Biopsychosocial Aspects in Individuals with Acute and Chronic Rotator Cuff Related Shoulder Pain: Classification Based on a Decision Tree Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Procedures
2.3. Sociodemographic Aspects
2.4. Biological Aspects Related to General Clinical Health Status
2.5. Biological Aspects Related to Shoulder Clinical Condition
2.6. Biological Aspects Related to Sensory Function
2.6.1. Two-Point Discrimination Threshold (TPDT)
2.6.2. Left/Right Judgment Task (LRJT)
2.6.3. Pressure Pain Threshold (PPT)
2.6.4. Temporal Summation (TS)
2.6.5. Conditioned Pain Modulation
2.7. Psychosocial Aspects
2.8. Statistical Analysis
3. Results
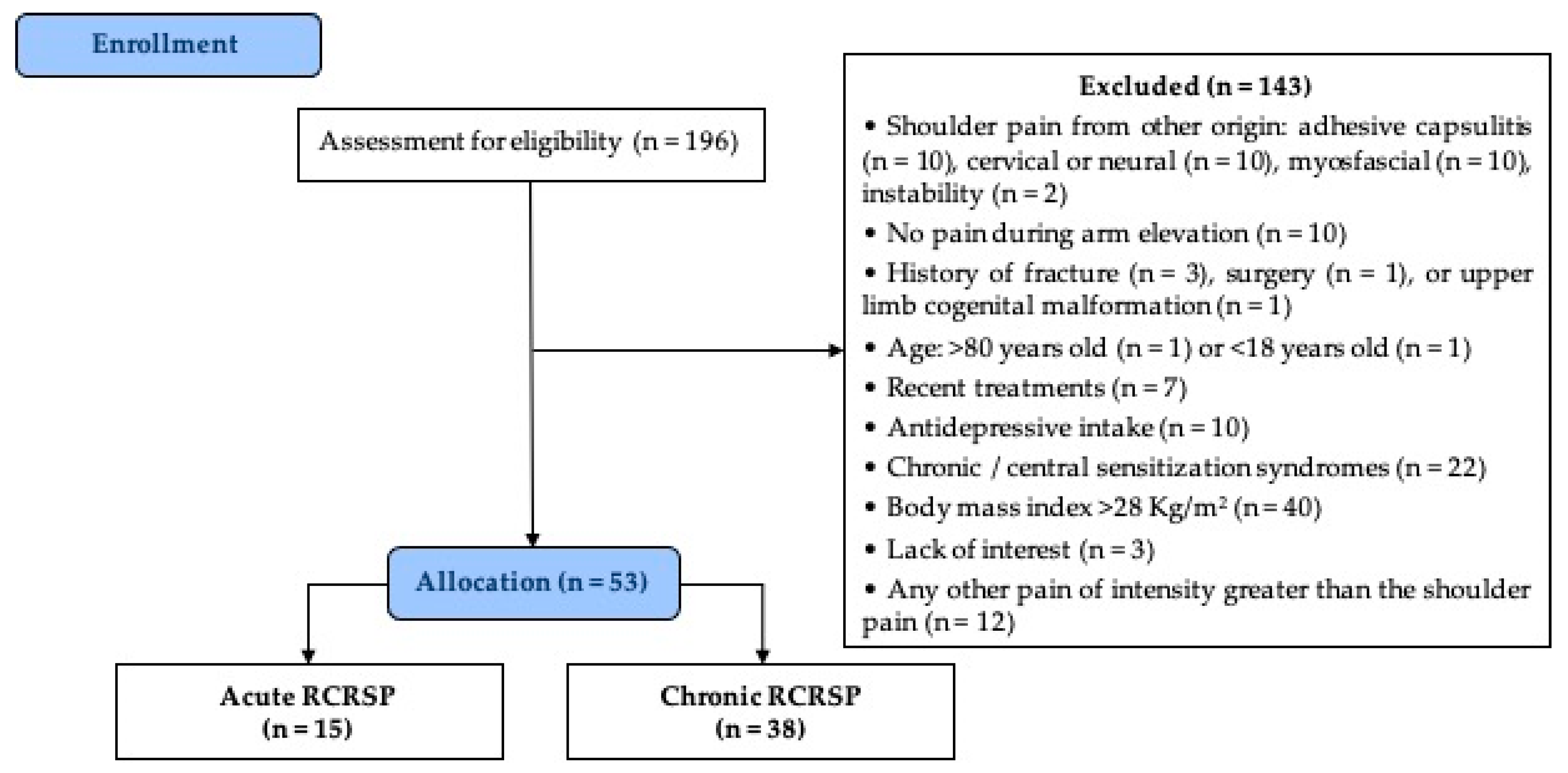
3.1. Study Population
3.2. Population characteristics
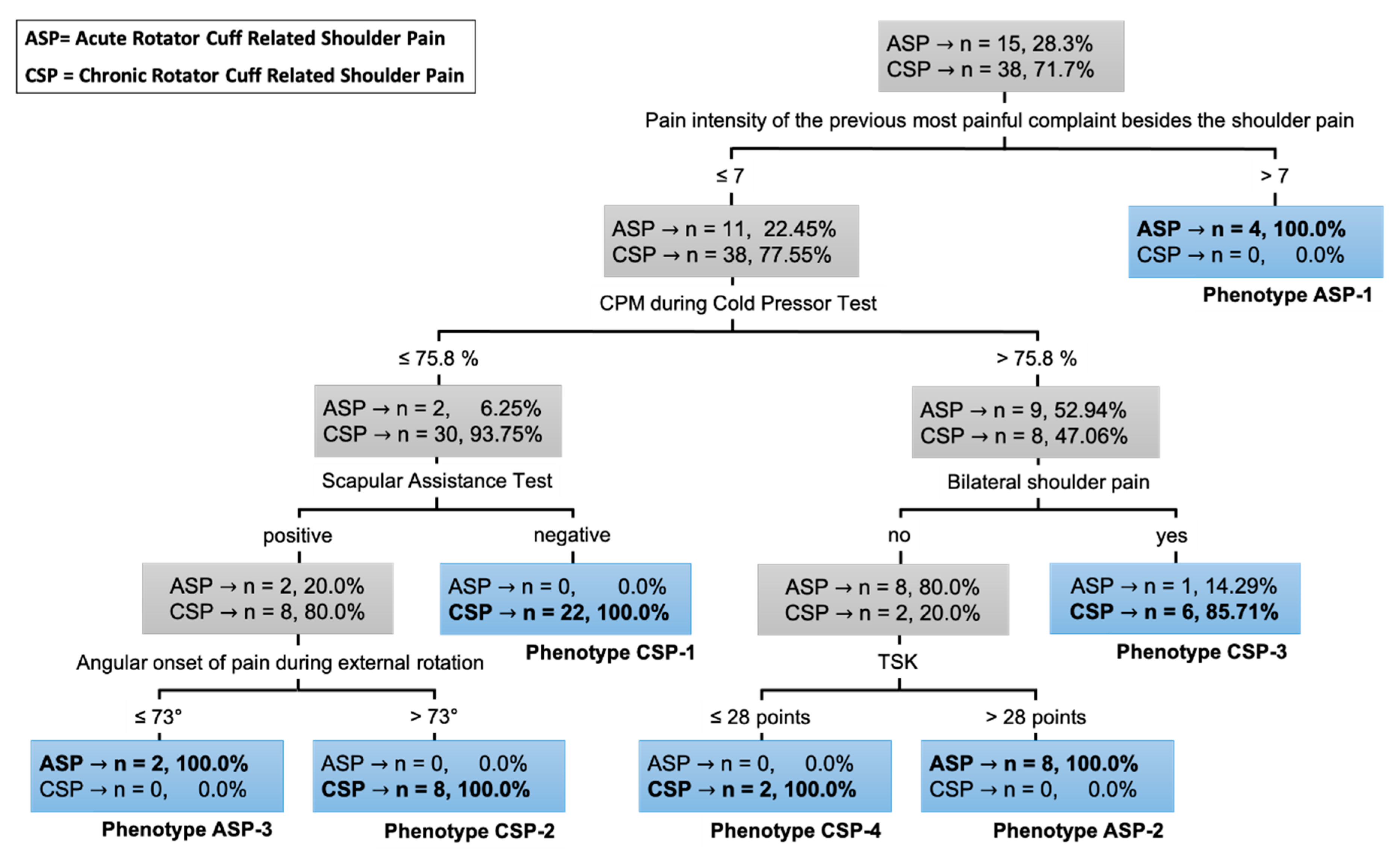
3.3. Clinical Decision Tree
- -
- ASP-1: presence of a previous painful complaint higher than seven points in another region of the body in addition to shoulder pain (n = 4; 26.7%);
- -
- ASP-2: presence of a previous pain lower than or equal to seven points and conditioned pain modulation during the cold pressor test higher than 75.8% of change on PPT-deltoid associated with unilateral pain and TSK score higher than 28 points (n = 8; 53.3%);
- -
- ASP-3: presence of a previous pain lower or equal to seven points and conditioned pain modulation during the cold pressor test lower than or equal to 75.8% of change on PPT-deltoid associated with positive scapular assistance test and angular onset of pain during external rotation lower than or equal to 73 degrees (n = 2; 13.3%).
- -
- CSP-1: conditioned pain modulation during the cold pressor test lower than or equal to 75.8% of change on PPT-deltoid associated with negative scapular assistance test (n = 22; 57.9%);
- -
- CSP-2: conditioned pain modulation during the cold pressor test lower than or equal to 75.8% of change on PPT-deltoid associated with positive scapular assistance test and angular onset of pain during external rotation higher than 73 degrees (n = 8; 21.0%);
- -
- CSP-3: conditioned pain modulation during the cold pressor test higher than 75.8% of change on PPT-deltoid associated with bilateral pain (n = 6; 15.8%);
- -
- CSP-4: conditioned pain modulation during the cold pressor test higher than 75.8% of change on PPT-deltoid associated with unilateral pain and a TSK score lower than or equal to 28 points (n = 2; 5.3%).
4. Discussion
4.1. Interpretation of the Results According to Literature
4.2. Implications for Clinical Practice
4.3. Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Luime, J.; Koes, B.; Hendriksen, I.; Burdorf, A.; Verhagen, A.; Miedema, H.; Verhaar, J. Prevalence and incidence of shoulder pain in the general population: A systematic review. Scand. J. Rheumatol. 2004, 33, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Littlewood, C.; Bateman, M.; Connor, C.; Gibson, J.; Horsley, I.; Jaggi, A.; Jones, V.; Meakins, A.; Scott, M. Physiotherapists’ recommendations for examination and treatment of rotator cuff related shoulder pain: A consensus exercise. Physiother. Pract. Res. 2019, 40, 87–94. [Google Scholar] [CrossRef]
- Lewis, J. Rotator cuff related shoulder pain: Assessment, management and uncertainties. Man. Ther. 2016, 23, 57–68. [Google Scholar] [CrossRef] [PubMed]
- Haik, M.; Alburquerque-Sendín, F.; Moreira, R.; Pires, E.; Camargo, P. Effectiveness of physical therapy treatment of clearly defined subacromial pain: A systematic review of randomised controlled trials. Br. J. Sports Med. 2016, 50, 1124–1134. [Google Scholar] [CrossRef]
- Pieters, L.; Lewis, J.; Kuppens, K.; Jochems, J.; Bruijstens, T.; Joossens, L.; Struyf, F. An update of systematic reviews examining the effectiveness of conservative physical therapy interventions for subacromial shoulder pain. J. Orthop. Sports Phys. Ther. 2020, 50, 131–141. [Google Scholar] [CrossRef]
- Croft, P.; Pope, D.; Silman, A. The clinical course of shoulder pain: Prospective cohort study in primary care. Br. Med. J. 1996, 313, 7–8. [Google Scholar] [CrossRef]
- Bot, S.D.M.; van der Waal, J.M.; Terwee, C.B.; van der Windt, D.A.W.M.; Scholten, R.J.P.M.; Bouter, L.M.; Dekker, J. Predictors of outcome in neck and shoulder symptoms-A cohort study in general practice. Spine (Phila. Pa. 1976). 2005, 30, E459–E470. [Google Scholar] [CrossRef]
- Noten, S.; Struyf, F.; Lluch, E.; D’Hoore, M.; Van Looveren, E.; Meeus, M. Central Pain Processing in Patients with Shoulder Pain: A Review of the Literature. Pain Pract. 2017, 17, 267–280. [Google Scholar] [CrossRef]
- Sanchis, M.N.; Lluch, E.; Nijs, J.; Struyf, F.; Kangasperko, M. The role of central sensitization in shoulder pain: A systematic literature review. Semin. Arthritis Rheum. 2015, 44, 710–716. [Google Scholar] [CrossRef]
