Reducing the Breast Cancer Risk and Radiation Dose of Radiography for Scoliosis in Children: A Phantom Study
Abstract
1. Introduction
2. Materials and Methods
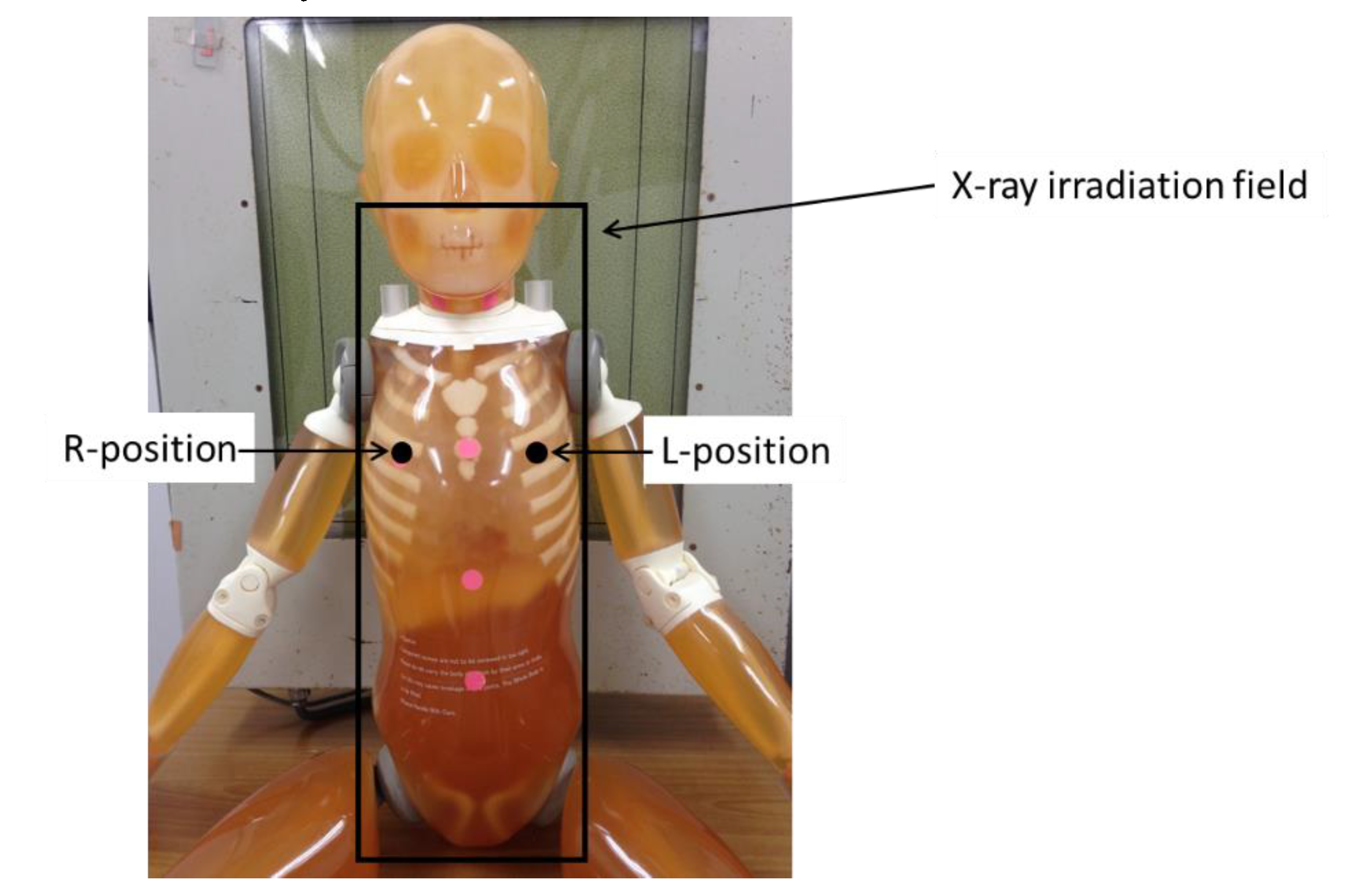
2.1. Evaluation of BSDs during FRs
2.2. Calculation of the Effective Doses of FRs Using the Monte Carlo Method
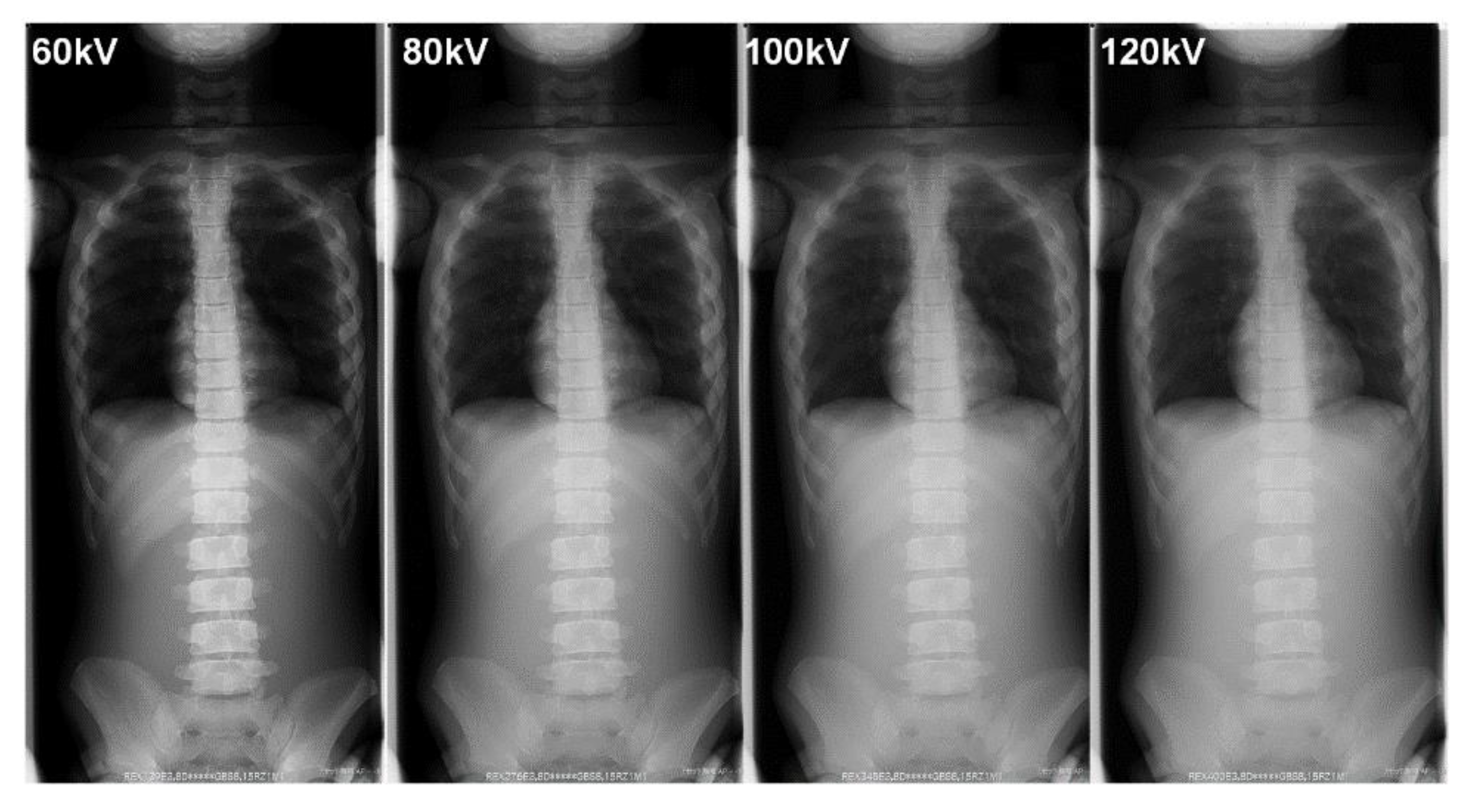
3. Results
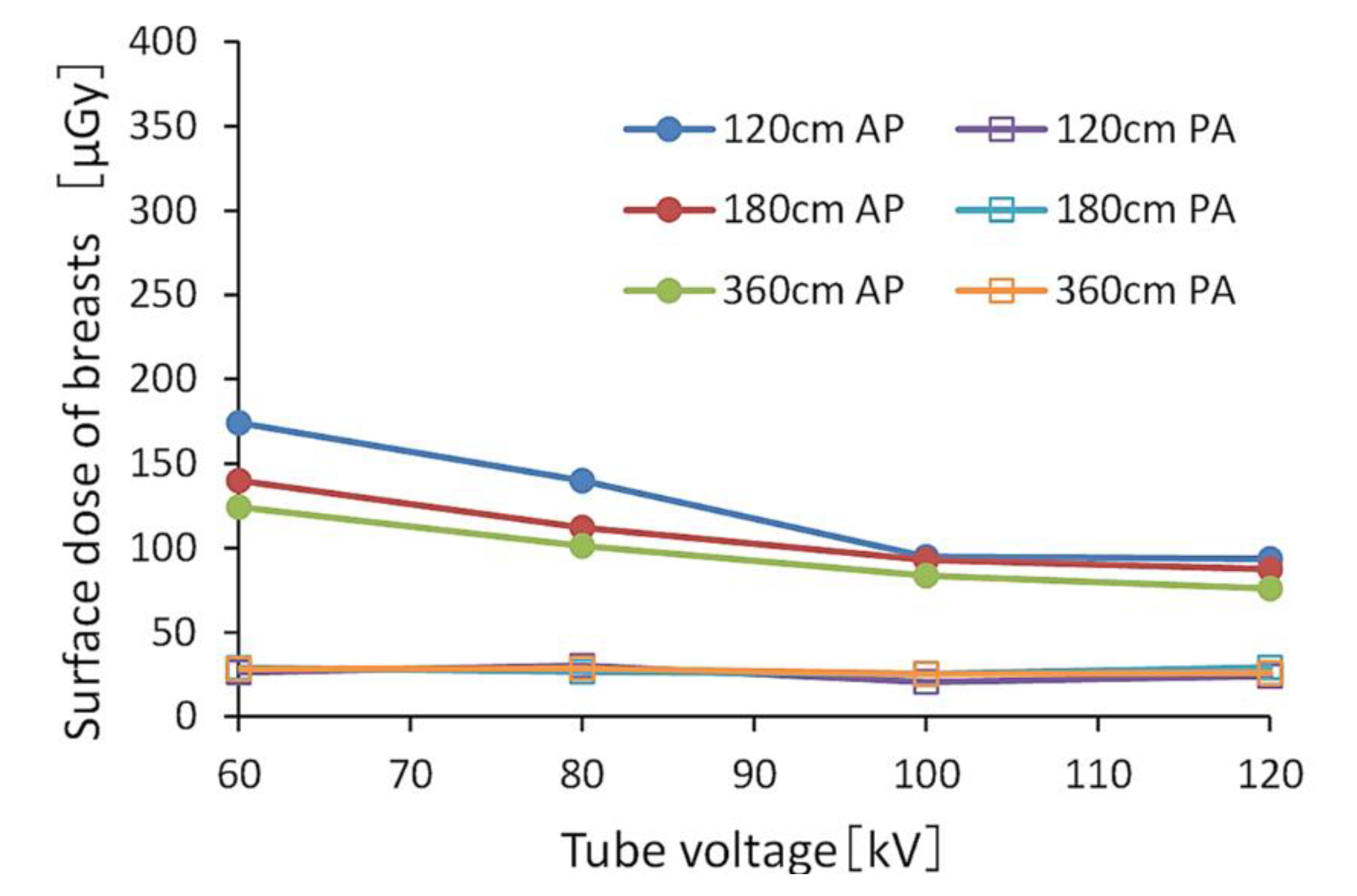
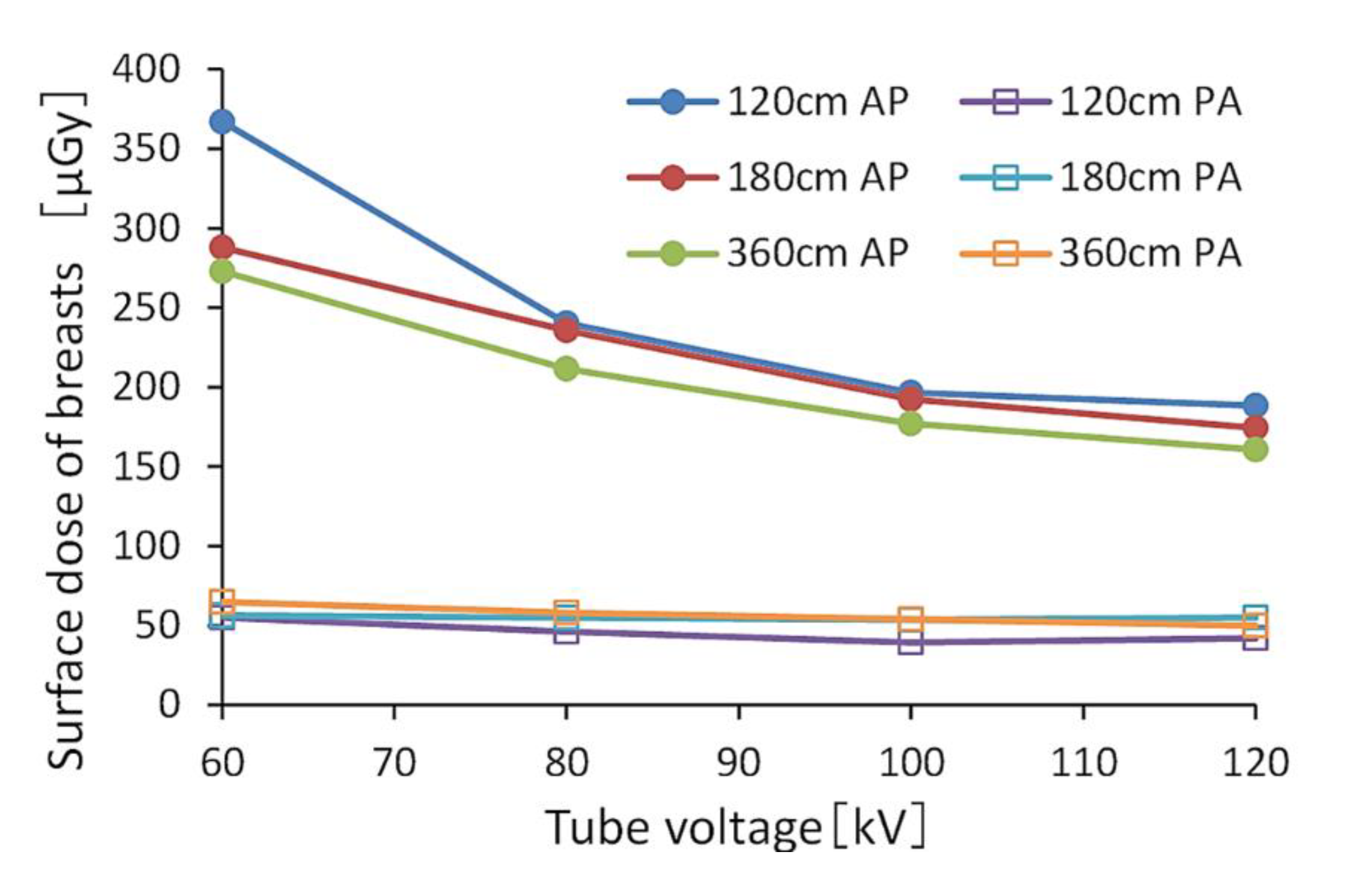
3.1. BSDs during FRs
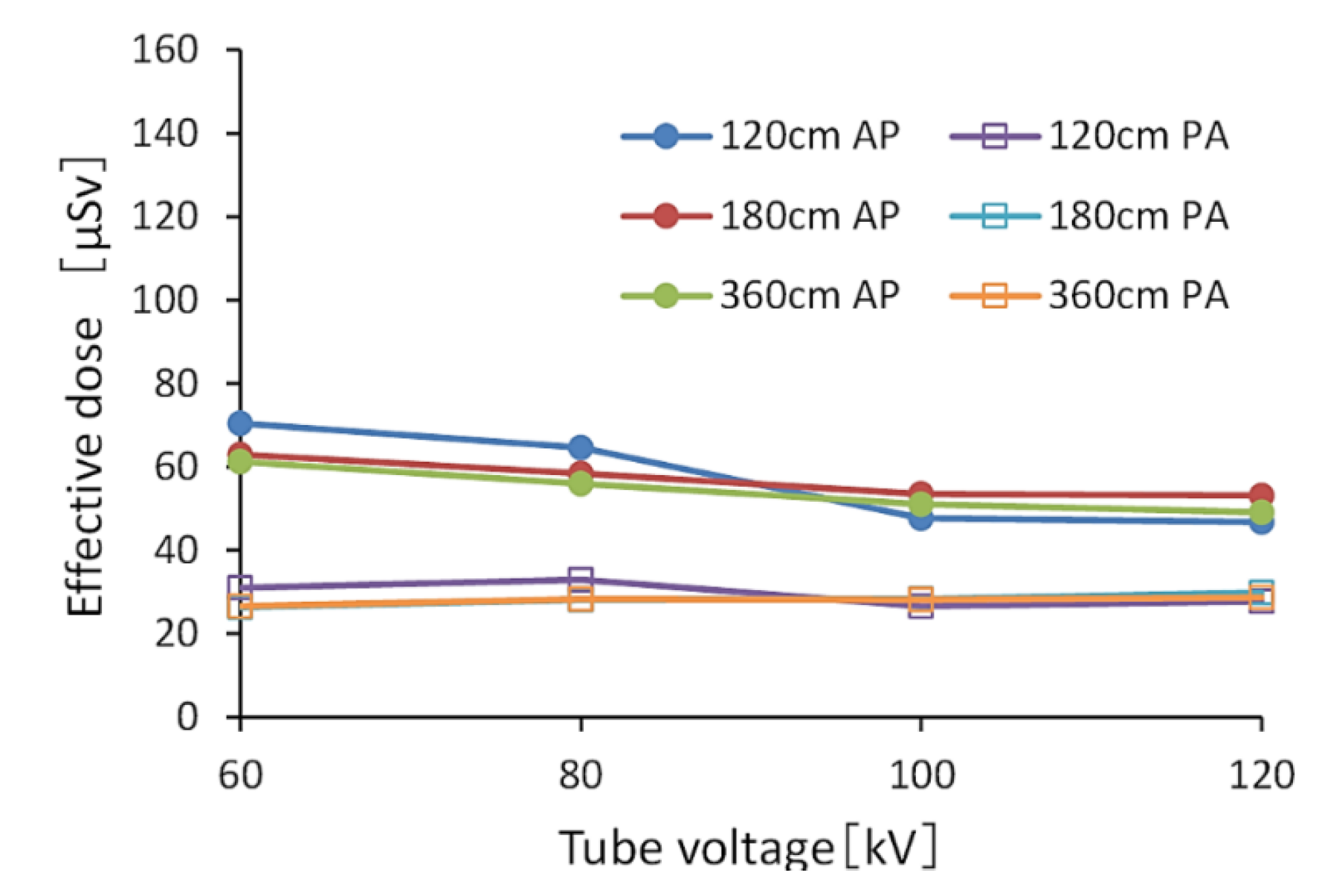
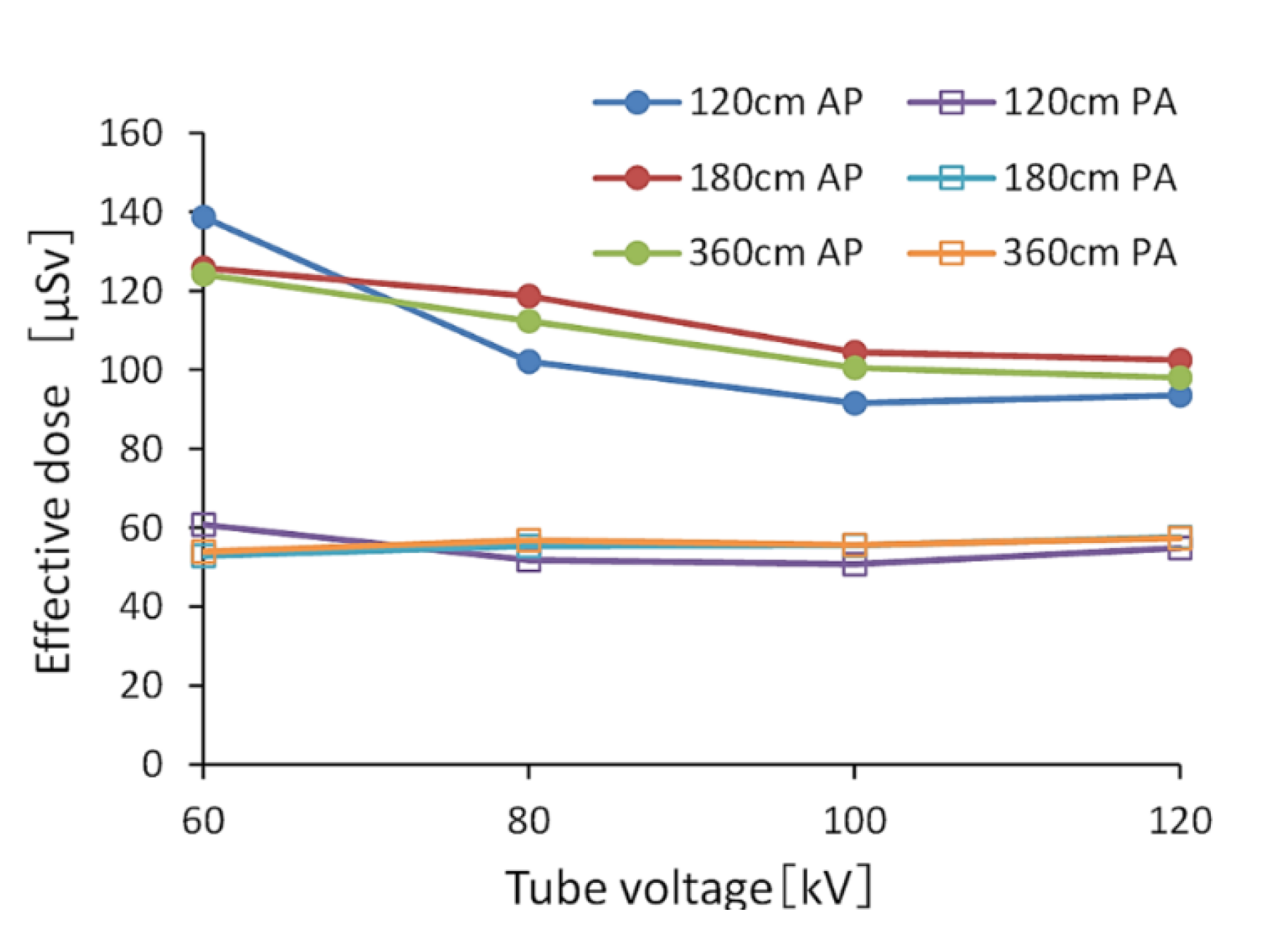
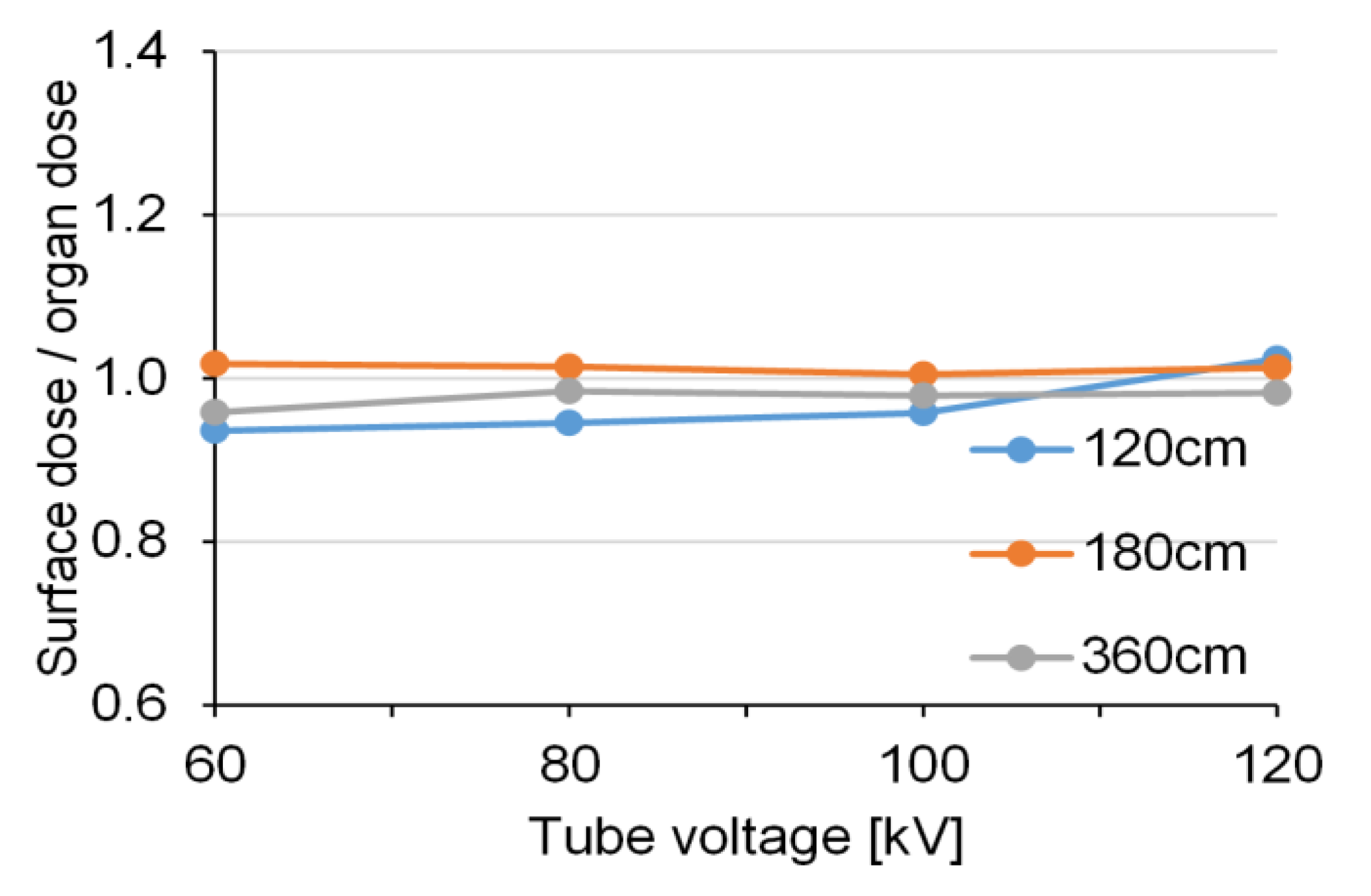
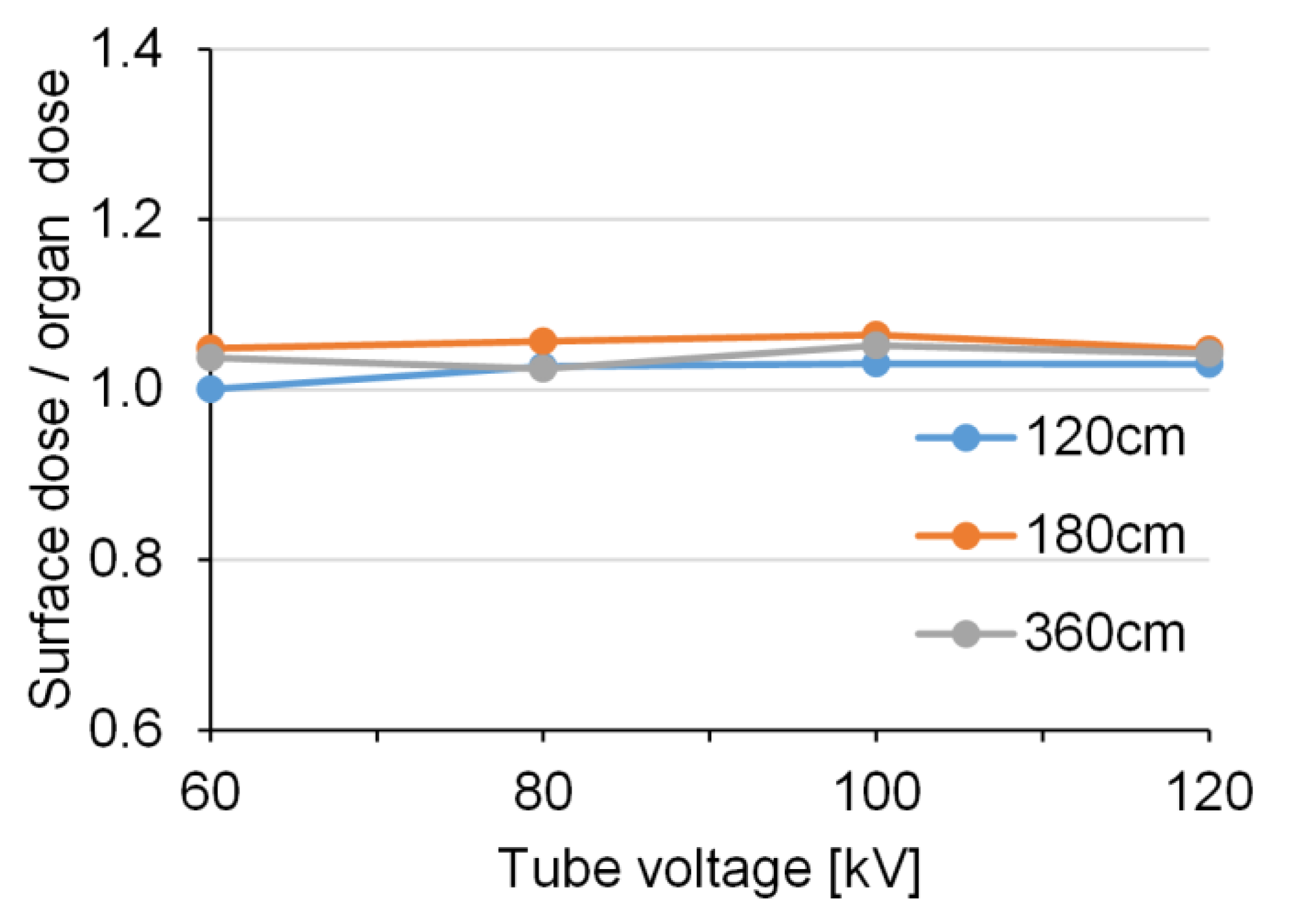
3.2. Effective Doses during FRs Using PMC Based on the Monte Carlo Method
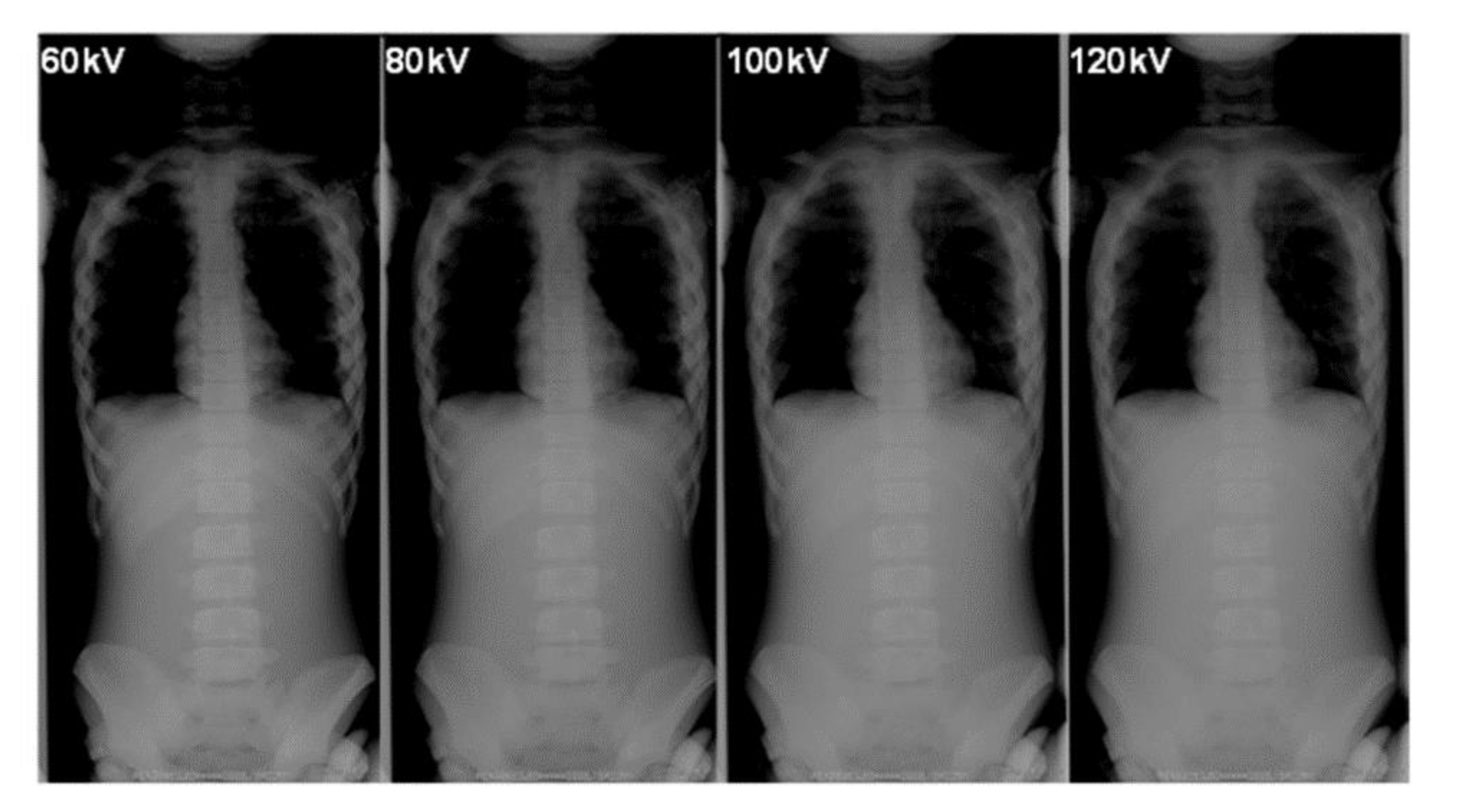
4. Discussion
Limitation
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chida, K.; Kaga, Y.; Haga, Y.; Kataoka, N.; Kumasaka, E.; Meguro, T.; Zuguchi, M. Occupational Eye Dose in Interventional Cadiology Procedures. Am. J. Roentgenol. 