The Impact of Metabolic Health and Obesity on Liver Transplant Candidates and Recipients
Abstract
:1. Introduction
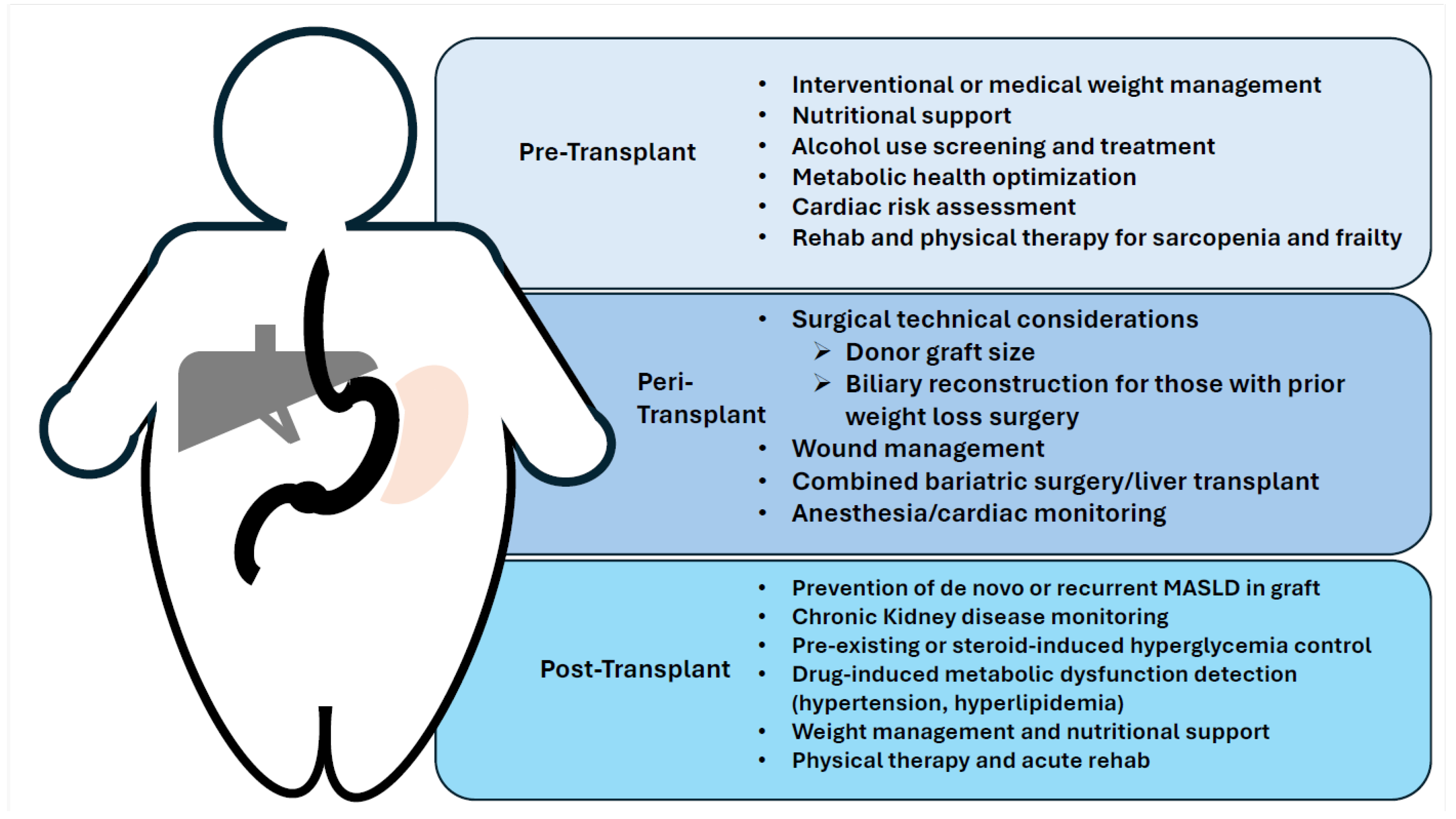
2. Liver Transplant Evaluation and Pre-Transplant Management
2.1. Cardiac Risk Assessment
2.2. Evaluation of Renal Disease
2.3. Sarcopenic Obesity and Frailty
2.4. Hepatocellular Carcinoma
3. Concurrent Alcohol Use in Patients with Obesity and Poor Metabolic Health
3.1. Obesity and Metabolic Health Management
3.2. Nutrition
3.3. Medical Obesity Management
3.4. Medical Management of Other Metabolic Health Factors
4. Interventional Obesity Management: Bariatric Surgery and Endobariatric Procedures
5. Living Donor Liver Transplantation
6. Surgical Considerations for Liver Transplantation in Patients with Obesity and Poor Metabolic Health
7. Simultaneous Bariatric Surgery and Liver Transplantation
8. Post-Liver Transplant Management of Patients with Poor Metabolic Health
8.1. Post-Liver Transplant Morbidity and Mortality
8.2. Immunosuppression and Poor Metabolic Health
8.3. Chronic Kidney Disease
8.4. Recurrent MASLD in the Liver Allograft
9. Conclusions and Future Directions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| Chronic liver disease | CLD |
| United States | US |
| Metabolic dysfunction-associated steatotic liver disease | MASLD |
| Metabolic dysfunction-associated steatohepatitis | MASH |
| Liver transplantation | LT |
| Cardiovascular | CV |
| Coronary artery disease | CAD |
| Chronic kidney disease | CKD |
| Steatotic liver disease | SLD |
| Metabolic dysfunction- and alcohol-associated liver disease | MetALD |
| Alcohol use disorder | AUD |
| Alcohol-associated liver disease | ALD |
| Roux-en-Y gastric bypass | RYGB |
| American Association for the Study of Liver Diseases | AASLD |
| Body mass index | BMI |
| Glucagon-like peptide-1 receptor agonists | GLP-1 RAs |
| Sleeve gastrectomy | SG |
| Living donor liver transplants | LDLT |
| Graft–recipient weight ratio | GRWR |
| Model for End-Stage Liver Disease | MELD |
| Portal vein thrombosis | PVT |
| Calcineurin inhibitors | CNI |
References
- Moon, A.M.; Singal, A.G.; Tapper, E.B. Contemporary Epidemiology of Chronic Liver Disease and Cirrhosis. Clin. Gastroenterol. Hepatol. 2020, 18, 2650–2666. [Google Scholar] [CrossRef] [PubMed]
- Powell, E.E.; Wong, V.W.; Rinella, M. Non-alcoholic fatty liver disease. Lancet 2021, 397, 2212–2224. [Google Scholar] [CrossRef] [PubMed]
- Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z. The metabolic syndrome. Lancet 2005, 365, 1415–1428. [Google Scholar] [CrossRef] [PubMed]
- Rinella, M.E.; Lazarus, J.V.; Ratziu, V.; Francque, S.M.; Sanyal, A.J.; Kanwal, F.; Romero, D.; Abdelmalek, M.F.; Anstee, Q.M.; Arab, J.P.; et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J. Hepatol. 2023, 79, 1542–1556. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, M.; Schrode, K.M.; Pan, D.; Kermah, D.; Puri, V.; Zarrinpar, A.; Elisha, D.; Najjar, S.M.; Friedman, T.C. Sex-Specific Differences in the Association Between Race/Ethnicity and NAFLD Among US Population. Front. Med. 2021, 8, 795421. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.; Anstee, Q.M.; Marietti, M.; Hardy, T.; Henry, L.; Eslam, M.; George, J.; Bugianesi, E. Global burden of NAFLD and NASH: Trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Burra, P.; Becchetti, C.; Germani, G. NAFLD and liver transplantation: Disease burden, current management and future challenges. JHEP Rep. 2020, 2, 100192. [Google Scholar] [CrossRef] [PubMed]
- Scientific Registry of Transplant Recipients. 2021 SRTR Annual Report. Available online: https://srtr.transplant.hrsa.gov/annual_reports/2021_ADR_Preview.aspx (accessed on 12 December 2023).
