Radiographic Assessment of Transverse Tarsometatarsal Instability Complicated by Metatarsus Adductus in Hallux Valgus Patients
Abstract
1. Introduction
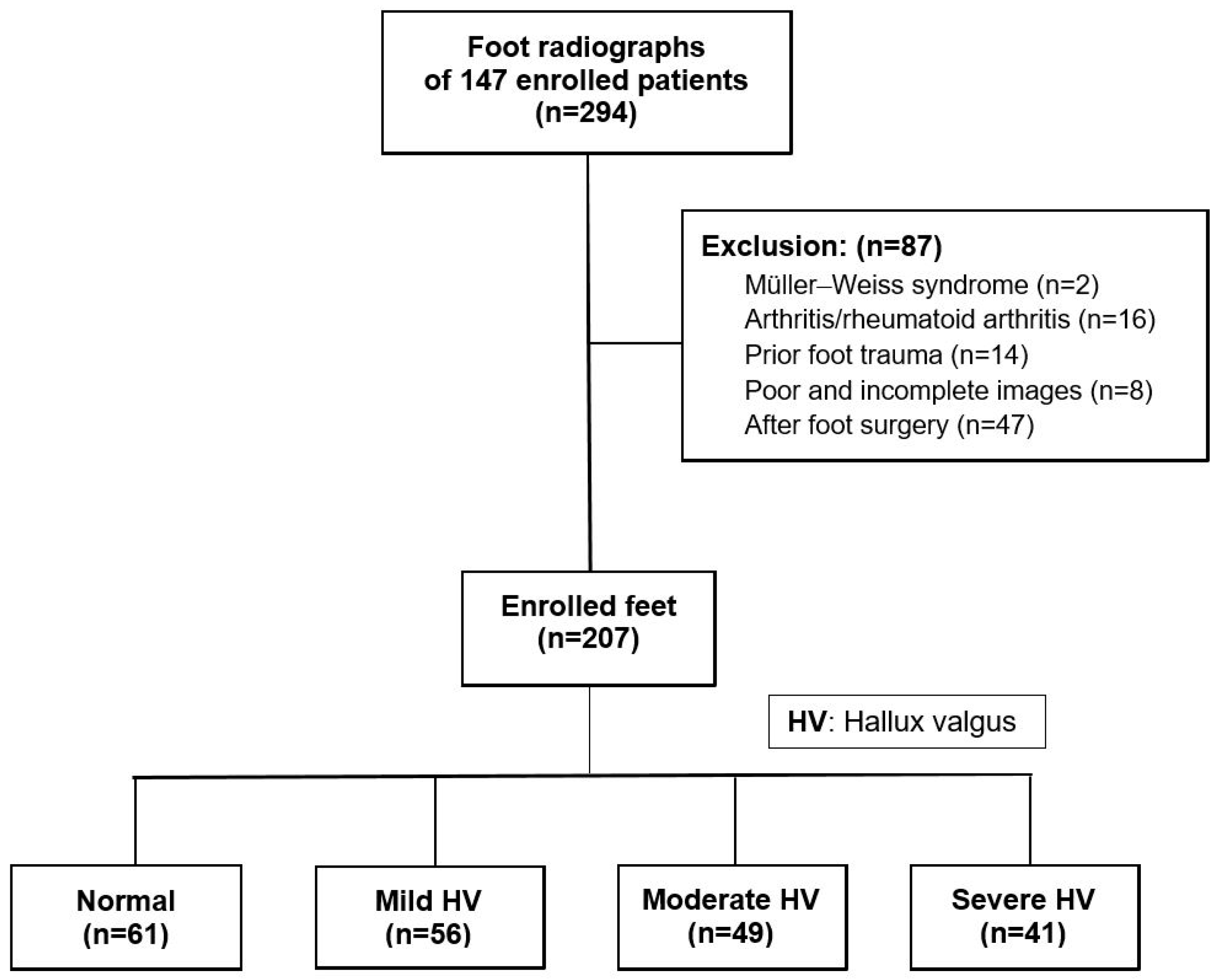
2. Materials and Methods
2.1. Patient Recruitment
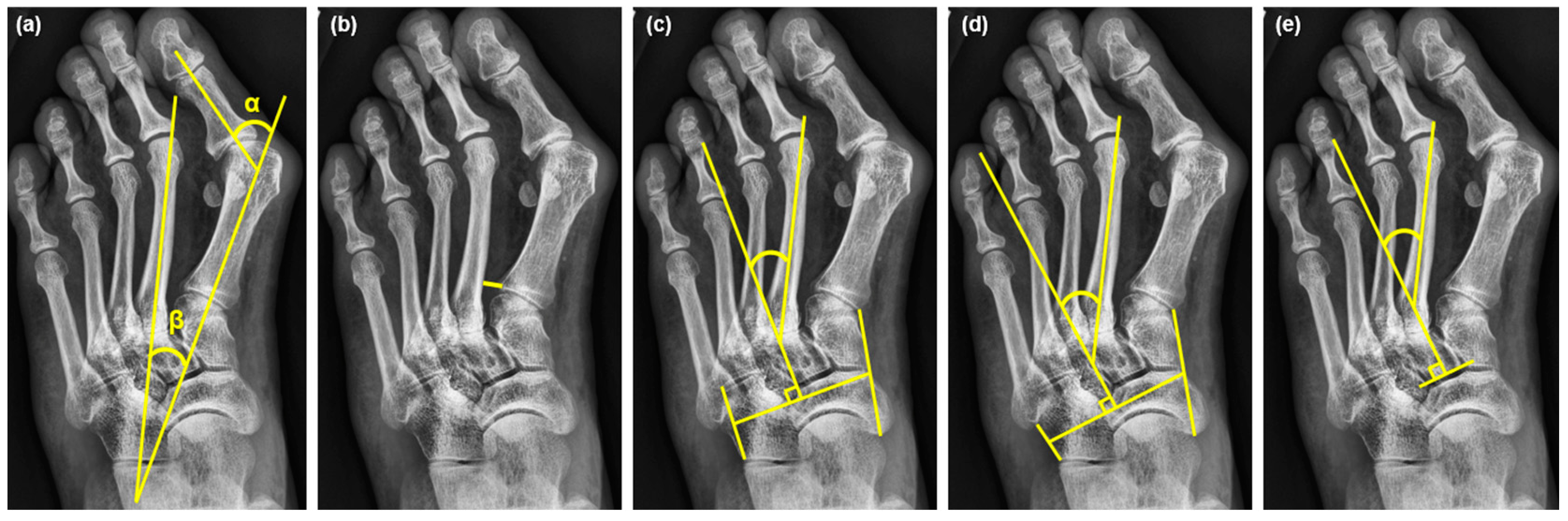
2.2. Radiographic Measurements
2.3. The Severity of HV and Cutoff Value of MAA
2.4. The Intraclass Correlation Coefficient (ICC) Analysis and Determination of the Cutoff Value of the M1-2 Distance
2.5. Statistical Analysis
3. Results
3.1. Demographics of the Enrolled Cases
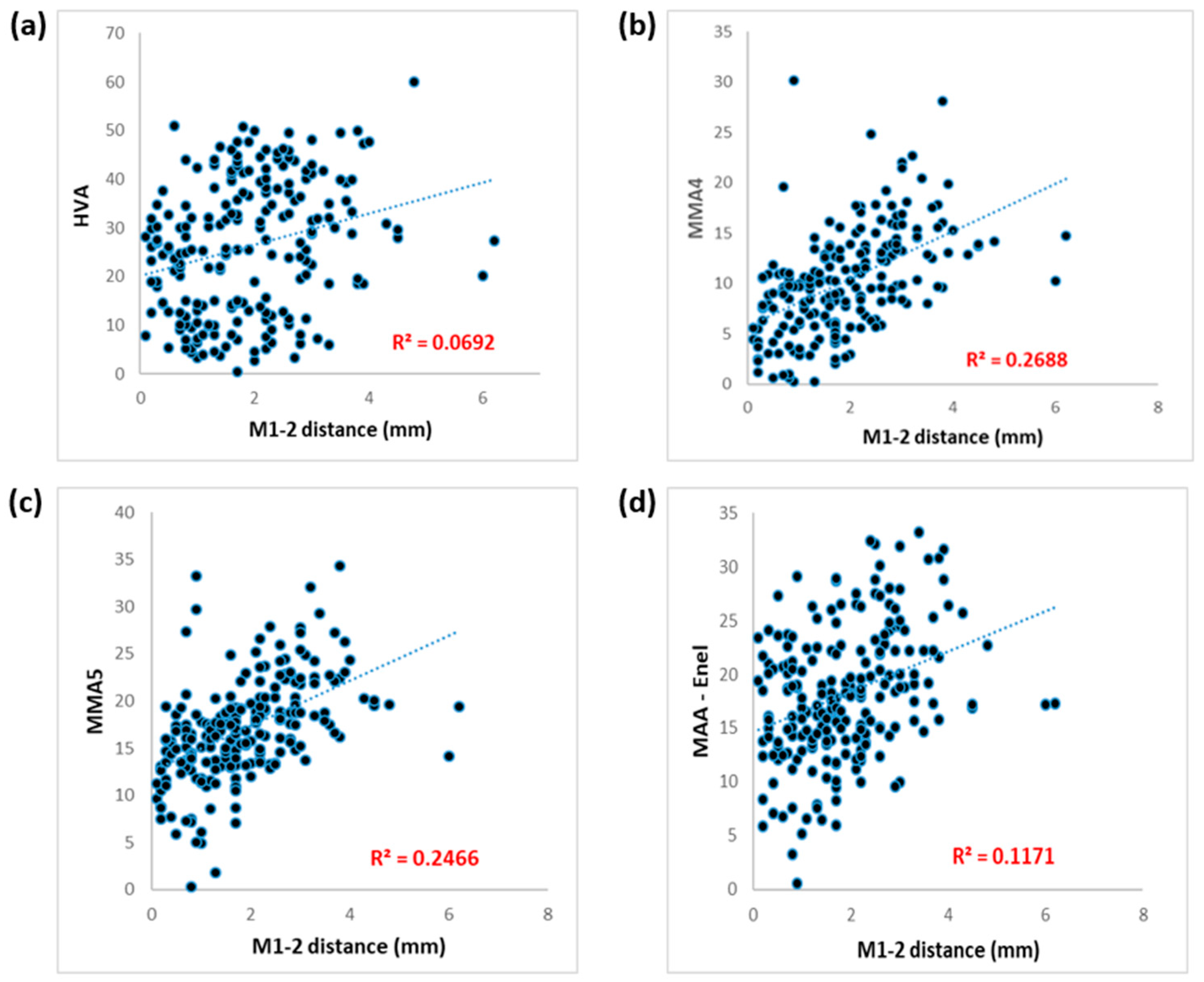
3.2. Correlations between M1-2 Distance and HVA, IMA, and MAAs
3.3. The Difference in M1-2 Distance between Patients with and without MA
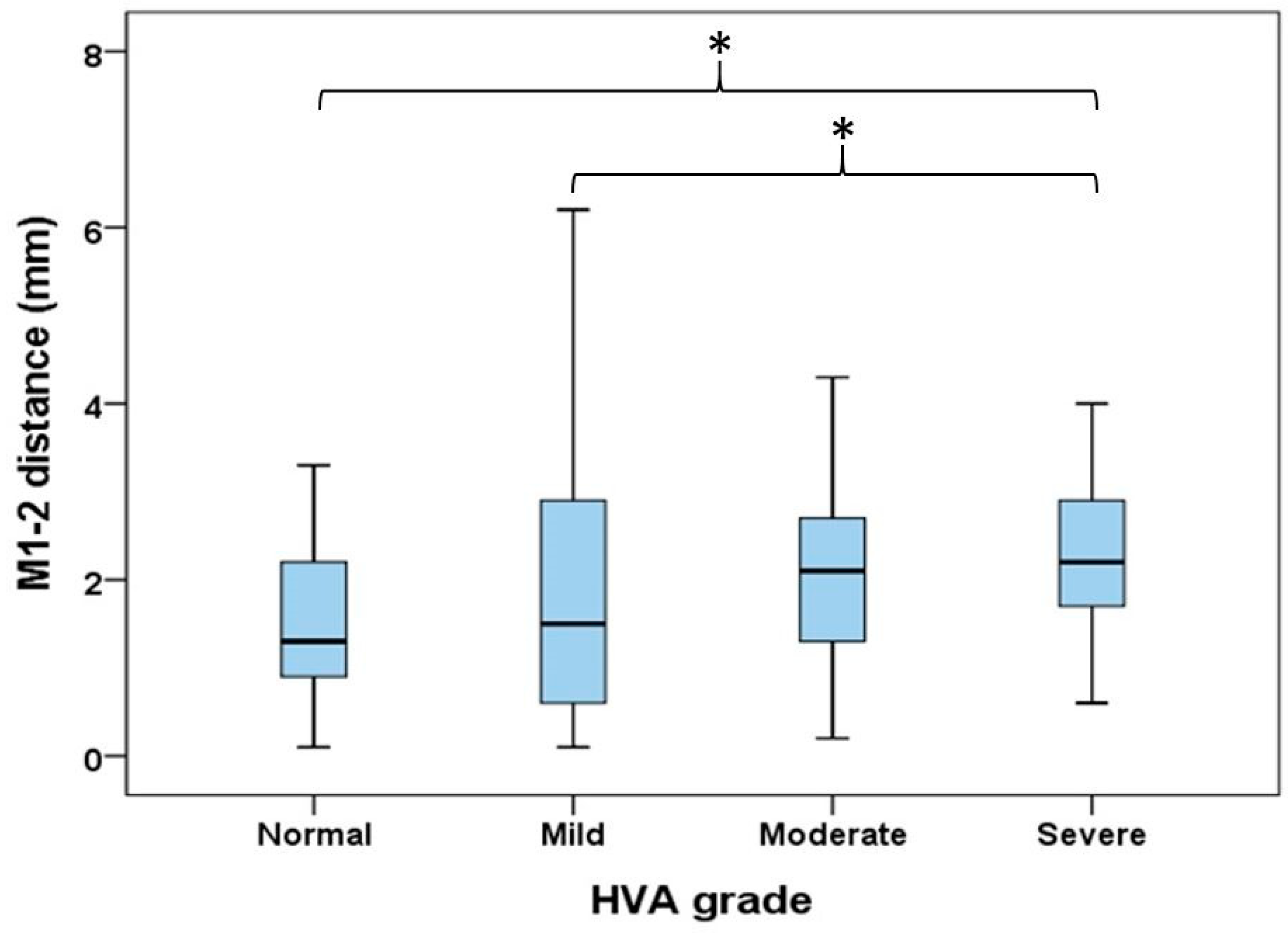
3.4. Comparisons of M1-2 Distance in Different Severities of HV
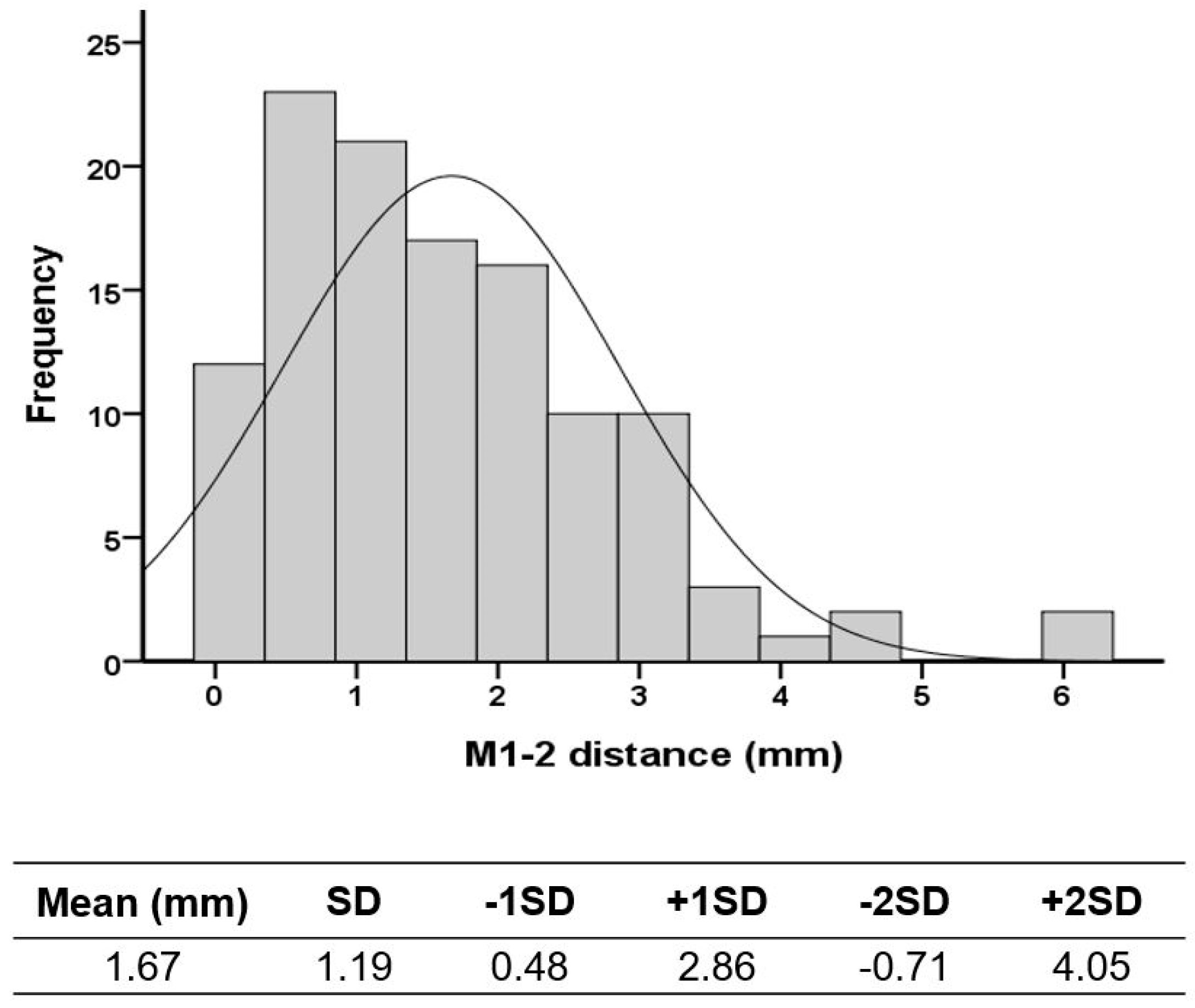
3.5. The Determination of the Cutoff Value of the M1-2 Distance
3.6. ICC of M1-2 Distance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dietz, F.R. Intoeing--fact, fiction and opinion. Am. Fam. Physician 1994, 50, 1249–1259, 1262–1264. [Google Scholar]
- Dawoodi, A.I.; Perera, A. Radiological assessment of metatarsus adductus. Foot Ankle Surg. 2012, 18, 1–8. [Google Scholar] [CrossRef]
- Aiyer, A.A.; Shariff, R.; Ying, L.; Shub, J.; Myerson, M.S. Prevalence of metatarsus adductus in patients undergoing hallux valgus surgery. Foot Ankle Int. 2014, 35, 1292–1297. [Google Scholar] [CrossRef]
