Advanced Ankle and Foot Sonoanatomy: Imaging Beyond the Basics
Abstract
:1. Introduction
2. Ligaments
2.1. Bassett’s Ligament
2.1.1. Anatomy
2.1.2. Scanning Technique
2.1.3. Clinical Relevance
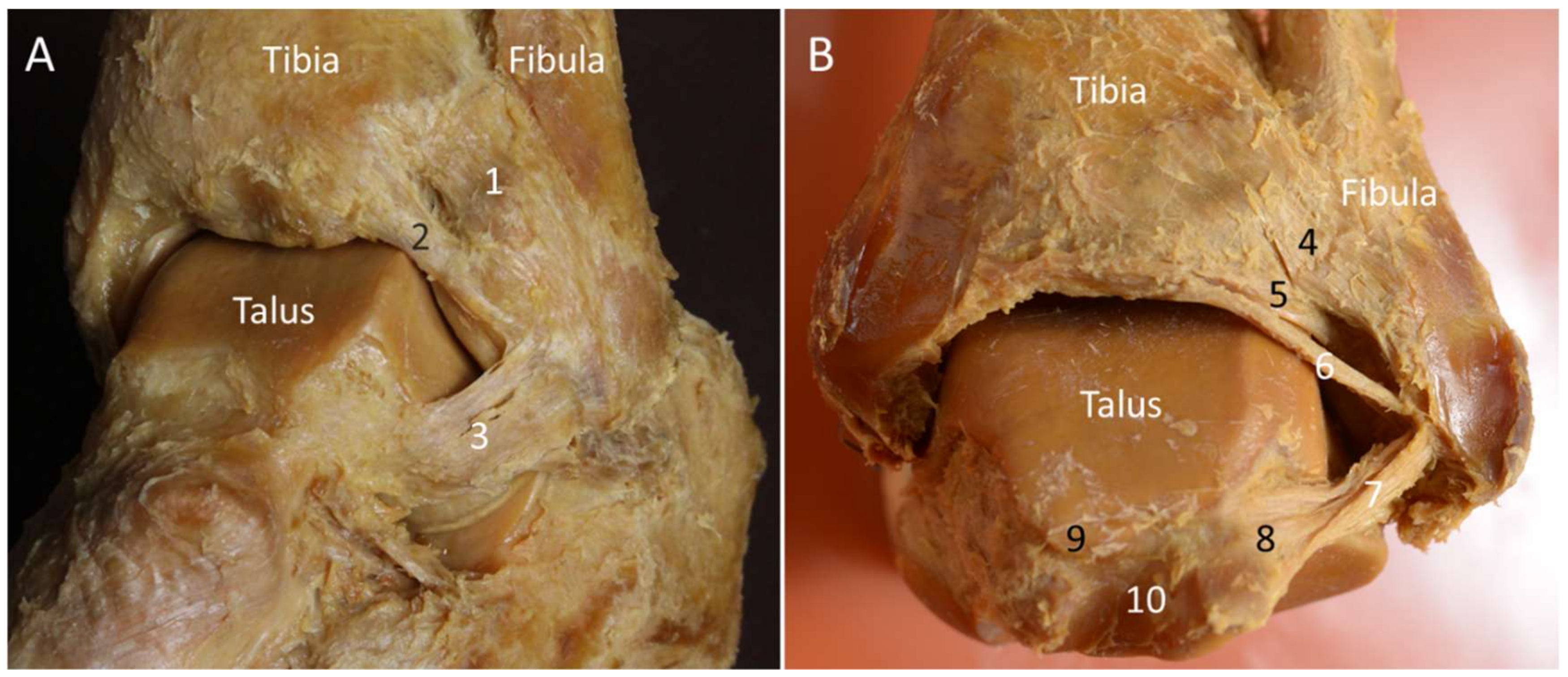
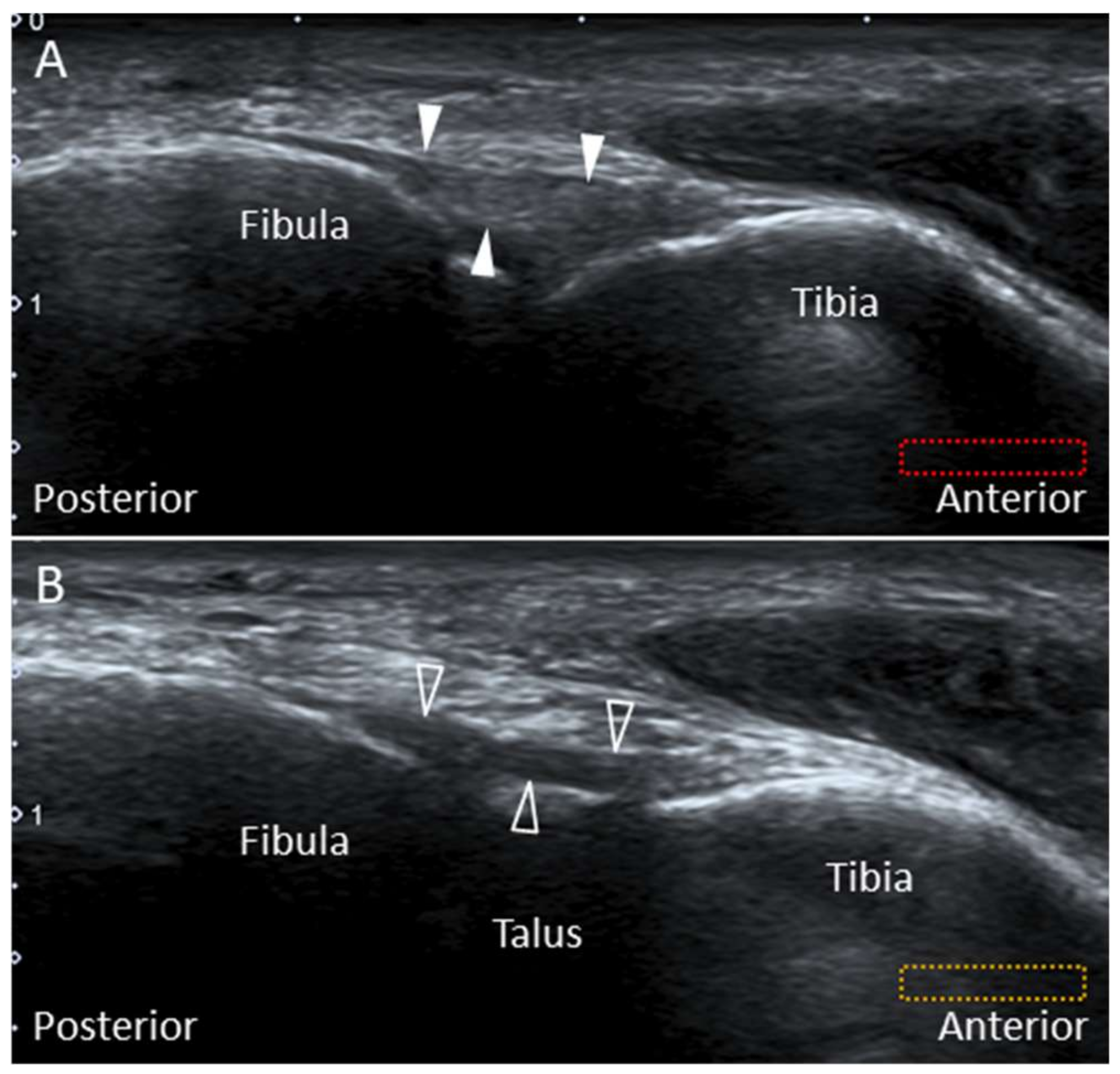
2.2. Posterior Inferior Tibiofibular Ligament
2.2.1. Anatomy
2.2.2. Scanning Technique
2.2.3. Clinical Relevance
2.3. Intermalleolar Ligament
2.3.1. Anatomy
2.3.2. Scanning Technique
2.3.3. Clinical Relevance
2.4. Posterior Talofibular Ligament (PTFL)
2.4.1. Anatomy
2.4.2. Scanning Technique
2.4.3. Clinical Relevance
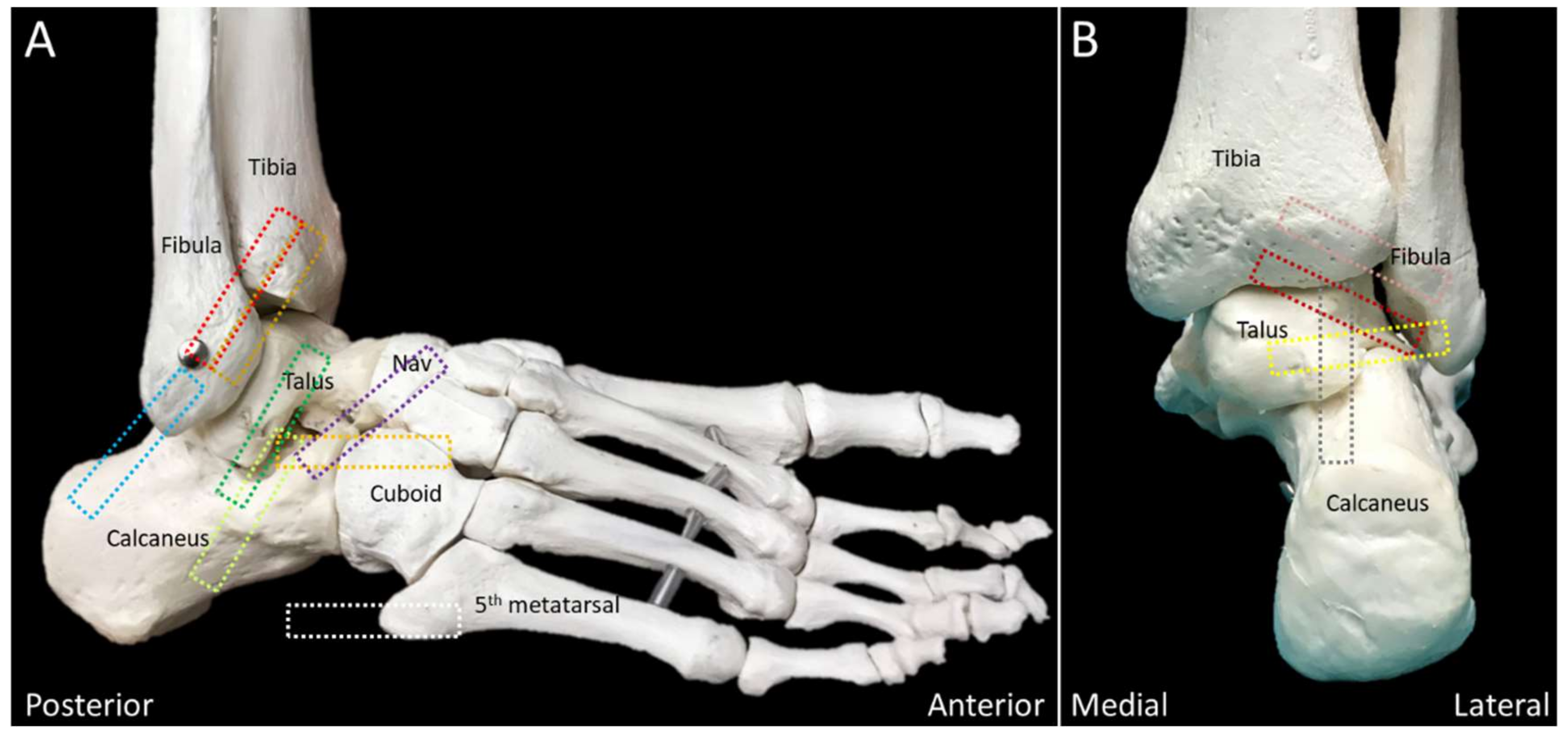
2.5. Lateral Talocalcaneal Ligament
2.5.1. Anatomy
2.5.2. Scanning Technique
2.5.3. Clinical Relevance
2.6. Bifurcate Ligament
2.6.1. Anatomy
2.6.2. Scanning Technique
2.6.3. Clinical Relevance
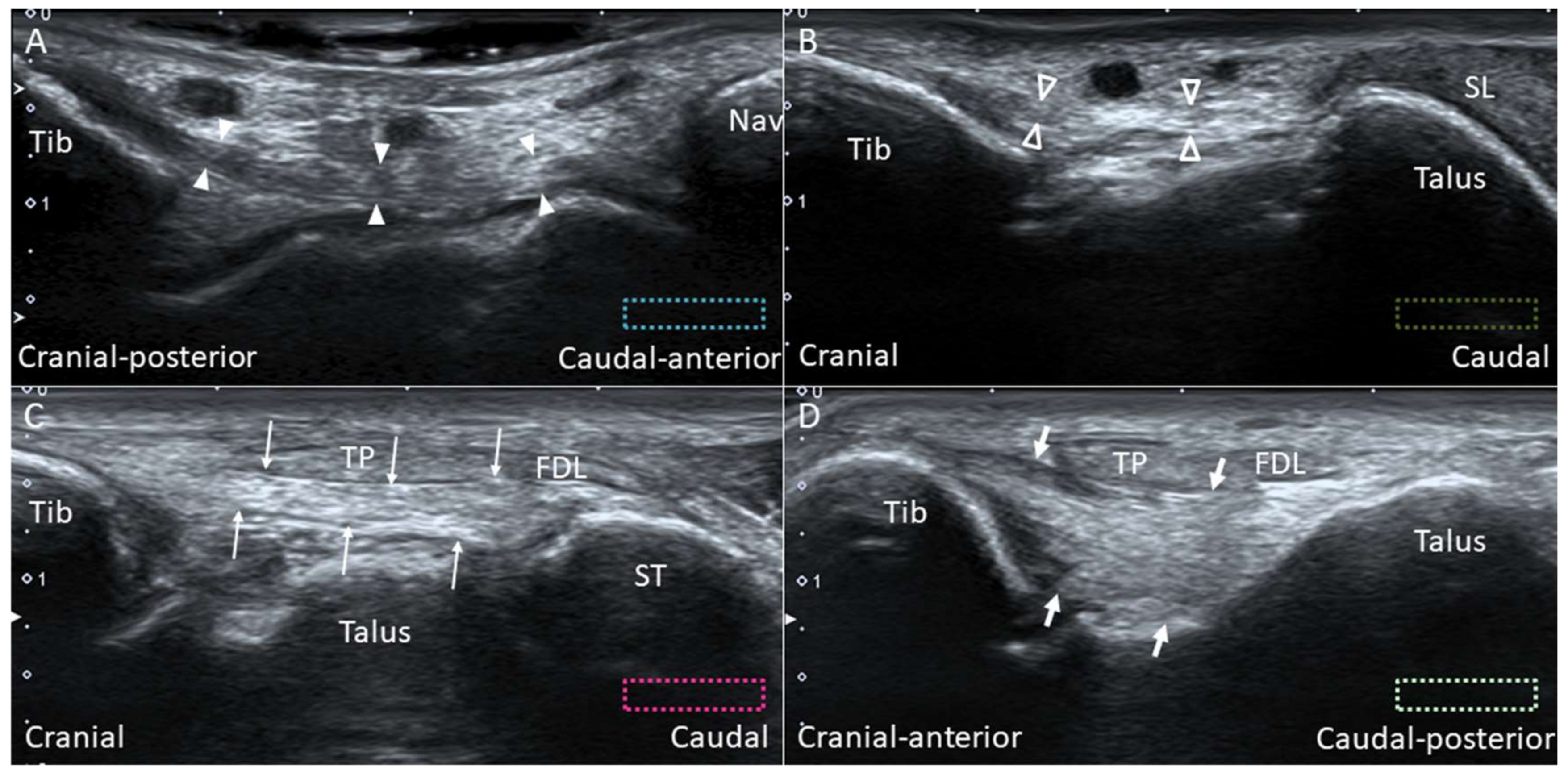
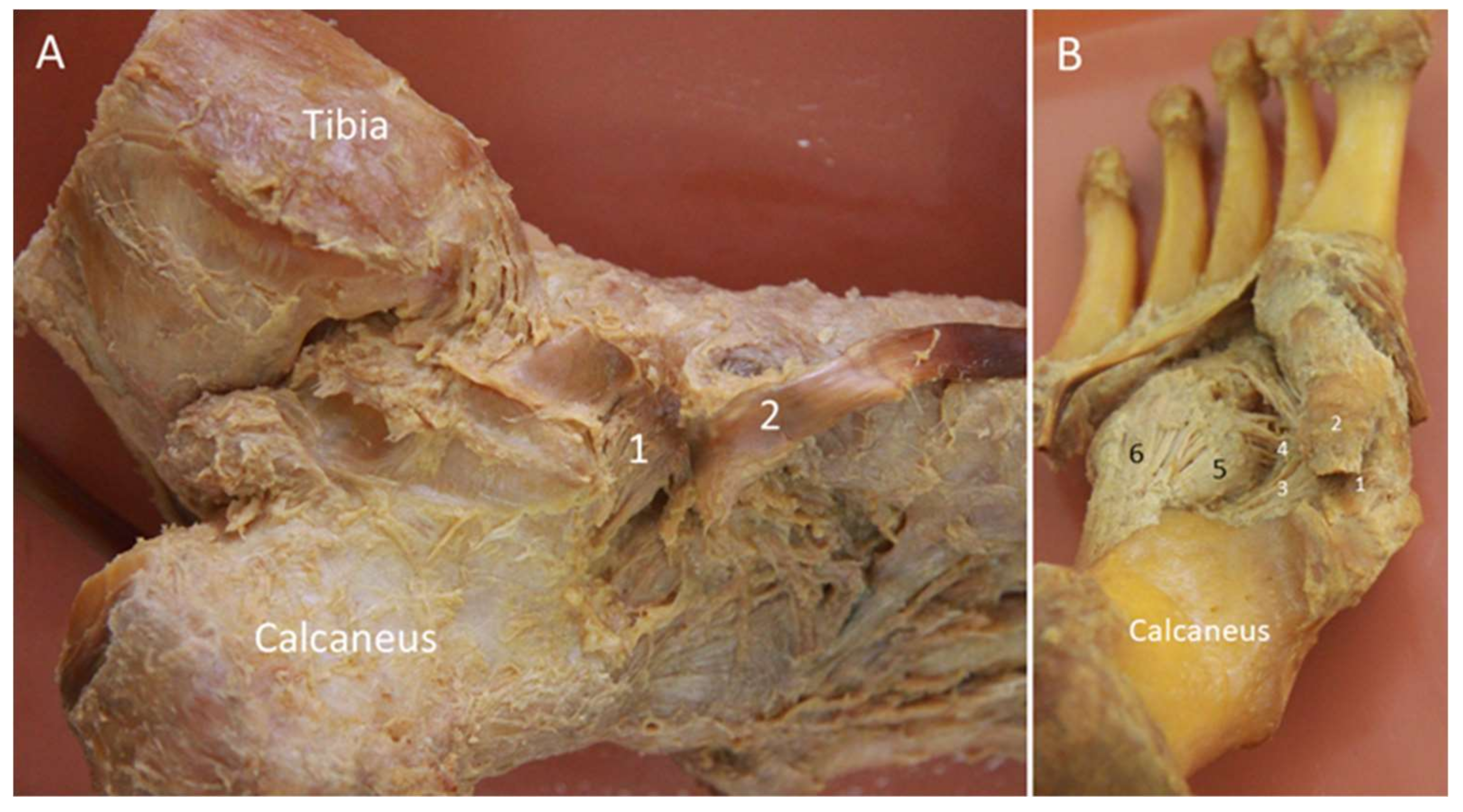
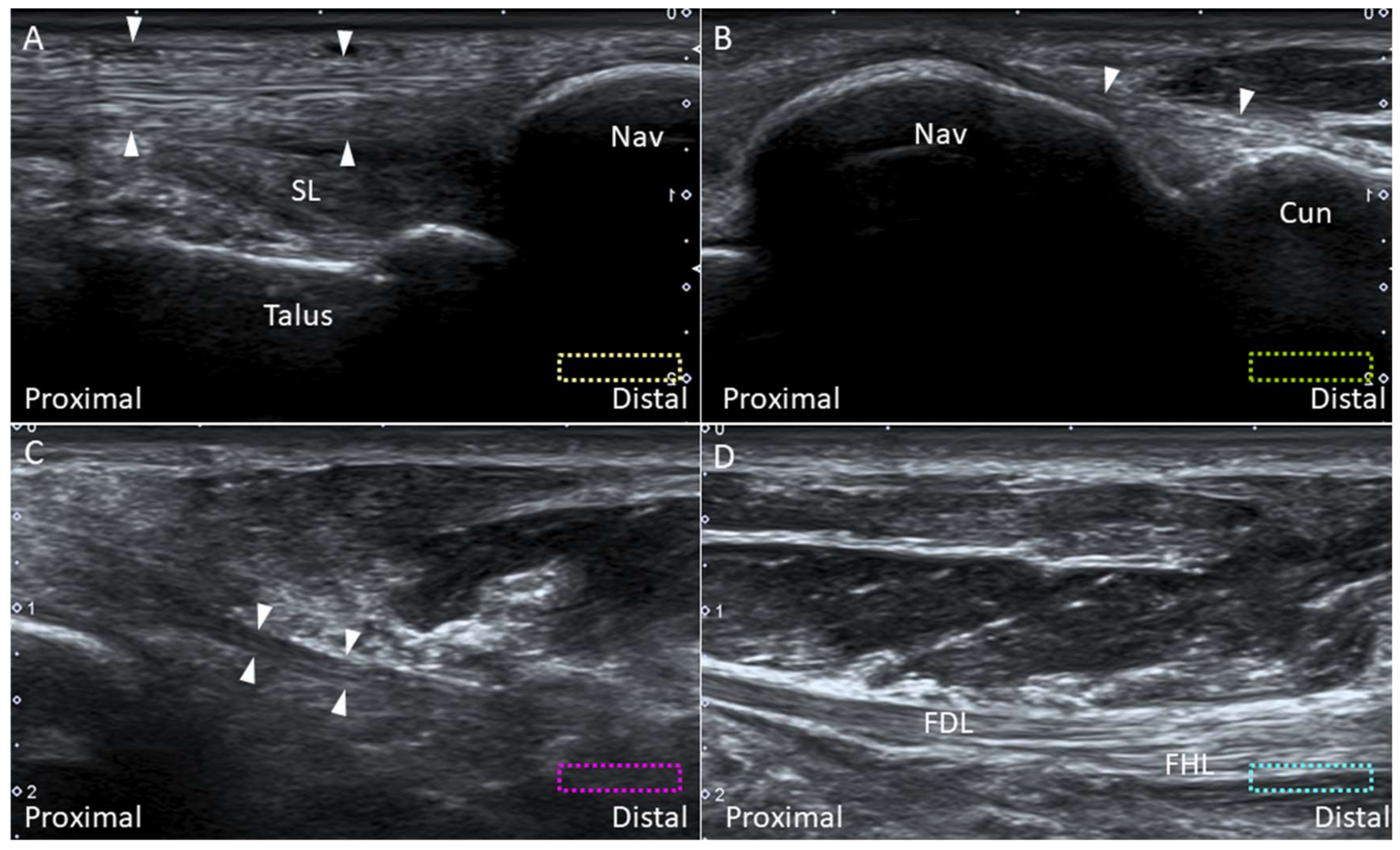
2.7. Deltoid Ligament
2.7.1. Anatomy
2.7.2. Scanning Technique
2.7.3. Clinical Relevance
2.8. Spring Ligament
2.8.1. Anatomy
2.8.2. Scanning Technique
2.8.3. Clinical Relevance
2.9. Plantar Ligament
2.9.1. Anatomy
2.9.2. Scanning Technique
2.9.3. Clinical Relevance
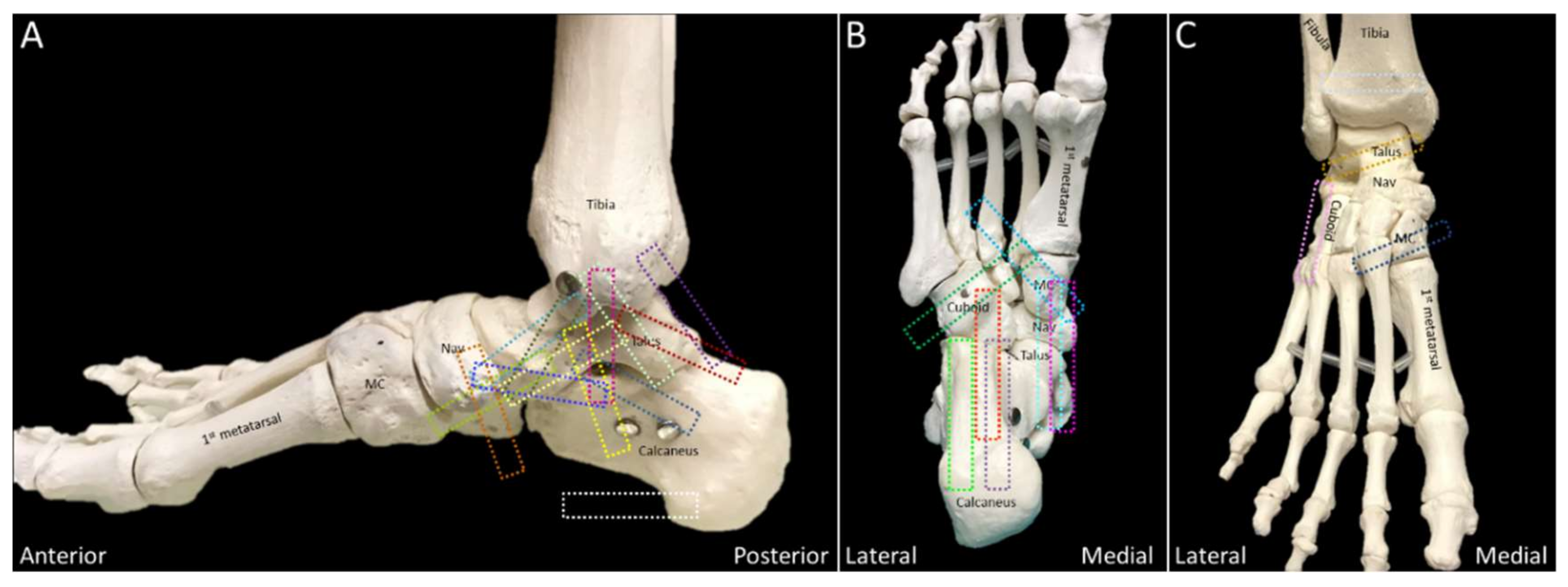
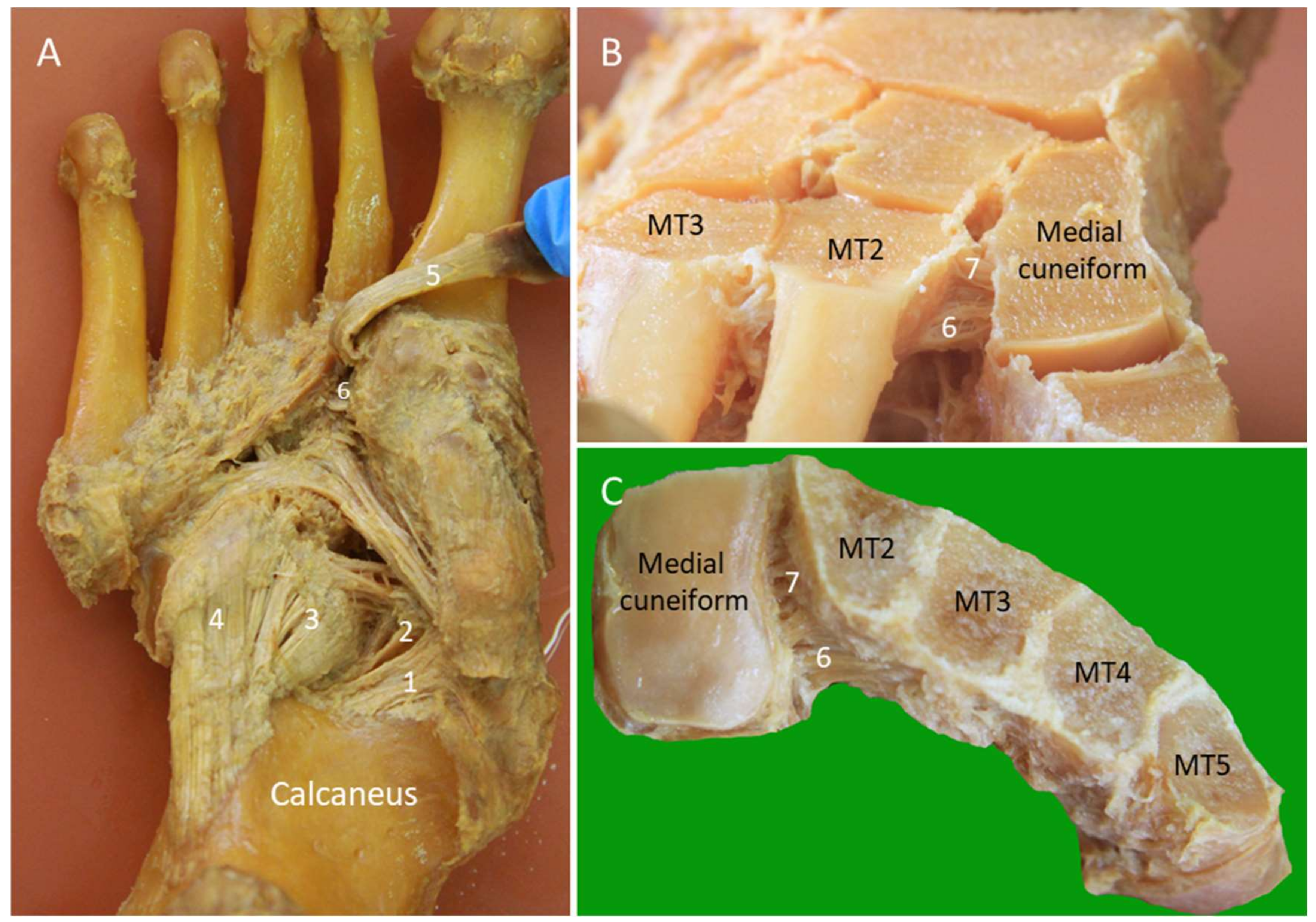
2.10. Lisfranc Ligament Complex
2.10.1. Anatomy
2.10.2. Scanning Technique
2.10.3. Clinical Relevance
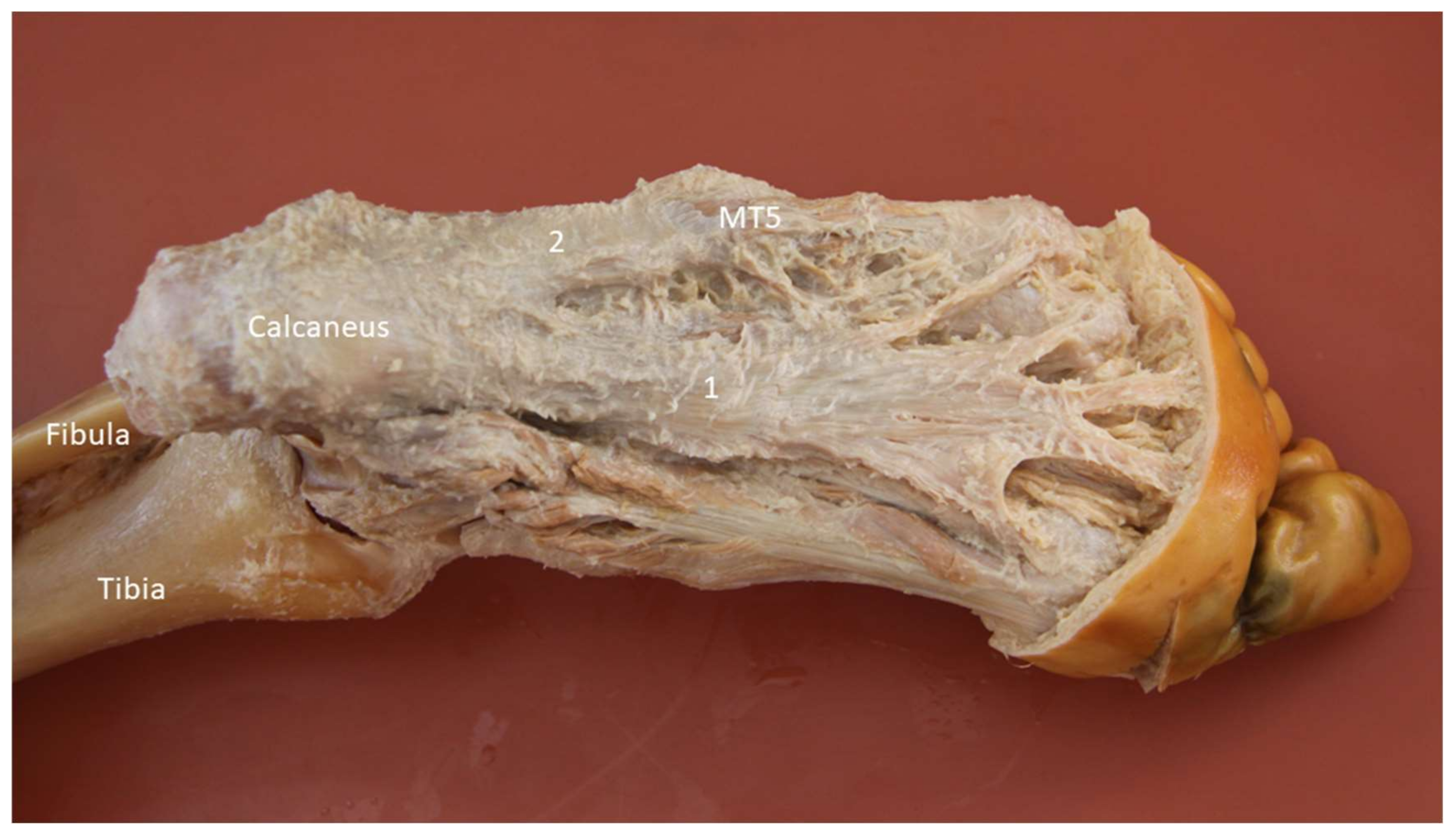
2.11. Lateral Cord of the Plantar Fascia
2.11.1. Anatomy
2.11.2. Scanning Technique
2.11.3. Clinical Relevance
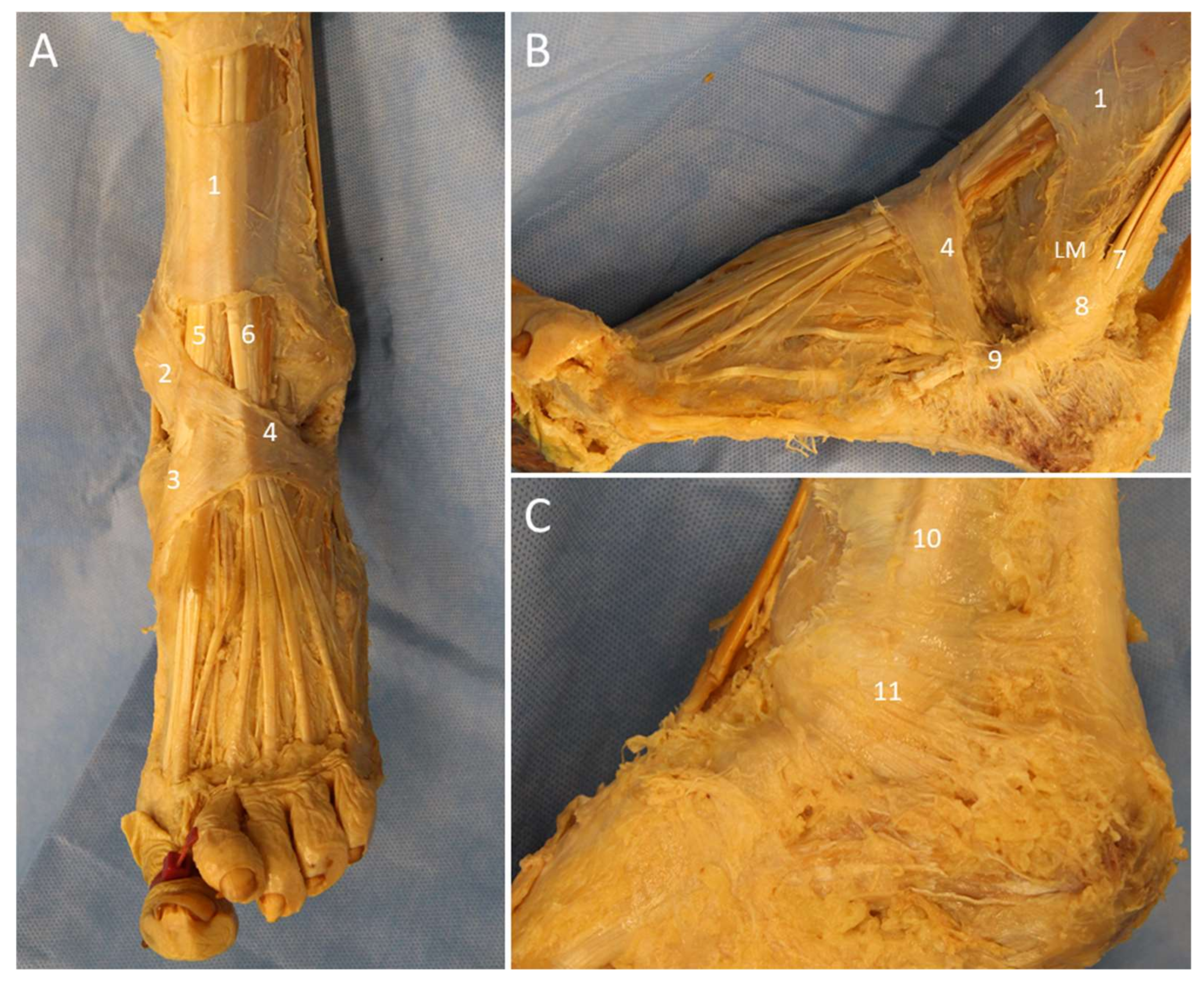
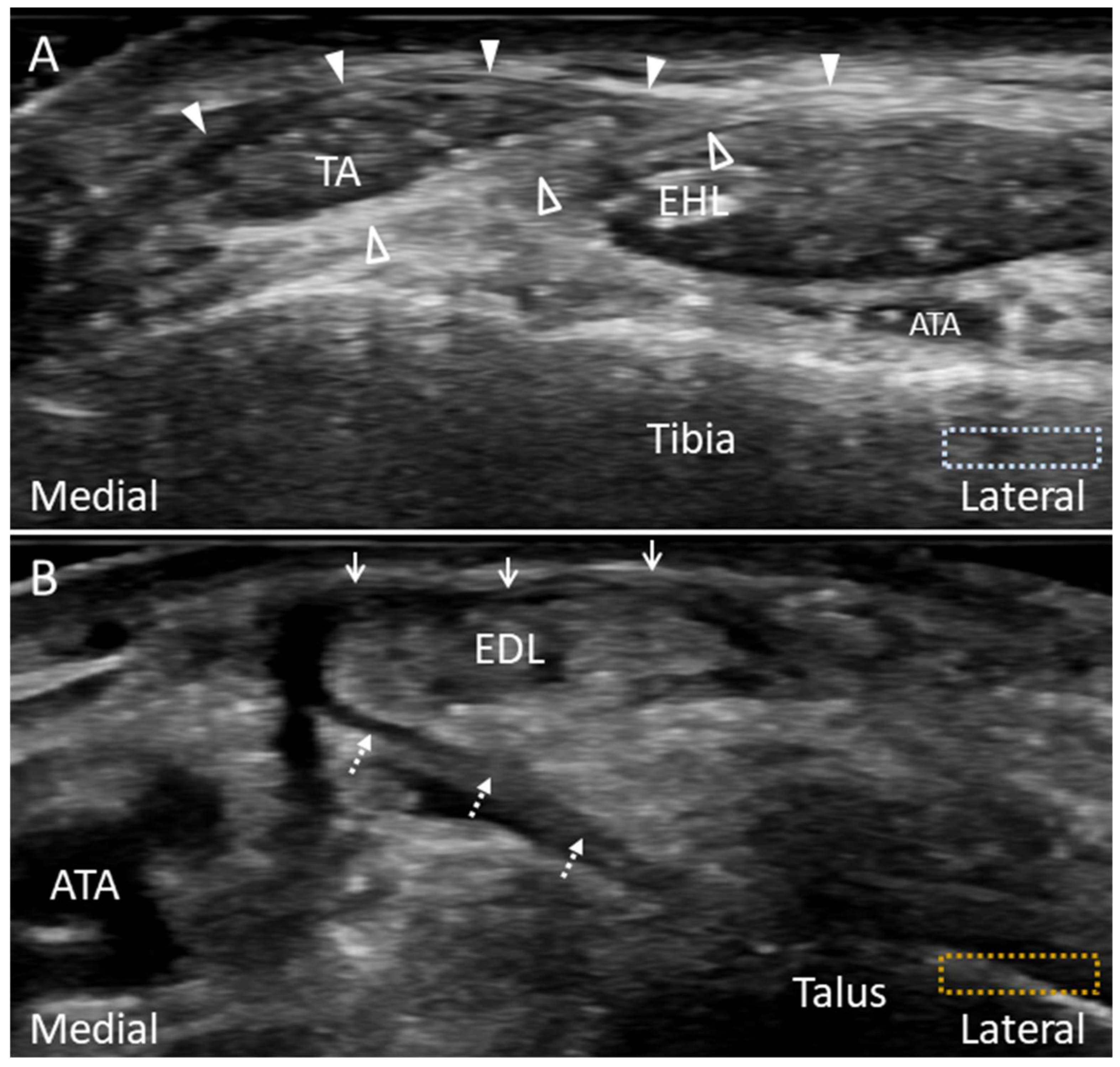
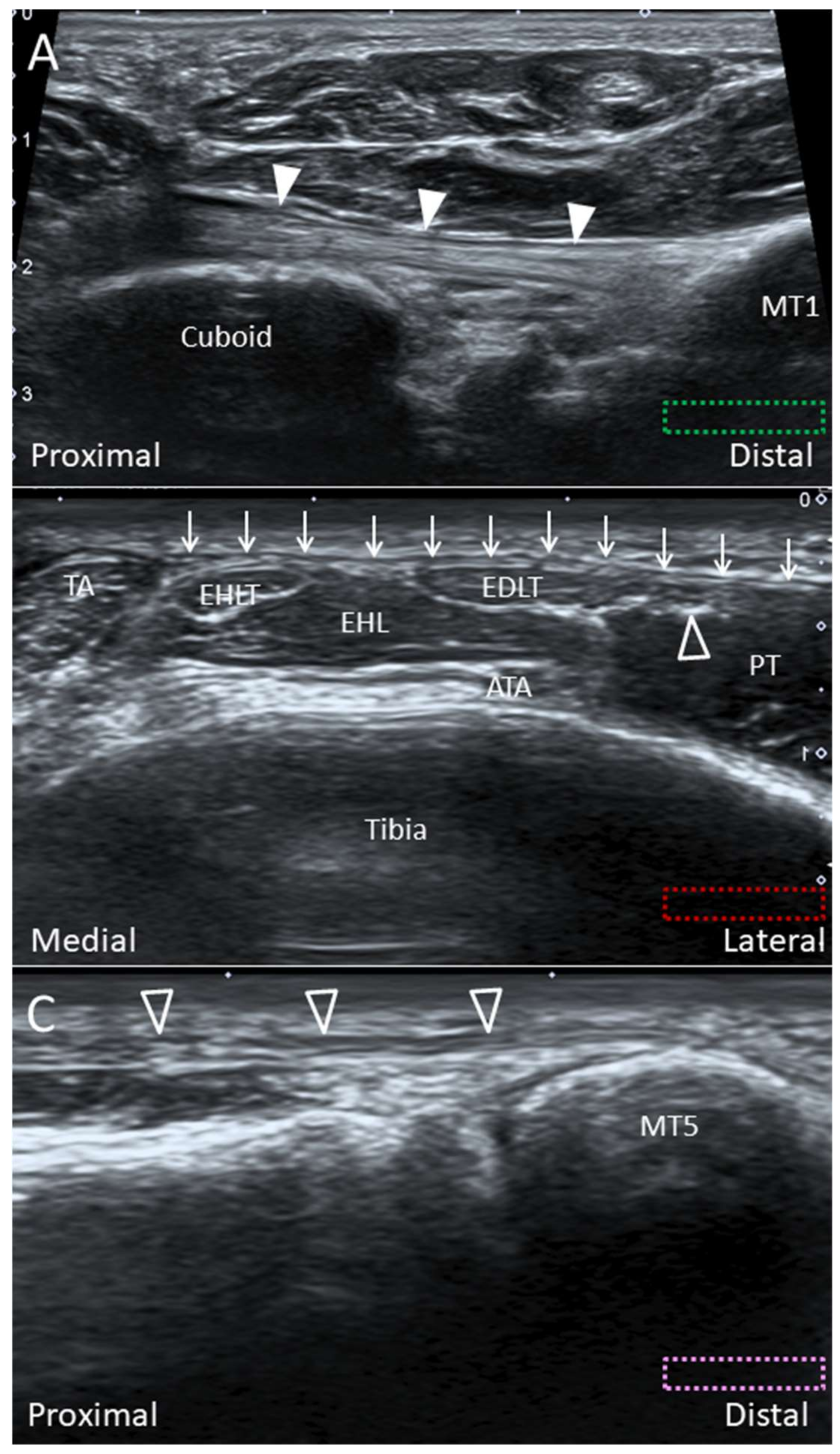
3. Retinacula
3.1. Anatomy
3.2. Scanning Technique
3.3. Clinical Relevance
4. Tendons
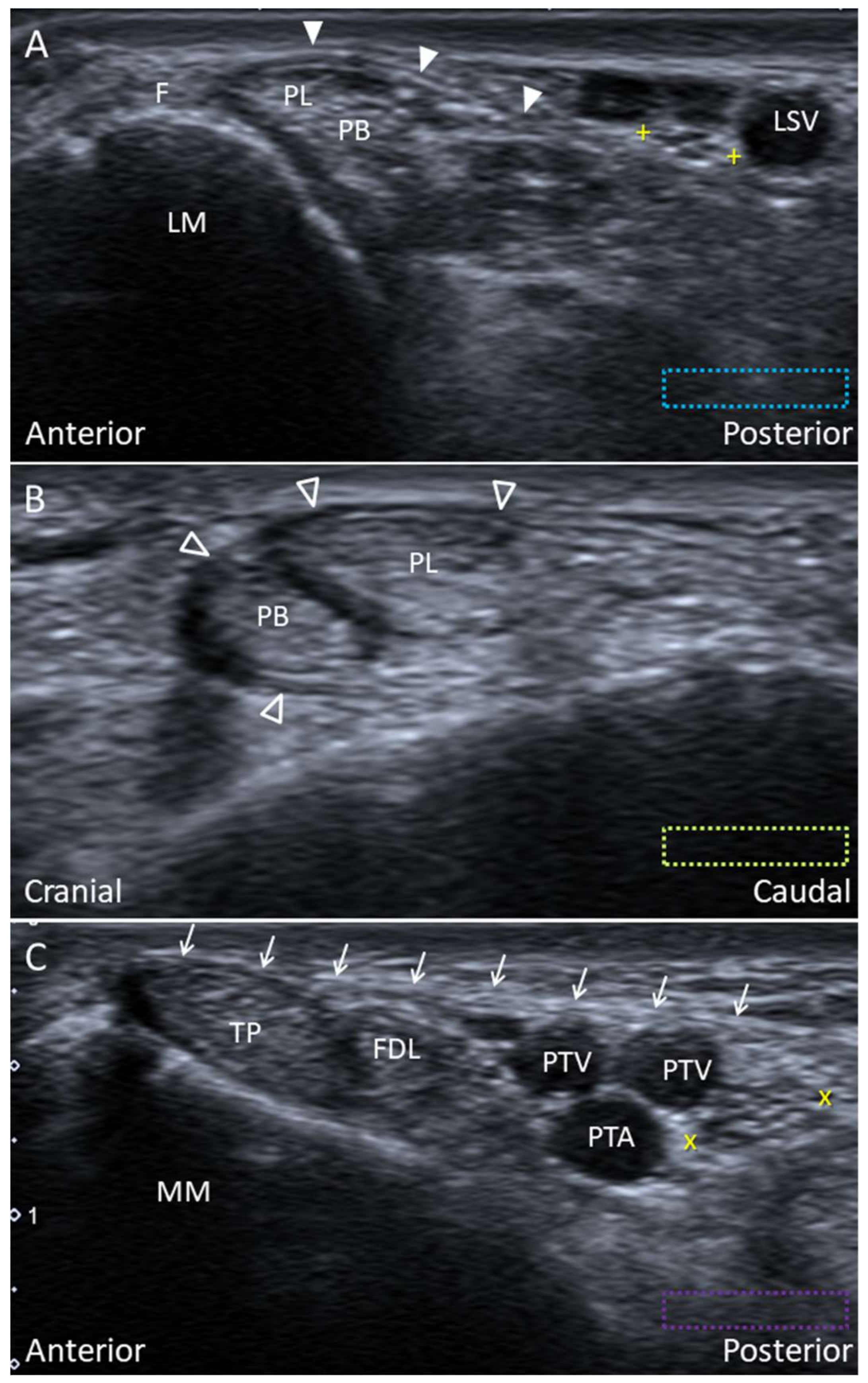
4.1. Peroneus Longus Tendon
4.1.1. Anatomy
4.1.2. Scanning Technique
4.1.3. Clinical Relevance
4.2. Peroneus Tertius Tendon
4.2.1. Anatomy
4.2.2. Scanning Technique
4.2.3. Clinical Relevance
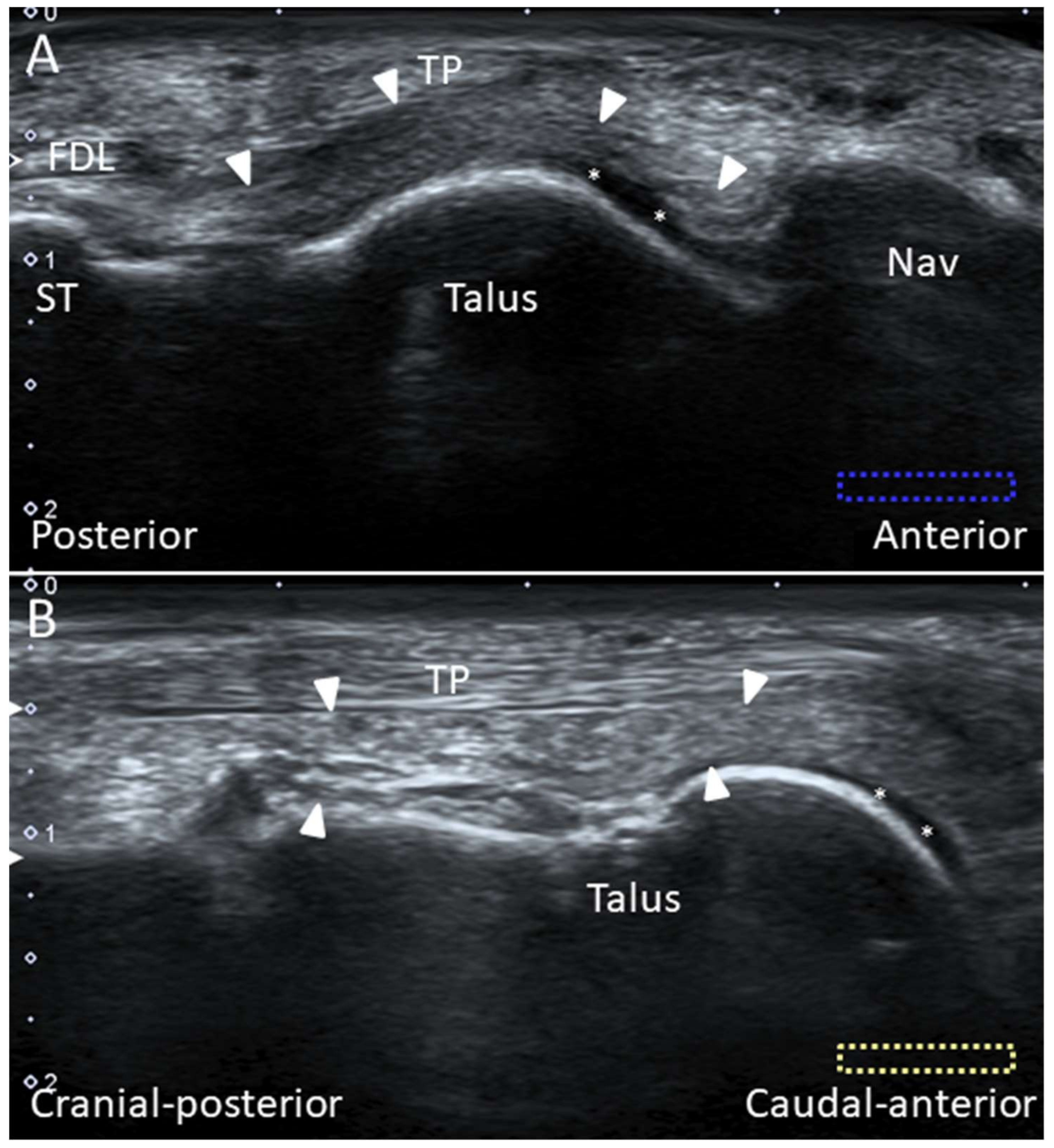
4.3. Tibialis Posterior Tendon