- Duell, P.B.; Welty, F.K.; Miller, M.; Chait, A.; Hammond, G.; Ahmad, Z.; Cohen, D.E.; Horton, J.D.; Pressman, G.S.; Toth, P.P.; et al. Nonalcoholic Fatty Liver Disease and Cardiovascular Risk: A Scientific Statement from the American Heart Association. Arterioscler. Thromb. Vasc. Biol. 2022, 42, e168–e185. [Google Scholar] [CrossRef] [PubMed]
- Barman, P.M.; VanWagner, L.B. Cardiac Risk Assessment in Liver Transplant Candidates: Current Controversies and Future Directions. Hepatology 2021, 73, 2564–2576. [Google Scholar] [CrossRef]
- Targher, G.; Byrne, C.D.; Lonardo, A.; Zoppini, G.; Barbui, C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: A meta-analysis. J. Hepatol. 2016, 65, 589–600. [Google Scholar] [CrossRef]
- Byrne, C.D.; Targher, G. Ectopic fat, insulin resistance, and nonalcoholic fatty liver disease: Implications for cardiovascular disease. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 1155–1161. [Google Scholar] [CrossRef] [PubMed]
- Vanwagner, L.B.; Bhave, M.; Te, H.S.; Feinglass, J.; Alvarez, L.; Rinella, M.E. Patients transplanted for nonalcoholic steatohepatitis are at increased risk for postoperative cardiovascular events. Hepatology 2012, 56, 1741–1750. [Google Scholar] [CrossRef]
- Satapathy, S.K.; Vanatta, J.M.; Helmick, R.A.; Flowers, A.; Kedia, S.K.; Jiang, Y.; Ali, B.; Eason, J.; Nair, S.P.; Ibebuogu, U.N. Outcome of Liver Transplant Recipients with Revascularized Coronary Artery Disease: A Comparative Analysis with and without Cardiovascular Risk Factors. Transplantation 2017, 101, 793–803. [Google Scholar] [CrossRef]
- Martin, P.; DiMartini, A.; Feng, S.; Brown, R., Jr.; Fallon, M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology 2014, 59, 1144–1165. [Google Scholar] [CrossRef] [PubMed]
- Gopaldas, R.R.; Chu, D.; Cornwell, L.D.; Dao, T.K.; LeMaire, S.A.; Coselli, J.S.; Bakaeen, F.G. Cirrhosis as a moderator of outcomes in coronary artery bypass grafting and off-pump coronary artery bypass operations: A 12-year population-based study. Ann. Thorac. Surg. 2013, 96, 1310–1315. [Google Scholar] [CrossRef] [PubMed]
- Yasui, K.; Sumida, Y.; Mori, Y.; Mitsuyoshi, H.; Minami, M.; Itoh, Y.; Kanemasa, K.; Matsubara, H.; Okanoue, T.; Yoshikawa, T. Nonalcoholic steatohepatitis and increased risk of chronic kidney disease. Metabolism 2011, 60, 735–739. [Google Scholar] [CrossRef] [PubMed]
- Musso, G.; Gambino, R.; Tabibian, J.H.; Ekstedt, M.; Kechagias, S.; Hamaguchi, M.; Hultcrantz, R.; Hagstrom, H.; Yoon, S.K.; Charatcharoenwitthaya, P.; et al. Association of non-alcoholic fatty liver disease with chronic kidney disease: A systematic review and meta-analysis. PLoS Med. 2014, 11, e1001680. [Google Scholar] [CrossRef]
- Pawarode, A.; Fine, D.M.; Thuluvath, P.J. Independent risk factors and natural history of renal dysfunction in liver transplant recipients. Liver Transpl. 2003, 9, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Singal, A.K.; Hasanin, M.; Kaif, M.; Wiesner, R.; Kuo, Y.F. Nonalcoholic Steatohepatitis is the Most Rapidly Growing Indication for Simultaneous Liver Kidney Transplantation in the United States. Transplantation 2016, 100, 607–612. [Google Scholar] [CrossRef]
- Torre, A.; Aguirre-Valadez, J.M.; Arreola-Guerra, J.M.; Garcia-Flores, O.R.; Garcia-Juarez, I.; Cruz-Rivera, C.; Correa-Rotter, R.; Nino-Cruz, J.A. Creatinine versus Cystatin C for Estimating GFR in Patients with Liver Cirrhosis. Am. J. Kidney Dis. 2016, 67, 342–344. [Google Scholar] [CrossRef]
- Donini, L.M.; Busetto, L.; Bischoff, S.C.; Cederholm, T.; Ballesteros-Pomar, M.D.; Batsis, J.A.; Bauer, J.M.; Boirie, Y.; Cruz-Jentoft, A.J.; Dicker, D.; et al. Definition and Diagnostic Criteria for Sarcopenic Obesity: ESPEN and EASO Consensus Statement. Obes. Facts 2022, 15, 321–335. [Google Scholar] [CrossRef] [PubMed]
- Batsis, J.A.; Mackenzie, T.A.; Lopez-Jimenez, F.; Bartels, S.J. Sarcopenia, sarcopenic obesity, and functional impairments in older adults: National Health and Nutrition Examination Surveys 1999–2004. Nutr. Res. 2015, 35, 1031–1039. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.C.; Tandon, P.; Bernal, W.; Tapper, E.B.; Ekong, U.; Dasarathy, S.; Carey, E.J. Malnutrition, Frailty, and Sarcopenia in Patients with Cirrhosis: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 2021, 74, 1611–1644. [Google Scholar] [CrossRef]
- Chun, H.S.; Lee, M.; Lee, H.A.; Lee, S.; Kim, S.; Jung, Y.J.; Lee, C.; Kim, H.; Lee, H.A.; Kim, H.Y.; et al. Risk Stratification for Sarcopenic Obesity in Subjects with Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2023, 21, 2298–2307.e18. [Google Scholar] [CrossRef] [PubMed]
- Knoedler, S.; Schliermann, R.; Knoedler, L.; Wu, M.; Hansen, F.J.; Matar, D.Y.; Obed, D.; Vervoort, D.; Haug, V.; Hundeshagen, G.; et al. Impact of sarcopenia on outcomes in surgical patients: A systematic review and meta-analysis. Int. J. Surg. 2023, 109, 4238–4262. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.J.; Wang, L.C.; Kuo, H.T.; Fang, Y.C.; Lee, H.F. Significant effects of late evening snack on liver functions in patients with liver cirrhosis: A meta-analysis of randomized controlled trials. J. Gastroenterol. Hepatol. 2019, 34, 1143–1152. [Google Scholar] [CrossRef] [PubMed]
- Meena, B.L.; Taneja, S.; Tandon, P.; Sahni, N.; Soundararajan, R.; Gorsi, U.; De, A.; Verma, N.; Premkumar, M.; Duseja, A.; et al. Home-based intensive nutrition therapy improves frailty and sarcopenia in patients with decompensated cirrhosis: A randomized clinical trial. J. Gastroenterol. Hepatol. 2023, 38, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.C.; Covinsky, K.E.; Dodge, J.L.; Boscardin, W.J.; Segev, D.L.; Roberts, J.P.; Feng, S. Development of a novel frailty index to predict mortality in patients with end-stage liver disease. Hepatology 2017, 66, 564–574. [Google Scholar] [CrossRef]