- Struyf, F.; Lluch, E.; Falla, D.; Meeus, M.; Noten, S.; Nijs, J. Influence of shoulder pain on muscle function: Implications for the assessment and therapy of shoulder disorders. Eur. J. Appl. Physiol. 2015, 115, 225–234. [Google Scholar] [CrossRef]
- Reyes, B.A.; Hull, B.R.; Kurth, A.B.; Kukowski, N.R.; Mulligan, E.P.; Khazzam, M.S. Do Magnetic Resonance Imaging Characteristics of Full-Thickness Rotator Cuff Tears Correlate With Sleep Disturbance? Orthop. J. Sport. Med. 2017, 5, 2325967117735319. [Google Scholar] [CrossRef] [PubMed]
- Dunn, W.R.; Kuhn, J.E.; Sanders, R.; An, Q.; Baumgarten, K.M.; Bishop, J.Y.; Brophy, R.H.; Carey, J.L.; Holloway, G.B.; Jones, G.L.; et al. Symptoms of pain do not correlate with rotator cuff tear severity: A cross-sectional study of 393 patients with a symptomatic atraumatic full-thickness rotator cuff tear. J. Bone Joint Surg. Am. 2014, 96, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Clausen, M.B.; Witten, A.; Holm, K.; Christensen, K.B.; Attrup, M.L.; Hölmich, P.; Thorborg, K. Glenohumeral and scapulothoracic strength impairments exists in patients with subacromial impingement, but these are not reflected in the shoulder pain and disability index. BMC Musculoskelet. Disord. 2017, 18, 302. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, L.P.; Barreto, R.P.G.; Pereira, N.D.; Camargo, P.R. Comparison of scapular kinematics and muscle strength between those with a positive and a negative Scapular Assistance Test. Clin. Biomech. 2020, 73, 166–171. [Google Scholar] [CrossRef]
- Coats-Thomas, M.S.; Massimini, D.F.; Warner, J.J.P.; Seitz, A.L. In Vivo Evaluation of Subacromial and Internal Impingement Risk in Asymptomatic Individuals. Am. J. Phys. Med. Rehabil. 2018, 97, 659–665. [Google Scholar] [CrossRef]
- Vecchio, P.; Kavanagh, R.; Hazleman, B.L.; King, R.H. Shoulder pain in a community-based rheumatology clinic. Br. J. Rheumatol. 1995, 34, 440–442. [Google Scholar] [CrossRef]
- Ngomo, S.; Mercier, C.; Bouyer, L.J.; Savoie, A.; Roy, J.S. Alterations in central motor representation increase over time in individuals with rotator cuff tendinopathy. Clin. Neurophysiol. 2015, 126, 365–371. [Google Scholar] [CrossRef]
- Tagliaferri, S.D.; Miller, C.T.; Owen, P.J.; Mitchell, U.H.; Brisby, H.; Fitzgibbon, B.; Masse-Alarie, H.; Van Oosterwijck, J.; Belavy, D.L. Domains of Chronic Low Back Pain and Assessing Treatment Effectiveness: A Clinical Perspective. Pain Pract. 2020, 20, 211–225. [Google Scholar] [CrossRef]
- Heerkens, R.J.; Köke, A.J.; Lötters, F.J.; Smeets, R.J. Motor imagery performance and tactile acuity in patients with complaints of arms, neck and shoulder. Pain Manag. 2018, 8, 277–286. [Google Scholar] [CrossRef]
- Mena-del Horno, S.; Balasch-Bernat, M.; Dueñas, L.; Reis, F.; Louw, A.; Lluch, E. Laterality judgement and tactile acuity in patients with frozen shoulder: A cross-sectional study. Musculoskelet. Sci. Pract. 2020, 47, 102136. [Google Scholar] [CrossRef]
- Kuppens, K.; Hans, G.; Roussel, N.; Struyf, F.; Fransen, E.; Cras, P.; Van Wilgen, C.P.; Nijs, J. Sensory processing and central pain modulation in patients with chronic shoulder pain: A case-control study. Scand. J. Med. Sci. Sports 2017, 28, 1183–1192. [Google Scholar] [CrossRef] [PubMed]
- Haik, M.N.; Evans, K.; Smith, A.; Henríquez, L.; Bisset, L. People with musculoskeletal shoulder pain demonstrate no signs of altered pain processing. Musculoskelet. Sci. Pract. 2019, 39, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Gwilym, S.E.; Oag, H.C.L.; Tracey, I.; Carr, A.J. Evidence that central sensitisation is present in patients with shoulder impingement syndrome and influences the outcome after surgery. Bone Joint J. 2011, 93-B, 498–502. [Google Scholar] [CrossRef] [PubMed]
- Paul, T.M.; Hoo, J.S.; Chae, J.; Wilson, R.D. Central hypersensitivity in patients with subacromial impingement syndrome. Arch. Phys. Med. Rehabil. 2012, 93, 2206–2209. [Google Scholar] [CrossRef]
- Plinsinga, M.L.; Brink, M.S.; Vicenzino, B.; Van Wilgen, C.P. Evidence of nervous system sensitization in commonly presenting and persistent painful tendinopathies: A systematic review. J. Orthop. Sports Phys. Ther. 2015, 45, 864–875. [Google Scholar] [CrossRef]
- Simon, C.B.; Valencia, C.; Coronado, R.A.; Wu, S.S.; Li, Z.; Dai, Y.; Farmer, K.W.; Moser, M.M.; Wright, T.W.; Fillingim, R.B.; et al. Biopsychosocial Influences on Shoulder Pain: Analyzing the Temporal Ordering of Postoperative Recovery. J. Pain 2020, 21, 808–819. [Google Scholar] [CrossRef]
- Martinez-Calderon, J.; Struyf, F.; Meeus, M.; Luque-Suarez, A. The association between pain beliefs and pain intensity and/or disability in people with shoulder pain: A systematic review. Musculoskelet. Sci. Pract. 2018, 37, 29–57. [Google Scholar] [CrossRef]
