Endometrial Cancer Risk Prediction According to Indication of Diagnostic Hysteroscopy in Post-Menopausal Women
Abstract
1. Introduction
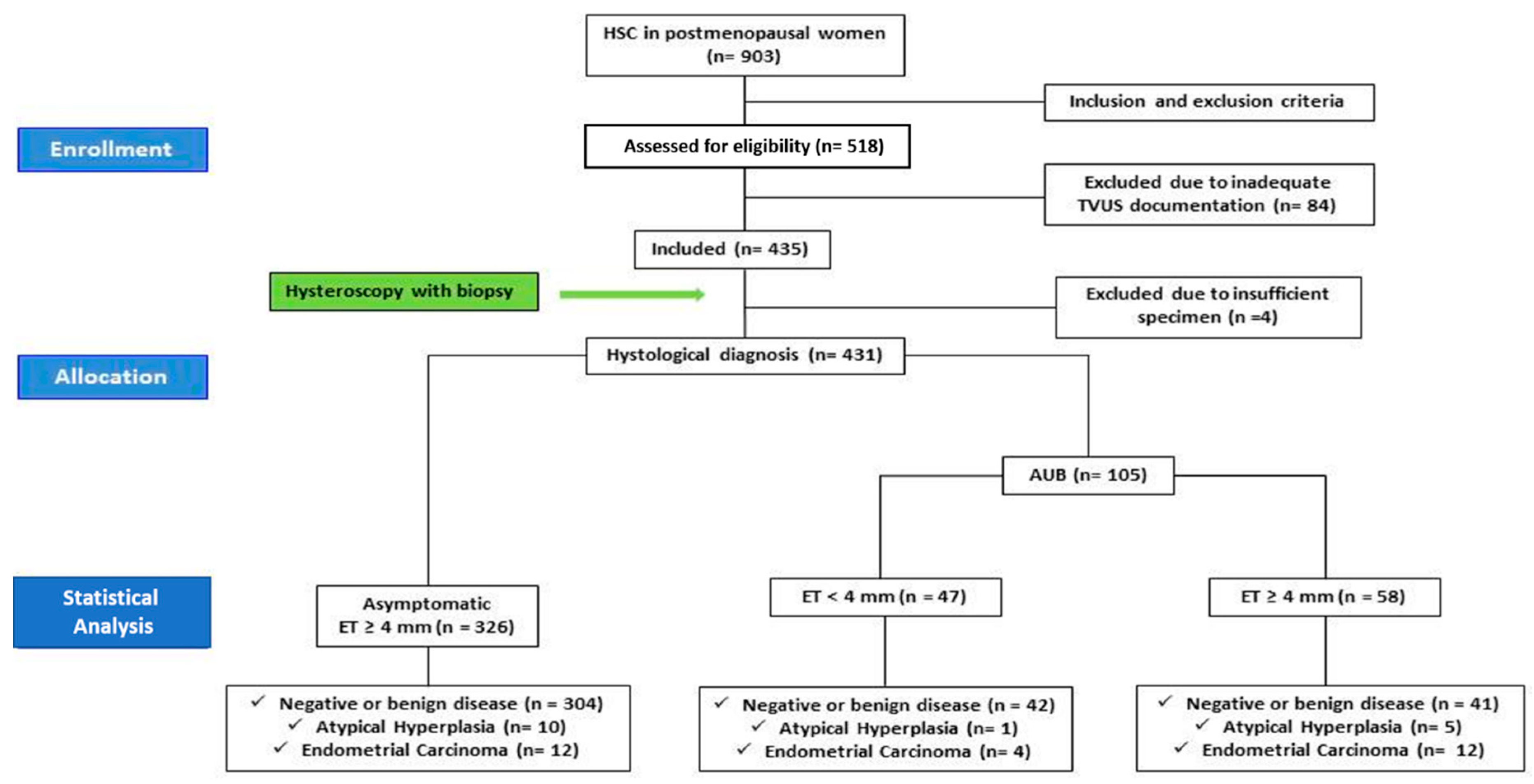
2. Materials and Methods
2.1. Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection and Definition of Groups
2.4. Diagnostic Hysteroscopy and Endometrial Sampling
2.5. Outcomes of the Study
2.6. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
3.2. Risk of Endometrial Cancer and Atypical Hyperplasia
3.3. Diagnostic Test Accuracy
3.4. Impact of Other Factors on the Risk of EC
4. Discussion
4.1. General Considerations
4.2. Main Findings
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Secord, A.A.; Hasselblad, V.; Von Gruenigen, V.E.; Gehrig, P.A.; Modesitt, S.C.; Bae-Jump, V.; Havrilesky, L.J. Body mass index and mortality in endometrial cancer: A systematic review and meta-analysis. Gynecol. Oncol. 2016, 140, 184–190. [Google Scholar] [CrossRef] [PubMed]
- American Cancer Society. Cancer Facts & Figures 2015; American Cancer Society: Atlanta, GA, USA, 2015. [Google Scholar]
- Yaşa, C.; Dural, O.; Baştu, E.; Uğurlucan, F.G.; Nehir, A.; Iyibozkurt, A.C. Evaluation of the diagnostic role of transvaginal ultrasound measurements of endometrial thickness to detect endometrial malignancy in asymptomatic postmenopausal women. Arch. Gynecol. Obstet. 2016, 294, 311–316. [Google Scholar] [CrossRef] [PubMed]
- The Use of Hysteroscopy for the Diagnosis and Treatment of Intrauterine Pathology: ACOG Committee Opinion, Number 800. Obstet. Gynecol. 2020, 135, e138–e148. [CrossRef]
- Vitale, S.G. The Biopsy Snake Grasper Sec. VITALE: A New Tool for Office Hysteroscopy. J. Minim. Invasive Gynecol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Litta, P.; Merlin, F.; Saccardi, C.; Pozzan, C.; Sacco, G.; Fracas, M.; Capobianco, G.; Dessole, S. Role of hysteroscopy with endometrial biopsy to rule out endometrial cancer in postmenopausal women with abnormal uterine bleeding. Maturitas 2005, 50, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Dibi, R.P.; Zettler, C.G.; Pessini, S.A.; Ayub, A.V.; De Almeida, S.B.; Da Silveira, G.P. Tamoxifen use and endometrial lesions. Menopause 2009, 16, 293–300. [Google Scholar] [CrossRef]
