Analyzing 24-Hour Blood Pressure Measurements with a Novel Cuffless Pulse Transit Time Device in Clinical Practice—Does the Software for Heartbeat Detection Matter?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
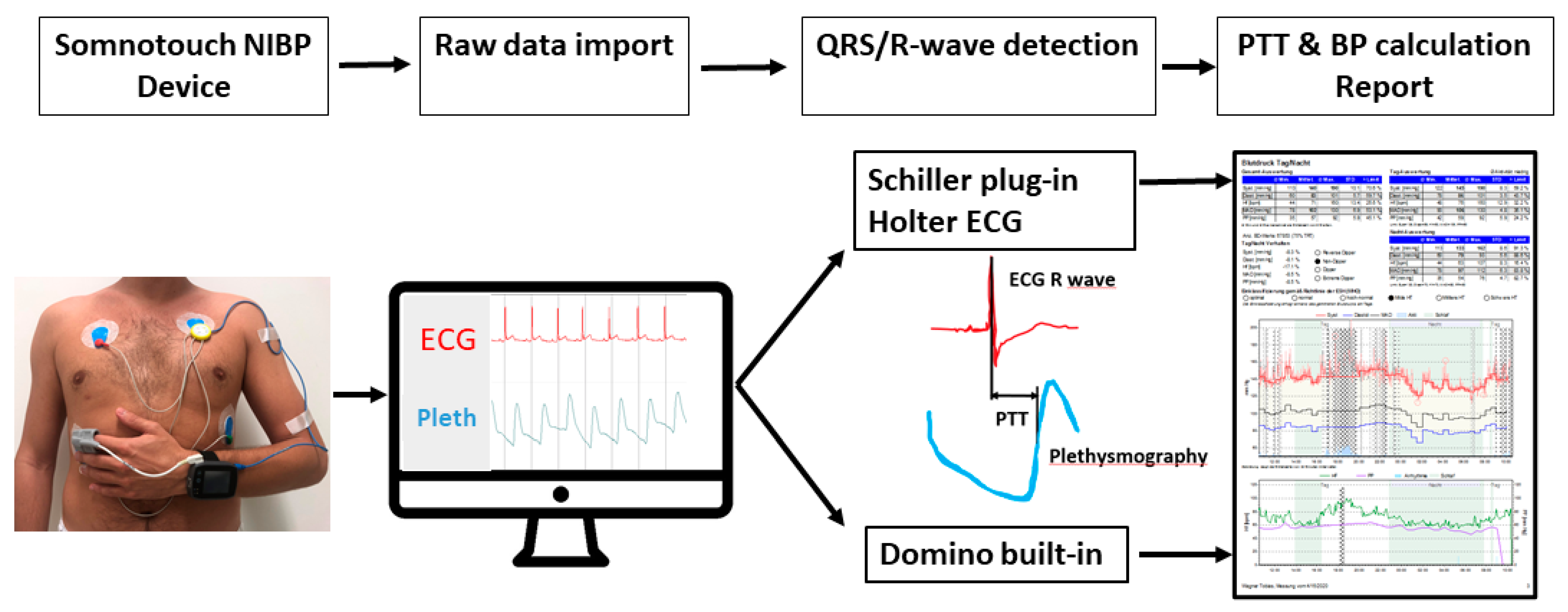
2.2. Device Characteristics and Placement
2.3. Assessment of 24-Hour Blood Pressure Measurement Results
2.4. Blood Pressure Classification
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Comparison of Blood Pressure Results Derived from DominoBP and SchillerBP Software
3.3. Analysis of Samples with an Absolute Blood Pressure Difference of >5 mmHg between Data Generated by DominoBP and SchillerBP Software
3.4. Impact of an Absolute Blood Pressure Difference of > 5 mmHg between Data Generated by DominoBP and SchillerBP Software on Blood Pressure Classification
4. Discussion
4.1. Limitations
4.2. Perspectives
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertensionThe Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Vischer, A.S.; Burkard, T. Principles of Blood Pressure Measurement—Current Techniques, Office vs Ambulatory Blood Pressure Measurement. In Hypertension: From Basic Research to Clinical Practice; Islam, M.d.S., Ed.; Advances in Experimental Medicine and Biology; Springer International Publishing: Cham, Germany, 2017; pp. 85–96. ISBN 978-3-319-44251-8. [Google Scholar]
- Parati, G.; Stergiou, G.; O’Brien, E.; Asmar, R.; Beilin, L.; Bilo, G.; Clement, D.; de la Sierra, A.; de Leeuw, P.; Dolan, E.; et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J. Hypertens. 2014, 32, 1359–1366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, M.; Barbosa, K.; Ho, V.; Griggs, D.; Ghirmai, T.; Krishnan, S.K.; Hsiai, T.K.; Chiao, J.-C.; Cao, H. Cuff-Less and Continuous Blood Pressure Monitoring: A Methodological Review. Technologies 2017, 5, 21. [Google Scholar] [CrossRef] [Green Version]
- Bilo, G.; Zorzi, C.; Ochoa Munera, J.E.; Torlasco, C.; Giuli, V.; Parati, G. Validation of the Somnotouch-NIBP noninvasive continuous blood pressure monitor according to the European Society of Hypertension International Protocol revision 2010. Blood Press. Monit. 