Clinical versus Ultrasound Measurements of Hyomental Distance Ratio for the Prediction of Difficult Airway in Patients with and without Morbid Obesity
Abstract
:1. Introduction
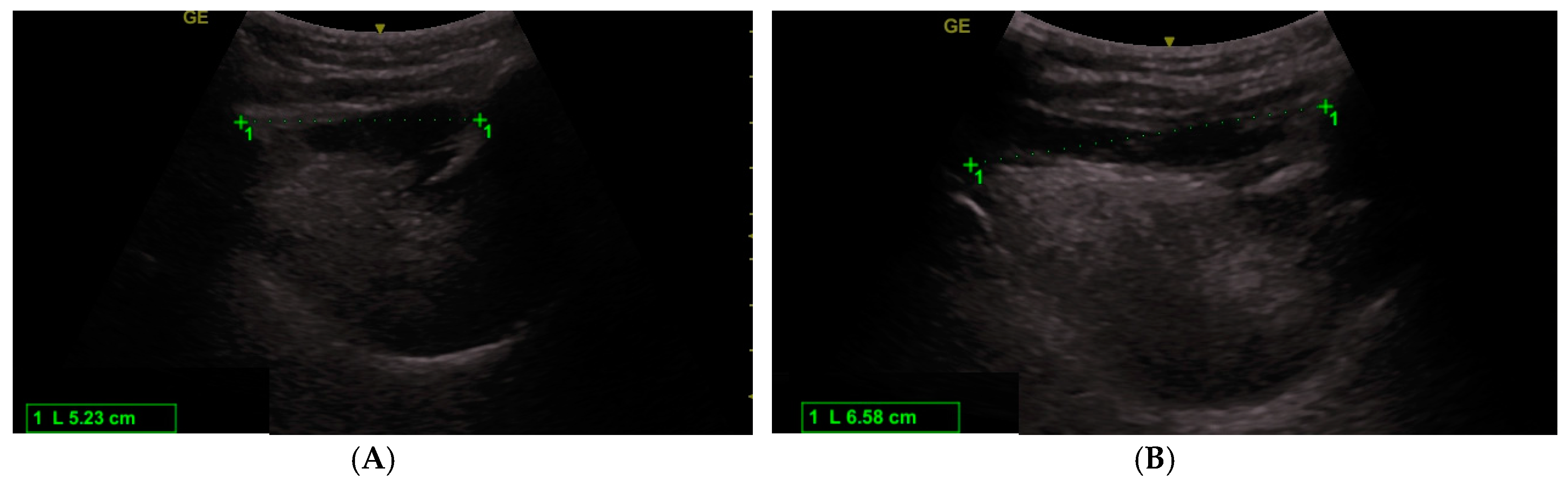
2. Materials and Methods
Data Analysis
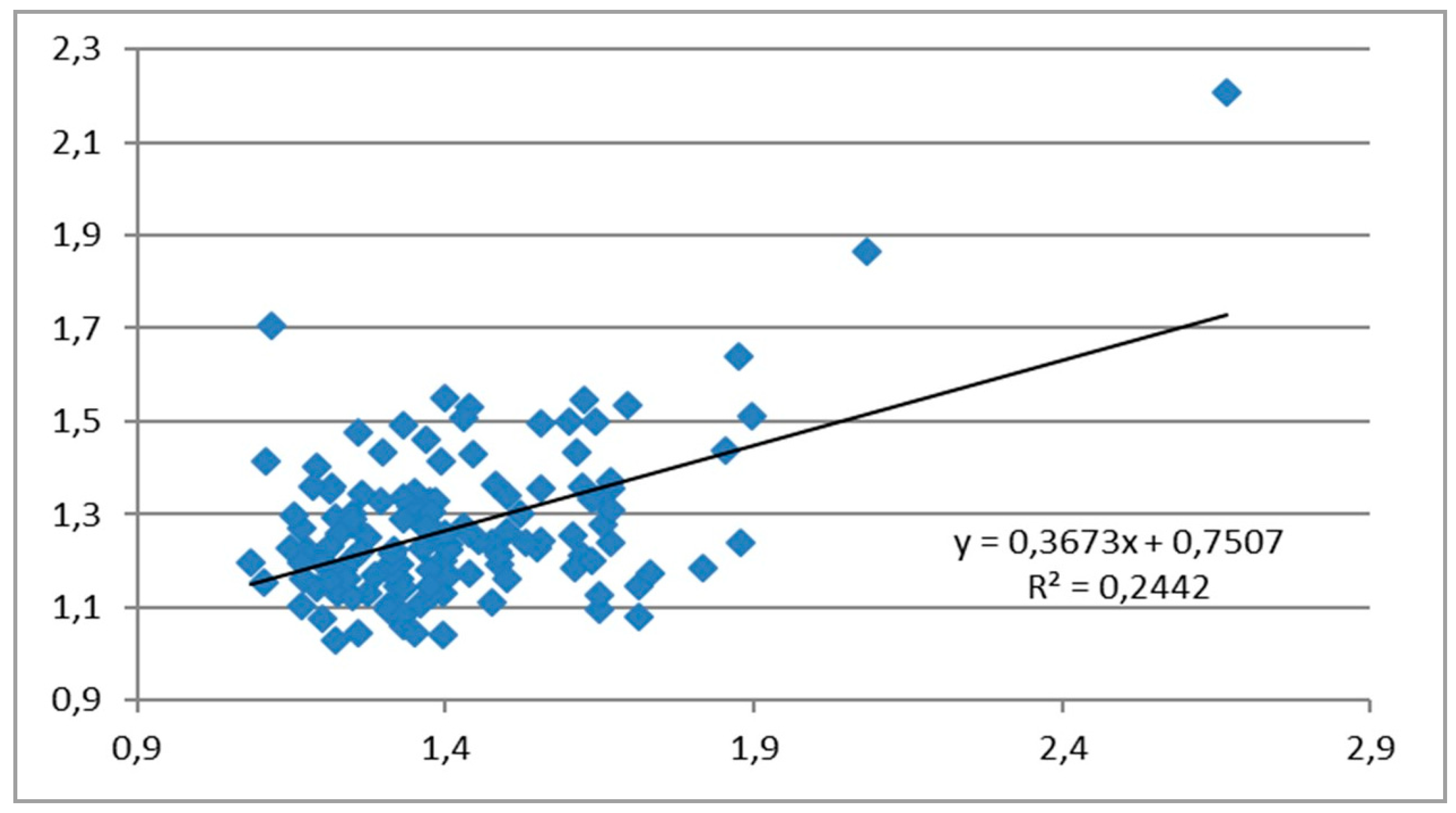
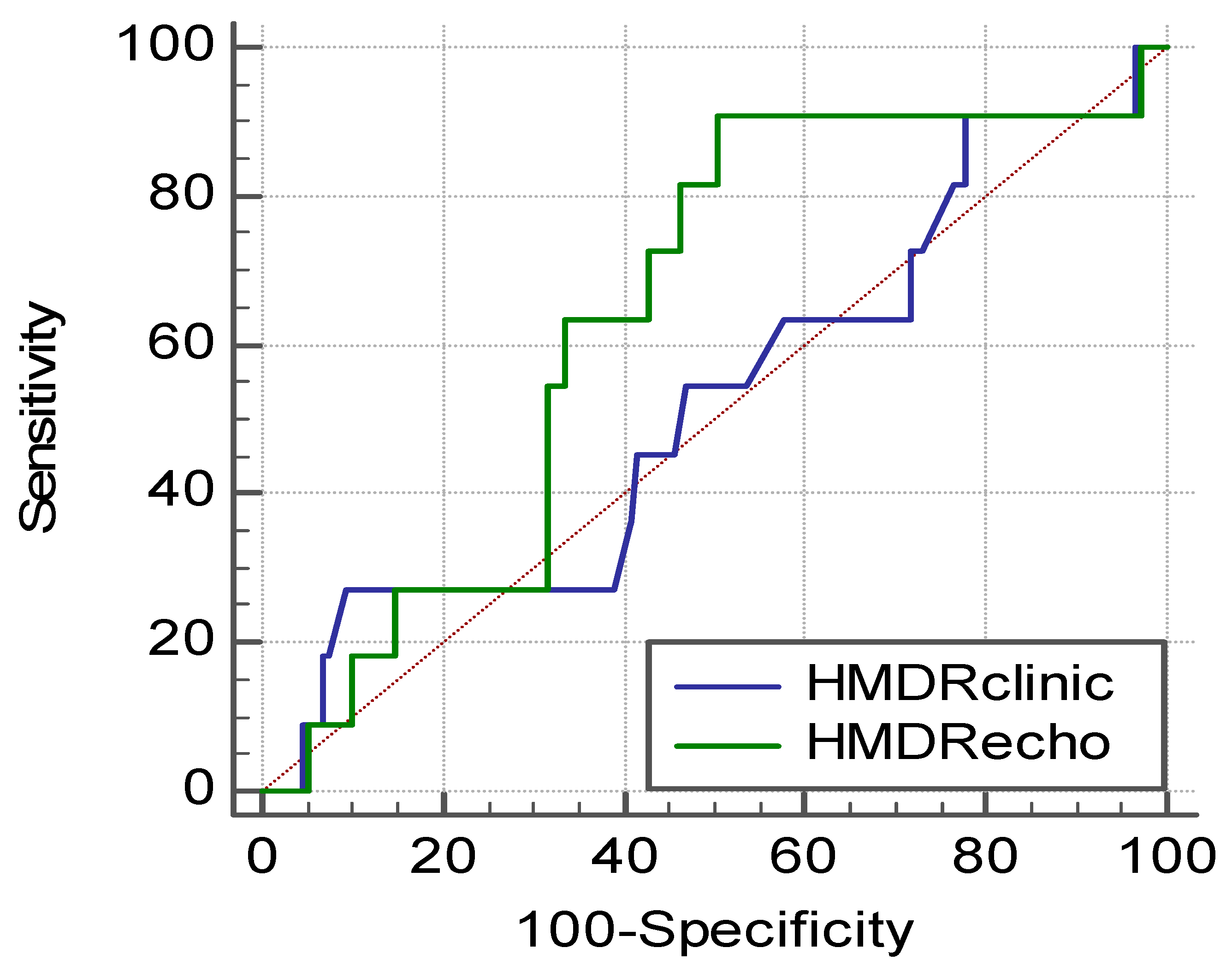
3. Results
4. Discussion
4.1. Clinical Studies
4.2. Imaging Studies
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Det, M.E.; Jivraj, N.; Adhikari, N.K.; Friedrich, J.O.; Pinto, R.; Simel, D.L.; Wijeysundera, D.N.; Scales, D.C. Will this patient be difficult to intubate? the rational clinical examination systematic review. JAMA 2019, 321, 493–503. [Google Scholar]
- Petrisor, C.; Dîrzu, D.; Trancă, S.; Hagău, N.; Bodolea, C. Preoperative difficult airway prediction using suprahyoid and infrahyoid ultrasonography derived measurements in anesthesiology. Med. U-ltrasonography 2019, 21, 83–88. [Google Scholar] [CrossRef]
- Huh, J.; Shin, H.Y.; Kim, S.H.; Yoon, T.K.; Kim, D.K. Diagnostic predictor of difficult laryngoscopy: The HMD ratio. Anesth. Analg. 2009, 108, 544–548. [Google Scholar] [CrossRef]
- Honarmand, A.; Safavi, M.; Ansari, N. A comparison of between hyomental distance ratios, ratio of height to thyromental, modified Mallamapati classification test and upper lip bite test in predicting difficult laryngoscopy of patients undergoing general anesthesia. Adv. Biomed. Res. 2014, 3, 166. [Google Scholar]
- Kalezić, N.; Lakićević, M.; Miličić, B.; Stojanović, M.; Sabljak, V.; Marković, D. HMD in the different head positions and HMD ratio in predicting difficult intubation. Bosn. J. basic Med. Sci. 2016, 16, 232. [Google Scholar]
