; Launay, F.; Josse, A.G.; Lamant, L.; Couret, B.; Arlet-Suau, E. Pulmonary involvement in Sweet’s syndrome: A case report and review of the literature. Int. J. Dermatol. 2006, 45, 677–680. [Google Scholar] [CrossRef] [PubMed]
- Joshi, T.P.; Friske, S.K.; Hsiou, D.A.; Duvic, M. New Practical Aspects of Sweet Syndrome. Am. J. Clin. Dermatol. 2022, 23, 301–318. [Google Scholar] [CrossRef]
- Shugarman, I.L.; Schmit, J.M.; Sbicca, J.A.; Wirk, B. Easily Missed Extracutaneous Manifestation of Malignancy-Associated Sweet’s Syndrome: Systemic Inflammatory Response Syndrome. J. Clin. Oncol. 2011, 29, e702–e705. [Google Scholar] [CrossRef]
- Aydemir, H.; Öztoprak, N.; Celebi, G.; Altinyazar, C.; Barut, F.; Piskin, N.; Akduman, D. Pulmonary and Central Nervous System Involvement in Sweet’s Syndrome: A Very Rare Case Report. Intern. Med. 2008, 47, 1481–1484. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.R.; Talpaz, M.; Kurzrock, R. Malignancy-associated Sweet’s syndrome: Review of the world literature. J. Clin. Oncol. 1988, 6, 1887–1897. [Google Scholar] [CrossRef]
- Hisanaga, K.; Hosokawa, M.; Sato, N.; Mochizuki, H.; Itoyama, Y.; Iwasaki, Y. Neuro-Sweet Disease. Arch. Neurol. 1999, 56, 1010–1013. [Google Scholar] [CrossRef] [PubMed]
- Oka, S.; Ono, K.; Nohgawa, M. Successful Treatment of Syndrome of Inappropriate Antidiuretic Hormone Secretion Associated with Neuro-Sweet Disease in Myelodysplastic Syndrome. Intern. Med. 2018, 57, 595–600. [Google Scholar] [CrossRef] [PubMed]
- Niculet, E.; Chioncel, V.; Elisei, A.M.; Miulescu, M.; Buzia, O.D.; Nwabudike, L.C.; Craescu, M.; Draganescu, M.; Bujoreanu, F.; Marinescu, E.; et al. Multifactorial expression of IL-6 with update on COVID-19 and the therapeutic strategies of its blockade (Review). Exp. Ther. Med. 2021, 21, 263. [Google Scholar] [CrossRef]
- Wallach, A.I.; Magro, C.M.; Franks, A.G.; Shapiro, L.; Kister, I. Protean Neurologic Manifestations of Two Rare Dermatologic Disorders: Sweet Disease and Localized Craniofacial Scleroderma. Curr. Neurol. Neurosci. Rep. 2019, 19, 11. [Google Scholar] [CrossRef] [PubMed]
- Kemmett, D.; Hunter, J.A. Sweet’s syndrome: A clinicopathologic review of twenty-nine cases. J. Am. Acad. Dermatol. 1990, 23, 503–507. [Google Scholar] [CrossRef]
- Sitjas, D.; Puig, L.; Cuatrecasas, M.; DE Moragas, J.M. Acute Febrile Neutrophilic Dermatosis (Sweet’s Syndrome). Int. J. Dermatol. 1993, 32, 261–268. [Google Scholar] [CrossRef]
- Gunawardena, D.; Gunawardena, K.; Ratnayaka, R.; Vasanthanathan, N. The clinical spectrum of Sweet’s syndrome (acute febrile neutrophilic dermatosis)—A report of eighteen cases. Br. J. Dermatol. 1975, 92, 363–373. [Google Scholar] [CrossRef]
