Establishing the Diagnostic Reference Levels for Common Dubai Health Adult Nuclear Medicine Examinations
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Survey Sample
3.2. CT Acquisition Parameters
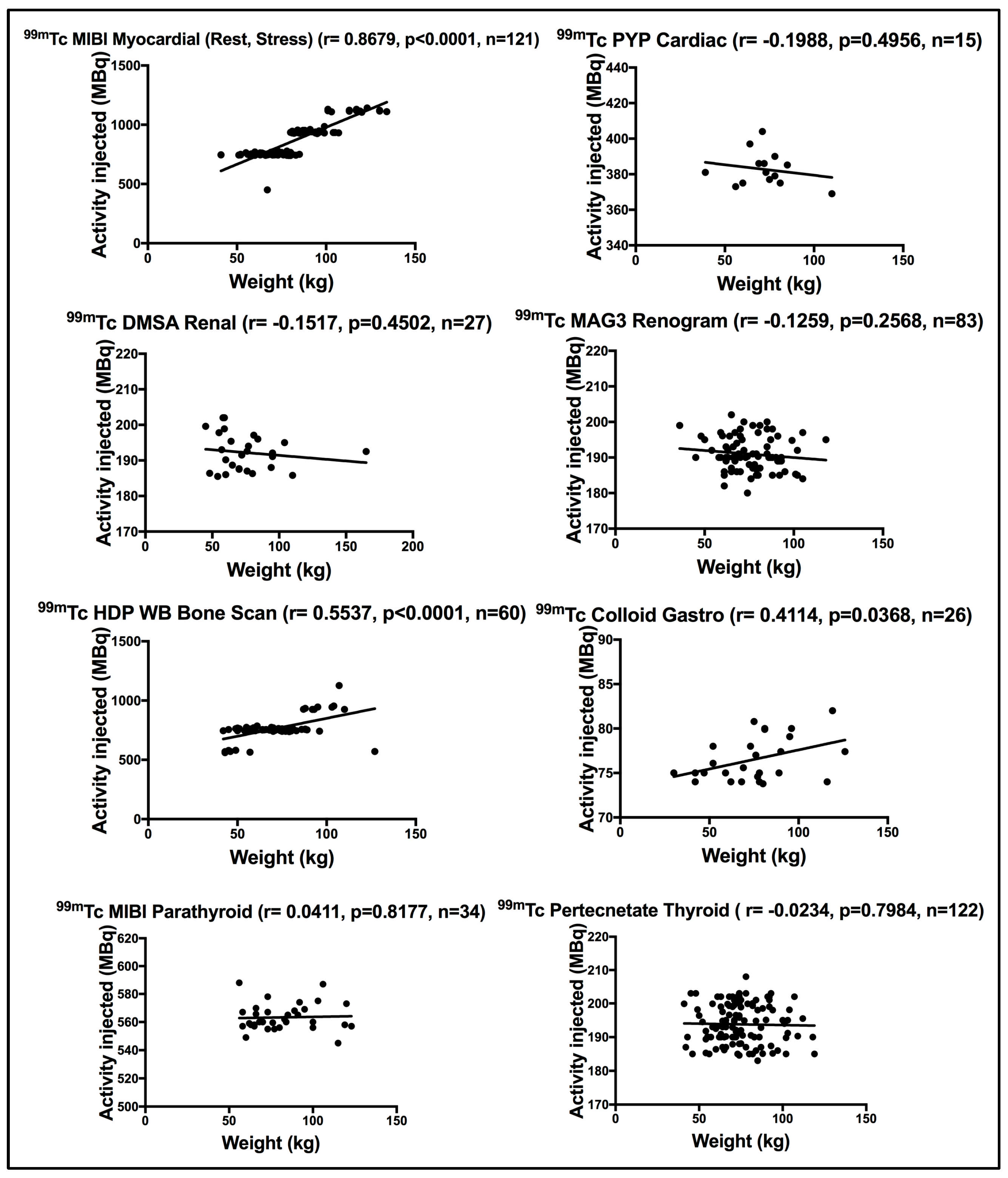
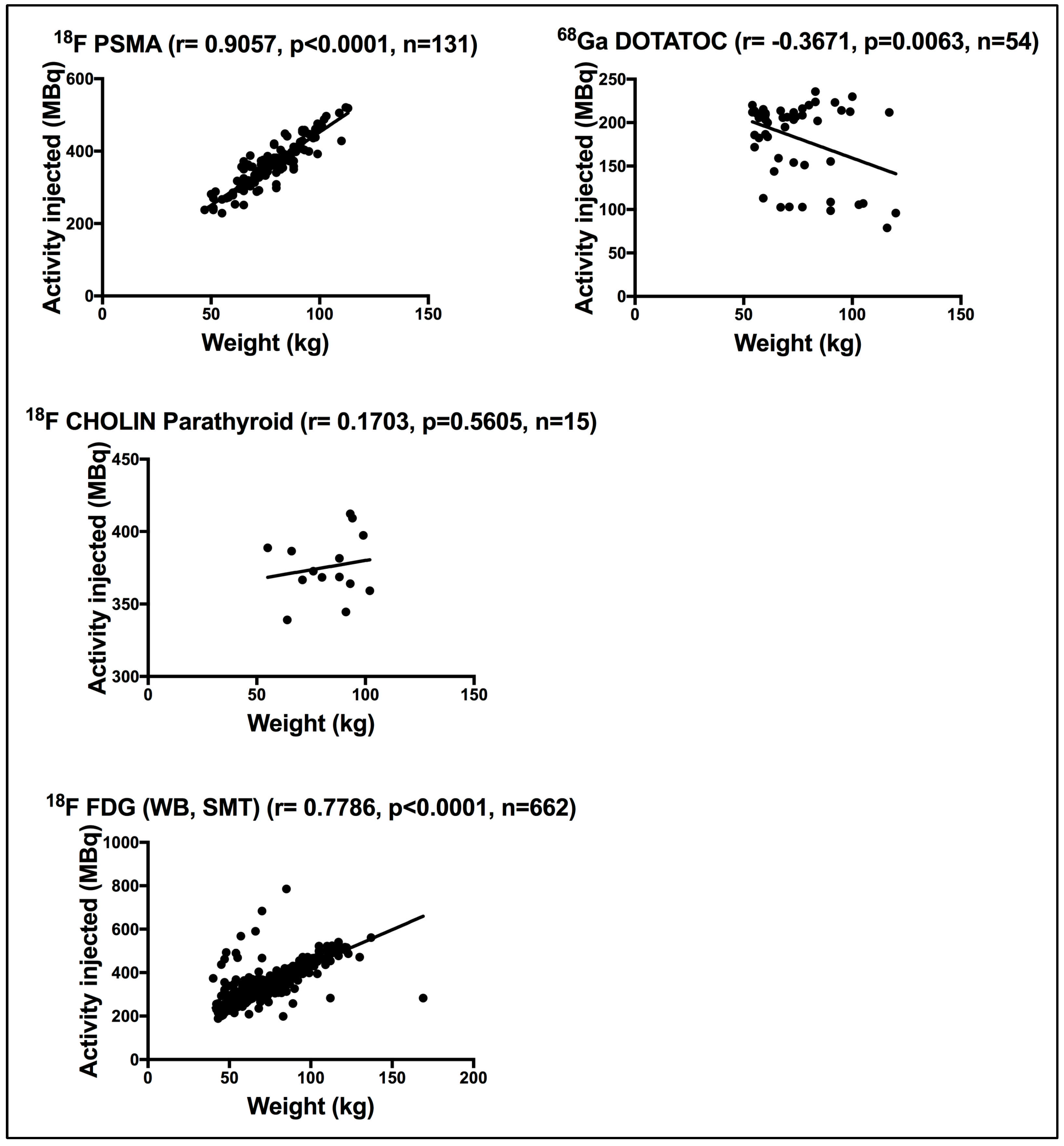
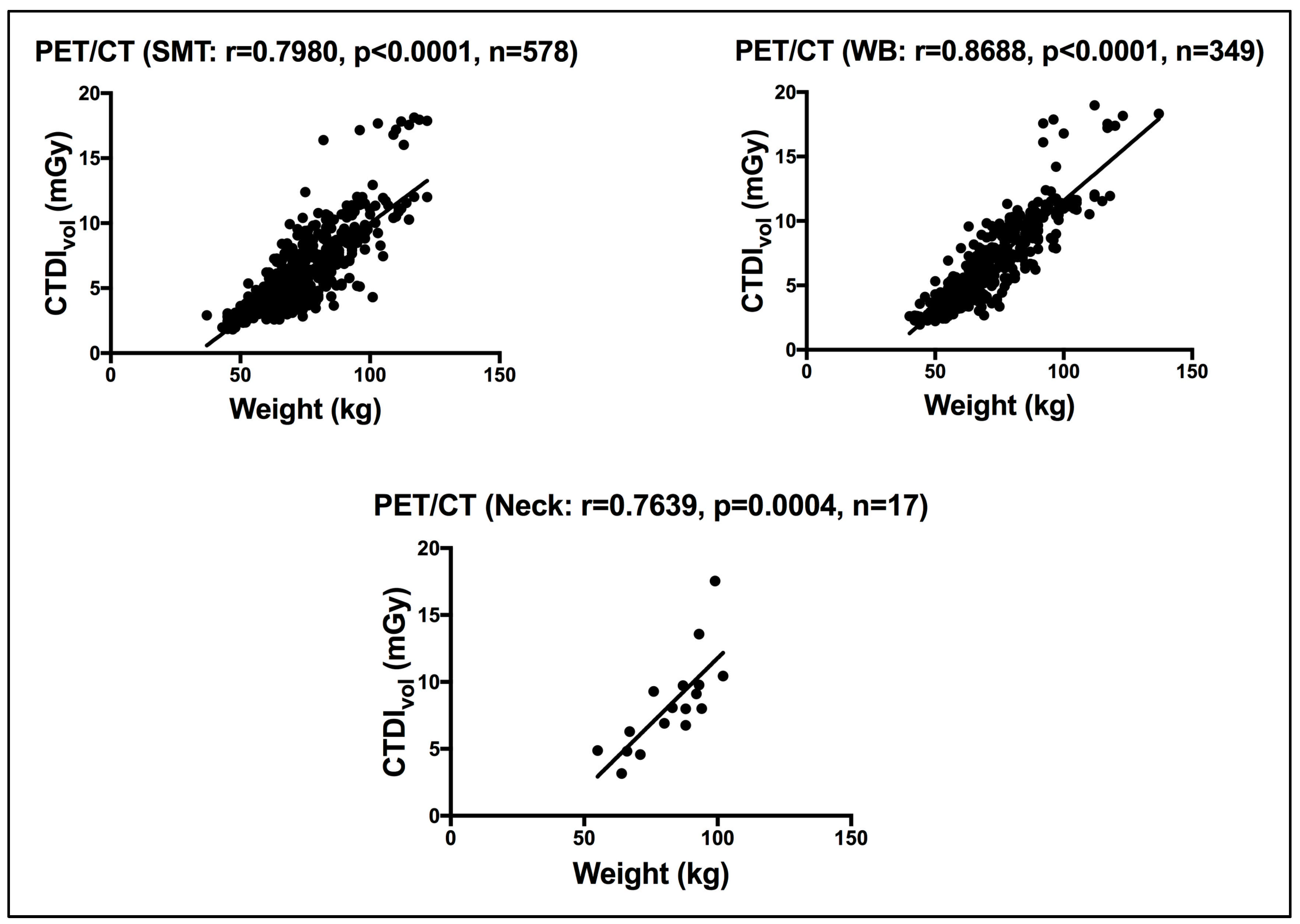
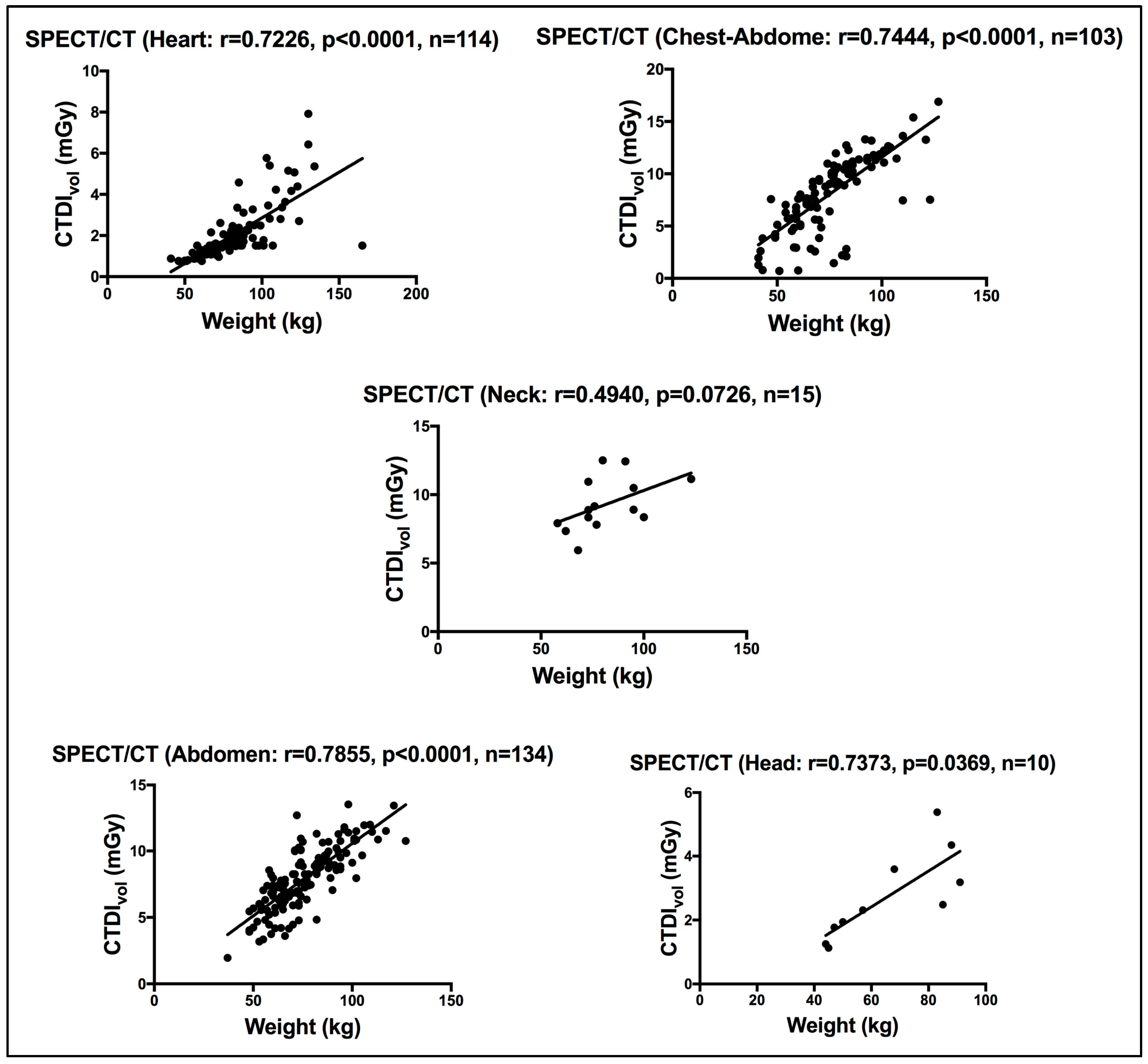
3.3. Weight Impact
3.3.1. Scintigraphy Procedures
3.3.2. PET Procedures
3.4. CTDIvol of the Hybrid CTs
3.5. Diagnostic Reference Levels, DRLs
3.5.1. DRLs for the Administered Activity for Scintigraphy and PET Procedures
3.5.2. DRLs for CTDIvol and DLP in the Hybrid CT Scans
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NM | (nuclear medicine) |
| DRL | (diagnostic reference level) |
| CT | (computed tomography) |
| PET | (positron emission tomography) |