- Lai, J.C.; Dodge, J.L.; Kappus, M.R.; Dunn, M.A.; Volk, M.L.; Duarte-Rojo, A.; Ganger, D.R.; Rahimi, R.S.; McCulloch, C.E.; Haugen, C.E.; et al. Changes in frailty are associated with waitlist mortality in patients with cirrhosis. J. Hepatol. 2020, 73, 575–581. [Google Scholar] [CrossRef]
- Duarte-Rojo, A.; Bloomer, P.M.; Rogers, R.J.; Hassan, M.A.; Dunn, M.A.; Tevar, A.D.; Vivis, S.L.; Bataller, R.; Hughes, C.B.; Ferrando, A.A.; et al. Introducing EL-FIT (Exercise and Liver FITness): A Smartphone App to Prehabilitate and Monitor Liver Transplant Candidates. Liver Transpl. 2021, 27, 502–512. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Koenig, A.B.; Abdelatif, D.; Fazel, Y.; Henry, L.; Wymer, M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016, 64, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Mittal, S.; El-Serag, H.B.; Sada, Y.H.; Kanwal, F.; Duan, Z.; Temple, S.; May, S.B.; Kramer, J.R.; Richardson, P.A.; Davila, J.A. Hepatocellular Carcinoma in the Absence of Cirrhosis in United States Veterans is Associated with Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2016, 14, 124–131.e1. [Google Scholar] [CrossRef] [PubMed]
- Piscaglia, F.; Svegliati-Baroni, G.; Barchetti, A.; Pecorelli, A.; Marinelli, S.; Tiribelli, C.; Bellentani, S.; Group, H.-N.I.S. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: A multicenter prospective study. Hepatology 2016, 63, 827–838. [Google Scholar] [CrossRef]
- Kanwal, F.; Kramer, J.R.; Mapakshi, S.; Natarajan, Y.; Chayanupatkul, M.; Richardson, P.A.; Li, L.; Desiderio, R.; Thrift, A.P.; Asch, S.M.; et al. Risk of Hepatocellular Cancer in Patients with Non-Alcoholic Fatty Liver Disease. Gastroenterology 2018, 155, 1828–1837.e2. [Google Scholar] [CrossRef] [PubMed]
- Ertle, J.; Dechene, A.; Sowa, J.P.; Penndorf, V.; Herzer, K.; Kaiser, G.; Schlaak, J.F.; Gerken, G.; Syn, W.K.; Canbay, A. Non-alcoholic fatty liver disease progresses to hepatocellular carcinoma in the absence of apparent cirrhosis. Int. J. Cancer 2011, 128, 2436–2443. [Google Scholar] [CrossRef] [PubMed]
- Yasui, K.; Hashimoto, E.; Komorizono, Y.; Koike, K.; Arii, S.; Imai, Y.; Shima, T.; Kanbara, Y.; Saibara, T.; Mori, T.; et al. Characteristics of patients with nonalcoholic steatohepatitis who develop hepatocellular carcinoma. Clin. Gastroenterol. Hepatol. 2011, 9, 428–433; quiz e450. [Google Scholar] [CrossRef] [PubMed]
- Saunders, D.; Seidel, D.; Allison, M.; Lyratzopoulos, G. Systematic review: The association between obesity and hepatocellular carcinoma—Epidemiological evidence. Aliment. Pharmacol. Ther. 2010, 31, 1051–1063. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.M.; Abdel-Wahab, R.; Kaseb, A.; Shalaby, A.; Phan, A.T.; El-Serag, H.B.; Hawk, E.; Morris, J.; Singh Raghav, K.P.; Lee, J.S.; et al. Obesity Early in Adulthood Increases Risk but Does Not Affect Outcomes of Hepatocellular Carcinoma. Gastroenterology 2015, 149, 119–129. [Google Scholar] [CrossRef]
- Schlesinger, S.; Aleksandrova, K.; Pischon, T.; Jenab, M.; Fedirko, V.; Trepo, E.; Overvad, K.; Roswall, N.; Tjonneland, A.; Boutron-Ruault, M.C.; et al. Diabetes mellitus, insulin treatment, diabetes duration, and risk of biliary tract cancer and hepatocellular carcinoma in a European cohort. Ann. Oncol. 2013, 24, 2449–2455. [Google Scholar] [CrossRef]
- Wang, C.; Wang, X.; Gong, G.; Ben, Q.; Qiu, W.; Chen, Y.; Li, G.; Wang, L. Increased risk of hepatocellular carcinoma in patients with diabetes mellitus: A systematic review and meta-analysis of cohort studies. Int. J. Cancer 2012, 130, 1639–1648. [Google Scholar] [CrossRef]
- Karagozian, R.; Baker, E.; Houranieh, A.; Leavitt, D.; Baffy, G. Risk profile of hepatocellular carcinoma reveals dichotomy among US veterans. J. Gastrointest. Cancer 2013, 44, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Esfeh, J.M.; Hajifathalian, K.; Ansari-Gilani, K. Sensitivity of ultrasound in detecting hepatocellular carcinoma in obese patients compared to explant pathology as the gold standard. Clin. Mol. Hepatol. 2020, 26, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.Q.; Fowler, K.J.; Liau, J.; Cunha, G.M.; Louie, A.L.; An, J.Y.; Bettencourt, R.; Jung, J.; Gitto, Z.; Hernandez, C.; et al. Comparative efficacy of an optimal exam between ultrasound versus abbreviated MRI for HCC screening in NAFLD cirrhosis: A prospective study. Aliment. Pharmacol. Ther. 2022, 55, 820–827. [Google Scholar] [CrossRef] [PubMed]
- Charlton, M.R.; Burns, J.M.; Pedersen, R.A.; Watt, K.D.; Heimbach, J.K.; Dierkhising, R.A. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology 2011, 141, 1249–1253. [Google Scholar] [CrossRef]
- Haldar, D.; Kern, B.; Hodson, J.; Armstrong, M.J.; Adam, R.; Berlakovich, G.; Fritz, J.; Feurstein, B.; Popp, W.; Karam, V.; et al. Outcomes of liver transplantation for non-alcoholic steatohepatitis: A European Liver Transplant Registry study. J. Hepatol. 2019, 71, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.J.; Cheung, R.; Ahmed, A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S. Hepatology 2014, 59, 2188–2195. [Google Scholar] [CrossRef] [PubMed]
- Adam, R.; Karam, V.; Cailliez, V.; JG, O.G.; Mirza, D.; Cherqui, D.; Klempnauer, J.; Salizzoni, M.; Pratschke, J.; Jamieson, N.; et al. 2018 Annual Report of the European Liver Transplant Registry (ELTR)—50-year evolution of liver transplantation. Transpl. Int. 2018, 31, 1293–1317. [Google Scholar] [CrossRef] [PubMed]
- Turati, F.; Trichopoulos, D.; Polesel, J.; Bravi, F.; Rossi, M.; Talamini, R.; Franceschi, S.; Montella, M.; Trichopoulou, A.; La Vecchia, C.; et al. Mediterranean diet and hepatocellular carcinoma. J. Hepatol. 2014, 60, 606–611. [Google Scholar] [CrossRef]