2015, 20, 291–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krisai, P.; Vischer, A.S.; Kilian, L.; Meienberg, A.; Mayr, M.; Burkard, T. Accuracy of 24-hour ambulatory blood pressure monitoring by a novel cuffless device in clinical practice. Heart Br. Card. Soc. 2019, 105, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M. The 2017 Clinical Practice Guideline for High Blood Pressure. JAMA 2017, 318, 2073–2074. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, E.; Atkins, N.; Stergiou, G.; Karpettas, N.; Parati, G.; Asmar, R.; Imai, Y.; Wang, J.; Mengden, T.; Shennan, A.; et al. European Society of Hypertension International Protocol revision 2010 for the validation of blood pressure measuring devices in adults. Blood Press. Monit. 2010, 15, 23–38. [Google Scholar] [CrossRef] [PubMed]
- Irving, G.; Holden, J.; Stevens, R.; McManus, R.J. Which cuff should I use? Indirect blood pressure measurement for the diagnosis of hypertension in patients with obesity: A diagnostic accuracy review. BMJ Open 2016, 6, e012429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gesche, H.; Grosskurth, D.; Küchler, G.; Patzak, A. Continuous blood pressure measurement by using the pulse transit time: Comparison to a cuff-based method. Eur. J. Appl. Physiol. 2012, 112, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Schiffrin, E.L. Vascular stiffening and arterial compliance. Implications for systolic blood pressure. Am. J. Hypertens. 2004, 17, 39S–48S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Callaghan, F.J.; Babbs, C.F.; Bourland, J.D.; Geddes, L.A. The relationship between arterial pulse-wave velocity and pulse frequency at different pressures. J. Med. Eng. Technol. 1984, 8, 15–18. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, H.; Yokoi, T.; Yoshika, M. Validation of the OMRON HBP-1300 upper arm blood pressure monitor, in oscillometry mode, for clinic use in a general population, according to the European Society of Hypertension International Protocol revision 2010. Blood Press. Monit. 2015, 20, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.; Zhao, D.; Pan, Y.; Ding, W.; Wei, Q.; Li, H.; Gao, P.; Mi, J. Validation of Omron HBP-1300 professional blood pressure monitor based on auscultation in children and adults. BMC Cardiovasc. Disord. 2016, 16, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hypertension in adults: Diagnosis and management|Guidance and guidelines|NICE. Available online: https://www.nice.org.uk/guidance/cg127 (accessed on 16 December 2018).
