A Broader Perspective on the Prenatal Diagnosis of Cornelia de Lange Syndrome: Review of the Literature and Case Presentation
Abstract
:1. Introduction
2. Genetics of CDLS and Prenatal Genetic Testing for CDLS
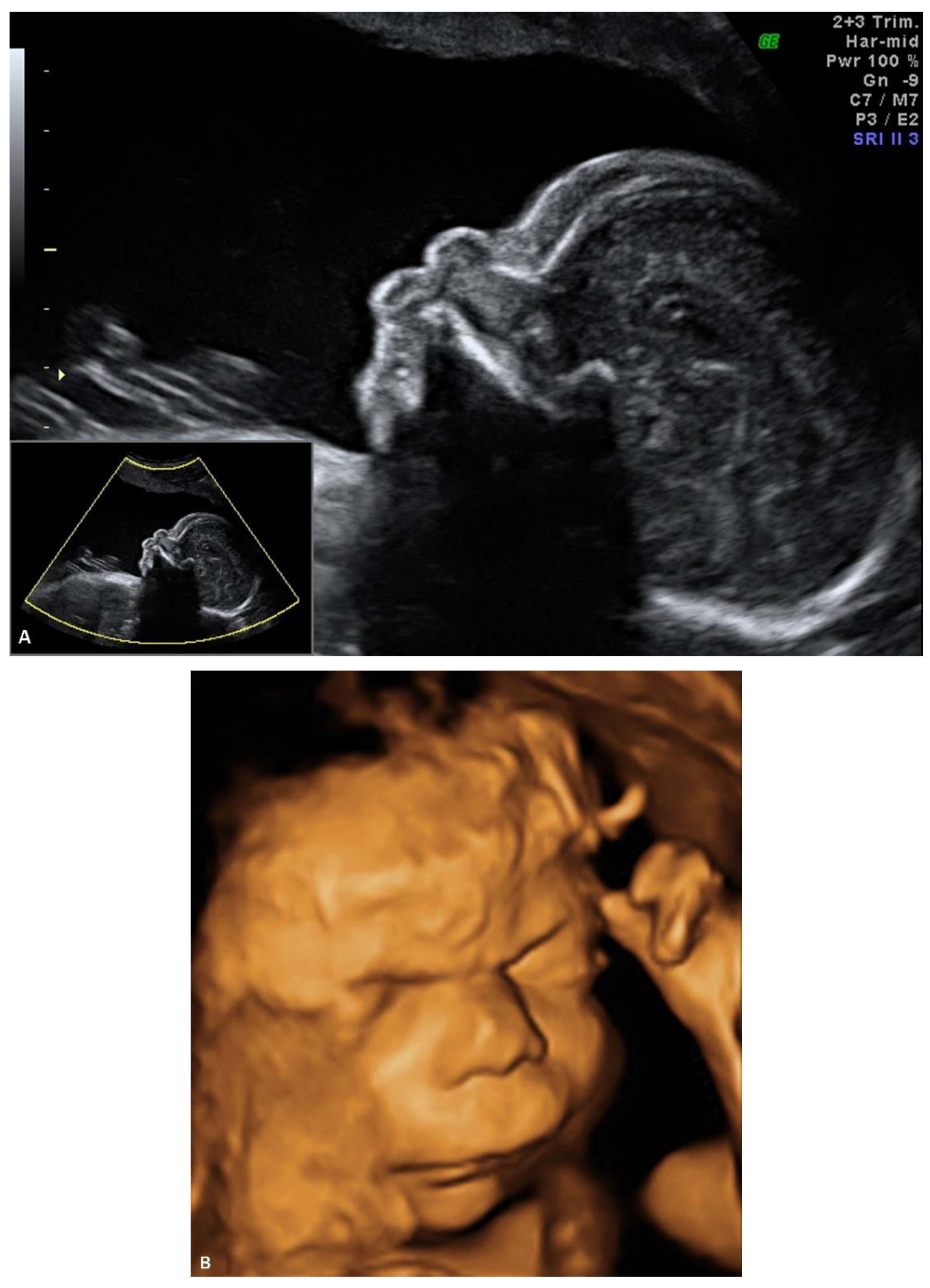
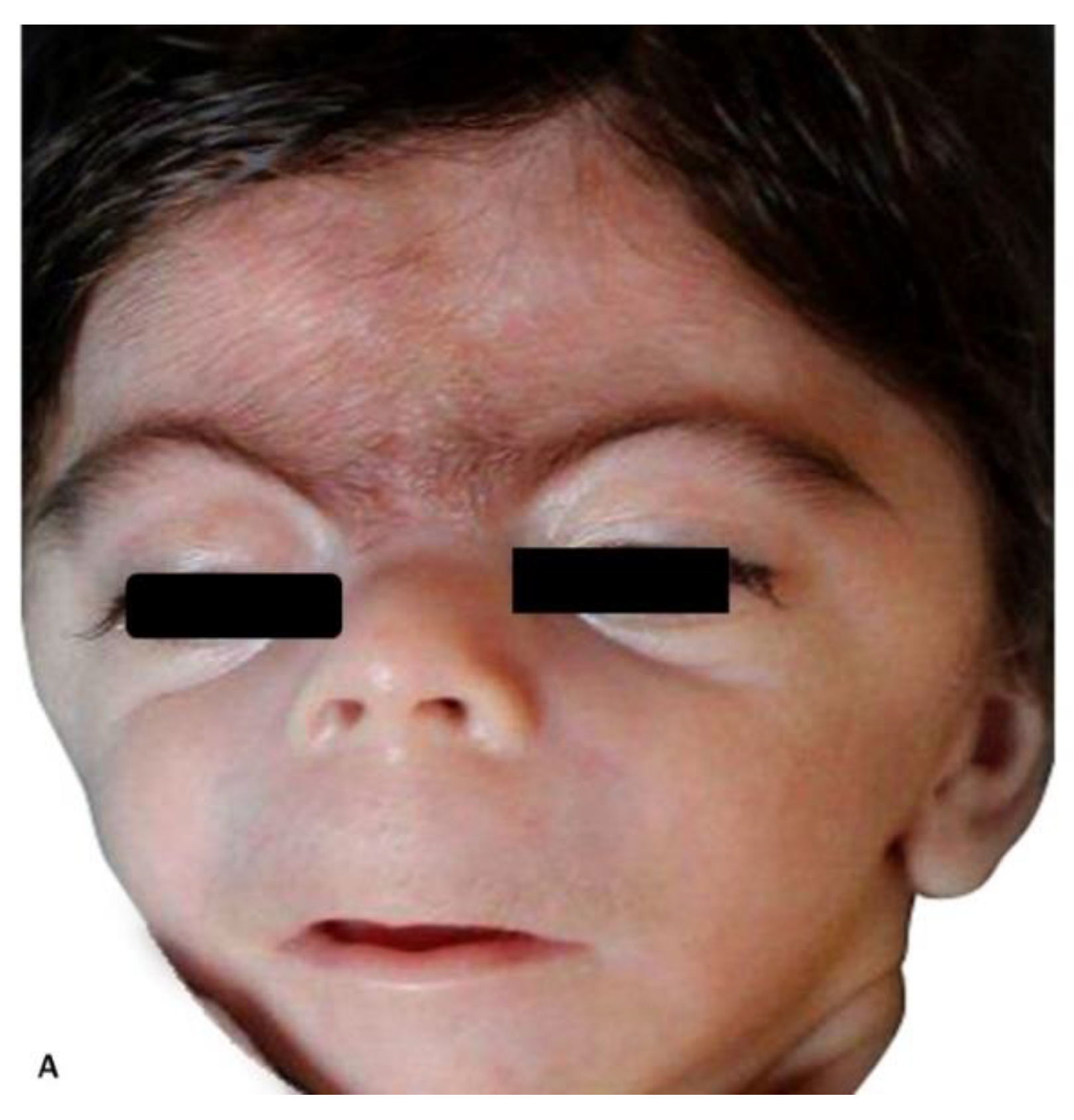
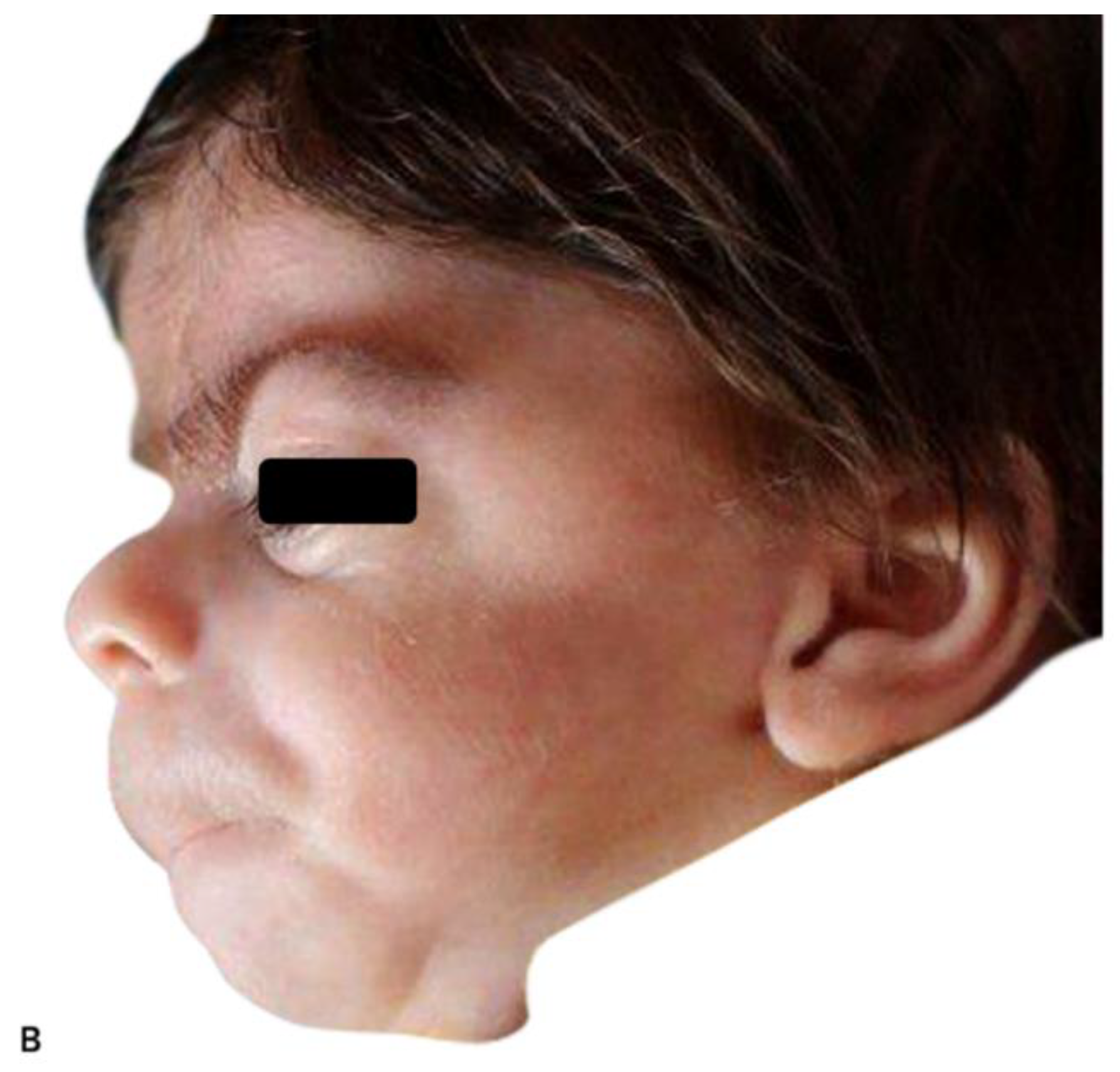
3. Ultrasound Prenatal Diagnosis of CDLS
4. Prenatal Presentation of a Classical CDLS Case
5. Discussion
5.1. The Geneticist’s Point of View
5.2. The Fetal Medicine Specialist’s Point of View
Author Contributions
Funding
Conflicts of Interest
References
- Deardorff, M.A.; Noon, S.E.; Krantz, I.D. Cornelia de Lange Syndrome 2020 October 15. In Gene Reviews® [Internet]; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Stephens, K., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993–2020. [Google Scholar]
- Kline, A.D.; Moss, J.F.; Selicorni, A.; Bisgaard, A.M.; Deardorff, M.A.; Gillett, P.M.; Ishman, S.L.; Kerr, L.M.; Levin, A.V.; Mulder, P.A.; et al. Diagnosis and management of Cornelia de Lange syndrome: First international consensus statement. Nat. Rev. Genet. 2018, 19, 649–666. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Avagliano, L.; Parenti, I.; Grazioli, P.; Di Fede, E.; Parodi, C.; Mariani, M.; Kaiser, F.J.; Selicorni, A.; Gervasini, C.; Massa, V. Chromatinopathies: A focus on Cornelia de Lange syndrome. Clin. Genet. 2020, 97, 3–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kline, A.D.; Grados, M.; Sponseller, P.; Levy, H.P.; Blagowidow, N.; Schoedel, C.; Rampolla, J.; Clemens, D.K.; Krantz, I.; Kimball, A.; et al. Natural history of aging in Cornelia de Lange syndrome. Am. J. Med. Genet. C Semin. Med. Genet. 2007, 145C, 248–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jackson, L.; Kline, A.D.; Barr, M.A.; Koch, S. De Lange syndrome: A clinical review of 310 individuals. Am. J. Med. Genet. 1993, 47, 940–946. [Google Scholar] [CrossRef] [PubMed]
- Boyle, M.I.; Jespersgaard, C.; Brøndum-Nielsen, K.; Bisgaard, A.M.; Tümer, Z. Cornelia de Lange syndrome. Clin. Genet. 2015, 88, 1–12. [Google Scholar] [CrossRef]
- Cascella, M.; Muzio, M.R. Cornelia de Lange Syndrome 4 July 2020. In Stat Pearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Barisic, I.; Tokic, V.; Loane, M.; Bianchi, F.; Calzolari, E.; Garne, E.; Wellesley, D.; Dolk, H.; EUROCAT Working Group. Descriptive epidemiology of Cornelia de Lange syndrome in Europe. Am. J. Med. Genet. A 2008, 146A, 51–59. [Google Scholar] [CrossRef]