- Aiyer, A.; Shub, J.; Shariff, R.; Ying, L.; Myerson, M. Radiographic Recurrence of Deformity After Hallux Valgus Surgery in Patients With Metatarsus Adductus. Foot Ankle Int. 2016, 37, 165–171. [Google Scholar] [CrossRef]
- Cavalheiro, C.S.; Arcuri, M.H.; Guil, V.R.; Gali, J.C. Hallux valgus anatomical alterations and its correlation with the radiographic findings. Acta Ortop. Bras. 2020, 28, 12–15. [Google Scholar] [CrossRef]
- Talaski, G.M.; Baumann, A.N.; Sleem, B.; Anastasio, A.T.; Walley, K.C.; O’Neill, C.N.; Adams, S.B. Weightbearing Imaging Assessment of Midfoot Instability in Patients with Confirmed Hallux Valgus Deformity: A Systematic Review of the Literature. Diagnostics 2024, 14, 193. [Google Scholar] [CrossRef]
- Banks, A.S.; Hsu, Y.S.; Mariash, S.; Zirm, R. Juvenile hallux abducto valgus association with metatarsus adductus. J. Am. Podiatr. Med. Assoc. 1994, 84, 219–224. [Google Scholar] [CrossRef]
- La Reaux, R.L.; Lee, B.R. Metatarsus adductus and hallux abducto valgus: Their correlation. J. Foot Surg. 1987, 26, 304–308. [Google Scholar]
- Ferrari, J.; Malone-Lee, J. A radiographic study of the relationship between metatarsus adductus and hallux valgus. J. Foot Ankle Surg. 2003, 42, 9–14. [Google Scholar] [CrossRef]
