Both Autopsy and Computed Tomography Are Necessary for Accurately Detecting Rib Fractures Due to Cardiopulmonary Resuscitation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. PMCT
2.4. Forensic Autopsy
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Characteristics of Rib Fractures
3.3. Detection by Autopsy according to Fracture Type on PMCT
3.4. Logistic Regression Model for Findings That Were Negative on Autopsy but Positive on PMCT
3.5. Logistic Regression Model for Findings That Were Negative on PMCT but Positive on Autopsy
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Neumar, R.W.; Shuster, M.; Callaway, C.W.; Gent, L.M.; Atkins, D.L.; Bhanji, F.; Brooks, S.C.; de Caen, A.R.; Donnino, M.W.; Ferrer, J.M.E.; et al. Part 1: Executive Summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015, 132, S315–S367. [Google Scholar] [CrossRef] [PubMed]
- Baubin, M.; Sumann, G.; Rabl, W.; Eibl, G.; Wenzel, V.; Mair, P. Increased frequency of thorax injuries with ACD-CPR. Resuscitation 1999, 41, 33–38. [Google Scholar] [CrossRef]
- Oschatz, E.; Wunderbaldinger, P.; Sterz, F.; Holzer, M.; Kofler, J.; Slatin, H.; Janata, K.; Eisenburger, P.; Bankier, A.A.; Laggner, A.N. Cardiopulmonary resuscitation performed by bystanders does not increase adverse effects as assessed by chest radiography. Anesth. Analg. 2001, 93, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Krischer, J.P.; Fine, E.G.; Davis, J.H.; Nagel, E.L. Complications of cardiac resuscitation. Chest 1987, 92, 287–291. [Google Scholar] [CrossRef] [PubMed]
- Hoke, R.S.; Chamberlain, D. Skeletal chest injuries secondary to cardiopulmonary resuscitation. Resuscitation 2004, 63, 327–338. [Google Scholar] [CrossRef] [PubMed]
- Jalalzadeh, H.; Giannakopoulos, G.F.; Berger, F.H.; Fronczek, J.; van de Goot, F.R.W.; Reijnders, U.J.; Zuidema, W.P. Post mortem imaging compared with autopsy in trauma victims--a systematic review. Forensic Sci. Int. 2015, 257, 29–48. [Google Scholar] [CrossRef] [PubMed]
- Oberladstaetter, D.; Braun, P.; Freund, M.C.; Rabl, W.; Paal, P.; Baubin, M. Autopsy is more sensitive than computed tomography in detection of LUCAS-CPR related non-dislocated chest fractures. Resuscitation 2012, 83, e89–e90. [Google Scholar] [CrossRef] [PubMed]
- Smekal, D.; Hansen, T.; Sandler, H.; Rubertsson, S. Comparison of computed tomography and autopsy in detection of injuries after unsuccessful cardiopulmonary resuscitation. Resuscitation 2013, 84, 357–360. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, R.; Makino, Y.; Chiba, F.; Torimitsu, S.; Yajima, D.; Inokuchi, G.; Motomura, A.; Hashimoto, M.; Hoshioka, Y.; Shinozaki, T.; et al. Frequency and influencing factors of cardiopulmonary resuscitation-related injuries during implementation of the American Heart Association 2010 Guidelines: A retrospective study based on autopsy and postmortem computed tomography. Int. J. Legal Med. 2017, 131, 1655–1663. [Google Scholar] [CrossRef] [PubMed]
