The Quantitative Skeletal Muscle Ultrasonography in Elderly with Dynapenia but Not Sarcopenia Using Texture Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Grouping
2.2. Anthropometric Measurement
2.3. Strength and Physical Performance
2.4. Ultrasound Measurement Protocol
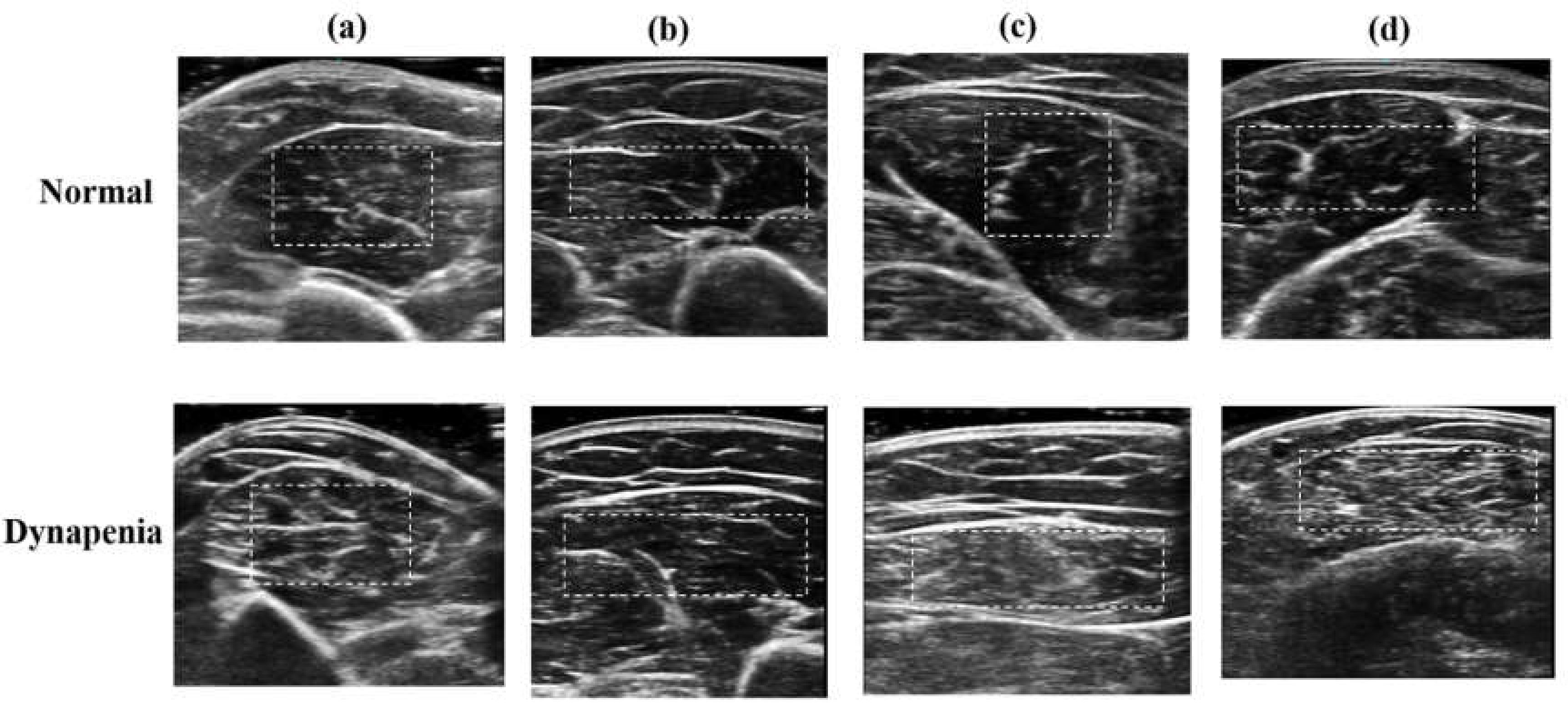
2.5. Texture Analysis of Ultrasound Image
- (a)
- Autocorrelation (AUT) refers to repeating patterns of gray levels, measuring amount of regularity as well as the fineness/coarseness of texture.
- (b)
- Contrast (CON) measures the local intensity contrast between a pixel and its neighbor over the whole image. Low CON values indicate the similar gray levels of each pixel pair.
- (c)
- Cluster prominence (CPR) measures the grouping of pixels to characterize the clustering tendency of the pixels.