- Zachwieja, J.; Neyman-Bartkowiak, A.; Rabiega, A.; Wojciechowska, M.; Barabasz, M.; Musielak, A.; Silska-Dittmar, M.; Ostalska-Nowicka, D. Comparison of cuff-based and cuffless continuous blood pressure measurements in children and adolescents. Clin. Exp. Hypertens. 2020, 42, 512–518. [Google Scholar] [CrossRef] [PubMed]




| Method | Device/Components | Basic Principles of Measurement | Advantages | Disadvantages |
|---|---|---|---|---|
| Mercury Sphygmomanometer | Sphygmomanometer and auscultation by observer | Manual inflation and deflation of the cuff and auscultation of Korotkoff sounds. First sound appearing is the systolic blood pressure, the complete disappearance of the sound indicates diastolic blood pressure | Gold-standard for non-invasive brachial blood pressure measurement. Reference device in validation studies for single measurement comparisons | Safety and economic concerns related to mercury use. Prone to observer related errors. No ABPM * possible |
| Aneroid Sphygmomanometer | Sphygmomanometer and auscultation by observer | Lever and belly system instead of mercury sphygmomanometer | No mercury. Low-priced devices | Prone to observer related errors. No ABPM possible |
| Oscillometric or auscultatory automated BP devices | Monitor including cuff and bladder (Different validated models commercially available) | Oscillometric pressure changes of cuff pressure or Korotkoff sounds are registered by electronic sensors in the cuff, and BP is calculated by device-specific algorithms ABPM by single intermittent measurements over 24 h, usually every 20 to 30 min | Cost-effective. Standard in most clinical settings. Specific devices for ABPM available. Devices can be used for at-home blood pressure measurement. | Different measurement protocols available. Large number of non-validated devices on the market. Discomfort for the patient. Intermittent measurement in case of ABPM. |
| Pulse-Transit Time Measurement (PTT) | Monitor, Finger-photoplethysmograph, ECG (e.g., Somnotouch-NIBP (Somnomedic GmbH, Randersacker, Germany)) | Time-interval between R-wave on the ECG and the arrival of the corresponding pulse wave at the finger-photoplethysmograph (PTT) can be calculated. After calibration to a single standard, BP measurement changes in PTT are translated into changes of BP values according to specific algorithms. Beat-to-beat BP calculation. | Less discomfort for patients. Device for ABPM. Beat-to-beat blood pressure measurement possible. 24h-ECG, pulse oximetry and actigraphy as additional information over 24 h. | Validated for single measurements. Seems to result in higher BP values, when used over 24 h compared to standard devices. More complex analysis of examinations. |
