Long-Term Effects of Angiotensin Receptor–Neprilysin Inhibitors on Myocardial Function in Chronic Heart Failure Patients with Reduced Ejection Fraction
Abstract
1. Introduction
2. Materials and Methods
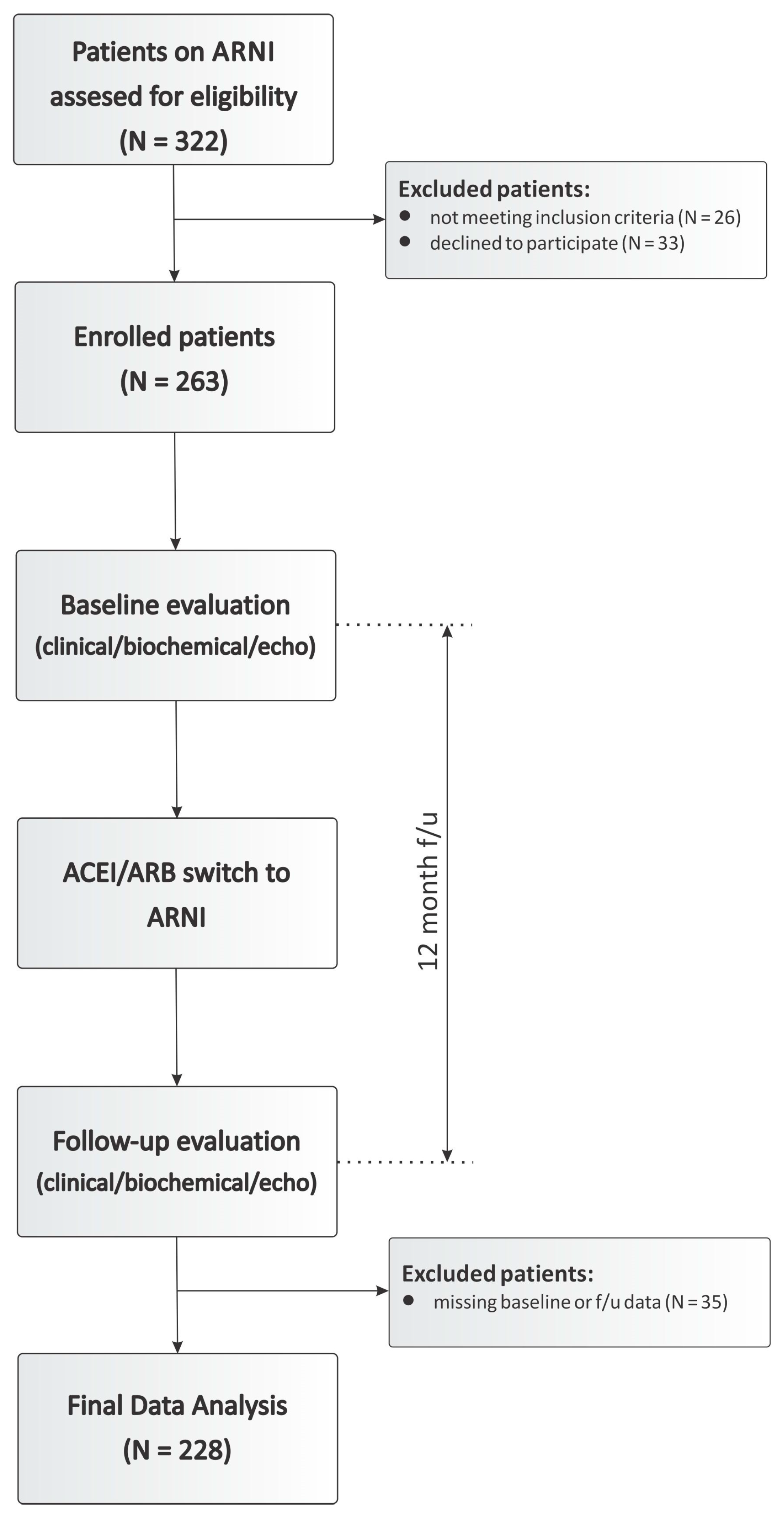
2.1. Study Population
2.2. Study Design
2.3. Laboratory Tests
2.4. NT-proBNP Measurement
2.5. Echocardiography
2.6. Study End Points
2.7. Statistical Methods and Analysis
3. Results
3.1. Patient Characteristics
3.2. Effects of ARNI on Ventricular Reverse Remodeling
3.3. The Association of Neurohumoral Modulation and Reverse Remodeling
3.4. Response to ARNI and Reverse Remodeling
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- McMurray, J.J.; Packer, M.; Desai, A.S.; Gong, J.; Lefkowitz, M.P.; Rizkala, A.R.; Rouleau, J.L.; Shi, V.C.; Solomon, S.D.; Swedberg, K.; et al. Angiotensin-Neprilysin Inhibition versus Enalapril in Heart Failure. N. Engl. J. Med. 2014, 371, 993–1004. [Google Scholar] [CrossRef] [PubMed]
- Devore, A.D.; Braunwald, E.; Morrow, D.A.; Duffy, C.I.; Ambrosy, A.P.; Chakraborty, H.; McCague, K.; Rocha, R.; Velazquez, E.J. Initiation of Angiotensin-Neprilysin Inhibition After Acute Decompensated Heart Failure: Secondary Analysis of the Open-label Extension of the PIONEER-HF Trial. JAMA Cardiol. 2020, 5, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Wachter, R.; Senni, M.; Belohlavek, J.; Straburzynska-Migaj, E.; Witte, K.K.; Kobalava, Z.; Fonseca, C.; Goncalvesova, E.; Cavusoglu, Y.; Fernandez, A.; et al. Initiation of sacubitril/valsartan in haemodynamically stabilised heart failure patients in hospital or early after discharge: Primary results of the randomised TRANSITION study. Eur. J. Heart Fail. 2019, 21, 998–1007. [Google Scholar] [CrossRef] [PubMed]
- Kramer, D.G.; Trikalinos, T.A.; Kent, D.M.; Antonopoulos, G.V.; Konstam, M.A.; Udelson, J.E. Quantitative Evaluation of Drug or Device Effects on Ventricular Remodeling as Predictors of Therapeutic Effects on Mortality in Patients With Heart Failure and Reduced Ejection Fraction. J. Am. Coll. Cardiol. 2010, 56, 392–406. [Google Scholar] [CrossRef]
- Mangiafico, S.; Costello-Boerrigter, L.C.; Andersen, I.A.; Cataliotti, A.; Burnett, J.C. Neutral endopeptidase inhibition and the natriuretic peptide system: An evolving strategy in cardiovascular therapeutics. Eur. Heart J. 2012, 34, 886–893. [Google Scholar] [CrossRef]
- Januzzi, J.L.; Prescott, M.F.; Butler, J.; Felker, G.M.; Maisel, A.S.; McCague, K.; Camacho, A.; Piña, I.L.; Rocha, R.A.; Shah, A.M.; et al. Association of Change in N-Terminal Pro-B-Type Natriuretic Peptide Following Initiation of Sacubitril-Valsartan Treatment With Cardiac Structure and Function in Patients With Heart Failure With Reduced Ejection Fraction. JAMA 2019, 322, 1–11. [Google Scholar] [CrossRef]