- (d)
- Dissimilarity (DIS) measures the distance between pairs of pixels and is conceptually similar to the CON feature.
- (e)
- Energy (ENE) measures the repetition of the pixel pairs to represent textural uniformity. High ENE values occur when the occurrence of repeated pixel pairs is high.
- (f)
- Entropy (ENP) measures the randomness of gray level distribution to describe the degree of complication of textures of an image. The randomly distributed gray levels tend to have high ENP values.
- (g)
- Homogeneity (HOM) measures the local homogeneity of a pixel pair. The HOM value is high if the gray level differences in the pixel pairs are small.
- (h)
- Maximum probability (MAXP) is retrieved from maximum value in the pixel pair. High MAXP values represent the high occurrence of the most predominant pixel pair.
- (i)
- Sum variance (SVAR) measures the dispersion of the gray levels and is mathematically equal to the cluster tendency feature.
2.6. The Definition of Dynapenia Without Sarcopenia
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Parameter | Position | Cutoff Point | Accuracy | Sensitivity | Specificity | PPV | NPV | Positive Likelihood Ratios | Negative Likelihood Ratios |
|---|---|---|---|---|---|---|---|---|---|
| Autocorrelation | Biceps brachii | 7.89 | 86% | 94% | 78% | 81% | 93% | 4.25 | 0.07 |
| Triceps brachii | 10.39 | 67% | 61% | 72% | 69% | 65% | 2.20 | 0.54 | |
| Medial gastrocnemius | 9.48 | 78% | 67% | 89% | 86% | 73% | 6.00 | 0.38 | |
| Rectus femoris | 7.96 | 78% | 61% | 94% | 92% | 71% | 11.00 | 0.41 | |
| Cluster prominence | Biceps brachii | 141.01 | 61% | 56% | 67% | 63% | 60% | 1.67 | 0.67 |
| Triceps brachii | 188.84 | 64% | 67% | 61% | 63% | 65% | 1.71 | 0.55 | |
| Medial gastrocnemius | 203.55 | 64% | 78% | 50% | 61% | 69% | 1.56 | 0.44 | |
| Rectus femoris | 206.87 | 69% | 89% | 50% | 64% | 82% | 1.78 | 0.22 | |
| Sum variance | Biceps brachii | 16.47 | 89% | 94% | 83% | 85% | 94% | 5.67 | 0.07 |
| Triceps brachii | 23.25 | 69% | 61% | 78% | 73% | 67% | 2.75 | 0.50 | |
| Medial gastrocnemius | 20.30 | 78% | 67% | 89% | 86% | 73% | 6.00 | 0.38 | |
| Rectus femoris | 12.67 | 78% | 89% | 67% | 73% | 86% | 2.67 | 0.17 |
References
- Wilkinson, D.J.; Piasecki, M.; Atherton, P.J. The age-related loss of skeletal muscle mass and function: Measurement and physiology of muscle fibre atrophy and muscle fibre loss in humans. Ageing Res. Rev. 2018, 47, 123–132. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef]
- Chen, L.K.; Liu, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Bahyah, K.S.; Chou, M.Y.; Chen, L.Y.; Hsu, P.S.; Krairit, O.; et al. Sarcopenia in Asia: Consensus report of the Asian Working Group for Sarcopenia. J. Am. Med. Dir. Assoc. 2014, 15, 95–101. [Google Scholar] [CrossRef]
- Studenski, S.A.; Peters, K.W.; Alley, D.E.; Cawthon, P.M.; McLean, R.R.; Harris, T.B.; Ferrucci, L.; Guralnik, J.M.; Fragala, M.S.; Kenny, A.M.; et al. The FNIH sarcopenia project: Rationale, study description, conference recommendations, and final estimates. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 547–558. [Google Scholar] [CrossRef]