- Montemayor-Cruz, J.M.; Guerrero-Ledezma, R.M. Diagnostic utility of the HMD ratio as predictor of difficult intubation at UMAE 25. Gac. Med. Mex. 2015, 151, 559–566. [Google Scholar]
- Tantri, A.R.; Firdaus, R.; Salomo, S.T. Predictors of difficult intubation among Malay patients in Indonesia. Anesthesiol. Pain Med. 2016, 6, e34848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rao, S.T.; Gowda, V.; Reddy, R.V. HMD ratio as a diagnostic predictor of difficult laryngoscopy. Indian J. Appl. Res. 2013, 3, 511–513. [Google Scholar] [CrossRef]
- Rana, S.; Verma, V.; Bhandari, S.; Sharma, S.; Koundal, V.; Chaudhary, S.K. Point-of-care ultrasound in the airway assessment: A correlation of ultrasonography-guided parameters to the Cormack–Lehane Classification. Saudi J. Anaesth. 2018, 12, 292. [Google Scholar] [CrossRef]
- Petrisor, C.; Szabo, R.; Constantinescu, C.; Prie, A.; Tranca, S.; Hagau, N. The performance of ultrasound-based quantification of the hyomental distance ratio in predicting difficult airway in anaesthesia: A STARD-compliant prospective diagnostic study. Eur. J. Anaesthesiol. 2018, 35, 627–628. [Google Scholar] [CrossRef]
- Petrisor, C.; Szabo, R.; Constantinescu, C.; Prie, A.; Hagau, N. Ultrasound-based assessment of hyomental distances in neutral, ramped, and maximum hyperextended positions, and derived ratios, for the prediction of difficult airway in the obese population: A pilot diagnostic accuracy study. Anaesthesiol. Intensive Ther. 2018, 50, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Koundal, V.; Rana, S.; Thakur, R.; Chauhan, V.; Ekke, S.; Kumar, M. The usefulness of point of care ultrasound (POCUS) in preanaesthetic airway assessment. Indian J. Anaesth. 2019, 63, 1022. [Google Scholar] [PubMed]
