Agreement between Ultra-Short-Term and Standard Heart Rate Variability Analysis in Resting and Post-Exercise Conditions
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Experimental Protocols
2.3. Data Collection
2.4. Statistical Analysis
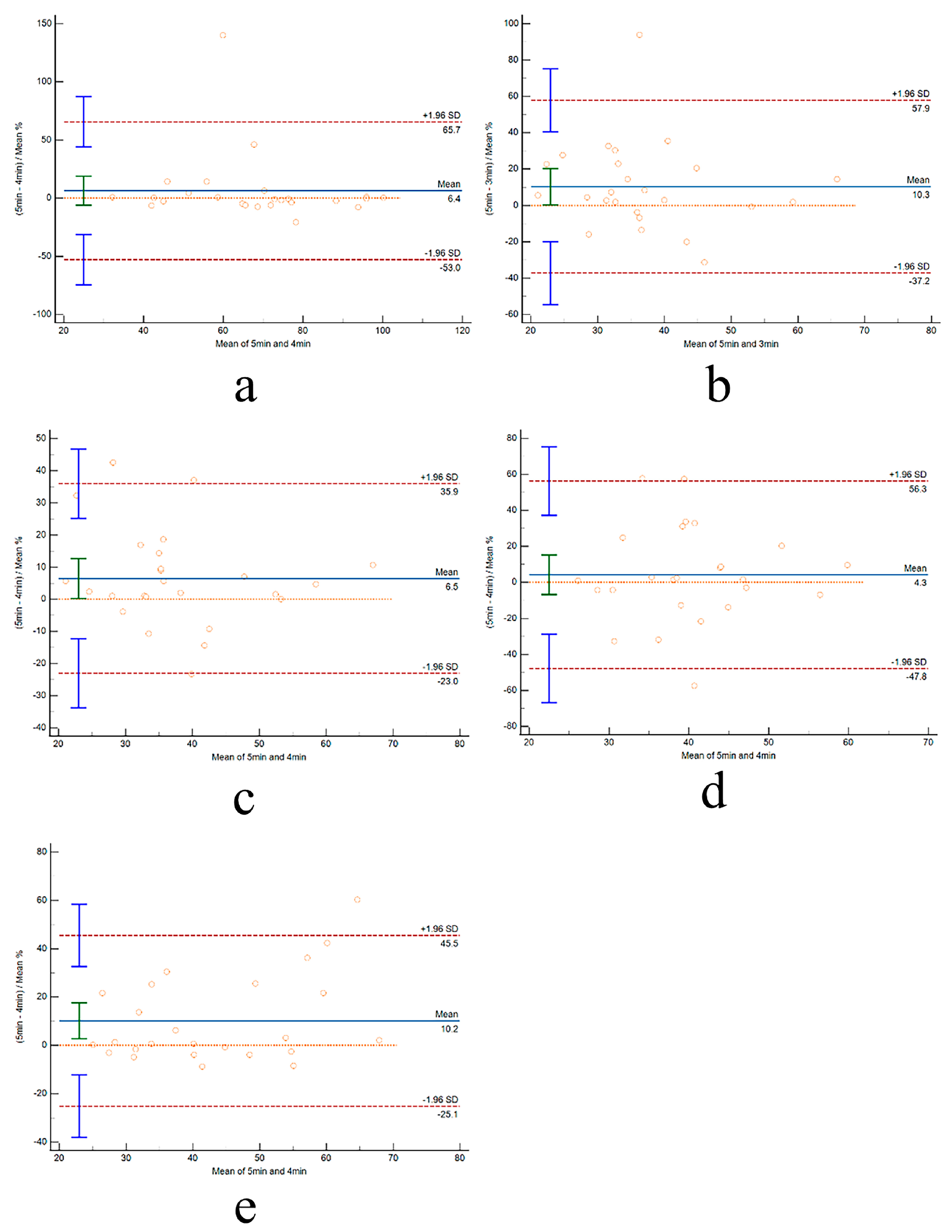
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mejía-Mejía, E.; Budidha, K.; Abay, T.Y.; May, J.M.; Kyriacou, P.A. Heart Rate Variability (HRV) and Pulse Rate Variability (PRV) for the Assessment of Autonomic Responses. Front. Physiol. 2020, 11, 779. [Google Scholar] [CrossRef] [PubMed]
- Hayıroğlu, M.; Çinier, G.; Yüksel, G.; Pay, L.; Durak, F.; Çınar, T.; İnan, D.; Parsova, K.E.; Vatanoğlu, E.G.; Şeker, M.; et al. Effect of a mobile application and smart devices on heart rate variability in diabetic patients with high cardiovascular risk: A sub-study of the LIGHT randomized clinical trial. Kardiol. Pol. 2021, 79, 1239–1244. [Google Scholar] [CrossRef] [PubMed]
- Asarcikli, L.D.; Hayiroglu, M.; Osken, A.; Keskin, K.; Kolak, Z.; Aksu, T. Heart rate variability and cardiac autonomic functions in post-COVID period. J. Interv. Card. Electrophysiol. 2022, 63, 715–721. [Google Scholar] [CrossRef] [PubMed]
- Marasingha-Arachchige, S.U.; Rubio-Arias, J.; Alcaraz, P.E.; Chung, L.H. Factors that affect heart rate variability following acute resistance exercise: A systematic review and meta-analysis. J. Sport. Health Sci. 2022, 11, 376–392. [Google Scholar] [CrossRef] [PubMed]
- Nunan, D.; Sandercock, G.R.; Brodie, D.A. A quantitative systematic review of normal values for short-term heart rate variability in healthy adults. Pacing Clin. Electrophysiol. 2010, 33, 1407–1417. [Google Scholar] [CrossRef] [PubMed]
- Uhlig, S.; Meylan, A.; Rudolph, U. Reliability of short-term measurements of heart rate variability: Findings from a longitudinal study. Biol. Psychol. 2020, 154, 107905. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, F.; Meehan, Z.M.; Zerr, C.L. A Critical Review of Ultra-Short-Term Heart Rate Variability Norms Research. Front. Neurosci. 2020, 14, 594880. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public. Health 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed]
- Volpes, G.; Barà, C.; Busacca, A.; Stivala, S.; Javorka, M.; Faes, L.; Pernice, R. Feasibility of Ultra-Short-Term Analysis of Heart Rate and Systolic Arterial Pressure Variability at Rest and during Stress via Time-Domain and Entropy-Based Measures. Sensors 2022, 22, 9149. [Google Scholar] [CrossRef] [PubMed]
