Predictors of Loss of Functional Independence in Parkinson’s Disease: Results from the COPPADIS Cohort at 2-Year Follow-Up and Comparison with a Control Group
Abstract
:1. Introduction
2. Methods
2.1. Data Analysis
2.2. Standard Protocol Approvals, Registrations, and Patient Consents
2.3. Data Availability
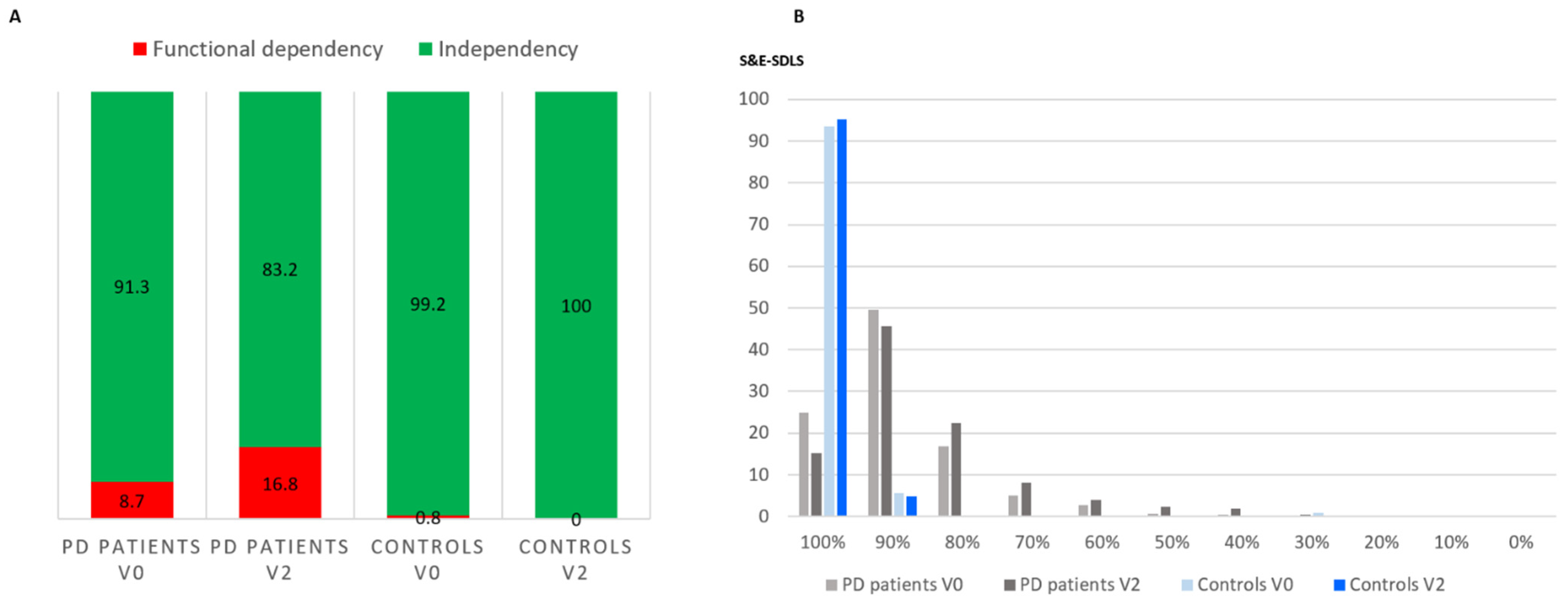
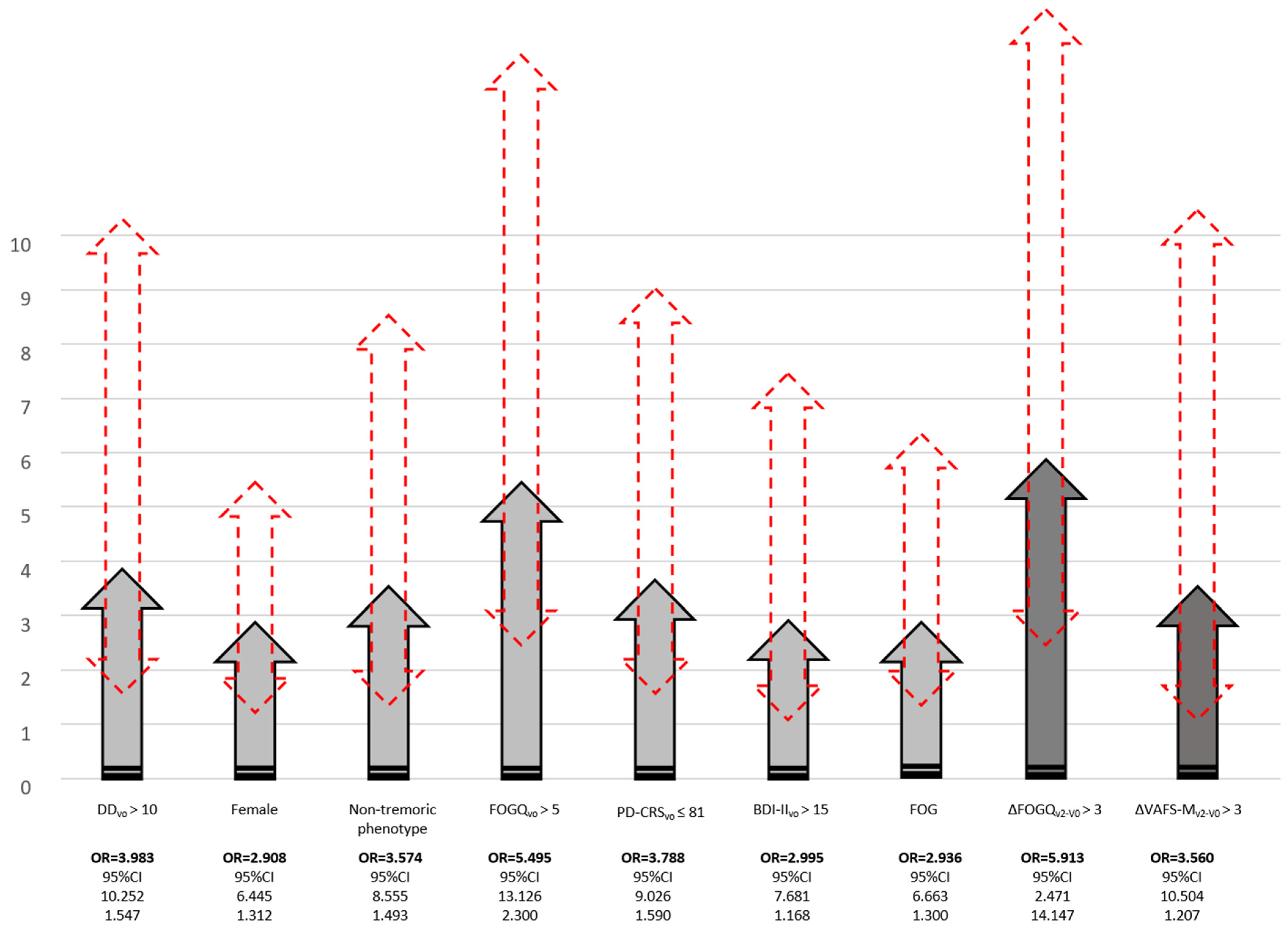
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Financial Disclosures
Appendix A
| Name (Last Name, First Name) | Location | Role | Contribution |
| Astrid Adarmes, Daniela | Hospital Universitario Virgen del Rocío, Sevilla, Spain | Site investigator | Evaluation of participants and/or data management |
| Almeria, Marta | Hospital Universitari Mutua de Terrassa, Terrassa, Barcelona, Spain | Site investigator | Neuropsychologist; evaluation of participants |
| Alonso Losada, Maria Gema | Hospital Álvaro Cunqueiro, Complejo Hospitalario Universitario de Vigo (CHUVI), Vigo, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Alonso Cánovas, Araceli | Hospital Universitario Ramón y Cajal, Madrid, Spain | Site investigator | Evaluation of participants and/or data management |
| Alonso Frech, Fernando | Hospital Universitario Clínico San Carlos, Madrid, Spain | Site investigator | Evaluation of participants and/or data management |
| Alonso Redondo, Ruben | Hospital Universitario Lucus Augusti (HULA), Lugo, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Aneiros Díaz, Ángel | Complejo Hospitalario Universitario de Ferrol (CHUF), Ferrol, A Coruña, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Álvarez, Ignacio | Hospital Universitari Mutua de Terrassa, Terrassa, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Álvarez Sauco, María | Hospital General Universitario de Elche, Elche, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Arnáiz, Sandra | Complejo Asistencial Universitario de Burgos, Burgos, Spain | Site investigator | Evaluation of participants and/or data management |
| Arribas, Sonia | Hospital Universitari Mutua de Terrassa, Terrassa, Barcelona, Spain | Site investigator | Neuropsychologist; evaluation of participants |
| Ascunce Vidondo, Arancha | Complejo Hospitalario de Navarra, Pamplona, Spain | Site investigator | Evaluation of participants and/or data management |
| Aguilar, Miquel | Hospital Universitari Mutua de Terrassa, Terrassa, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Ávila Rivera, Maria Asunción | Consorci Sanitari Integral, Hospital General de L’Hospitalet, L’Hospitalet de Llobregat, Barcelona, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Bernardo Lambrich, Noemí | Hospital de Tortosa Verge de la Cinta (HTVC), Tortosa, Tarragona, Spain | Site investigator | Evaluation of participants and/or data management |
| Bejr-Kasem, Helena | Hospital de Sant Pau, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Blázquez Estrada, Marta | Hospital Universitario Central de Asturias, Oviedo, Spain | Site investigator | Evaluation of participants and/or data management |
| Botí González, Maria Ángeles | Hospital Universitari Mutua de Terrassa, Terrassa, Barcelona, Spain | Site investigator | Neuropsychologist; evaluation of participants |
| Borrué, Carmen | Hospital Infanta Sofía, Madrid, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Buongiorno, Maria Teresa | Hospital Universitari Mutua de Terrassa, Terrassa, Barcelona, Spain | Site investigator | Nurse study coordinator |
| Cabello González, Carolina | Complejo Hospitalario de Navarra, Pamplona, Spain | Site investigator | Scheduling of evaluations |
| Cabo López, Iria | Complejo Hospitalario Universitario de Pontevedra (CHOP), Pontevedra, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Caballol, Nuria | Consorci Sanitari Integral, Hospital Moisés Broggi, Sant Joan Despí, Barcelona, Spain. | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Cámara Lorenzo, Ana | Hospital Clínic de Barcelona, Barcelona, Spain | Site investigator | Nurse study coordinator |
| Canfield Medina, Héctor | Complejo Hospitalario Universitario de Ferrol (CHUF), Ferrol, A Coruña, Spain | Site investigator | Evaluation of participants and/or data management |
| Carrillo, Fátima | Hospital Universitario Virgen del Rocío, Sevilla, Spain | Site investigator | Evaluation of participants and/or data management |
| Carrillo Padilla, Francisco José | Hospital Universitario de Canarias, San Cristóbal de la Laguna, Santa Cruz de Tenerife, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Casas, Elena | Complejo Asistencial Universitario de Burgos, Burgos, Spain | Site investigator | Evaluation of participants and/or data management |
| Catalán, Maria José | Hospital Universitario Clínico San Carlos, Madrid, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Clavero, Pedro | Complejo Hospitalario de Navarra, Pamplona, Spain | Site investigator | Evaluation of participants and/or data management |
| Cortina Fernández, A | Complejo Hospitalario Universitario de Ferrol (CHUF), Ferrol, A Coruña, Spain | Site investigator | Coordination of blood extractions |
| Cosgaya, Marina | Hospital Clínic de Barcelona, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Cots Foraster, Anna | Institut d’Assistència Sanitària (IAS)—Instituí Cátala de la Salud. Girona, Spain | Site investigator | Evaluation of participants and/or data management |
| Crespo Cuevas, Ane | Hospital del Mar, Barcelona, Spain. | Site investigator | Evaluation of participants and/or data management |
| Cubo, Esther | Complejo Asistencial Universitario de Burgos, Burgos, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| De Deus Fonticoba, Teresa | Complejo Hospitalario Universitario de Ferrol (CHUF), Ferrol, A Coruña, Spain | Site investigator | Nurse study coordinatorEvaluation of participants and/or data management |