2013, 200, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Chida, K.; Inaba, Y.; Masuyama, H.; Yanagawa, I.; Mori, I.; Saito, H.; Maruoka, S.; Zuguchi, M. Evaluating the Performance of a MOSFET Dosimeter at Diagnostic X-ray Energies for Interventional Radiology. Radiol. Phys. Technol. 2009, 2, 58–61. [Google Scholar] [CrossRef] [PubMed]
- Chida, K.; Inaba, Y.; Masuyama, H.; Yanagawa, I.; Mori, I.; Saito, H.; Maruoka, S.; Zuguchi, M. Comparison of Dose at an Interventional Reference Point Between the Displayed Estimated Value and Measured Value. Radiol. Phys. Technol. 2011, 4, 189–193. [Google Scholar] [CrossRef]
- Morishima, Y.; Chida, K.; Watanabe, H. Estimation of the Dose of Radiation Received by Patient and Physician During a Videofluoroscopic Swallowing Study. Dysphagia 2016, 31, 574–578. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, N.; Abdul Karim, M.K.; Abu Hassan, H.; Ahmad Kamarudin, M.; Ding Wong, J.H.; Ng, K.H. Diagnostic Reference Level of Radiation Dose and Image Quality among Paediatric CT Examinations in a Tertiary Hospital in Malaysia. Diagnostics 2020, 10, 591. [Google Scholar] [CrossRef]
