Assessment of 3D Lumbosacral Vascular Anatomy for OLIF51 by Non-Enhanced MRI and CT Medical Image Fusion Technique
Abstract
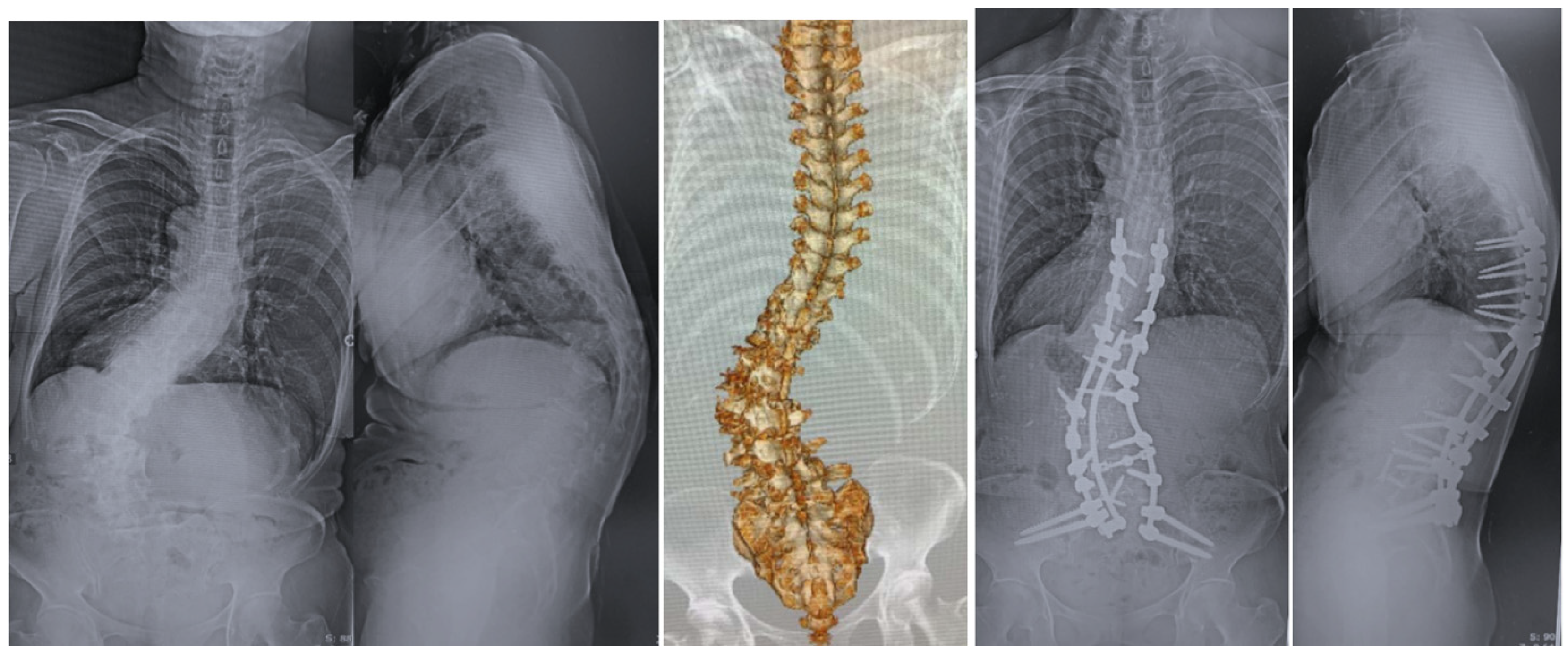
:1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Image Technique
2.3. CT–MRI Fusion Image
2.4. Evaluation of Merged Images
3. Results
3.1. Radiological Evaluations
3.2. Clinical Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Konno, S.; Kikuchi, S.; Nagaosa, Y. The relationship between intramuscular pressure of the paraspinal muscles and low back pain. Spine 1994, 19, 2186–2189. [Google Scholar] [CrossRef]
- Hosogane, N.; Watanabe, K.; Yagi, M.; Kaneko, S.; Toyama, Y.; Matsumoto, M. Scoliosis is Risk Factor for Gastroesophageal Reflex Disease in Adult Spina Deformity. Clin. Spine Surg. 2017, 30, E480–E484. [Google Scholar] [CrossRef]
- Roussouly, P.; Gollogly, S.; Berthonnaud, E.; Dimnet, J. Classification of the normal variation in the sagittal aligment of the human lumber spine and pelvis in the standing position. Spine 2005, 30, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Lafage, V.; Patel, A.; Farcy, J.P. Sagittal plane consideration and the pelvis in the adult patient. Spine 2009, 34, 1828–1833. [Google Scholar] [CrossRef] [PubMed]
- Anand, N.; Baron, E.M.; Khandehroo, B.; Kahwaty, S. Long-term 2- to 5-year clinical and functional outcomes of minimally invasive surgery for adult scoliosis. Spine 2013, 38, 1566–1575. [Google Scholar] [CrossRef]
- Tanaka, M.; Fujiwara, Y.; Uotani, K.; Maste, P.; Yamauchi, T. C-Arm-Free Circumferential Minimally Invasive Surgery for Adult Spinal Deformity: Technical Note. World Neurosurg. 2020, 143, 235–246. [Google Scholar] [CrossRef] [PubMed]
- Kotani, Y.; Ikeura, A.; Tokunaga, H.; Saito, T. Single-level controlled comparison of OLIF51 and percutaneous screw in lateral position versus MIS-TLIF for lumbosacral degenerative disorders: Clinical and radiologic study. J. Orthop. Sci. 2020, 20, S0949–S2658. [Google Scholar] [CrossRef]
- Choi, J.; Rhee, I.; Ruparel, S. Assessment of Great Vessels for Anterior Access of L5/S1 Using Patient Positioning. Asian Spine J. 2020, 14, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Anand, N.; Alayan, A.; Agrawal, A.; Kahwaty, S.; Nomoto, E.; Khandehroo, B. Analysis of Spino-Pelvic Parameters and Segmental Lordosis with L5-S1 Oblique Lateral Interbody Fusion at the Bottom of a Long Construct in Circumferential Minimally Invasive Surgical Correction of Adult Spinal Deformity. World Neurosurg. 2019, 130, e1077–e1083. [Google Scholar] [CrossRef] [PubMed]
- Bateman, D.K.; Millhouse, P.W.; Shahi, N.; Kadam, A.B.; Maltenfort, M.G.; Koerner, J.D.; Vaccaro, A.R. Anterior lumbar spine surgery: A systematic review and meta-analysis of associated complications. Spine J. 2015, 15, 1118–1132. [Google Scholar] [CrossRef] [PubMed]