| De Fábregues-Boixar, Oriol | Hospital Universitario Vall d’Hebron, Barcelona, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Díez Fairen, M | Hospital Universitari Mutua de Terrassa, Terrassa, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Dotor García-Soto, Julio | Hospital Universitario Virgen Macarena, Sevilla, Spain | Site investigator/PI | Evaluation of participants and/or data management |
| Erro, Elena | Complejo Hospitalario de Navarra, Pamplona, Spain | Site investigator | Evaluation of participants and/or data management |
| Escalante, Sonia | Hospital de Tortosa Verge de la Cinta (HTVC), Tortosa, Tarragona, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Estelrich Peyret, Elena | Institut d’Assistència Sanitària (IAS)—Instituí Cátala de la Salud. Girona, Spain | Site investigator | Evaluation of participants and/or data management |
| Fernández Guillán, Noelia | Complejo Hospitalario Universitario de Ferrol (CHUF), Ferrol, A Coruña, Spain | Site investigator | Neuroimaging studies |
| Gámez, Pedro | Complejo Asistencial Universitario de Burgos, Burgos, Spain | Site investigator | Evaluation of participants and/or data management |
| Gallego, Mercedes | Hospital La Princesa, Madrid, Spain | Site investigator | Evaluation of participants and/or data management |
| García Caldentey, Juan | Centro Neurológico Oms 42, Palma de Mallorca, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| García Campos, Cristina | Hospital Universitario Virgen Macarena, Sevilla, Spain | Site investigator | Evaluation of participants and/or data management |
| García Moreno, Jose Manuel | Hospital Universitario Virgen Macarena, Sevilla, Spain | Site investigator/PI (until MAR/21) | Coordination at the center Evaluation of participants and/or data management |
| Gastón, Itziar | Complejo Hospitalario de Navarra, Pamplona, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Gómez Garre, María del Pilar | Hospital Universitario Virgen del Rocío, Sevilla, Spain | Site investigator | Genetic studies coordination |
| Gómez Mayordomo, Víctor | Hospital Clínico San Carlos, Madrid, Spain | Site investigator | Evaluation of participants and/or data management |
| González Aloy, Javier | Institut d’Assistència Sanitària (IAS)—Instituí Cátala de la Salud. Girona, Spain | Site investigator | Evaluation of participants and/or data management |
| González Aramburu, Isabel | Hospital Universitario Marqués de Valdecilla, Santander, Spain | Site investigator | Evaluation of participants and/or data management |
| González Ardura, Jessica | Hospital Universitario Lucus Augusti (HULA), Lugo, Spain | Site investigator/PI (until FEB/21) | Evaluation of participants and/or data management |
| González García, Beatriz | Hospital La Princesa, Madrid, Spain | Site investigator | Nurse study coordinator |
| González Palmás, Maria Josefa | Complejo Hospitalario Universitario de Pontevedra (CHOP), Pontevedra, Spain | Site investigator | Evaluation of participants and/or data management |
| González Toledo, Gabriel Ricardo | Hospital Universitario de Canarias, San Cristóbal de la Laguna, Santa Cruz de Tenerife, Spain | Site investigator | Evaluation of participants and/or data management |
| Golpe Díaz, Ana | Complejo Hospitalario Universitario de Ferrol (CHUF), Ferrol, A Coruña, Spain | Site investigator | Laboratory analysis coordination |
| Grau Solá, Mireia | Consorci Sanitari Integral, Hospital Moisés Broggi, Sant Joan Despí, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Guardia, Gemma | Hospital Universitari Mutua de Terrassa, Terrassa, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Hernández Vara, Jorge | Hospital Universitario Vall d’Hebron, Barcelona, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Horta Barba, Andrea | Hospital de Sant Pau, Barcelona, Spain | Site investigator | Neuropsychologist; evaluation of participants |
| Idoate Calderón, Daniel | Complejo Hospitalario Universitario de Pontevedra (CHOP), Pontevedra, Spain | Site investigaor | Neuropsychologist; evaluation of participants |
| Infante, Jon | Hospital Universitario Marqués de Valdecilla, Santander, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Jesús, Silvia | Hospital Universitario Virgen del Rocío, Sevilla, Spain | Site investigator | Evaluation of participants and/or data management |
| Kulisevsky, Jaime | Hospital de Sant Pau, Barcelona, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Kurtis, Mónica | Hospital Ruber Internacional, Madrid, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Labandeira, Carmen | Hospital Álvaro Cunqueiro, Complejo Hospitalario Universitario de Vigo (CHUVI), Vigo, Spain | Site investigator | Evaluation of participants and/or data management |
| Labrador Espinosa, Miguel Ángel | Hospital Universitario Virgen del Rocío, Sevilla, Spain | Site investigator | Neuroimaging data analysis |
| Lacruz, Francisco | Complejo Hospitalario de Navarra, Pamplona, Spain | Site investigator | Evaluation of participants and/or data management |
| Lage Castro, Melva | Complejo Hospitalario Universitario de Pontevedra (CHOP), Pontevedra, Spain | Site investigator | Evaluation of participants and/or data management |
| Lastres Gómez, Sonia | Complejo Hospitalario Universitario de Pontevedra (CHOP), Pontevedra, Spain | Site investigator | Neuropsychologist; evaluation of participants |
| Legarda, Inés | Hospital Universitario Son Espases, Palma de Mallorca, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| López Ariztegui, Nuria | Complejo Hospitalario de Toledo, Toledo, Spain | Site investigator/PI | Evaluation of participants and/or data management |