- Clark, B.C.; Manini, T.M. Sarcopenia =/= dynapenia. J. Gerontol. 2008, 63, 829–834. [Google Scholar]
- Manini, T.M.; Clark, B.C. Dynapenia and aging: An update. The journals of gerontology Series A. Biol. Sci. Med. Sci. 2012, 67, 28–40. [Google Scholar] [CrossRef]
- Tieland, M.; Trouwborst, I.; Clark, B.C. Skeletal muscle performance and ageing. J. Cachexia Sarcopenia Muscle 2018, 9, 3–19. [Google Scholar] [CrossRef]
- Lee, K.; Shin, Y.; Huh, J.; Sung, Y.S.; Lee, I.S.; Yoon, K.H.; Kim, K.W. Recent Issues on Body Composition Imaging for Sarcopenia Evaluation. Korean J. Radiol. 2019, 20, 205–217. [Google Scholar] [CrossRef]
- Ticinesi, A.; Meschi, T.; Narici, M.V.; Lauretani, F.; Maggio, M. Muscle Ultrasound and Sarcopenia in Older Individuals: A Clinical Perspective. J. Am. Med. Dir. Assoc. 2017, 18, 290–300. [Google Scholar] [CrossRef]
- Strasser, E.M.; Draskovits, T.; Praschak, M.; Quittan, M.; Graf, A. Association between ultrasound measurements of muscle thickness, pennation angle, echogenicity and skeletal muscle strength in the elderly. Age 2013, 35, 2377–2388. [Google Scholar] [CrossRef]
- Chang, K.-V.; Wu, W.-T.; Huang, K.-C.; Jan, W.H.; Han, D.-S. Limb muscle quality and quantity in elderly adults with dynapenia but not sarcopenia: An ultrasound imaging study. Exp. Gerontol. 2018, 108, 54–61. [Google Scholar] [CrossRef]
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Nishio, N.; Abe, Y.; Kakehi, T.; Fujimoto, J.; Tanaka, T.; Ohji, S.; Otobe, Y.; et al. Differential Characteristics of Skeletal Muscle in Community-Dwelling Older Adults. J. Am. Med. Dir. Assoc. 2017, 18, 807.e809–807.e816. [Google Scholar] [CrossRef]
- Hughes, M.S.; Marsh, J.N.; Wallace, K.D.; Donahue, T.A.; Connolly, A.M.; Lanza, G.M.; Wickline, S.A. Sensitive ultrasonic detection of dystrophic skeletal muscle in patients with duchenne muscular dystrophy using an entropy-based signal receiver. Ultrasound Med. Biol. 2007, 33, 1236–1243. [Google Scholar] [CrossRef]
- Hwang, H.E.; Hsu, T.R.; Lee, Y.H.; Wang, H.K.; Chiou, H.J.; Niu, D.M. Muscle ultrasound: A useful tool in newborn screening for infantile onset pompe disease. Medicine 2017, 96, e8415. [Google Scholar] [CrossRef]
- Akima, H.; Hioki, M.; Yoshiko, A.; Koike, T.; Sakakibara, H.; Takahashi, H.; Oshida, Y. Intramuscular adipose tissue determined by T1-weighted MRI at 3T primarily reflects extramyocellular lipids. Magn. Reson. Imaging 2016, 34, 397–403. [Google Scholar] [CrossRef]
- Pillen, S.; Tak, R.O.; Zwarts, M.J.; Lammens, M.M.Y.; Verrijp, K.N.; Arts, I.M.P.; van der Laak, J.A.; Hoogerbrugge, P.M.; van Engelen, B.G.M.; Verrips, A. Skeletal muscle ultrasound: Correlation between fibrous tissue and echo intensity. Ultrasound Med. Biol. 2009, 35, 443–446. [Google Scholar] [CrossRef]
- Haralick, R.M.; Shanmugam, K.; Dinstein, I.H. Textural Features for Image Classification. IEEE Trans. Syst. Man Cybern. 1973, 3, 610–621. [Google Scholar]
- Unser, M. Sum and Difference Histograms for Texture Classification. IEEE Trans. Pattern Anal. Mach. Intell. 1986, 8, 118–125. [Google Scholar]
- Pillen, S. Skeletal muscle ultrasound. Eur. J. Transl. Myol. 2010, 1, 145–155. [Google Scholar]