4.3.1. Anatomy
4.3.2. Scanning Technique
4.3.3. Clinical Relevance
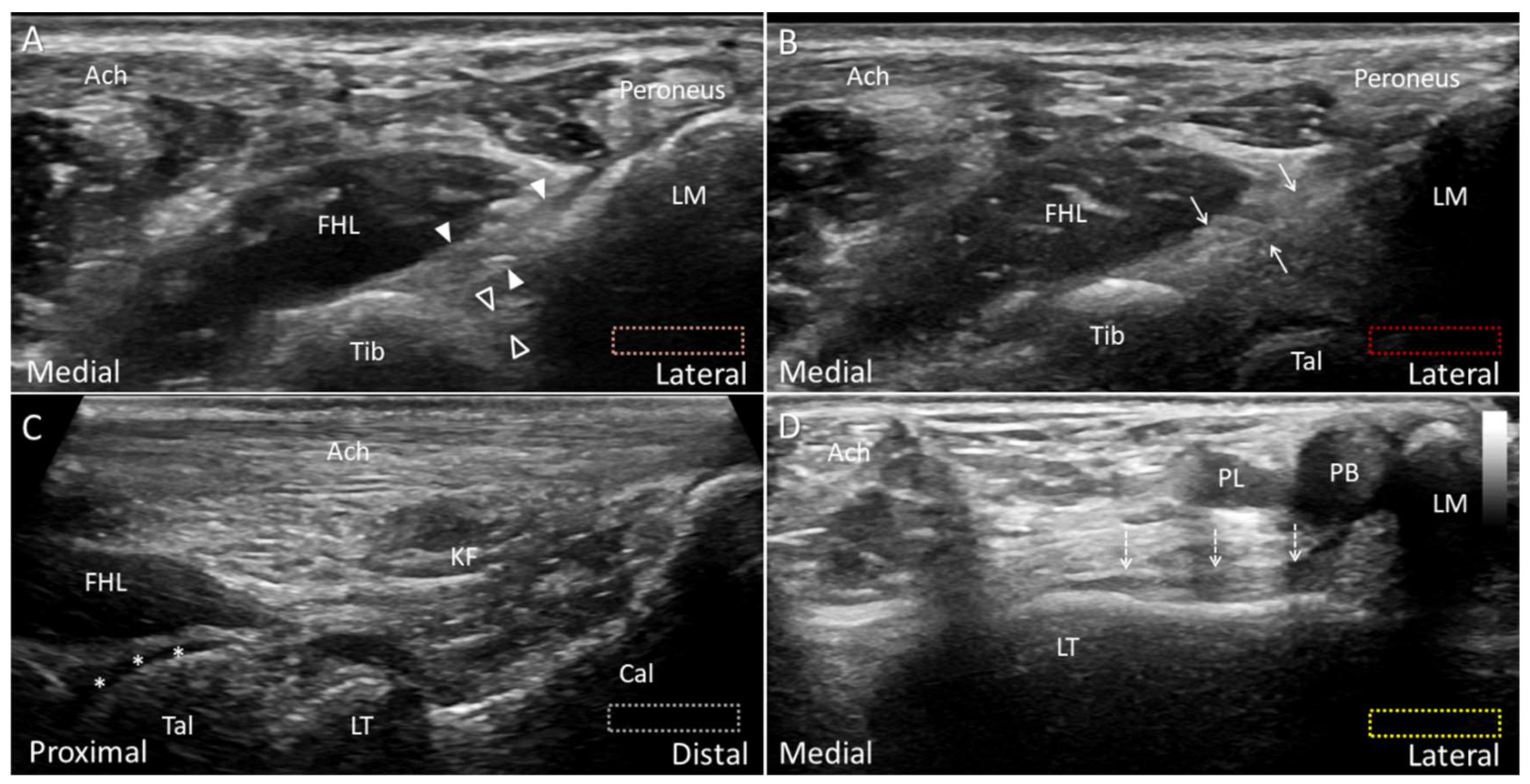
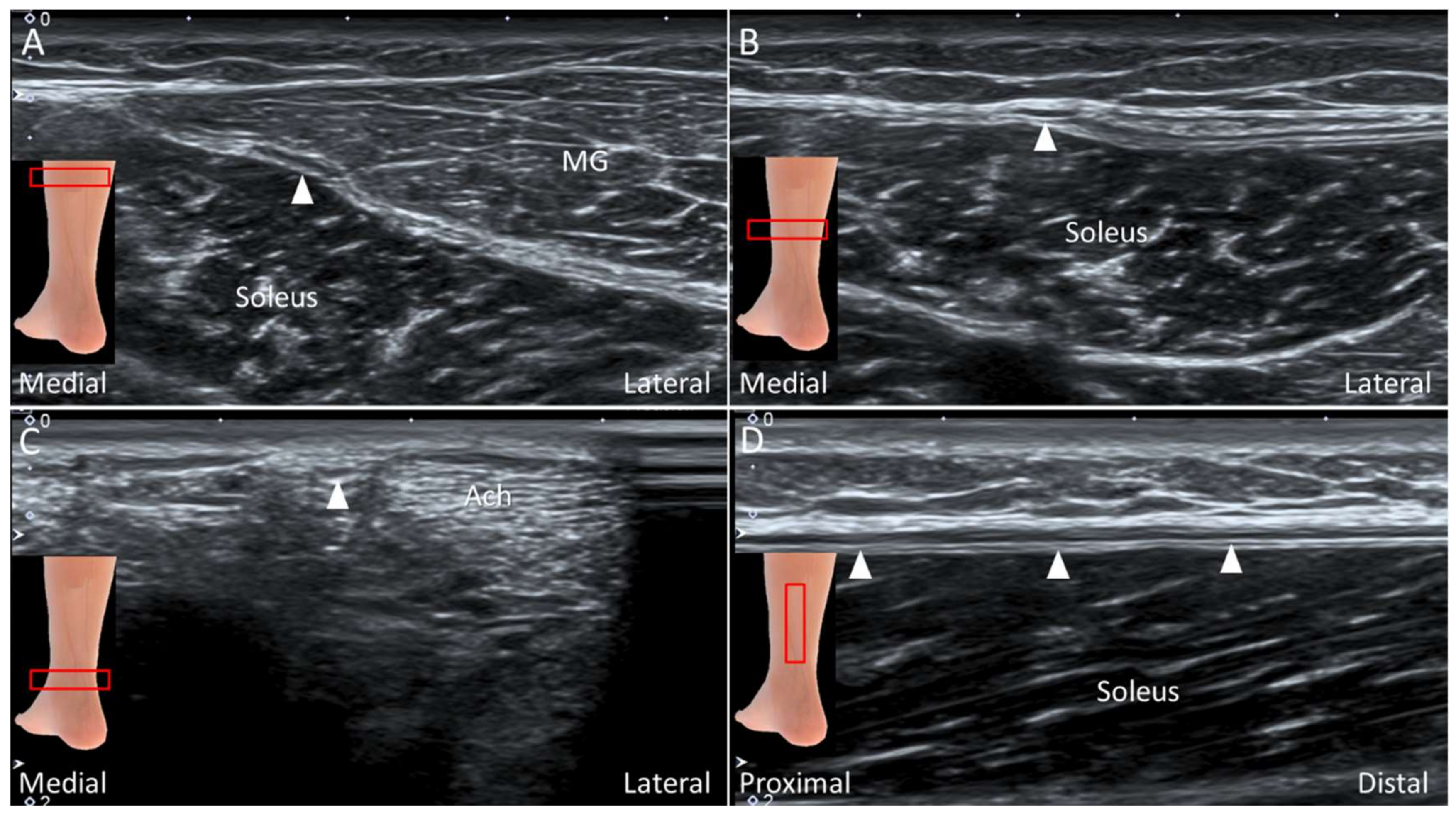
4.4. Plantaris Tendon
4.4.1. Anatomy
4.4.2. Scanning Technique
4.4.3. Clinical Relevance
5. Nerves
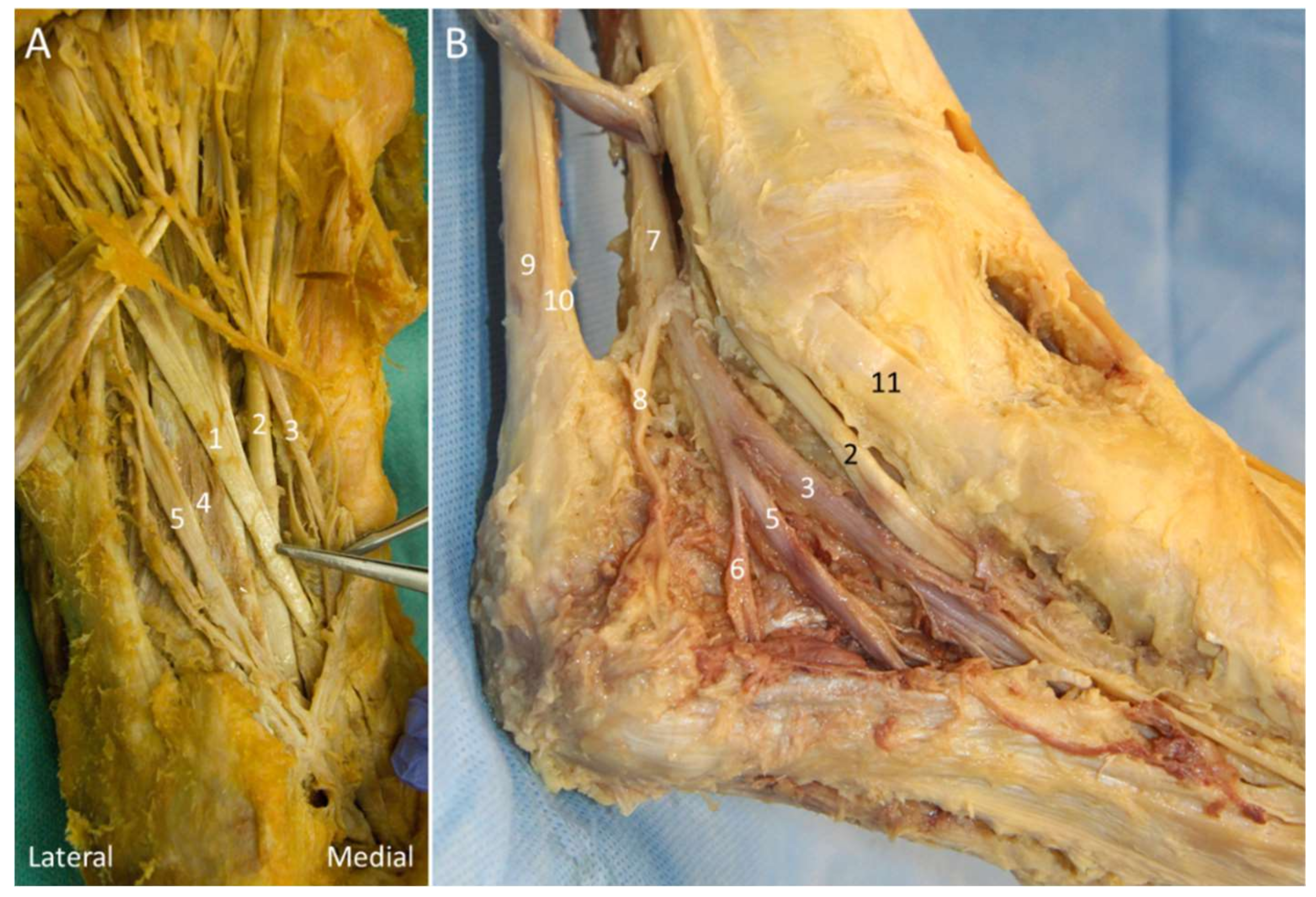
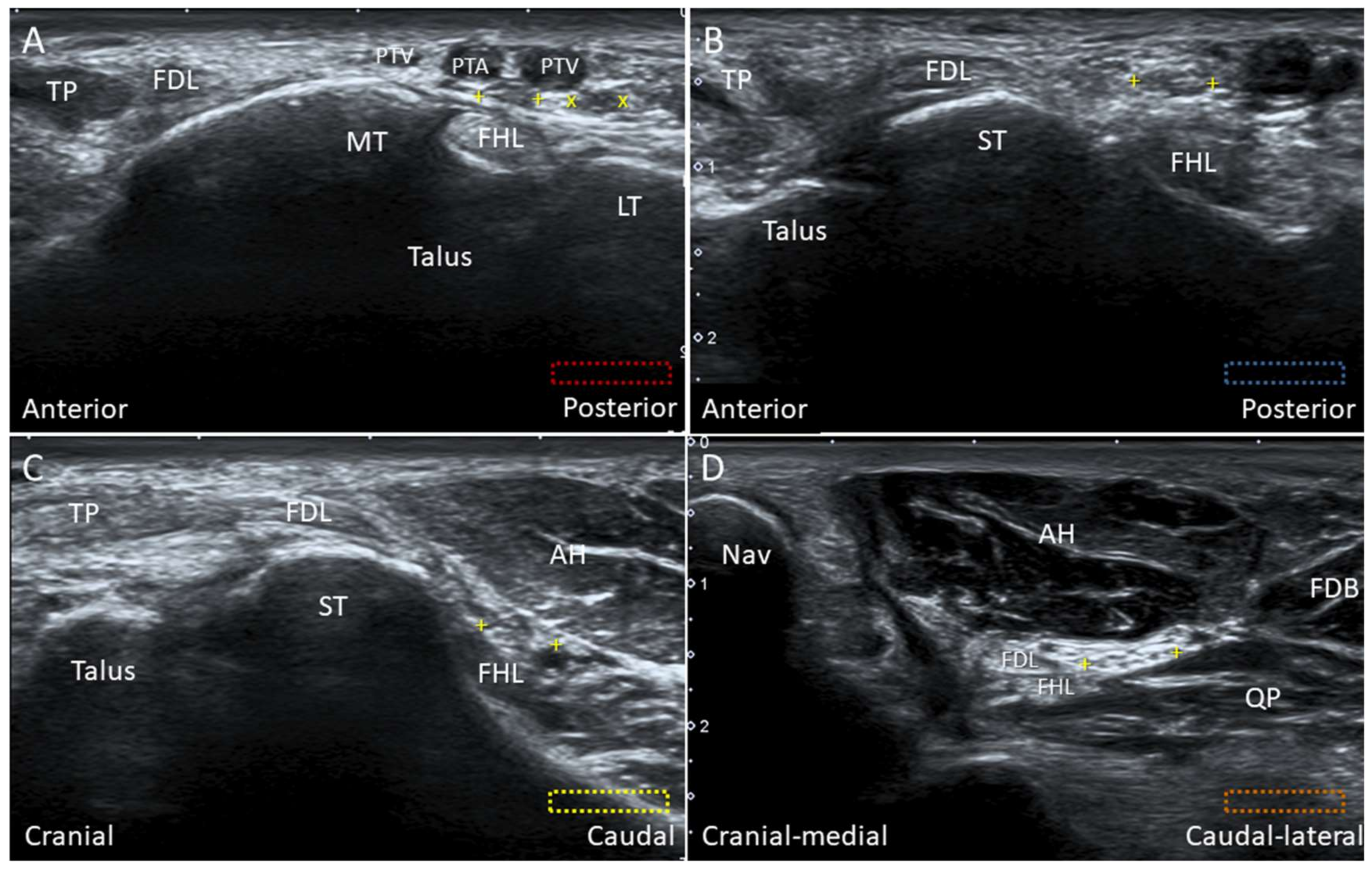
5.1. Medial Plantar Nerve (Over the Knot of Henry)
5.1.1. Anatomy
5.1.2. Scanning Technique
5.1.3. Clinical Relevance
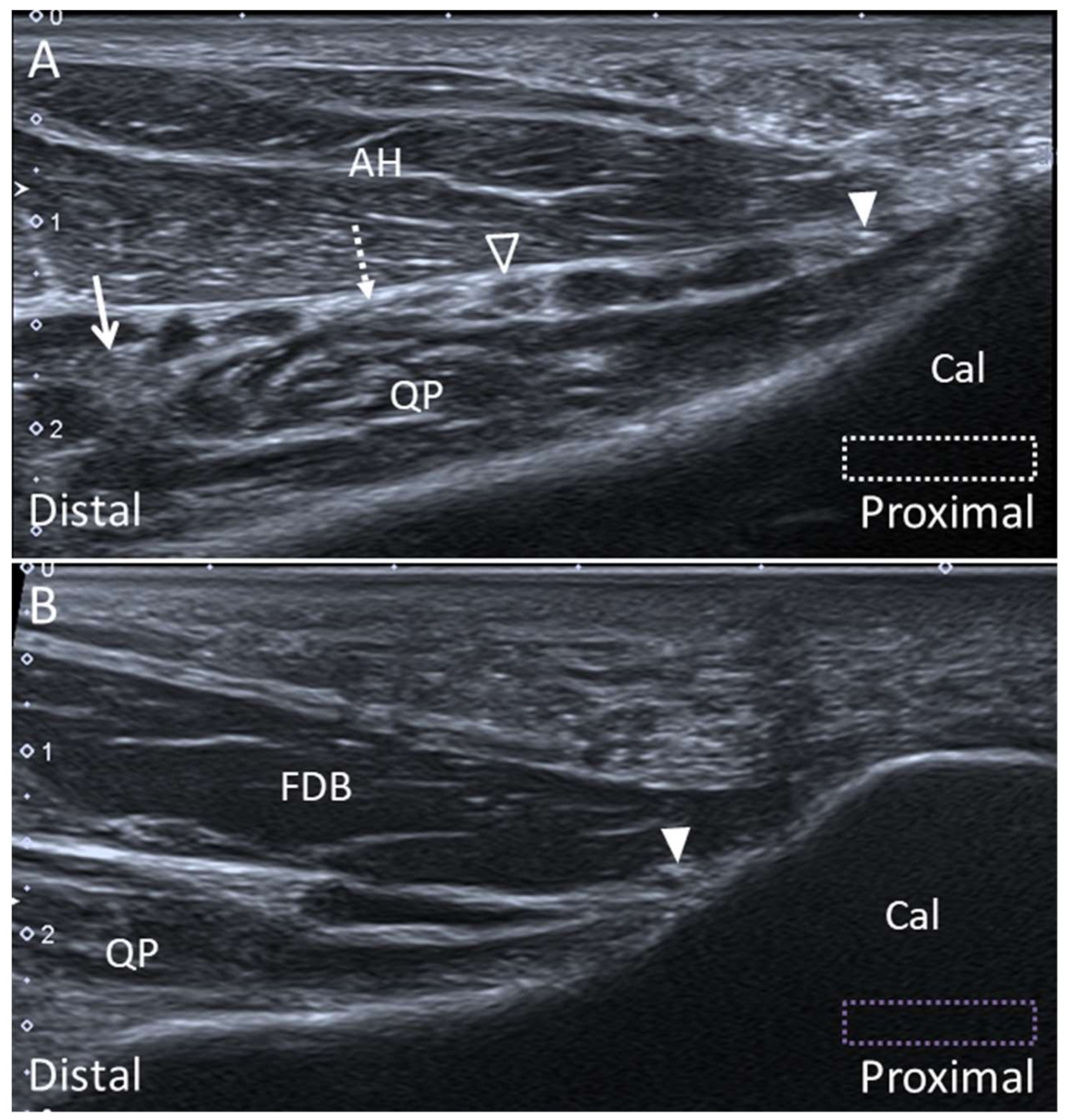
5.2. Baxter Nerve
5.2.1. Anatomy
5.2.2. Scanning Technique
5.2.3. Clinical Relevance
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Thomas, M.J.; Roddy, E.; Zhang, W.; Menz, H.B.; Hannan, M.T.; Peat, G.M. The population prevalence of foot and ankle pain in middle and old age: A systematic review. Pain 2011, 152, 2870–2880. [Google Scholar] [CrossRef]
- Wang, J.C.; Chang, K.V.; Wu, W.T.; Han, D.S.; Ozcakar, L. Ultrasound-guided standard vs dual-target subacromial corticosteroid injections for shoulder impingement syndrome: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2019, 100, 2119–2128. [Google Scholar] [CrossRef]
- Wu, W.T.; Chang, K.V.; Mezian, K.; Nanka, O.; Lin, C.P.; Ozcakar, L. Basis of shoulder nerve entrapment syndrome: An ultrasonographic study exploring factors influencing cross-sectional area of the suprascapular nerve. Front. Neurol. 2018, 9, 902. [Google Scholar] [CrossRef] [Green Version]
- Park, J.W.; Lee, S.J.; Choo, H.J.; Kim, S.K.; Gwak, H.C.; Lee, S.M. Ultrasonography of the ankle joint. Ultrasonography 2017, 36, 321–335. [Google Scholar] [CrossRef] [Green Version]
- Ozcakar, L.; Kara, M.; Chang, K.V.; Bayram Carli, A.; Hung, C.Y.; Tok, F.; Wu, C.H.; Akkaya, N.; Hsiao, M.Y.; Tekin, L.; et al. Euro-musculus/usprm. Basic Scanning protocols for ankle and foot. Eur. J. Phys. Rehabil. Med. 2015, 51, 647–653. [Google Scholar]
- Edama, M.; Kageyama, I.; Kikumoto, T.; Takabayashi, T.; Inai, T.; Hirabayashi, R.; Ito, W.; Nakamura, E.; Ikezu, M.; Kaneko, F.; et al. Morphological characteristics of the lateral talocalcaneal ligament: A large-scale anatomical study. Surg. Radiol. Anat. 2019, 41, 25–28. [Google Scholar] [CrossRef]