- Kashiwagi, Y.; Sasakawa, T.; Tampo, A.; Kawata, D.; Nishiura, T.; Kokita, N.; Iwasaki, H.; Fujita, S. Computed tomography findings of complications resulting from cardiopulmonary resuscitation. Resuscitation 2015, 88, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Schulze, C.; Hoppe, H.; Schweitzer, W.; Schwendener, N.; Grabherr, S.; Jackowski, C. Rib fractures at postmortem computed tomography (PMCT) validated against the autopsy. Forensic Sci. Int. 2013, 233, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.M.; Lynch, M.; O’Donnell, C. ‘Buckle’ rib fracture: An artifact following cardio-pulmonary resuscitation detected on postmortem CT. Leg. Med. 2011, 13, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Holcombe, S.A.; Wang, S.C.; Grotberg, J.B. The effect of age and demographics on rib shape. J. Anat. 2017, 231, 229–247. [Google Scholar] [PubMed]
- Lederer, W.; Mair, D.; Rabl, W.; Baubin, M. Frequency of rib and sternum fractures associated with out-of-hospital cardiopulmonary resuscitation is underestimated by conventional chest X-ray. Resuscitation 2004, 60, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Babbs, C.F.; Kemeny, A.E.; Quan, W.; Freeman, G. A new paradigm for human resuscitation research using intelligent devices. Resuscitation 2008, 77, 306–315. [Google Scholar] [CrossRef] [PubMed]
- Hellevuo, H.; Sainio, M.; Nevalainen, R.; Huhtala, H.; Olkkola, K.T.; Tenhunen, J.; Hoppu, S. Deeper chest compression—More complications for cardiac arrest patients? Resuscitation 2013, 84, 760–765. [Google Scholar] [CrossRef] [PubMed]
| Variable | n = 62 |
|---|---|
| Age (years) | 60 (42–77) |
| Male sex | 39 (63%) |
| Height (cm) | 162 (156–172) |
| Weight (kg) | 54 (45–69) |
| Body mass index (kg/m2) | 21 (18–24) |
| Patients with rib fractures | 40 (65%) |
| No. of rib fractures per patient | 4 (0–11) |
| Cause of death | |
| Cardiac origin | 24 (39%) |
| Respiratory disease | 11 (18%) |
| Cerebral disorder | 8 (13%) |
| Other | 19 (31%) |
| Variables | All Detected Fractures | Detected by PMCT | Detected by Autopsy | Kappa Value |
|---|---|---|---|---|
| At all ribs | 339 | 289 | 272 | 0.78 |
| Rib number | ||||
| 1 | 7 | 0 | 7 | N/A |
| 2 | 40 | 34 | 36 | 0.85 |
| 3 | 60 | 54 | 47 | 0.79 |
| 4 | 72 | 66 | 55 | 0.78 |
| 5 | 65 | 60 | 52 | 0.82 |
| 6 | 48 | 44 | 41 | 0.86 |
| 7 | 31 | 22 | 23 | 0.60 |
| 8 | 10 | 5 | 8 | 0.45 |
| 9 | 4 | 3 | 2 | 0.39 |
| 10 | 2 | 1 | 1 | 0.00 |
| 11 | 0 | 0 | 0 | N/A |
| 12 | 0 | 0 | 0 | N/A |
| Fracture location | ||||
| Parasternal | 171 | 144 | 136 | 0.74 |
| Anterolateral | 151 | 136 | 122 | 0.80 |
| Posterolateral | 8 | 5 | 5 | 0.40 |
| Paravertebral | 9 | 4 | 9 | 0.61 |
| Thoracic side | ||||
| Right | 184 | 157 | 149 | 0.78 |
| Left | 155 | 132 | 123 | 0.77 |
| Sex | ||||
| Female | 165 | 134 | 138 | 0.77 |
| Male | 174 | 155 | 134 | 0.79 |