- Faucon, A.L.; Bobrie, G.; Clément, O. Nephrotoxicity of iodinated contrast media: From pathophysiology to prevention strategies. Eur. J. Radiol. 2019, 116, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Krause, D.; Marycz, D.; Ziada, K.M. Nonrenal Complications of Contrast Media. Interv. Cardiol. Clin. 2020, 9, 311–319. [Google Scholar] [CrossRef]
- Shen, F.H.; Samartzis, D.; Khanna, A.J.; Anderson, D.G. Minimally invasive techniques for lumbar interbody fusions. Orthop. Clin. N. Am. 2007, 38, 373–386. [Google Scholar] [CrossRef] [PubMed]
- Dakwar, E.; Cardona, R.F.; Smith, D.A.; Uribe, J.S. Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg. Focus 2010, 28, E8. [Google Scholar] [CrossRef] [Green Version]
- Malham, G.M.; Parker, R.M.; Ellis, N.J.; Blecher, C.M.; Chow, F.Y.; Claydon, M.H. Anterior lumbar interbody fusion using recombinant human bone morphogenetic protein-2: A prospective study of complications. J. Neurosurg. Spine 2014, 21, 851–860. [Google Scholar] [CrossRef] [Green Version]
- Rao, P.J.; Maharaj, M.M.; Phan KAbeygunasekara, M.L.; Mobbs, R.J. Indirect foraminal decompression after anterior lumbar interbody fusion: A prospective radiographic study using a new pedicle to pedicle technique. Spine J. 2015, 15, 817–824. [Google Scholar] [CrossRef] [PubMed]
- Mundis, G.M.; Akbarnia, B.A.; Phillips, F.M. Adult deformity correction through minimally invasive lateral approach techniques. Spine 2010, 35 (Suppl. 26), S312–S321. [Google Scholar] [CrossRef] [Green Version]
- Zhu, L.; Wang, J.; Zhang, L.; Feng, X. Outcomes of Oblique Lateral Interbody Fusion for Adult Spinal Deformity: A Systematic Review and Meta-Analysis. Glob. Spine J. 2021, 13, 2192568220979145. [Google Scholar]
- Molinares, D.M.; Davis, T.T.; Fung, D.A. Retroperitoneal oblique corridor to the L2-S1 intervertebral discs: An MRI study. J. Neurosurg. Spine 2016, 24, 248–255. [Google Scholar] [CrossRef] [Green Version]
- Davis, T.T.; Hynes, R.A.; Fung, D.A.; Spann, S.W.; MacMillan, M.; Kwon, B.; Liu, J.; Acosta, F.; Drochner, T.E. Retroperitoneal oblique corridor to the L2-S1 intervertebral discs in the lateral position: An anatomic study. J. Neurosurg. Spine 2014, 21, 785–793. [Google Scholar] [CrossRef]
- Liu, L.; Liang, Y.; Zhang, H.; Wang, H.; Guo, C.; Pu, X.; Zhang, C.; Wang, L.; Wang, J.; Lv, Y.; et al. Imaging Anatomical Research on the Operative Windows of Oblique Lumbar Interbody Fusion. PLoS ONE 2016, 11, e0163452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hlubek, R.J.; Theodore, N.; Chang, S.W. CT/MRI Fusion for Vascular Mapping and Navigated Resection of a Paraspinal Tumor. World Neurosurg. 2016, 89, 732.e7–732.e12. [Google Scholar] [CrossRef] [PubMed]
- Leong, J.L.; Batra, P.S.; Citardi, M.J. CT-MR image fusion for the management of skull base lesions. Otolaryngol. Head Neck Surg. 2006, 134, 868–876. [Google Scholar] [CrossRef] [PubMed]
- Li, J.X.; Mobbs, R.J.; Phan, K. Morphometric MRI Imaging Study of the Corridor for the Oblique Lumbar Interbody Fusion Technique at L1-L5. World Neurosurg. 2018, 111, e678–e685. [Google Scholar]