- Edama, M.; Takabayashi, T.; Inai, T.; Hirabayashi, R.; Ikezu, M.; Kaneko, F.; Kanta, M.; Kageyama, I. Morphological features of the posterior intermalleolar ligament. Surg. Radiol. Anat. 2019, 41, 1441–1443. [Google Scholar] [CrossRef] [PubMed]
- Vega, J.; Malagelada, F.; Manzanares Cespedes, M.C.; Dalmau-Pastor, M. The lateral fibulotalocalcaneal ligament complex: An ankle stabilizing isometric structure. Knee Surg. Sports Traumatol. Arthrosc. 2018. [Google Scholar] [CrossRef] [PubMed]
- Doring, S.; Provyn, S.; Marcelis, S.; Shahabpour, M.; Boulet, C.; de Mey, J.; de Smet, A.; De Maeseneer, M. Ankle and midfoot ligaments: Ultrasound with anatomical correlation: A review. Eur. J. Radiol. 2018, 107, 216–226. [Google Scholar] [CrossRef] [PubMed]
- Moroni, S.; Zwierzina, M.; Starke, V.; Moriggl, B.; Montesi, F.; Konschake, M. Clinical-anatomic mapping of the tarsal tunnel with regard to Baxter’s neuropathy in recalcitrant heel pain syndrome: Part I. Surg. Radiol. Anat. 2019, 41, 29–41. [Google Scholar] [CrossRef] [Green Version]
- Wu, W.T.; Chang, K.V.; Mezian, K.; Nanka, O.; Yang, Y.C.; Hsu, Y.C.; Hsu, P.C.; Ozcakar, L. Ulnar wrist pain revisited: ultrasound diagnosis and guided injection for triangular fibrocartilage complex injuries. J. Clin. Med. 2019, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, K.V.; Mezian, K.; Nanka, O.; Wu, W.T.; Lou, Y.M.; Wang, J.C.; Martinoli, C.; Ozcakar, L. Ultrasound Imaging for the cutaneous nerves of the extremities and relevant entrapment syndromes: from anatomy to clinical implications. J. Clin. Med. 2018, 7. [Google Scholar] [CrossRef] [Green Version]
- Umans, H.R.; Cerezal, L. Anterior ankle impingement syndromes. Semin. Musculoskelet. Radiol. 2008, 12, 146–153. [Google Scholar] [CrossRef] [Green Version]
