A Comparison of a Standard Macintosh Blade Laryngoscope, Pentax-AWS Videolaryngoscope and Intubrite Videolaryngoscope for Tracheal Intubation in Manikins in Sitting and Prone Positions: A Randomized Cross-Over Study
Abstract
:1. Introduction
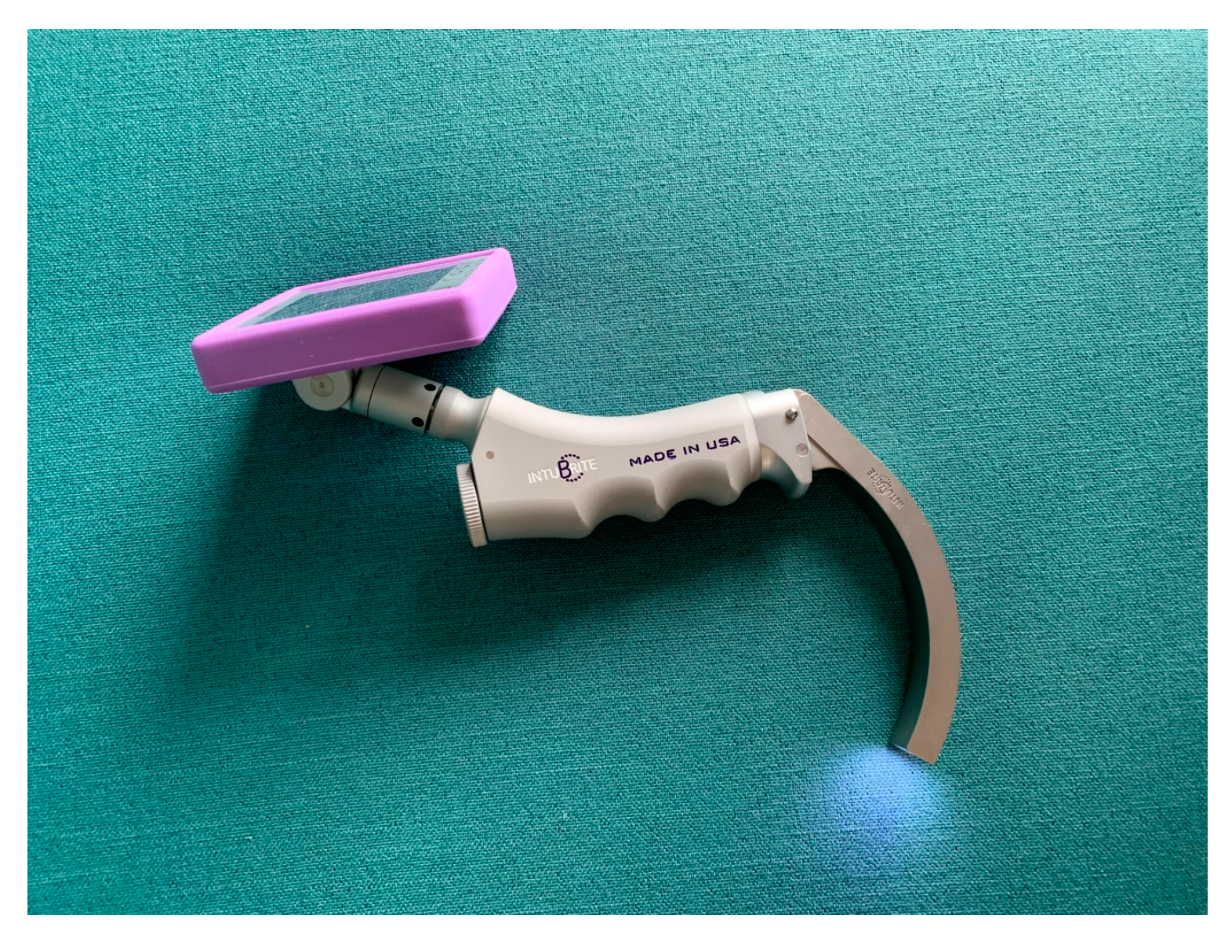
2. Materials and Methods
3. Results
4. Discussion
4.1. Significance of the Study Results
4.2. Comparison with Other Published Studies on This Topic-Similarities and Differences
4.3. Limitations of the Study
- This is the first study that compares two types of videolaryngoscopes, channeled and non-channeled, in relation to the effectiveness and possible complications of tracheal intubation in specific patient positioning in both the sitting and prone positions.