- Dessouky, R.; Heineman, N.; Zhang, L.; Hummel, J.; Skweres, J.; Wukich, D.; Chhabra, A. Hallux valgus and metatarsus adductus measurements: Inter-reader reliability and correlations on radiographs and MRI. Clin. Radiol. 2018, 73, 1057.e1057–1057.e1011. [Google Scholar] [CrossRef]
- Dawoodi, A.I.; Perera, A. Reliability of metatarsus adductus angle and correlation with hallux valgus. Foot Ankle Surg. 2012, 18, 180–186. [Google Scholar] [CrossRef]
- Coughlin, M.J.; Roger, A. Mann Award. Juvenile hallux valgus: Etiology and treatment. Foot Ankle Int. 1995, 16, 682–697. [Google Scholar] [CrossRef]
- Conti, M.S.; Caolo, K.C.; Ellis, S.J.; Cody, E.A. Radiographic and Clinical Outcomes of Hallux Valgus and Metatarsus Adductus Treated With a Modified Lapidus Procedure. Foot Ankle Int. 2021, 42, 38–45. [Google Scholar] [CrossRef]
- Reddy, S.C. Management of Hallux Valgus in Metatarsus Adductus. Foot Ankle Clin. 2020, 25, 59–68. [Google Scholar] [CrossRef]
- Kantak, A.P. The Metatarsal Axis Deviation Angle: A Novel Angular Measurement for Planning Surgery of Severe Hallux Valgus. J. Foot Ankle Surg. (Asia-Pac.) 2017, 4, 97–99. [Google Scholar] [CrossRef]
- Kimura, T.; Kubota, M.; Suzuki, N.; Hattori, A.; Saito, M. Weightbearing Computed Tomography and 3-Dimensional Analysis of Mobility Changes of the First Ray After Proximal Oblique Osteotomy for Hallux Valgus. Foot Ankle Int. 2021, 42, 333–339. [Google Scholar] [CrossRef]