- Liao, Y.Y.; Yang, K.C.; Lee, M.J.; Huang, K.C.; Chen, J.D.; Yeh, C.K. Multifeature analysis of an ultrasound quantitative diagnostic index for classifying nonalcoholic fatty liver disease. Sci. Rep. 2016, 6, 35083. [Google Scholar] [CrossRef]
- Liao, Y.Y.; Wu, J.C.; Li, C.H.; Yeh, C.K. Texture feature analysis for breast ultrasound image enhancement. Ultrason. Imaging 2011, 33, 264–278. [Google Scholar] [CrossRef]
- Han, D.S.; Chang, K.V.; Li, C.M.; Lin, Y.H.; Kao, T.W.; Tsai, K.S.; Wang, T.G.; Yang, W.S. Skeletal muscle mass adjusted by height correlated better with muscular functions than that adjusted by body weight in defining sarcopenia. Sci. Rep. 2016, 6, 19457. [Google Scholar] [CrossRef]
- Delmonico, M.J.; Harris, T.B.; Visser, M.; Park, S.W.; Conroy, M.B.; Velasquez-Mieyer, P.; Boudreau, R.; Manini, T.M.; Nevitt, M.; Newman, A.B.; et al. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am. J. Clin. Nutr. 2009, 90, 1579–1585. [Google Scholar] [CrossRef]
- Beaudart, C.; Zaaria, M.; Pasleau, F.; Reginster, J.Y.; Bruyere, O. Health Outcomes of Sarcopenia: A Systematic Review and Meta-Analysis. PLoS ONE 2017, 12, e0169548. [Google Scholar] [CrossRef]
- Buckinx, F.; Landi, F.; Cesari, M.; Fielding, R.A.; Visser, M.; Engelke, K.; Maggi, S.; Dennison, E.; Al-Daghri, N.M.; Allepaerts, S.; et al. Pitfalls in the measurement of muscle mass: A need for a reference standard. J. Cachexia Sarcopenia Muscle 2018, 9, 269–278. [Google Scholar] [CrossRef]
- Scherbakov, N.; Doehner, W. Do we need a reference standard for the muscle mass measurements? ESC Heart Fail 2018, 5, 741–744. [Google Scholar] [CrossRef]
- Zaidman, C.M.; Malkus, E.C.; Siener, C.; Florence, J.; Pestronk, A.; Al-Lozi, M. Qualitative and quantitative skeletal muscle ultrasound in late-onset acid maltase deficiency. Muscle Nerve 2011, 44, 418–423. [Google Scholar] [CrossRef]
- Mul, K.; Horlings, C.G.C.; Vincenten, S.C.C.; Voermans, N.C.; van Engelen, B.G.M.; van Alfen, N. Quantitative muscle MRI and ultrasound for facioscapulohumeral muscular dystrophy: Complementary imaging biomarkers. J. Neurol. 2018, 265, 2646–2655. [Google Scholar] [CrossRef]
- Narici, M.V.; Maganaris, C.N.; Reeves, N.D.; Capodaglio, P. Effect of aging on human muscle architecture. J. Appl. Physiol. 2003, 95, 2229–2234. [Google Scholar] [CrossRef]
- Massey, G.; Evangelidis, P.; Folland, J. Influence of contractile force on the architecture and morphology of the quadriceps femoris. Exp. Physiol. 2015, 100, 1342–1351. [Google Scholar] [CrossRef]
- Morse, C.I.; Thom, J.M.; Birch, K.M.; Narici, M.V. Changes in triceps surae muscle architecture with sarcopenia. Acta Physiol. Scand. 2005, 183, 291–298. [Google Scholar] [CrossRef]
- Fukumoto, Y.; Ikezoe, T.; Yamada, Y.; Tsukagoshi, R.; Nakamura, M.; Mori, N.; Kimura, M.; Ichihashi, N. Skeletal muscle quality assessed from echo intensity is associated with muscle strength of middle-aged and elderly persons. Eur. J. Appl. Physiol. 2012, 112, 1519–1525. [Google Scholar] [CrossRef]