- Subhas, N.; Vinson, E.N.; Cothran, R.L.; Santangelo, J.R.; Nunley, J.A., 2nd; Helms, C.A. MRI appearance of surgically proven abnormal accessory anterior-inferior tibiofibular ligament (Bassett’s ligament). Skelet. Radiol. 2008, 37, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Golano, P.; Vega, J.; de Leeuw, P.A.; Malagelada, F.; Manzanares, M.C.; Gotzens, V.; van Dijk, C.N. Anatomy of the ankle ligaments: A pictorial essay. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 557–569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hermans, J.J.; Beumer, A.; de Jong, T.A.; Kleinrensink, G.J. Anatomy of the distal tibiofibular syndesmosis in adults: A pictorial essay with a multimodality approach. J. Anat. 2010, 217, 633–645. [Google Scholar] [CrossRef]
- Ogilvie-Harris, D.J.; Reed, S.C.; Hedman, T.P. Disruption of the ankle syndesmosis: Biomechanical study of the ligamentous restraints. Arthroscopy 1994, 10, 558–560. [Google Scholar] [CrossRef]
- Golano, P.; Mariani, P.P.; Rodriguez-Niedenfuhr, M.; Mariani, P.F.; Ruano-Gil, D. Arthroscopic anatomy of the posterior ankle ligaments. Arthroscopy 2002, 18, 353–358. [Google Scholar] [CrossRef]
- Trouilloud, P.; Dia, A.; Grammont, P.; Gelle, M.C.; Autissier, J.M. Variations in the calcaneo-fibular ligament (lig. calcaneofibulare). Application to the kinematics of the ankle. Bull. l’Association Anat. 1988, 72, 31–35. [Google Scholar]
- Hertel, J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J. Athl. Train. 2002, 37, 364–375. [Google Scholar]
- Karlsson, J.; Eriksson, B.I.; Renstrom, P.A. Subtalar ankle instability. A review. Sports Med. 1997, 24, 337–346. [Google Scholar] [CrossRef]
- Kafka, R.M.; Aveytua, I.L.; Choi, P.J.; DiLandro, A.C.; Tubbs, R.S.; Loukas, M.; Mintz, D.N.; Baidya, R.; Kumar, S.; Sangari, S.K.; et al. Anatomico-radiological study of the bifurcate ligament of the foot with clinical significance. Cureus 2019, 11, 3847. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walter, W.R.; Hirschmann, A.; Tafur, M.; Rosenberg, Z.S. Imaging of chopart (midtarsal) joint complex: normal anatomy and posttraumatic findings. Am. J. Roentgenol. 2018, 211, 416–425. [Google Scholar] [CrossRef] [PubMed]
