Aldosterone-Mediated Sodium Retention Is Reflected by the Serum Sodium to Urinary Sodium to (Serum Potassium)2 to Urinary Potassium (SUSPPUP) Index
Abstract
:1. Introduction
2. Patients and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| MDPI | Multidisciplinary Digital Publishing Institute |
| DOAJ | Directory of open access journals |
| TLA | Three letter acronym |
| LD | linear dichroism |
References
- Willenberg, H.S.; Schinner, S.; Ansurudeen, I. New mechanisms to control aldosterone synthesis. Horm. Metab. Res. 2008, 40, 435–441. [Google Scholar] [CrossRef]
- Choi, M.; Scholl, U.I.; Yue, P.; Björklund, P.; Zhao, B.; Nelson-Williams, C.; Ji, W.; Cho, Y.; Patel, A.; Men, C.J.; et al. K+ channel mutations in adrenal aldosterone–producing adenomas and hereditary hypertension. Science 2011, 331, 768–772. [Google Scholar] [CrossRef] [Green Version]
- Boulkroun, S.; Beuschlein, F.; Rossi, G.P.; Golib-Dzib, J.F.; Fischer, E.; Amar, L.; Mulatero, P.; Samson-Couterie, B.; Hahner, S.; Quinkler, M.; et al. Prevalence, clinical, and molecular correlates of KCNJ5 mutations in primary aldosteronism. Hypertension 2012, 59, 592–598. [Google Scholar] [CrossRef] [Green Version]
- Charmandari, E.; Sertedaki, A.; Kino, T.; Merakou, C.; Hoffman, D.A.; Hatch, M.M.; Hurt, D.E.; Lin, L.; Xekouki, P.; Stratakis, C.A.; et al. A novel point mutation in the KCNJ5 gene causing primary hyperaldosteronism and early-onset autosomal dominant hypertension. J. Clin. Endocrinol. Metab. 2012, 97, 1532–1539. [Google Scholar] [CrossRef] [Green Version]
- Azizan, E.A.; Murthy, M.; Stowasser, M.; Gordon, R.; Kowalski, B.; Xu, S.; Brown, M.J.; O’Shaughnessy, K.M. Somatic mutations affecting the selectivity filter of KCNJ5 are frequent in 2 large unselected collections of adrenal aldosteronomas. Hypertension 2012, 59, 587–591. [Google Scholar] [CrossRef]
- Xekouki, P.; Hatch, M.M.; Lin, L.; de Rodrigo, A.; Azevedo, M.; de la Luz Sierra, M.; Levy, I.; Saloustros, E.; Moraitis, A.; Horvath, A.; et al. KCNJ5 mutations in the National Institutes of Health cohort of patients with primary hyperaldosteronism: An infrequent genetic cause of Conn’s syndrome. Endocr. Relat. Cancer. 2012, 19, 255–260. [Google Scholar] [CrossRef] [Green Version]
- Åkerström, T.; Crona, J.; Delgado Verdugo, A.; Starker, L.F.; Cupisti, K.; Willenberg, H.S.; Knoefel, W.T.; Saeger, W.; Feller, A.; Ip, J.; et al. Comprehensive re-sequencing of adrenal aldosterone producing lesions reveal three somatic mutations near the KCNJ5 potassium channel selectivity filter. PLoS ONE 2012, 7, e41926. [Google Scholar]