- Gottlieb, C.C.; Mishra, A.; Belliveau, D.; Green, P.; Heathcote, J.G. Ocular Involvement in Acute Febrile Neutrophilic Dermatosis (Sweet Syndrome): New Cases and Review of the Literature. Surv. Ophthalmol. 2008, 53, 219–226. [Google Scholar] [CrossRef]
- Driesch, P.V.D. Sweet’s syndrome (acute febrile neutrophilic dermatosis). J. Am. Acad. Dermatol. 1994, 31, 535–556. [Google Scholar] [CrossRef]
- Ghoufi, L.; Ortonne, N.; Ingen-Housz-Oro, S.; Barhoumi, W.; Begon, E.; Haioun, C.; Pautas, C.; Beckerich, F.; Robin, C.; Wolkenstein, P.; et al. Histiocytoid Sweet Syndrome Is More Frequently Associated with Myelodysplastic Syndromes Than the Classical Neutrophilic Variant: A Comparative Series of 62 Patients. Medicine 2016, 95, e3033. [Google Scholar] [CrossRef]
- Obiorah, I.E.; Patel, B.A.; Groarke, E.M.; Wang, W.; Trick, M.; Ombrello, A.K.; Ferrada, M.A.; Wu, Z.; Gutierrez-Rodrigues, F.; Lotter, J.; et al. Benign and malignant hematologic manifestations in patients with VEXAS syndrome due to somatic mutations in UBA1. Blood Adv. 2021, 5, 3203–3215. [Google Scholar] [CrossRef]
- Calvo, K.R. Skin in the game: The emergence of myelodysplasia cutis. Blood 2022, 139, 1132–1134. [Google Scholar] [CrossRef]
- Walker, D.C.; Cohen, P.R. Trimethoprim-sulfamethoxazole-associated acute febrile neutrophilic dermatosis: Case report and review of drug-induced Sweet’s syndrome. J. Am. Acad. Dermatol. 1996, 34, 918–923. [Google Scholar] [CrossRef] [PubMed]
- Nofal, A.; Abdelmaksoud, A.; Amer, H.; Nofal, E.; Yosef, A.; Gharib, K.; Albalat, W.; Eldesouky, F.; Ebrahim, H.M.; Abdelshafy, A.S.; et al. Sweet’s syndrome: Diagnostic criteria revisited. JDDG J. Dtsch. Dermatol. Ges. 2017, 15, 1081–1088. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.R. Skin lesions of Sweet syndrome and its dorsal hand variant contain vasculitis: An oxymoron or an epiphenomenon? Arch. Dermatol. 2002, 138, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Galaria, N.A.; Junkins-Hopkins, J.M.; Kligman, D.; James, W.D. Neutrophilic dermatosis of the dorsal hands: Pustular vasculitis revisited. J. Am. Acad. Dermatol. 2000, 43, 870–874. [Google Scholar] [CrossRef] [PubMed]
- Struton, G.; Weedon, D.; Robertson, I. Pustular vasculitis of the hands. J. Am. Acad. Dermatol. 1995, 32, 192–198. [Google Scholar] [CrossRef]
- Cohen, P.R. Subcutaneous Sweet’s syndrome: A variant of acute febrile neutrophilic dermatosis that is included in the histopathologic differential diagnosis of neutrophilic panniculitis. J. Am. Acad. Dermatol. 2005, 52, 927–928. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.R.; Holder, W.; Rapini, R. Concurrent Sweet’s syndrome and erythema nodosum: A report, world literature review and mechanism of pathogenesis. J. Rheumatol. 1992, 19, 814–820. Available online: https://pubmed.ncbi.nlm.nih.gov/1613717/ (accessed on 6 January 2023).