| SPECT | (single-photon emission tomography) |
| 18F | (Fluorine-18) |
| 18F PSMA | (18F-prostate-specific membrane antigen) |
| ICRP | (International Commission on Radiological Protection) |
| IAEA | (International Atomic Energy Agency) |
| WHO | (World Health Organization) |
| UAE | (United Arab Emirates) |
| FANR | (Federal Authority for Nuclear Regulation) |
| CTDIvol | (volume Computed Tomography Dose Index) |
| DLP | (Dose Length Product) |
| iNDRLs | (initial National DRLs) |
| DSREC | (Dubai Scientific Research Ethics Committee) |
| DOSE TQM | (Electronic patient radiation dose monitoring and tracking system) |
| GE | (General Electric) |
| DICOM | (Digital imaging and communication in medicine) |
| Tc-99m | (Technetium- 99m) |
| HDP | (Hydroxydiphosphonate) |
| MIBI | (Methoxyisobutylisonitrile) |
| DMSA | (Dimercaptosuccinic Acid) |
| MAG3 | (Mercaptoacetyltriglycine) |
| PYP | (Pyrophosphate) |
| FDG | (fluorodeoxyglucose) |
| WB | (whole body) |
| SMT | (skull to mid-thigh) |
| 68Ga | (Gallium-68) |
| DOTATOC | (Edotreotide (USAN, also known as (DOTA0-Phe1-Tyr3) octreotide, a somatostatin receptor targeted ligand) |
| kVp | (Peak kilovoltage) |
| mAs | (tube current) |
| AC | (attenuation correction) |
| L | (localization) |
| Bq | (Becquerel) |
| MBq | (MegaBecquerel) |
| mGy | (Milligray) |
References
- ICRP 26. International Commission on Radiological Protection (ICRP). Recommendations of the International Commission on Radiological Protection. ICRP publication 26. Ann. ICRP 1977, 1, 1–80. [Google Scholar]
- Hung, H.T.; Tuyen, P.N.; Tai, D.T.; Long, H.Q.; Sulieman, A.; Omer, H.; Tamam, N.; Almujally, A.; Ghow, J.; Lee, T.Y. Assessment of radiation exposure in a nuclear medicine department of an oncology hospital. J. Radiat. Res. Appl. Sci. 2023, 16, 100564. [Google Scholar] [CrossRef]
- Adelstein, S.J. Radiation risk in nuclear medicine. Semin. Nucl. Med. 2014, 44, 187–192. [Google Scholar] [CrossRef]
- Ribeiro, J.C.; de Mendes, J.D.; de Sa, L.V. Attributable patient risk in nuclear medicine procedures and establishment of diagnostic reference levels. J. Appl. Med. Phys. 2023, 24, e13658. [Google Scholar]
- Vañó, E.; Miller, D.L.; Martin, C.J.; Rehani, M.M.; Kang, K.; Rosenstein, M.; Ortiz-López, P.; Mattsson, S.; Padovani, R.; Rogers, A.; et al. ICRP Publication 135: Diagnostic Reference Levels in Medical Imaging. Ann. ICRP 2017, 46, 1–144. [Google Scholar] [CrossRef]
- SSG-46; Radiation Protection and Safety in Medical Uses of Ionizing Radiation. IAEA: Vienna, Austria, 2018; pp. 1–340.