- Bogumil, D.; Park, S.Y.; Le Marchand, L.; Haiman, C.A.; Wilkens, L.R.; Boushey, C.J.; Setiawan, V.W. High-Quality Diets Are Associated with Reduced Risk of Hepatocellular Carcinoma and Chronic Liver Disease: The Multiethnic Cohort. Hepatol. Commun. 2019, 3, 437–447. [Google Scholar] [CrossRef]
- Tamura, T.; Wada, K.; Konishi, K.; Goto, Y.; Mizuta, F.; Koda, S.; Hori, A.; Tanabashi, S.; Matsushita, S.; Tokimitsu, N.; et al. Coffee, Green Tea, and Caffeine Intake and Liver Cancer Risk: A Prospective Cohort Study. Nutr. Cancer 2018, 70, 1210–1216. [Google Scholar] [CrossRef]
- Simon, T.G.; Henson, J.; Osganian, S.; Masia, R.; Chan, A.T.; Chung, R.T.; Corey, K.E. Daily Aspirin Use Associated with Reduced Risk for Fibrosis Progression in Patients with Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2019, 17, 2776–2784.e4. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Singh, P.P.; Singh, A.G.; Murad, M.H.; Sanchez, W. Anti-diabetic medications and the risk of hepatocellular cancer: A systematic review and meta-analysis. Am. J. Gastroenterol. 2013, 108, 881–891; quiz 892. [Google Scholar] [CrossRef] [PubMed]
- German, M.N.; Lutz, M.K.; Pickhardt, P.J.; Bruce, R.J.; Said, A. Statin Use is Protective against Hepatocellular Carcinoma in Patients with Nonalcoholic Fatty Liver Disease: A Case-control Study. J. Clin. Gastroenterol. 2020, 54, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Zou, B.; Odden, M.C.; Nguyen, M.H. Statin Use and Reduced Hepatocellular Carcinoma Risk in Patients with Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2023, 21, 435–444.e6. [Google Scholar] [CrossRef] [PubMed]
- Sanyal, A.J.; Van Natta, M.L.; Clark, J.; Neuschwander-Tetri, B.A.; Diehl, A.; Dasarathy, S.; Loomba, R.; Chalasani, N.; Kowdley, K.; Hameed, B.; et al. Prospective Study of Outcomes in Adults with Nonalcoholic Fatty Liver Disease. N. Engl. J. Med. 2021, 385, 1559–1569. [Google Scholar] [CrossRef] [PubMed]
- Mozes, F.E.; Lee, J.A.; Vali, Y.; Alzoubi, O.; Staufer, K.; Trauner, M.; Paternostro, R.; Stauber, R.E.; Holleboom, A.G.; van Dijk, A.M.; et al. Performance of non-invasive tests and histology for the prediction of clinical outcomes in patients with non-alcoholic fatty liver disease: An individual participant data meta-analysis. Lancet Gastroenterol. Hepatol. 2023, 8, 704–713. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, J.E.; Christian, N.J.; Flum, D.R.; Pomp, A.; Pories, W.J.; Wolfe, B.M.; Courcoulas, A.P.; Belle, S.H. Postoperative Behavioral Variables and Weight Change 3 Years after Bariatric Surgery. JAMA Surg. 2016, 151, 752–757. [Google Scholar] [CrossRef] [PubMed]
- Svensson, P.A.; Anveden, A.; Romeo, S.; Peltonen, M.; Ahlin, S.; Burza, M.A.; Carlsson, B.; Jacobson, P.; Lindroos, A.K.; Lonroth, H.; et al. Alcohol consumption and alcohol problems after bariatric surgery in the Swedish obese subjects study. Obesity 2013, 21, 2444–2451. [Google Scholar] [CrossRef] [PubMed]
- King, W.C.; Chen, J.Y.; Courcoulas, A.P.; Dakin, G.F.; Engel, S.G.; Flum, D.R.; Hinojosa, M.W.; Kalarchian, M.A.; Mattar, S.G.; Mitchell, J.E.; et al. Alcohol and other substance use after bariatric surgery: Prospective evidence from a U.S. multicenter cohort study. Surg. Obes. Relat. Dis. 2017, 13, 1392–1402. [Google Scholar] [CrossRef]
- Conason, A.; Teixeira, J.; Hsu, C.H.; Puma, L.; Knafo, D.; Geliebter, A. Substance use following bariatric weight loss surgery. JAMA Surg. 2013, 148, 145–150. [Google Scholar] [CrossRef]
- Alvarado-Tapias, E.; Marti-Aguado, D.; Kennedy, K.; Fernandez-Carrillo, C.; Ventura-Cots, M.; Morales-Arraez, D.; Atkinson, S.R.; Clemente-Sanchez, A.; Argemi, J.; Bataller, R. Bariatric Surgery Is Associated with Alcohol-Related Liver Disease and Psychiatric Disorders Associated with AUD. Obes. Surg. 2023, 33, 1494–1505. [Google Scholar] [CrossRef] [PubMed]
- Yarra, P.; Dunn, W.; Younossi, Z.; Kuo, Y.F.; Singal, A.K. Association of Previous Gastric Bypass Surgery and Patient Outcomes in Alcohol-Associated Cirrhosis Hospitalizations. Dig. Dis. Sci. 2023, 68, 1026–1034. [Google Scholar] [CrossRef] [PubMed]
- Anugwom, C.; Thomson, M.; Freese, R.L.; Lake, J.R.; Lim, N. Lower survival and higher rates of cirrhosis in patients with ROUX-EN-Y gastric bypass hospitalised with alcohol-associated hepatitis. BMJ Open Gastroenterol. 2023, 10, e001083. [Google Scholar] [CrossRef] [PubMed]
- Sobell, L.C.; Agrawal, S.; Sobell, M.B.; Leo, G.I.; Young, L.J.; Cunningham, J.A.; Simco, E.R. Comparison of a quick drinking screen with the timeline followback for individuals with alcohol problems. J. Stud. Alcohol. 2003, 64, 858–861. [Google Scholar] [CrossRef] [PubMed]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; de la Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption—II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef] [PubMed]
- Lim, N.; Leventhal, T.M.; Thomson, M.J.; Hassan, M.; Thompson, J.; Adams, A.; Chinnakotla, S.; Humphreville, V.; Kandaswamy, R.; Kirchner, V.; et al. Protocolized screening and detection of occult alcohol use before and after liver transplant: Lessons learned from a quality improvement initiative. Clin. Transplant. 2023, 37, e15036. [Google Scholar] [CrossRef] [PubMed]
- Arab, J.P.; Izzy, M.; Leggio, L.; Bataller, R.; Shah, V.H. Management of alcohol use disorder in patients with cirrhosis in the setting of liver transplantation. Nat. Rev. Gastroenterol. Hepatol. 2022, 19, 45–59. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Marchesini, G.; Pinto-Cortez, H.; Petta, S. Epidemiology of Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis: Implications for Liver Transplantation. Transplantation 2019, 103, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Scientific Registry of Transplant Recipients. Request for Information. Available online: https://www.srtr.org/reports/optnsrtr-annual-data-report: (accessed on 15 December 2023).