- Santrock, R.D.; Smith, B. Hallux Valgus Deformity and Treatment: A Three-Dimensional Approach: Modified Technique for Lapidus Procedure. Foot Ankle Clin. 2018, 23, 281–295. [Google Scholar] [CrossRef]
- Klaue, K.; Hansen, S.T.; Masquelet, A.C. Clinical, quantitative assessment of first tarsometatarsal mobility in the sagittal plane and its relation to hallux valgus deformity. Foot Ankle Int. 1994, 15, 9–13. [Google Scholar] [CrossRef]
- Dietze, A.; Bahlke, U.; Martin, H.; Mittlmeier, T. First ray instability in hallux valgus deformity: A radiokinematic and pedobarographic analysis. Foot Ankle Int. 2013, 34, 124–130. [Google Scholar] [CrossRef]
- Lee, H.Y.; Lalevee, M.; Mansur, N.S.B.; Vandelune, C.A.; Dibbern, K.N.; Barg, A.; Femino, J.E.; de Cesar Netto, C. Multiplanar instability of the first tarsometatarsal joint in hallux valgus and hallux rigidus patients: A case-control study. Int. Orthop. 2022, 46, 255–263. [Google Scholar] [CrossRef]
- Voellmicke, K.V.; Deland, J.T. Manual examination technique to assess dorsal instability of the first ray. Foot Ankle Int. 2002, 23, 1040–1041. [Google Scholar] [CrossRef]
- Doty, J.F.; Coughlin, M.J.; Hirose, C.; Stevens, F.; Schutt, S.; Kennedy, M.; Grebing, B.; Smith, B.; Cooper, T.; Golanó, P.; et al. First metatarsocuneiform joint mobility: Radiographic, anatomic, and clinical characteristics of the articular surface. Foot Ankle Int. 2014, 35, 504–511. [Google Scholar] [CrossRef]