- New techniques and devices for airway management should be tested for possible application in very difficult airway scenarios (e.g., in entrapped patients or for intubation in patients requiring prone position such as for spinal neurosurgery procedures). This study provides answers on the efficacy of the evaluated videolaryngoscopes in such situations.
- Although main limitation of this study is that it was a manikin study, the human study can be performed as a follow up of this study, taking into consideration the important results of this work.
4.4. Potential Implications for Future Research
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ellard, L.; Wong, D.T. Should we induce general anesthesia in the prone position? Curr. Opin. Anaesthesiol. 2014, 27, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Gaszynski, T. Algorithm for management of sudden unexpected extubation in patient positioned in prone position. Anaesthesiol. Intensive Ther. 2020, 52, 2. [Google Scholar] [CrossRef] [PubMed]
- Chui, J.; Craen, R.A. An update on the prone position: Continuing Professional Development. Can. J. Anesth. 2016, 63, 737–767. [Google Scholar] [CrossRef] [PubMed]
- Lopez, A.M.; Valero, R.; Hurtado, P.; Gambs, P.; Pons, M.; Anglada, T. Comparison of the LMA Supreme™ with the LMA Proseal™ for airway management in patients anaesthetized in prone position. Br. J. Anaesth. 2011, 107, 265–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Cosmo, G.; Congedo, E. Unintentional tracheal extubation during prone position: What is the best rescue airway device? J. Emerg. Trauma Shock 2017, 10, 2–3. [Google Scholar] [CrossRef]
- Timmermann, A.; Eich, C.; Russo, S.; Natge, U.; Brauer, A.; Rosenblatt, W.H.; Braun, U. Prehospital airway management: A prospective evaluation of anaesthesia trained emergency physicians. Resuscitation 2006, 70, 179–185. [Google Scholar] [CrossRef]
- Gaszynski, T. Airway Management for General Anesthesia in Patients With Rheumatic Diseases—New Possibilities. Reumatologia 2019, 57, 69–71. [Google Scholar] [CrossRef]
- Andjelic, S. Face-to-face intubation in traumatised patients. Anestezjol. Ratow. 2009, 3, 193–197. [Google Scholar]
- Van Zundert, T.C.; Van Zundert, A.A. Tracheal intubation of patients in non-standard positions requires training. Minerva Anestesiol. 2013, 79, 679–682. [Google Scholar]
- Asai, T. Pentax-AWS and Macintosh laryngoscope in restricted access. Anaesthesia 2009, 64, 1114–1117. [Google Scholar] [CrossRef]
- Sadamori, T.; Kusunoki, S.; Otani, T.; Ishida, M.; Masuda, R.; Tamura, T.; Takeda, T.; Tsumura, R.; Shokawa, T.; Kondo, T.; et al. Airway Scope for emergency intubations: Usefulness of a new video-laryngoscope. Hiroshima J. Med. Sci. 2008, 57, 99–104. [Google Scholar]