- Vilar-Gomez, E.; Martinez-Perez, Y.; Calzadilla-Bertot, L.; Torres-Gonzalez, A.; Gra-Oramas, B.; Gonzalez-Fabian, L.; Friedman, S.L.; Diago, M.; Romero-Gomez, M. Weight Loss Through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis. Gastroenterology 2015, 149, 367–378.e5; quiz e314–e365. [Google Scholar] [CrossRef]
- Rinella, M.E.; Neuschwander-Tetri, B.A.; Siddiqui, M.S.; Abdelmalek, M.F.; Caldwell, S.; Barb, D.; Kleiner, D.E.; Loomba, R. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology 2023, 77, 1797–1835. [Google Scholar] [CrossRef]
- Kouvari, M.; Boutari, C.; Chrysohoou, C.; Fragkopoulou, E.; Antonopoulou, S.; Tousoulis, D.; Pitsavos, C.; Panagiotakos, D.B.; Mantzoros, C.S.; ATTICA Study Investigators. Mediterranean diet is inversely associated with steatosis and fibrosis and decreases ten-year diabetes and cardiovascular risk in NAFLD subjects: Results from the ATTICA prospective cohort study. Clin. Nutr. 2021, 40, 3314–3324. [Google Scholar] [CrossRef] [PubMed]
- Wijarnpreecha, K.; Thongprayoon, C.; Ungprasert, P. Coffee consumption and risk of nonalcoholic fatty liver disease: A systematic review and meta-analysis. Eur. J. Gastroenterol. Hepatol. 2017, 29, e8–e12. [Google Scholar] [CrossRef] [PubMed]
- Malespin, M.H.; Barritt, A.S.t.; Watkins, S.E.; Schoen, C.; Tincopa, M.A.; Corbin, K.D.; Mospan, A.R.; Munoz, B.; Trinh, H.N.; Weiss, L.M.; et al. Weight Loss and Weight Regain in Usual Clinical Practice: Results from the TARGET-NASH Observational Cohort. Clin. Gastroenterol. Hepatol. 2022, 20, 2393–2395.e4. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, D.; Shikora, S.A.; Aarts, E.; Aminian, A.; Angrisani, L.; Cohen, R.V.; de Luca, M.; Faria, S.L.; Goodpaster, K.P.S.; Haddad, A.; et al. 2022 American Society of Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) Indications for Metabolic and Bariatric Surgery. Obes. Surg. 2023, 33, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Lv, X.; Dong, Y.; Hu, L.; Lu, F.; Zhou, C.; Qin, S. Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) for the management of nonalcoholic fatty liver disease (NAFLD): A systematic review. Endocrinol. Diabetes Metab. 2020, 3, e00163. [Google Scholar] [CrossRef] [PubMed]
- Yen, F.S.; Hou, M.C.; Cheng-Chung Wei, J.; Shih, Y.H.; Hsu, C.Y.; Hsu, C.C.; Hwu, C.M. Glucagon-like Peptide-1 Receptor Agonist Use in Patients with Liver Cirrhosis and Type 2 Diabetes. Clin. Gastroenterol. Hepatol. 2023, 166, S-1472–S-1473. [Google Scholar] [CrossRef] [PubMed]
- Volpe, S.; Lisco, G.; Racaniello, D.; Fanelli, M.; Colaianni, V.; Vozza, A.; Triggiani, V.; Sabbà, C.; Tortorella, C.; De Pergola, G.; et al. Once-Weekly Semaglutide Induces an Early Improvement in Body Composition in Patients with Type 2 Diabetes: A 26-Week Prospective Real-Life Study. Nutrients 2022, 14, 2414. [Google Scholar] [CrossRef] [PubMed]
- Volpe, S.; Lisco, G.; Fanelli, M.; Racaniello, D.; Colaianni, V.; Lavarra, V.; Triggiani, D.; Crudele, L.; Triggiani, V.; Sabbà, C.; et al. Oral semaglutide improves body composition and preserves lean mass in patients with type 2 diabetes: A 26-week prospective real-life study. Front. Endocrinol. 2023, 14, 1240263. [Google Scholar] [CrossRef] [PubMed]
- Wharton, S.; Lau, D.C.W.; Vallis, M.; Sharma, A.M.; Biertho, L.; Campbell-Scherer, D.; Adamo, K.; Alberga, A.; Bell, R.; Boulé, N.; et al. Obesity in adults: A clinical practice guideline. CMAJ 2020, 192, E875–E891. [Google Scholar] [CrossRef]
- Vallis, T.M.; Macklin, D.; Russell-Mayhew, S. Canadian Adult Obesity Clinical Practice Guidelines: Effective Psychological and Behavioural Interventions in Obesity Management. Available online: https://obesitycanada.ca/guidelines/behavioural (accessed on 24 April 2024).
- Johns, D.J.; Hartmann-Boyce, J.; Jebb, S.A.; Aveyard, P.; Behavioural Weight Management Review Group. Diet or exercise interventions vs. combined behavioral weight management programs: A systematic review and meta-analysis of direct comparisons. J. Acad. Nutr. Diet. 2014, 114, 1557–1568. [Google Scholar] [CrossRef]
- Lv, N.; Azar, K.M.J.; Rosas, L.G.; Wulfovich, S.; Xiao, L.; Ma, J. Behavioral lifestyle interventions for moderate and severe obesity: A systematic review. Prev. Med. 2017, 100, 180–193. [Google Scholar] [CrossRef] [PubMed]
- Boursier, J.; Anty, R.; Carette, C.; Cariou, B.; Castera, L.; Caussy, C.; Fontaine, H.; Garioud, A.; Gourdy, P.; Guerci, B.; et al. Management of diabetes mellitus in patients with cirrhosis: An overview and joint statement. Diabetes Metab. 2021, 47, 101272. [Google Scholar] [CrossRef] [PubMed]
- Vargas, J.I.; Arrese, M.; Shah, V.H.; Arab, J.P. Use of Statins in Patients with Chronic Liver Disease and Cirrhosis: Current Views and Prospects. Curr. Gastroenterol. Rep. 2017, 19, 43. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, D.E.; Serper, M.A.; Mehta, R.; Fox, R.; John, B.; Aytaman, A.; Baytarian, M.; Hunt, K.; Albrecht, J.; Njei, B.; et al. Effects of Hypercholesterolemia and Statin Exposure on Survival in a Large National Cohort of Patients with Cirrhosis. Gastroenterology 2019, 156, 1693–1706.e12. [Google Scholar] [CrossRef]
- American Society for Metabolic and Bariatric Surgery. Estimate of Bariatric Surgery Numbers, 2011–2018. Available online: https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers (accessed on 12 January 2024).