- Martinez-Calderon, J.; Meeus, M.; Struyf, F.; Miguel Morales-Asencio, J.; Gijon-Nogueron, G.; Luque-Suarez, A. The role of psychological factors in the perpetuation of pain intensity and disability in people with chronic shoulder pain: A systematic review. BMJ Open 2018, 8, 1–16. [Google Scholar] [CrossRef]
- Martinez-Calderon, J.; Struyf, F.; Meeus, M.; Morales-Ascencio, J.M.; Luque-Suarez, A. Influence of psychological factors on the prognosis of chronic shoulder pain: Protocol for a prospective cohort study. BMJ Open 2017, 7, e012822. [Google Scholar] [CrossRef]
- Luque-Suarez, A.; Martinez-Calderon, J.; Navarro-Ledesma, S.; Morales-Asencio, J.M.; Meeus, M.; Struyf, F. Kinesiophobia Is Associated With Pain Intensity and Disability in Chronic Shoulder Pain: A Cross-Sectional Study. J. Manip. Physiol. Ther. 2020, 17–19. [Google Scholar] [CrossRef]
- van der Windt, D.A.W.M.; Kuijpers, T.; Jellema, P.; van der Heijden, G.J.M.G.; Bouter, L.M. Do psychological factors predict outcome in both low-back pain and shoulder pain? Ann. Rheum. Dis. 2007, 66, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Chester, R.; Khondoker, M.; Shepstone, L.; Lewis, J.S.; Jerosch-herold, C. Self-efficacy and risk of persistent shoulder pain: Results of a Classification and Regression Tree (CART) analysis. Br. J. Sport. Med. 2019, 53, 825–834. [Google Scholar] [CrossRef] [PubMed]
- Wong, W.K.; Li, M.Y.; Yung, P.S.-H.; Leong, H.T. The effect of psychological factors on pain, function and quality of life in patients with rotator cuff tendinopathy: A systematic review. Musculoskelet. Sci. Pract. 2020, 47, 102173. [Google Scholar] [CrossRef] [PubMed]
- Chester, R.; Jerosch-herold, C.; Lewis, J.; Shepstone, L. Psychological factors are associated with the outcome of physiotherapy for people with shoulder pain: A multicentre longitudinal cohort study. Br. J. Sport. Med. 2018, 52, 269–275. [Google Scholar] [CrossRef]
- Coronado, R.A.; Seitz, A.L.; Pelote, E.; Archer, K.R.; Jain, N.B. Are psychosocial factors associated with patient-reported outcome measures in patients with rotator cuff tears? A systematic review. Clin. Orthop. Relat. Res. 2018, 476, 810–829. [Google Scholar] [CrossRef]
- Karels, C.H.; Bierma-Zeinstra, S.M.A.; Burdorf, A.; Verhagen, A.P.; Nauta, A.P.; Koes, B.W. Social and psychological factors influenced the course of arm, neck and shoulder complaints. J. Clin. Epidemiol. 2007, 60, 839–848. [Google Scholar] [CrossRef]
- Cios, K.J.; Moore, G.W. Uniqueness of medical data mining. Artif. Intell. Med. 2002, 26, 1–24. [Google Scholar] [CrossRef]
- Lemon, S.C.; Ph, D.; Roy, J.; Ph, D.; Clark, M.A.; Ph, D.; Rakowski, W.; Ph, D.; Med, A.B. Classification and Regression Tree Analysis in Public Health: Methodological Review and Comparison With Logistic Regression. Ann. Behav. Med. 2003, 26, 172–181. [Google Scholar] [CrossRef]
- Merskey, H.; Bogduk, N. Classification of Chronic Pain. Descriptons of Chronic Pain Syndromes and Definitions of Pain Terms, 2nd ed.; Merskey, H., Bogduk, N., Eds.; IASP Press: Seatle, WA, USA, 1994; ISBN 0-931092-05-1. [Google Scholar]
- Alburquerque-Sendín, F.; Camargo, P.; Vieira, A.; Salvini, T. Bilateral myofascial trigger points and pressure pain thresholds in the shoulder muscles in patients with unilateral shoulder impingement syndrome: A blinded, controlled study. Clin. J. Pain 2013, 29, 478–486. [Google Scholar] [CrossRef]
- Kromer, T.O.; Sieben, J.M.; de Bie, R.A.; Bastiaenen, C.H.G. Influence of Fear-Avoidance Beliefs on Disability in Patients With Subacromial Shoulder Pain in Primary Care: A Secondary Analysis. Phys. Ther. 2014, 94, 1775–1784. [Google Scholar] [CrossRef]
- Camargo, P.R.; Alburquerque-Sendín, F.; Avila, M.A.; Haik, M.N.; Vieira, A.; Salvini, T.F. Effects of stretching and strengthening exercises, with and without manual therapy, on scapular kinematics, function, and pain in individuals with shoulder impingement: A randomized controlled trial. J. Orthop. Sports Phys. Ther. 2015, 45, 984–997. [Google Scholar] [CrossRef] [PubMed]
- Burns, S.A.; Cleland, J.A.; Carpenter, K.; Mintken, P.E. Interrater reliability of the cervicothoracic and shoulder physical examination in patients with a primary complaint of shoulder pain. Phys. Ther. Sport 2016, 18, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Van Der Windt, D.A.W.M.; Koes, B.W.; Boeke, A.J.P.; Devillé, W.; De Jong, B.A.; Bouter, L.M. Shoulder disorders in general practice: Prognostic indicators of outcome. Br. J. Gen. Pract. 1996, 46, 519–523. [Google Scholar] [PubMed]