- Cohen, P.R. Sweet’s Syndrome Presenting as Conjunctivitis. Arch. Ophthalmol. 1993, 111, 587–588. [Google Scholar] [CrossRef]
- Cohen, P.R.; Kurzrock, R. Erratum. Am. Rev. Respir. Dis. 1992, 146, 269. [Google Scholar] [CrossRef]
- Chen, O.; Partarrieu-Mejías, F.; Alarcón-Cabrera, R. Erythema and bullae on the face and hands of a farm worker. Clin. Exp. Dermatol. 2018, 44, 99–101. [Google Scholar] [CrossRef]
- Esposito, I.; Fossati, B.; Peris, K.; De Simone, C. A rare case of bullous Sweet’s syndrome in a patient with inactive ulcerative colitis. J. Eur. Acad. Dermatol. Venereol. 2019, 33, e380–e381. [Google Scholar] [CrossRef]
- Giannoni, M.; Rizzetto, G.; Sapigni, C.; Paolinelli, M.; Tagliati, C.; Diotallevi, F.; Campanati, A.; Mandolesi, A.; Pepi, L.; Offidani, A. Bullous Sweet’s syndrome in a patient with ulcerative colitis: A rare case report. Acta Dermatovenerol. Alp. Pannonica Adriat. 2020, 29. [Google Scholar] [CrossRef]
- Tatu, A.L.; Nwabudike, L.C. Bullous Reactions Associated With COX-2 Inhibitors. Am. J. Ther. 2017, 24, e477–e480. [Google Scholar] [CrossRef]
- Garcia, E.C.; Ramos, J.D.P.V.; Ortiz, R.A. Cellulitis-like Sweet Syndrome caused by adalimumab therapy for severe hidradenitis suppurativa. Australas. J. Dermatol. 2020, 61, e448–e449. [Google Scholar] [CrossRef]
- Mitaka, H.; Jammal, R.; Saabiye, J.; Yancovitz, S.; Perlman, D.C. Giant cellulitis-like Sweet syndrome: An underrecognized clinical variant mimicking skin and soft tissue infection. Idcases 2020, 21, e00874. [Google Scholar] [CrossRef]
- Okuyama, S.; Nito, T.; Yanagawa, N.; Tajima, K. Giant cellulitis-like Sweet syndrome as an initial clinical presentation of acute myeloblastic leukemia with t(6;9)(p23;q34): DEK-CAN and internal duplications of FMS-like tyrosine kinase 3. Ann. Hematol. 2019, 98, 787–788. [Google Scholar] [CrossRef] [PubMed]
- Kroshinsky, D.; Alloo, A.; Rothschild, B.; Cummins, J.; Tan, J.; Montecino, R.; Hoang, M.P.; Duncan, L.; Mihm, M.; Sepehr, A. Necrotizing Sweet syndrome: A new variant of neutrophilic dermatosis mimicking necrotizing fasciitis. J. Am. Acad. Dermatol. 2012, 67, 945–954. [Google Scholar] [CrossRef] [PubMed]
- Malone, J.C.; Slone, S.P.; Wills-Frank, L.A.; Fearneyhough, P.K.; Lear, S.C.; Goldsmith, L.J.; Hood, A.F.; Callen, J.P. Vascular Inflammation (Vasculitis) in Sweet Syndrome. Arch. Dermatol. 2002, 138, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Requena, L.; Kutzner, H.; Palmedo, G.; Pascual, M.; Fernández-Herrera, J.; Fraga, J.; García-Díez, A.; Yus, E.S. Histiocytoid Sweet Syndrome: A dermal infiltration of immature neutrophilic granulocytes. Arch. Dermatol. 2005, 141, 834–842. [Google Scholar] [CrossRef] [PubMed]
- Libby, T.J.; Fleming, K.; Amin, B. Histiocytoid Sweet syndrome harboring an isocitrate dehydrogenase 1 mutation: A case report and retrospective analysis of 29 cases of histiocytoid Sweet syndrome. J. Cutan. Pathol. 2019, 46, 290–292. [Google Scholar] [CrossRef] [PubMed]
- Villarreal-Villarreal, C.D.; Ocampo-Candiani, J.; Villarreal-Martínez, A. Sweet Syndrome: A Review and Update. Actas Dermo-Sifiliográficas 2016, 107, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Sweet, R.B. An Acute Febrile Neutrophtlic Dermatosts. Br. J. Dermatol. 1964, 76, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Meyer, V.; Schneider, S.; Bonsmann, G.; Beissert, S. Experimentally Confirmed Induction of Sweet’s Syndrome by Phototesting. Acta Dermato-Venereol. 2011, 91, 720–721. [Google Scholar] [CrossRef] [PubMed]