- Chida, K.; Saito, H.; Otani, H.; Kohzuki, M.; Takahashi, S.; Yamada, S.; Shirato, K.; Zuguchi, M. Relationship between Fluoroscopic Time, Dose-Area Product, Body Weight, and Maximum Radiation Skin Dose in Cardiac Interventional Procedure. Am. J. Roentgenol. 2006, 186, 774–778. [Google Scholar] [CrossRef]
- Chida, K.; Inaba, Y.; Saito, H.; Ishibashi, T.; Takahashi, S.; Kohzuki, M.; Zuguchi, M. Radiation Dose of Interventional Radiology System Using a Flat-Panel Detector. Am. J. Roentgenol. 2009, 193, 1680–1685. [Google Scholar] [CrossRef]
- Chida, K.; Kato, M.; Inaba, Y.; Kobayashi, R.; Nakamura, M.; Abe, Y.; Zuguchi, M. Real-Time Patient Radiation Dosimeter for Use in Interventional Radiology. Phys. Med. 2016, 32, 1475–1478. [Google Scholar] [CrossRef]
- Inaba, Y.; Kobayashi, R.; Chida, K.; Zuguchi, M. Effectiveness of a Novel Real-Time Dosimeter in Interventional Radiology: A Comparison of New and Old Radiation Sensors. Radiol. Phys. Technol. 2018, 11, 445–450. [Google Scholar] [CrossRef]
- Kato, M.; Chida, K.; Nakamura, M.; Toyoshima, H.; Terata, K.; Abe, Y. New Real-Time Patient Radiation Dosimeter for Use in Radiofrequency Catheter Ablation. J. Radiat. Res. 2019, 60, 215–220. [Google Scholar] [CrossRef]