- Almufleh, A.; Marbach, J.; Chih, S.; Stadnick, E.; Davies, R.; Liu, P.; Mielniczuk, L. Ejection fraction improvement and reverse remodeling achieved with Sacubitril/Valsartan in heart failure with reduced ejection fraction patients. Am. J. Cardiovasc. Dis. 2017, 7, 108–113. [Google Scholar]
- Martens, P.; Beliën, H.; Dupont, M.; Vandervoort, P.; Mullens, W. The reverse remodeling response to sacubitril/valsartan therapy in heart failure with reduced ejection fraction. Cardiovasc. Ther. 2018, 36, e12435. [Google Scholar] [CrossRef]
- Bayard, G.; Da Costa, A.; Pierrard, R.; Roméyer-Bouchard, C.; Guichard, J.B.; Isaaz, K. Impact of sacubitril/valsartan on echo parameters in heart failure patients with reduced ejection fraction a prospective evaluation. IJC Heart Vasc. 2019, 25, 100418. [Google Scholar] [CrossRef]
- Raina, A.; Meeran, T. Right Ventricular Dysfunction and Its Contribution to Morbidity and Mortality in Left Ventricular Heart Failure. Curr. Heart Fail. Rep. 2018, 15, 94–105. [Google Scholar] [CrossRef]
- Elliott, P.; Andersson, B.; Arbustini, E.; Bilinska, Z.; Cecchi, F.; Charron, P.; Dubourg, O.; Kühl, U.; Maisch, B.; McKenna, W.J.; et al. Classification of the cardiomyopathies. Kardiol. Pol. 2008, 66, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. J. Heart Fail. 2016, 18, 891–975. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging. 2015, 16, 233–271. [Google Scholar] [CrossRef] [PubMed]
- The Consensus Trial Study Group. Effects of Enalapril on Mortality in Severe Congestive Heart Failure. N. Engl. J. Med. 1987, 316, 1429–1435. [Google Scholar] [CrossRef]
- SOLVD Investigators. Effect of Enalapril on Survival in Patients with Reduced Left Ventricular Ejection Fractions and Congestive Heart Failure. N. Engl. J. Med. 1991, 325, 293–302. [Google Scholar] [CrossRef]
- CIBIS-II Investigators. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): A randomised trial. Lancet 1999, 353, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Pitt, B.; Zannad, F.; Remme, W.J.; Cody, R.; Castaigne, A.; Perez, A.; Palensky, J.; Wittes, J. The Effect of Spironolactone on Morbidity and Mortality in Patients with Severe Heart Failure. N. Engl. J. Med. 1999, 341, 709–717. [Google Scholar] [CrossRef]
- Nijst, P.; Martens, P.; Mullens, W. Heart Failure with Myocardial Recovery—The Patient Whose Heart Failure Has Improved: What Next? Prog. Cardiovasc. Dis. 2017, 60, 226–236. [Google Scholar] [CrossRef]
- D’Elia, E.; Iacovoni, A.; Vaduganathan, M.; Lorini, F.L.; Perlini, S.; Senni, M. Neprilysin inhibition in heart failure: Mechanisms and substrates beyond modulating natriuretic peptides. Eur. J. Heart Fail. 2017, 19, 710–717. [Google Scholar] [CrossRef]