- Andruszkiewicz, P.; Wojtczak, J.; Sobczyk, D.; Stach, O.; Kowalik, I. Effectiveness and validity of sonographic upper airway evaluation to predict difficult laryngoscopy. J. Ultrasound Med. 2016, 35, 2243–2252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Budde, A.O.; Desciak, M.; Reddy, V.; Falcucci, O.A.; Vaida, S.J.; Pott, L.M. The prediction of difficult intubation in obese patients using mirror indirect laryngoscopy: A prospective pilot study. J. Anaesthesiol. Clini. Pharmacol. 2013, 29, 183. [Google Scholar] [CrossRef]
- Shiga, T.; Wajima, Z.I.; Inoue, T.; Sakamoto, A. Predicting Difficult Intubation in Apparently Normal PatientsA Meta-analysis of Bedside Screening Test Performance. Anesthesiology 2005, 103, 429–437. [Google Scholar] [CrossRef]
- Samsoon, G.L.; Young, J.R. Difficult tracheal intubation: A retrospective study. Anaesthesia 1987, 42, 487–490. [Google Scholar] [CrossRef]
- Khan, Z.H.; Mohammadi, M.; Rasouli, M.R.; Farrokhnia, F.; Khan, R.H. The diagnostic value of the upper lip bite test combined with sternomental distance, thyromental distance, and interincisor distance for prediction of easy laryngoscopy and intubation: A prospective study. Anesth. Analg. 2009, 109, 822–824. [Google Scholar] [CrossRef] [Green Version]
- Wojtczak, J.A. Submandibular sonography assessment of HMDs and ratio, tongue size, and floor of the mouth musculature using portable sonography. J. Ultrasound Med. 2012, 31, 523–528. [Google Scholar] [CrossRef]
- Wojtczak, J.; Bonadonna, P. Pocket mobile smartphone system for the point-of-care submandibular ultrasonography. Am. J. Emerg. Med. 2013, 31, 573–577. [Google Scholar] [CrossRef]
- El-Orbany, M.; Woehlck, H.; Salem, M.R. Head and neck position for direct laryngoscopy. Anesth. Analg. 2011, 113, 103–109. [Google Scholar] [CrossRef]