- Kuijpers, T.; van der Windt, D.A.W.M.; Boeke, A.J.P.; Twisk, J.W.R.; Vergouwe, Y.; Bouter, L.M.; van der Heijden, G.J.M.G. Clinical prediction rules for the prognosis of shoulder pain in general practice. Pain 2006, 120, 276–285. [Google Scholar] [CrossRef]
- Valencia, C.; Kindler, L.L.; Fillingim, R.B.; George, S.Z. Investigation of central pain processing in shoulder pain: Converging results from two musculoskeletal pain models. J. Pain 2012, 13, 81–89. [Google Scholar] [CrossRef]
- Valencia, C.; Kindler, L.L.; Fillingim, R.B.; George, S.Z. Stability of conditioned pain modulation in two musculoskeletal pain models: Investigating the influence of shoulder pain intensity and gender. BMC Musculoskelet. Disord. 2013, 14, 182. [Google Scholar] [CrossRef]
- Mayer, T.G.; Neblett, R.; Cohen, H. The development and psychometric validation of the central sensitization inventory. Pain Pract. 2012, 12, 276–285. [Google Scholar] [CrossRef]
- Neblett, R.; Cohen, H.; Choi, Y.; Hartzell, M.M.; Williams, M.; Mayer, T.G.; Gatchel, R.J. The central sensitization inventory (CSI): Establishing clinically significant values for identifying central sensitivity syndromes in an outpatient chronic pain sample. J. Pain 2013, 14, 438–445. [Google Scholar] [CrossRef]
- Nijs, J.; Van Houdenhove, B.; Oostendorp, R.A.B. Recognition of central sensitization in patients with musculoskeletal pain: Application of pain neurophysiology in manual therapy practice. Man. Ther. 2010, 15, 135–141. [Google Scholar] [CrossRef]
- Galeotti, N.; Ghelardini, C.; Grazioli, I.; Uslenghi, C. Indomethacin, caffeine and prochlorperazine alone and combined revert hyperalgesia in in vivo models of migraine. Pharmacol. Res. 2002, 46, 245–250. [Google Scholar] [CrossRef]
- Stöhr, T.; Krause, E.; Selve, N. Lacosamide displays potent antinociceptive effects in animal models for inflammatory pain. Eur. J. Pain 2006, 10, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Alghadir, A.H.; Anwer, S.; Iqbal, A.; Iqbal, Z.A. Test-retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J. Pain Res. 2018, 11, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Yao, M.; Yao, M.; Xu, B.P.; Xu, B.P.; Li, Z.J.; Li, Z.J.; Zhu, S.; Zhu, S.; Tian, Z.R.; Tian, Z.R.; et al. A comparison between the low back pain scales for patients with lumbar disc herniation: Validity, reliability, and responsiveness. Health Qual. Life Outcomes 2020, 18, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.P.; Turner, J.A.; Romano, J.M. What is the maximum number of levels needed in pain intensity measurement? Pain 1994, 58, 387–392. [Google Scholar] [CrossRef]
- Caumo, W.; Antunes, L.C.; Elkfury, J.L.; Herbstrith, E.G.; Sipmann, R.B.; Souza, A.; Torres, I.L.S.; Dos Santos, V.S.; Neblett, R. The central sensitization inventory validated and adapted for a Brazilian population: Psychometric properties and its relationship with brain-derived neurotrophic factor. J. Pain Res. 2017, 10, 2109–2122. [Google Scholar] [CrossRef]
- Mintken, P.E.; Glynn, P.; Cleland, J.A. Psychometric properties of the shortened disabilities of the Arm, Shoulder, and Hand Questionnaire (QuickDASH) and Numeric Pain Rating Scale in patients with shoulder pain. J. Shoulder Elb. Surg. 2009, 18, 920–926. [Google Scholar] [CrossRef]
- Kolber, M.J.; Vega, F.; Widmayer, K.; Cheng, M.-S.S. The reliability and minimal detectable change of shoulder mobility measurements using a digital inclinometer. Physiother. Theory Pract. 2011, 27, 176–184. [Google Scholar] [CrossRef]
- Uhl, T.L.; Kibler, W.B.; Gecewich, B.; Tripp, B.L. Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy 2009, 25, 1240–1248. [Google Scholar] [CrossRef]
- Kibler, W.B.; Ludewig, P.M.; McClure, P.W.; Michener, L.A.; Bak, K.; Sciascia, A.D. Clinical implications of scapular dyskinesis in shoulder injury: The 2013 consensus statement from the “Scapular Summit”. Br. J. Sports Med. 2013, 47, 877–885. [Google Scholar] [CrossRef]
- Rabin, A.; Irrgang, J.J.; Fitzgerald, G.K.; Eubanks, A. The Intertester Reliability of the Scapular Assistance Test. J. Orthop. Sports Phys. Ther. 2006, 36, 653–660. [Google Scholar] [CrossRef]
- Neer, C.S. 2nd Anterior acromioplasty for the chronic impingement syndrome in the shoulder: A preliminary report. J. Bone Joint Surg. Am. 1972, 54, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Jobe, F.W.; Moynes, D.R. Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries. Am. J. Sports Med. 1982, 10, 336–339. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, R.J.; Kennedy, J.C. Impingement syndrome in athletes. Am. J. Sports Med. 1979, 8, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Michener, L.A.; Walsworth, M.K.; Doukas, W.C.; Murphy, K.P. Reliability and Diagnostic Accuracy of 5 Physical Examination Tests and Combination of Tests for Subacromial Impingement. Arch. Phys. Med. Rehabil. 2009, 90, 1898–1903. [Google Scholar] [CrossRef]