- Bhuiyan, Z.A.; Klein, M.; Hammond, P.; van Haeringen, A.; Mannens, M.M.; Van Berckelaer-Onnes, I.; Hennekam, R.C. Genotype-phenotype correlations of 39 patients with Cornelia De Lange syndrome: The Dutch experience. J. Med. Genet. 2006, 43, 568–575. [Google Scholar] [CrossRef] [Green Version]
- Yan, J.; Saifi, G.M.; Wierzba, T.H.; Withers, M.; Bien-Willner, G.A.; Limon, J.; Stankiewicz, P.; Lupski, J.R.; Wierzba, J. Mutational and genotype-phenotype correlation analyses in 28 Polish patients with Cornelia de Lange syndrome. Am. J. Med. Genet. A 2006, 140, 1531–1541. [Google Scholar] [CrossRef]
- Selicorni, A.; Russo, S.; Gervasini, C.; Castronovo, P.; Milani, D.; Cavalleri, F.; Bentivegna, A.; Masciadri, M.; Domi, A.; Divizia, M.T.; et al. Clinical score of 62 Italian patients with Cornelia de Lange syndrome and correlations with the presence and type of NIPBL mutation. Clin. Genet. 2007, 72, 98–108. [Google Scholar] [CrossRef]
- Mariani, M.; Decimi, V.; Bettini, L.R.; Maitz, S.; Gervasini, C.; Masciadri, M.; Ajmone, P.; Kullman, G.; Dinelli, M.; Panceri, R.; et al. Adolescents and adults affected by Cornelia de Lange syndrome: A report of 73 Italian patients. Am. J. Med. Genet. C Semin. Med. Genet. 2016, 172, 206–213. [Google Scholar] [CrossRef]
- Cereda, A.; Mariani, M.; Rebora, P.; Sajeva, A.; Ajmone, P.F.; Gervasini, C.; Russo, S.; Kullmann, G.; Valsecchi, G.; Selicorni, A. A new prognostic index of severity of intellectual disabilities in Cornelia de Lange syndrome. Am. J. Med. Genet. C Semin. Med. Genet. 2016, 172, 179–189. [Google Scholar] [CrossRef]
- Pié, J.; Puisac, B.; Hernández-Marcos, M.; Teresa-Rodrigo, M.E.; Gil-Rodríguez, M.; Baquero-Montoya, C.; Ramos-Cáceres, M.; Bernal, M.; Ayerza-Casas, A.; Bueno, I.; et al. Special cases in Cornelia de Lange syndrome: The Spanish experience. Am. J. Med. Genet. C Semin. Med. Genet. 2016, 172, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Hei, M.; Gao, X.; Wu, L. Clinical and genetic study of 20 patients from China with Cornelia de Lange syndrome. BMC Pediatr. 2018, 18, 64. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Li, X.; Cui, J.; Dong, R.; Lv, Y.; Wang, D.; Zhang, H.; Li, X.; Li, Z.; Ma, J.; et al. Analysis of clinical and genetic characteristics in 10 Chinese individuals with Cornelia de Lange syndrome and literature review. Mol. Genet. Genom. Med. 2020, 8, e1471. [Google Scholar] [CrossRef] [PubMed]
- Dowsett, L.; Porras, A.R.; Kruszka, P.; Davis, B.; Hu, T.; Honey, E.; Badoe, E.; Thong, M.K.; Leon, E.; Girisha, K.M.; et al. Cornelia de Lange syndrome in diverse populations. Am. J. Med. Genet. A 2019, 179, 150–158. [Google Scholar] [CrossRef]