| López Díaz, Luis Manuel | Hospital Da Costa de Burela, Lugo, Spain | Site investigator | Evaluation of participants and/or data management |
| López Manzanares, Lydia | Hospital La Princesa, Madrid, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| López Seoane, Balbino | Complejo Hospitalario Universitario de Ferrol (CHUF), Ferrol, A Coruña, Spain | Site investigator | Neuroimaging studies |
| Lucas del Pozo, Sara | Hospital Universitario Vall d’Hebron, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Macías, Yolanda | Fundación Hospital de Alcorcón, Madrid, Spain | Site investigator | Evaluation of participants and/or data management |
| Mata, Marina | Hospital Infanta Sofía, Madrid, Spain | Site investigator | Evaluation of participants and/or data management |
| Martí Andres, Gloria | Hospital Universitario Vall d’Hebron, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Martí, Maria José | Hospital Clínic de Barcelona, Barcelona, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Martínez Castrillo, Juan Carlos | Hospital Universitario Ramón y Cajal, Madrid, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Martinez-Martin, Pablo | Centro Nacional de Epidemiología y CIBERNED, Instituto de Salud Carlos III. Madrid | Collaborator in statistical and methods analysis | Methods and statistical reviewer |
| McAfee, Darrian | University of Maryland School of Medicine | Collaborator in English style | English style reviewer |
| Meitín, Maria Teresa | Hospital Da Costa de Burela, Lugo, Spain | Site investigator | Evaluation of participants and/or data management |
| Menéndez González, Manuel | Hospital Universitario Central de Asturias, Oviedo, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Méndez del Barrio, Carlota | Hospital Universitario Virgen del Rocío, Sevilla, Spain | Site investigator | Evaluation of participants and/or data management |
| Mir, Pablo | Hospital Universitario Virgen del Rocío, Sevilla, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Miranda Santiago, Javier | Complejo Asistencial Universitario de Burgos, Burgos, Spain | Site investigator | Evaluation of participants and/or data management |
| Morales Casado, Maria Isabel | Complejo Hospitalario de Toledo, Toledo, Spain. | Site investigator | Evaluation of participants and/or data management |
| Moreno Diéguez, Antonio | Complejo Hospitalario Universitario de Ferrol (CHUF), Ferrol, A Coruña, Spain | Site investigator | Neuroimaging studies |
| Nogueira, Víctor | Hospital Da Costa de Burela, Lugo, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Novo Amado, Alba | Complejo Hospitalario Universitario de Ferrol (CHUF), Ferrol, A Coruña, Spain | Site investigator | Neuroimaging studies |
| Novo Ponte, Sabela | Hospital Universitario Puerta de Hierro, Madrid, Spain. | Site investigator | Evaluation of participants and/or data management |
| Ordás, Carlos | Hospital Rey Juan Carlos, Madrid, Spain, Madrid, Spain. | Site Investigator | Evaluation of participants and/or data management |
| Pagonabarraga, Javier | Hospital de Sant Pau, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Pareés, Isabel | Hospital Ruber Internacional, Madrid, Spain | Site investigator | Evaluation of participants and/or data management |
| Pascual-Sedano, Berta | Hospital de Sant Pau, Barcelona, Spain | Site Investigator | Evaluation of participants and/or data management |
| Pastor, Pau | Hospital Universitari Mutua de Terrassa, Terrassa, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Pérez Fuertes, Aída | Complejo Hospitalario Universitario de Ferrol (CHUF), Ferrol, A Coruña, Spain | Site investigator | Blood analysis |
| Pérez Noguera, Rafael | Hospital Universitario Virgen Macarena, Sevilla, Spain | Site investigator | Evaluation of participants and/or data management |
| Planas-Ballvé, Ana | Consorci Sanitari Integral, Hospital Moisés Broggi, Sant Joan Despí, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Planellas, Lluís | Hospital Clínic de Barcelona, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Prats, Marian Ángeles | Institut d’Assistència Sanitària (IAS)—Instituí Cátala de la Salud. Girona, Spain | Site investigator | Evaluation of participants and/or data management |
| Prieto Jurczynska, Cristina | Hospital Rey Juan Carlos, Madrid, Spain, Madrid, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Puente, Víctor | Hospital del Mar, Barcelona, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Pueyo Morlans, Mercedes | Hospital Universitario de Canarias, San Cristóbal de la Laguna, Santa Cruz de Tenerife, Spain | Site investigator | Evaluation of participants and/or data management |
| Puig Daví, Arnau | Hospital de Sant Pau, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Redondo, Nuria | Hospital La Princesa, Madrid, Spain | Site Investigator | Evaluation of participants and/or data management |
| Rodríguez Méndez, Luisa | Complejo Hospitalario Universitario de Ferrol (CHUF), Ferrol, A Coruña, Spain | Site investigator | Blood analysis |
| Rodríguez Pérez, Amparo Belén | Hospital General Universitario de Elche, Elche, Spain | Site investigator | Evaluation of participants and/or data management |
| Roldán, Florinda | Hospital Universitario Virgen del Rocío, Sevilla, Spain | Site investigator | Neuroimaging studies |
| Ruíz de Arcos, María | Hospital Universitario Virgen Macarena, Sevilla, Spain. | Site investigator | Evaluation of participants and/or data management |
| Ruíz Martínez, Javier | Hospital Universitario Donostia, San Sebastián, Spain | Site investigator | Evaluation of participants and/or data management |