- Lau, L.; Perez, M. Global Initiative on Radiation Safety in Healthcare Settings; Technical Meeting Report; World Health Organization: Geneva, Switzerland, 2008; pp. 1–100. [Google Scholar]
- FANR-RG-007; Regulatory Guide Radiation Safety Version 0. Federal Authority for Nuclear Regulation (FANR): Abu Dhabi, United Arab Emirates, 2012.
- FANR-REG-24; Basic Safety Standards for Facilities and Activities Involving Ionizing Radiation Other Than in Nuclear Facilities Version. Federal Authority for Nuclear Regulation (FANR): Abu Dhabi, United Arab Emirates, 2018.
- FANR 2018; FANR-Initial Guidance. National Diagnostic Reference Levels (NDRLs). FANR: Abu Dhabi, United Arab Emirates, 2018.
- Qaelum N.V. Dose Patient Radiation Dose Monitoring System User Manual 19.02; Qaelum: Leuven, Belgium, 2019; pp. 1–135. [Google Scholar]
- Miller, C.; Filipow, L.; Jackson, S. A review of activity quantification by planar imaging methods. J. Nucl. Med. Technol. 1995, 23, 3–9. [Google Scholar]
- Masoomi, M.; Al-Shammeri, I.; Al-Kandari, L.; Elrahman, H.; Al-Shammeri, J. National diagnostic reference level (DRL) for nuclear medicine computed tomography-positron emission tomography hybrid imaging studies for Kuwait population: Second phase dose aduit-2019. BJR|Open 2021, 3, 20210020. [Google Scholar] [CrossRef]
- Abe, K.; Hosono, M.; Igarashi, T.; Iimori, T.; Ito, T.; Nagahata, T.; Tsushima, H.; Watanabe, H. The 2020 national diagnostic reference levels for nuclear medicine in Japan. Ann. Nucl. Med. 2020, 34, 799–806. [Google Scholar] [CrossRef]
- Alkybari, E.M.; Alhulail, A.A.; Sulieman, A.; Faqeeh, J.M.; Albatly, A.A.; Alqarni, A.O. Deriving local diagnostic reference levels for four common PET/CT procedures in a Saudi Arabian hospital. J. Radiat. Res. Appl. Sci. 2023, 15, 380–385. [Google Scholar] [CrossRef]
- AAPM Task Group 23. The Measurement, Reporting, and Management of Radiation Dose in CT; Report of AAPM Task Group 23; American Association of Physicists in Medicine: New York, NY, USA, 2008. [Google Scholar]
- Bongartz, G.; Golding, S.J.; Jurik, A.G.; Leonardi, M.; van Persijn, E.; Rodriguez, R.; Schneider, K.; Calzado, A.; Geleijns, J.; Jessen, K.A.; et al. European Guidelines for Multisclice Computed Tomography. 2004. Available online: http://www.drs.dk/guidelines/ct/quality/index.htm (accessed on 9 April 2025).
- Fayad, H.; Ahmed, S.; El Khatib, A.; Ghujeh, A.; Aly, A.; Kharita, M.H.; Al-Naemi, H. National diagnostic reference levels for nuclear medicine in Qatar. J. Nucl. Med. Technol. 2023, 51, 63–67. [Google Scholar] [CrossRef]
- Roch, P.; Celier, D.; Dessaud, C.; Etard, C. Patient exposure from nuclear medicine in France: National follow-up and influence of the technology through diagnostic reference levels data analysis. Radiat. Prot. Dosim. 2018, 179, 87–94. [Google Scholar] [CrossRef]
- ARPANSA. Current Australian Diagnostic Reference Levels for Nuclear Medicine. 2023. Available online: https://www.arpansa.gov.au/research-and-expertise/surveys/national-diagnostic-reference-level-service/current-australian-drls/nm#nmct (accessed on 14 January 2025).
- Skovorodko, K.; Komiagiene, R.; Maciusovic, M.; Gilys, L.; Vajauskas, D.; Grigoniene, V.; Ziliukas, J.; Raudoniene, J.; Griciene, B. Nationwide survey or radiation doses received by patients in nuclear medicine imaging procedure. J. Radiol. Prot. 2022, 4, 031507. [Google Scholar] [CrossRef]
- Song, H.C.; Na, M.H.; Kim, J.; Cho, S.G.; Park, J.K.; Kang, K.W. Diagnostic reference levels for adult nuclear medicine imaging established from the national survey in Korea. Nucl. Med. Mol. Imaging 2019, 53, 64–70. [Google Scholar] [CrossRef]
- Health Information and Quality Authority. National Diagnostic Reference Levels (DRLs) for Nuclear Medicine Procedures. Available online: https://www.hiqa.ie/sites/default/files/2023-11/National-diagnostic-reference-levels-(DRLs)-for-nuclear-medicine-procedures.pdf (accessed on 14 January 2025).