- Park, H.B.; Yokota, A.; Gill, H.S.; El Rassi, G.; McFarland, E.G. Diagnostic accuracy of clinical tests for the different degrees of subacromial impingement syndrome. J. Bone Jt. Surg. Am. 2005, 87, 1446–1455. [Google Scholar]
- Orfale, A.G.; Araújo, P.M.P.; Ferraz, M.B.; Natour, J. Translation into Brazilian Portuguese, cultural adaptation and evaluation of the reliability of the Disabilities of the Arm, Shoulder and Hand Questionnaire. Braz. J. Med. Biol. Res. 2005, 38, 293–302. [Google Scholar] [CrossRef]
- Rolke, R.; Magerl, W.; Campbell, K.A.; Schalber, C.; Caspari, S.; Birklein, F.; Treede, R.D. Quantitative sensory testing: A comprehensive protocol for clinical trials. Eur. J. Pain 2006, 10, 77–88. [Google Scholar] [CrossRef]
- Gröne, E.; Crispin, A.; Fleckenstein, J.; Irnich, D.; Treede, R.D.; Lang, P.M. Test order of quantitative sensory testing facilitates mechanical hyperalgesia in healthy volunteers. J. Pain 2012, 13, 73–80. [Google Scholar] [CrossRef]
- Breckenridge, J.D.; Mcauley, J.H.; Butler, D.S.; Stewart, H.; Moseley, G.L.; Ginn, K.A. The development of a shoulder specific left/right judgement task: Validity & reliability. Musculoskelet. Sci. Pract. 2017, 28, 39–45. [Google Scholar]
- Botnmark, I.; Tumilty, S.; Mani, R. Tactile acuity, body schema integrity and physical performance of the shoulder: A cross-sectional study. Man. Ther. 2016, 23, 9–16. [Google Scholar] [CrossRef]
- Wikstrom, E.A.; Allen, G. Reliability of two-point discrimination thresholds using a 4-2-1 stepping algorithm algorithm. Somat. Mot. Res. 2016, 33, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Chesterton, L.S.; Sim, J.; Wright, C.C.; Foster, N.E. Interrater Reliability of Algometry in Measuring Pressure Pain Thresholds in Healthy Humans, Using Multiple Raters. Clin. J. Pain 2007, 23, 760–766. [Google Scholar] [CrossRef] [PubMed]
- Granot, M.; Granovsky, Y.; Sprecher, E.; Nir, R.R.; Yarnitsky, D. Contact heat-evoked temporal summation: Tonic versus repetitive-phasic stimulation. Pain 2006, 122, 295–305. [Google Scholar] [CrossRef] [PubMed]
- Yarnitsky, D.; Granot, M.; Granovsky, Y. Pain modulation profile and pain therapy: Between pro- and antinociception. Pain 2014, 155, 663–665. [Google Scholar] [CrossRef]
- Collin, S.M.; Nijs, J.; Meeus, M.; Poli, A.; Willekens, B.; Ickmans, K. Endogenous Pain Facilitation Rather Than Inhibition Differs Between People with Chronic Fatigue Syndrome, Multiple Sclerosis, and Controls: An Observational Study. Pain Physician 2017, 20, E489–E497. [Google Scholar]
- Yarnitsky, D.; Bouhassira, D.; Drewes, A.M.; Fillingim, R.B.; Granot, M.; Hansson, P.; Landau, R.; Marchand, S.; Matre, D.; Nilsen, K.B.; et al. Recommendations on practice of conditioned pain modulation (CPM) testing. Eur. J. Pain 2014, 19, 805–806. [Google Scholar] [CrossRef]
- Oono, Y.; Nie, H.; Matos, R.L.; Wang, K.; Arendt-Nielsen, L. The inter- and intra-individual variance in descending pain modulation evoked by different conditioning stimuli in healthy men. Scand. J. Pain 2011, 2, 162–169. [Google Scholar] [CrossRef]
- Imai, Y.; Petersen, K.K.; Mørch, C.D.; Nielsen, L.A. Comparing test – retest reliability and magnitude of conditioned pain modulation using different combinations of test and conditioning stimuli. Somat. Mot. Res. 2016, 33, 169–177. [Google Scholar] [CrossRef]
- Abreu, A.M.; Faria, C.D.C.M.; Cardoso, S.M.V.; Teixeira-Salmela, L.F. Versão brasileira do Fear Avoidance Beliefs Questionnaire Questionnaire. Cad. Saude Publica 2008, 24, 615–623. [Google Scholar] [CrossRef]
- Siqueira, F.B.; Teixeira-Salmela, L.F.; Magalhães, L.D.C. Análise das propriedades psicométricas da versão brasileira da Escala Tampa de Cinesiofobia. Acta Orthop. Bras. 2007, 15, 19–24. [Google Scholar] [CrossRef]
- Waddell, G.; Newton, M.; Henderson, I.; Somerville, D.; Main, C.J. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 1993, 52, 157–168. [Google Scholar] [CrossRef]
- Kori, K.; Miller, R.; Todd, D. Kinesiophobia: A new view of chronic pain behavior. Pain Manag. 1990, 3, 35–43. [Google Scholar]
- de Souza, F.S.; da Silva Marinho, C.; Siqueira, F.B.; Maher, C.G.; Costa, L.O.P. Psychometric Testing Confirms That the Brazilian-Portuguese Adaptations, the Original Versions of the Fear-Avoidance Beliefs Questionnaire, and the Tampa Scale of Kinesiophobia Have Similar Measurement Properties. Spine (Phila. Pa. 1976) 2008, 33, 1028–1033. [Google Scholar] [CrossRef] [PubMed]
- Lundberg, M.; Grimby-Ekman, A.; Verbunt, J.; Simmonds, M.J. Pain-related fear: A critical review of the related measures. Pain Res. Treat. 2011, 2011, 494196. [Google Scholar] [CrossRef] [PubMed]