- Ranzini, A.C.; Day-Salvatore, D.; Farren-Chavez, D.; McLean, D.A.; Greco, R. Prenatal diagnosis of de Lange syndrome. J. Ultrasound Med. 1997, 16, 755–758. [Google Scholar] [CrossRef]
- Sepulveda, W.; Wong, A.E.; Dezerega, V. Brachmann-de Lange Syndrome: Prenatal diagnosis with 2- and 3-dimensional sonography. J. Ultrasound Med. 2009, 28, 401–404. [Google Scholar] [CrossRef]
- Kanellopoulos, V.; Iavazzo, C.; Tzanatou, C.; Papadakis, E.; Tassis, K. A case of third trimester diagnosis of Cornelia de Lange syndrome. Arch. Gynecol. Obstet. 2011, 283, 59–63. [Google Scholar] [CrossRef]
- Thellier, E.; Levaillant, J.M.; Roume, J.; Quarello, E.; Bault, J.P. Cornelia de Lange syndrome: Specific features for prenatal diagnosis. Ultrasound Obstet. Gynecol. 2017, 49, 668–670. [Google Scholar] [CrossRef]
- Avagliano, L.; Bulfamante, G.P.; Massa, V. Cornelia de Lange syndrome: To diagnose or not to diagnose in utero? Birth Defects Res. 2017, 109, 771–777. [Google Scholar] [CrossRef]
- Manouvrier, S.; Espinasse, M.; Vaast, P.; Boute, O.; Farre, I.; Dupont, F.; Puech, F.; Gosselin, B.; Farriaux, J.P. Brachmann-de Lange syndrome: Pre- and postnatal findings. Am. J. Med. Genet. 1996, 62, 268–273. [Google Scholar] [CrossRef]
- Boog, G.; Sagot, F.; Winer, N.; David, A.; Nomballais, M.F. Brachmann-de Lange syndrome: A cause of early symmetric fetal growth delay. Eur. J. Obstet. Gynecol. Reprod. Biol. 1999, 85, 173–177. [Google Scholar] [CrossRef]
- Sekimoto, H.; Osada, H.; Kimura, H.; Kamiyama, M.; Arai, K.; Sekiya, S. Prenatal findings in Brachmann-de Lange syndrome. Arch. Gynecol. Obstet. 2000, 263, 182–184. [Google Scholar] [CrossRef] [PubMed]
- Urban, M.; Hartung, J. Ultrasonographic and clinical appearance of a 22-week-old fetus with Brachmann-de Lange syndrome. Am. J. Med. Genet. 2001, 102, 73–75. [Google Scholar] [CrossRef]
- Huang, W.H.; Porto, M. Abnormal first-trimester fetal nuchal translucency and Cornelia De Lange syndrome. Obstet. Gynecol. 2002, 99 Pt 2, 956–958. [Google Scholar]
- Marino, T.; Wheeler, P.G.; Simpson, L.L.; Craigo, S.D.; Bianchi, D.W. Fetal diaphragmatic hernia and upper limb anomalies suggest Brachmann-de Lange syndrome. Prenat. Diagn. 2002, 22, 144–147. [Google Scholar] [CrossRef]
- Chong, K.; Keating, S.; Hurst, S.; Summers, A.; Berger, H.; Seaward, G.; Martin, N.; Friedberg, T.; Chitayat, D. Cornelia de Lange syndrome (CdLS): Prenatal and autopsy findings. Prenat. Diagn. 2009, 29, 489–494. [Google Scholar] [CrossRef]