- Scholl, U.I.; Stölting, G.; Schewe, J.; Thiel, A.; Tan, H.; Nelson-Williams, C.; Vichot, A.A.; Jin, S.C.; Loring, E.; Untiet, V.; et al. CLCN2 chloride channel mutations in familial hyperaldosteronism type II. Nat. Genet. 2018, 50, 349–354. [Google Scholar] [CrossRef]
- Willenberg, H.S. How to escape from primary aldosteronism? News and views on an adrenal disorder of salt retention. Horm. Metab. Res. 2017, 49, 151–163. [Google Scholar] [CrossRef]
- Conn, J.W.; Part, I. Painting background. Part II. Primary aldosteronism, a new clinical syndrome. 1954. J. Lab. Clin. Med. 1990, 116, 253–267. [Google Scholar]
- Willenberg, H.S.; Kolentini, C.; Quinkler, M.; Cupisti, K.; Krausch, M.; Schott, M.; Scherbaum, W.A. The serum sodium to urinary sodium to (serum potassium)2 to urinary potassium (SUSPPUP) ratio in patients with primary aldosteronism. Eur. J. Clin. Invest. 2009, 39, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Balaş, M.; Zosin, I.; Maser-Gluth, C.; Hermsen, D.; Cupisti, K.; Schott, M.; Schinner, S.; Knoefel, W.T.; Scherbaum, W.A.; Willenberg, H.S. Indicators of mineralocorticoid excess in the evaluation of primary aldosteronism. Hypertens. Res. 2010, 33, 850–856. [Google Scholar] [CrossRef] [PubMed]
- Steichen, O.; Blanchard, A.; Plouin, P.F. Assessment of serum sodium to urinary sodium divided by (serum potassium)2 to urinary potassium as a screening tool for primary aldosteronism. Eur. J. Clin. Invest. 2011, 41, 189–194. [Google Scholar] [CrossRef]
- Funder, J.W.; Carey, R.M.; Fardella, C.; Gomez-Sanchez, C.E.; Mantero, F.; Stowasser, M.; Young, W.F., Jr.; Montori, V.M. Endocrine Society. Case detection, diagnosis and treatment of patients with primary aldosteronism: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2008, 93, 3266–3281. [Google Scholar] [CrossRef] [Green Version]
- Willenberg, H.S.; Vonend, O.; Schott, M.; Gao, X.; Blondin, D.; Saleh, A.; Rump, L.C.; Scherbaum, W.A. Comparison of the saline infusion test and the fludrocortisone suppression test in the diagnosis of primary aldosteronism. Horm. Metab. Res. 2012, 44, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Kardalas, E.; Paschou, S.A.; Anagnostis, P.; Muscogiuri, G.; Siasos, G.; Vryonidou, A. Hypokalemia: A clinical update. Endocr. Connect. 2018, 7, R135–R146. [Google Scholar] [CrossRef] [PubMed]