- Young, K.; Kim, J.S.; Cho, H.k.; Kim, H.S. Sagittal and axial mobility of 1st ray in hallux valgus. J. Foot Ankle Res. 2014, 7, A133. [Google Scholar] [CrossRef]
- De Bruijn, J.; Hagemeijer, N.C.; Rikken, Q.G.H.; Husseini, J.S.; Saengsin, J.; Kerkhoffs, G.; Waryasz, G.; Guss, D.; DiGiovanni, C.W. Lisfranc injury: Refined diagnostic methodology using weightbearing and non-weightbearing radiographs. Injury 2022, 53, 2318–2325. [Google Scholar] [CrossRef]
- Karasick, D.; Wapner, K.L. Hallux valgus deformity: Preoperative radiologic assessment. AJR Am. J. Roentgenol. 1990, 155, 119–123. [Google Scholar] [CrossRef]
- Mann, R.A.; Coughlin, M.J. Hallux valgus—Etiology, anatomy, treatment and surgical considerations. Clin. Orthop. Relat. Res. 1981, 157, 31–41. [Google Scholar] [CrossRef]
- Bland, M. An Introduction to Medical Statistics; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Siegel, S. Nonparametric Statistics. Am. Stat. 1957, 11, 13–19. [Google Scholar] [CrossRef]
- Dygut, J.; Piwowar, M. Muscular Systems and Their Influence on Foot Arches and Toes Alignment-Towards the Proper Diagnosis and Treatment of Hallux Valgus. Diagnostics 2022, 12, 2945. [Google Scholar] [CrossRef]
- Myerson, M.; Allon, S.; McGarvey, W. Metatarsocuneiform arthrodesis for management of hallux valgus and metatarsus primus varus. Foot Ankle 1992, 13, 107–115. [Google Scholar] [CrossRef]