- Inaba, Y.; Nakamura, M.; Zuguchi, M.; Chida, K. Development of Novel Real-Time Radiation Systems Using 4-Channel Sensors. Sensors 2020, 20, 2741. [Google Scholar] [CrossRef] [PubMed]
- American College of Radiology (ACR) and the Society for Pediatric Radiology (SPR). Practice Parameter for the Performance of Radiography for Scoliosis in Children: Acr Practice Guideline Scoliosis; Resolution 32: Reston, VA, USA, 2009. [Google Scholar]
- Doody, M.M.; Lonstein, J.E.; Stovall, M.; Hacker, D.G.; Luckyanov, N.; Land, C.E. Breast Cancer Mortality After Diagnostic Radiography: Findings From the U.S. Scoliosis Cohort Study. Spine 2000, 25, 2052–2063. [Google Scholar] [CrossRef] [PubMed]
- Almén, A.J.; Mattsson, S. Dose distribution at radiographic examination of the spine in pediatric radiology. Spine 1996, 21, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Hallen, S.; Martling, K.; Mattsson, S. Dosimetry at X-ray examination of scoliosis. Radiat. Prot. Dosim. 1992, 43, 49–54. [Google Scholar] [CrossRef]
- Hoffman, D.A.; Lonstein, J.E.; Morin, M.M.; Visscher, W.; Harris, B.S., III; Boice, J.D., Jr. Breast cancer in women with scoliosis exposed to multiple diagnostic X-rays. J. Nat. Cancer Inst. 1989, 81, 1307–1312. [Google Scholar] [CrossRef] [PubMed]
- Bone, C.M.; Hsieh, G.H. The risk of carcinogenesis from radiographs to paediatric orthopaedic patients. J. Pediatr. Orthop. 2000, 20, 251–254. [Google Scholar] [CrossRef]
- Levy, A.R.; Goldberg, M.S.; Mayo, N.E.; Hanley, J.A.; Poitras, B. Reducing the lifetime risk of cancer from spinal radiographs among people with adolescent idiopathic scoliosis. Spine 1996, 21, 1540–1547. [Google Scholar] [CrossRef]
- Gialousis, G.; Yiakoumakis, E.N.; Makri, T.K.; Papadoupoulou, D.; Karlatira, M.; Karaiskos, P.; Papaodysseas, S.; Evlogias, N.; Dimitriou, P.A.; Georgiou, E.K. Comparison of dose from radiological examination for scoliosis in children among two pediatric hospitals by monte carlo simulation. Health Phys. 2008, 94, 471–478. [Google Scholar] [CrossRef]
- Ruiz, M.J.; Gonzalez, L.; Vano, E.; Martinez, A. Measurement of radiation doses in the most frequent simple examinations in pediatric radiology and its dependence on patient age. Br. J. Radiol. 1991, 64, 929–933. [Google Scholar] [CrossRef]