- Parsapour, K.; Reep, M.D.; Gohar, K.; Shah, V.; Church, A.; Shwayder, T.A. Familial Sweet’s syndrome in 2 brothers, both seen in the first 2 weeks of life. J. Am. Acad. Dermatol. 2003, 49, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Zamanian, A.; Ameri, A. Acute febrile neutrophilic dermatosis (Sweet’s syndrome): A study of 15 cases in Iran. Int. J. Dermatol. 2007, 46, 571–574. [Google Scholar] [CrossRef]
- Chiang, C.-T.; Chan, H.-L.; Kuo, T.-T.; Wang, P.-N. Correspondence. Int. J. Dermatol. 1997, 36, 717–720. [Google Scholar] [CrossRef]
- Chan, M.P.; Duncan, L.M.; Nazarian, R.M. Subcutaneous Sweet syndrome in the setting of myeloid disorders: A case series and review of the literature. J. Am. Acad. Dermatol. 2013, 68, 1006–1015. [Google Scholar] [CrossRef]
- Vignon-Pennamen, M.D.; Osio, A.; Battistella, M. Histiocytoid Sweet Syndrome and Myelodysplastic Syndrome. JAMA Dermatol. 2017, 153, 835–836. [Google Scholar] [CrossRef]
- Snyder, R.; Libby, T.; Raciti, P.; Amin, B.; Jacobson, M.; Rakheja, D.; Fleming, K.; Bartenstein, M.; Zhu, C.; Goel, S.; et al. Myelodysplastic Syndrome and Sweet’s Syndrome Are Associated with a Mutation in Isocitrate Dehydrogenase 1. Anticancer Res. 2018, 38, 2201–2205. [Google Scholar] [CrossRef] [PubMed]
- Alegría-Landa, V.; Cerroni, L.; Requena, L. Histiocytoid Sweet Syndrome and Myelodysplastic Syndrome—Reply. JAMA Dermatol. 2017, 153, 836–837. [Google Scholar] [CrossRef] [PubMed]
- Haber, R.; Feghali, J.; El Gemayel, M. Risk of malignancy in histiocytoid Sweet syndrome: A systematic review and reappraisal. J. Am. Acad. Dermatol. 2020, 83, 661–663. [Google Scholar] [CrossRef] [PubMed]
- Kamimura, A.; Yanagisawa, H.; Tsunemi, Y.; Kusano, T.; Arai, E.; Tsuchida, T.; Nakamura, K. Normolipemic xanthomatized Sweet’s syndrome: A variant of Sweet’s syndrome with myelodysplastic syndrome. J. Dermatol. 2021, 48, 695–698. [Google Scholar] [CrossRef] [PubMed]
- Nwabudike, L.C.; Tatu, A.L. Koebner’s sheep in Wolf’s clothing: Does the isotopic response exists as a distinct phenomenon? J. Eur. Acad. Dermatol. Venereol. 2018, 32, e336–e337. [Google Scholar] [CrossRef]
- Natkunarajah, J.; Gordon, K.; Chow, J.; Sarkany, R.; Millington, G.W.; Marsden, R.A. Photoaggravated Sweet’s syndrome. Clin. Exp. Dermatol. 2010, 35, e18–e19. [Google Scholar] [CrossRef]
- Tatu, A.; Nadasdy, T.; Bujoreanu, F.; Niculet, E.; Nwabudike, L.; Radaschin, D. 168 New considerations regarding vesicular rashes associated with SARS-CoV2 infection and Koebner phenomenon. J. Investig. Dermatol. 2022, 142, S208. [Google Scholar] [CrossRef]
- Tatu, A.L.; Baroiu, L.; Fotea, S.; Anghel, L.; Polea, E.D.; Nadasdy, T.; Chioncel, V.; Nwabudike, L.C. A Working Hypothesis on Vesicular Lesions Related to COVID-19 Infection, Koebner Phenomena Type V, and a Short Review of Related Data. Clin. Cosmet. Investig. Dermatol. 2021, 14, 419–423. [Google Scholar] [CrossRef]
- Kazmi, S.M.; Pemmaraju, N.; Patel, K.P.; Cohen, P.R.; Daver, N.; Tran, K.M.; Ravandi, F.; Duvic, M.; Garcia-Manero, G.; Pierce, S.; et al. Characteristics of Sweet Syndrome in Patients with Acute Myeloid Leukemia. Clin. Lymphoma Myeloma Leuk. 2014, 15, 358–363. [Google Scholar] [CrossRef]
- Observational Study of the Genetic Architecture of Neutrophil-Mediated Inflammatory Skin Diseases. Clin-icalTrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT01952275 (accessed on 1 March 2023).