- Ornig, M.; Tschauner, S.; Holweg, P.L.; Hohenberger, G.M.; Bratschitsch, G.; Leithner, A.; Leitner, L. A novel method of clinical first tarsometatarsal joint hypermobility testing and radiologic verification. Wien. Klin. Wochenschr. 2021, 133, 209–215. [Google Scholar] [CrossRef]
- Faber, F.W.; Kleinrensink, G.J.; Mulder, P.G.; Verhaar, J.A. Mobility of the first tarsometatarsal joint in hallux valgus patients: A radiographic analysis. Foot Ankle Int. 2001, 22, 965–969. [Google Scholar] [CrossRef]
- Hardy, R.H.; Clapham, J.C. Observations on hallux valgus; based on a controlled series. J. Bone Joint Surg. Br. 1951, 33-b, 376–391. [Google Scholar] [CrossRef]
- Myerson, M.S.; Cerrato, R. Current management of tarsometatarsal injuries in the athlete. Instr. Course Lect. 2009, 58, 583–594. [Google Scholar]
- Porter, D.A.; Barnes, A.F.; Rund, A.; Walrod, M.T. Injury Pattern in Ligamentous Lisfranc Injuries in Competitive Athletes. Foot Ankle Int. 2019, 40, 185–194. [Google Scholar] [CrossRef]
- Faciszewski, T.; Burks, R.T.; Manaster, B.J. Subtle injuries of the Lisfranc joint. J. Bone Joint Surg. Am. 1990, 72, 1519–1522. [Google Scholar] [CrossRef]
- Sripanich, Y.; Weinberg, M.W.; Krähenbühl, N.; Rungprai, C.; Mills, M.K.; Saltzman, C.L.; Barg, A. Imaging in Lisfranc injury: A systematic literature review. Skeletal Radiol. 2020, 49, 31–53. [Google Scholar] [CrossRef]