- Cormack, R.S.; Lehane, J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984, 39, 1105–1111. [Google Scholar] [CrossRef] [PubMed]
- Siriussawakul, A.; Maboonyanon, P.; Kueprakone, S.; Samankatiwat, S.; Komoltri, C.; Thanakiattiwibun, C. Predictive performance of a multivariable difficult intubation model for obese patients. PLoS ONE 2018, 13, e0203142. [Google Scholar] [CrossRef] [PubMed]
- Greenland, K.B. Airway assessment based on a three column model of direct laryngoscopy. Anaesth. Intensive Care 2010, 38, 14–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ji, C.; Ni, Q.; Chen, W. Diagnostic accuracy of radiology (CT, X-ray, US) for predicting difficult intubation in adults: A meta-analysis. J. Clin. Anesth. 2018, 45, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Šustic, A. Role of ultrasound in the airway management of critically ill patients. Crit. Care. Med. 2007, 35, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Juvin, P.; Lavaut, E.; Dupont, H.; Lefevre, P.; Demetriou, M.; Dumoulin, J.L. Difficult tracheal intubation is more common in obese than in lean patients. Anesth. Analg. 2003, 97, 595–600. [Google Scholar] [CrossRef]
- Ezri, T.; Gewürtz, G.; Sessler, D.I.; Medalion, B.; Szmuk, P.; Hagberg, C.; Susmallian, S. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia 2003, 58, 1111–1114. [Google Scholar] [CrossRef]

| Patients without Morbid Obesity | Patients with Morbid Obesity | p-Value | |
|---|---|---|---|
| N | 139 | 21 | |
| BMI (kg/m2) | 28.23 ± 4.93 | 48.30 ± 7.45 | <0.001 |
| Neck circumference (cm) | 42.56 ± 5.04 | 47.86 ± 5.11 | <0.001 |
| Mallampati scores 3 and 4 | 27/139 (19.42%) | 9/20 (42.85%) | 0.016 |