- Gremmler, B.; Kunert, M.; Schleiting, H.; Kisters, K.; Ulbricht, L.J. Relation between N-terminal pro-brain natriuretic peptide values and invasively measured left ventricular hemodynamic indices. Exp. Clin. Cardiol. 2003, 8, 91–94. [Google Scholar] [PubMed]
- Linde, C.; Daubert, C.; Abraham, W.T.; Sutton, M.S.J.; Ghio, S.; Hassager, C.; Herre, J.M.; Bergemann, T.; Gold, M.R. Impact of Ejection Fraction on the Clinical Response to Cardiac Resynchronization Therapy in Mild Heart Failure. Circ. Heart Fail. 2013, 6, 1180–1189. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Balmforth, C.; Simpson, J.; Shen, L.; Jhund, P.S.; Lefkowitz, M.; Rizkala, A.R.; Rouleau, J.L.; Shi, V.; Solomon, S.D.; Swedberg, K.; et al. Outcomes and Effect of Treatment According to Etiology in HFrEF. JACC Heart Fail. 2019, 7, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Cicoira, M.; Zanolla, L.; Rossi, A.; Golia, G.; Franceschini, L.; Brighetti, G.; Marino, P.; Zardini, P. Long-term, dose-dependent effects of spironolactone on left ventricular function and exercise tolerance in patients with chronic heart failure. J. Am. Coll. Cardiol. 2002, 40, 304–310. [Google Scholar] [CrossRef]


| Variable | Baseline (N = 228) | Follow-Up (N = 228) | p |
|---|---|---|---|
| Age, y | 57 ± 11 | / | |
| Male gender (%) | 189 (83) | / | |
| Ischemic heart failure (%) | 82 (36) | / | |
| Sodium, mmol/L | 140 ± 2 | 141 ± 3 | 0.78 |
| Potassium, mmol/L | 4.7 ± 0.5 | 4.8 ± 0.4 | 0.45 |
| Creatinine, µmol/L | 95 ± 34 | 97 ± 38 | 0.48 |
| Bilirubin, µmol/L | 17 ± 13 | 16 ± 10 | 0.28 |
| NT-proBNP, pg/mL (IQR) | 1324 (605, 3281) | 792 (329, 2022) | 0.001 |
| Comorbidities | |||
| Hypertension (%) | 123 (54) | / | |
| Diabetes (%) | 52 (23) | / | |
| Hyperlipidemia (%) | 129 (57) | / | |
| Chronic kidney disease (%) | 56 (24) | / | |
| Atrial fibrillation (%) | 67 (29) | / | |
| Baseline medical therapy | |||
| ACEI/ARB (%) | 228 (100) | 0 | / |
| % of target dose | 70 | 0 | / |
| ARNI (%) | 0 | 228 (100) | / |
| % of target dose | 0 | 69 | / |
| Beta blockers (%) | 228 (100) | 228 (100) | / |
| % of target dose | 63 | 63 | / |
| MRA (%) | 157 (69) | 157 (69) | / |
| % of target dose | 100 | 100 | / |
| Digoxin (%) | 23 (10) | 27 (12) | 0.58 |
| ICD/CRT (%) | 64 (28) | 64 (28) | / |
| Variable | Group A (N = 102) | Group B (N = 126) | p |
|---|---|---|---|
| Age, y | 60 ± 10 | 55 ± 11 | 0.005 |
| Male gender (%) | 84 (82) | 106 (84) | 0.97 |
| Ischemic heart failure (%) | 49 (48) | 35 (28) | 0.002 |
| Creatinine, µmol/L | 100 ± 39 | 95 ± 37 | 0.39 |
| Bilirubin, µmol/L | 16 ± 8 | 15 ± 12 | 0.74 |