- Burma, J.S.; Graver, S.; Miutz, L.N.; Macaulay, A.; Copeland, P.V.; Smirl, J.D. The validity and reliability of ultra-short-term heart rate variability parameters and the influence of physiological covariates. J. Appl. Physiol. (1985) 2021, 130, 1848–1867. [Google Scholar] [CrossRef] [PubMed]
- Canino, M.C.; Dunn-Lewis, C.; Proessl, F.; LaGoy, A.D.; Hougland, J.R.; Beck, A.L.; Vaughan, G.P.; Sterczala, A.J.; Connaboy, C.; Kraemer, W.J.; et al. Finding a rhythm: Relating ultra-short-term heart rate variability measures in healthy young adults during rest, exercise, and recovery. Auton. Neurosci. 2022, 239, 102953. [Google Scholar] [CrossRef] [PubMed]
- Tarvainen, M.P.; Niskanen, J.P.; Lipponen, J.A.; Ranta-Aho, P.O.; Karjalainen, P.A. Kubios HRV--heart rate variability analysis software. Comput. Methods Programs Biomed. 2014, 113, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Laborde, S.; Mosley, E.; Thayer, J.F. Heart Rate Variability and Cardiac Vagal Tone in Psychophysiological Research—Recommendations for Experiment Planning, Data Analysis, and Data Reporting. Front. Psychol. 2017, 8, 213. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Jiao, Y.; Du, C.; Zhang, X.; Chen, X.; Xu, F.; Jiang, C. Driver Stress Detection Using Ultra-Short-Term HRV Analysis under Real World Driving Conditions. Entropy 2023, 25, 194. [Google Scholar] [CrossRef] [PubMed]
- Thayer, J.F.; Ahs, F.; Fredrikson, M.; Sollers, J.J., 3rd; Wager, T.D. A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health. Neurosci. Biobehav. Rev. 2012, 36, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Hwang, H.B.; Park, S.; Kim, S.; Ha, J.H.; Jang, Y.; Hwang, S.; Park, H.K.; Lee, J.; Kim, I.Y. Mental Stress Assessment Using Ultra Short Term HRV Analysis Based on Non-Linear Method. Biosensors 2022, 12, 465. [Google Scholar] [CrossRef] [PubMed]
- Castaldo, R.; Montesinos, L.; Melillo, P.; James, C.; Pecchia, L. Ultra-short term HRV features as surrogates of short term HRV: A case study on mental stress detection in real life. BMC Med. Inform. Decis. Mak. 2019, 19, 12. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.S.; Pagaduan, J.C.; Bezerra, P.; Crowley-McHattan, Z.J.; Kuo, C.D.; Clemente, F.M. Agreement of Ultra-Short-Term Heart Rate Variability Recordings During Overseas Training Camps in Under-20 National Futsal Players. Front. Psychol. 2021, 12, 621399. [Google Scholar] [CrossRef] [PubMed]