| Sánchez Alonso, Pilar | Hospital Universitario Puerta de Hierro, Madrid, Spain | Site investigator | Evaluation of participants and/or data management |
| Sánchez-Carpintero, Macarena | Complejo Hospitalario Universitario de Ferrol (CHUF), Ferrol, A Coruña, Spain | Site investigator | Neuroimaging studies |
| Sánchez Díez, Gema | Hospital Universitario Ramón y Cajal, Madrid, Spain | Site investigator | Evaluation of participants and/or data management |
| Sánchez Rodríguez, Antonio | Hospital Universitario Marqués de Valdecilla, Santander, Spain | Site investigator | Evaluation of participants and/or data management |
| Santacruz, Pilar | Hospital Clínic de Barcelona, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Santos García, Diego | CHUAC, Complejo Hospitalario Universitario de A Coruña | Coordinator of the Project | Coordination of the COPPADIS-2015 |
| Segundo Rodríguez, José Clemente | Complejo Hospitalario de Toledo, Toledo, Spain | Site investigator | Evaluation of participants and/or data management |
| Seijo, Manuel | Complejo Hospitalario Universitario de Pontevedra (CHOP), Pontevedra, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Sierra, María | Hospital Universitario Marqués de Valdecilla, Santander, Spain | Site investigator | Evaluation of participants and/or data management |
| Solano, Berta | Institut d’Assistència Sanitària (IAS)—Instituí Cátala de la Salud. Girona, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Suárez Castro, Ester | Complejo Hospitalario Universitario de Ferrol (CHUF), Ferrol, A Coruña, Spain | Site investigator | Evaluation of participants and/or data management |
| Tartari, Juan Pablo | Hospital Universitari Mutua de Terrassa, Terrassa, Barcelona, Spain | Site investigator | Evaluation of participants and/or data management |
| Valero, Caridad | Hospital Arnau de Vilanova, Valencia, Spain | Site investigator | Evaluation of participants and/or data management |
| Vargas, Laura | Hospital Universitario Virgen del Rocío, Sevilla, Spain | Site investigator | Evaluation of participants and/or data management |
| Vela, Lydia | Fundación Hospital de Alcorcón, Madrid, Spain | Site investigator/PI | Coordination at the center Evaluation of participants and/or data management |
| Villanueva, Clara | Hospital Universitario Clínico San Carlos, Madrid, Spain | Site investigator | Evaluation of participants and/or data management |
| Vives, Bárbara | Hospital Universitario Son Espases, Palma de Mallorca, Spain | Site investigator | Evaluation of participants and/or data management |
| Villar, Maria Dolores | Hospital Universitario de Canarias, San Cristóbal de la Laguna, Santa Cruz de Tenerife, Spain | Site investigator | Evaluation of participants and/or data management |
References
- Covinsky, K.E.; Palmer, R.M.; Fortinsky, R.H.; Counsell, S.R.; Stewart, A.L.; Rn, D.K.; Ma, C.J.B.; Landefeld, C.S. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: Increased vulnerability with age. J. Am. Geriatr. Soc. 2003, 51, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Macleod, A.D.; Dalen, I.; Tysnes, O.B.; Larsen, J.P.; Counsell, C.E. Development and validation of prognostic survival models in newly diagnosed Parkinson’s disease. Mov. Disord. 2017, 33, 108–116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bjornestad, A.; Tysnes, O.-B.; Larsen, J.P.; Alves, G. Reliability of three disability scales for detection of independence loss in Parkinson’s disease. Parkinsons Dis. 2016, 2016, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Nieuwboer, A.; Kwakkel, G.; Rochester, L.; Jones, D.; van Wegen, E.; Willems, A.M.; Chavret, F.; Hetherington, V.; Baker, K.; Lim, I. Cueing training in the home improves gait-related mobility in Parkinson’s disease: The RESCUE trial. J. Neurol. Neurosurg. Psychiatry 2007, 78, 134–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chandler, C.; Folse, H.; Gal, P.; Chavan, A.; Proskorovsky, I.; Franco-Villalobos, C.; Wang, Y.; Ward, A. Modeling long-term health and economic implications of new treatment strategies for Parkinson’s disease: An individual patient simulation study. J. Mark. Access Health Policy 2021, 9, 1922163. [Google Scholar] [CrossRef]
- Alves, G.; Wentzel-Larsen, T.; Aarsland, D.; Larsen, J.P. Progression of motor impairment and disability in Parkinson disease: A population-based study. Neurology 2005, 65, 1436–1441. [Google Scholar] [CrossRef]
- Muslimovic, D.; Post, B.; Speelman, J.D.; Schmand, B.; De Haan, R.J. For the CARPA Study Group Determinants of disability and quality of life in mild to moderate Parkinson disease. Neurology 2008, 70, 2241–2247. [Google Scholar] [CrossRef]
- Macleod, A.D.; Counsell, C.E. Predictors of functional dependency in Parkinson’s disease. Mov. Disord. 2016, 31, 1482–1488. [Google Scholar] [CrossRef] [Green Version]
- Bjornestad, A.; Tysnes, O.B.; Larsen, J.P.; Alves, G. Loss of independence in early Parkinson disease: A 5-year population-based incident cohort study. Neurology 2016, 87, 1599–1606. [Google Scholar] [CrossRef]
- MacLeod, A.D.; Grieve, J.W.K.; Counsell, C.E. A systematic review of loss of independence in Parkinson’s disease. J. Neurol. 2015, 263, 1–10. [Google Scholar] [CrossRef]
- Santos-García, D.; Mir, P.; Cubo, E.; Vela, L.; Rodríguez-Oroz, M.C.; Martí, M.J.; Arbelo, J.M.; Infante, J.; Kulisevsky, J.; Martínez-Martín, P.; et al. COPPADIS-2015 (COhort of Patients with Parkinson’s DIsease in Spain, 2015): An ongoing global Parkinson’s disease project about disease progression with more than 1000 subjects included. Results from the baseline evaluation. Eur. J. Neurol. 2019, 26, 1399–1407. [Google Scholar] [CrossRef]