| NT-proBNP, pg/mL (IQR) | 1612 (709, 3573) | 1112 (513, 3027) | 0.03 |
| LVEF (%) | 33 ± 7 | 27 ± 8 | <0.001 |
| LVEDD, cm | 6.5 ± 0.9 | 6.5 ± 0.7 | 0.75 |
| TAPSE, cm | 1.7 ± 0.5 | 1.7 ± 0.4 | 0.78 |
| Comorbidities | |||
| Hypertension (%) | 59 (58) | 63 (50) | 0.20 |
| Diabetes (%) | 27 (26) | 26 (21) | 0.41 |
| Hyperlipidemia (%) | 62 (61) | 67 (53) | 0.19 |
| Chronic kidney disease (%) | 24 (23) | 32 (25) | 0.89 |
| Atrial fibrillation (%) | 32 (31) | 35 (28) | 0.76 |
| Baseline medical therapy | |||
| ACEI/ARB (%) | 102 (100) | 126 (100) | / |
| Beta blockers (%) | 102 (100) | 126 (100) | / |
| MRA (%) | 85 (83) | 93 (74) | 0.86 |
| Digoxin (%) | 12 (12) | 11 (9) | 0.53 |
| ICD/CRT (%) | 34 (33) | 29 (23) | 0.10 |
| ARNI dose | |||
| Low dose (%) | 22 (22) | 15 (12) | 0.03 |
| Intermediate dose (%) | 39 (38) | 49 (39) | 0.94 |
| High dose (%) | 41 (40) | 62 (49) | 0.47 |
| Variable | B | p | 95% Confidence Interval | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| Age > 60 years | −0.129 | 0.713 | 0.443 | 1.745 |
| Ischemic heart failure | −0.699 | 0.044 | 0.252 | 0.981 |
| LVEF > 30% | −1.711 | 0.001 | 0.087 | 0.374 |
| NT-proBNP > 1500 pg/mL | −0.813 | 0.035 | 0.208 | 0.945 |
| Low-dose ARNI therapy | −0.588 | 0.232 | 0.212 | 1.456 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poglajen, G.; Anžič-Drofenik, A.; Zemljič, G.; Frljak, S.; Cerar, A.; Okrajšek, R.; Šebeštjen, M.; Vrtovec, B. Long-Term Effects of Angiotensin Receptor–Neprilysin Inhibitors on Myocardial Function in Chronic Heart Failure Patients with Reduced Ejection Fraction. Diagnostics 2020, 10, 522. https://doi.org/10.3390/diagnostics10080522
Poglajen G, Anžič-Drofenik A, Zemljič G, Frljak S, Cerar A, Okrajšek R, Šebeštjen M, Vrtovec B. Long-Term Effects of Angiotensin Receptor–Neprilysin Inhibitors on Myocardial Function in Chronic Heart Failure Patients with Reduced Ejection Fraction. Diagnostics. 2020; 10(8):522. https://doi.org/10.3390/diagnostics10080522
Chicago/Turabian StylePoglajen, Gregor, Ajda Anžič-Drofenik, Gregor Zemljič, Sabina Frljak, Andraž Cerar, Renata Okrajšek, Miran Šebeštjen, and Bojan Vrtovec. 2020. "Long-Term Effects of Angiotensin Receptor–Neprilysin Inhibitors on Myocardial Function in Chronic Heart Failure Patients with Reduced Ejection Fraction" Diagnostics 10, no. 8: 522. https://doi.org/10.3390/diagnostics10080522
APA StylePoglajen, G., Anžič-Drofenik, A., Zemljič, G., Frljak, S., Cerar, A., Okrajšek, R., Šebeštjen, M., & Vrtovec, B. (2020). Long-Term Effects of Angiotensin Receptor–Neprilysin Inhibitors on Myocardial Function in Chronic Heart Failure Patients with Reduced Ejection Fraction. Diagnostics, 10(8), 522. https://doi.org/10.3390/diagnostics10080522





