Are Gender Differences Important for Autoimmune Liver Diseases?
Abstract
:1. Introduction
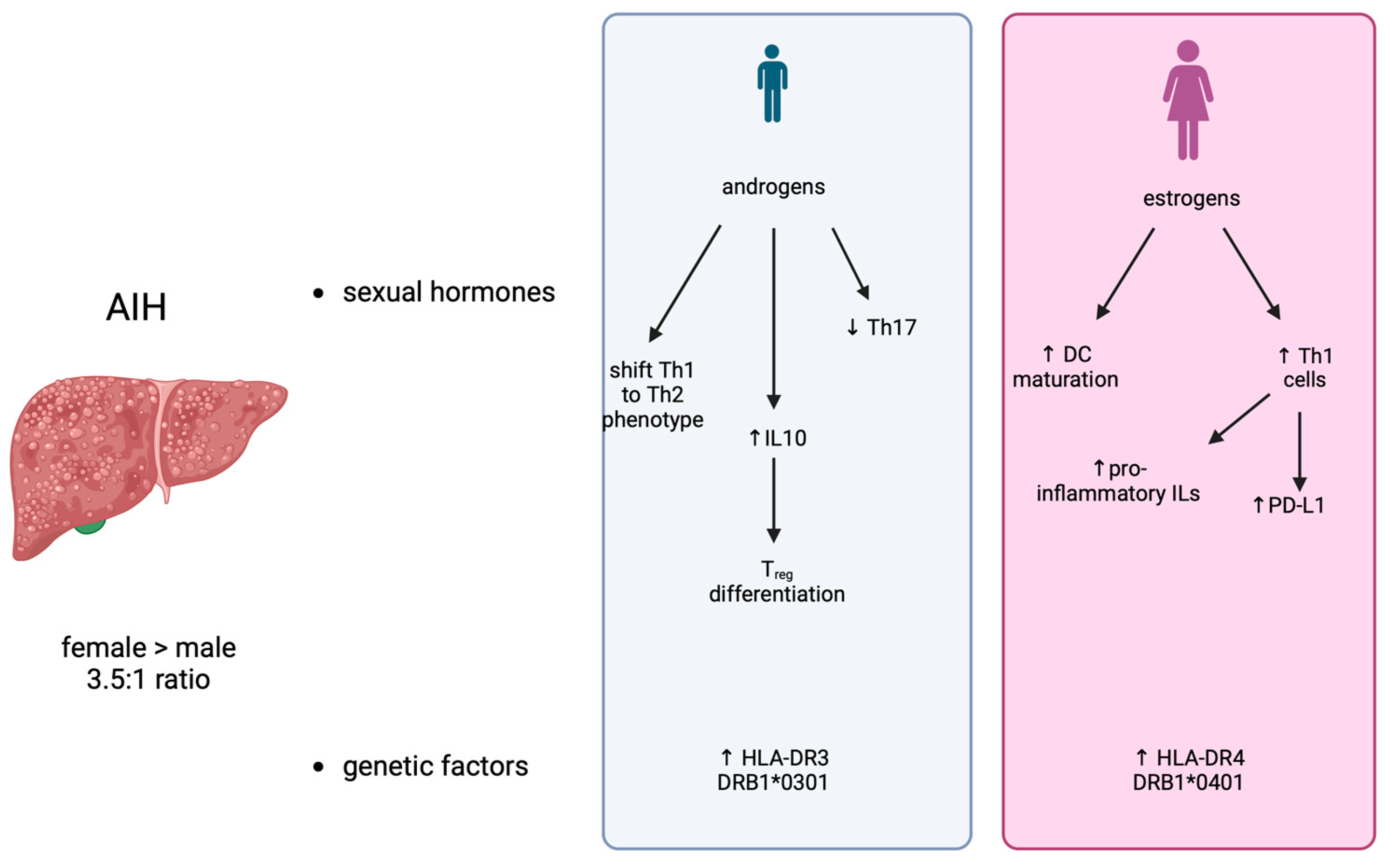
2. Autoimmune Hepatitis
2.1. Factors Responsible for Gender Differences
2.2. Clinical Course
3. Primary Biliary Cholangitis
3.1. Factors Responsible for Gender Differences
3.2. Clinical Course
4. Primary Sclerosing Cholangitis
Role of Gender in PSC
5. Overlap Syndromes
6. IgG4-Related Disease
7. Sex Disparities in Autoimmune Liver Diseases in Pediatrics
8. Conclusions and Future Perspectives
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Kardashian, A.; Serper, M.; Terrault, N.; Nephew, L.D. Health disparities in chronic liver disease. Hepatology 2023, 77, 1382–1403. [Google Scholar] [CrossRef] [PubMed]
- Castrucci, B.C.; Auerbach, J. Meeting Individual Social Needs Falls Short of Addressing Social Determinants of Health. Health Aff. Forefr. 2019, 77, 25–28. [Google Scholar]
- Ortona, E.; Delunardo, F.; Baggio, G.; Malorni, W. A sex and gender perspective in medicine: A new mandatory challenge for human health. Preface. Ann. Ist. Super. Sanita 2016, 52, 146–148. [Google Scholar] [CrossRef] [PubMed]
- Westergaard, D.; Moseley, P.; Sørup, F.K.H.; Baldi, P.; Brunak, S. Population-wide analysis of differences in disease progression patterns in men and women. Nat. Commun. 2019, 10, 666. [Google Scholar] [CrossRef]
- Sayaf, K.; Gabbia, D.; Russo, F.P.; De Martin, S. The Role of Sex in Acute and Chronic Liver Damage. Int. J. Mol. Sci. 2022, 23, 10654. [Google Scholar] [CrossRef]
- Sayaf, K.; Zanotto, I.; Gabbia, D.; Alberti, D.; Pasqual, G.; Zaramella, A.; Fantin, A.; De Martin, S.; Russo, F.P. Sex Drives Functional Changes in the Progression and Regression of Liver Fibrosis. Int. J. Mol. Sci. 2023, 24, 16452. [Google Scholar] [CrossRef]
- Baggio, G.; Corsini, A.; Floreani, A.; Giannini, S.; Zagonel, V. Gender medicine: A task for the third millennium. Clin. Chem. Lab. Med. CCLM 2013, 51, 713–727. [Google Scholar] [CrossRef]
- Manns, M.P.; Lohse, A.W.; Vergani, D. Autoimmune hepatitis—Update 2015. J. Hepatol. 2015, 62, S100–S111. [Google Scholar] [CrossRef]
- Grønbæk, L.; Vilstrup, H.; Jepsen, P. Autoimmune hepatitis in Denmark: Incidence, prevalence, prognosis, and causes of death. A nationwide registry-based cohort study. J. Hepatol. 2014, 60, 612–617. [Google Scholar] [CrossRef]
- Bittermann, T.; Lewis, J.D.; Levy, C.; Goldberg, D.S. Sociodemographic and geographic differences in the US epidemiology of autoimmune hepatitis with and without cirrhosis. Hepatology 2023, 77, 367–378. [Google Scholar] [CrossRef]
- Yuming, Z.; Ruqi, T.; Gershwin, M.E.; Xiong, M. Autoimmune Hepatitis. Clin. Liver Dis. 2024, 28, 15–35. [Google Scholar] [CrossRef] [PubMed]
- Castiella, A. Drug-induced autoimmune liver disease: A diagnostic dilemma of an increasingly reported disease. World J. Hepatol. 2014, 6, 160. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.; Wu, T.Y.; Cottagiri, M.; Nyandjo, M.; Njoku, D.B. Induction of Drug-Induced, Autoimmune Hepatitis in BALB/c Mice for the Study of Its Pathogenic Mechanisms. J. Vis. Exp. 2020, 159, 59174. [Google Scholar] [CrossRef]
- Cho, J.; Kim, L.; Li, Z.; Rose, N.R.; Talor, M.V.; Njoku, D.B. Sex bias in experimental immune-mediated, drug-induced liver injury in BALB/c mice: Suggested roles for Tregs, estrogen, and IL-6. PLoS ONE 2013, 8, e61186. [Google Scholar] [CrossRef] [PubMed]
- Schramm, C.; Herkel, J.; Beuers, U.; Kanzler, S.; Galle, P.R.; Lohse, A.W. Pregnancy in Autoimmune Hepatitis: Outcome and Risk Factors. Am. J. Gastroenterol. 2006, 101, 556–560. [Google Scholar] [CrossRef] [PubMed]
- Buchel, E.; Van Steenbergen, W.; Nevens, F.; Fevery, J. Improvement of Autoimmune Hepatitis During Pregnancy Followed by Flare-Up After Delivery. Am. J. Gastroenterol. 2002, 97, 3160–3165. [Google Scholar] [CrossRef] [PubMed]
- Heneghan, M.A. Management and outcome of pregnancy in autoimmune hepatitis. Gut 2001, 48, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Izumi, Y.; Kaneko, A.; Oku, K.; Kimura, M.; Tanaka, S.; Tada, H.; Tatsumi, K.; Takano, T.; Hidaka, Y.; Amino, N. Development of liver dysfunction after delivery is possibly due to postpartum autoimmune hepatitis. A report of three cases. J. Intern. Med. 2002, 252, 361–367. [Google Scholar] [CrossRef]