- Wilmink, F.A.; Papatsonis, D.N.; Grijseels, E.W.; Wessels, M.W. Cornelia de Lange syndrome: A recognizable fetal phenotype. Fetal. Diagn. Ther. 2009, 26, 50–53. [Google Scholar] [CrossRef]
- Pajkrt, E.; Griffin, D.R.; Chitty, L.S. Brachmann-de Lange syndrome: Definition of prenatal sonographic features to facilitate definitive prenatal diagnosis. Prenat. Diagn. 2010, 30, 865–872. [Google Scholar] [CrossRef]
- Clark, D.M.; Sherer, I.; Deardorff, M.A.; Byrne, J.L.; Loomes, K.M.; Nowaczyk, M.J.; Jackson, L.G.; Krantz, I.D. Identification of a prenatal profile of Cornelia de Lange syndrome (CdLS): A review of 53 CdLS pregnancies. Am. J. Med. Genet. A 2012, 158A, 1848–1856. [Google Scholar] [CrossRef] [Green Version]
- Kliewer, M.A.; Kahler, S.G.; Hertzberg, B.S.; Bowie, J.D. Fetal biometry in the Brachmann-de Lange syndrome. Am. J. Med. Genet. 1993, 47, 1035–1041. [Google Scholar] [CrossRef] [PubMed]
- Bruner, J.P.; Hsia, Y.E. Prenatal findings in Brachmann-de Lange syndrome. Obstet. Gynecol. 1990, 76, 966–968. [Google Scholar] [PubMed]
- Drolshagen, L.F.; Durmon, G.; Berumen, M.; Burks, D.D. Prenatal ultrasonographic appearance of “Cornelia de Lange” syndrome. J. Clin. Ultrasound 1992, 20, 470–474. [Google Scholar] [CrossRef] [PubMed]
- Spaggiari, E.; Vuillard, E.; Khung-Savatovsky, S.; Muller, F.; Oury, J.F.; Delezoide, A.L.; Guimiot, F. Ultrasound detection of eyelashes: A clue for prenatal diagnosis of Cornelia de Lange syndrome. Ultrasound Obstet. Gynecol. 2013, 41, 341–342. [Google Scholar] [CrossRef] [PubMed]
- Dempsey, M.A.; Knight Johnson, A.E.; Swope, B.S.; Moldenhauer, J.S.; Sroka, H.; Chong, K.; Chitayat, D.; Briere, L.; Lyon, H.; Palmer, N.; et al. Molecular confirmation of nine cases of Cornelia de Lange syndrome diagnosed prenatally. Prenat. Diagn. 2014, 34, 163–167. [Google Scholar] [CrossRef]
- Hague, J.; Twiss, P.; Mead, Z.; Park, S.M. Clinical Diagnosis of Classical Cornelia de Lange Syndrome Made from Postmortem Examination of Second Trimester Fetus With Novel NIPBL Pathogenic Variant. Pediatr. Dev. Pathol. 2019, 22, 475–479. [Google Scholar] [CrossRef]
- Richards, S.; Aziz, N.; Bale, S.; Bick, D.; Das, S.; Gastier-Foster, J.; Grody, W.W.; Hegde, M.; Lyon, E.; Spector, E.; et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015, 17, 405–424. [Google Scholar] [CrossRef]
- Nedelea, F.; Veduta, A.; Duta, S.; Vayna, A.M.; Panaitescu, A.; Peltecu, G.; Duba, H.C. Prenatal Genetic Testing for Dopa-Responsive Dystonia—Clinical Judgment in the Context of Next Generation Sequencing. J. Med. Life 2018, 11, 343–345. [Google Scholar]