- Gallini, R.E.; Belletti, S.; Berna, V.; Giugni, U. Adult and child doses in standardized X-ray examinations. Radiat Prot. Dosim. 1992, 43, 41–47. [Google Scholar] [CrossRef]
- Gogos, K.A.; Yakoumakis, E.N.; Tsalafoutas, I.A.; Makri, T.K. Radiation dose considerations in common pediatric x-ray examinations. Pediatric Radiol. 2003, 33, 236–240. [Google Scholar] [CrossRef] [PubMed]
- Hensen, J.; Jurik, A.G.; Fiirgaard, B.; Egund, N. Optimisations of scoliosis examination in children. Pediatr. Radiol. 2003, 33, 52–765. [Google Scholar] [CrossRef] [PubMed]
- United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR). Epidemiological Studies of Radiation and Cancer UNSCEAR 2006 Report (Scientific Annex A) Vol. I. UNSCEAR. 2008. Available online: http://www.unscear.org/docs/reports/2006/07-82087_Report_Annex_A_2006_Web_corr.pdf (accessed on 20 September 2020).
- Chida, K.; Kato, M.; Kagaya, Y.; Zuguchi, M.; Saito, H.; Ishibashi, T.; Takahashi, S.; Yamada, S.; Takai, Y. Radiation dose and radiation protection for patients and physicians during interventional procedure. J. Radiat. Res. 2010, 51, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Bacher, K.; Bogaert, E.; Lapere, R.; De Wolf, D.; Thierens, H. Patient-specific dose and radiation risk estimation in pediatric cardiac catheterization. Circulation 2005, 111, 83–89. [Google Scholar] [CrossRef]
- Ideguchi, R.; Yoshida, K.; Ohtsuru, A.; Takamura, N.; Tsuchida, T.; Kimura, H.; Uetani, M.; Kudo, T. The present state of radiation exposure from pediatric CT examinations in Japan-what do we have to do? J. Radiat. Res. 2018, 59 (Suppl. 2), ii130–ii136. [Google Scholar] [CrossRef]
- Chida, K.; Ohno, T.; Kakizaki, S.; Takegawa, M.; Yuuki, H.; Nakada, M.; Takahashi, S.; Zuguchi, M. Radiation Dose to the Pediatric Cardiac Catheterization and Intervention Patient. Am. J. Roentgenol. 2010, 195, 1175–1179. [Google Scholar] [CrossRef] [PubMed]
- Pediatric Whole Body Phantom “PBU-70”, Kyoto Kagaku Co., Ltd. Available online: https://www.kyotokagaku.com/jp/educational/products/detail03/ph-2c.html (accessed on 23 September 2020).