| Control | HV | p Value | |
|---|---|---|---|
| Patients (N) | 46 | 101 | |
| Age | 57.50 (51.8–65.0) | 57.00 (37.0–66.5) | 0.887 |
| Sex | 0.203 | ||
| Female | 32 (69.6%) | 80 (79.2%) | |
| Male | 14 (30.4%) | 21 (20.8%) | |
| Feet (N) | 61 | 146 | |
| Side | 0.693 | ||
| Right | 27 (44.3%) | 69 (47.3%) | |
| Left | 34 (55.7%) | 77 (52.7%) | |
| HVA (degrees) | <0.001 ** | ||
| ≤15 | 61 (100.0%) | 0 (0.0%) | |
| >15 | 0 (0.0%) | 146 (100.0%) |
| M1-2 Distance | ||
|---|---|---|
| rs | p Value | |
| HVA | 0.272 | <0.001 ** |
| IMA | 0.171 | 0.014 * |
| MAA4 | 0.574 | <0.001 ** |
| MAA5 | 0.569 | <0.001 ** |
| Modified Engel’s MAA | 0.341 | <0.001 ** |
| N (%) | M1-2 Distance (mm) | p Value | |
|---|---|---|---|
| MAA4 (deg.) | <0.001 ** | ||
| ≤14 | 167 (80.7%) | 1.6 (0.8–2.2) | |
| >14 | 40 (19.3%) | 2.9 (2.3–3.4) | |
| MAA5 (deg.) | <0.001 ** | ||
| ≤20 | 157 (75.8%) | 1.5 (0.8–2.2) | |
| >20 | 50 (24.2%) | 2.8 (2.2–3.3) | |
| Modified Engel’s MMA (deg.) | <0.001 ** | ||
| ≤24 | 169 (81.6%) | 1.6 (0.8–2.3) | |
| >24 | 38 (18.4%) | 2.7 (1.8–3.0) |
| Normal | Mild | Moderate | Severe | p Value | |
|---|---|---|---|---|---|
| M1-2 distance (mm) | 1.5 ± 0.8 | 1.8 ± 1.5 | 2.0 ± 1.0 | 2.3 ± 0.9 | 0.001 ** |
| MAA4 (deg.) | 8.81 ± 5.19 | 10.11 ± 4.27 | 10.80 ± 4.31 | 11.67 ± 6.46 | 0.026 * |