- Funder, J.W.; Carey, R.M.; Mantero, F.; Murad, M.H.; Reincke, M.; Shibata, H.; Stowasser, M.; Young, W.F., Jr. The Management of Primary Aldosteronism: Case detection, diagnosis, and treatment: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2016, 101, 1889–1916. [Google Scholar] [CrossRef]
- Schirpenbach, C.; Reincke, M. Primary aldosteronism: Current knowledge and controversies in Conn’s syndrome. Nat. Clin. Pract. Endocrinol. Metab. 2007, 3, 220–227. [Google Scholar] [CrossRef]
- Morimoto, R.; Omata, K.; Ito, S.; Satoh, F. Progress in the Management of Primary Aldosteronism. Am. J. Hypertens. 2018, 31, 522–531. [Google Scholar] [CrossRef] [Green Version]
- Farrugia, F.A.; Zavras, N.; Martikos, G.; Tzanetis, P.; Charalampopoulos, A.; Misiakos, E.P.; Sotiropoulos, D.; Koliakos, N. A short review of primary aldosteronism in question and answer fashion. Endocr. Regul. 2018, 52, 27–40. [Google Scholar] [CrossRef] [Green Version]
- Williams, B.; MacDonald, T.M.; Morant, S.V.; Webb, D.J.; Sever, P.; McInnes, G.T.; Ford, I.; Cruickshank, J.K.; Caulfield, M.J.; Padmanabhan, S.; et al. British Hypertension Society programme of Prevention and Treatment of Hypertension with Algorithm based Therapy (PATHWAY) Study Group. Endocrine and haemodynamic changes in resistant hypertension and blood pressure responses to spironolactone or amiloride: The PATHWAY-2 mechanisms substudies. Lancet Diabetes Endo. 2018, 6, 464–475. [Google Scholar]
- Appel, L.J.; Anderson, C.A.M. Compelling evidence for public health action to reduce salt intake. N. Engl. J. Med. 2010, 362, 650–652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, Q.; Liu, T.; Kuklina, E.V.; Flanders, W.D.; Hong, Y.; Gillespie, C.; Chang, M.H.; Gwinn, M.; Dowling, N.; Khoury, M.J.; et al. Sodium and potassium intake and mortality among US adults: Prospective data from the Third National Health and Nutrition Examination Survey. Arch. Intern. Med. 2011, 171, 1183–1191. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Parameter | PA | EH | AI | REF |
|---|---|---|---|---|
| number, n | 69 | 102 | 26 | 28 |
| mean age [years] | 53.8 | 53.9 | 51.5 | 40.9 |
| females, n | 35 (50.7%)2 | 69 (67.6%) | 20 (76.9%) | 21 (75.0%) |
| SBP [mmHg] | 155.9 ± 20.7 | 150.1 ± 19.1 | 125.5 ± 22.4 | 131.9 ± 19.3 |
| DBP [mmHg] | 89.8 ± 12.5 | 89.0 ± 10.2 | 76.6 ± 13.4 | 79.9 ± 11.4 |
| Parameter | PA | EH | REF | AI |
|---|---|---|---|---|
| NaS [mmol/L] | 143.0 (142.0–144.2) | 142.0 (140.0–143.0) | 140.0 (140.0–142.0) | 142 (139.0–143.0) |
| NaU [mmol/L] | 88.0 ± 51.2 | 128.5 (83.0–168.0) | 145.1 ± 68.4 | 125 (83.0–158.0) |