| Height | ||||
| <160 cm | 195 | 161 | 164 | 0.78 |
| ≥160 cm | 144 | 128 | 108 | 0.77 |
| Weight | ||||
| <50 kg | 212 | 177 | 177 | 0.78 |
| ≥50 kg | 127 | 112 | 95 | 0.76 |
| BMI | ||||
| <21 kg/m2 | 185 | 160 | 148 | 0.79 |
| ≥21 kg/m2 | 154 | 129 | 124 | 0.77 |
| Age | ||||
| <75 years | 148 | 131 | 101 | 0.71 |
| >75 years | 191 | 158 | 171 | 0.82 |
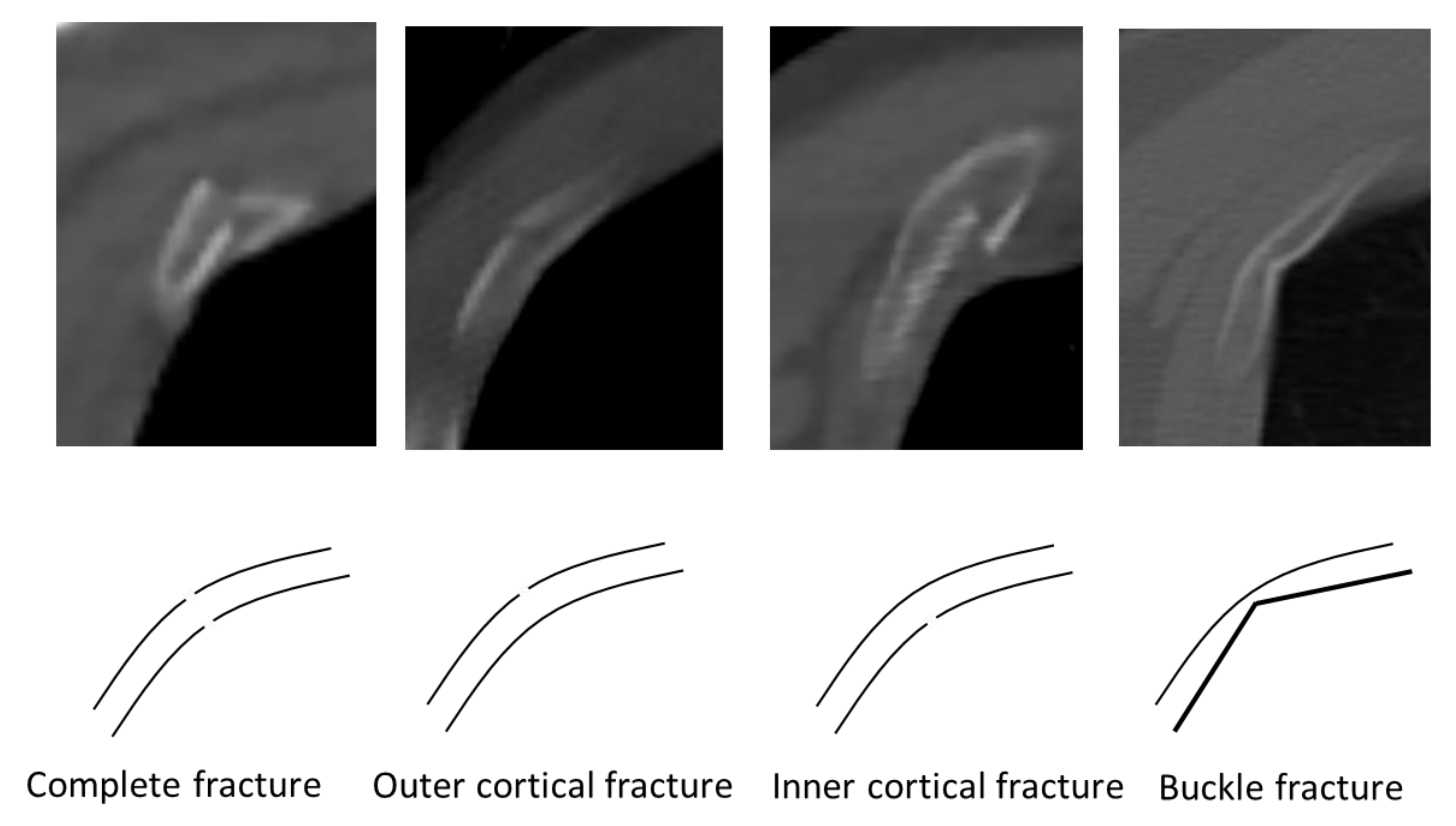
| Type of Fracture on PMCT | Detected on Autopsy, n (%) | p-Value |
|---|---|---|
| Complete (n = 106) | 100 (94) | <0.01 |
| Outer cortical (n = 14) | 9 (64) | |
| Inner cortical (n = 23) | 22 (96) | |
| Buckle (n = 146) | 91 (62) |
| A | ||
| Parameter | Odds Ratio | p-Value |
| Rib number | ||
| 4–6 | 0.88 | 0.67 |
| 1–3 and 7–12 | 1.14 | |
| Location | ||
| Anterior (parasternal, anterolateral) | 0.23 | 0.09 |
| Posterior (posteolateral, paravertebral) | 4.33 | |
| Type | ||
| Complete fractures | 0.12 | <0.01* |
| Incomplete fractures (outer cortical, inner cortical, and buckle) | 8.49 | |
| Sex | ||
| Female | 1.13 | 0.73 |
| Male | 0.88 | |
| Height | ||
| <160 cm | 0.91 | 0.82 |
| ≥160 cm | 1.10 | |
| Weight | ||
| <50 kg | 0.67 | 0.33 |
| ≥50 kg | 1.50 | |
| Age | ||
| <75 years | 3.83 | <0.01* |
| ≥75 years | 0.26 | |
| B | ||
| Parameter | Odds Ratio | p-Value |
| Rib number | ||
| 4–6 | 0.33 | <0.01* |
| 1–3 and 7–12 | 3.07 | |
| Location | ||
| Anterior (parasternal, anterolateral) | 0.21 | 0.01* |
| Posterior (posteolateral, paravertebral) | 4.76 | |
| Sex | ||
| Female | 1.74 | 0.15 |
| Male | 0.57 | |
| Height | ||
| <160 cm | 1.13 | 0.78 |
| ≥160 cm | 0.88 | |
| Weight | ||
| <50 kg | 0.86 | 0.74 |
| ≥50 kg | 1.16 | |
| Age | ||
| <75 years | 1.42 | 0.36 |
| ≥75 years | 0.70 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hamanaka, K.; Nishiyama, K.; Nakamura, M.; Takaso, M.; Hitosugi, M. Both Autopsy and Computed Tomography Are Necessary for Accurately Detecting Rib Fractures Due to Cardiopulmonary Resuscitation. Diagnostics 2020, 10, 697. https://doi.org/10.3390/diagnostics10090697
Hamanaka K, Nishiyama K, Nakamura M, Takaso M, Hitosugi M. Both Autopsy and Computed Tomography Are Necessary for Accurately Detecting Rib Fractures Due to Cardiopulmonary Resuscitation. Diagnostics. 2020; 10(9):697. https://doi.org/10.3390/diagnostics10090697
Chicago/Turabian StyleHamanaka, Kunio, Kei Nishiyama, Mami Nakamura, Marin Takaso, and Masahito Hitosugi. 2020. "Both Autopsy and Computed Tomography Are Necessary for Accurately Detecting Rib Fractures Due to Cardiopulmonary Resuscitation" Diagnostics 10, no. 9: 697. https://doi.org/10.3390/diagnostics10090697
APA StyleHamanaka, K., Nishiyama, K., Nakamura, M., Takaso, M., & Hitosugi, M. (2020). Both Autopsy and Computed Tomography Are Necessary for Accurately Detecting Rib Fractures Due to Cardiopulmonary Resuscitation. Diagnostics, 10(9), 697. https://doi.org/10.3390/diagnostics10090697