| Volume-clamp-technique Finapres (FINger Arterial PRESsure) | Finger-cuff and bladder, Finger-plethysmograph (Finapres (Finapres Medical Systems BV, Enschede, Netherlands)) | Finger arterial pressure and waveform is measured using a finger cuff and an inflatable bladder in combination with a finger-plethysmograph. After calibration to standard BP, beat-to-beat blood pressure is calculated according to specific algorithms. | Less discomfort for the patient. Beat-to-beat blood pressure measurement. | Incomplete validation. No ABPM possible. (Portapress not available on the market anymore) Used mainly for research purposes. |
| Characteristic | Overall (n = 234) | |
|---|---|---|
| Sex (male), n | 148 (63.2%) | |
| Age, years | 51.9 (±13.3, (19–75)) | |
| Calibration systolic BP, mmHg | 129 (±23, (81–223)) | |
| Calibration diastolic BP, mmHg | 83 (±16, (55–116)) | |
| Classification | Systolic BP | Diastolic BP |
| Calibration low *, n | 130 (55.6) | 97 (41.5) |
| Calibration medium *, n | 92 (39.3) | 122 (52.1) |
| Calibration high *, n | 12 (5.1) | 15 (6.4) |
| DominoBP Awake | ||
| Normotensive, n | 144 (61.5) | 113 (48.3) |
| Stage 1 **, n | 49 (20.9) | 71 (30.3) |
| Stage 2 **, n | 41 (17.5) | 50 (21.4) |
| Severe hypertension ** °, n | 5 (2.1) | 7 (2.9) |
| SchillerBP Awake | ||
| Normotensive, n | 142 (60.7) | 118 (50.4) |
| Stage 1 **, n | 53 (22.6) | 66 (28.2) |
| Stage 2 **, n | 39 (16.7) | 50 (21.4) |
| Severe hypertension ** °, n | 4 (1.7) | 7 (2.9) |
| All Patients n (%) n = 234 | Patients with ≤ 5 mmHg Difference between DominoBP and SchillerBP n = 210 * | Patients with > 5 mmHg Difference between DominoBP and SchillerBP n = 24 * | * p-Value | |
|---|---|---|---|---|
| Sinus Rhythm | 232 (99.1%) | 208 (99.0%) | 24 (100%) | 1.00 |
| Persistent or Paroxysmal Atrial Fibrillation | 4 (1.7%) | 4 (1.9%) | 0 (0%) | 1.0 |
| Premature Atrial Contractions ≥ 5% | 0 (0%) | 0 (0%) | 0 (0%) | 1.0 |
| Premature Ventricular Contractions ≥ 5% | 2 (0.9%) | 1 (0.5%) | 1 (4.2%) | 0.195 |
| Right Bundle Branch Block | 7 (3.0%) | 5 (2.4%) | 2 (8.3%) | 0.154 |
| Left Bundle Branch Block | 5 (2.1%) | 3 (1.4%) | 2 (8.3%) | 0.0833 |
| BP, mmHg | DominoBP | SchillerBP | p-Values |
|---|---|---|---|
| Systolic | |||
| 24-hour | 128 (116–141) | 129 (118–142) | 0.268 |
| Awake | 130 (119–143) | 131 (119–144) | 0.022 |
| Asleep | 126 (114–139) | 126 (114–139) | 0.424 |
| Diastolic | |||
| 24-hour | 84 (76–92) | 84 (76–92) | 0.569 |
| Awake | 85 (77–93) | 85 (77–93) | 0.507 |
| Asleep | 82 (75–91) | 82 (74–91) | 0.612 |
| Systolic BP (mmHg) | Mean Difference (SD) | Mean Absolute Difference (SD) |
| 24-hour | 0.22 (± 2.59) | 1.5 (± 1.7) |
| Awake | 0.39 (± 2.55) | 1.5 (± 1.6) |
| Asleep | −0.04 (± 2.97) | 1.7 (± 1.8) |
| Diastolic BP (mmHg) | ||
| 24-hour | 0.13 (± 2.23) | 1.1 (± 1.3) |