| KS [mmol/L] | 3.6 (3.3–3.9) | 4.3 ± 0.4 | 4.3 (4.2–4.4) | 4.3 ± 0.4 |
| KU [mmol/L] | 56.1 ± 25.6 | 48.0 (37.0–73.0) | 55.0 (44.0–75.0) | 50.7 ± 24.3 |
| SUSPPUP [L/mmol] | 7.4 (4.2–12.3) | 3.2 (2.3–4.3) | 3.4 ± 1.4 | 2.9 ± 1.2 |
| aldosterone [ng/L] | 161.0 (108.5–252.7) | 64.0 (40.0–106.0) | 57.0 (33.0–94.0) | 11.0 (11.0–28.0) |
| renin [ng/L] | 1.9 (1.2–4.2) | 8.9 (2.8–26.0) | 5.8 (3.6–12.5) | 114 ± 391.0 |
| ARR [ng/L: ng/L] | 71.7 (40.2–132.7) | 9.1 (2.1–23.6) | 7.5 (4.1–20.0) | 1.9 (0.3–4.1) |
| ARR×SUSPPUP [L/mmol] | 495.5 (232.9–1131.8) | 28.8 (5.8–84.5) | 23.3 (12.3–46.0) | 3.4 (1.3–11.5) |
| Parameter | PA vs. EH | PA vs. REF | PA vs. AI | EH vs. REF | EH vs. AI | REF vs. AI |
|---|---|---|---|---|---|---|
| KS | p < 0.0001 | p < 0.0001 | p < 0.0001 | n.s. | n.s. | n.s. |
| NaS | p < 0.0001 | p < 0.0001 | p < 0.0001 | n.s. | n.s. | n.s. |
| NaU | p < 0.0001 | p < 0.0001 | p < 0.0001 | n.s. | n.s. | n.s. |
| aldosterone | p < 0.0001 | p < 0.0001 | p < 0.0001 | n.s. | p < 0.0001 | p < 0.0001 |
| renin | p < 0.0001 | p < 0.0001 | p < 0.0001 | n.s. | n.s. | n.s. |
| SUSPPUP | p < 0.0001 | p < 0.0001 | p < 0.0001 | n.s. | n.s. | n.s. |
| ARR | p < 0.0001 | p < 0.0001 | p < 0.0001 | n.s. | p < 0.0001 | p < 0.0001 |
| ARR×SUSPPUP | p < 0.0001 | p < 0.0001 | p < 0.0001 | n.s. | p < 0.0001 | p < 0.0001 |
| Parameter | AUC | Optimal Cut-Off | Sensitivity [%] | Specificity [%] | PPV [%] | NPV [%] |
|---|---|---|---|---|---|---|
| ARR | 0.910 | 28.2 | 87.0 | 81.4 | 75.9 | 90.2 |
| KS | 0.891 | 3.9 | 79.7 | 85.3 | 78.3 | 85.3 |
| SUSPPUP | 0.835 | 5.25 | 69.6 | 87.2 | 78.7 | 80.9 |
| ARR×SUSPPUP | 0.942 | 110.3 | 92.7 | 81.4 | 77.1 | 94.3 |
| Parameter | Systolic BP [mmHg] | Diastolic BP [mmHg] | Serum Potassium [mmol/L] | ARR | SUSPPUP [L/mmol] | ARR×SUSPPUP [L/mmol] |
|---|---|---|---|---|---|---|
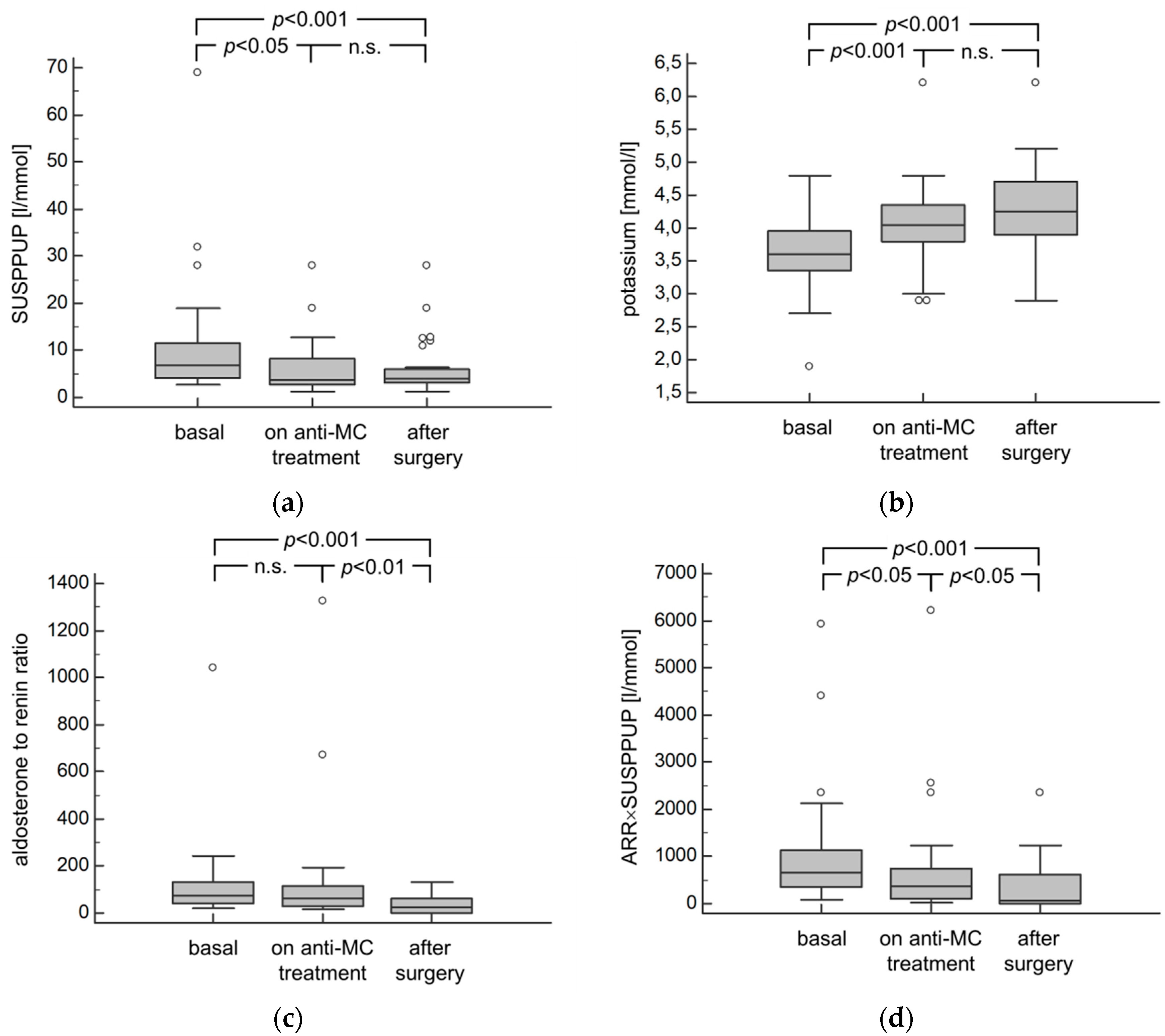
| baseline | 154.9 ± 43.5 | 91.1 ± 13.4 | 3.6 ± 0.6 | 74 (42.2–136.5) | 7.2 (4.9–12.2) | 718 (380–1121) |
| after surgery | 143.3 ± 19.1 | 87.0 ± 12.7 | 4.2 ± 0.7 | 23 (2.0–63.0) | 3.9 (3.0–6.0) | 46 (6–567) |
| correlation | r = 0.56 (p = 0.01) | r = 0.83 (p < 0.001) | r = 0.27 (n.s.) | r = 0.03 (n.s.) | r = 0.37 (n.s.) | r = 0.05 (n.s.) |
| significance of change | p < 0.05 | p < 0.05 | p < 0.001 | p = 0.001 | p = 0.001 | p < 0.001 |
| Medication | KS w [mmol/L] | KS w/o [mmol/L] | ARR w | ARR w/o | SUSPPUP w [L/mmol] | SUSPPUP w/o [L/mmol] | ARR×SUSPPUP w [L/mmol] | ARR×SUSPPUP w/o [L/mmol] | |