| ULBT | 14 edentolous patients 1/125 | 1 patient edentolous 0/20 | 0.54 |
| HMDclin neutral | 4.36 ± 0.90 | 4.54 ± 1.04 | 0.46 |
| HMDclin extended | 6.09 ± 1.31 | 6.34 ± 1.59 | 0.50 |
| HMDRclin | 1.40 ± 0.21 | 1.41 ± 0.33 | 0.92 |
| HMDecho neutral | 4.16 ± 0.49 | 4.75 ± 0.47 | 0.54 |
| HMDecho extended | 5.23 ± 0.59 | 5.71 ± 0.63 | 0.0036 |
| HMDRecho | 1.26 ± 0.16 | 1.20 ± 0.07 | 0.00314 |
| Cormack–Lehane score III/IV | 9/139 (6.47%) | 2/21 (9.52%) | 0.60 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petrișor, C.; Trancă, S.; Szabo, R.; Simon, R.; Prie, A.; Bodolea, C. Clinical versus Ultrasound Measurements of Hyomental Distance Ratio for the Prediction of Difficult Airway in Patients with and without Morbid Obesity. Diagnostics 2020, 10, 140. https://doi.org/10.3390/diagnostics10030140
Petrișor C, Trancă S, Szabo R, Simon R, Prie A, Bodolea C. Clinical versus Ultrasound Measurements of Hyomental Distance Ratio for the Prediction of Difficult Airway in Patients with and without Morbid Obesity. Diagnostics. 2020; 10(3):140. https://doi.org/10.3390/diagnostics10030140
Chicago/Turabian StylePetrișor, Cristina, Sebastian Trancă, Robert Szabo, Robert Simon, Adrian Prie, and Constantin Bodolea. 2020. "Clinical versus Ultrasound Measurements of Hyomental Distance Ratio for the Prediction of Difficult Airway in Patients with and without Morbid Obesity" Diagnostics 10, no. 3: 140. https://doi.org/10.3390/diagnostics10030140
APA StylePetrișor, C., Trancă, S., Szabo, R., Simon, R., Prie, A., & Bodolea, C. (2020). Clinical versus Ultrasound Measurements of Hyomental Distance Ratio for the Prediction of Difficult Airway in Patients with and without Morbid Obesity. Diagnostics, 10(3), 140. https://doi.org/10.3390/diagnostics10030140