- Westbrook, R.H.; Yeoman, A.D.; Kriese, S.; Heneghan, M.A. Outcomes of pregnancy in women with autoimmune hepatitis. J. Autoimmun. 2012, 38, J239–J244. [Google Scholar] [CrossRef]
- Delpy, L.; Douin-Echinard, V.; Garidou, L.; Bruand, C.; Saoudi, A.; Guéry, J.-C. Estrogen Enhances Susceptibility to Experimental Autoimmune Myasthenia Gravis by Promoting Type 1-Polarized Immune Responses. J. Immunol. 2005, 175, 5050–5057. [Google Scholar] [CrossRef]
- Seillet, C.; Rouquié, N.; Foulon, E.; Douin-Echinard, V.; Krust, A.; Chambon, P.; Arnal, J.-F.; Guéry, J.-C.; Laffont, S. Estradiol Promotes Functional Responses in Inflammatory and Steady-State Dendritic Cells through Differential Requirement for Activation Function-1 of Estrogen Receptor α. J. Immunol. 2013, 190, 5459–5470. [Google Scholar] [CrossRef]
- Siracusa, M.C.; Overstreet, M.G.; Housseau, F.; Scott, A.L.; Klein, S.L. 17β-Estradiol Alters the Activity of Conventional and IFN-Producing Killer Dendritic Cells. J. Immunol. 2008, 180, 1423–1431. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.Y.; Buenafe, A.C.; Matejuk, A.; Ito, A.; Zamora, A.; Dwyer, J.; Vandenbark, A.A.; Offner, H. Estrogen inhibition of EAE involves effects on dendritic cell function. J. Neurosci. Res. 2002, 70, 238–248. [Google Scholar] [CrossRef] [PubMed]
- Papenfuss, T.L.; Powell, N.D.; McClain, M.A.; Bedarf, A.; Singh, A.; Gienapp, I.E.; Shawler, T.; Whitacre, C.C. Estriol Generates Tolerogenic Dendritic Cells In Vivo That Protect against Autoimmunity. J. Immunol. 2011, 186, 3346–3355. [Google Scholar] [CrossRef]
- Bebo, B.F.; Schuster, J.C.; Vandenbark, A.A.; Offner, H. Androgens alter the cytokine profile and reduce encephalitogenicity of myelin-reactive T cells. J. Immunol. 1999, 162, 35–40. [Google Scholar] [CrossRef]
- Schwinge, D.; Carambia, A.; Quaas, A.; Krech, T.; Wegscheid, C.; Tiegs, G.; Prinz, I.; Lohse, A.W.; Herkel, J.; Schramm, C. Testosterone Suppresses Hepatic Inflammation by the Downregulation of IL-17, CXCL-9, and CXCL-10 in a Mouse Model of Experimental Acute Cholangitis. J. Immunol. 2015, 194, 2522–2530. [Google Scholar] [CrossRef]
- Liva, S.M.; Voskuhl, R.R. Testosterone Acts Directly on CD4+ T Lymphocytes to Increase IL-10 Production. J. Immunol. 2001, 167, 2060–2067. [Google Scholar] [CrossRef]
- Henze, L.; Schwinge, D.; Schramm, C. The Effects of Androgens on T Cells: Clues to Female Predominance in Autoimmune Liver Diseases? Front. Immunol. 2020, 11, 1567. [Google Scholar] [CrossRef] [PubMed]
- Meester, I.; Manilla-Muñoz, E.; León-Cachón, R.B.R.; Paniagua-Frausto, G.A.; Carrión-Alvarez, D.; Ruiz-Rodríguez, C.O.; Rodríguez-Rangel, X.; García-Martínez, J.M. SeXY chromosomes and the immune system: Reflections after a comparative study. Biol. Sex Differ. 2020, 11, 3. [Google Scholar] [CrossRef]
- Liberal, R.; Grant, C.R.; Mieli-Vergani, G.; Vergani, D. Autoimmune hepatitis: A comprehensive review. J. Autoimmun. 2013, 41, 126–139. [Google Scholar] [CrossRef]
- Al-Chalabi, T.; Underhill, J.A.; Portmann, B.C.; McFarlane, I.G.; Heneghan, M.A. Impact of gender on the long-term outcome and survival of patients with autoimmune hepatitis. J. Hepatol. 2008, 48, 140–147. [Google Scholar] [CrossRef]
- Czaja, A.J.; Donaldson, P.T. Gender effects and synergisms with histocompatibility leukocyte antigens in type 1 autoimmune hepatitis. Am. J. Gastroenterol. 2002, 97, 2051–2057. [Google Scholar] [CrossRef] [PubMed]
- Czaja, A.J. Genetic Factors Affecting the Occurrence, Clinical Phenotype, and Outcome of Autoimmune Hepatitis. Clin. Gastroenterol. Hepatol. 2008, 6, 379–388. [Google Scholar] [CrossRef] [PubMed]
- Béland, K.; Lapierre, P.; Alvarez, F. Influence of genes, sex, age and environment on the onset of autoimmune hepatitis. World J. Gastroenterol. 2009, 15, 1025. [Google Scholar] [CrossRef] [PubMed]
- Vento, S.; Guella, L.; Mirandola, F.; Cainelli, F.; Di Perri, G.; Solbiati, M.; Concia, E.; Ferraro, T. Epstein-Barr virus as a trigger for autoimmune hepatitis in susceptible individuals. Lancet 1995, 346, 608–609. [Google Scholar] [CrossRef] [PubMed]