- Sehn, F.; Chachamovich, E.; Vidor, L.P.; Dall-Agnol, L.; Custódio de Souza, I.C.; Torres, I.L.S.; Fregni, F.; Caumo, W. Cross-Cultural Adaptation and Validation of the Brazilian Portuguese Version of the Pain Catastrophizing Scale. Pain Med. 2012, 13, 1425–1435. [Google Scholar] [CrossRef]
- Lopes, R.A.; Dias, R.C.; De Queiroz, B.Z.; De Britto Rosa, N.M.; Pereira, L.D.S.M.; Dias, J.M.D.; Magalhães, L.D.C. Psychometric properties of the Brazilian version of the Pain Catastrophizing Scale for acute low back pain. Arq. Neuropsiquiatr. 2015, 73, 436–444. [Google Scholar] [CrossRef]
- Salvetti, M.G.; Pimenta, C.A.M. Validação da Chronic Pain Self-Efficacy Scale para a Língua Portuguesa. Rev. Psiq. Clin. 2005, 32, 202–210. [Google Scholar] [CrossRef]
- Vignola, R.C.B.; Tucci, A.M. Adaptation and validation of the depression, anxiety and stress scale (DASS) to Brazilian Portuguese. J. Affect. Disord. 2014, 155, 104–109. [Google Scholar] [CrossRef]
- Andrade, V.; Kind, P.; Maia, A.C.; De Menezes, R.M.; Reis, C.D.B.; Souza, M.N.; Martins, D.; Gomes, L.; Nichele, D.; Calazans, J.; et al. Societal Preferences for EQ-5D Health States from a Brazilian Population Survey. Value Health Reg. Issues 2013, 2, 405–412. [Google Scholar] [CrossRef]
- Bagattini, Â.M.; Camey, S.A.; Miguel, S.R.; Andrade, M.V.; de Souza Noronha, K.V.M.; Monica, M.A.; Lima, A.F.; Santos, M.; Polanczyk, C.A.; Cruz, L.N. Electronic Version of the EQ-5D Quality-of-Life Questionnaire: Adaptation to a Brazilian Population Sample. Value Health Reg. Issues 2018, 17, 88–93. [Google Scholar] [CrossRef]
- Witten, I.H.; Frank, E. Data Mining-Practical Machine Learning Tools and Techniques, 2nd ed.; Gray, J., Ed.; Elsevier Inc.: San Francisco, CA, USA, 2005; ISBN 0120884070. [Google Scholar]
- Pasini, A. Artificial neural networks for small dataset analysis. J. Thorac. Dis. 2015, 7, 953–960. [Google Scholar] [PubMed]
- Rushing, C.; Bulusu, A.; Hurwitz, H.I.; Nixon, A.B.; Pang, H. A leave-one-out cross-validation SAS macro for the identification of markers associated with survival. Comput. Biol. Med. 2015, 57, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Jayawardana, K.; Schramm, S.-J.; Tembe, V.; Mueller, S.; Thompson, J.F.; Scolyer, R.A.; Mann, G.J.; Yang, J. Identification, Review, and Systematic Cross-Validation of microRNA Prognostic Signatures in Metastatic Melanoma. J. Investig. Dermatol. 2016, 136, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Torres-Cueco, R.; van Wilgen, C.P.; Girbés, E.L.; Struyf, F.; Roussel, N.; Van Oosterwijck, J.; Daenen, L.; Kuppens, K.; Vanderweeën, L.; et al. Applying Modern Pain Neuroscience in Clinical Practice: Criteria for the Classification of Central Sensitization Pain. Pain Physician 2014, 17, 447–457. [Google Scholar] [PubMed]
- Kwon, M.; Altin, M.; Duenas, H.; Alev, L. The role of descending inhibitory pathways on chronic pain modulation and clinical implications. Pain Pract. 2014, 14, 656–667. [Google Scholar] [CrossRef]
- Teles, A.R.; Ocay, D.D.; Bin Shebreen, A.; Tice, A.; Saran, N.; Ouellet, J.A.; Ferland, C.E. Evidence of impaired pain modulation in adolescents with idiopathic scoliosis and chronic back pain. Spine J. 2019, 19, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Lewis, G.N.; Rice, D.A.; McNair, P.J. Conditioned pain modulation in populations with chronic pain: A systematic review and meta-analysis. J. Pain 2012, 13, 936–944. [Google Scholar] [CrossRef]
- Yarnitsky, D. Conditioned pain modulation (the diffuse noxious inhibitory control-like effect): Its relevance for acute and chronic pain states. Curr. Opin. Anaesthesiol. 2010, 23, 611–615. [Google Scholar] [CrossRef]
- Ossipov, M.H.; Morimura, K.; Porreca, F. Descending pain modulation and chronification of pain. Curr. Opin. Support. Palliat. Care 2014, 8, 143–151. [Google Scholar]
- de Resende, M.A.; Silva, L.F.S.; Sato, K.; Arendt-Nielsen, L.; Sluka, K.A. Blockade of opioid receptors in the medullary reticularis nucleus dorsalis, but not the rostral ventromedial medulla, prevents analgesia produced by diffuse noxious inhibitory control in rats with muscle inflammation. J. Pain 2011, 12, 687–697. [Google Scholar] [CrossRef]
- Schliessbach, J.; Lütolf, C.; Streitberger, K.; Scaramozzino, P.; Arendt-Nielsen, L.; Curatolo, M. Reference values of conditioned pain modulation. Scand. J. Pain 2019, 19, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Pud, D.; Granovsky, Y.; Yarnitsky, D. The methodology of experimentally induced diffuse noxious inhibitory control (DNIC)-like effect in humans. Pain 2009, 144, 16–19. [Google Scholar] [CrossRef] [PubMed]
- Yarnitsky, D.; Crispel, Y.; Eisenberg, E.; Granovsky, Y.; Ben-Nun, A.; Sprecher, E.; Best, L.A.; Granot, M. Prediction of chronic post-operative pain: Pre-operative DNIC testing identifies patients at risk. Pain 2008, 138, 22–28. [Google Scholar] [CrossRef]