|---|---|---|---|---|---|---|---|---|---|
| BBL | in PA | 3.5 ± 0.5 | 3.6 ± 0.5 | 65.2 (40.0–129.6) | 76.1 (41.6–136.6) | 7.30 (4.2–12.1) | 8.2 (4.0–13.6) | 495 (228–1090) | 498 (257–1499) |
| in EH | 4.3 (4.1–4.6) | 4.3 ± 0.3 | 8.5 (2.4–21.7) | 10.0 (1.8–23.9) | 3.3 (2.4–4.7) | 2.9 (2.3–4.3) | 30 (8–104) | 28 (5–73) | |
| ACEI | in PA | 3.5 ± 0.6 | 3.6 ± 0.5 | 62.8 (34.4–78.2) | 81.8 (42.3–164.6) | 8.9 (3.9–15.5) | 7.3 (4.3–11.2) | 440 (235–1112) | 503 (228–1717) |
| in EH | 4.2 (4.0–4.6) | 4.3 ± 0.4 | 1.3 (0.7–9.0) | 12.2 (6.2–26.3) | 3.2 (2.3–4.0) | 3.2 (2.3–4.5) | 5 (1–26) | 46 (18–226) | |
| ARB | in PA | 3.5 ± 0.6 | 3.6 (3.3–3.9) | 74.0 (44.1–148.2) | 71.1 (40.1–129.4) | 7.3 (5.4–13.3) | 7.4 (4.0–12.4) | 495 (312–1637) | 498 (196–1084) |
| in EH | 4.3 ± 0.6 | 4.3 ± 0.3 | 22.1 (7.3–61.6) | 8.5 (1.8–20.1) | 3.5 (2.3–4.4) | 2.9 (2.1–3.4) | 52 (13–167) | 21.4 (6–73) | |
| diuretics | in PA | 3.5 ± 0.6 | 3.6 (3.5–3.9) | 67.8 (36.6–161.2) | 74.0 (42.1–113.2) | 8.2 (4.8–12.7) | 7.3 (3.9–12.7) | 510 (228–1951) | 485 (266–1066) |
| in EH | 4.1 ± 0.5 | 4.4 ± 0.3 | 5.7 (1.5–29.2) | 9.6 (2.2–22.1) | 3.1 (2.4–3.8) | 3.2 (2.3–4.5) | 20 (5–100) | 30 (9–194) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanaan, E.; Haase, M.; Vonend, O.; Reincke, M.; Schott, M.; Willenberg, H.S. Aldosterone-Mediated Sodium Retention Is Reflected by the Serum Sodium to Urinary Sodium to (Serum Potassium)2 to Urinary Potassium (SUSPPUP) Index. Diagnostics 2020, 10, 545. https://doi.org/10.3390/diagnostics10080545
Kanaan E, Haase M, Vonend O, Reincke M, Schott M, Willenberg HS. Aldosterone-Mediated Sodium Retention Is Reflected by the Serum Sodium to Urinary Sodium to (Serum Potassium)2 to Urinary Potassium (SUSPPUP) Index. Diagnostics. 2020; 10(8):545. https://doi.org/10.3390/diagnostics10080545
Chicago/Turabian StyleKanaan, Evelien, Matthias Haase, Oliver Vonend, Martin Reincke, Matthias Schott, and Holger S. Willenberg. 2020. "Aldosterone-Mediated Sodium Retention Is Reflected by the Serum Sodium to Urinary Sodium to (Serum Potassium)2 to Urinary Potassium (SUSPPUP) Index" Diagnostics 10, no. 8: 545. https://doi.org/10.3390/diagnostics10080545
APA StyleKanaan, E., Haase, M., Vonend, O., Reincke, M., Schott, M., & Willenberg, H. S. (2020). Aldosterone-Mediated Sodium Retention Is Reflected by the Serum Sodium to Urinary Sodium to (Serum Potassium)2 to Urinary Potassium (SUSPPUP) Index. Diagnostics, 10(8), 545. https://doi.org/10.3390/diagnostics10080545