- Edama, M.; Ikezu, M.; Kaneko, F.; Kikumoto, T.; Takabayashi, T.; Hirabayashi, R.; Inai, T.; Kageyama, I. Morphological features of the bifurcated ligament. Surg. Radiol. Anat. 2019, 41, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Henari, S.; Banks, L.N.; Radovanovic, I.; Queally, J.; Morris, S. Ultrasonography as a diagnostic tool in assessing deltoid ligament injury in supination external rotation fractures of the ankle. Orthopedics 2011, 34, 639–643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mengiardi, B.; Pfirrmann, C.W.; Vienne, P.; Hodler, J.; Zanetti, M. Medial collateral ligament complex of the ankle: MR appearance in asymptomatic subjects. Radiology 2007, 242, 817–824. [Google Scholar] [CrossRef]
- Crim, J. Medial-sided ankle pain: deltoid ligament and beyond. Magn. Reson. Imaging Clin. N. Am. 2017, 25, 63–77. [Google Scholar] [CrossRef]
- Bastias, G.F.; Dalmau-Pastor, M.; Astudillo, C.; Pellegrini, M.J. Spring ligament instability. Foot Ankle Clin. 2018, 23, 659–678. [Google Scholar] [CrossRef]
- Davis, W.H.; Sobel, M.; DiCarlo, E.F.; Torzilli, P.A.; Deng, X.; Geppert, M.J.; Patel, M.B.; Deland, J. Gross, histological, and microvascular anatomy and biomechanical testing of the spring ligament complex. Foot Ankle Int. 1996, 17, 95–102. [Google Scholar] [CrossRef]
- Hardy, R.H. Observations on the structure and properties of the plantar calcaneo-navicular ligament in man. J. Anat. 1951, 85, 135–139. [Google Scholar]
- Mansour, R.; Teh, J.; Sharp, R.J.; Ostlere, S. Ultrasound assessment of the spring ligament complex. Eur. Radiol. 2008, 18, 2670–2675. [Google Scholar] [CrossRef] [PubMed]
- Woodward, S.; Jacobson, J.A.; Femino, J.E.; Morag, Y.; Fessell, D.P.; Dong, Q. Sonographic evaluation of Lisfranc ligament injuries. J. Ultrasound Med. 2009, 28, 351–357. [Google Scholar] [CrossRef] [Green Version]
- Ablimit, A.; Ding, H.Y.; Liu, L.G. Magnetic resonance imaging of the Lisfranc ligament. J. Orthop. Surg. Res. 2018, 13, 282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Granata, J.D.; Philbin, T.M. The midfoot sprain: A review of Lisfranc ligament injuries. Physician Sportsmed. 2010, 38, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, D.F.; Nazarian, L.N.; Smith, J. Enthesopathy of the lateral cord of the plantar fascia. J. Ultrasound Med. 2014, 33, 1711–1716. [Google Scholar] [CrossRef] [PubMed]