| MAA5 (deg.) | 15.45 ± 6.25 | 16.77 ± 4.09 | 17.75 ± 5.15 | 18.92 ± 5.70 | 0.028 * |
| Modified Engel’s MAA (deg.) | 14.92 ± 5.71 | 18.27 ± 5.26 | 19.93 ± 5.71 | 20.74 ± 6.77 | <0.001 ** |
| ICC | 95% CI | p Value | |
|---|---|---|---|
| Lower–Upper | |||
| Intra-observer | 0.966 | (0.937–0.982) | <0.001 ** |
| Inter-observer | 0.988 | (0.977–0.994) | <0.001 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, S.-P.; Shih, C.-M.; Wu, Y.-H.; Chen, Y.-S. Radiographic Assessment of Transverse Tarsometatarsal Instability Complicated by Metatarsus Adductus in Hallux Valgus Patients. Life 2024, 14, 718. https://doi.org/10.3390/life14060718
Wang S-P, Shih C-M, Wu Y-H, Chen Y-S. Radiographic Assessment of Transverse Tarsometatarsal Instability Complicated by Metatarsus Adductus in Hallux Valgus Patients. Life. 2024; 14(6):718. https://doi.org/10.3390/life14060718
Chicago/Turabian StyleWang, Shun-Ping, Cheng-Min Shih, Yu-Hsien Wu, and Yuan-Shao Chen. 2024. "Radiographic Assessment of Transverse Tarsometatarsal Instability Complicated by Metatarsus Adductus in Hallux Valgus Patients" Life 14, no. 6: 718. https://doi.org/10.3390/life14060718
APA StyleWang, S.-P., Shih, C.-M., Wu, Y.-H., & Chen, Y.-S. (2024). Radiographic Assessment of Transverse Tarsometatarsal Instability Complicated by Metatarsus Adductus in Hallux Valgus Patients. Life, 14(6), 718. https://doi.org/10.3390/life14060718