- Fujii, A.; Mizutani, Y.; Hattori, Y.; Takahashi, T.; Ohnishi, H.; Yoshida, S.; Seishima, M. Sweet’s Syndrome Successfully Treated with Granulocyte and Monocyte Adsorption Apheresis. Case Rep. Dermatol. 2017, 9, 13–18. [Google Scholar] [CrossRef]
- Agarwal, A.; Barrow, W.; Selim, M.A.; Nicholas, M.W. Refractory Subcutaneous Sweet Syndrome Treated With Adalimumab. JAMA Dermatol. 2016, 152, 842. [Google Scholar] [CrossRef] [PubMed]
- Nelis, S.; Azerad, M.A.; Drowart, A.; Lewalle, P.; Efira, A. Sweet’s syndrome induced by pegfilgrastim during a myelodysplastic syndrome AREB2: A case report. La Rev. Med. Interne 2019, 40, 258–261. [Google Scholar] [CrossRef] [PubMed]
| Antibiotics |
|---|
| Minocycline |
| Norfloxacin |
| Quinupristin/dalfopristin |
| Nitrofurantoin |
| Ofloxacin |
| Trimethoprim-sulfamethoxazole |
| Antiepileptics |
| Diazepam |
| Carbamazepine |
| Antihuman immunodeficiency virus drugs |
| Abacavir |
| Antihypertensives |
| Hydralazine |
| Antineoplastics |
| Imatinib mesylate |
| Bortezomib |
| Lenalidomide |
| Antipsychotics |
| Clozapine |
| Antithyroid hormone synthesis drugs |
| Propylthiouracil |
| Colony stimulating factors |
| Granulocyte-colony stimulating factor |
| Pegfilgrastim |
| Granulocyte-macrophage-colony stimulating factor |
| Contraceptives |
| Levonorgestrel-releasing intrauterine system |
| Levonorgestrel/ethinyl estradiol |
| Diuretics |
| Furosemide |
| Nonsteroidal anti-inflammatory agents |
| Diclofenac |
| Celecoxib |
| Retinoids |
| 13-cis-retinoic acid |
| All-trans retinoic acid |
| Major Criteria |
|---|
| 1. Erythematous plaques or nodules, painful, with sudden debut |
| 2. Neutrophilic infiltrate and absence of vasculitis on histopathological examination |
| Minor criteria |
| 1. Fever > 38 °C |
| 2. Presence of inflammatory disease, pregnancy, or history of recent upper respiratory infection, gastrointestinal infection, or vaccination |
| 3. Responsiveness to systemic glucocorticoid therapy or potassium iodide |
| 4. Modified laboratory values at presentation (three of the following): a. ESR > 20 mm/h b. Elevated C—reactive protein c. leukocytosis > 8000/µL d. neutrophils > 70% |
| Constant Features * |
|---|
| 1. Clinical: Sudden onset of painful or tender erythematous papules, plaques, or nodules |
| 2. Histopathological: Dense dermal neutrophilic infiltrate |
| Variable features ** |
| 1. Clinical |
| Fever > 38 °C Atypical skin lesions (including hemorrhagic blisters, pustular lesions, cellulitis-like-lesions) |
| 2. Histopathological |
| Presence or absence of leukocytoclastic vasculitis Subcutaneous variant Histiocytoid variant Xanthomatoid variant Cryptococcoid variant |
| 3. Laboratory |
| Elevated ESR Elevated C—reactive protein levels Leukocytosis Neutrophilia Anemia |
| Study | Age | Lesion Type/Location | Clinical Symptoms | CBC | Skin Biopsy with Histopathological Findings | Cytogenetic Analysis | Other Laboratory Findings | MDS Type | MDS Prognostic | ∆Time between MDS and SS |
|---|---|---|---|---|---|---|---|---|---|---|
| Satoko Oka et al. [23] | 66 | Rash over both legs | fever | WBC-normal; RBC-2.9 mil/mm3; Hb 9.2 g/dL, platelets–normal | Neutrophilic infiltration of the dermis and the absence of leukocytoclastic vasculitis, cutaneous vasculitis and thrombosis | 46, XX | CRP level: 20.9 mg/dL; HLA-B54 positive/HLA-B51 negative | RA; MDS-SLD | Good | 270 days |