- Tiegs, G.; Hentschel, J.; Wendel, A. A T cell-dependent experimental liver injury in mice inducible by concanavalin A. J. Clin. Investig. 1992, 90, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.M.; O’Connor, A.M.; Hart, J.; Merel, N.H.; Te, H.S. Autoimmune hepatitis associated with the use of black cohosh: A case study. Menopause 2004, 11, 575–577. [Google Scholar] [CrossRef] [PubMed]
- Alla, V.; Abraham, J.; Siddiqui, J.; Raina, D.; Wu, G.Y.; Chalasani, N.P.; Bonkovsky, H.L. Autoimmune Hepatitis Triggered by Statins. J. Clin. Gastroenterol. 2006, 40, 757–761. [Google Scholar] [CrossRef] [PubMed]
- Czaja, A.J. Incorporating the Molecular Mimicry of Environmental Antigens into the Causality of Autoimmune Hepatitis. Dig. Dis. Sci. 2023, 68, 2824–2842. [Google Scholar] [CrossRef]
- Zhang, X.; Chen, B.; Zhao, L.; Li, H. The Gut Microbiota: Emerging Evidence in Autoimmune Diseases. Trends Mol. Med. 2020, 26, 862–873. [Google Scholar] [CrossRef]
- Rosser, E.C.; De Gruijter, N.M.; Matei, D.E. Mini-Review: Gut-Microbiota and the Sex-Bias in Autoimmunity—Lessons Learnt From Animal Models. Front. Med. 2022, 9, 910561. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Z.; Yang, L.; Chu, H. The Gut Microbiota: A Novel Player in Autoimmune Hepatitis. Front. Cell. Infect. Microbiol. 2022, 12, 947382. [Google Scholar] [CrossRef] [PubMed]
- Yuksel, M.; Wang, Y.; Tai, N.; Peng, J.; Guo, J.; Beland, K.; Lapierre, P.; David, C.; Alvarez, F.; Colle, I.; et al. A novel “humanized mouse” model for autoimmune hepatitis and the association of gut microbiota with liver inflammation. Hepatology 2015, 62, 1536–1550. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhu, N.; Su, X.; Gao, Y.; Yang, R. Gut-Microbiota-Derived Metabolites Maintain Gut and Systemic Immune Homeostasis. Cells 2023, 12, 793. [Google Scholar] [CrossRef] [PubMed]
- Terziroli Beretta-Piccoli, B.; Mieli-Vergani, G.; Vergani, D. HLA, gut microbiome and hepatic autoimmunity. Front. Immunol. 2022, 13, 980768. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Li, J.; Zhu, Y.; Chen, C.; Liu, J.; Gu, S.; Zheng, Y.; Li, Y. Causal effects of gut microbiome on autoimmune liver disease: A two-sample Mendelian randomization study. BMC Med. Genom. 2023, 16, 232. [Google Scholar] [CrossRef] [PubMed]
- Birn-Rydder, R.; Jensen, M.D.; Jepsen, P.; Grønbæk, L. Extrahepatic autoimmune diseases in autoimmune hepatitis: Effect on mortality. Liver Int. 2022, 42, 2466–2472. [Google Scholar] [CrossRef]
- Lee, D.U.; Kwon, J.; Koo, C.; Han, J.; Fan, G.H.; Jung, D.; Addonizio, E.A.; Chang, K.; Urrunaga, N.H. Clinical implications of gender and race in patients admitted with autoimmune hepatitis: Updated analysis of US hospitals. Frontline Gastroenterol. 2023, 14, 111–123. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.D.; Jepsen, P.; Vilstrup, H.; Grønbæk, L. Increased Cancer Risk in Autoimmune Hepatitis: A Danish Nationwide Cohort Study. Am. J. Gastroenterol. 2022, 117, 129–137. [Google Scholar] [CrossRef]
- Yan, L.-J.; Yao, S.-Y.; Meng, G.-X.; Liu, K.-X.; Li, H.-C.; Ding, Z.-N.; Dong, Z.-R.; Hong, J.-G.; Chen, Z.-Q.; Li, T. Sex and regional disparities in incidence of hepatocellular carcinoma in autoimmune hepatitis: A systematic review and meta-analysis. Hepatol. Int. 2021, 15, 1413–1420. [Google Scholar] [CrossRef]
- Orlando, R.; De Martin, S.; Andrighetto, L.; Floreani, M.; Palatini, P. Fluvoxamine pharmacokinetics in healthy elderly subjects and elderly patients with chronic heart failure. Br. J. Clin. Pharmacol. 2010, 69, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Palatini, P.; De Martin, S. Pharmacokinetic drug interactions in liver disease: An update. World J. Gastroenterol. 2016, 22, 1260–1278. [Google Scholar] [CrossRef] [PubMed]
- Hartl, J.; Miquel, R.; Zachou, K.; Wong, G.-W.; Asghar, A.; Pape, S.; Sebode, M.; Peiseler, M.; Zenouzi, R.; Ehlken, H.; et al. Features and outcome of AIH patients without elevation of IgG. JHEP Rep. 2020, 2, 100094. [Google Scholar] [CrossRef]
- Gabbia, D.; Dalla Pozza, A.; Albertoni, L.; Lazzari, R.; Zigiotto, G.; Carrara, M.; Baldo, V.; Baldovin, T.; Floreani, A.; De Martin, S. Pregnane X receptor and constitutive androstane receptor modulate differently CYP3A-mediated metabolism in early- and late-stage cholestasis. World J. Gastroenterol. 2017, 23, 7519–7530. [Google Scholar] [CrossRef] [PubMed]