- Gaszynski, T. Forces applied by the laryngoscope blade onto the tongue during intubation attempts: A comparison between Mackintosh, AirTraq and Pentax AWS in a mannequin study. Eur. J. Anaesthesiol. 2011, 28, 463–464. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, T.; Shiga, T.; Homma, Y.; Koyama, Y.; Goto, T. Comparison of the force applied on oral structures during intubation attempts by novice physicians between the Macintosh direct laryngoscope, Airway Scope and C-MAC PM: A high-fidelity simulator-based study. BMJ Open 2016, 23, e011039. [Google Scholar] [CrossRef] [PubMed]
- Gaszynski, T.; Aleksandrowicz, D. Evaluation of pressure on tongue during intubation efforts. Trends in Anaesth. Crit. Care 2017, 12, 20. [Google Scholar] [CrossRef]
- Ong, J.R.; Chong, C.F.; Chen, C.C.; Wang, T.L.; Lin, C.M.; Chang, S.C. Comparing the performance of traditional direct laryngoscope with three indirect laryngoscopes: A prospective manikin study in normal and difficult airway scenarios. Emerg. Med. Australas. 2011, 23, 606–614. [Google Scholar] [CrossRef] [PubMed]
- Varney, S.M.; Dooley, M.; Bebarta, V.S. Faster intubation with direct laryngoscopy vs handheld videoscope in uncomplicated manikin airways. Am. J. Emerg. Med. 2009, 27, 259–261. [Google Scholar] [CrossRef]
- Komasawa, N.; Ueki, R.; Itani, M.; Nomura, H.; Nishi, S.I.; Kaminoh, Y. Evaluation of tracheal intubation in several positions by the Pentax-AWS Airway Scope: A manikin study. J. Anesth. 2010, 24, 908–912. [Google Scholar] [CrossRef]
- Samantaray, A. Tracheal intubation in the prone position with an intubating laryngeal mask airway following posterior spine impaled knife injury. Saudi J. Anaesth. 2011, 5, 329–331. [Google Scholar] [CrossRef]
- Baer, K.; Nyström, B. Routine intubation in the prone position. Upsala J. Med. Sci. 2012, 117, 411–414. [Google Scholar] [CrossRef]
- Douglass, J.; Frase, J.; Andrzejowski, J. Awake intubation and awake prone positioning of a morbidly obese patient for lumbar spine surgery. Anaesthesia 2014, 69, 166–169. [Google Scholar] [CrossRef]
- Suzuki, H.; Nakajima, W.; Aoyagi, M.; Takahashi, M.; Kuzuta, T.; Osaki, M. [A case of endotracheal intubation in prone position utilizing PENTAX-Airwayscope for morbidly obese patient]. Masui. Jpn. J. Anesthesiol. 2012, 61, 384–386. [Google Scholar]
- Suzuki, A.; Terao, M.; Aizawa, K.; Sasakawa, T.; Henderson, J.J.; Iwasaki, H. Pentax-AWS airway Scope as an alternative for awake flexible fiberoptic intubation of a morbidly obese patient in the semi-sitting position. J. Anesth. 2009, 23, 162–163. [Google Scholar] [CrossRef] [PubMed]
- Vermelis, A.M.; Mateijsen, N.; Giebelen, D.; Meeusen, V.; Wong, D.T.; Van Zundert, A.A. Successful use of videolaryngoscopy in an adult patient with acute epiglottitis: A case report. Acta Anaesthesiol. Belg. 2010, 61, 67–70. [Google Scholar] [PubMed]
- Kranke, P. Penny wise, pound foolish. Trade-offs when using the laryngeal mask airway for spine surgery in the prone position. Eur. J. Anaesthesiol. 2014, 31, 249–252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hinkelbein, J. PRO: Laryngeal mask can be used for surgery in the prone position. Eur. J. Anaesthesiol. 2014, 31, 253–255. [Google Scholar] [CrossRef]