- Watanabe, Y.; Yamada, Y.; Fukumoto, Y.; Ishihara, T.; Yokoyama, K.; Yoshida, T.; Miyake, M.; Yamagata, E.; Kimura, M. Echo intensity obtained from ultrasonography images reflecting muscle strength in elderly men. Clin. Interv. Aging 2013, 8, 993–998. [Google Scholar] [CrossRef]
- Cadore, E.L.; Izquierdo, M.; Conceicao, M.; Radaelli, R.; Pinto, R.S.; Baroni, B.M.; Vaz, M.A.; Alberton, C.L.; Pinto, S.S.; Cunha, G.; et al. Echo intensity is associated with skeletal muscle power and cardiovascular performance in elderly men. Exp. Gerontol. 2012, 47, 473–478. [Google Scholar] [CrossRef]
- Rech, A.; Radaelli, R.; Goltz, F.R.; da Rosa, L.H.; Schneider, C.D.; Pinto, R.S. Echo intensity is negatively associated with functional capacity in older women. Age 2014, 36, 9708. [Google Scholar] [CrossRef]
- Lopez, P.; Wilhelm, E.N.; Rech, A.; Minozzo, F.; Radaelli, R.; Pinto, R.S. Echo intensity independently predicts functionality in sedentary older men. Muscle Nerve 2017, 55, 9–15. [Google Scholar] [CrossRef]
- Berger, J.; Bunout, D.; Barrera, G.; de la Maza, M.P.; Henriquez, S.; Leiva, L.; Hirsch, S. Rectus femoris (RF) ultrasound for the assessment of muscle mass in older people. Arch. Gerontol. Geriatr. 2015, 61, 33–38. [Google Scholar] [CrossRef]
- Ismail, C.; Zabal, J.; Hernandez, H.J.; Woletz, P.; Manning, H.; Teixeira, C.; DiPietro, L.; Blackman, M.R.; Harris-Love, M.O. Diagnostic ultrasound estimates of muscle mass and muscle quality discriminate between women with and without sarcopenia. Front. Physiol. 2015, 6, 302. [Google Scholar] [CrossRef]
| Total | Non-Dynapenia | Dynapenia | p-Value | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| N (%) | 36 | 18 (50%) | 18 (50%) | |
| Demographics | ||||
| Men, n (%) | 8 (22.2%) | 4 (22.2%) | 4 (22.2%) | 1.000 |
| Age (years) | 72.69 (5.80) | 70.88 (4.17) | 74.50 (6.71) | 0.060 |
| Waist (cm) | 80.53 (8.53) | 78.51 (8.59) | 82.55 (8.20) | 0.158 |
| BMI (kg/m2) | 23.58 (3.37) | 22.78 (3.50) | 24.39 (7.31) | 0.702 |
| Physical performance | ||||
| Handgrip (kg) | 24.14 (7.57) | 29.28 (6.32) | 19.00 (4.72) | <0.0001 |
| Gait speed (m/s) | 1.21 (0.30) | 1.30 (0.25) | 1.11 (0.31) | 0.056 |
| SMI (kg/m2) | 6.19 (0.83) | 6.15 (0.77) | 6.24 (0.91) | 0.751 |
| Health behavior | N (%) | N (%) | N (%) | p-value |
| Smoke (current) | 1 (2.8%) | 1 (5.6%) | 0 (0.0%) | 1.000 |
| Alcohol (current) | 9 (25%) | 6 (33.0%) | 3 (16.7%) | 0.248 |
| Betel nut (current) | 2 (5.6%) | 1 (5.6%) | 1 (5.6%) | 1.000 |
| Exercise (regular) | 17 (47.2%) | 10 (55.6%) | 7 (38.9%) | 0.317 |
| Upper Extremity | Lower Extremity | |||
|---|---|---|---|---|
| Biceps Brachii | Triceps Brachii | Medial Gastrocnemius | Rectus Femoris | |
| Autocorrelation (AUT) | + *** | + *** | + ** | + * |
| Contrast (CON) | + ** | + ** | + | + |
| Cluster Prominence (CPR) | + | + * | + * | + |
| Dissimilarity (DIS) | + ** | + ** | + | + |
| Energy (ENE) | − | − * | − | − |
| Entropy (ENP) | 2020 * | + ** | + | + |
| Homogeneity (HOM) | − ** | − * | − | + |
| Maximum probability (MAXP) | − | − * | − * | − |
| Sum variance (SVAR) | + *** | + *** | + ** | + * |
| Biceps Brachii | Triceps Brachii | Medial Gastrocnemius | Rectus Femoris | |||||
|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | AUC (95%CI) | OR (95%CI) | AUC (95%CI) | OR (95%CI) | AUC (95%CI) | OR (95%CI) | AUC (95%CI) | |