- Levy, C.; Manns, M.; Hirschfield, G. New Treatment Paradigms in Primary Biliary Cholangitis. Clin. Gastroenterol. Hepatol. 2023, 21, 2076–2087. [Google Scholar] [CrossRef] [PubMed]
- Floreani, A.; Gabbia, D.; De Martin, S. Current Perspectives on the Molecular and Clinical Relationships between Primary Biliary Cholangitis and Hepatocellular Carcinoma. Int. J. Mol. Sci. 2024, 25, 2194. [Google Scholar] [CrossRef] [PubMed]
- Floreani, A.; Gabbia, D.; De Martin, S. Primary biliary cholangitis: Primary autoimmune disease or primary secretory defect. Expert Rev. Gastroenterol. Hepatol. 2023, 17, 863–870. [Google Scholar] [CrossRef]
- Boonstra, K.; Bokelaar, R.; Stadhouders, P.H.; Tuynman, H.A.; Poen, A.C.; van Nieuwkerk, K.M.; Witteman, E.M.; Hamann, D.; Witteman, B.J.; Beuers, U.; et al. Increased cancer risk in a large population-based cohort of patients with primary biliary cirrhosis: Follow-up for up to 36 years. Hepatol. Int. 2014, 8, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Li, J.; Haller, I.V.; Romanelli, R.J.; VanWormer, J.J.; Rodriguez, C.V.; Raebel, M.A.; Boscarino, J.A.; Schmidt, M.A.; Daida, Y.G.; et al. Factors Associated with Prevalence and Treatment of Primary Biliary Cholangitis in United States Health Systems. Clin. Gastroenterol. Hepatol. 2018, 16, 1333–1341.e6. [Google Scholar] [CrossRef]
- Hirschfield, G.M.; Beuers, U.; Corpechot, C.; Invernizzi, P.; Jones, D.; Marzioni, M.; Schramm, C. EASL Clinical Practice Guidelines: The diagnosis and management of patients with primary biliary cholangitis. J. Hepatol. 2017, 67, 145–172. [Google Scholar] [CrossRef]
- Quintero, O.L.; Amador-Patarroyo, M.J.; Montoya-Ortiz, G.; Rojas-Villarraga, A.; Anaya, J.-M. Autoimmune disease and gender: Plausible mechanisms for the female predominance of autoimmunity. J. Autoimmun. 2012, 38, J109–J119. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.; Zhu, B.; Qu, Y.; Zhang, W. Abnormal Expression of ERα in Cholangiocytes of Patients with Primary Biliary Cholangitis Mediated Intrahepatic Bile Duct Inflammation. Front. Immunol. 2019, 10, 2815. [Google Scholar] [CrossRef] [PubMed]
- Alvaro, D. Estrogens and the pathophysiology of the biliary tree. World J. Gastroenterol. 2006, 12, 3537. [Google Scholar] [CrossRef] [PubMed]
- Matalka, K.Z. The effect of estradiol, but not progesterone, on the production of cytokines in stimulated whole blood, is concentration-dependent. Neuro Endocrinol. Lett. 2003, 24, 185–191. [Google Scholar] [PubMed]
- Bae, H.R.; Leung, P.S.C.; Tsuneyama, K.; Valencia, J.C.; Hodge, D.L.; Kim, S.; Back, T.; Karwan, M.; Merchant, A.S.; Baba, N.; et al. Chronic expression of interferon-gamma leads to murine autoimmune cholangitis with a female predominance. Hepatology 2016, 64, 1189–1201. [Google Scholar] [CrossRef] [PubMed]
- Bae, H.R.; Hodge, D.L.; Yang, G.; Leung, P.S.C.; Chodisetti, S.B.; Valencia, J.C.; Sanford, M.; Fenimore, J.M.; Rahman, Z.S.M.; Tsuneyama, K.; et al. The interplay of type I and type II interferons in murine autoimmune cholangitis as a basis for sex-biased autoimmunity. Hepatology 2018, 67, 1408–1419. [Google Scholar] [CrossRef] [PubMed]
- Carbone, M.; Bonato, G.; Invernizzi, P. Female preponderance of primary biliary cholangitis is all about our understanding of its autoimmune nature. Hepatology 2018, 67, 1210–1212. [Google Scholar] [CrossRef] [PubMed]
- Alvaro, D.; Invernizzi, P.; Onori, P.; Franchitto, A.; De Santis, A.; Crosignani, A.; Sferra, R.; Ginanni-Corradini, S.; Grazia Mancino, M.; Maggioni, M.; et al. Estrogen receptors in cholangiocytes and the progression of primary biliary cirrhosis. J. Hepatol. 2004, 41, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Priester, S.; Onori, P.; Venter, J.; Renzi, A.; Franchitto, A.; Munshi, M.K.; Wise, C.; Dostal, D.E.; Marzioni, M.; et al. Castration inhibits biliary proliferation induced by bile duct obstruction: Novel role for the autocrine trophic effect of testosterone. Am. J. Physiol.-Gastrointest. Liver Physiol. 2011, 301, G981–G991. [Google Scholar] [CrossRef]