- Santos-García, D.; Mir, P.; Cubo, E.; Vela, L.; Rodríguez-Oroz, M.C.; Martí, M.J.; Arbelo, J.M.; Infante, J.; Kulisevsky, J.; Martínez-Martín, P.; et al. COPPADIS-2015 (COhort of Patients with PArkinson’s DIsease in Spain, 2015), a global–clinical evaluations, serum biomarkers, genetic studies and neuroimaging-prospective, multicenter, non-interventional, long-term study on Parkinson’s disease progression. BMC Neurol. 2016, 16, 26. [Google Scholar]
- Schwab, R.S.; England, A.C. In Third Symposium on Parkinson’s Disease; And, E., Livingstone, S., Eds.; Sage: Edinburgh, UK, 1969; pp. 152–157. [Google Scholar]
- Shulman, L.M.; Armstrong, M.; Ellis, T.; Gruber-Baldini, A.; Horak, F.; Nieuwboer, A.; Parashos, S.; Post, B.; Rogers, M.; Siderowf, A.; et al. Disability Rating Scales in Parkinson’s Disease: Critique and Recommendations. Mov. Disord. 2016, 3, 1455–1565. [Google Scholar] [CrossRef]
- Santos-García, D.; de Deus-Fonticoba, T.; Suárez Castro, E.; Aneiros Díaz, M.Á.; Feal-Painceiras, M.J.; Paz-González, J.M.; García-Sancho, C.; Jesús, S.; Mir, P.; Planellas, L.; et al. The impact of freezing of gait on functional dependency in Parkinson’s disease with regard to motor phenotype. Neurol Sci. 2020, 41, 2883–2892. [Google Scholar] [CrossRef] [PubMed]
- Schade, S.; Mollenhauer, B.; Trenkwalder, C. Levodopa Equivalent Dose Conversion Factors: An Updated Proposal Including Opicapone and Safinamide. Mov. Disord. Clin. Pract. 2020, 7, 343–345. [Google Scholar] [CrossRef] [PubMed]
- Simuni, T.; Caspell-Garcia, C.; Coffey, C.S.; Weintraub, D.; Mollenhauer, B.; Lasch, S.; Tanner, C.M.; Jennings, D.; Kieburtz, K.; Chahine, L.; et al. Baseline prevalence and longitudinal evolution of non-motor symptoms in early Parkinson’s disease: The PPMI cohort. J. Neurol. Neurosurg. Psychiatry 2017, 89, 78–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stebbins, G.T.; Goetz, C.G.; Burn, D.J.; Jankovic, J.; Khoo, T.K.; Tilley, B.C. How to identify tremor dominant and postural instability/gait difficulty groups with the movement disorder society unified Parkinson’s disease rating scale: Comparison with the unified Parkinson’s disease rating scale. Mov. Disord. 2013, 28, 668–670. [Google Scholar] [CrossRef]
- Amboni, M.; Stocchi, F.; Abbruzzese, G.; Morgante, L.; Onofrj, M.; Ruggieri, S.; Tinazzi, M.; Zappia, M.; Attar, M.; Colombo, D.; et al. Prevalence and associated features of self-reported freezing of gait in Parkinson disease: The DEEP FOG study. Park. Relat. Disord. 2015, 21, 644–649. [Google Scholar] [CrossRef] [PubMed]
- Santos-García, D.; de Deus Fonticoba, T.; Suárez Castro, E.; Aneiros Díaz, A.; Paz González, J.M.; Feal Panceiras, M.J.; García Sancho, C.; Jesús, S.; Mir, P.; Aguilar, M.; et al. High ultrasensitive serum C-reactive protein may be related to freezing of gait in Parkinson’s disease patients. J. Neural Transm. 2019, 126, 1599–1608. [Google Scholar] [CrossRef]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, progression, and mortality. Neurology 1967, 17, 427–442. [Google Scholar] [CrossRef] [Green Version]
- Hoehn, M.M.M. Result of chronic levodopa therapy and its modification by bromocriptine in Parkinson’s disease. Acta Neurol. Scand. 2009, 71, 97–106. [Google Scholar] [CrossRef]
- Chia, L.-G.; Liu, L.-H. Parkinson’s disease in Taiwan: An analysis of 215 patients. Neuroepidemiology 1992, 11, 113–120. [Google Scholar] [CrossRef]
- Hely, M.A.; Reid, W.G.J.; Adena, M.A.; Halliday, G.M.; Morris, J.G.L. The Sydney multicenter study of Parkinson’s disease: The inevitability of dementia at 20 years. Mov. Disord. 2008, 23, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Velseboer, D.C.; Broeders, M.; Post, B.; van Geloven, N.; Speelman, J.D.; Schmand, B.; de Haan, R.J.; de Bie, R.M.A.; on behalf of the CARPA Study Group. Prognostic factors of motor impairment, disability, and quality of life in newly diagnosed PD. Neurology 2013, 80, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Auyeung, M.; Tsoi, T.H.; Mok, V.; Cheung, C.M.; Lee, C.N.; Li, R.; Yeung, E. Ten year survival and outcomes in a prospective cohort of new onset Chinese Parkinson’s disease patients. J. Neurol. Neurosurg. Psychiatry 2012, 83, 607–611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scigliano, G.; Musicco, M.; Soliveri, P.; Girotti, F.; Giovannini, P.; Fetoni, V.; Caraceni, T. Progression and prognosis in Parkinson’s disease in relation to concomitant cerebral or peripheral vasculopathy. Adv. Neurol. 1996, 69, 305–309. [Google Scholar] [PubMed]
- Tison, F.; Barberger-Gateau, P.; Dubroca, B.; Henry, P.; Dartigues, J.F. Dependency in Parkinson’s disease: A population-based survey in nondemented elderly subjects. Mov. Disord. 1997, 2, 910–915. [Google Scholar] [CrossRef]
- Hariz, G.M.; Forsgren, L. Activities of daily living and quality of life in persons with newly diagnosed Parkinson’s disease according to subtype of disease, and in comparison to healthy controls. Acta Neurol. Scand. 2011, 123, 20–27. [Google Scholar] [CrossRef]
- Santos-García, D.; de Deus, T.; Cores, C.; Canfield, H.; González, J.P.; Miró, C.M.; Aymerich, L.V.; Suárez, E.; Jesús, S.; Aguilar, M.; et al. Predictors of Global Non-Motor Symptoms Burden Progression in Parkinson’s Disease. Results from the COPPADIS Cohort at 2-Year Follow-Up. J. Pers. Med. 2021, 11, 626. [Google Scholar] [CrossRef]
- Jasinska-Myga, B.; Heckman, M.G.; Wider, C.; Putzke, J.D.; Wszolek, Z.K.; Uitti, R.J. Loss of ability to work and ability to live independently in Parkinson’s disease. Parkinsonism Relat. Disord. 2012, 18, 130–135. [Google Scholar] [CrossRef] [Green Version]