- Huisman, S.A.; Redeker, E.J.; Maas, S.M.; Mannens, M.M.; Hennekam, R.C. High rate of mosaicism in individuals with Cornelia de Lange syndrome. J. Med. Genet. 2013, 50, 339–344. [Google Scholar] [CrossRef]
- Ansari, M.; Poke, G.; Ferry, Q.; Williamson, K.; Aldridge, R.; Meynert, A.M.; Bengani, H.; Chan, C.Y.; Kayserili, H.; Avci, S.; et al. Genetic heterogeneity in Cornelia de Lange syndrome (CdLS) and CdLS-like phenotypes with observed and predicted levels of mosaicism. J. Med. Genet. 2014, 51, 659–668. [Google Scholar] [CrossRef] [Green Version]
- Mannini, L.; Cucco, F.; Quarantotti, V.; Krantz, I.D.; Musio, A. Mutation spectrum and genotype-phenotype correlation in Cornelia de Lange syndrome. Hum. Mutat. 2013, 34, 1589–1596. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pié, J.; Gil-Rodríguez, M.C.; Ciero, M.; López-Viñas, E.; Ribate, M.P.; Arnedo, M.; Deardorff, M.A.; Puisac, B.; Legarreta, J.; de Karam, J.C.; et al. Mutations and variants in the cohesion factor genes NIPBL, SMC1A, and SMC3 in a cohort of 30 unrelated patients with Cornelia de Lange syndrome. Am. J. Med. Genet. A 2010, 152A, 924–929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schoumans, J.; Wincent, J.; Barbaro, M.; Djureinovic, T.; Maguire, P.; Forsberg, L.; Staaf, J.; Thuresson, A.C.; Borg, A.; Nordgren, A.; et al. Comprehensive mutational analysis of a cohort of Swedish Cornelia de Lange syndrome patients. Eur. J. Hum. Genet. 2007, 15, 143–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tonkin, E.T.; Wang, T.J.; Lisgo, S.; Bamshad, M.J.; Strachan, T. NIPBL, encoding a homolog of fungal Scc2-type sister chromatid cohesion proteins and fly Nipped-B, is mutated in Cornelia de Lange syndrome. Nat. Genet. 2004, 36, 636–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, J.; Krantz, I.D. Cornelia de Lange syndrome, cohesin, and beyond. Clin. Genet. 2009, 76, 303–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarogni, P.; Pallotta, M.M.; Musio, A. Cornelia de Lange syndrome: From molecular diagnosis to therapeutic approach. J. Med. Genet. 2020, 57, 289–295. [Google Scholar] [CrossRef]
- Borck, G.; Redon, R.; Sanlaville, D.; Rio, M.; Prieur, M.; Lyonnet, S.; Vekemans, M.; Carter, N.P.; Munnich, A.; Colleaux, L.; et al. NIPBL mutations and genetic heterogeneity in Cornelia de Lange syndrome. J. Med. Genet. 2004, 41, e128. [Google Scholar] [CrossRef] [Green Version]