- Gerussi, A.; Lucà, M.; Cristoferi, L.; Ronca, V.; Mancuso, C.; Milani, C.; D’Amato, D.; O’Donnell, S.E.; Carbone, M.; Invernizzi, P. New Therapeutic Targets in Autoimmune Cholangiopathies. Front. Med. 2020, 7, 117. [Google Scholar] [CrossRef]
- Asselta, R.; Paraboschi, E.M.; Gerussi, A.; Cordell, H.J.; Mells, G.F.; Sandford, R.N.; Jones, D.E.; Nakamura, M.; Ueno, K.; Hitomi, Y.; et al. X Chromosome Contribution to the Genetic Architecture of Primary Biliary Cholangitis. Gastroenterology 2021, 160, 2483–2495.e26. [Google Scholar] [CrossRef] [PubMed]
- Mohr, A.; Atif, M.; Balderas, R.; Gorochov, G.; Miyara, M. The role of FOXP3+ regulatory T cells in human autoimmune and inflammatory diseases. Clin. Exp. Immunol. 2019, 197, 24–35. [Google Scholar] [CrossRef]
- Adejumo, A.C.; Akhtar, D.H.; Dennis, B.B.; Cholankeril, G.; Alayo, Q.; Ogundipe, O.A.; Kim, D.; Ahmed, A. Gender and Racial Differences in Hospitalizations for Primary Biliary Cholangitis in the USA. Dig. Dis. Sci. 2021, 66, 1461–1476. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.H.; Chiu, Y.L.; Lin, J.C.; Chen, H.W. New insights into sex differences in primary biliary cholangitis. Gender difference in primary biliary cholangitis. J. Pak. Med. Assoc. 2022, 72, 896–900. [Google Scholar] [CrossRef] [PubMed]
- Sy, A.M.; Ferreira, R.D.; John, B.V. Hepatocellular Carcinoma in Primary Biliary Cholangitis. Clin. Liver Dis. 2022, 26, 691–704. [Google Scholar] [CrossRef]
- Trivedi, P.J.; Lammers, W.J.; van Buuren, H.R.; Parés, A.; Floreani, A.; Janssen, H.L.A.; Invernizzi, P.; Battezzati, P.M.; Ponsioen, C.Y.; Corpechot, C.; et al. Stratification of hepatocellular carcinoma risk in primary biliary cirrhosis: A multicentre international study. Gut 2016, 65, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Floreani, A.; Gabbia, D.; De Martin, S. Obeticholic Acid for Primary Biliary Cholangitis. Biomedicines 2022, 10, 2464. [Google Scholar] [CrossRef]
- Kulik, L.; El-Serag, H.B. Epidemiology and Management of Hepatocellular Carcinoma. Gastroenterology 2019, 156, 477–491.e1. [Google Scholar] [CrossRef]
- Yeh, S.-H.; Chen, P.-J. Gender disparity of hepatocellular carcinoma: The roles of sex hormones. Oncology 2010, 78 (Suppl. 1), 172–179. [Google Scholar] [CrossRef]
- Floreani, A.; De Martin, S.; Ikeura, T.; Okazaki, K.; Gershwin, M.E. Gut microbial profiling as a therapeutic and diagnostic target for managing primary biliary cholangitis. Expert Opin. Orphan Drugs 2020, 8, 507–514. [Google Scholar] [CrossRef]
- Cazzagon, N.; Sarcognato, S.; Floreani, A.; Corrà, G.; De Martin, S.; Guzzardo, V.; Russo, F.P.; Guido, M. Cholangiocyte senescence in primary sclerosing cholangitis is associated with disease severity and prognosis. JHEP Rep. 2021, 3, 100286. [Google Scholar] [CrossRef] [PubMed]
- Hirschfield, G.M.; Karlsen, T.H.; Lindor, K.D.; Adams, D.H. Primary sclerosing cholangitis. Lancet 2013, 382, 1587–1599. [Google Scholar] [CrossRef] [PubMed]
- Barberio, B.; Massimi, D.; Cazzagon, N.; Zingone, F.; Ford, A.C.; Savarino, E.V. Prevalence of Primary Sclerosing Cholangitis in Patients With Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. Gastroenterology 2021, 161, 1865–1877. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Gao, X.; He, Z.; Jia, H.; Chen, M.; Wang, X.; Hong, L.; Cui, Y.; Wan, J. Prevalence of inflammatory bowel disease in patients with primary sclerosing cholangitis: A systematic review and meta-analysis. Liver Int. 2022, 42, 1814–1822. [Google Scholar] [CrossRef]
- Molodecky, N.A.; Kareemi, H.; Parab, R.; Barkema, H.W.; Quan, H.; Myers, R.P.; Kaplan, G.G. Incidence of primary sclerosing cholangitis: A systematic review and meta-analysis. Hepatology 2011, 53, 1590–1599. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, P.J.; Bowlus, C.L.; Yimam, K.K.; Razavi, H.; Estes, C. Epidemiology, Natural History, and Outcomes of Primary Sclerosing Cholangitis: A Systematic Review of Population-based Studies. Clin. Gastroenterol. Hepatol. 2022, 20, 1687–1700.e4. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, A. Current understanding of primary biliary cholangitis. Clin. Mol. Hepatol. 