- Al Shurbaji, M.; El Haout, S.; Chanchal, A.; Dhou, S.; Dalah, E. Investigating the effect of patient-related factors on computed tomography radiation dose using regression and correlation analysis. Appl. Sci. 2024, 14, 1071. [Google Scholar] [CrossRef]
- Iball, G.R.; Bebbington, N.A.; Burniston, M.; Edyvean, S.; Fraser, L.; Julyan, P.; Parkar, N.; Wood, T. A national survey of computed tomography doses in hybrid PET-CT and SPECT-CT examinations in the UK. Nucl. Med. Commun. 2017, 38, 459–470. [Google Scholar] [CrossRef]
- Bebbington, N.; Haddock, B.T.; Bertilsson, H.; Hippelainen, E.; Husby, E.M.; Tunninen, V.I.; Soderberg, M. A Nordic survey of CT doses in hybrid PET/CT and SPECT/CT examinations. EJNMMI Phys. 2019, 6, 24. [Google Scholar] [CrossRef]
- Alnaaimi, M.; Alduaij, M.A.; Shenawy, F.A.; Algaily, M.M.; Mohammedzein, T.S.; Alkandri, F.A.; Shaban, M.O.; Alenezi, S.A. National diagnostic reference levels for nuclear medicine in Kuwait. J. Nucl. Med. Technol. 2022, 50, 54–59. [Google Scholar] [CrossRef]
- ICRP 105. International Commission on Radiological Protection Radiological protection in medicine. ICRP Publication 105. Ann. ICRP 2007, 37, 1–63. [Google Scholar] [CrossRef]
- ICRP 103. International Commission on Radiological Protection, The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann. ICRP 2007, 37, 1–332. [Google Scholar] [CrossRef]
- Dalah, E.Z.; Al Zarooni, M.M.; Binismail, F.Y.; Beevi, H.A.; Siraj, M.; Pottybindu, S. Typical and local diagnostic reference levels for chest and abdomen radiography examinations in Dubai Health sector. J. Imaging 2025, 11, 21. [Google Scholar] [CrossRef]
- Dalah, E.Z.; AlKaabi, M.K.; Al-Awadhi, H.A.; Antony, N.A. Screening Mammography Diagnostic Reference Level System According to Compressed Breast Thickness: Dubai Health. J. Imaging 2024, 10, 188. [Google Scholar] [CrossRef]
- Damilakis, J.; Frija, G.; Brkljacic, B.; Vano, E.; Loose, R.; Paulo, G.; Brat, H.; Tsapaki, V. How to establish and use local diagnostic reference levels: An ESR EuroSafe imaging expert statement. Insight Imaging 2023, 14, 27. [Google Scholar] [CrossRef]
- Tsapaki, V. Radiation dose optimization in diagnostic and interventional radiology: Current issues and future perspectives. Phys. Med. 2020, 79, 16–21. [Google Scholar] [CrossRef]
- Dalah, E.Z.; Alsuwaidi, J.S.; Hamed, M.S.; Gani, A.A.; Beevi, H.A.; Panangatil, A.G.; Funelar, C.O.; Ferrer, A.Y.; Al Hussein, S.; Albedwawi, S.A. Challenges experienced in establishing clinical indication based diagnostic reference levels: Pilot study. Eur. J. Radiol. 2022, 14, 110046. [Google Scholar] [CrossRef]
- Habibzadeh, M.A.; Ay, M.R.; Asl, A.R.; Ghadiri, H.; Zaidi, H. Impact of miscentering on patient dose and image noise in X-ray CT imaging: Phantom and clinical studies. Phys. Med. 2012, 28, 191–199. [Google Scholar] [CrossRef]
- Mayo-Smith, W.W.; Hara, A.K.; Mahesh, M.; Sahani, D.V.; Pavlicek, W. How I do it: Managing radiation dose in CT. Radiology 2014, 273, 657–672. [Google Scholar] [CrossRef]
- ICRP 52. Protection of the Patient in Nuclear Medicine (and Statement from the 1987 Como Meeting of ICRP). ICRP Publication 52. Ann. ICRP 1987, 17, 1–53. [Google Scholar]
- Australian Government 14.2. Australian Radiation Protection and Nuclear Safety Agency, SAFETY GUIDE, Radiation Protection in Nuclear Medicine Radiation Protection Series Publication No. 14.2. This publication was approved by the Radiation Health Committee on 16 July 2008, and endorsed for publication by the Radiation Health & Safety Advisory Council on 8 August 2008. Available online: https://www.arpansa.gov.au/regulation-and-licensing/regulatory-publications/radiation-protection-series/guides-and-recommendations/rps14-2 (accessed on 9 April 2025).