- McKay, A.K.A.; Stellingwerff, T.; Smith, E.S.; Martin, D.T.; Mujika, I.; Goosey-Tolfrey, V.L.; Sheppard, J.; Burke, L.M. Defining Training and Performance Caliber: A Participant Classification Framework. Int. J. Sports Physiol. Perform. 2022, 17, 317–331. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Munoz, M.L.; van Roon, A.; Riese, H.; Thio, C.; Oostenbroek, E.; Westrik, I.; de Geus, E.J.; Gansevoort, R.; Lefrandt, J.; Nolte, I.M.; et al. Validity of (Ultra-)Short Recordings for Heart Rate Variability Measurements. PLoS ONE 2015, 10, e0138921. [Google Scholar] [CrossRef] [PubMed]
- Pecchia, L.; Castaldo, R.; Montesinos, L.; Melillo, P. Are ultra-short heart rate variability features good surrogates of short-term ones? State-of-the-art review and recommendations. Healthc. Technol. Lett. 2018, 5, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Yao, R.; Yin, G.; Li, J. Consecutive ultra-short-term heart rate variability to track dynamic changes in autonomic nervous system during and after exercise. Physiol. Meas. 2017, 38, 1384–1395. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Shi, P.; Yu, H.; Liu, Y. An optimization study of the ultra-short period for HRV analysis at rest and post-exercise. J. Electrocardiol. 2020, 63, 57–63. [Google Scholar] [CrossRef] [PubMed]
- De Vito, G.; Galloway, S.D.; Nimmo, M.A.; Maas, P.; McMurray, J.J. Effects of central sympathetic inhibition on heart rate variability during steady-state exercise in healthy humans. Clin. Physiol. Funct. Imaging 2002, 22, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Pham, T.; Lau, Z.J.; Chen, S.H.A.; Makowski, D. Heart Rate Variability in Psychology: A Review of HRV Indices and an Analysis Tutorial. Sensors 2021, 21, 3998. [Google Scholar] [CrossRef] [PubMed]
- Okutucu, S.; Karakulak, U.N.; Aytemir, K.; Oto, A. Heart rate recovery: A practical clinical indicator of abnormal cardiac autonomic function. Expert. Rev. Cardiovasc. Ther. 2011, 9, 1417–1430. [Google Scholar] [CrossRef] [PubMed]
- Tulppo, M.P.; Kiviniemi, A.M.; Hautala, A.J.; Kallio, M.; Seppänen, T.; Tiinanen, S.; Mäkikallio, T.H.; Huikuri, H.V. Sympatho-vagal interaction in the recovery phase of exercise. Clin. Physiol. Funct. Imaging 2011, 31, 272–281. [Google Scholar] [CrossRef] [PubMed]