- Guillard, A.; Chastang, C.; Fenelon, G. Long-term study of 416 cases of Parkinson disease. Prognostic factors and therapeutic implications. Rev. Neurol. 1986, 142, 207–214. [Google Scholar] [PubMed]
- Ren, J.; Hua, P.; Li, Y.; Pan, C.; Yan, L.; Yu, C.; Zhang, L.; Xu, P.; Zhang, M.; Liu, W. Comparison of Three Motor Subtype Classifications in de novo Parkinson’s Disease Patients. Front. Neurol. 2020, 11, 601225. [Google Scholar] [CrossRef] [PubMed]
- Sperens, M.; Georgiev, D.; Eriksson Domellöf, M.; Forsgren, L.; Hamberg, K.; Hariz, G.M. Activities of daily living in Parkinson’s disease: Time/gender perspective. Acta Neurol. Scand. 2020, 141, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Georgiev, D.; Hamberg, K.; Hariz, M.; Forsgren, L.; Hariz, G.M. Gender differences in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 2007, 78, 819–824. [Google Scholar]
- Martinez-Martin, P.A.P.; Pecurariu, C.F.; Odin, C.A.; van Hilten, J.; Antonini, A.; Rojo-Abuin, J.M.; Borges, V.; Trenkwalder, C.; Aarsland, D.; Brooks, D.; et al. Gender-related differences in the burden of non-motor symptoms in Parkinson’s disease. J. Neurol. 2012, 259, 1639–1647. [Google Scholar] [CrossRef] [PubMed]
- Santos García, D.; de Deus Fonticoba, T.; Cores, C.; COPPADIS Study Group. Predictors of Clinically Significant Quality of Life Impairment in Parkinson’s Disease. NPJ Parkinson Dis. 2021. accepted. [Google Scholar]
- Stocchi, F.; Abbruzzese, G.; Ceravolo, R.; Cortelli, P.; D’Amelio, M.; De Pandis, M.F.; Fabbrini, G.; Pacchetti, C.; Pezzoli, G.; Tessitore, A.; et al. Prevalence of fatigue in Parkinson disease and its clinical correlates. Neurology 2014, 83, 215–220. [Google Scholar] [CrossRef]
- Cole, S.A.; Woodard, J.L.; Juncos, J.L.; Kogos, J.L.; Youngstrom, E.A.; Watts, R.L. Depression and disability in Parkinson’s disease. J. Neuropsychiatry Clin. Neurosci. 1996, 8, 20–25. [Google Scholar]
- Bowman, T.; Gervasoni, E.; Parelli, R.; Jonsdottir, J.; Ferrarin, M.; Cattaneo, D.; Carpinella, I. Predictors of mobility domain of health-related quality of life after rehabilitation in Parkinson’s disease: A pilot study. Arch. Physiother. 2018, 8, 10. [Google Scholar] [CrossRef]
- Ginis, P.; Nieuwboer, A.; Dorfman, M.; Ferrari, A.; Gazit, E.; Canning, C.G.; Rocchi, L.; Chiari, L.; Hausdorff, J.M.; Mirelman, A. Feasibility and effects of home-based smartphone-delivered automated feedback training for gait in people with Parkinson’s disease: A pilot randomized controlled trial. Parkinsonism Relat. Disord. 2016, 22, 28–34. [Google Scholar] [CrossRef] [Green Version]
- Ginis, P.; Nackaerts, E.; Nieuwboer, A.; Heremans, E. Cueing for people with Parkinson’s disease with freezing of gait: A narrative review of the state-of-the-art and novel perspectives. Ann. Phys. Rehabil. Med. 2018, 61, 407–413. [Google Scholar] [CrossRef]
- Tosserams, A.; Wit, L.; Sturkenboom, I.H.; Nijkrake, M.J.; Bloem, B.R.; Nonnekes, J. Perception and Use of Compensation Strategies for Gait Impairment by Persons With Parkinson Disease. Neurology 2021. [Google Scholar] [CrossRef] [PubMed]
- A King, L.; Horak, F.B. Delaying Mobility Disability in People With Parkinson Disease Using a Sensorimotor Agility Exercise Program. Phys. Ther. 2009, 89, 384–393. [Google Scholar] [CrossRef]
- Ou, R.; Yang, J.; Cao, B.; Wei, Q.; Chen, K.; Chen, X.; Zhao, B.; Wu, Y.; Song, W.; Shang, H. Progression of non-motor symptoms in Parkinson’s disease among different age populations: A two-year follow-up study. J. Neurol. Sci. 2016, 360, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Prakash, K.M.; Nadkarni, N.V.; Lye, W.K.; Yong, M.H.; Chew, L.M.; Tan, E.K. A longitudinal study of non-motor symptom burden in Parkinson’s disease after a transition to expert care. Parkinsonism Relat. Disord. 2015, 21, 843–847. [Google Scholar] [CrossRef] [PubMed]
- Antonini, A.; Barone, P.; Marconi, R.; Morgante, L.; Zappulla, S.; Pontieri, F.E.; Ramat, S.; Ceravolo, M.G.; Meco, G.; Cicarelli, G.; et al. The progression of non-motor symptoms in Parkinson’s disease and their contribution to motor disability and quality of life. J. Neurol. 2012, 259, 2621–2631. [Google Scholar] [CrossRef] [PubMed]
- Santos García, D.; de Deus Fonticoba, T.; Suárez Castro, E.; Borrué, C.; Mata, M.; Solano Vila, B.; Cots Foraster, A.; Álvarez Sauco, M.; Rodríguez Pérez, A.B.; Vela, L.; et al. Non-motor symptoms burden, mood, and gait problems are the most significant factors contributing to a poor quality of life in non-demented Parkinson’s disease patients: Results from the COPPADIS Study Cohort. Parkinsonism Relat. Disord. 2019, 66, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Mancini, M.; Bloem, B.R.; Horak, F.B.; Lewis, S.J.; Nieuwboer, A.; Nonnekes, J. Clinical and methodological challenges for assessing freezing of gait: Future perspectives. Mov. Disord. 2019, 34, 783–790. [Google Scholar] [CrossRef] [PubMed]

| S&E-ADLSV2—S&E-ADLSV0 | N | p | |
|---|---|---|---|
| Age at baseline | −0.017 | 507 | 0.704 |
| Disease duration (at V0) | −0.023 | 487 | 0.609 |
| N. of non-antipark. drugs (at V0) | 0.002 | 507 | 0.965 |
| Change at V2 (V2 vs. V0) | |||
| LEDD | |||
| Number of non-antipark. Drugs | −0.067 | 483 | 0.143 |
| UPDRS-III (OFF) | −0.250 | 441 | <0.0001 |
| UPDRS-IV | −0.155 | 485 | 0.001 |
| FOGQ | −0.328 | 502 | <0.0001 |
| PD-CRS | 0.003 | 494 | 0.955 |
| NMSS | −0.243 | 499 | <0.0001 |
| BDI-II | −0.214 | 500 | <0.0001 |
| PDSS | 0.168 | 501 | <0.0001 |
| QUIP-RS | −0.033 | 450 | 0.482 |
| NPI | −0.236 | 389 | <0.0001 |
| VAS-PAIN | −0.148 | 497 | 0.001 |
| VASF–physical | −0.152 | 497 | 0.001 |
| VASF–mental | −0.199 | 497 | <0.0001 |
| PDQ-39SI | −0.407 | 499 | <0.0001 |
| PQ-10 | 0.137 | 497 | 0.002 |
| EUROHIS-QOL8 | 0.193 | 501 | <0.0001 |