- ACOG Committee Opinion, No. 734: The Role of Transvaginal Ultrasonography in Evaluating the Endometrium of Women with Postmenopausal Bleeding. Obstet. Gynecol. 2018, 131, e124–e129. [CrossRef]
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 440: The Role of Transvaginal Ultrasonography in the Evaluation of Postmenopausal Bleeding. Obstet. Gynecol. 2009, 114 Pt 1, 409–411. [Google Scholar] [CrossRef]
- Goldstein, R.B.; Bree, R.L.; Benson, C.B.; Benacerraf, B.R.; Bloss, J.D.; Carlos, R.; Fleischer, A.C.; Goldstein, S.R.; Hunt, R.B.; Kurman, R.J.; et al. Evaluation of the woman with postmenopausal bleeding: Society of Radiologists in Ultrasound-Sponsored Consensus Conference statement. J. Ultrasound Med. 2001, 20, 1025–1036. [Google Scholar] [CrossRef]
- Wolfman, W. No. 249-Asymptomatic Endometrial Thickening. J. Obstet. Gynaecol. Can. 2018, 40, 367–e377. [Google Scholar] [CrossRef]
- Osmers, R.; Völksen, M.; Rath, W.; Kuhn, W. Vaginal sonography: A screening method for early detection of ovarian tumors and endometrial cancers? Arch. Gynecol. Obstet. 1989, 245, 602–606. [Google Scholar] [CrossRef] [PubMed]
- Doubilet, P.M. Diagnosis of abnormal uterine bleeding with imaging. Menopause 2011, 18, 421–424. [Google Scholar] [CrossRef] [PubMed]
- Alcázar, J.L.; Bonilla, L.; Marucco, J.; Padilla, A.I.; Chacón, E.; Manzour, N.; Salas, A. Risk of endometrial cancer and endometrial hyperplasia with atypia in asymptomatic postmenopausal women with endometrial thickness ≥11 mm: A systematic review and meta-analysis. J. Clin. Ultrasound 2018, 46, 565–570. [Google Scholar]
- Saccardi, C.; Gizzo, S.; Patrelli, T.S.; Ancona, E.; Anis, O.; Di Gangi, S.; Vacilotto, A.; D’Antona, D.; Nardelli, G.B. Endometrial surveillance in tamoxifen users: Role, timing and accuracy of hysteroscopic investigation: Observational longitudinal cohort study. Endocr. Relat. Cancer 2013, 20, 455–462. [Google Scholar] [CrossRef][Green Version]
- Società Italiana di Diabetologia e Associazione Medici Diabetologi. Standard Italiani per la Cura del Diabete Mellito; Società Italiana di Diabetologia e Associazione Medici Diabetologi: Rome, Italy, 2018; Available online: https://aemmedi.it/wp-content/uploads/2009/06/AMD-Standard-unico1.pdf.