- Alkhybari, E.; McEntee, M.F.; Brennan, P.C.; Willowson, K.P.; Kench, P.L. Diagnostic reference levels for 18F-FDG whole body PET/CT procedures: Results from a survey of 12 centres in Australia and New Zealand. J. Med. Imaging Radiat. Oncol. 2019, 63, 291–299. [Google Scholar] [CrossRef]
- European Union. European Guidelines on Diagnostic Reference Levels for Paediatric Imaging; Radiation Protection N 185; European Union: Belgium, Brussels, 2018. [Google Scholar]
| Study | kV | Smart mA | Rotation Time (s) | Pitch | Slice Thickness (mm) | Speed (mm/Rotation) | Total Exposure Time (s) | Detector Rows |
|---|---|---|---|---|---|---|---|---|
| Neck | 120 | 20–440 | 0.5 | 1.375 | 5.0 | 13.75 | 15.34 | 16 |
| Head | 120 | 20–440 | 0.5 | 1.350 | 5.0 | 13.50 | 15.63 | 8 |
| Heart | 120 | 10–440 | 0.8 | 0.938 | 5.0 | 18.75 | 18.47 | 16 |
| Abdomen/Chest-Abdomen | 120 | 20–440 | 0.5 | 1.375 | 5.0 | 27.50 | 7.91 | 16 |
| Study | kV | Smart mA | Rotation Time (s) | Pitch | Slice Thickness (mm) | Speed (mm/Rotation) | Total Exposure Time (s) | Detector Rows |
|---|---|---|---|---|---|---|---|---|
| SMT | 120–140 | 30–300 | 0.8 | 1.375 | 5.0 | 55.0 | 15.11 | 40 |
| WB | 120–140 | 30–300 | 0.8 | 1.375 | 5.0 | 55.0 | 27.10 | 40 |
| Head and Neck | 120 | 30–300 | 0.8 | 0.984 | 3.75 | 39.37 | - | 40 |
| Procedure and Radiopharmaceutical | Scan Acquisition | Age, Year (Minimum–Maximum) | Weight, kg | Sample Size | Activity Injected, MBq | International References, MBq | |
|---|---|---|---|---|---|---|---|
| Median (DRL) | 75TH PER | ||||||
| Myocardial (Rest or Stress) and 99mTc MIBI | SPECT | 28–90 | 41–134 + | 121 | 767 | 940 | 926 Qatar [18], 650 France [19], 600 Australia [20], 750: rest, 550: stress Lithuania [21] |
| 60–80 | 56 | 752 | 761 | 880 Japan [14], | |||
| Cardiac and 99mTc PYP | PLANAR+SPECT | 27–87 | 39–110 - | 15 | 381 | 388 | 800 Japan [14], |
| Bone scan and 99mTc HDP | PLANAR+SPECT ++ | 15–77 | 42–127 * | 60 | 755 | 767 | 740 Qatar [18], 925 Korea [22], 670 France [19], 900 Australia [20], 950 Japan [14], 658 Irish [23], |
| Gastro Emptying and 99mTc Colloid | PLANAR | 24–86 | 30–126 * | 26 | 75 | 78 | 36 Qatar [18], 111 Korea [22], 40 Australia [20], |
| Renal (static scan) and 99mTc DMSA | PLANAR *** | 16–87 | 45–165 - | 27 | 192 | 196 | 101 Qatar [19], 185 Korea [22], 210 Japan [14], 84 [Irish [23], |
| Renogram (dynamic scan) and 99mTc MAG3 | PLANAR | 16–82 | 36–118 - | 84 | 190 | 195 | 189 Qatar [18], 500 Korea [22], 180 France [19], 300 Australia [20], 380 Japan [14], 105 Irish [23], 100 Lithuania [21] |
| Thyroid Imaging and 99mTc Pertechnetate | PLANAR | 15–78 | 41–119 ** | 128 | 193 | 200 | 195 Qatar [18], 217 Korea [22], 110 France [19], 200 Australia [20], 300 Japan [14], 100 Irish [22], |
| Parathyroid and 99mTc MIBI | PLANAR+SPECT ++ | 31–87 | 56–123 ** | 34 | 560 | 568 | 384 Qatar [18], 740 Korea [22], 800 Australia [20], 800 Japan [14], 740 Irish [23], 740 Lithuania [21] |
| Procedure and Radiopharmaceutical | Age, Year (Minimum–Maximum) | Weight, kg | Sample Size | Activity Injected, MBq | International References, MBq | |
|---|---|---|---|---|---|---|
| Median (DRL) | 75TH PER | |||||
| Oncology (whole body, WB/skull- to mid-thigh, SMT) and 18F FDG | 16–92 | 40–169 + | 662 | 343 | 381 | 258 Qatar [18], 370 Korea [22], 260 France [19], 270 Australia [20], 334 Australia [22], 500 Lithuania [21] |