| All Sample (N = 507) | Functional Independency (N = 422) | Functional Dependency (N = 85) | p | |
|---|---|---|---|---|
| Age at baseline | 62.63 ± 8.55 | 62.47 ± 8.41 | 63.41 ± 9.04 | 0.187 |
| Males (%) | 58.8 | 60.7 | 49.4 | 0.047 |
| Disease duration (at V0) | 5.5 ± 4.21 | 4.99 ± 3.59 | 8 ± 5.83 | <0.0001 |
| At V0 | ||||
| N. of non-antipark. drugs | 2.52 ± 2.38 | 2.33 ± 2.2 | 3.44 ± 2.94 | 0.002 |
| LEDD | 577.96 ± 382.76 | 537.56 ± 386.79 | 785.85 ± 498.27 | <0.0001 |
| UPDRS-III (OFF) | 22.56 ± 10.56 | 20.89 ± 10 | 27.98 ± 11.13 | <0.0001 |
| UPDRS-IV | 2 ± 2.41 | 1.63 ± 2.03 | 3.87 ± 3.21 | <0.0001 |
| FOGQ | 3.74 ± 4.67 | 2.89 ± 3.87 | 7.87 ± 5.92 | <0.0001 |
| Non-tremotic motor phenotype (%) | 52.3 | 47.9 | 74.1 | <0.0001 |
| PD-CRS | 91.98 ± 15.75 | 93.64 ± 15.21 | 83.71 ± 15.84 | <0.0001 |
| NMSS | 44.72 ± 37.48 | 40.24 ± 35.82 | 66.94 ± 37.82 | <0.0001 |
| BDI-II | 8.27 ± 6.95 | 7.38 ± 6.45 | 12.67 ± 7.64 | <0.0001 |
| PDSS | 117.16 ± 24.53 | 118.9 ± 24.3 | 108.52 ± 23.95 | <0.0001 |
| QUIP-RS | 4.41 ± 8.65 | 4.26 ± 8.72 | 5.13 ± 8.32 | 0.213 |
| NPI | 5.78 ± 7.93 | 4.63 ± 0.23 | 11.23 ± 11.93 | <0.0001 |
| VAS-PAIN | 2.57 ± 2.91 | 2.34 ± 2.79 | 3.71 ± 3.25 | 0.001 |
| VASF–physical | 2.58 ± 2.91 | 2.35 ± 2.79 | 3.71 ± 3.25 | <0.0001 |
| VASF–mental | 2.08 ± 2.05 | 1.93 ± 2.4 | 2.78 ± 2.88 | 0.019 |
| PDQ-39SI | 16.54 ± 12.9 | 14.32 ± 11.24 | 27.52 ± 14.9 | <0.0001 |
| PQ-10 | 7.28 ± 1.53 | 7.43 ± 1.47 | 6.54 ± 1.63 | <0.0001 |
| EUROHIS-QOL8 | 3.78 ± 0.53 | 3.85 ± 0.52 | 3.44 ± 0.48 | <0.0001 |
| S&E-ADLS | 88.58 ± 10.19 | 90.62 ± 8.04 | 78.47 ± 13.31 | <0.0001 |
| At V2 | ||||
| To be receiving levodopa | 89.4 | 87.7 | 97.6 | 0.008 |
| To be receiving a dopamine agonist | 72.4 | 72.8 | 70.7 | 0.706 |
| To be receiving a MAO-B inhibitor | 76.9 | 77.8 | 72.3 | 0.274 |
| To be receiving a COMT inhibitor | 28.9 | 25.1 | 48.2 | <0.0001 |
| To practice regular execise | 74.3 | 76.8 | 61.9 | 0.004 |
| To assist regularly to a PD association | 16.3 | 16.2 | 16.7 | 0.913 |
| Change at V2 (V2 vs. V0) | ||||
| LEDD | +186.38 ± 326.51 | +175.19 ± 307.72 | +242.73 ± 405.89 | 0.102 |
| Number of non-antipark. Drugs | +0.55 ± 1.56 | +0.5. ± 1.53 | +0.83 ± 1.67 | 0.154 |
| UPDRS-III (OFF) | +3.3 ± 10.26 | +2.74 ± 3.76 | +5.92 ± 12.08 | 0.01 |
| UPDRS-IV | +0.67 ± 2.52 | +0.55 ± 2.19 | +1.23 ± 3.71 | 0.052 |
| FOGQ | +1.17 ± 4.16 | +0.78 ± 3.64 | +3.11 ± 5.75 | <0.0001 |
| PD-CRS | −1.83 ± 11.85 | −1.22 ± 10.99 | −4.89 ± 15.2 | 0.03 |
| NMSS | +8.29 ± 34.47 | +6.5 ± 31.68 | +17.11 ± 45.03 | 0.015 |
| BDI-II | +0.28 ± 7.72 | +0.34 ± 7.6 | −0.06 ± 8.34 | 0.663 |
| PDSS | +0.74 ± 26.09 | +0.83 ± 24.88 | +0.26 ± 31.59 | 0.893 |
| QUIP-RS | +0.05 ± 9.14 | +0.19 ± 8.28 | −0.59 ± 12.51 | 0.128 |
| NPI | +0.35 ± 8.82 | +0.26 ± 7.92 | +0.74 ± 12.04 | 0.325 |
| VAS-PAIN | +0.33 ± 3.33 | +0.29 ± 3.22 | +0.54 ± 3.8 | 0.554 |
| VASF–physical | +0.31 ± 2.97 | +0.27 ± 2.9 | +0.48 ± 3.33 | 0.367 |
| VASF–mental | +0.11 ± 2.84 | −0.03 ± 2.63 | +0.78 ± 3.65 | 0.038 |
| PDQ-39SI | +3.5 ± 12.1 | +2.2 ± 10.4 | +9.94 ± 16.96 | <0.0001 |
| PQ-10 | −0.15 ± 1.73 | −0.13 ± 1.71 | −0.26 ± 1.83 | 0.351 |
| EUROHIS-QOL8 | −0.02 ± 0.59 | −0.04 ± 0.57 | +0.09 ± 0.67 | 0.151 |
| S&E-ADLS | −4.32 ± 11.76 | −1.49 ± 8.32 | −18.35 ± 15.72 | <0.0001 |
| βa | βb | 95% ICa | 95% ICb | pa | pb | |
|---|---|---|---|---|---|---|
| At V0 (baseline) | ||||||
| Age | 0.000 | N. A. | −0.121–0.120 | N. A. | 0.996 | N. A. |
| Gender (female) | −0.048 | N. A. | −3.243–0.957 | N. A. | 0.285 | N. A. |
| Disease duration (at V0) | −0.107 | −0.121 | −0.556–−0.066 | −0.548–−0.051 | 0.013 | 0.018 |
| At V0 | ||||||
| Number of non-antipark. drugs | −0.028 | N. A. | −0.571–0.294 | N. A. | 0.529 | N. A. |
| LEDD | −0.049 | N. A. | −0.004–0.001 | N. A. | 0.275 | N. A. |
| UPDRS-III (OFF) | −0.049 | N. A. | −0.159–0.047 | N. A. | 0.283 | N. A. |
| UPDRS-IV | −0.122 | −0.297 | −1.008–−0.169 | −2.023–−0.929 | 0.006 | <0.0001 |
| FOGQ | −0.052 | N. A. | −0.433–0.044 | N. A. | 0.241 | N. A. |
| Non-tremoric motor phenotype | 0.035 | N. A. | −1.228–2.884 | N. A. | 0.429 | N. A. |
| PD-CRS | 0.093 | 0.16 | 0.004–0.135 | 0.057–0.180 | 0.038 | <0.0001 |
| NMSS | −0.047 | N. A. | −0.042–0.013 | N. A. | 0.291 | N. A. |
| BDI-II | −0.021 | N. A. | −0.183–0.114 | N. A. | 0.646 | N. A. |
| PDSS | −0.000 | N. A. | −0.042–0.042 | N. A. | 0.997 | N. A. |
| QUIP-RS | −0.014 | N. A. | −0.142– 0.104 | N. A. | 0.759 | N. A. |
| NPI | −0.114 | −0.092 | −0.315–−0.029 | −0.265–−0.010 | 0.018 | 0.035 |
| VAS-PAIN | −0.046 | N. A. | −0.537–0.169 | N. A. | 0.307 | N. A. |
| VASF–physical | −0.063 | −0.138 | −0.656–0.108 | −1.054–−0.161 | 0.159 | 0.008 |
| VASF–mental | −0.014 | N. A. | −0.476–0.349 | N. A. | 0.762 | N. A. |
| S&E-ADLS | −0.264 | −0.533 | −0.309–−0.174 | −0.713–−0.497 | <0.0001 | <0.0001 |
| At V2 | ||||||
| To be receiving levodopa | −0.050 | N. A. | −5.248–−1.420 | N. A. | 0.26 | N. A. |
| To be receiving a dopamine agonist | 0.035 | N. A. | −1.391–3.216 | N. A. | 0.437 | N. A. |
| To be receiving a MAO-B inhibitor | 0.057 | N. A. | −0.866–4.036 | N. A. | 0.204 | N. A. |
| To be receiving a COMT inhibitor | −0.059 | N. A. | −3.800–0.759 | N. A. | 0.191 | N. A. |
| To practice regular exercise | 0.094 | 0.128 | 0.173–4.908 | 1.313–5.958 | 0.036 | 0.002 |
| To assist regularly to a PD association | −0.010 | N. A. | −3.131–2.475 | N. A. | 0.818 | N. A. |
| Change at V2 (V2 vs. V0) | ||||||
| LEDD | −0.102 | N. A. | −0.007–−0.001 | N. A. | 0.025 | N. A. |
| Number of non-antipark. drugs | −0.138 | N. A. | −1.707–−0.384 | N. A. | 0.002 | N. A. |
| UPDRS-III (OFF) | −0.256 | −0.122 | −0.404–0.192 | −0.233–−0.043 | <0.0001 | 0.005 |
| UPDRS-IV | −0.149 | −0.154 | −1.103–−0.282 | −1.123–−0.272 | 0.001 | 0.001 |