| S. Nelis et al. [74] | 46 | Conjunctivitis and erythematous nodular rash on lower right eyelid, elbows, forearms and legs | fever | Pancytopenia, Hb 8.1 g/dL; WBC 1550/mm3; Platelets 16.000/mm3 | Dense inflammatory infiltrate, consisting of neutrophils, edema of the papillary dermis and extravasation of red blood cells without sign of vasculitis | N/A | CRP level: 200 mg/L | MDS-EB1/MDS-EB2 | N/A | 11 days of Chemo/3 days of Filgrastim |
| F. da Encarnação Roque Diamantino et al. [1] | 79 | Erythematous, circular plaques, pseudo vesicular, with light pink centers, painful, sized from 0.5 to 3 cm, located on the neck, torso and upper arms | fever | WBC 3.400/mm3; non-megaloblastic macrocytic anemia (later state) | Inflammatory infiltrate, dense and with perivascular disposition, consisting mainly of neutrophils, many with leukocytoclasia | N/A | ESR 50 mm/h | MDS-SLD | N/A | 0 days |
| A. Mizes et al. [15] | 59 | Violaceous papules located on upper and lower limbs | fever | Pancytopenia, Hb 6.0 g/dL, Platelets 30.000/mm3 | Focal parakeratosis and mild spongiosis overlying a deep dermal, subcutaneous, and peri-eccrine neutrophil rich inflammatory infiltrate | KMT2A—FISH analysis | CRP level: 38.39 mg/L, ESR 140 mm/h | MDS-EB2 | Poor | 1 day |
| A. Kamimura et al. [65] | 62 | Erythema and papules on chest, later on upper extremities | subfever | WBC normal, Hb 8.1 g/dL, Platelets normal | Dense infiltration into the dermis, comprising neutrophils, foamy histiocytes, and leukocytoclastic deposits extending into the mid and deep dermis. Neutrophilic infiltration with leukocytoclasia, numerous xanthomatized cells with large foamy cytoplasm faintly positive for myeloperoxidase (MPO), CD68 (PGM-1), and CD163 | N/A | CRP 2.34 mg/dL | MDS-SLD (Mgk) | N/A | 60 days |
| T. J. Libby et al. [53] | 50 | Erythematous papulonodules on his trunk and extremities | N/A | neutropenia and macrocytic anemia | Lobular and septal panniculitis with mononuclear cells that expressed CD68 and myeloperoxidase, later dermal and subcutaneous HSS | N/A | N/A | MDS with IDH-1 mutation | N/A | 60 days |
| Yun Li et al. [3] | 63 | Tender erythematous skin lesions on the face, neck, and extremities. | fever | WBC- normal, Hb 5.1 g/dL, Platelets 21.000/mm3 | Mild subepidermal edema, a diffuse infiltrate of predominantly mature neutrophils, and nuclear dust, no evidence of vasculitis or epidermal involvement | N/A | ESR 80 mm/h | MDS-EB1 | N/A | 30 days |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferea, C.R.; Mihai, S.N.; Balan, G.; Badescu, M.C.; Tutunaru, D.; Tatu, A.L. Sweet Syndrome Associated with Myelodysplastic Syndrome—A Review of a Multidisciplinary Approach. Life 2023, 13, 809. https://doi.org/10.3390/life13030809
Ferea CR, Mihai SN, Balan G, Badescu MC, Tutunaru D, Tatu AL. Sweet Syndrome Associated with Myelodysplastic Syndrome—A Review of a Multidisciplinary Approach. Life. 2023; 13(3):809. https://doi.org/10.3390/life13030809
Chicago/Turabian StyleFerea, Cătălina Roxana, Stejara Nicoleta Mihai, Gabriela Balan, Minerva Codruta Badescu, Dana Tutunaru, and Alin Laurențiu Tatu. 2023. "Sweet Syndrome Associated with Myelodysplastic Syndrome—A Review of a Multidisciplinary Approach" Life 13, no. 3: 809. https://doi.org/10.3390/life13030809
APA StyleFerea, C. R., Mihai, S. N., Balan, G., Badescu, M. C., Tutunaru, D., & Tatu, A. L. (2023). Sweet Syndrome Associated with Myelodysplastic Syndrome—A Review of a Multidisciplinary Approach. Life, 13(3), 809. https://doi.org/10.3390/life13030809