- Newman, E.; Umans, H.; Elsinger, E.; Tobin, K.S. Not one of the usual suspects: MRI features of insertional lateral cord plantar fasciopathy. Am. J. Roentgenol. 2018, 211, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.V.; Wu, W.T.; Ozcakar, L. Ultrasonographic imaging for the diagnosis and guided injection of the lateral cord of the plantar fascia in a Jogger. Am. J. Phys. Med. Rehabil. 2019, 98, 36–37. [Google Scholar] [CrossRef] [PubMed]
- Demondion, X.; Canella, C.; Moraux, A.; Cohen, M.; Bry, R.; Cotten, A. Retinacular disorders of the ankle and foot. Semin. Musculoskelet. Radiol. 2010, 14, 281–291. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, S.; Becciolini, M. Ultrasound features of ankle retinacula: Normal appearance and pathologic findings. J. Ultrasound Med. 2019. [Google Scholar] [CrossRef]
- Bianchi, S.; Martinoli, C. Ultrasound of the Musculoskeletal System; Springer: Berlin, Germany; New York, NY, USA, 2007; p. 974. [Google Scholar]
- Rosenberg, Z.S.; Bencardino, J.; Astion, D.; Schweitzer, M.E.; Rokito, A.; Sheskier, S. MRI features of chronic injuries of the superior peroneal retinaculum. Am. J. Roentgenol. 2003, 181, 1551–1557. [Google Scholar] [CrossRef]
- Stone, T.J.; Rosenberg, Z.S.; Velez, Z.R.; Ciavarra, G.; Prost, R.; Bencardino, J.T. Subluxation of the peroneus long tendon in the cuboid tunnel: Is it normal or pathologic? An ultrasound and magnetic resonance imaging study. Skelet. Radiol. 2016, 45, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Shyamsundar, S.; Wazir, A.; Allen, P.E. Variations in the insertion of peroneus longus tendon—A cadaver study. Foot Ankle Surg. 2012, 18, 293–295. [Google Scholar] [CrossRef] [PubMed]
- Henrie, A.M.; Oberg, P.; Willick, S. Partial peroneus longus tendon rupture at its distal insertion in a runner: A case presentation. PM R J. Inj. Funct. Rehabil. 2013, 5, 155–158. [Google Scholar] [CrossRef]