| FOGQ | −0.405 | −0.316 | −1.436–−1.015 | −1.175–−0.671 | <0.0001 | <0.0001 |
| PD-CRS | 0.067 | N. A. | −0.021–0.155 | N. A. | 0.135 | N. A. |
| NMSS | −0.282 | N. A. | −0.125–−0.068 | N. A. | <0.0001 | N. A. |
| BDI-II | −0.264 | N. A. | −0.397–0.131 | N. A. | <0.0001 | N. A. |
| PDSS | 0.182 | N. A. | 0.043–0.121 | N. A. | <0.0001 | N. A. |
| QUIP-RS | −0.008 | N. A. | −0.133–0.111 | N. A. | 0.865 | N. A. |
| NPI | −0.168 | N. A. | −0.366–−0.095 | N. A. | 0.001 | N. A. |
| VAS-PAIN | −0.127 | N. A. | −0.758–−0.140 | N. A. | 0.004 | N. A. |
| VASF–physical | −0.116 | −0.140 | −0.804–−0.112 | −0.920–−0.178 | 0.01 | 0.004 |
| VASF–mental | −0.193 | N. A. | −1.156–−0.441 | N. A. | <0.0001 | N. A. |
| ORa | ORb | 95% ICa | 95% ICb | pa | pb | |
|---|---|---|---|---|---|---|
| At V0 (baseline) | ||||||
| Age | 1.013 | N. A. | 0.985–1.042 | N. A. | 0.354 | N. A. |
| Gender (female) | 1.602 | 2.334 | 1.003–2.559 | 1.127–4.833 | 0.049 | 0.022 |
| Disease duration (at V0) | 1.163 | 1.098 | 1.001–1.227 | 1.008–1.195 | <0.0001 | 0.031 |
| At V0 | ||||||
| Number of non-antipark. drugs | 1.19 | N. A. | 1.088–1.302 | N. A. | <0.0001 | N. A. |
| LEDD | 1.001 | N. A. | 1.001–1.002 | N. A. | <0.0001 | N. A. |
| UPDRS-III (OFF) | 1.063 | N. A. | 1.040–1.087 | N. A. | <0.0001 | N. A. |
| UPDRS-IV | 1.377 | N. A. | 1.255–1.511 | N. A. | <0.0001 | N. A. |
| FOGQ | 1.208 | 1.199 | 1.152–1.267 | 1.092–1.317 | <0.0001 | <0.0001 |
| Non-tremoric motor phenotype (%) | 3.119 | N. A. | 1.851–5.254 | N. A. | <0.0001 | N. A. |
| PD-CRS | 0.959 | 0.964 | 0.944–0.975 | 0.942–0.987 | <0.0001 | <0.0001 |
| NMSS | 1.016 | N. A. | 1.010–1.022 | N. A. | <0.0001 | N. A. |
| BDI-II | 1.101 | N. A. | 1.066–1.137 | N. A. | <0.0001 | N. A. |
| PDSS | 0.985 | N. A. | 0.997–0.993 | N. A. | 0.001 | N. A. |
| QUIP-RS | 1.011 | N. A. | 0.985–1.037 | N. A. | 0.409 | N. A. |
| NPI | 1.088 | 1.048 | 1.057–1.120 | 1.007–1.091 | <0.0001 | 0.02 |
| VAS-PAIN | 1.162 | N. A. | 1.076–1.254 | N. A. | <0.0001 | N. A. |
| VASF–physical | 1.268 | N. A. | 1.162–1.384 | N. A. | <0.0001 | N. A. |
| VASF–mental | 1.133 | N. A. | 1.038–1.236 | N. A. | 0.005 | N. A. |
| S&E-ADLS | 0.895 | 0.926 | 0.872–0.920 | 0.889–0.965 | <0.0001 | <0.0001 |
| At V2 | ||||||
| To be receiving levodopa | 5.77 | N. A. | 1.377–24.175 | N. A. | 0.016 | N. A. |
| To be receiving a dopamine agonist | 0.808 | N. A. | 0.533–1.515 | N. A. | 0.687 | N. A. |
| To be receiving a MAO-B inhibitor | 0.749 | N. A. | 0.439–1.276 | N. A. | 0.288 | N. A. |
| To be receiving a COMT inhibitor | 2.764 | N. A. | 1.704–4.485 | N. A. | <0.0001 | N. A. |
| To practice regular exercise | 0.488 | N. A. | 0.173–4.908 | N. A. | 0.005 | N. A. |
| To assist regularly to a PD association | 1.024 | N. A. | 0.545–1.922 | N. A. | 0.942 | N. A. |
| Change at V2 (V2 vs. V0) | ||||||
| LEDD | 1.001 | N. A. | 1.000–1.001 | N. A. | 0.093 | N. A. |
| Number of non-antipark. drugs | 1.141 | N. A. | 0.985–1.322 | N. A. | 0.079 | N. A. |
| UPDRS-III (OFF) | 1.03 | N. A. | 1.006–1.054 | N. A. | 0.014 | N. A. |
| UPDRS-IV | 1.109 | N. A. | 1.012–1.216 | N. A. | 0.027 | N. A. |
| FOGQ | 1.137 | 1.305 | 1.075–1.201 | 1.195–1.424 | <0.0001 | <0.0001 |
| PD-CRS | 0.974 | N. A. | 0.954–0.994 | N. A. | 0.011 | N. A. |
| NMSS | 1.009 | N. A. | 1.002–1.015 | N. A. | 0.011 | N. A. |
| BDI-II | 0.993 | N. A. | 0.963–1.024 | N. A. | 0.662 | N. A. |
| PDSS | 0.999 | N. A. | 0.090–1.008 | N. A. | 0.853 | N. A. |
| QUIP-RS | 0.991 | N. A. | 0.964–1.018 | N. A. | 0.494 | N. A. |
| NPI | 1.006 | N. A. | 0.978–1.035 | N. A. | 0.677 | N. A. |
| VAS-PAIN | 1.023 | N. A. | 0.953–1.098 | N. A. | 0.533 | N. A. |
| VASF–physical | 1.025 | N. A. | 0.947–1.109 | N. A. | 0.548 | N. A. |
| VASF–mental | 1.106 | 1.236 | 1.019–1.200 | 1.093–1.379 | 0.016 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos García, D.; de Deus Fonticoba, T.; Cores Bartolomé, C.; Naya Ríos, L.; García Roca, L.; Martínez Miró, C.; Canfield, H.; Jesús, S.; Aguilar, M.; Pastor, P.; et al. Predictors of Loss of Functional Independence in Parkinson’s Disease: Results from the COPPADIS Cohort at 2-Year Follow-Up and Comparison with a Control Group. Diagnostics 2021, 11, 1801. https://doi.org/10.3390/diagnostics11101801
Santos García D, de Deus Fonticoba T, Cores Bartolomé C, Naya Ríos L, García Roca L, Martínez Miró C, Canfield H, Jesús S, Aguilar M, Pastor P, et al. Predictors of Loss of Functional Independence in Parkinson’s Disease: Results from the COPPADIS Cohort at 2-Year Follow-Up and Comparison with a Control Group. Diagnostics. 2021; 11(10):1801. https://doi.org/10.3390/diagnostics11101801
Chicago/Turabian StyleSantos García, Diego, Teresa de Deus Fonticoba, Carlos Cores Bartolomé, Lucía Naya Ríos, Lucía García Roca, Cristina Martínez Miró, Hector Canfield, Silvia Jesús, Miquel Aguilar, Pau Pastor, and et al. 2021. "Predictors of Loss of Functional Independence in Parkinson’s Disease: Results from the COPPADIS Cohort at 2-Year Follow-Up and Comparison with a Control Group" Diagnostics 11, no. 10: 1801. https://doi.org/10.3390/diagnostics11101801
APA StyleSantos García, D., de Deus Fonticoba, T., Cores Bartolomé, C., Naya Ríos, L., García Roca, L., Martínez Miró, C., Canfield, H., Jesús, S., Aguilar, M., Pastor, P., Cosgaya, M., García Caldentey, J., Caballol, N., Legarda, I., Hernández Vara, J., Cabo, I., López Manzanares, L., González Aramburu, I., Ávila Rivera, M. A., ... COPPADIS Study Group. (2021). Predictors of Loss of Functional Independence in Parkinson’s Disease: Results from the COPPADIS Cohort at 2-Year Follow-Up and Comparison with a Control Group. Diagnostics, 11(10), 1801. https://doi.org/10.3390/diagnostics11101801