- Miller, A.; Jalil, S.; Hussan, H.; Kelly, S.; Hinton, A.; Hanje, J.; Michaels, A.; Conteh, L.; Black, S.; Mumtaz, K. Apprising the choice of bariatric surgery in patients with compensated cirrhosis with morbid obesity: Results of a national analysis. Updates Surg. 2021, 73, 1899–1908. [Google Scholar] [CrossRef]
- Lassailly, G.; Caiazzo, R.; Buob, D.; Pigeyre, M.; Verkindt, H.; Labreuche, J.; Raverdy, V.; Leteurtre, E.; Dharancy, S.; Louvet, A.; et al. Bariatric Surgery Reduces Features of Nonalcoholic Steatohepatitis in Morbidly Obese Patients. Gastroenterology 2015, 149, 379–388; quiz e315–e376. [Google Scholar] [CrossRef]
- Aminian, A.; Al-Kurd, A.; Wilson, R.; Bena, J.; Fayazzadeh, H.; Singh, T.; Albaugh, V.L.; Shariff, F.U.; Rodriguez, N.A.; Jin, J.; et al. Association of Bariatric Surgery with Major Adverse Liver and Cardiovascular Outcomes in Patients with Biopsy-Proven Nonalcoholic Steatohepatitis. JAMA 2021, 326, 2031–2042. [Google Scholar] [CrossRef]
- Ahmed, S.; Pouwels, S.; Parmar, C.; Kassir, R.; de Luca, M.; Graham, Y.; Mahawar, K.; Collaborative, G.B.R. Outcomes of Bariatric Surgery in Patients with Liver Cirrhosis: A Systematic Review. Obes. Surg. 2021, 31, 2255–2267. [Google Scholar] [CrossRef]
- Patton, H.; Heimbach, J.; McCullough, A. AGA Clinical Practice Update on Bariatric Surgery in Cirrhosis: Expert Review. Clin. Gastroenterol. Hepatol. 2021, 19, 436–445. [Google Scholar] [CrossRef]
- Idriss, R.; Hasse, J.; Wu, T.; Khan, F.; Saracino, G.; McKenna, G.; Testa, G.; Trotter, J.; Klintmalm, G.; Asrani, S.K. Impact of Prior Bariatric Surgery on Perioperative Liver Transplant Outcomes. Liver Transpl. 2019, 25, 217–227. [Google Scholar] [CrossRef]
- Yemini, R.; Nesher, E.; Winkler, J.; Carmeli, I.; Azran, C.; Ben David, M.; Mor, E.; Keidar, A. Bariatric surgery in solid organ transplant patients: Long-term follow-up results of outcome, safety, and effect on immunosuppression. Am. J. Transplant. 2018, 18, 2772–2780. [Google Scholar] [CrossRef] [PubMed]
- Jirapinyo, P.; McCarty, T.R.; Dolan, R.D.; Shah, R.; Thompson, C.C. Effect of Endoscopic Bariatric and Metabolic Therapies on Nonalcoholic Fatty Liver Disease: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2022, 20, 511–524.e1. [Google Scholar] [CrossRef] [PubMed]
- Chierici, A.; Alromayan, M.; De Fatico, S.; Drai, C.; Vinci, D.; Anty, R.; Schiavo, L.; Iannelli, A. Is bariatric surgery safer before, during, or after liver transplantation? A systematic review and meta-analysis. J. Liver Transplant. 2023, 9, 100139. [Google Scholar] [CrossRef]
- Osseis, M.; Lazzati, A.; Salloum, C.; Gavara, C.G.; Compagnon, P.; Feray, C.; Lim, C.; Azoulay, D. Sleeve Gastrectomy after Liver Transplantation: Feasibility and Outcomes. Obes. Surg. 2018, 28, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Al-Nowaylati, A.R.; Al-Haddad, B.J.; Dorman, R.B.; Alsaied, O.A.; Lake, J.R.; Chinnakotla, S.; Slusarek, B.M.; Sampson, B.K.; Ikramuddin, S.; Buchwald, H.; et al. Gastric bypass after liver transplantation. Liver Transpl. 2013, 19, 1324–1329. [Google Scholar] [CrossRef] [PubMed]
- Hirshorn, R.E.; Schaubel, D.E.; Abt, P.L.; Reddy, K.R.; Bittermann, T. Living donor liver transplantation in the United States for alcohol-associated liver disease and nonalcoholic steatohepatitis: An evaluation in the current era. Liver Transpl. 2023, 30, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.; Goyal, N.; Nayeem, M.; Pareek, S.; Gupta, S. Living donor liver transplantation in patients weighing >/=100 kg: Low graft weight and obesity do not impact outcomes. Liver Transpl. 2017, 23, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Sugawara, Y.; Tamura, S.; Kaneko, J.; Takazawa, Y.; Aoki, T.; Hasegawa, K.; Sakamoto, Y.; Yamashiki, N.; Kokudo, N. Living donor liver transplantation for non-alcoholic steatohepatitis: A single center experience. Hepatol. Res. 2014, 44, E3–E10. [Google Scholar] [CrossRef]
- Schwimmer, J.B.; Celedon, M.A.; Lavine, J.E.; Salem, R.; Campbell, N.; Schork, N.J.; Shiehmorteza, M.; Yokoo, T.; Chavez, A.; Middleton, M.S.; et al. Heritability of nonalcoholic fatty liver disease. Gastroenterology 2009, 136, 1585–1592. [Google Scholar] [CrossRef]
- Xu, R.; Tao, A.; Zhang, S.; Deng, Y.; Chen, G. Association between patatin-like phospholipase domain containing 3 gene (PNPLA3) polymorphisms and nonalcoholic fatty liver disease: A HuGE review and meta-analysis. Sci. Rep. 2015, 5, 9284. [Google Scholar] [CrossRef]
- Singhal, A.; Wilson, G.C.; Wima, K.; Quillin, R.C.; Cuffy, M.; Anwar, N.; Kaiser, T.E.; Paterno, F.; Diwan, T.S.; Woodle, E.S.; et al. Impact of recipient morbid obesity on outcomes after liver transplantation. Transpl. Int. 2015, 28, 148–155. [Google Scholar] [CrossRef]
- Heimbach, J.K.; Watt, K.D.; Poterucha, J.J.; Ziller, N.F.; Cecco, S.D.; Charlton, M.R.; Hay, J.E.; Wiesner, R.H.; Sanchez, W.; Rosen, C.B.; et al. Combined liver transplantation and gastric sleeve resection for patients with medically complicated obesity and end-stage liver disease. Am. J. Transplant. 2013, 13, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Schaeffer, D.F.; Yoshida, E.M.; Buczkowski, A.K.; Chung, S.W.; Steinbrecher, U.P.; Erb, S.E.; Scudamore, C.H. Surgical morbidity in severely obese liver transplant recipients—A single Canadian Centre Experience. Ann. Hepatol. 2009, 8, 38–40. [Google Scholar] [CrossRef]
- Agopian, V.G.; Kaldas, F.M.; Hong, J.C.; Whittaker, M.; Holt, C.; Rana, A.; Zarrinpar, A.; Petrowsky, H.; Farmer, D.; Yersiz, H.; et al. Liver transplantation for nonalcoholic steatohepatitis: The new epidemic. Ann. Surg. 2012, 256, 624–633. [Google Scholar] [CrossRef] [PubMed]
- LaMattina, J.C.; Foley, D.P.; Fernandez, L.A.; Pirsch, J.D.; Musat, A.I.; D’Alessandro, A.M.; Mezrich, J.D. Complications associated with liver transplantation in the obese recipient. Clin. Transplant. 2012, 26, 910–918. [Google Scholar] [CrossRef] [PubMed]
- Moore, H.B.; Bababekov, Y.J.; Pomposelli, J.J.; Adams, M.A.; Crouch, C.; Yoeli, D.; Choudhury, R.A.; Ferrell, T.; Burton, J.R.; Pomfret, E.A.; et al. The vexing triad of obesity, alcohol, and coagulopathy predicts the need for multiple operations in liver transplantation. Am. J. Surg. 2022, 224, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Q.; Haque, O.; Yeh, H.; Markmann, J.F.; Dageforde, L.A. The impact of race and comorbid conditions on adult liver transplant outcomes in obese recipients. Transpl. Int. 2021, 34, 2834–2845. [Google Scholar] [CrossRef] [PubMed]