2021, 27, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Weismüller, T.J.; Trivedi, P.J.; Bergquist, A.; Imam, M.; Lenzen, H.; Ponsioen, C.Y.; Holm, K.; Gotthardt, D.; Färkkilä, M.A.; Marschall, H.-U.; et al. Patient Age, Sex, and Inflammatory Bowel Disease Phenotype Associate with Course of Primary Sclerosing Cholangitis. Gastroenterology 2017, 152, 1975–1984.e8. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, K.; Rupp, C.; Hov, J.R.; Steinebrunner, N.; Weiss, K.-H.; Stiehl, A.; Brune, M.; Schaefer, P.K.Y.; Schemmer, P.; Sauer, P.; et al. A Frequent PNPLA3 Variant Is a Sex Specific Disease Modifier in PSC Patients with Bile Duct Stenosis. PLoS ONE 2013, 8, e58734. [Google Scholar] [CrossRef]
- Rühlemann, M.; Liwinski, T.; Heinsen, F.-A.; Bang, C.; Zenouzi, R.; Kummen, M.; Thingholm, L.; Tempel, M.; Lieb, W.; Karlsen, T.; et al. Consistent alterations in faecal microbiomes of patients with primary sclerosing cholangitis independent of associated colitis. Aliment. Pharmacol. Ther. 2019, 50, 580–589. [Google Scholar] [CrossRef]
- Sabino, J.; Vieira-Silva, S.; Machiels, K.; Joossens, M.; Falony, G.; Ballet, V.; Ferrante, M.; Van Assche, G.; Van der Merwe, S.; Vermeire, S.; et al. Primary sclerosing cholangitis is characterised by intestinal dysbiosis independent from IBD. Gut 2016, 65, 1681–1689. [Google Scholar] [CrossRef] [PubMed]
- Liwinski, T.; Heinsen-Groth, F.; Rühlemann, M.; Zenouzi, R.; Kummen, M.; Hov, J.; Karlsen, T.; Bang, C.; Lohse, A.; Franke, A.; et al. The intestinal microbiota of patients with PSC are different from healthy controls and patients with ulcerative colitis across geographical regions. Z. Für Gastroenterol. 2018, 56, E2–E89. [Google Scholar] [CrossRef]
- Chazouillères, O.; Wendum, D.; Serfaty, L.; Montembault, S.; Rosmorduc, O.; Poupon, R. Primary biliary cirrhosis-autoimmune hepatitis overlap syndrome: Clinical features and response to therapy: Primary Biliary Cirrhosis-Autoimmune Hepatitis Overlap Syndrome: Clinical Features and Response to Therapy. Hepatology 1998, 28, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Yang, Z.; Zhong, R. Primary biliary cirrhosis and cancer risk: A systematic review and meta-analysis. Hepatology 2012, 56, 1409–1417. [Google Scholar] [CrossRef] [PubMed]
- Freedman, B.L.; Danford, C.J.; Patwardhan, V.; Bonder, A. Treatment of Overlap Syndromes in Autoimmune Liver Disease: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 1449. [Google Scholar] [CrossRef] [PubMed]
- Deneau, M.R.; El-Matary, W.; Valentino, P.L.; Abdou, R.; Alqoaer, K.; Amin, M.; Amir, A.Z.; Auth, M.; Bazerbachi, F.; Broderick, A.; et al. The natural history of primary sclerosing cholangitis in 781 children: A multicenter, international collaboration. Hepatology 2017, 66, 518–527. [Google Scholar] [CrossRef] [PubMed]
- Gregorio, G. Autoimmune hepatitis/sclerosing cholangitis overlap syndrome in childhood: A 16-year prospective study. Hepatology 2001, 33, 544–553. [Google Scholar] [CrossRef] [PubMed]
- Ricciuto, A.; Kamath, B.M.; Hirschfield, G.M.; Trivedi, P.J. Primary sclerosing cholangitis and overlap features of autoimmune hepatitis: A coming of age or an age-ist problem? J. Hepatol. 2023, 79, 567–575. [Google Scholar] [CrossRef] [PubMed]
- Lanzillotta, M.; Mancuso, G.; Della-Torre, E. Advances in the diagnosis and management of IgG4 related disease. BMJ 2020, 369, m1067. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, P.; Zhang, X.; Lin, W.; Tang, H.; Li, J.; Wang, M.; Liu, X.; Fei, Y.; Chen, H.; et al. Sex disparities in clinical characteristics and prognosis of immunoglobulin G4-related disease: A prospective study of 403 patients. Rheumatol. Oxf. Engl. 2019, 58, 820–830. [Google Scholar] [CrossRef]
- Karim, F.; Loeffen, J.; Bramer, W.; Westenberg, L.; Verdijk, R.; Van Hagen, M.; Van Laar, J. IgG4-related disease: A systematic review of this unrecognized disease in pediatrics. Pediatr. Rheumatol. 2016, 14, 18. [Google Scholar] [CrossRef]