- Gillis, L.A.; McCallum, J.; Kaur, M.; DeScipio, C.; Yaeger, D.; Mariani, A.; Kline, A.D.; Li, H.H.; Devoto, M.; Jackson, L.G.; et al. NIPBL mutational analysis in 120 individuals with Cornelia de Lange syndrome and evaluation of genotype-phenotype correlations. Am. J. Hum. Genet. 2004, 75, 610–623. [Google Scholar] [CrossRef] [Green Version]
- Deardorff, M.A.; Wilde, J.J.; Albrecht, M.; Dickinson, E.; Tennstedt, S.; Braunholz, D.; Mönnich, M.; Yan, Y.; Xu, W.; Gil-Rodríguez, M.C.; et al. RAD21 mutations cause a human cohesinopathy. Am. J. Hum. Genet. 2012, 90, 1014–1027. [Google Scholar] [CrossRef] [Green Version]
- Gudmundsson, S.; Annerén, G.; Marcos-Alcalde, Í.; Wilbe, M.; Melin, M.; Gómez-Puertas, P.; Bondeson, M.L. A novel RAD21 p. (Gln592del) variant expands the clinical description of Cornelia de Lange syndrome type 4—Review of the literature. Eur. J. Med. Genet. 2019, 62, 103526. [Google Scholar] [CrossRef]
- Krab, L.C.; Marcos-Alcalde, I.; Assaf, M.; Balasubramanian, M.; Andersen, J.B.; Bisgaard, A.M.; Fitzpatrick, D.R.; Gudmundsson, S.; Huisman, S.A.; Kalayci, T.; et al. Delineation of phenotypes and genotypes related to cohesin structural protein RAD21. Hum. Genet. 2020, 139, 575–592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deardorff, M.A.; Kaur, M.; Yaeger, D.; Rampuria, A.; Korolev, S.; Pie, J.; Gil-Rodríguez, C.; Arnedo, M.; Loeys, B.; Kline, A.D.; et al. Mutations in cohesin complex members SMC3 and SMC1A cause a mild variant of Cornelia de Lange syndrome with predominant mental retardation. Am. J. Hum. Genet. 2007, 80, 485–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gil-Rodríguez, M.C.; Deardorff, M.A.; Ansari, M.; Tan, C.A.; Parenti, I.; Baquero-Montoya, C.; Ousager, L.B.; Puisac, B.; Hernández-Marcos, M.; Teresa-Rodrigo, M.E.; et al. De novo heterozygous mutations in SMC3 cause a range of Cornelia de Lange syndrome-overlapping phenotypes. Hum. Mutat. 2015, 36, 454–462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olley, G.; Ansari, M.; Bengani, H.; Grimes, G.R.; Rhodes, J.; von Kriegsheim, A.; Blatnik, A.; Stewart, F.J.; Wakeling, E.; Carroll, N.; et al. BRD4 interacts with NIPBL and BRD4 is mutated in a Cornelia de Lange-like syndrome. Nat. Genet. 2018, 50, 329–332. [Google Scholar] [CrossRef] [PubMed]
- Parenti, I.; Gervasini, C.; Pozojevic, J.; Graul-Neumann, L.; Azzollini, J.; Braunholz, D.; Watrin, E.; Wendt, K.S.; Cereda, A.; Cittaro, D.; et al. Broadening of cohesinopathies: Exome sequencing identifies mutations in ANKRD11 in two patients with Cornelia de Lange-overlapping phenotype. Clin. Genet. 2016, 89, 74–81. [Google Scholar] [CrossRef]