- Conzen, K.D.; Vachharajani, N.; Collins, K.M.; Anderson, C.D.; Lin, Y.; Wellen, J.R.; Shenoy, S.; Lowell, J.A.; Doyle, M.B.; Chapman, W.C. Morbid obesity in liver transplant recipients adversely affects longterm graft and patient survival in a single-institution analysis. HPB 2015, 17, 251–257. [Google Scholar] [CrossRef]
- Fujikawa, T.; Fujita, S.; Mizuno, S.; Shenkman, E.; Vogel, B.; Lipori, P.; Hemming, A.W.; Nelson, D.; Reed, A.I. Clinical and financial impact of obesity on the outcome of liver transplantation. Transplant. Proc. 2006, 38, 3612–3614. [Google Scholar] [CrossRef]
- Nair, S.; Vanatta, J.M.; Arteh, J.; Eason, J.D. Effects of obesity, diabetes, and prior abdominal surgery on resource utilization in liver transplantation: A single-center study. Liver Transpl. 2009, 15, 1519–1524. [Google Scholar] [CrossRef]
- Alvarez, J.; Mei, X.; Daily, M.; Shah, M.; Grigorian, A.; Berger, J.; Marti, F.; Gedaly, R. Tipping the Scales: Liver Transplant Outcomes of the Super Obese. J. Gastrointest. Surg. 2016, 20, 1628–1635. [Google Scholar] [CrossRef] [PubMed]
- Anselmo, A.; Siragusa, L.; Sensi, B.; Bacchiocchi, G.; Pellicciaro, M.; Manzia, T.M.; Gentileschi, P.; Tisone, G. High-priority liver transplantation and simultaneous sleeve gastrectomy in MELD 32 end-stage liver disease: A case report with long-term follow-up. Obes. Res. Clin. Pract. 2022, 16, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, E.S.M.; de Mello, F.P.T.; Pimentel, L.S.; Andrade, R.O.; Girão, C.; César, C.; El-Kadre, L.J.; de Barros, F.; Coelho, H.S.M.; Brito, A.; et al. Combined liver transplantation with sleeve gastrectomy: A pioneer case series from Brazil. Updates Surg. 2022, 74, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Tariq, N.; Saharia, A.; Nwokedi, U.; Hobeika, M.J.; Mobley, C.M.; Hsu, D.; Potter, L.M.; Moore, L.W.; Elaileh, A.; Sherman, V.; et al. Combined liver transplantation and sleeve gastrectomy: Report of a brief-interval staged approach. Liver Transpl. 2023, 29, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Gunturu, N.S.; Castillo-Larios, R.; Bowers, S.; Edwards, M.; Burns, J.; Perry, D.; Elli, E.F. Combined Sleeve Gastrectomy with Liver Transplant in Patients with Obesity: A Feasibility Study. Obes. Surg. 2022, 32, 3600–3604. [Google Scholar] [CrossRef] [PubMed]
- Iannelli, A.; Petrucciani, N. Low Molecular Weight Heparin in Liver Transplant Recipients After Sleeve Gastrectomy. Liver Transpl. 2021, 27, 1505–1506. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Yeo, D.; Crawford, M.; Strasser, S.I.; McCaughan, G.W. Beware of Portal Vein Thrombosis After Laparoscopic Sleeve Gastrectomy in Liver Transplant Recipients. Liver Transpl. 2021, 27, 1066–1067. [Google Scholar] [CrossRef] [PubMed]
- Nesher, E.; Mor, E.; Shlomai, A.; Naftaly-Cohen, M.; Yemini, R.; Yussim, A.; Brown, M.; Keidar, A. Simultaneous Liver Transplantation and Sleeve Gastrectomy: Prohibitive Combination or a Necessity? Obes. Surg. 2017, 27, 1387–1390. [Google Scholar] [CrossRef] [PubMed]
- Zamora-Valdes, D.; Watt, K.D.; Kellogg, T.A.; Poterucha, J.J.; Di Cecco, S.R.; Francisco-Ziller, N.M.; Taner, T.; Rosen, C.B.; Heimbach, J.K. Long-term outcomes of patients undergoing simultaneous liver transplantation and sleeve gastrectomy. Hepatology 2018, 68, 485–495. [Google Scholar] [CrossRef]
- Giannis, D.; Geropoulos, G.; Kakos, C.D.; Lu, W.; El Hadwe, S.; Fornasiero, M.; Robertson, A.; Parmar, C. Portomesenteric Vein Thrombosis in Patients Undergoing Sleeve Gastrectomy: An Updated Systematic Review and Meta-Analysis of 101,914 Patients. Obes. Surg. 2023, 33, 2991–3007. [Google Scholar] [CrossRef]
- Ryan, R.J.; Heimbach, J.K.; Diwan, T.D. Timing is everything: Sleeve gastrectomy and liver transplantation. Liver Transpl. 2023, 29, 354–355. [Google Scholar] [CrossRef] [PubMed]
- Rinella, M.E.; Satapathy, S.K.; Brandman, D.; Smith, C.; Elwir, S.; Xia, J.; Gibson, M.; Figueredo, C.; Angirekula, M.; Vanatta, J.M.; et al. Factors Impacting Survival in Those Transplanted for NASH Cirrhosis: Data from the NailNASH Consortium. Clin. Gastroenterol. Hepatol. 2023, 21, 445–455.e2. [Google Scholar] [CrossRef] [PubMed]
- Jamil, O.K.; Sandikci, B.; Faust, N.; Cotter, T.G.; Paul, S.; di Sabato, D.; Fung, J.; Charlton, M. Relatively Poor Long-term Outcomes Following Liver Transplantation for NASH in the United States. Transplantation 2022, 106, 2006–2018. [Google Scholar] [CrossRef] [PubMed]
- John, P.R.; Thuluvath, P.J. Outcome of patients with new-onset diabetes mellitus after liver transplantation compared with those without diabetes mellitus. Liver Transpl. 2002, 8, 708–713. [Google Scholar] [CrossRef] [PubMed]
- van den Berg, E.H.; Douwes, R.M.; de Meijer, V.E.; Schreuder, T.C.M.A.; Blokzijl, H. Liver transplantation for NASH cirrhosis is not performed at the expense of major post-operative morbidity. Dig. Liver Dis. 2018, 50, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Neuberger, J.M.; Bechstein, W.O.; Kuypers, D.R.; Burra, P.; Citterio, F.; De Geest, S.; Duvoux, C.; Jardine, A.G.; Kamar, N.; Kramer, B.K.; et al. Practical Recommendations for Long-term Management of Modifiable Risks in Kidney and Liver Transplant Recipients: A Guidance Report and Clinical Checklist by the Consensus on Managing Modifiable Risk in Transplantation (COMMIT) Group. Transplantation 2017, 101 (Suppl. 2), S1–S56. [Google Scholar] [CrossRef]
- Chandrakumaran, A.; Siddiqui, M.S. Implications of Nonalcoholic Steatohepatitis as the Cause of End-Stage Liver Disease Before and After Liver Transplant. Gastroenterol. Clin. N. Am. 2020, 49, 165–178. [Google Scholar] [CrossRef]
- Ferreira, A.P.; Machado, M.V. Impact of pretransplant frailty and sarcopenia on the post-transplant prognosis of patients with liver cirrhosis: A systematic review. Eur. J. Gastroenterol. Hepatol. 2021, 33 (Suppl. 1), e883–e897. [Google Scholar] [CrossRef]