- Martín-Nares, E.; Baenas, D.F.; Cuellar Gutiérrez, M.C.; Hernández-Molina, G.; Ortiz, A.C.; Neira, O.; Gutiérrez, M.A.; Calvo, R.; Saad, E.J.; Elgueta Pinochet, S.; et al. Clinical and Serological Features in Latin American IgG4-Related Disease Patients Differ According to Sex, Ethnicity, and Clinical Phenotype. JCR J. Clin. Rheumatol. 2022, 28, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Kersten, R.; Trampert, D.C.; Herta, T.; Hubers, L.M.; Maillette De Buy Wenniger, L.J.; Verheij, J.; Van De Graaf, S.F.J.; Beuers, U. IgG4-related cholangitis—A mimicker of fibrosing and malignant cholangiopathies. J. Hepatol. 2023, 79, 1502–1523. [Google Scholar] [CrossRef]
- Sokollik, C.; McLin, V.A.; Vergani, D.; Terziroli Beretta-Piccoli, B.; Mieli-Vergani, G. Juvenile autoimmune hepatitis: A comprehensive review. J. Autoimmun. 2018, 95, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Afaa, T.J.; Amegan-Aho, K.H.; Dono, M.T.; Odei, E.; Awuku, Y.A. Clinical characteristics of paediatric autoimmune hepatitis at a referral hospital in Sub Saharan Africa. PLoS ONE 2020, 15, e0239964. [Google Scholar] [CrossRef] [PubMed]
- Haghighat, M.; Mardani, S.; Dehghani, S.M.; Javaherizadeh, H. Clinical and laboratory data in pediatric autoimmune hepatitis: Study from referral center in Iran. Rev. Gastroenterol. Peru Organo Of. Soc. Gastroenterol. Peru 2020, 40, 149–154. [Google Scholar] [CrossRef]
- Saadah, O.I.; Khayat, A.; Alsufyani, H.A.; Bin-Taleb, Y. Paediatric autoimmune liver diseases: A descriptive study of patients from Saudi Arabia. Arab J. Gastroenterol. 2021, 22, 146–150. [Google Scholar] [CrossRef]
- Mogahed, E.; El-Karaksy, H.; Zaki, H.; Abdullatif, H. Autoimmune hepatitis in Egyptian children: A single center experience. Int. J. Immunopathol. Pharmacol. 2022, 36, 205873842110732. [Google Scholar] [CrossRef] [PubMed]
- Sutton, H.; Tayler, R.; Chalmers, I.; Cowieson, J.; Fraser, K.; Henderson, P.; Hansen, R. The Epidemiology of Pediatric Autoimmune Hepatitis in Scotland: A National Cohort Study. JPGN Rep. 2022, 3, e223. [Google Scholar] [CrossRef]
- Ludz, C.; Stirnimann, G.; Semela, D.; Mertens, J.; Kremer, A.E.; Filipowicz Sinnreich, M.; Sokollik, C.; Bernsmeier, C.; Bresson-Hadni, S.; McLin, V.; et al. Epidemiology, clinical features and management of autoimmune hepatitis in Switzerland: A retrospective and prospective cohort study. Swiss Med. Wkly. 2023, 153, 40102. [Google Scholar] [CrossRef]
- Altamimi, E.; Al Omari, D.; Obeidat, H.; Barham, K. Retrospective, single-center analysis of autoimmune hepatitis in Jordanian children: Clinical features, treatments, and outcomes. BMC Pediatr. 2024, 24, 102. [Google Scholar] [CrossRef] [PubMed]
- Warner, S.; Rajanayagam, J.; Russell, E.; Lloyd, C.; Ferguson, J.; Kelly, D.A.; Hirschfield, G.M. Biliary disease progression in childhood onset autoimmune liver disease: A 30-year follow-up into adulthood. JHEP Rep. 2024, 6, 100901. [Google Scholar] [CrossRef] [PubMed]
- Maggiore, G.; Bernard, O.; Mosca, A.; Ballot, E.; Johanet, C.; Jacquemin, E. Long-term outcomes of patients with type 1 or 2 autoimmune hepatitis presenting in childhood. J. Hepatol. 2023, 78, 979–988. [Google Scholar] [CrossRef] [PubMed]
- Dahlan, Y.; Smith, L.; Simmonds, D.; Jewell, L.D.; Wanless, I.; Heathcote, E.J.; Bain, V.G. Pediatric-onset primary biliary cirrhosis. Gastroenterology 2003, 125, 1476–1479. [Google Scholar] [CrossRef] [PubMed]
- Floreani, A.; Ostuni, P.A.; Ferrara, F.; Guido, M. Primary biliary cirrhosis: When and why does the disease develop? Dig. Liver Dis. 2006, 38, 272–275. [Google Scholar] [CrossRef]
- Invernizzi, P.; Alessio, M.G.; Smyk, D.S.; Lleo, A.; Sonzogni, A.; Fabris, L.; Candusso, M.; Bogdanos, D.P.; Iorio, R.; Torre, G. Autoimmune hepatitis type 2 associated with an unexpected and transient presence of primary biliary cirrhosis-specific antimitochondrial antibodies: A case study and review of the literature. BMC Gastroenterol. 2012, 12, 92. [Google Scholar] [CrossRef]
- Ullah, K.; Uddin, S.; Dogar, A.W.; Jan, Z.U.; Abbas, S.H. Primary biliary cirrhosis in early childhood—A rare case report. Int. J. Surg. Case Rep. 2021, 85, 106215. [Google Scholar] [CrossRef] [PubMed]
- Mieli-Vergani, G.; Vergani, D. Unique features of primary sclerosing cholangitis in children. Curr. Opin. Gastroenterol. 2010, 26, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Mieli-Vergani, G.; Vergani, D. Sclerosing Cholangitis in Children and Adolescents. Clin. Liver Dis. 2016, 20, 99–111. [Google Scholar] [CrossRef]