| Awake | 0.13 (± 2.23) | 1.1 (± 1.5) |
| Asleep | -0.06 (± 2.71) | 1.4 (± 1.9) |
| <135 mmHg | ≥135; <150 mmHg | ≥150 mmHg | ≥180 mmHg | Overall | |
|---|---|---|---|---|---|
| n (%) | (n = 144) | (n = 49) | (n = 41) | (n = 5) | (n = 234) |
| 24-hour | |||||
| Mean difference, mmHg | 0.35 (±2.74) | 0.24 (±1.57) | 0.03 (±2.87) | −0.20 (±1.64) | 0.22 (±2.59) |
| ≤2 mmHg | 114 (79.1%) | 42 (85.7%) | 34 (82.9%) | 4 (80%) | 190 (81.1%) |
| ≤5 mmHg | 136 (94.4%) | 49 (100%) | 37 (90.2%) | 5 (100%) | 222 (94.8%) |
| ≤10 mmHg | 142 (98.6%) | 49 (100%) | 40 (97.5%) | 5 (100%) | 231 (98.7%) |
| ≤15 mmHg | 144 (100%) | 49 (100%) | 41 (100%) | 5 (100%) | 234 (100%) |
| Awake | |||||
| Mean difference, mmHg | 0.51 (± 2.65) | 0.35 (± 1.82) | 0.29 (± 2.81) | −0.20 (±1.64) | 0.39 (±2.59) |
| ≤2 mmHg | 116 (80.5%) | 43 (87.7%) | 34 (82.9%) | 4 (80%) | 193 (82.4%) |
| ≤5 mmHg | 139 (96.5%) | 48 (97.9%) | 38 (92.6%) | 5 (100%) | 225 (96.1%) |
| ≤10 mmHg | 142 (98.6%) | 49 (100%) | 40 (97.5%) | 5 (100%) | 231 (98.7%) |
| ≤15 mmHg | 144 (100%) | 49 (100%) | 41 (100%) | 5 (100%) | 234 (100%) |
| Asleep | |||||
| Mean difference, mmHg | 0.13 (±3.18) | −0.16 (±1.80) | −0.24 (±3.22) | 0.40 (± 2.60) | −0.04 (±2.97) |
| ≤2 mmHg | 114 (79.1%) | 42 (85.7%) | 32 (78.0%) | 4 (80%) | 188 (80.3%) |
| ≤5 mmHg | 135 (93.7%) | 48 (97.9%) | 36 (87.8%) | 5 (100%) | 219 (93.5%) |
| ≤10 mmHg | 142 (98.6%) | 49 (100%) | 40 (97.5%) | 5 (100%) | 231 (98.7%) |
| ≤15 mmHg | 143 (99.3%) | 49 (100%) | 41 (100%) | 5 (100%) | 233 (99.5%) |
| <85 mmHg | ≥85; <95 mmHg | ≥95 mmHg | ≥110 mmHg | Overall | |
|---|---|---|---|---|---|
| n (%) | (n = 113) | (n = 71) | (n = 50) | (n = 7) | (n = 234) |
| 24-hour | |||||
| Mean difference, mmHg | 0.22 (± 1.92) | 0.35 (± 2.26) | −0.39 (± 2.75) | 0.29 (± 0.75) | 0.13 (± 2.23) |
| ≤2 mmHg | 99 (88.3%) | 60 (84.5%) | 46 (90.1%) | 7 (100%) | 205 (87.6%) |
| ≤5 mmHg | 111 (99.1%) | 68 (95.7%) | 49 (96.0%) | 7 (100%) | 228 (97.4%) |
| ≤10 mmHg | 111 (99.1%) | 71 (100%) | 50 (98.0%) | 7 (100%) | 232 (99.1%) |
| ≤15 mmHg | 112 (100%) | 71 (100%) | 50 (98.0%) | 7 (100%) | 233 (99.5%) |
| Awake | |||||
| Mean difference, mmHg | 0.23 (± 1.93) | 0.34 (± 2.24) | −0.39 (± 2.75) | −0.14 (± 0.90) | 0.13 (± 2.23) |
| ≤2 mmHg | 100 (79.1%) | 62 (87.3%) | 46 (90.1%) | 7 (100%) | 208 (88.8%) |
| ≤5 mmHg | 111 (99.1%) | 68 (95.7%) | 49 (96.0%) | 7 (100%) | 228 (93.5%) |
| ≤10 mmHg | 111 (99.1%) | 70 (98.5%) | 50 (98.0%) | 7 (100%) | 231 (98.2%) |
| ≤15 mmHg | 112 (100%) | 71 (100%) | 50 (98.0%) | 7 (100%) | 233 (99.5%) |
| Asleep | |||||
| Mean difference, mmHg | 0.04 (± 2.54) | 0.18 (± 2.45) | −0.61 (± 3.34) | 0.00 (± 0.57) | −0.06 (± 2.71) |
| ≤2 mmHg | 99 (88.3%) | 61 (85.9%) | 44 (86.2%) | 7 (100%) | 204 (87.1%) |
| ≤5 mmHg | 107 (95.5%) | 68 (95.7%) | 48 (94.1%) | 7 (100%) | 223 (95.2%) |