- Staender, S. CON: Laryngeal mask must not be used for surgery in the prone position. Eur. J. Anaesthesiol. 2014, 31, 256–258. [Google Scholar] [CrossRef]
- Olsen, K.S.; Petersen, J.T.; Pedersen, N.A.; Rovsing, L. Self-positioning followed by induction of anesthesia and insertion of laryngeal mask airway versus endotracheal intubation and subsequent positioning in the prone position. Eur. J. Anaesthesiol. 2014, 31, 259–265. [Google Scholar] [CrossRef] [Green Version]
- Brimacombe, J.R.; Wenzel, V.; Keller, C. The ProSeal laryngeal mask airway in prone position: A retrospective audit of 245 patients. Anaesth. Intensive Care 2007, 35, 222–225. [Google Scholar] [CrossRef] [Green Version]
- Sharma, V.; Verghese, C.; McKenna, P.J. Prospective audit on the use of the LMA-Supreme for airway management of adult patients undergoing elective orthopaedic surgery in prone position. Br. J. Anaesthesiol. 2010, 105, 228–232. [Google Scholar] [CrossRef] [Green Version]
- Taxas, S.; Gopinath, A. Laryngeal mask airway classic as a rescue device after accidental extubation in a neonate in prone position. Indian J. Anaesth. 2011, 55, 542. [Google Scholar]
- Raphael, J.; Rosenthal-Ganon, T.; Gozal, Y. Emergency airway management with laryngeal mask airway in patient placed in prone position. J. Clin. Anaesth. 2004, 16, 560–561. [Google Scholar] [CrossRef] [PubMed]
- Dingeman, R.S.; Goumnerrova, L.C.; Goobie, S.M. The use of a laryngeal mask airway for emergency airway in a prone position child. Anesth. Analg. 2005, 100, 670–671. [Google Scholar] [CrossRef] [PubMed]
- Abrishami, A.; Zilberman, P.; Chung, F. Brief report: Airway rescue with insertion of laryngeal mask airway devices with patients in the prone position. Can. J. Anaesth. 2010, 57, 1014–1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Zudert, A.; Kuczkowski, K.M.; Tijssen, F.; Weber, E. Direct laryngoscopy and endotracheal intubation in the prone position following traumatic thoracic spine injury. J. Anesth. 2008, 22, 170–172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaszynski, T. Intubation in prone position using AirTraq Avant videolaryngoscope. J. Clin. Monit. Comput. 2019, 33, 173–174. [Google Scholar] [CrossRef]
- Gaszynski, T. Local anaesthesia for ‘awake intubation’ using the TruView PCD video laryngoscope. Anaesthesiol. Intensive Ther. 2014, 46, 210–211. [Google Scholar]
- Gaszynski, T. Comparison of the C-Mac video laryngoscope with the McGrath Series 5 video laryngoscope concerning an extremely difficult airway. Anaesthesiol. Intensive Ther. 2016, 48, 55–57. [Google Scholar] [CrossRef] [Green Version]
- Hsieh, P.S.; Ma, H.P.; Wong, C.S.; Ong, J.R. Emergency tracheal intubation in an ankylosing spondylitis patient in a sitting position using an airway scope combined with face-to-face and digital intubation. J. Emerg. Med. 2018, 54, 674–677. [Google Scholar] [CrossRef]