- Feleus, A.; van Dalen, T.; Bierma-Zeinstra, S.M.; Bernsen, R.M.; Verhaar, J.A.; Koes, B.W.; Miedema, H.S. Kinesiophobia in patients with non-traumatic arm, neck and shoulder complaints: A prospective cohort study in general practice. BMC Musculoskelet. Disord. 2007, 8, 117. [Google Scholar] [CrossRef] [PubMed]
- De Baets, L.; Matheve, T.; Meeus, M.; Struyf, F.; Timmermans, A. The influence of cognitions, emotions and behavioral factors on treatment outcomes in musculoskeletal shoulder pain: A systematic review. Clin. Rehabil. 2019, 33, 980–991. [Google Scholar] [CrossRef]
- Schliessbach, J.; Siegenthaler, A.; Streitberger, K.; Eichenberger, U.; Nüesch, E.; Jüni, P.; Arendt-Nielsen, L.; Curatolo, M. The prevalence of widespread central hypersensitivity in chronic pain patients. Eur. J. Pain 2013, 17, 1502–1510. [Google Scholar] [CrossRef]
- Coronado, R.A.; Simon, C.B.; Valencia, C.; George, S.Z. Experimental pain responses support peripheral and central sensitization in patients with unilateral shoulder pain. Clin. J. Pain 2014, 30, 143–151. [Google Scholar] [CrossRef]
- Mlekusch, S.; Neziri, A.Y.; Limacher, A.; Juni, P.; Arendt-Nielsen, L.; Curatolo, M. Conditioned pain modulation in patients with acute and chronic low back pain. Clin. J. Pain 2016, 32, 116–121. [Google Scholar] [CrossRef]
- Kamonseki, D.H.; Haik, M.N.; Camargo, P.R. Scapular movement training versus standardized exercises for individuals with chronic shoulder pain: Protocol for a randomized controlled trial. Braz. J. Phys. Ther. 2020. [Google Scholar] [CrossRef]
- Struyf, F.; Geraets, J.; Noten, S.; Meeus, M.; Nijs, J. A multivariable prediction model for the chronification of non-traumatic shoulder pain: A systematic review. Pain Physician 2016, 19, 1–10. [Google Scholar]
- Santello, G.; Rossi, D.M.; Martins, J.; de Libardoni, T.C.; de Oliveira, A.S. Effects on shoulder pain and disability of teaching patients with shoulder pain a home-based exercise program: A randomized controlled trial. Clin. Rehabil. 2020. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.A.; Ryan, C.G.; Cooper, L.; Ellington, D.; Whittle, R.; Lavender, M.; Dixon, J.; Atkinson, G.; Cooper, K.; Martin, D.J. Pain Neuroscience Education for Adults With Chronic Musculoskeletal Pain: A Mixed-Methods Systematic Review and Meta-Analysis. J. Pain 2019, 20, 1140.e1–1140.e22. [Google Scholar] [CrossRef] [PubMed]
- Brox, J.I.; Staff, P.H.; Ljunggren, A.E.; Brevik, J.I. Arthroscopic surgery compared with supervised exercises in patients with rotator cuff disease (stage II impingement syndrome). BMJ 1993, 307, 899–903. [Google Scholar] [CrossRef] [PubMed]
- Haahr, J.P.; Østergaard, S.; Dalsgaard, J.; Norup, K.; Frost, P.; Lausen, S.; Holm, E.A.; Andersen, J.H. Exercises versus arthroscopic decompression in patients with subacromial impingement: A randomised, controlled study in 90 cases with a one year follow up. Ann. Rheum. Dis. 2005, 64, 760–764. [Google Scholar] [CrossRef] [PubMed]
- Boutevillain, L.; Dupeyron, A.; Rouch, C.; Richard, E.; Coudeyre, E. Facilitators and barriers to physical activity in people with chronic low back pain: A qualitative study. PLoS ONE 2017, 12, e0179826. [Google Scholar] [CrossRef]
- Raja, S.N.; Carr, D.B.; Cohen, M.; Finnerup, N.B.; Flor, H.; Gibson, S.; Keefe, F.J.; Mogil, J.S.; Ringkamp, M.; Sluka, K.A.; et al. The revised International Association for the Study of Pain definition of pain: Concepts, challenges, and compromises. Pain 2020, 161, 1976–1982. [Google Scholar] [CrossRef]
- Barreto, R.P.G.; Braman, J.P.; Ludewig, P.M.; Ribeiro, L.P.; Camargo, P.R. Bilateral magnetic resonance imaging findings in individuals with unilateral shoulder pain. J. Shoulder Elb. Surg. 2019, 28, 1699–1706. [Google Scholar] [CrossRef]
- Apkarian, A.V.; Sosa, Y.; Sonty, S.; Levy, R.M.; Harden, R.N.; Parrish, T.B.; Gitelman, D.R. Chronic back pain is associated with decreased prefrontal and thalamic gray matter density. J. Neurosci. 2004, 24, 10410–10415. [Google Scholar] [CrossRef]
- Rodrigues-De-Souza, D.P.; Fernández-De-Las-Peñas, C.; Martín-Vallejo, F.J.; Blanco-Blanco, J.F.; Moro-Gutiérrez, L.; Alburquerque-Sendín, F. Differences in pain perception, health-related quality of life, disability, mood, and sleep between Brazilian and Spanish people with chronic non-specific low back pain. Braz. J. Phys. Ther. 2016, 20, 412–421. [Google Scholar] [CrossRef]
- UTHealth, S. of B.I. Biostatistics Fot the Clinicians. Lesson 3: Clinical Decision Making in a Multivariable Environment. Available online: https://www.uth.tmc.edu/uth_orgs/educ_dev/oser/L3_2.HTM (accessed on 25 September 2020).