| ≤ 10 mmHg | 110 (98.2%) | 71 (100%) | 49 (96.0%) | 7 (100%) | 230 (98.2%) |
| ≤15 mmHg | 112 (100%) | 71 (100%) | 50 (98.0%) | 7 (100%) | 233 (99.5%) |
| Characteristics | Overall (n = 24) | |
|---|---|---|
| Sex (male), n | 18 (75%) | |
| Age, years | 54.5 (±13.1, (31–74)) | |
| Calibration systolic BP, mmHg | 132.8 (±30.3, (98–223)) | |
| Calibration diastolic BP, mmHg | 83 (±13.8, (62–112)) | |
| Systolic BP | Diastolic BP | |
| Absolute BP Differences > 5mmHg n (% of 234 patients) | ||
| 24-hour | 12 (5.1%) | 6 (2.5%) |
| Awake | 9 (3.8%) | 6 (2.5%) |
| Asleep | 15 (6.4%) | 11 (4.7%) |
| Blood Pressure Ranges in Different BP Categories n/subjects (%) | ||
| Calibration BP | ||
| Low * | 13/130 (10%) | 11/97 (11.3%) |
| Medium | 9/92 (9.8%) | 12/122 (9.8%) |
| High | 2/12 (16.7%) | 1/1 (6.7%) |
| DominoBP Awake | ||
| Normotensive | 14/144 (9.7%) | 11/113 (9.7%) |
| Stage 1 ** | 4/49 (8.2%) | 7/71 (9.9%) |
| Stage 2 ** | 6/41 (14.6%) | 6/50 (12%) |
| Severe hypertension ** ° | 1/5 (20%) | 0/7 (0%) |
| SchillerBP Awake | ||
| Normotensive | 11/142 (7.7%) | 14/11 (11.9%) |
| Stage 1 ** | 8/53 (15.1%) | 3/66 (4.5%) |
| Stage 2 ** | 5/39 (12.8%) | 7/50 (14%) |
| Severe hypertension ** ° | 1/4 (25%) | 1/7 (14.3%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kilian, L.; Krisai, P.; Socrates, T.; Arranto, C.; Pfister, O.; Meienberg, A.; Mayr, M.; Vischer, A.S.; Burkard, T. Analyzing 24-Hour Blood Pressure Measurements with a Novel Cuffless Pulse Transit Time Device in Clinical Practice—Does the Software for Heartbeat Detection Matter? Diagnostics 2020, 10, 361. https://doi.org/10.3390/diagnostics10060361
Kilian L, Krisai P, Socrates T, Arranto C, Pfister O, Meienberg A, Mayr M, Vischer AS, Burkard T. Analyzing 24-Hour Blood Pressure Measurements with a Novel Cuffless Pulse Transit Time Device in Clinical Practice—Does the Software for Heartbeat Detection Matter? Diagnostics. 2020; 10(6):361. https://doi.org/10.3390/diagnostics10060361
Chicago/Turabian StyleKilian, Leo, Philipp Krisai, Thenral Socrates, Christian Arranto, Otmar Pfister, Andrea Meienberg, Michael Mayr, Annina S. Vischer, and Thilo Burkard. 2020. "Analyzing 24-Hour Blood Pressure Measurements with a Novel Cuffless Pulse Transit Time Device in Clinical Practice—Does the Software for Heartbeat Detection Matter?" Diagnostics 10, no. 6: 361. https://doi.org/10.3390/diagnostics10060361
APA StyleKilian, L., Krisai, P., Socrates, T., Arranto, C., Pfister, O., Meienberg, A., Mayr, M., Vischer, A. S., & Burkard, T. (2020). Analyzing 24-Hour Blood Pressure Measurements with a Novel Cuffless Pulse Transit Time Device in Clinical Practice—Does the Software for Heartbeat Detection Matter? Diagnostics, 10(6), 361. https://doi.org/10.3390/diagnostics10060361