- Deardorff, M.A.; Porter, N.J.; Christianson, D.W. Structural aspects of HDAC8 mechanism and dysfunction in Cornelia de Lange syndrome spectrum disorders. Protein Sci. 2016, 25, 1965–1976. [Google Scholar] [CrossRef] [Green Version]
- Kaiser, F.J.; Ansari, M.; Braunholz, D.; Concepción Gil-Rodríguez, M.; Decroos, C.; Wilde, J.J.; Fincher, C.T.; Kaur, M.; Bando, M.; Amor, D.J.; et al. Loss-of-function HDAC8 mutations cause a phenotypic spectrum of Cornelia de Lange syndrome-like features.; ocular hypertelorism.; large fontanelle and X-linked inheritance. Hum. Mol. Genet. 2014, 23, 2888–2900. [Google Scholar] [CrossRef] [Green Version]
- Parenti, I.; Gervasini, C.; Pozojevic, J.; Wendt, K.S.; Watrin, E.; Azzollini, J.; Braunholz, D.; Buiting, K.; Cereda, A.; Engels, H.; et al. Expanding the clinical spectrum of the ‘HDAC8-phenotype’—Implications for molecular diagnostics, counseling and risk prediction. Clin. Genet. 2016, 89, 564–573. [Google Scholar] [CrossRef]
- Musio, A.; Selicorni, A.; Focarelli, M.L.; Gervasini, C.; Milani, D.; Russo, S.; Vezzoni, P.; Larizza, L. X-linked Cornelia de Lange syndrome owing to SMC1L1 mutations. Nat. Genet. 2006, 38, 528–530. [Google Scholar] [CrossRef]
- Borck, G.; Zarhrate, M.; Bonnefont, J.P.; Munnich, A.; Cormier-Daire, V.; Colleaux, L. Incidence and clinical features of X-linked Cornelia de Lange syndrome due to SMC1L1 mutations. Hum. Mutat. 2007, 28, 205–206. [Google Scholar] [CrossRef]
- Huisman, S.; Mulder, P.A.; Redeker, E.; Bader, I.; Bisgaard, A.M.; Brooks, A.; Cereda, A.; Cinca, C.; Clark, D.; Cormier-Daire, V.; et al. Phenotypes and genotypes in individuals with SMC1A variants. Am. J. Med. Genet. A 2017, 173, 2108–2125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woods, S.A.; Robinson, H.B.; Kohler, L.J.; Agamanolis, D.; Sterbenz, G.; Khalifa, M. Exome sequencing identifies a novel EP300 frame shift mutation in a patient with features that overlap Cornelia de Lange syndrome. Am. J. Med. Genet. A 2014, 164A, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Yuan, B.; Pehlivan, D.; Karaca, E.; Patel, N.; Charng, W.L.; Gambin, T.; Gonzaga-Jauregui, C.; Sutton, V.R.; Yesil, G.; Bozdogan, S.T.; et al. Global transcriptional disturbances underlie Cornelia de Lange syndrome and related phenotypes. J. Clin. Investig. 2015, 125, 636–651. [Google Scholar] [CrossRef] [PubMed]
- Vayna, A.M.; Veduta, A.; Duta, S.; Panaitescu, A.M.; Stoica, S.; Buinoiu, N.; Nedelea, F.; Peltecu, G. Diagnosis of Fetal Structural Anomalies at 11 to 14 Weeks. J. Ultrasound Med. 2018, 37, 2063–2073. [Google Scholar] [CrossRef] [Green Version]

| Prenatal Ultrasound Diagnosis | |