- Yammine, K.; Eric, M. The fibularis (peroneus) tertius muscle in humans: a meta-analysis of anatomical studies with clinical and evolutionary implications. BioMed Res. Int. 2017, 2017, 6021707. [Google Scholar] [CrossRef] [PubMed]
- McGoldrick, N.P.; Bergin, D.; Kearns, S.R. Peroneus tertius tendon tear causing lateral ankle pain in a child. J. Foot Ankle Surg. 2017, 56, 854–856. [Google Scholar] [CrossRef] [PubMed]
- Witvrouw, E.; Borre, K.V.; Willems, T.M.; Huysmans, J.; Broos, E.; De Clercq, D. The significance of peroneus tertius muscle in ankle injuries: A prospective study. Am. J. Sports Med. 2006, 34, 1159–1163. [Google Scholar] [CrossRef]
- Sammarco, G.J.; Henning, C. Peroneus tertius muscle as a cause of snapping and ankle pain: A case report. Am. J. Sports Med. 2007, 35, 1377–1379. [Google Scholar] [CrossRef]
- Donovan, A.; Rosenberg, Z.S.; Bencardino, J.T.; Velez, Z.R.; Blonder, D.B.; Ciavarra, G.A.; Adler, R.S. Plantar tendons of the foot: MR imaging and US. Radiographics 2013, 33, 2065–2085. [Google Scholar] [CrossRef] [Green Version]
- De Maeseneer, M.; Madani, H.; Lenchik, L.; De Mey, J.; Provyn, S.; Shahabpour, M. Ultrasound of the distal insertions of the ankle and foot tendons with anatomical correlation: A review. Can. Assoc. Radiol. J. 2018, 69, 282–292. [Google Scholar] [CrossRef]
- Simpson, S.L.; Hertzog, M.S.; Barja, R.H. The plantaris tendon graft: An ultrasound study. J. Hand Surg. 1991, 16, 708–711. [Google Scholar] [CrossRef]
- Hung, C.Y.; Chang, K.V. An uncommon cause of posterior leg pain- ultrasound image of plantaris tendinopathy. J. Clin. Diagn. Res. 2016, 10, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.V.; Wu, W.T.; Ozcakar, L. Ultrasonography imaging for the diagnosis and guided injection of plantaris tendon strain in a patient with tennis leg. Am. J. Phys. Med. Rehabil. 2018, 97, 60–61. [Google Scholar] [CrossRef] [PubMed]