- Di Giorgio, A.; Vergani, D.; Mieli-Vergani, G. Cutting edge issues in juvenile sclerosing cholangitis. Dig. Liver Dis. 2022, 54, 417–427. [Google Scholar] [CrossRef]
- Terziroli Beretta-Piccoli, B.; Vergani, D.; Mieli-Vergani, G. Autoimmune sclerosing cholangitis: Evidence and open questions. J. Autoimmun. 2018, 95, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Bittencourt, P.L.; Goldberg, A.C.; Cançado, E.L.R.; Porta, G.; Carrilho, F.J.; Farias, A.Q.; Palacios, S.A.; Chiarella, J.M.; Abrantes-Lemos, C.P.; Baggio, V.L.; et al. Genetic Heterogeneity in Susceptibility to Autoimmune Hepatitis Types 1 and 2. Am. J. Gastroenterol. 1999, 94, 1906–1913. [Google Scholar] [CrossRef] [PubMed]


| Autoimmune Disease | Risk Factors | Results | Refs. |
|---|---|---|---|
| AIH | Increased IL-4 activated CD4+ T cells | Female BALB/C mice develop a more severe drug-induced AIH Tregs confer protection against drug-induced autoimmune hepatitis | [13,14] |
| Estrogens | Estrogens promote DC maturation, leading to an increase in Th1 cells activity, increased production of proinflammatory ILs, Estrogens upregulate the expression of checkpoint inhibitors, e.g., PD-L1 | [20,21,22,23,24] | |
| Androgens | Androgens may influence the pathogenesis of AIH by shifting the Th-1 to the Th-2 phenotype, reducing hepatic Th-17 and increasing IL-10 secretion, which drives Treg differentiation | [25,26,27,28] | |
| Pregnancy | Pregnancy increases risk of fetal and maternal complications and flares in AIH activity after delivery | [15,16,17] | |
| HLA-DR3 | Increased expression of HLA-DR3 (DRB1*0301) in male AIH patients | [31] | |
| HLA-DR4 | Increased HLA-DR4 (DRB1*0401) in female AIH patients | [32] | |
| PBC | Estrogens | ERα and Erβ modulate cholangiocyte response to damage, activating intracellular cascades involving ERK1/2 and PI3-kinase/AKT Estrogens stimulate the secretion of different growth factors in proliferating cholangiopathies and shift Th cells from Th1 to the Th2 phenotype Sexual hormone regulation of TLRs affect type 1 IFN that may impact on PBC progression Estrogens exert a homeostatic positive effect on cholangiocytes | [3,62,63,64,67] |
| Androgens | Testosterone stimulates AR proliferation cholangiocytes in a rodent model of cholestasis | [69] | |
| Inactivation of X chromosome | Female-specific heterogeneous population of cells with biallelic expression of some X-linked genes with a locus in which there is a super-enhancer targeting genes, e.g., FOXP3, affect Tregs and are critical for the maintenance of immune tolerance | [71,72] | |
| PSC | I148M variant polymorphism | Male carriers of the I148M variant showed significant reduced actuarial survival free of liver transplantation data | [89] |
| Country (Ref.) | Type | N. | Female % | Acute Onset | Age (Mean or Median Years) | Mortality |
|---|---|---|---|---|---|---|
| Ghana [105] | Retrospective | 13 | 61.5% | 15.7% | 10 (5–13) | 28.5% |
| Iran [106] | Retrospective | 86 | 66.27% | - | 9.1 ± 4.36 | 10.5% |
| Saudi Arabia [107] | Cross-sectional | 25 | 56% | 16% | 9.4 ± 4.2 | 0% |
| Egypt [108] | Retrospective | 34 | 64.7% | 51% | 8 ± 3 | 2.9% |
| Scotland [109] | Prospective | 30 | 64% | 44.4% | 11.4 (1–15.9) | 0% |
| Switzerland [110] | Retro- and prospective | 30 | 53% | - | 12.5 (8–15) | 0% |
| Jordania [111] | Retrospective | 16 | 75% | 31.3% | 9.4 ± 4.13 | 18.8% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Floreani, A.; Gabbia, D.; De Martin, S. Are Gender Differences Important for Autoimmune Liver Diseases? Life 2024, 14, 500. https://doi.org/10.3390/life14040500
Floreani A, Gabbia D, De Martin S. Are Gender Differences Important for Autoimmune Liver Diseases? Life. 2024; 14(4):500. https://doi.org/10.3390/life14040500
Chicago/Turabian StyleFloreani, Annarosa, Daniela Gabbia, and Sara De Martin. 2024. "Are Gender Differences Important for Autoimmune Liver Diseases?" Life 14, no. 4: 500. https://doi.org/10.3390/life14040500
APA StyleFloreani, A., Gabbia, D., & De Martin, S. (2024). Are Gender Differences Important for Autoimmune Liver Diseases? Life, 14(4), 500. https://doi.org/10.3390/life14040500