| Autocorrelation | 2.51 (1.24−5.07) ** | 0.94 (0.86−1.00) | 2.48 (1.16−5.30) * | 0.90 (0.81−0.99) | 1.58 (1.01−2.47) * | 0.86 (0.73−0.99)) | 1.56 (0.99−2.46) | 0.85 (0.73−0.98) |
| Cluster prominence | 1.01 (1.00−1.02) | 0.84 (0.71−0.97) | 1.01 (1.00−1.02) * | 0.91 (0.80−1.00) | 0.99 (0.99−1.01) | 0.78 (0.63−0.94) | 1.01 (1.00−1.01) * | 0.84 (0.71−0.97) |
| Sum variance | 1.45 (1.10−1.91) ** | 0.94 (0.87−1.00) | 1.57 (1.08−2.28) * | 0.91 (0.82−1.00) | 1.20 (1.00−1.44) * | 0.85 (0.71−0.99) | 1.18 (0.99−1.39) | 0.84 (0.71−0.97) |
| Muscle | Parameter | Age | BMI | SMI | Grip | Gait |
|---|---|---|---|---|---|---|
| Biceps brachii | AUT | 0.18 | 0.02 | −0.07 | −0.46 ** | 0.16 |
| CPR | −0.09 | −0.25 | −0.18 | −0.11 | −0.33 | |
| SVAR | 0.17 | 0.06 | −0.05 | −0.47 ** | 0.17 | |
| Triceps brachii | AUT | 0.20 | −0.02 | −0.17 | −0.46 ** | 0.08 |
| CPR | −0.06 | 0.13 | −0.04 | −0.34 * | 0.07 | |
| SVAR | 0.17 | −0.001 | −0.14 | −0.44 ** | 0.08 | |
| Medial gastrocnemius | AUT | 0.18 | 0.18 | 0.02 | −0.49 ** | 0.35 * |
| CPR | −0.54 *** | −0.09 | −0.10 | 0.12 | −0.24 | |
| SVAR | 0.18 | 0.19 | 0.01 | −0.50 ** | 0.35 * | |
| Rectus femoris | AUT | −0.05 | 0.09 | −0.09 | −0.47 ** | −0.09 |
| CPR | −0.37 | 0.07 | −0.07 | −0.16 | −0.30 | |
| SVAR | −0.02 | 0.09 | −0.09 | −0.46 ** | −0.09 |
| Parameter | Adjusted R2 | |||
|---|---|---|---|---|
| Model 1 | Model 2 | p-Value * | ||
| Autocorrelation (AUT) | Biceps brachii | 0.371 | 0.506 | 0.004 |
| Triceps brachii | 0.466 | 0.016 | ||
| Medial gastrocnemius | 0.438 | 0.010 | ||
| Rectus femoris | 0.422 | 0.064 | ||
| Cluster prominence (CPR) | Biceps brachii | 0.371 | 0.371 | 0.330 |
| Triceps brachii | 0.425 | 0.058 | ||
| Medial gastrocnemius | 0.353 | 0.749 | ||
| Rectus femoris | 0.374 | 0.299 | ||
| Sum variance (SVAR) | Biceps brachii | 0.371 | 0.516 | 0.003 |
| Triceps brachii | 0.467 | 0.016 | ||
| Medial gastrocnemius | 0.483 | 0.010 | ||
| Rectus femoris | 0.412 | 0.087 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, K.-C.; Liao, Y.-Y.; Chang, K.-V.; Huang, K.-C.; Han, D.-S. The Quantitative Skeletal Muscle Ultrasonography in Elderly with Dynapenia but Not Sarcopenia Using Texture Analysis. Diagnostics 2020, 10, 400. https://doi.org/10.3390/diagnostics10060400
Yang K-C, Liao Y-Y, Chang K-V, Huang K-C, Han D-S. The Quantitative Skeletal Muscle Ultrasonography in Elderly with Dynapenia but Not Sarcopenia Using Texture Analysis. Diagnostics. 2020; 10(6):400. https://doi.org/10.3390/diagnostics10060400
Chicago/Turabian StyleYang, Kuen-Cheh, Yin-Yin Liao, Ke-Vin Chang, Kuo-Chin Huang, and Der-Sheng Han. 2020. "The Quantitative Skeletal Muscle Ultrasonography in Elderly with Dynapenia but Not Sarcopenia Using Texture Analysis" Diagnostics 10, no. 6: 400. https://doi.org/10.3390/diagnostics10060400
APA StyleYang, K.-C., Liao, Y.-Y., Chang, K.-V., Huang, K.-C., & Han, D.-S. (2020). The Quantitative Skeletal Muscle Ultrasonography in Elderly with Dynapenia but Not Sarcopenia Using Texture Analysis. Diagnostics, 10(6), 400. https://doi.org/10.3390/diagnostics10060400