|---|---|
| Cardinal Features * | |
| Synophrys and/or thick eyebrows | Possible, especially with volumetric ultrasound [18,19,20,21,22] |
| Short nose, concave nasal ridge and/or upturned nasal tip | Possible, on volumetric rendering or good midsagittal view of the fetal face [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32] |
| Long and/or smooth philtrum | Possible, on volumetric rendering or good midsagittal view of the fetal face [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32] |
| Thin upper lip vermilion and/or downturned corners of mouth | Possible with volumetric ultrasound [21,32] |
| Hand oligodactyly and/or adactyly | Possible; mandatory if severe defect [20,21,22,30,31,32] |
| Congenital diaphragmatic hernia | Possible in most cases [22,28,31,32] |
| Suggestive features * | |
| Global developmental delay and/or intellectual disability | Postnatal diagnosis |
| Prenatal growth retardation (<2SD) | Yes [18,21,22,23,24,31,32,33] |
| Postnatal growth retardation (<2SD) | Postnatal diagnosis |
| Microcephaly | Yes [18,22,23,24,31,33] |
| Small hands and/or feet | Difficult to objectively assess, very few reports of prenatal diagnosis [31] |
| Short fifth finger | Yes [21,22] |
| Hirsutism | Difficult prenatal diagnosis [21,22] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panaitescu, A.M.; Duta, S.; Gica, N.; Botezatu, R.; Nedelea, F.; Peltecu, G.; Veduta, A. A Broader Perspective on the Prenatal Diagnosis of Cornelia de Lange Syndrome: Review of the Literature and Case Presentation. Diagnostics 2021, 11, 142. https://doi.org/10.3390/diagnostics11010142
Panaitescu AM, Duta S, Gica N, Botezatu R, Nedelea F, Peltecu G, Veduta A. A Broader Perspective on the Prenatal Diagnosis of Cornelia de Lange Syndrome: Review of the Literature and Case Presentation. Diagnostics. 2021; 11(1):142. https://doi.org/10.3390/diagnostics11010142
Chicago/Turabian StylePanaitescu, Anca Maria, Simona Duta, Nicolae Gica, Radu Botezatu, Florina Nedelea, Gheorghe Peltecu, and Alina Veduta. 2021. "A Broader Perspective on the Prenatal Diagnosis of Cornelia de Lange Syndrome: Review of the Literature and Case Presentation" Diagnostics 11, no. 1: 142. https://doi.org/10.3390/diagnostics11010142
APA StylePanaitescu, A. M., Duta, S., Gica, N., Botezatu, R., Nedelea, F., Peltecu, G., & Veduta, A. (2021). A Broader Perspective on the Prenatal Diagnosis of Cornelia de Lange Syndrome: Review of the Literature and Case Presentation. Diagnostics, 11(1), 142. https://doi.org/10.3390/diagnostics11010142