- Bryan, W.; Giuseppe, M.; Wilko, S.; Enrico, A.R.; Michel, A.; Michel, B.; Denis, L.C.; Antonio, C.; Giovanni de, S.; Anna, D.; et al. ESC Scientific Document Group, 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar]
- Dueholm, M.; Hjorth, I.M.D.; Secher, P.; Jørgensen, A.; Ørtoft, G. Structured Hysteroscopic Evaluation of Endometrium in Women With Postmenopausal Bleeding. J. Minim. Invasive Gynecol. 2015, 22, 1215–1224. [Google Scholar] [CrossRef]
- Giannella, L.; Mfuta, K.; Setti, T.; Boselli, F.; Bergamini, E.; Cerami, L. Diagnostic accuracy of endometrial thickness for the detection of intra-uterine pathologies and appropriateness of performed hysteroscopies among asymptomatic postmenopausal women. Eur. J. Obstet. Gynecol. Reprod. Boil. 2014, 177, 29–33. [Google Scholar] [CrossRef]
- Kim, A.; Lee, J.Y.; Chun, S.; Kim, H.Y. Diagnostic utility of three-dimensional power Doppler ultrasound for postmenopausal bleeding. Taiwan J. Obstet. Gynecol. 2015, 54, 221–226. [Google Scholar] [CrossRef]
- Mohr, S.B.; Garland, C.F.; Gorham, E.D.; Grant, W.B.; Garland, F.C. Is ultraviolet B irradiance inversely associated with incidence rates of endometrial cancer: An ecological study of 107 countries. Prev. Med. 2007, 45, 327–331. [Google Scholar] [CrossRef]
- Long, B.; Clarke, M.A.; Morillo, A.D.M.; Wentzensen, N.; Bakkum-Gamez, J.N. Ultrasound detection of endometrial cancer in women with postmenopausal bleeding: Systematic review and meta-analysis. Gynecol. Oncol. 2020. pii: S0090-8258(20)30085-8. [Google Scholar] [CrossRef]
- Li, Y.-T.; Lee, W.-L.; Tsui, K.-H. Endometrial thickness still presents a best reference to predict endometrial cancer. Taiwan J. Obstet. Gynecol. 2016, 55, 148–149. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Breijer, M.C.; Mol, B.W.J. Transvaginal ultrasound measurement of the endometrium remains the first line test for investigating postmenopausal bleeding but integration of patient characteristics into testing may further improve diagnostic algorithms. BJOG 2015, 123, 447. [Google Scholar] [CrossRef]
- Tabor, A.; Watt, H.C.; Wald, N.J. Endometrial thickness as a test for endometrial cancer in women with postmenopausal vaginal bleeding. Obstet. Gynecol. 2002, 99, 663–670. [Google Scholar] [PubMed]
- Colombo, N.; Preti, E.; Landoni, F.; Carinelli, S.; Colombo, A.; Marini, C.; Sessa, C.; ESMO Guidelines Working Group. Endometrial cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2013, 24 (Suppl. S6), vi33–vi38. [Google Scholar] [CrossRef] [PubMed]
- Leone, F.P.G.; Timmerman, D.; Bourne, T.; Valentin, L.; Epstein, E.; Goldstein, S.R.; Marret, H.; Parsons, A.K.; Gull, B.; Istre, O.; et al. Terms, definitions and measurements to describe the sonographic features of the endometrium and intrauterine lesions: A consensus opinion from the International Endometrial Tumor Analysis (IETA) group. Ultrasound Obstet. Gynecol. 2010, 35, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Tinelli, R.; Tinelli, F.G.; Cicinelli, E.; Malvasi, A.; Tinelli, A. The role of hysteroscopy with eye-directed biopsy in postmenopausal women with uterine bleeding and endometrial atrophy. Menopause 2008, 15 Pt 1, 737–742. [Google Scholar] [CrossRef]
- Dueholm, M.; Marinovskij, E.; Hansen, E.S.; Møller, C.; Ørtoft, G. Diagnostic methods for fast-track identification of endometrial cancer in women with postmenopausal bleeding and endometrial thickness greater than 5 mm. Menopause 2015, 22, 616–626. [Google Scholar] [CrossRef]