- De Maeseneer, M.; Madani, H.; Lenchik, L.; Kalume Brigido, M.; Shahabpour, M.; Marcelis, S.; de Mey, J.; Scafoglieri, A. Normal anatomy and compression areas of nerves of the foot and ankle: Us and mr imaging with anatomic correlation. Radiographics 2015, 35, 1469–1482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Presley, J.C.; Maida, E.; Pawlina, W.; Murthy, N.; Ryssman, D.B.; Smith, J. Sonographic visualization of the first branch of the lateral plantar nerve (baxter nerve): Technique and validation using perineural injections in a cadaveric model. J. Ultrasound Med. 2013, 32, 1643–1652. [Google Scholar] [CrossRef] [PubMed]
- Alshami, A.M.; Souvlis, T.; Coppieters, M.W. A review of plantar heel pain of neural origin: Differential diagnosis and management. Man. Ther. 2008, 13, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Ling, Z.X.; Kumar, V.P. The myofascial compartments of the foot: A cadaver study. J. Bone Jt. Surg. Br. Vol. 2008, 90, 1114–1118. [Google Scholar] [CrossRef] [Green Version]
- Singh, G.; Kumar, V.P. Neuroanatomical basis for the tarsal tunnel syndrome. Foot Ankle Int. 2012, 33, 513–518. [Google Scholar] [CrossRef]







© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hung, C.-Y.; Chang, K.-V.; Mezian, K.; Naňka, O.; Wu, W.-T.; Hsu, P.-C.; Özçakar, L. Advanced Ankle and Foot Sonoanatomy: Imaging Beyond the Basics. Diagnostics 2020, 10, 160. https://doi.org/10.3390/diagnostics10030160
Hung C-Y, Chang K-V, Mezian K, Naňka O, Wu W-T, Hsu P-C, Özçakar L. Advanced Ankle and Foot Sonoanatomy: Imaging Beyond the Basics. Diagnostics. 2020; 10(3):160. https://doi.org/10.3390/diagnostics10030160
Chicago/Turabian StyleHung, Chen-Yu, Ke-Vin Chang, Kamal Mezian, Ondřej Naňka, Wei-Ting Wu, Po-Cheng Hsu, and Levent Özçakar. 2020. "Advanced Ankle and Foot Sonoanatomy: Imaging Beyond the Basics" Diagnostics 10, no. 3: 160. https://doi.org/10.3390/diagnostics10030160
APA StyleHung, C.-Y., Chang, K.-V., Mezian, K., Naňka, O., Wu, W.-T., Hsu, P.-C., & Özçakar, L. (2020). Advanced Ankle and Foot Sonoanatomy: Imaging Beyond the Basics. Diagnostics, 10(3), 160. https://doi.org/10.3390/diagnostics10030160