- Dunn, M.A.; Rogal, S.S.; Duarte-Rojo, A.; Lai, J.C. Physical Function, Physical Activity, and Quality of Life after Liver Transplantation. Liver Transpl. 2020, 26, 702–708. [Google Scholar] [CrossRef]
- Krasnoff, J.B.; Vintro, A.Q.; Ascher, N.L.; Bass, N.M.; Paul, S.M.; Dodd, M.J.; Painter, P.L. A randomized trial of exercise and dietary counseling after liver transplantation. Am. J. Transplant. 2006, 6, 1896–1905. [Google Scholar] [CrossRef]
- Bhati, C.; Idowu, M.O.; Sanyal, A.J.; Rivera, M.; Driscoll, C.; Stravitz, R.T.; Kohli, D.R.; Matherly, S.; Puri, P.; Gilles, H.; et al. Long-term Outcomes in Patients Undergoing Liver Transplantation for Nonalcoholic Steatohepatitis-Related Cirrhosis. Transplantation 2017, 101, 1867–1874. [Google Scholar] [CrossRef] [PubMed]
- Cotter, T.G.; Charlton, M. Nonalcoholic Steatohepatitis after Liver Transplantation. Liver Transpl. 2020, 26, 141–159. [Google Scholar] [CrossRef]
- Watt, K.D.; Charlton, M.R. Metabolic syndrome and liver transplantation: A review and guide to management. J. Hepatol. 2010, 53, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Charlton, M.R. Improving long-term outcomes after liver transplantation. Clin. Liver Dis. 2014, 18, 717–730. [Google Scholar] [CrossRef] [PubMed]
- Russo, M.W. The Care of the Postliver Transplant Patient. J. Clin. Gastroenterol. 2017, 51, 683–692. [Google Scholar] [CrossRef] [PubMed]
- Hoskova, L.; Malek, I.; Kopkan, L.; Kautzner, J. Pathophysiological mechanisms of calcineurin inhibitor-induced nephrotoxicity and arterial hypertension. Physiol. Res. 2017, 66, 167–180. [Google Scholar] [CrossRef] [PubMed]
- Lucey, M.R.; Terrault, N.; Ojo, L.; Hay, J.E.; Neuberger, J.; Blumberg, E.; Teperman, L.W. Long-term management of the successful adult liver transplant: 2012 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Liver Transpl. 2013, 19, 3–26. [Google Scholar] [CrossRef] [PubMed]
- Midtvedt, K.; Neumayer, H.H. Management strategies for posttransplant hypertension. Transplantation 2000, 70, SS64–SS69. [Google Scholar] [PubMed]
- Becchetti, C.; Dirchwolf, M.; Schropp, J.; Magini, G.; Mullhaupt, B.; Immer, F.; Dufour, J.F.; Banz, V.; Berzigotti, A.; Bosch, J.; et al. Use of statins after liver transplantation is associated with improved survival: Results of a nationwide study. Aliment. Pharmacol. Ther. 2022, 56, 1194–1204. [Google Scholar] [CrossRef]
- Ojo, A.O.; Held, P.J.; Port, F.K.; Wolfe, R.A.; Leichtman, A.B.; Young, E.W.; Arndorfer, J.; Christensen, L.; Merion, R.M. Chronic renal failure after transplantation of a nonrenal organ. N. Engl. J. Med. 2003, 349, 931–940. [Google Scholar] [CrossRef]
- Saeed, N.; Glass, L.; Sharma, P.; Shannon, C.; Sonnenday, C.J.; Tincopa, M.A. Incidence and Risks for Nonalcoholic Fatty Liver Disease and Steatohepatitis Post-liver Transplant: Systematic Review and Meta-analysis. Transplantation 2019, 103, e345–e354. [Google Scholar] [CrossRef]
- Czarnecka, K.; Czarnecka, P.; Tronina, O.; Bączkowska, T.; Jagielska, A.; Durlik, M. Metabolic Profile of Liver Transplant Recipients and Determinants of their Body Fat Distribution. Obesities 2023, 3, 225–242. [Google Scholar] [CrossRef]
- Silva, A.C.; Nogueira, P.; Machado, M.V. Hepatic steatosis after liver transplantation: A systematic review and meta-analysis. Liver Transpl. 2023, 29, 431–448. [Google Scholar] [CrossRef]
- Paka, P.; Lieber, S.R.; Lee, R.A.; Desai, C.S.; Dupuis, R.E.; Barritt, A.S. Perioperative glucose management and outcomes in liver transplant recipients: A qualitative systematic review. World J. Transplant. 2018, 8, 75–83. [Google Scholar] [CrossRef]
| Medication Class | Metabolic Impacts | Strategies to Reduce Risk |
|---|---|---|
| Calcineurin inhibitors (i.e., tacrolimus, cyclosporine) | Increased risk of diabetes, dyslipidemia, hypertension | Minimize level to achieve normal organ function |
| Corticosteroids (i.e., prednisone) | Increased risk of diabetes, dyslipidemia, hypertension, weight gain | Early steroid withdrawal |
| mTOR inhibitors (i.e., sirolimus, everolimus) | Increased risk of dyslipidemia | Minimize level to achieve normal organ function. Avoid in patients with significant hyperlipidemia or high cardiovascular risk |
| Therapy | Examples | Weight Loss Observed | MASH Resolution | Improvement in Fibrosis Observed |
|---|---|---|---|---|
| Nutrition interventions | ||||
| Dietary changes | Mediterranean diet | If >10% weight loss | Yes | Yes |
| Exercise interventions | ||||
| Exercise | Moderate exercise 5 times per week for at least a total of 150 min | Variable | Yes | Potential benefit |
| Medical therapies | ||||
| SGLT-2 inhibitors | Dapagliflozin, Empagliflozin | 2–3% | Potential benefit | Unknown |
| GLP-1 receptor agonists | Semaglutide | 13% | Yes | Potential benefit |
| GLP-1/GIP receptor agonists | Tirzepatide | 20.9% | Potential benefit | Unknown |
| Endoscopic therapies | ||||
| Bariatric endoscopy | Endoscopic sleeve gastroplasty, primary obesity surgery endoluminal | 14% | Potential benefit | Potential benefit |
| Surgical interventions | ||||
| Bariatric surgery | Sleeve gastrectomy, Roux-en-Y gastric bypass | 30% | Yes | Yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vogel, A.S.; Roediger, R.; von Ahrens, D.; Fortune, B.E.; Schwartz, J.M.; Frager, S.; Chacko, K.R.; Tow, C.Y. The Impact of Metabolic Health and Obesity on Liver Transplant Candidates and Recipients. Life 2024, 14, 685. https://doi.org/10.3390/life14060685
Vogel AS, Roediger R, von Ahrens D, Fortune BE, Schwartz JM, Frager S, Chacko KR, Tow CY. The Impact of Metabolic Health and Obesity on Liver Transplant Candidates and Recipients. Life. 2024; 14(6):685. https://doi.org/10.3390/life14060685
Chicago/Turabian StyleVogel, Alexander S., Rebecca Roediger, Dagny von Ahrens, Brett E. Fortune, Jonathan M. Schwartz, Shalom Frager, Kristina R. Chacko, and Clara Y. Tow. 2024. "The Impact of Metabolic Health and Obesity on Liver Transplant Candidates and Recipients" Life 14, no. 6: 685. https://doi.org/10.3390/life14060685
APA StyleVogel, A. S., Roediger, R., von Ahrens, D., Fortune, B. E., Schwartz, J. M., Frager, S., Chacko, K. R., & Tow, C. Y. (2024). The Impact of Metabolic Health and Obesity on Liver Transplant Candidates and Recipients. Life, 14(6), 685. https://doi.org/10.3390/life14060685