| 60–80 | 339 | 334 | 358 | 368 Irish [23], 307 Saudi Aribia [15] | ||
| Oncology (Prostate) and 18F PSMA | 44–99 | 47–113 + | 131 | 363 | 499 | - |
| 60–80 | 65 | 341 | 362 | 184 Saudi Aribia [15] | ||
| Endocrine and 68Ga DOTATOC | 15–74 | 54–120 - | 54 | 206 | 212 | 200 Australia [20], 172 Saudi Aribia [15] |
| Parathyroid and 18F CHOLIN | 27–95 | 55–102 - | 18 | 369 | 391 | - |
| Target Body Part/Purpose of Use | Weight, kg | Sample Size | CTDIvol, mGy | DLP, mGy.cm | International References | |||
|---|---|---|---|---|---|---|---|---|
| Median (DRL) | 75TH PER | Median (DRL) | 75TH PER | CTDIvol, mGy | DLP, mGy.cm | |||
| Neck/AC and L | 58–123 ** | 14 | 8.90 | 11.00 | 380 | 451 | 5.80 - Japan [14], 7.2 Australia [20], 5.90 UK [24], 5.46 Irish [22], 5.9 [26], 4.5 - Kuwait [27] | 210 - Japan [14], 240 Australia [20], 210 UK [24], 124 Irish [22], 199 [26], 181 - Kuwait [27] |
| Head/AC and L | 44–91 ** | 10 | 2.40 | 3.78 | 96 | 158 | - | - |
| Heart/AC and L | 41–165 | 114 | 1.57 | 2.36 | 42 | 60 | - | - |
| 60–80 | 49 | 1.47 | 1.60 | 35 | 47 | 4.50 Japan [14], 2.2 [26], 2.1 UK [24], 4.26 Qatar [18] | 180 Japan [14], 53 [26], 36 UK [24], 104 Qatar [18] | |
| Abdomen/AC and L | 37–127 | 134 | 7.82 | 9.71 | 500 | 716 | 5.00 Japan [14] | 210 Japan [14] |
| 60–80 | 61 | 7.20 | 8.11 | 438 | 600 | - | - | |
| Chest-Abdomen/AC and L | 41–127 | 103 | 8.77 | 10.84 | 641 | 860 | 4.10 * Japan [14] | 170 * Japan [14] |
| 60–80 | 44 | 8.10 | 9.51 | 631 | 775 | 4.86 Qatar [18] | 211 Qatar [18] | |
| Target Body Part/Purpose of Use | Weight, kg | Sample Size | CTDIvol, mGy | DLP, mGy.cm | International References | |||
|---|---|---|---|---|---|---|---|---|
| Median (DRL) | 75TH PER | Median (DRL) | 75TH PER | CTDIvol, mGy | DLP, mGy.cm | |||
| Neck, AC and L | 55–102 ** | 17 | 8.00 | 9.75 | 676 | 805 | - | - |
| Whole body, WB/AC and L | 40–137 | 349 | 6.35 | 9.26 | 748 | 1070 | - | - |
| 60–80 | 171 | 6.11 | 7.36 | 700 | 892 | 6.1 Japan [14], 5.7 Irish [23], 4.1 Kuwait [13], 2.9 [26] | 600 Japan [14], 665 Irish [23], 684 Kuwait [13], 310 [26] | |
| Skull to mid-thigh, SMT/AC and L | 37–122 | 578 | 5.73 | 8.0 | 660 | 948 | - | - |
| 60–80 | 298 | 5.11 | 6.40 | 561 | 766 | 4.20 and 5.3 Australia [20], 5.30 Qatar [18] | 430 and 555 Australia [20], 548 Qatar [18] | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dalah, E.Z.; Al Mazrouei, N.K.; Al Ali, Z.A. Establishing the Diagnostic Reference Levels for Common Dubai Health Adult Nuclear Medicine Examinations. Life 2025, 15, 649. https://doi.org/10.3390/life15040649
Dalah EZ, Al Mazrouei NK, Al Ali ZA. Establishing the Diagnostic Reference Levels for Common Dubai Health Adult Nuclear Medicine Examinations. Life. 2025; 15(4):649. https://doi.org/10.3390/life15040649
Chicago/Turabian StyleDalah, Entesar Z., Najlaa K. Al Mazrouei, and Zahra A. Al Ali. 2025. "Establishing the Diagnostic Reference Levels for Common Dubai Health Adult Nuclear Medicine Examinations" Life 15, no. 4: 649. https://doi.org/10.3390/life15040649
APA StyleDalah, E. Z., Al Mazrouei, N. K., & Al Ali, Z. A. (2025). Establishing the Diagnostic Reference Levels for Common Dubai Health Adult Nuclear Medicine Examinations. Life, 15(4), 649. https://doi.org/10.3390/life15040649