- Saccardi, C.; Gizzo, S.; Vitagliano, A.; Noventa, M.; Micaglio, M.; Parotto, M.; Fiorese, M.; Litta, P. Peri-incisional and intraperitoneal ropivacaine administration: A new effective tool in pain control after laparoscopic surgery in gynecology: A randomized controlled clinical trial. Surg. Endosc. 2016, 30, 5310–5318. [Google Scholar] [CrossRef]
- Noventa, M.; Ancona, E.; Quaranta, M.; Vitagliano, A.; Cosmi, E.; D’Antona, D.; Gizzo, S. Intrauterine Morcellator Devices: The Icon of Hysteroscopic Future or Merely a Marketing Image? A Systematic Review Regarding Safety, Efficacy, Advantages, and Contraindications. Reprod. Sci. 2015, 22, 1289–1296. [Google Scholar] [CrossRef]
- Smith-Bindman, R.; Weiss, E.; Feldstein, V. How thick is too thick? When endometrial thickness should prompt biopsy in postmenopausal women without vaginal bleeding. Ultrasound Obstet. Gynecol. 2004, 24, 558–565. [Google Scholar] [CrossRef]
- Linkov, F.; Edwards, R.; Balk, J.; Yurkovetsky, Z.; Stadterman, B.; Lokshin, A.; Taioli, E. Endometrial hyperplasia, endometrial cancer and prevention: Gaps in existing research of modifiable risk factors. Eur. J. Cancer 2008, 44, 1632–1644. [Google Scholar] [CrossRef]
- Eitan, R.; Saenz, C.C.; Venkatraman, E.S.; Hann, L.; Bach, A.; Gretz, E.; Barakat, R.R.; Chi, D.S. Pilot study prospectively evaluating the use of the measurement of preoperative sonographic endometrial thickness in postmenopausal patients with endometrial cancer. Menopause 2005, 12, 27–30. [Google Scholar] [CrossRef]
- Maatela, J.; Aromaa, A.; Salmi, T.; Pohja, M.; Vuento, M.; Grönroos, M. The risk of endometrial cancer in diabetic and hypertensive patients: A nationwide record-linkage study in Finland. Ann. Chir. Gynaecol. Suppl. 1994, 208, 20–24. [Google Scholar] [PubMed]
- Anderson, G.L.; Judd, H.L.; Kaunitz, A.M.; Barad, D.H.; Beresford, S.A.; Pettinger, M.; Liu, J.; McNeeley, S.G.; Lopez, A.M.; Women’s Health Initiative Investigators. Effects of estrogen plus progestin on gynecologic cancers and associated diagnostic procedures: The Women’ss Health Initiative randomized trial. JAMA 2003, 290, 1739–1748. [Google Scholar] [CrossRef] [PubMed]
- Martínez_Rubio, M.; Alcazar, J. Ultrasonographic and pathological endometrial findings in asymptomatic postmenopausal women taking antihypertensive drugs. Maturitas 2003, 46, 27–32. [Google Scholar] [CrossRef]
- Sit, A.S.Y.; Modugno, F.; Hill, L.M.; Martin, J.; Weissfeld, J.L. Transvaginal ultrasound measurement of endometrial thickness as a biomarker for estrogen exposure. Cancer Epidemiol. Biomark. Prev. 2004, 13, 1459–1465. [Google Scholar]
- Aarestrup, J.; Gamborg, M.; Tilling, K.; Ulrich, L.G.; Sørensen, T.I.; Baker, J.L. Childhood body mass index growth trajectories and endometrial cancer risk. Int. J. Cancer 2017, 140, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Andolf, E.; Dahlander, K.; Aspenberg, P. Ultrasound thickness of the endometrium correlated to body weight in asymptomatic postmenopausal women. Obstet. Gynecol. 1993, 82, 936–940. [Google Scholar]
- Arem, H.; Pfeiffer, R.M.; Moore, S.C.; Brinton, L.A.; Matthews, C.E. Body mass index, physical activity, and television time in relation to mortality risk among endometrial cancer survivors in the NIH-AARP Diet and Health Study cohort. Cancer Causes Control 2016, 27, 1403–1409. [Google Scholar] [CrossRef]