- Oshika, H.; Koyama, Y.; Taguri, M.; Maruyama, K.; Hirabayashi, G.; Yamada, S.M.; Kohno, M.; Andoh, T. Supraglottic airway device versus a channeled or non-channeled blade-type videolaryngoscope for accidental extubation in the prone position: A randomized crossover manikin study. Medicine 2018, 97, e11190. [Google Scholar] [CrossRef]






| Gender | Experience Distribution | Estimated Number of Annual ETI Experience |
|---|---|---|
| 7 female/4 male | Mean 4 years (6 months–6 years) | 892 ± 78 |
| Scenario | Laryngoscope | Min. | Max. | Mean | SD | p Value |
|---|---|---|---|---|---|---|
| Supine | MCL | 6 | 70 | 13 | 18.93 | - |
| Pentax-AWS | 3 | 40 | 12 | 10.98 | 0.2765 * | |
| Intubrite | 7 | 24 | 12 | 5.75 | 0.2011 * | |
| Prone | MCL | 12 | 58 | 35 | 16.58 | - |
| Pentax-AWS | 5 | 82 | 12 | 22.13 | 0.0422 * | |
| Intubrite | 8 | 63 | 24 | 17.45 | 0.1365 * | |
| Sitting position | MCL | 13 | 57 | 17 | 17.33 | - |
| Pentax-AWS | 6 | 54 | 15 | 15.9 | 0.1708 * | |
| Intubrite | 7 | 41 | 17 | 11.32 | 0.0900 * |
| Scenario | Laryngoscope | Min. | Max. | Mean | SD | p Value |
|---|---|---|---|---|---|---|
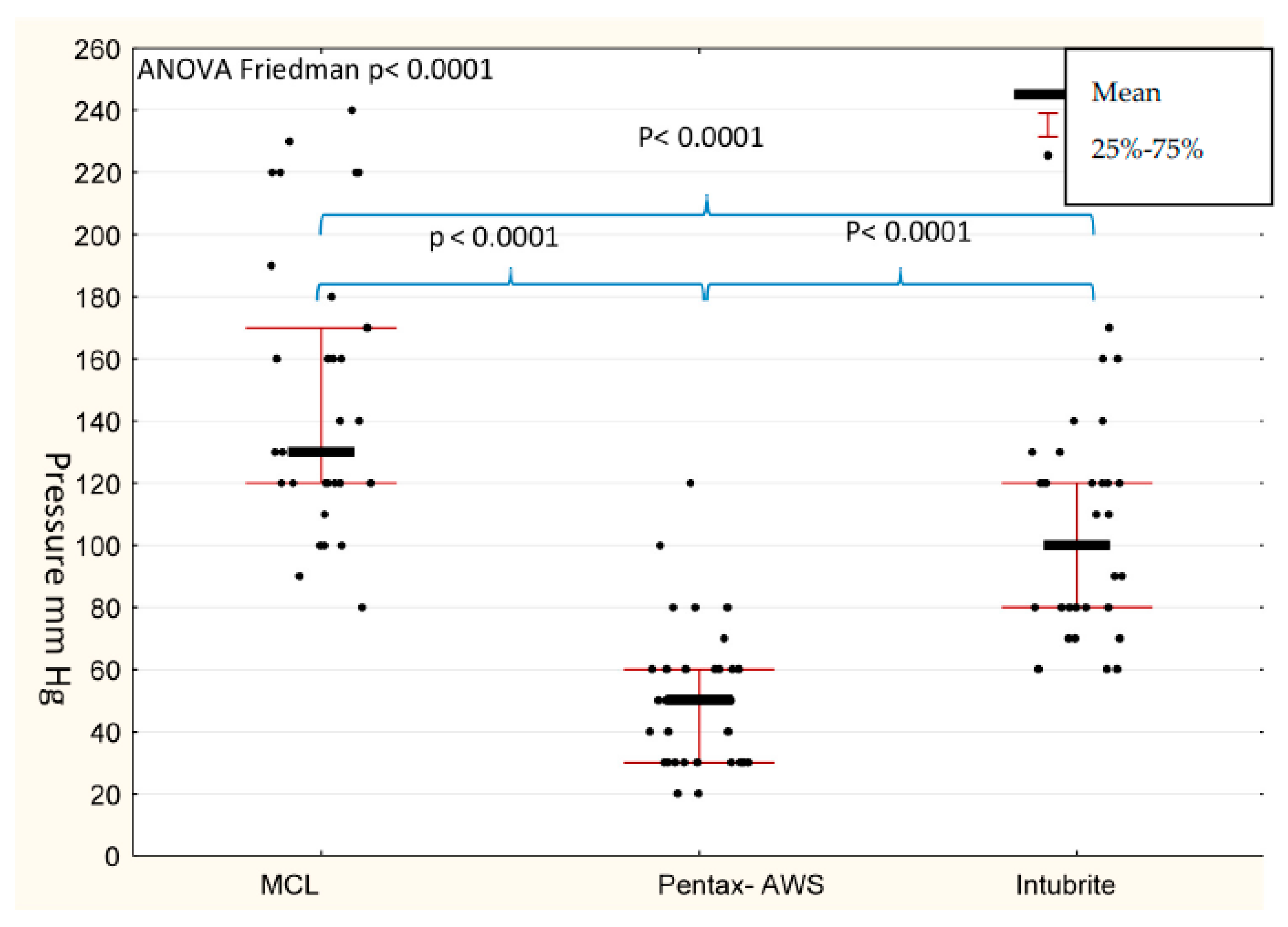
| Supine | MCL | 100 | 220 | 120 | 46.27 | - |
| Pentax-AWS | 20 | 100 | 40 | 28.57 | 0.0006 * | |
| Intubrite | 60 | 170 | 100 | 22.52 | 0.0139 * | |
| Prone | MCL | 80 | 230 | 130 | 44.78 | - |
| Pentax-AWS | 20 | 60 | 50 | 23.66 | 0.0009 * | |
| Intubrite | 70 | 160 | 120 | 37.24 | 0.0547 | |
| Sitting position | MCL | 90 | 240 | 130 | 46.74 | - |
| Pentax-AWS | 30 | 120 | 60 | 14.89 | 0.0057 * | |
| Intubrite | 60 | 130 | 100 | 29.41 | 0.0010 * |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaszyński, T.M. A Comparison of a Standard Macintosh Blade Laryngoscope, Pentax-AWS Videolaryngoscope and Intubrite Videolaryngoscope for Tracheal Intubation in Manikins in Sitting and Prone Positions: A Randomized Cross-Over Study. Diagnostics 2020, 10, 603. https://doi.org/10.3390/diagnostics10080603
Gaszyński TM. A Comparison of a Standard Macintosh Blade Laryngoscope, Pentax-AWS Videolaryngoscope and Intubrite Videolaryngoscope for Tracheal Intubation in Manikins in Sitting and Prone Positions: A Randomized Cross-Over Study. Diagnostics. 2020; 10(8):603. https://doi.org/10.3390/diagnostics10080603
Chicago/Turabian StyleGaszyński, Tomasz M. 2020. "A Comparison of a Standard Macintosh Blade Laryngoscope, Pentax-AWS Videolaryngoscope and Intubrite Videolaryngoscope for Tracheal Intubation in Manikins in Sitting and Prone Positions: A Randomized Cross-Over Study" Diagnostics 10, no. 8: 603. https://doi.org/10.3390/diagnostics10080603
APA StyleGaszyński, T. M. (2020). A Comparison of a Standard Macintosh Blade Laryngoscope, Pentax-AWS Videolaryngoscope and Intubrite Videolaryngoscope for Tracheal Intubation in Manikins in Sitting and Prone Positions: A Randomized Cross-Over Study. Diagnostics, 10(8), 603. https://doi.org/10.3390/diagnostics10080603