- Seidenbusch, M.; Schneider, K. Conversion coefficients for determining organ doses in paediatric spine radiography. Pediatric Radiol. 2014, 44, 434–456. [Google Scholar] [CrossRef]
- Alrehily, F.; Hogg, P.; Twiste, M.; Johansen, S.; Tootell, A. Scoliosis imaging: An analysis of radiation risk in the CT scan projection radiograph and a comparison with projection radiography and EOS. Radiography 2019, 25, e68–e74. [Google Scholar] [CrossRef]
- Larson, A.N.; Schueler, B.A.; Dubousset, J. Radiation in Spine Deformity: State-of-the-Art Reviews. Spine Deform. 2019, 7, 386–394. [Google Scholar] [CrossRef]
- Chida, K.; Kaga, Y.; Haga, Y.; Takeda, K.; Zuguchi, M. Quality control phantom for flat panel detector X-ray systems. Health Phys. 2013, 104, 97–101. [Google Scholar] [CrossRef]
- Haga, Y.; Chida, K.; Kaga, Y.; Sota, M.; Meguro, T.; Zuguchi, M. Occupational Dose in Interventional Radiology Procedures. Sci. Rep. 2017, 7, 569. [Google Scholar] [CrossRef] [PubMed]
- Inaba, Y.; Chida, K.; Kobayashi, R.; Zuguchi, M. A cross-sectional study of the radiation dose and image quality of X-ray equipment used in IVR. J. Appl. Clin. Med. Phys. 2016, 17, 391–401. [Google Scholar] [CrossRef] [PubMed]
- Chida, K.; Sai, M.; Saito, H.; Takase, K.; Zuguchi, M.; Sasaki, M.; Sato, T. Relationship between the pixel value in digital subtraction angiography and iodine concentration: Study in high iodine concentration with original phantom. Tohoku J. Exp. Med. 2000, 190, 169–176. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shan, H.; Zhang, Y.; Yang, Q.; Kruger, U.; Kalra, M.K.; Sun, L.; Cong, W.; Wang, G. 3-D Convolutional Encoder-Decoder Network for Low-Dose CT via Transfer Learning From a 2-D Trained Network. IEEE Trans. Med. Imaging 2018, 37, 1522–1534. [Google Scholar] [CrossRef] [PubMed]
- Shan, H.; Padole, A.; Homayounieh, F.; Kruger, U. Competitive performance of a modularized deep neural network compared to commercial algorithms for low-dose CT image reconstruction. Nat. Mach. Intell. 2019, 1, 269–276. [Google Scholar] [CrossRef]
- Lee, D.; Choi, S.; Kim, H.J. Performance evaluation of image denoising developed using convolutional denoising autoencoders in chest radiography. In Nuclear Instruments and Methods in Physics Research Section A: Accelerators, Spectrometers, Detectors and Associated Equipment; Elsevier: Amsterdam, The Netherlands, 2018; Volume 884, pp. 97–104. [Google Scholar]
| Focus-Image Receptor Distance (cm) | Tube Voltage (kV) | mAs | Beam Projection | Radiation Field Setting (cm2) | |
|---|---|---|---|---|---|
| Grid (−) | Grid (+) | ||||
| 120 | 60 | 6.4 | 12.6 | AP/PA | 20 × 47 * |
| 80 | 2.4 | 4 | |||
| 100 | 1 | 1.92 | |||
| 120 | 0.63 | 1.28 | |||
| 180 | 60 | 12.6 | 25.2 | AP/PA | 20 × 55 |
| 80 | 5 | 10 | |||
| 100 | 2.56 | 5 | |||
| 120 | 1.6 | 3.2 | |||
| 360 | 60 | 63 | 128 | AP/PA | 20 × 55 |
| 80 | 25 | 50 | |||
| 100 | 12.8 | 25 | |||
| 120 | 8 | 16 | |||
| Patient’s Age (years) | 5 |
| height (cm) | 110 |
| weight (kg) | 20 |
| Anode Angle | 12° |
| Tube Voltage | See Table 1 |
| Total Filtration | 2.8 mm aluminum |
| Monte Carlo Simulation | 107 photon histories |
| Grid (−) | Grid (+) | |||||||
|---|---|---|---|---|---|---|---|---|
| 60 kV | 80 kV | 100 kV | 120 kV | 60 kV | 80 kV | 100 kV | 120 kV | |
| 120 cm | 1.00 | 0.80 | 0.54 | 0.54 | 1.00 | 0.65 | 0.53 | 0.51 |
| 180 cm | 1.00 | 0.80 | 0.66 | 0.63 | 1.00 | 0.82 | 0.67 | 0.61 |
| 360 cm | 1.00 | 0.81 | 0.67 | 0.61 | 1.00 | 0.78 | 0.65 | 0.59 |
| Grid (−) | Grid (+) | |||||
|---|---|---|---|---|---|---|
| 120 cm | 180 cm | 360 cm | 120 cm | 180 cm | 360 cm | |
| 60 kV | 1.00 | 0.80 | 0.71 | 1.00 | 0.78 | 0.74 |
| 80 kV | 1.00 | 0.80 | 0.72 | 1.00 | 0.98 | 0.88 |
| 100 kV | 1.00 | 0.98 | 0.88 | 1.00 | 0.98 | 0.90 |
| 120 kV | 1.00 | 0.94 | 0.81 | 1.00 | 0.93 | 0.85 |
| Technical Parameters | Surface Dose [μGy] | ||
|---|---|---|---|
| Beam Projection | Grid | Tube Voltage [kV] | |
| PA | (−) (+) | 60–120 | 25–50 |
| AP | (−) | 100–120 | 75–95 |
| 60–100 | 95–170 | ||
| (+) | 100–120 | 160–200 | |
| 60–100 | 200–290 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nemoto, M.; Chida, K. Reducing the Breast Cancer Risk and Radiation Dose of Radiography for Scoliosis in Children: A Phantom Study. Diagnostics 2020, 10, 753. https://doi.org/10.3390/diagnostics10100753
Nemoto M, Chida K. Reducing the Breast Cancer Risk and Radiation Dose of Radiography for Scoliosis in Children: A Phantom Study. Diagnostics. 2020; 10(10):753. https://doi.org/10.3390/diagnostics10100753
Chicago/Turabian StyleNemoto, Manami, and Koichi Chida. 2020. "Reducing the Breast Cancer Risk and Radiation Dose of Radiography for Scoliosis in Children: A Phantom Study" Diagnostics 10, no. 10: 753. https://doi.org/10.3390/diagnostics10100753
APA StyleNemoto, M., & Chida, K. (2020). Reducing the Breast Cancer Risk and Radiation Dose of Radiography for Scoliosis in Children: A Phantom Study. Diagnostics, 10(10), 753. https://doi.org/10.3390/diagnostics10100753