| Acute RCRSP (n = 15) | Chronic RCRSP (n = 38) | p-Value | |
|---|---|---|---|
| Sociodemographic aspects | |||
| Age (years) | 31.0 [20.0] | 33.5 [24.3] | 0.54 |
| Sex | |||
| Male | 9 (60.0%) | 23 (60.5%) | 0.97 |
| Educational level | |||
| Incomplete elementary school | 1 (6.7%) | 1 (2.6%) | 0.40 |
| Elementary school | 0 (0.0) | 3 (7.9%) | |
| High school | 6 (40.0%) | 9 (23.7%) | |
| University education | 8 (53.3%) | 25 (65.8%) | |
| Marital status | |||
| Single | 7 (46.7%) | 16 (42.1%) | 0.92 |
| Married | 7 (46.7%) | 18 (47.4%) | |
| Divorced | 1 (6.7%) | 3 (7.9%) | |
| Widowed | 0 (0.0%) | 1 (2.6%) | |
| Arm dominance | |||
| Right | 6 (40.0%) | 9 (23.7%) | 0.25 |
| Left | 8 (53.3%) | 25 (65.8%) | |
| Employment status | |||
| Active | 14 (93.3%) | 33 (86.8%) | 0.66 |
| Retired | 1 (6.7%) | 5 (13.2%) | |
| Occupational demand | |||
| Physical | 2 (13.3%) | 7 (18.4%) | 0.44 |
| Psychological | 10 (66.7%) | 18 (47.4%) | |
| Both | 3 (20.0%) | 13 (34.2%) | |
| Presence of upper limb repetitive movement | |||
| Yes | 11 (73.3%) | 25 (65.8%) | 0.75 |
| No | 4 (26.7%) | 13 (34.2%) | |
| Frequency of physical activity (days/week) | 4 [4] | 4 [4] | 0.73 |
| Smoking status | |||
| Yes | 2 (13.3) | 5 (13.2) | 1.00 |
| No | 13 (86.7) | 33 (86.8) | |
| Biological aspects related to general clinical health status | |||
| Presence of any other pain previous to shoulder pain | 10 (66.7%) | 22 (57.9%) | 0.55 |
| Pain intensity of the previous most painful complaint besides the shoulder pain (0–10) | 4.8 ± 3.1 | 2.9 ± 1.6 | 0.10 |
| CSI-part A | 23.0 ± 9.8 | 28.0 ± 11.3 | 0.14 |
| Biological aspects related to shoulder clinical condition | |||
| Affected shoulder | |||
| Dominant | 6 (40.0%) | 14 (36.8%) | 0.44 |
| Non-dominant | 6 (40.0%) | 10 (26.3%) | |
| Both | 3 (20.0%) | 14 (36.8%) | |
| Duration of symptoms (months) | 3.0 [2.3] | 36.0 [48.8] | 0.001 |
| Pain intensity during arm movement (0–10) | 8.0 [4.0] | 7.0 [2.3] | 0.418 |
| ROM (degrees) | |||
| Angular onset of pain during abduction | 148.0 [35] | 132.0 [64.0] | 0.065 |
| Angular offset of pain during abduction | 175.0 [14] | 169.0 [15.0] | 0.43 |
| Angular onset of pain during external rotation | 85.5 ± 15.3 | 92.1 ± 19.0 | 0.23 |
| Angular offset of pain during external rotation | 95.9 ± 11.9 | 99.0 ± 13.1 | 0.43 |
| Scapular dyskinesis | |||
| Present | 14 (93.3%) | 36 (94.7%) | 1.00 |
| Absent | 1 (6.7%) | 2 (5.3%) | |
| Scapular assistance test | |||
| Positive | 5 (33.3%) | 11 (28.9%) | 0.75 |
| Negative | 10 (66.7%) | 27 (71.1%) | |
| Total number of positive special tests for shoulder rotator cuff related pain | 4.5 ± 2.1 | 4.9 ± 2.0 | 0.46 |
| DASH | 12.5 [15.0] | 18.3 [16.6] | 0.295 |
| Acute RCRSP (n = 15) | Chronic RCRSP (n = 38) | p-Value | |
|---|---|---|---|
| Biological aspects related to sensory function | |||
| TPDT-anterior (mm) | 34.9 ± 19.0 | 40.2 ± 15.8 | 0.30 |
| TPDT-posterior (mm) | 44.1 ± 16.7 | 44.9 ± 12.6 | 0.85 |
| LRJT-accuracy (%) | 100.0 [10.0] | 100.0 [0.0] | 0.55 |
| LRJT-time (s) | 1.4 [0.4] | 1.3 [0.5] | 0.60 |
| PPT-acromion (KPa) | 305.6 [215.0] | 271.0 [255.5] | 0.79 |
| PPT-deltoid (KPa) | 353.4 ± 163.3 | 360.0 ± 173.8 | 0.90 |
| PPT-tibialis anterior (KPa) | 379.0 [160.3] | 376.8 [208.4] | 0.91 |
| TS-acromion (0–10) | 3.0 [3.0] | 2.0 [3.0] | 0.62 |
| TS-tibialis anterior (0–10) | 3.0 [2.0] | 2.0 [2.3] | 0.15 |
| CPM during Cold Pressor Test (% change) | 82.2 ± 44.7 | 49.8 ± 42.5 | 0.02 * |
| CPM post-Cold Pressor Test (% change) | 7.2 ± 28.9 | 11.8 ± 32.5 | 0.64 |
| Psychosocial aspects | |||
| FABQ-Br | |||
| FABQ-PA | 15.1 ± 4.7 | 11.8 ± 6.4 | 0.08 |
| FABQ-W | 7.0 [13.0] | 8.5 [15.8] | 0.70 |
| TSK | 37.1 ± 3.2 | 35.9 ± 7.2 | 0.55 |
| PCS | |||
| Rumination | 6.7 ± 2.6 | 6.4 ± 3.4 | 0.80 |
| Magnification | 4.0 [5.0] | 3.0 [3.5] | 0.95 |
| Helplessness | 5.0 [10.0] | 3.0 [6.3] | 0.46 |
| CPSS | |||
| Pain management | 400.0 [110.0] | 390.0 [115.0] | 0.48 |
| Coping with symptoms | 612.0 ± 117.0 | 608.2 ± 109.2 | 0.91 |
| Physical function | 880.0 [110.0] | 875.0 [95.0] | 0.98 |
| Total score | 1950.0 [350.0] | 1860. [330.0] | 0.68 |
| DASS-21 | |||
| Depression | 0.0 [4.0] | 2.0 [3.0] | 0.43 |
| Anxiety | 1.0 [2.0] | 1.0 [2.3] | 0.41 |
| Stress | 1.0 [5.0] | 3.5 [7.3] | 0.47 |
| EQ-5 D | 0.82 [0.15] | 0.88 [0.11] | 0.93 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haik, M.N.; Alburquerque-Sendín, F.; Fernandes, R.A.S.; Kamonseki, D.H.; Almeida, L.A.; Liebano, R.E.; Camargo, P.R. Biopsychosocial Aspects in Individuals with Acute and Chronic Rotator Cuff Related Shoulder Pain: Classification Based on a Decision Tree Analysis. Diagnostics 2020, 10, 928. https://doi.org/10.3390/diagnostics10110928
Haik MN, Alburquerque-Sendín F, Fernandes RAS, Kamonseki DH, Almeida LA, Liebano RE, Camargo PR. Biopsychosocial Aspects in Individuals with Acute and Chronic Rotator Cuff Related Shoulder Pain: Classification Based on a Decision Tree Analysis. Diagnostics. 2020; 10(11):928. https://doi.org/10.3390/diagnostics10110928
Chicago/Turabian StyleHaik, Melina N, Francisco Alburquerque-Sendín, Ricardo A S Fernandes, Danilo H Kamonseki, Lucas A Almeida, Richard E Liebano, and Paula R Camargo. 2020. "Biopsychosocial Aspects in Individuals with Acute and Chronic Rotator Cuff Related Shoulder Pain: Classification Based on a Decision Tree Analysis" Diagnostics 10, no. 11: 928. https://doi.org/10.3390/diagnostics10110928
APA StyleHaik, M. N., Alburquerque-Sendín, F., Fernandes, R. A. S., Kamonseki, D. H., Almeida, L. A., Liebano, R. E., & Camargo, P. R. (2020). Biopsychosocial Aspects in Individuals with Acute and Chronic Rotator Cuff Related Shoulder Pain: Classification Based on a Decision Tree Analysis. Diagnostics, 10(11), 928. https://doi.org/10.3390/diagnostics10110928