- Litta, P.; Fabris, A.M.; Breda, E.; Bartolucci, C.; Conte, L.; Saccardi, C.; Nappi, L. Laparoscopic surgical staging of endometrial cancer: Does obesity influence feasibility and perioperative outcome? Eur. J. Gynaecol. Oncol. 2013, 34, 231–233. [Google Scholar]
- Gizzo, S.; Fabris, A.; Litta, P.; Saccardi, C. Estimated intermediate risk endometrial cancer: Debate and new perspectives on therapy individualization and prognosis establishment starting from a peculiar case. Int. J. Clin. Exp. Pathol. 2014, 7, 2664–2669. [Google Scholar] [PubMed]
| Variable | Pattern Characteristics |
|---|---|
| Generality | Atrofic Thickened Uneven |
| Surface | Regular Polypoid (Local v.s. Diffuse) Papillary projections (Local v.s. Diffuse) Irregular surface (Local v.s. Diffuse) |
| Necrosis | No evidence Surface necrosis Candy floss pattern Hyperintense white spots |
| Vessel pattern | Regular Irregular branching Irregular distribution |
| Gland pattern | Regular Dilated glands and glands with irregular openings |
| Suspected for | Regular Low-risk hyperplasia High-risk hyperplasia Adenocarcinoma |
| Variable | Frequency |
|---|---|
| Age (y) | 63.8 (±9.3) |
| BMI (kg/m2) | 26.07 (±5.31) |
| Overweight (n) | 114 (26.5%) |
| Obesity (n) | 97 (22.5%) |
| Hypertension (n) | 138 (32%) |
| Diabetes Mellitus (n) | 63 (15%) |
| Hormone Replacement Therapy (n) | 77 (17.9%) |
| Groups | EC | Negative | p Value |
| ET_Group (n = 326) (ET ≥ 4 mm asymptomatic) | 12 (3.7%) | 314 (96.3%) | <0.001 |
| AUB Group (n = 105) | 16 (15.2%) | 89 (84.8%) | |
| AUB Subgroup 1 (n = 47) (ET < 4 mm) | 4 (8.5%) | 43 (91.5%) | <0.001 |
| AUB Subgroup 2 (n = 58) (ET ≥ 4 mm) | 12 (20.7%) | 46 (79.3%) | |
| EC and Atypical Hyperplasia | Negative | p Value | |
| ET_Group (n = 326) (ET ≥ 4 mm asymptomatic) | 22 (6.7%) | 304 (93.3%) | <0.001 |
| AUB Group (n = 105) | 22 (21.0%) | 83 (79.0%) | |
| AUB Subgroup 1 (n = 47) (ET < 4 mm) | 5 (10.6%) | 42 (89.4%) | <0.001 |
| AUB Subgroup 2 (n = 58) (ET ≥ 4 mm) | 17 (29.3%) | 41 (70.7%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saccardi, C.; Vitagliano, A.; Marchetti, M.; Lo Turco, A.; Tosatto, S.; Palumbo, M.; De Lorenzo, L.S.; Vitale, S.G.; Scioscia, M.; Noventa, M. Endometrial Cancer Risk Prediction According to Indication of Diagnostic Hysteroscopy in Post-Menopausal Women. Diagnostics 2020, 10, 257. https://doi.org/10.3390/diagnostics10050257
Saccardi C, Vitagliano A, Marchetti M, Lo Turco A, Tosatto S, Palumbo M, De Lorenzo LS, Vitale SG, Scioscia M, Noventa M. Endometrial Cancer Risk Prediction According to Indication of Diagnostic Hysteroscopy in Post-Menopausal Women. Diagnostics. 2020; 10(5):257. https://doi.org/10.3390/diagnostics10050257
Chicago/Turabian StyleSaccardi, Carlo, Amerigo Vitagliano, Matteo Marchetti, Alice Lo Turco, Sofia Tosatto, Michela Palumbo, Luciana Serena De Lorenzo, Salvatore Giovanni Vitale, Marco Scioscia, and Marco Noventa. 2020. "Endometrial Cancer Risk Prediction According to Indication of Diagnostic Hysteroscopy in Post-Menopausal Women" Diagnostics 10, no. 5: 257. https://doi.org/10.3390/diagnostics10050257
APA StyleSaccardi, C., Vitagliano, A., Marchetti, M., Lo Turco, A., Tosatto, S., Palumbo, M., De Lorenzo, L. S., Vitale, S. G., Scioscia, M., & Noventa, M. (2020). Endometrial Cancer Risk Prediction According to Indication of Diagnostic Hysteroscopy in Post-Menopausal Women. Diagnostics, 10(5), 257. https://doi.org/10.3390/diagnostics10050257