- Hayıroğlu, M.; Altay, S. The Role of Artificial Intelligence in Coronary Artery Disease and Atrial Fibrillation. Balkan Med. J. 2023, 40, 151–152. [Google Scholar] [CrossRef] [PubMed]


| Age (Years) | Height (cm) | Weight (kg) | BMI (kg/m2) | HR (beats/s) |
|---|---|---|---|---|
| 22.63 ± 1.53 | 179.42 ± 5.23 | 73.41 ± 5.64 | 22.80 ± 0.59 | 61.67 ± 4.20 |
| 3 min | 4 min | 5 min | |
|---|---|---|---|
| RMSSD | |||
| Pre-E | 41.3 ± 16.8 | 41.0 ± 16.1 | 40.5 ± 15.2 |
| Post-E1 | 17.5 ± 9.8 * | 18.1 ± 10.1 | 18.7 ± 10.5 |
| Post-E2 | 20.6 ± 10.3 | 21.1 ± 11.1 | 21.6 ± 11.6 |
| Post-E3 | 19.6 ± 9.5 | 20.3 ± 10.1 | 20.5 ± 10.5 |
| SDNN | |||
| Pre-E | 63.7 ± 20.0 | 63.8 ± 19.6 | 65.9 ± 18.8 |
| Post-E1 | 39.8 ± 16.6 * | 43.0 ± 16.4 * | 46.7 ± 17.1 |
| Post-E2 | 42.8 ± 15.3 | 44.3 ± 18.6 | 44.3 ± 18.6 |
| Post-E3 | 43.8 ± 16.0 | 46.0 ± 18.2 | 49.6 ± 19.6 |
| 3 min | 4 min | |
|---|---|---|
| RMSSD | ||
| Pre-E | 0.98 | 0.99 |
| Post-E1 | 0.98 | 0.99 |
| Post-E2 | 0.98 | 0.99 |
| Post-E3 | 0.98 | 0.99 |
| SDNN | ||
| Pre-E | 0.86 | 0.89 |
| Post-E1 | 0.96 | 0.97 |
| Post-E2 | 0.95 | 0.99 |
| Post-E3 | 0.90 | 0.92 |
| 3 min | 4 min | |
|---|---|---|
| RMSSD | ||
| Pre-E | −0.05 | −0.03 |
| Post-E1 | −0.12 | −0.06 |
| Post-E2 | −0.09 | −0.04 |
| Post-E3 | −0.09 | −0.02 |
| SDNN | ||
| Pre-E | −0.12 | −0.11 |
| Post-E1 | −0.41 * | −0.28 * |
| Post-E2 | −0.09 | −0.01 |
| Post-E3 | −0.29 * | −0.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, K.; Guo, Z.; Qiao, Z.; Liu, M.; Yang, Y.; Xu, C. Agreement between Ultra-Short-Term and Standard Heart Rate Variability Analysis in Resting and Post-Exercise Conditions. Life 2024, 14, 837. https://doi.org/10.3390/life14070837
Jin K, Guo Z, Qiao Z, Liu M, Yang Y, Xu C. Agreement between Ultra-Short-Term and Standard Heart Rate Variability Analysis in Resting and Post-Exercise Conditions. Life. 2024; 14(7):837. https://doi.org/10.3390/life14070837
Chicago/Turabian StyleJin, Kai, Zhenxiang Guo, Zining Qiao, Meng Liu, Yi Yang, and Changnan Xu. 2024. "Agreement between Ultra-Short-Term and Standard Heart Rate Variability Analysis in Resting and Post-Exercise Conditions" Life 14, no. 7: 837. https://doi.org/10.3390/life14070837
APA StyleJin, K., Guo, Z., Qiao, Z., Liu, M., Yang, Y., & Xu, C. (2024). Agreement between Ultra-Short-Term and Standard Heart Rate Variability Analysis in Resting and Post-Exercise Conditions. Life, 14(7), 837. https://doi.org/10.3390/life14070837