- Cowburn, P.J.; Patel, H.; Pipes, R.R.; Parker, J.D. Contrast nephropathy post cardiac resynchronization therapy: An under-recognized complication with important morbidity. Eur. J. Heart Fail. 2005, 7, 899–903. [Google Scholar] [CrossRef] [Green Version]
- Song, S.J.; Shin, M.H.; Kim, J.T. Anatomical feasibility of right oblique approach for L5-S1 oblique lumbar interbody fusion. World Neurosurg. 2019, 132, e403–e408. [Google Scholar] [CrossRef]




| N = 15 | |
|---|---|
| Gender (Man: Woman) | 0:15 |
| Age (mean ± S.D.) (year) | 75.3±8.6 |
| Height (mean ± S.D.) (cm) | 154.2 ± 8.2 |
| Body weight (mean ± S.D.) (kg) | 59.3 ± 11.8 |
| Body mass index (mean ± S.D.) (kg/m2) | 24.9 ± 4.4 |
| History of abdominal surgery | Uterus surgery 2 |
| Radiological Evaluation | N = 15 |
|---|---|
| Inter common iliac vessel distance at L5 caudal endplate (mm) | 29.7 ± 10.7 |
| Inter common iliac vessel distance at S1 cranial endplate (mm) | 36.9 ± 10.3 |
| Distance from bifurcation of common iliac vein to L5 caudal endplate (mm) | 23.7 ± 10.9 |
| Distance from bifurcation of common iliac artery to L5 caudal endplate (mm) | 33.6 ± 10.1 |
| L5 vertebral body height (mm) | 24.8 ± 3.5 |
| Coronal deviation of bifurcation of common iliac vein (mm) (+;right, −;left) | 12.6 ± 12.3 |
| Coronal deviation of bifurcation of common iliac artery (mm) (+;right, −;left) | −0.79 ± 7.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nagamatsu, M.; Ruparel, S.; Tanaka, M.; Fujiwara, Y.; Uotani, K.; Arataki, S.; Yamauchi, T.; Takeshita, Y.; Takamoto, R.; Tanaka, M.; et al. Assessment of 3D Lumbosacral Vascular Anatomy for OLIF51 by Non-Enhanced MRI and CT Medical Image Fusion Technique. Diagnostics 2021, 11, 1744. https://doi.org/10.3390/diagnostics11101744
Nagamatsu M, Ruparel S, Tanaka M, Fujiwara Y, Uotani K, Arataki S, Yamauchi T, Takeshita Y, Takamoto R, Tanaka M, et al. Assessment of 3D Lumbosacral Vascular Anatomy for OLIF51 by Non-Enhanced MRI and CT Medical Image Fusion Technique. Diagnostics. 2021; 11(10):1744. https://doi.org/10.3390/diagnostics11101744
Chicago/Turabian StyleNagamatsu, Masakazu, Sameer Ruparel, Masato Tanaka, Yoshihiro Fujiwara, Koji Uotani, Shinya Arataki, Taro Yamauchi, Yoshiyuki Takeshita, Rika Takamoto, Masato Tanaka, and et al. 2021. "Assessment of 3D Lumbosacral Vascular Anatomy for OLIF51 by Non-Enhanced MRI and CT Medical Image Fusion Technique" Diagnostics 11, no. 10: 1744. https://doi.org/10.3390/diagnostics11101744
APA StyleNagamatsu, M., Ruparel, S., Tanaka, M., Fujiwara, Y., Uotani, K., Arataki, S., Yamauchi, T., Takeshita, Y., Takamoto, R., Tanaka, M., & Moriue, S. (2021). Assessment of 3D Lumbosacral Vascular Anatomy for OLIF51 by Non-Enhanced MRI and CT Medical Image Fusion Technique. Diagnostics, 11(10), 1744. https://doi.org/10.3390/diagnostics11101744







